Abstract
Over the past two decades, cannabis policies have liberalized in the United States, culminating in the legalization of recreational cannabis in Colorado and Washington state in 2012. This review will focus on the impact of recreational cannabis legalization in Colorado. While the prevalence of past-year and past-month cannabis use has remained relatively steady among adolescents post-legalization, the prevalence of young adult use has continued to rise. Cannabis products with increased potency have become more prevalent and widely used. There are concerns that the use of products with increased potency will increase risk for cannabis use and comorbid mental health disorders, particularly cannabis-induced psychosis and suicidal behavior, although more research is needed to fully understand the impact of high-potency products. Since the legalization of recreational cannabis, numerous additional public health concerns have emerged: unintentional overdoses requiring acute care visits, electronic vaping-associated lung injury, increased motor vehicle collisions related to cannabis consumption, and higher rates of cannabis use during pregnancy. Lessons learned from the first decade of cannabis legalization emphasize the need for research efforts to provide evidence-based guidelines, inform prevention strategies, and implement selective interventions for at-risk populations including youth, individuals with comorbid mental health disorders, and individuals who are pregnant.
Keywords: Cannabis use, Cannabis use disorder, Colorado, Recreational cannabis legalization, THC potency, Youth
Introduction
In the United States, public opinion on cannabis has transformed, leading to gradual changes in cannabis policy at the state level through political processes. To date, 36 states and the District of Columbia have legalized or decriminalized medical cannabis in some form. Additionally, 18 states have legalized recreational cannabis, with Colorado and Washington’s state being the first to do so in 2012. Overall, 68% and 34% of the US population now live in a state with legal access to medical and recreational cannabis, respectively [1]. Over the past decade, the body of literature investigating the impact of recreational cannabis legalization and the effects of cannabis use on youth has grown. Focusing on recreational cannabis legalization in Colorado, we will review regulations to protect youth, increasing cannabis potency and modes of use, the prevalence of cannabis and other substance use, and changing risk perceptions among Colorado youth. Next, we will review the impact of legalization on cannabis use disorder and comorbid mental health problems, including suicidal behavior and cannabis-induced psychosis. We will then explore other public health concerns that have emerged since cannabis legalization.
Cannabis legalization in Colorado
Medical cannabis legalization
In 1975, Colorado reduced charges for possession of cannabis of up to one ounce from a misdemeanor to a petty offense, marking the first re-legalization effort in Colorado history [2]. In 2000, Colorado voters approved Amendment 20, legalizing medical cannabis for specific medical conditions, requiring a prescription from a physician [3]. The United States Deputy Attorney General wrote a memorandum in 2009 to all United States Attorneys recommending low prioritization, or prosecutorial discretion, of enforcement of federal drug laws with considering medical cannabis patients and programs [4]. Near this time, the Colorado state legislature rejected caregiver-patient limits and authorized the creation of medical dispensaries [5]. Following these events, Colorado saw significant increases in the number of applications for medical cannabis per month, from 495 applications in January 2009 to 10,115 applications in December 2009 [3].
The canonization of cannabis as “medicine” by a political process rather than a scientific process presents a unique challenge for clinicians. The state of Colorado has not restricted medical cannabis health or physical benefits claims in advertising or merchandising; however, such claims may not be included on the label or packaging materials (C.R.S. 44-10-203(2)(f), C.R.R. 212-3). Simultaneously, minimal regulatory attention has been given negative health impacts of cannabis use, which dispensaries and providers have not been required to disclose. Perceptions about the benefits of medical cannabis may also be amplified by the hemp industry, which has expanded rapidly across the United States as a natural, herbal source of cannabidiol (CBD), a primary cannabinoid. To date, the impact of industry-sponsored health claims on perceived harm and patterns of cannabis use is unknown.
Legalization of medical cannabis is not associated with increased adolescent marijuana use or CUD whereas it is associated with increases in adults [6]. In Colorado, to obtain a medicinal cannabis license for youth under 20 years old, they must be diagnosed by two physicians from two different medical practices as having a disabling or debilitating medical condition. Prior work has demonstrated that youth with CUD are more likely to seek legal access to cannabis through a medical license, particularly when legal recreational cannabis is not available [7]. Other studies have demonstrated that youth with chronic medical conditions such as inflammatory bowel disease are likely to report cannabis use [8]. Many such youths do report relief of pain as a substantial motivator of use, although they also reported high incidences of CUD. Physicians caring for youth with medical conditions, particularly those associated with pain, should screen for cannabis use, assess the motivations for use including perceived benefit, as well as screen for symptoms of CUD.
Recreational cannabis legalization
Before recreational cannabis legalization, Colorado residents had favorable attitudes towards cannabis and one of the lowest rates of perceived harm in the United States [9]. In 2012, Colorado passed Amendment 64 to legalize possession and retail sales of recreational cannabis [10]. Under this amendment, adults aged 21 years or older are allowed to grow up to six cannabis plants privately (increased to 12 plants in 2018) [11]. Individuals may legally possess all cannabis from the plants they grow at home, legally possess up to one ounce while traveling, and give a gift of up to one ounce of cannabis to other citizens 21 years or older [10]. This law was met with a mixed reception by county legislators: a study of county-level cannabis policies found that only 23.4% of all Colorado counties allowed all types of recreational cannabis facilities and nearly half (48.4%) of Colorado counties prohibited all types of cannabis facilities as of April 1, 2019 [11]. Still, retail sales became available in January 2014 in the permitting counties, cultivating a marketspace for recreational sales of cannabis that has substantially grown. As of June 2020, 2709 licensed cannabis businesses were registered in Colorado, 60% of which were in three counties along the Front Range: Denver, El Paso, and Pueblo [5]. The year 2020 also saw annual record highs for cannabis sales in dispensaries of nearly $2.2 billion, with nearly $400 million in annual tax revenue [12].
Colorado statute distinguishes the licensing of medical and recreational cannabis dispensaries. While there are differences in individual daily sales limits and taxes, cannabis products are generally not exclusive to a category. Recreational cannabis sales comprise the largest proportion of Colorado sales, and most medical users also report recreational cannabis use [13]. Further, nearly three-fourths of adolescents entering substance use treatment report diversion of medical cannabis from registered users [7]. Adolescents who used diverted medical cannabis also reported using cannabis 20 or more days a month, very easy availability, and no friend disapproval of regular cannabis use [14]. Commercialization of cannabis and the implementation of dispensaries is also positively associated with problematic cannabis use in youth [15]. The perceived ease of access among Colorado high school students increased significantly from 46.5 to 52.1% in the first year of commercial sales [16].
Regulations to protect youth
With increasing evidence of the potential adverse effects of cannabis legalization on youth, Colorado has enacted several policies to reduce potential harm to this population. Though it is a dynamic process that has had varying levels of success [17], and many of the nuances of regulations are subject to county-by-county differences, certain measures are enacted statewide:
Legal age limit for purchasing and possession of 21 years old [10].
Regulated cannabis businesses may not exist or advertise on any outdoor sign that is within 500 feet of elementary or secondary schools, places of worship, or public playgrounds [18].
Possession or use of retail cannabis or its products is illegal on all school properties [19].
Each local jurisdiction may allow or ban retail cannabis businesses, regulate the density of retail cannabis shops, and extend limits from locations where children or other vulnerable populations (i.e., substance use treatment programs) are present [20].
Direct advertising to minors is not permitted [21].
To reduce the appeal to minors, Colorado has imposed limits on advertising. Specifically, television, radio, print, or internet ads or sponsorships related to cannabis retail are not permitted unless less than 30% of the audience is under 21 years old [18]. Similarly, outdoor advertising is generally prohibited, and individuals under 21 are not allowed inside dispensaries [18]. While efforts have been made to restrict recreational cannabis businesses and advertising to adult consumers, children and adolescents continue to experience increasing levels of exposure to the acceptability and availability of cannabis through the high prevalence of adult use, coverage and commentary by local media personalities, and presence of dispensaries near major attractions (i.e., sports arenas). Further, most cannabis businesses and dispensaries maintain online and social media presences. Few safeguards were implemented to minimize adolescent exposure and engagement online. Bierut et al. surveyed dispensaries in Colorado and found that only 5% require users to enter one’s birthdate and just over half (54%) require the user to affirm minimum age requirements by clicking “yes” [21]. Young adults aged 20–29 years old are the most common demographic to follow cannabis social media profiles, with 15% of followers being younger than 20 years old.
Other regulatory initiatives to prevent youth cannabis use in the community include criminal statutes targeting the provision of cannabis to minors by adults who are older than the youth by at least 2 years (Colorado Senate Bill 13-250) [22]. Moreover, the Colorado state legislature developed marijuana tax-funded youth outreach programs (Senate Bill 14-215), including the YESS Institute, a marijuana tax-funded afterschool program to enhance positive youth development, social/emotional learning, and education about cannabis use (www.yessinstitute.org) [23]. Other tax-funded programs include the High Costs Campaign, an advertising campaign to adolescents in Colorado about cannabis-related risks and facts (www.thehighcosts.com), and the Colorado Department of Public Health and Environment Retail Marijuana Education Program [23]. As these programs yield information on their longer-term effectiveness of preventing youth cannabis use, lessons will be learned on how to best protect Colorado youth from the potential harms related to cannabis legalization.
Early lessons from cannabis edibles
Initially, there was little regulation of edibles’ labeling, packaging, or manufacture in Colorado following the rollout of recreational sales [24]. One of the earliest and most urgent consequences of cannabis sales and commercialization in Colorado was a sharp rise in unintentional overdoses in adolescents and adults and symptomatic ingestion by children. Following the surge in individuals receiving medical cannabis in Colorado, there was a significant increase in emergency department visits for children less than 12 years old for cannabis exposure at an academic tertiary pediatric hospital in Colorado, with 57% of these cases being due to exposure to edibles [25]. Additionally, Colorado regional poison center cases for pediatric cannabis increased significantly and more than the national average from 2009 to 2015, with significant increases in pediatric cannabis exposures in the 2 years following recreational legalization [26].
In response to unintentional overdoses, new standard serving size and packaging requirements for edible products were enacted [27]. Colorado statute now requires a maximum THC dose equivalent of 10 mg per serving, with clear packaging and demarcation of servings, and a maximum content of 100 mg or less per package. Cannabis products must be sold and leave the store in child-resistant packaging and must not use images or cartoons that appeal to children. Packaging of edibles must also display the Universal Symbol for cannabis and require wording that the consumer may not feel the effects of THC intoxication for two or more hours after consumption [24]. Subsequently, the state-required testing for THC concentration for recreational cannabis edibles [28]. Warning labels are similarly required for cannabis product packaging, including statements about health risks, that the product was produced without regulatory oversight, warnings about driving while intoxicated with cannabis, and that the product is intended for use by individuals aged 21 years or older, among others [24].
Cannabis potency and modes of use
Perhaps the most significant impact of recreational cannabis legalization to date is the sharp increase in cannabis potency, products, and modes of use. Over the past two decades, Δ9-tetrahydrocannabinol (THC) potency, THC:cannabidiol (CBD) content, and products and modes of use have changed significantly [29-32]. State-regulated markets now offer flower products that are twice as potent as black-market flower products available just before recreational legalization (20–25% THC) [33, 34]. Further, licensed dispensaries also offer high-concentrate products that are up to four times more potent than dispensary flower and over seven times more potent than black-market flower (80–90% THC). Sampled concentrates as part of the state’s monitoring system routinely have THC concentrations as high as 90–95% [35].
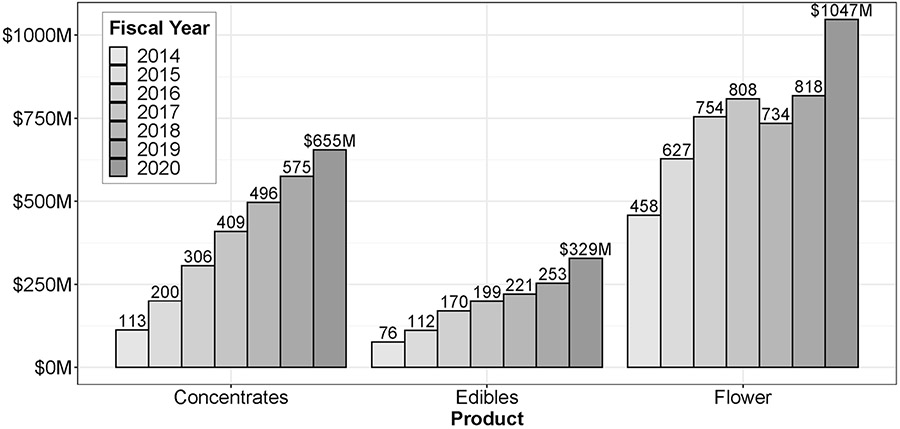
Since legal markets opened in Colorado, annual concentrate sales have increased by 480% (from $113 million up to $655 million), whereas flower sales have increased by 129% and edible sales have increased by 332% (Fig. 1). Whereas concentrates made up just 17% of the market in 2014, they now make up 32% in Colorado. Adolescent concentrate use appears to be common and may have significant psychosocial effects (for review, see Bidwell et al. [36]). Adolescents who report lifetime concentrate use (24%) make up 72% of those who report lifetime use of any cannabis product (33%) [37].
Fig. 1.
Annual cannabis sales in Colorado from 2014–2020 by product type. Annual sales in United States dollars (millions) is presented for concentrates, edibles, and flower-based products
The Colorado Department of Public Health and Environment (CDPHE) conducts a biennial survey of high school students, the Healthy Kids Colorado Survey (HKCS). While low response rates have impacted the survey over the past few years, important use patterns have emerged. In 2017, 35.6% of adolescents reported ingesting edibles, while 34.4% reported dabbing and 20.3% reported vaping. From 2015 to 2017, the use of high-concentrate cannabis products by dabbing (7.6%) or ingesting edibles (9.8%) as the primary method of consumption increased to their highest levels (from 4.3 and 2.1%, respectively) [38]. Adolescents who identify as male were more likely to report vaping, dabbing, and ingesting edibles [39]. Edible use was also more common among youth who wanted to discretely consume cannabis in public, including at school [40]. The prevalence of vaping was found to be highest among Asian and White adolescents, and vaping was associated with the diversion of marijuana from a person with a medical marijuana card (OR 3.4, 95% CI 2.0–5.6) [40].
Prevalence of cannabis use in youth
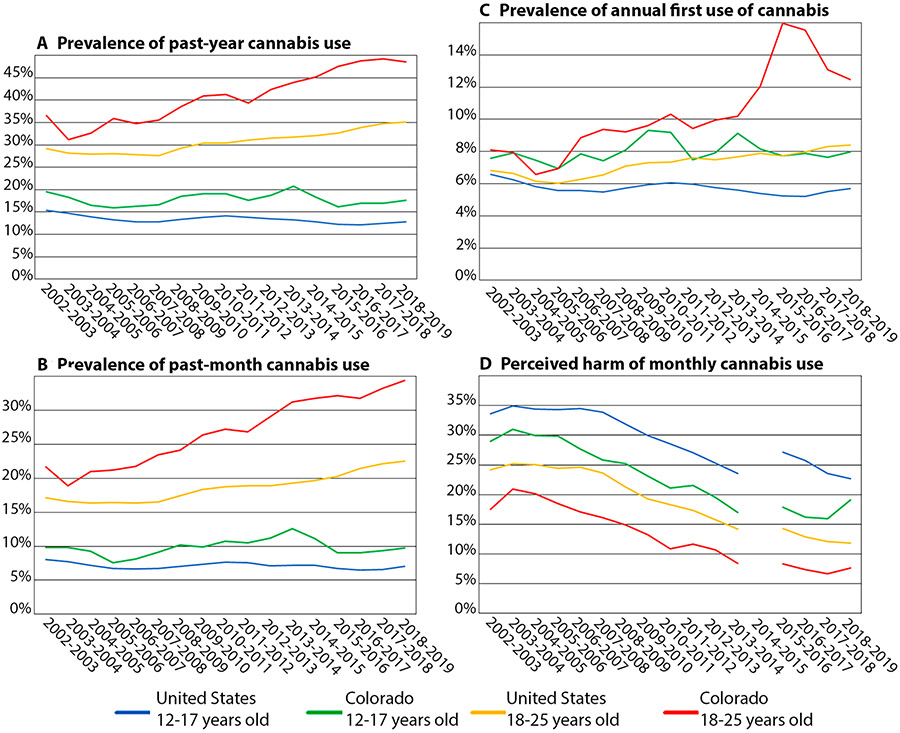
To date, research on the impact of recreational cannabis legalization on the prevalence of cannabis use among youth has demonstrated relatively stable prevalence among adolescents younger than 18 years old and increasing prevalence among young adults aged 18–25 years old [41]. The National Survey on Drug Use and Health (NSDUH) is conducted annually by the Substance Abuse and Mental Health Services Administration (SAMHSA) and surveys individuals aged 12 years old and older, allowing investigation of trends among youth [42]. The prevalence of cannabis use in adolescents aged 12–17 years old has remained relatively steady over the past two decades, though both the rates of past-year (17.6% vs. 12.8%) and past-month cannabis (9.8% vs 7.0%) use are notably higher in Colorado compared with the United States (Fig. 2a, b). Past-month cannabis use among Colorado youth aged 12–17 years old is 43% higher than the national average [43].
Fig. 2.
Prevalence of cannabis use and perceived harm in youth in Colorado compared to the United States in the NSDUH. Prevalence of a past-year cannabis use, b past-month cannabis use, and c annual first use of cannabis, as well as d perceived harm of monthly cannabis use, are presented from 2002 to 2019. Red: Colorado young adults aged 18–25 years old. Yellow: United States young adults (including Colorado) aged 18–25 years old. Green: Colorado adolescents aged 12–17 years old. Blue: United States adolescents (including Colorado) aged 12–17 years old. For perceived harm of monthly cannabis use (d), there is a one-year gap between 2014 and 2015 in data reported in the NSDUH
These findings are consistent with the analysis of MTF, a biennial survey of substance use among 8th, 10th, and 12th grade students, which found that states with legalized medical marijuana have a higher prevalence of adolescent marijuana use compared with states where marijuana is not legal (15.87% vs 13.27%, OR 1.27, 95% CI 1.07–1.51, p = 0.0057) [44, 45]. The prevalence of daily or almost daily users is also higher among Colorado adolescents than the national average [46]. Additionally, 80% of cannabis consumption may be accounted for by only 20% of users by some estimates [47].
Interestingly, in the HKCS, the highest rates of past 30-day cannabis use are observed among high school juniors and seniors (26.3% and 27.8%, respectively, followed by young adults aged 18–25 (26.1%) [48]. Adolescents who identify as gay, lesbian, or bisexual (30.9%), adolescents who identify as mixed race (27.1%), and adolescents who identify as Native Hawaiian or Pacific Islander (23.1%) reported a higher prevalence of past 30-day cannabis use. Other risk factors associated with past 30-day use include male gender, older age, lower perceived harmfulness or wrongfulness, earlier age of initiation (≤ 13 years old), and current cigarette or alcohol use [40]. While medical and recreational cannabis legalization has not been associated with further increases in the prevalence of adolescent cannabis use [9, 38, 46], the impact of acceptability and availability resulting in a culture of legalization is unknown.
Though steady in adolescents, the prevalence of cannabis use is increasing for young adults aged 18–25 years old, who, though often understudied in cannabis policy and research, remain at risk of the detrimental impact of cannabis use through the completion of neurodevelopment during young adulthood. Among NSDUH respondents, the prevalence of past-year and past-month cannabis use has increased in the United States over the past two decades, with a more rapid increase in Colorado (Fig. 2a, b). In 2019, the most recent NSDUH results are comparable to previous years, the prevalence of past-month cannabis use is at its highest level in Colorado and the United States (34.4% and 22.5%, respectively), with similarly high trends in past-year prevalence (48.5% and 35.1%, respectively) [42].
Per analysis of HKCS, the age of first use of cannabis has remained steady since 2013, with 82.1% first using cannabis before the age of 16 years [48]. This is consistent with results from NSDUH, which show a prevalence of annual first use of cannabis is higher among Colorado adolescents aged 12–17 years old compared to US peers (8.0% vs 5.7%, respectively), though relatively stable over the past two decades (Fig. 2c). As with the prevalence of past year and past 30-day cannabis use, a more concerning trend emerges among young adults, among whom the prevalence of annual first use of cannabis has increased among young adults aged 18–25 years old, with a more rapid rise among Colorado young adults (12.5% in Colorado vs. 8.4% in the US; Fig. 2c).
Risk perceptions
Overall, as recorded in the NSDUH, there has been a steady decline in perceptions of harm from cannabis use among youth in Colorado and the broader US (Fig. 2d). Risk perceptions also differ between cannabis products. In the 2013 HKCS, adolescents that endorsed lower perceived harmfulness were more likely to use combustible cannabis products, whereas adolescents who reported higher perceived harmfulness were more likely to report ingesting edibles or vaping [40]. By 2015, adolescents who reported higher perceived harm, wrongfulness, or parental disapproval were not associated with the prevalence of using combustible cannabis products, whereas these factors were associated with a lower prevalence of other modes of use, including edibles, vaping, and dabbing [39]. Further, in a survey of Colorado young adults aged 18–26 years old, Popova et al. found that combustible products were perceived as more dangerous than vaporizers and edibles [49]. Popova also found that the risk of unintentional overdose with higher potency products was perceived to be lower than the health risks of using combustible cannabis.
Use of other substances
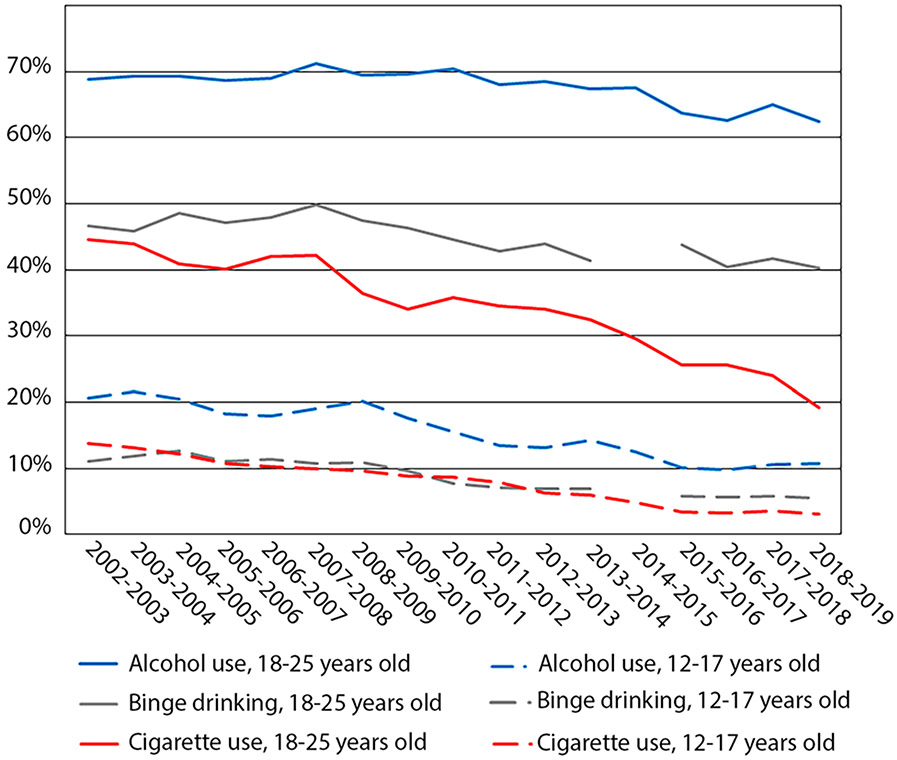
Adolescent cannabis use is associated with more frequent use of other substances and illicit drugs [50]. However, the impacts of recreational and medical cannabis laws on youth substance use are not well understood. In the two decades before cannabis legalization, steady declines have been observed in MTF for the prevalence of substances used measured among United States 8th, 10th, and 12th grade students, except for cannabis use and vaping [51]. In Colorado, youth tobacco and alcohol use has declined over the past two decades, similar to national trends (Fig. 3) [42]. One argument supporting cannabis legalization is a substitution, particularly for opioids, and a possible subsequent decrease in opioid overdose deaths. Unfortunately, opioid deaths have risen in Colorado through the period of legalization and continued to rise to an all-time high in 2019 [43].
Fig. 3.
Prevalence of past month alcohol use, binge drinking, and tobacco use in youth in Colorado in the NSDUH. The prevalence of past-month alcohol use (blue), binge drinking (gray), and tobacco use (red) is presented from 2002 to 2019 for young adults aged 18–25 years old (solid lines) and adolescents aged 12–17 years old (dashed lines). For the past month binge drinking (gray), there is a 1-year gap between 2014 and 2015 in data reported in the NSDUH
Cannabis use disorder
Before recreational cannabis legalization, studies found that regular adolescent cannabis use with onset before the age of 17 years old was associated with an increased risk of cannabis dependence through young adulthood [50]. Following the legalization of medical cannabis, higher rates of adolescent cannabis use disorder (CUD) were reported in Colorado [52]. Recently, Mennis and Stahler investigated CUD admission trends for adolescents aged 12–17 from 2008 to 2017 utilizing a national treatment database (Treatment Episode Data Set: Admissions, TEDS-A) comparing Colorado and Washington state to states where recreational cannabis use remains illicit [41]. This report showed treatment admission rates for CUD declined significantly across the United States, including Colorado and Washington. Taken together, it remains unclear if cannabis legalization is associated with an increased prevalence of CUD in adolescents.
Comorbid mental health disorders
Similar to CUD, the impact of cannabis legalization on comorbid mental health disorders remains understudied and unclear. A number of adolescents in the clinic report using cannabis to “self-medicate” depression, anxiety, trauma symptoms, and sleep problems. Among adults, in states with medical cannabis legalization, it appears to be more common to use cannabis to self-medicate psychiatric symptoms [53]. Further, Coloradans with a mental health condition are more likely to self-report cannabis use than Coloradans without a mental health condition [53]. Acute encounters of mental health disorders and cannabis use have also increased since recreational cannabis legalization. Colorado has experienced a five-fold greater prevalence of mental health diagnoses in Emergency Department (ED) visits associated with cannabis use between 2012 and 2014 [54]. There has also been a significant increase in adolescent cannabis-associated ED and urgent care visits experienced at Colorado children’s hospital from 2005 to 2015, resulting in 4202 episodes of care. Of those, 62% were diagnosed with cannabis use or problematic use and 71% received a comorbid psychiatric diagnosis, most commonly depression (39%) or mood disorder (22%) [55]. While more recent data are not available, these trends in comorbid mental health disorders and cannabis use are concerning and warrant further investigation.
Age of first marijuana use may be an important determinant of later mental health outcomes, often resulting in overall lower levels of psychological well-being [56]. Further, adolescent-onset cannabis exposure has been associated with dose-dependent increases in mood disorders, including depression, and an overall worse course of illnesses [57]. While many youths self-report using cannabis to ‘self-medicate’ anxiety, however, it does not always alleviate symptoms and cannabis may be anxiogenic at higher doses [57]. Cross-sectional and longitudinal studies have shown that adolescent and young adult cannabis users are at increased risk for anxiety and panic attacks [57]. A particular subset of youth with attention-deficit/hyperactivity disorder (ADHD) is especially vulnerable to substance use disorders, including earlier onset and increased severity. It is estimated that youth with ADHD are 7.9 times more likely to consume cannabis than those without ADHD [58].
Suicidal behavior
Suicide attempts are among the most serious mental health events associated with cannabis use in youth. Previous research has shown that regular adolescent cannabis use is associated with an increased risk of suicide attempts [50]. The suicide rate has increased in Colorado over the past 15 years, and the percent of suicides with cannabis present in the toxicology report has increased nearly threefold from 2006 to 2018 to a high of 23.3% [43]. Among youth aged 10–19 years old, cannabis is the most commonly identified substance (22%) and twice as common as alcohol (10%), whereas alcohol remains the most common substance identified on toxicology report in adults aged 20 years old or older (40% alcohol vs. 19% cannabis) [43].
While suicide rates and the percent testing positive for cannabis have both increased, research is inadequate to determine the role of cannabis in suicidal behavior or the impact of cannabis legalization. Analysis of the YRBS from 2011 to 2017 found cannabis use was most strongly associated with attempted suicide for adolescents using 1–2 days per month up to 20 or more days a month (prevalence ratio 1.98–4.51, respectively), attempted suicide (prevalence ratio 1.65–2.64, respectively), planned suicide (prevalence ratio 1.43–1.62, respectively), and seriously considered suicide (prevalence ratio 1.32–1.54, respectively) [59]. Notably, frequent cannabis use was significantly associated with a higher prevalence of each category of suicidal behavior, and effects were consistent with a dose–response effect.
Cannabis-induced psychosis
A second mental health outcome of particular concern is cannabis-induced psychosis. Over the past three decades, clinical research has identified a temporal association between cannabis use and psychosis [60-62]. It should be noted that most youth who use cannabis will not develop signs or symptoms of psychosis; the incidence of cannabis-induced psychosis is unknown. However, due to ongoing neurodevelopment, youth are particularly vulnerable to the adverse effects of cannabis [63]. The clinical course of cannabis-induced psychosis is variable in adolescents. While many adolescents achieving full remission in abstinence, some experience recurrent psychosis with continued cannabis use or develop early-onset schizophrenia. Yet, others developing treatment-refractory psychosis even when abstinent and residing in a restrictive setting (i.e., hospital or residential facility). Review of the literature has identified risk factors associated with cannabis-induced psychosis, including familial risk for psychosis or schizophrenia [64, 65] and high THC potency, duration of use, and initiation of marijuana use at a younger age [66-74]. As reviewed by Bagot et al., initiation of cannabis use in adolescence is associated with early-onset psychotic disorders, a worse course of illness, and poorer functional outcomes in a dose-dependent manner [75].
Education
Following recreational cannabis legalization, there was concern that high school graduation rates would decrease. Daily users before age 17 years had clear reductions in the odds of high-school completion (adjusted odds ratio 0.37, 95% CI 0.20–0.66) and degree attainment (0.38, 0.22–0.66) [50]. However, over the past decade, graduation rates have increased from 72.4% to a high of 81.9% in 2019–2020 [76]. Similarly, over this period, dropout rates have continued to decline from 3.0 to 1.8% in 2019–2020. To date, the impact of recreational cannabis legalization on academic achievement, post-secondary education, and employment is unknown.
Legal consequences
Cannabis-related offenses in Colorado schools peaked in 2014 at 1654 offenses and have remained relatively stable over the past 3 years [76]. Cannabis is also the number one reason for law enforcement contact with students, accounting for 24% of all contacts in 2018–2019 (1533 summons and 43 arrests). Of all school disciplinary incidents in the 2019–2020 school year, cannabis accounted for 5% of suspensions, 30% of expulsions, and 34% of law enforcement referrals [76]. For substance-related school disciplinary incidents, cannabis accounted for 70% of suspensions, 59% of expulsion, and 77% of law enforcement referrals. In 2012, Colorado passed legislation (Senate Bill 12-046 and House Bill 12-1345) to modify zero-tolerance policies and keep more students in school (66). Since that time, the drug expulsion rate has declined to its lowest level, whereas drug suspensions initially increased and have subsequently remained relatively stable [76].
In lieu of mandatory sentencing guidelines for adolescent cannabis offenses, most individuals are referred through juvenile diversion programs. The primary goal of diversion is to prevent recidivism among adolescents. Adolescents receive mental health and substance use disorder screening. Treatment and substance use monitoring by urine drug screen may be mandated by the court. Diversion programs are supported by state funds, as well as state and federal grants and marijuana tax cash fund awards [77]. Factors associated with decreased recidivism include receipt of restorative services; high levels of connection to an adult family member; and increase in protective services including a sense of accountability, self-esteem, locus of control, and connection to familial and non-familial adults and the community [78].
Other public health concerns
Acute care visits
In addition to increased emergency department/urgent care (ED/UC) visits for children, Colorado youth are also accessing emergency services due to cannabis use at higher rates. Past-year ED visits with cannabis-related ICD-10 codes are the highest among young adults aged 18–25 years old, and hospital admissions are highest among youth aged 9–17 years old [38]. Studies assessing adolescent ED/UC visits for cannabis-related concerns show similar trends, with rates increasing from 1.8/1000 ED/UC visits in 2009 to 4.9/1000 ED/UC visits in 2015 [55]. Cannabis abuse was the most common discharge ICD code (62%), and a comorbid psychiatric diagnosis was made for 71% of the visits [55].
Electronic vaping-associated lung injury
Recently, there has been increasing concern about marijuana-related lung injuries, particularly in otherwise healthy youth. Initial concerns favored chronic bronchitis with cannabis use, for which there is no evidence [79]. However, cannabis use is also associated with acute lung injuries. In 2018, three cases of adolescent males with acute cannabis-related lung injuries were reported with eosinophilic pneumonia, silica-induced pneumoconiosis, and acute hypersensitivity pneumonitis associated with recent cannabis use [80]. In 2019, there was a multistate outbreak of electronic vaping-associated lung injuries (EVALI) in the United States, including 805 cases and 12 deaths [81, 82]. These cases predominantly consisted of acute lung injuries, often necessitating intensive care interventions and intubation, in previously healthy individuals [81-83]. Over half of patients were youth younger than 25 years old (54.2%), with an additional quarter of patients (23.9%) of aged 25–34 years old. The Centers for Disease Control (CDC) revealed that 77% of patients used THC-containing products in the 30 days preceding the onset of symptoms. Subsequent analyses of recovered cartridges implicated vitamin E acetate, a diluent used in some cannabis oil products [84].
Motor vehicle collisions
An important public health concern related to cannabis legalization is the potential for increased cannabis-impaired driving. Studies have demonstrated that cannabis use affects motor and cognitive skills essential to driving [15], particularly among those who use cannabis occasionally as they may have less tolerance for THC [85]. Though the overall percent of adolescents reporting driving when they have been using cannabis or riding in a vehicle driven by someone using cannabis remained steady from 2011 to 2017 (21.7% in 2011; 19.7% in 2017) [14], cannabis-impaired driving among adults remains a public health concern that may be influenced by cannabis legalization and, more specifically, cannabis commercialization. For instance, medical cannabis legalization has been associated with a near doubling of the prevalence of driving while under the influence of cannabis [17]. However, it was not until the commercialization of medical cannabis in Colorado in mid-2009 that fatal motor vehicle crashes with drivers who were cannabis-positive increased significantly (5.9% in early 2009 to 10% at the end of 2011)—an increase not seen in states that did not adopt medical cannabis legalization [18]. Similar trends were observed following the start of recreational sales in 2014: the number of driving-under-the-influence (DUI) citations in which cannabis was the identified impairing substance increased 16% between 2014 and the first ten months of 2016 [20]. Additionally, fatalities in which the driver tested positive for cannabinoids increased by 80% between 2013 and 2015 in Colorado [15].
Use during pregnancy
Cannabis use during pregnancy and while breastfeeding has increased since recreational cannabis legalization [38]. More broadly, women in states where cannabis is legal are more likely to use cannabis in pregnancy than women in non-legal states [86]. Cross-sectional data from the 2014–2015 Colorado Pregnancy Risk Assessment Monitoring System (PRAMS) estimated the prevalence of cannabis use during pregnancy to be approximately 5.7% in Colorado, greater than the national estimates of 3.8% [87]. Furthermore, among women in CO who have ever used cannabis, 35.8% reported use during pregnancy [88]. The highest rates of cannabis use during pregnancy are among young women who themselves are vulnerable to cannabis use during neurodevelopment: adolescents aged 15–19 years old (13.3%), followed by young adults aged 20–24 years old (12.3%) [89]. Cannabis use is also more common among women with unintended pregnancies than planned pregnancies (10.4% vs 4.1%). In 2018, a statewide study found that 70% of dispensaries recommended using cannabis products for morning sickness [89]. Further, some medical providers in Colorado recommend cannabis to pregnant women, despite opposition by the American College of Obstetricians and Gynecologists [90].
Discussion
Over the past two decades, cannabis policies have become more permissive in the United States, culminating in the commercialization of recreational cannabis. As one of the first states to legalize recreational cannabis, Colorado started with minimal industry regulation and intervention by the state government. This may have been at the expense of Colorado youth, who ranked last in the priorities of regulators and stakeholders as the groundwork was established for recreational cannabis sales [91]. While cannabis use has remained stable among Colorado adolescents, the prevalence has increased among young adults, who continue to remain at risk of the neurodevelopmental consequences of cannabis use. Further, Colorado youth of all ages use at higher rates compared to the United States. However, one notable limitation of cannabis legalization research is that prevalence is not a sufficient surrogate measure of the frequency of cannabis use or the quantity of cannabis consumed by individuals. Thus, it remains unknown if cannabis legalization is associated with other changes in patterns of cannabis use.
One of the principal effects of recreational cannabis legalization has been commercialization, which resulted in unprecedented THC concentrations nearing 25% in flower-based products 95% in concentrate products. Of particular concern, the THC:cannabidiol (CBD, THC:CBD) ratio has increased sharply from 14:1 to more than 80:1 [92]. THC, which mediates the intoxicating effect of cannabis, is a cannabinoid receptor partial agonist [93]. Conversely, CBD is a cannabinoid receptor antagonist. It is hypothesized that CBD exerts some neuroprotective effects against the negative impacts of THC. To date, the neurodevelopmental, addiction, and mental health impacts of high THC products remain unknown [94]. Along with the rise in THC potency, product availability and modes of use have also changed, with increased prevalence of high concentrate products including vaping, edibles, and wax.
To date, the effectiveness of cannabis regulations and policies has not been studied in Colorado. Under-regulation of the cannabis industry, however, resulted in variable and undisclosed product potency and increased unintentional overdoses among all age ranges. It is important for regulatory agencies to consider mandated potency testing, product labeling, and packaging to enhance consumer protections. The average consumer is not able to quantify the potency of cannabis nor the amount consumed at one time. While there is a cap on THC content per serving for edibles, the same guidelines should be considered for other cannabis products. For example, anecdotally, cannabis industry representatives in Colorado recommend a serving size of half a grain of sand for wax, whereas many youth reports using one or more teaspoons of wax at a time. THC potency caps have not been implemented in Colorado, though such measures may provide further consumer protections and emphasize the health concerns of high-potency THC products.
Throughout the stages of cannabis legalization, there have also been notable decreases in perceived risks of cannabis. Recreational cannabis legalization has resulted in increased exposure to cannabis in a socially acceptable perspective [41]. One possible determinant of perceived harm may be counterbalancing claims of health benefits. Because cannabis is often described as “natural” and medical uses are canonized in medical cannabis policies and may be publicly touted, many youths view it as less harmful and less addictive than other drugs and medications including anti-depressants, anxiolytics, and opioids [49]. Further, Bierut et al. surveyed licensed cannabis retailers and found that the majority in Colorado made health claims regarding cannabis use [21]. This is particularly concerning as Colorado statutes expressly forbid cannabis retailers from making or promoting health claims. Conversely, none of the retail stores listed harmful or adverse effects of cannabis use.
Colorado statute does require cannabis products to be labeled with the following warning statements: “This product was produced without regulatory oversight for health, safety, or efficacy” and “There may be long term physical or mental health risks from use of marijuana including additional risks for women who are or may become pregnant or are breastfeeding. Use of marijuana may impair your ability to drive a car or operate machinery” [95]. However, as reviewed herein, numerous specific safety concerns have emerged including CUD, comorbid mental health disorders, suicidal behavior, cannabis-induced psychosis, risk of overdose or other effects requiring acute care management, EVALI, and neurodevelopmental risks to unborn children exposed in utero. Further, a recent review by Volkow et al. identified the following risks with a high level of confidence: addiction to cannabis and other substances, diminished lifetime achievement, motor vehicle accidents, and symptoms of chronic bronchitis [79]. Other risks with a moderate level of confidence include abnormal brain development, progression to use of other drugs, schizophrenia, and depression or anxiety. While many warnings are associated with cannabis use and further studies are needed, it remains vital to provide evidence-based guidance to consumers in the form of direct, specific warnings.
In addition, selective interventions should be developed to educate populations most at risk of the adverse consequences of cannabis use, including youth. As noted above, risk perceptions have decreased significantly among youth. Risk perceptions influence product selections to avoid combustible products or conceal use. However, many youth do not recognize signs or symptoms of CUD, nor do they recognize harms of frequent cannabis use. As reported by Silins et al., daily use of cannabis before age 17 years old is associated with decreased odds of completing school or attaining a degree, development of CUD, use of other illicit drugs, and suicide attempt [50]. One challenge presented by changing perceptions of cannabis harm and acceptability may be shifting attitudes toward treatment and decreased treatment-seeking behaviors.
While access to substance use treatment is wholly inadequate, youth seldom recognize symptoms of problematic cannabis use. In a study of perceived harm Popova et al. found that many respondents could describe physiologic changes due to regular cannabis use, though they generally did not identify these signs of tolerance as indicative of problematic use or CUD [49]. However, many discussed using higher potency products or higher amounts to overcome these physiologic changes to achieve getting high. Further, few respondents reported withdrawal symptoms. More research is needed to understand barriers to engaging youth into treatment and to develop harm reduction strategies in which youth with problematic cannabis use may be more willing to engage [96]. Diversion programs should also be considered a necessary component of addressing problematic cannabis use and substance-using behaviors and crimes among youth. Such programs in Colorado have proven effective to engage adolescents in substance use and mental health treatment and decrease recidivism rates.
A second at-risk population that would benefit from targeted educational resources and selective interventions consists of individuals with comorbid mental health disorders. Prior to recreational cannabis legalization, numerous studies established associations between cannabis use and multiple mental health disorders and adverse outcomes, of which suicidal behavior and cannabis-induced psychosis are the most concerning. Approximately 33% of adolescents with a substance use disorder and 80% of adolescents entering treatment for a substance use disorder also have another comorbid mental health disorder [97]. Co-occurring substance use and psychiatric disorders have poorer treatment outcomes, earlier time to episodes of return to use, and increased treatment dropout. However, the mechanism by which comorbid disorders interact with problematic cannabis use remains unclear [98-100].
The most common mental health disorders associated with CUD include depression and anxiety disorders, psychosis, and earlier onset of mania than youth who do not use cannabis [101]. There are overlapping symptoms which may contribute to the maintenance of comorbid disorders, including a motivational state, loss of energy, affective flattening, and lower overall relationship and life satisfaction [102]. Notably, quasi-experimental family-controlled study designs support an elevated risk of suicidality and non-suicidal self-injurious behavior associated with cannabis use [103-107]. Further, some evidence suggests that adolescents who use concentrates are more likely to report paranoia [108], consistent with studies finding that frequent, high-THC cannabis use is associated with earlier psychosis onset than lower-THC cannabis used at a similar frequency [67].
Unborn children of women who are pregnant or may become pregnant comprise a third at-risk population. The prevalence of cannabis use has increased among pregnant women, with the greatest increases in adolescents and young women. It is concerning that medical professionals and cannabis dispensaries continue to recommend cannabis use given the mounting evidence of negative consequences to the unborn child. Perinatal exposures to cannabis are of concern as they have been associated with decreased IQ, impaired cognitive function, and attentional capabilities in children [109, 110]. THC rapidly crosses the placenta, with cord blood THC levels measured three to six times lower than that found in maternal blood, though there is greater transfer early in pregnancy, when the fetus may be most vulnerable to the neurodevelopmental consequences of cannabis exposure [111].
In conclusion, cannabis policies have evolved through political processes that have outpaced and, in some cases, superseded scientific research. The prevalence of cannabis use should not be the only, nor is it an adequate, public health measure of the impact of cannabis legalization. Little is known about the frequency of cannabis use among youth in more permissive regions. Further, increases in THC potency and changes in modes of use continue to severely outpace cannabis research. It is vital for the medical and research communities to conduct studies that will provide evidence to inform future policies and regulations. Particularly as the need for adolescent addiction psychiatric care has exceeded systems capacity, evidence-based prevention and selective intervention strategies are imperative to help protect youth and other at-risk populations in this changing cannabis landscape.
Funding
Dr. Hinckley was supported by the National Institute on Drug Abuse (NIDA) “AACAP Physician Scientist Program in Substance Use” (K12DA000357). Dr. Bhatia was supported by a postdoctoral T32 (T32 MH015442). Dr. Hopfer was supported by NIDA grants R01DA042744 and R01DA032555.
Footnotes
Conflict of interest The authors have no real or perceived conflicts of interest or competing interests to report.
Consent for publication The authors give consent for publication of this work.
Reference
- 1.Carnevale J, Kagan R, Murphy P, Esrick J (2017) A practical framework for regulating for-profit recreational marijuana in US States: lessons from Colorado and Washington. Int J Drug Policy 42:71–85. 10.1016/j.drugpo.2017.03.001 [DOI] [PubMed] [Google Scholar]
- 2.Breathes W (2012) The history of cannabis in Colorado…or how the state went to pot. Westword. https://www.westword.com/news/the-history-of-cannabis-in-coloradoor-how-the-state-went-to-pot-5118475. Accessed 22 Nov 2021 [Google Scholar]
- 3.Davis J, Mendelson B, Berkes J, Suleta K, Corsi K, Booth R (2016) Public health effects of medical marijuana legalization in Colorado. Am J Prev Med 50(3):373–379. 10.1016/j.amepre.2015.06.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden D (2009) Memorandum for selected United States attorneys: Investigations and prosecutions in states authorizing the medical use of marijuana. US Department of Justice, Office of the Deputy Attorney General. https://www.justice.gov/sites/default/files/opa/legacy/2009/10/19/medical-marijuana.pdf. Accessed 1 Oct 2021 [Google Scholar]
- 5.Reed J (2021) Impacts of marijuana legalization in Colorado: A report pursuant to C.R.S. 24-33.4-516. Colorado Division of Criminal Justice Department of Public Safety. https://cdpsdocs.state.co.us/ors/docs/reports/2021-SB13-283_Rpt.pdf. Accessed 22 Nov 2021 [Google Scholar]
- 6.Leung J, Chu C, Stjepanovic D, Hall W (2018) Has the legalisation of medical and recreational cannabis use in the USA affected the prevalence of cannabis use and cannabis use disorders? Curr Addict Rep 5(4):403–417 [Google Scholar]
- 7.Salomonsen-Sautel S, Sakai J, Thurstone C, Corley R, Hopfer C (2012) Medical marijuana use among adolescents in substance abuse treatment. J Am Acad Child Adolesc Psychiatry 51(7):694–702. 10.1016/j.jaac.2012.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffenberg E, Newman H, Collins C, Tarbell S, Leinwand K (2017) Cannabis and pediatric inflammatory bowel disease: change blossoms a mile high. J Pediatr Gastroenterol Nutr 64(2):265–271. 10.1097/mpg.0000000000001393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cerda M, Wall M, Feng T, Keyes K, Sarvet A, Schulenberg J, O’Malley P, Pacula R, Galea S, Hasin D (2017) Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr 171(2):142–149. 10.1001/jamapediatrics.2016.3624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hickenlooper G (2014) Experimenting with pot: the state of Colorado’s legalization of marijuana. Milbank Q 92(2):243–249. 10.1111/1468-0009.12056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Payan D, Brown P, Song A (2021) County-level recreational marijuana policies and local policy changes in Colorado and Washington state (2012–2019). Milbank Q. 10.1111/1468-0009.12535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ricciardi T (2021) Colorado marijuana sales hit $2.2 billion in highest-selling year yet. Denver Post. https://www.denverpost.com/2021/02/09/colorado-cannabis-2020-record-sales-year-2-billion/. Accessed 22 Nov 2021 [Google Scholar]
- 13.Pacula R, Jacobson M, Maksabedian E (2016) In the weeds: a baseline view of cannabis use among legalizing states and their neighbours. Addiction 111(6):973–980. 10.1111/add.13282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thurstone C, Lieberman S, Schmiege S (2011) Medical marijuana diversion and associated problems in adolescent substance treatment. Drug Alcohol Depend 118(2–3):489–492. 10.1016/j.drugalcdep.2011.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pacula R, Powell D, Heaton P, Sevigny E (2015) Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manag 34(1):7–31. 10.1002/pam.21804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harpin S, Brooks-Russell A, Ma M, James K, Levinson A (2018) Adolescent marijuana use and perceived ease of access before and after recreational marijuana implementation in Colorado. Subst Use Misuse 53(3):451–456. 10.1080/10826084.2017.1334069 [DOI] [PubMed] [Google Scholar]
- 17.Subritzky T, Lenton S, Pettigrew S (2019) Cannabis and youth protection in Colorado’s commercial adult-use market: a qualitative investigation. Int J Drug Policy 74:116–126. 10.1016/j.drugpo.2019.09.007 [DOI] [PubMed] [Google Scholar]
- 18.Marijuana Enforcement Division (2020) Colorado marijuana rules: 1 CCR 212-3. https://www.sos.state.co.us/CCR/GenerateRulePdf.do?ruleVersionId=8439. Accessed 22 Nov 2021
- 19.Jahn C et al. (2013) Senate bill 13–283. https://cdpsdocs.state.co.us/ccjj/Resources/Leg/Mandates/SB13-283.pdf. Accessed 22 Nov 2021 [Google Scholar]
- 20.City and County of Denver (2021) Council bill no. CB21-0216. https://www.denvergov.org/files/assets/public/business-licensing/documents/marijuana-omnibus-bill.pdf. Accessed 22 Nov 2021
- 21.Bierut T, Krauss M, Sowles S, Cavazos-Rehg P (2017) Exploring marijuana advertising on weedmaps, a popular online directory. Prev Sci 18(2):183–192. 10.1007/s11121-016-0702-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flick P (2017) Analysis of senate bill 13-250: Concerning changes to sentencing of persons convicted of drug crimes. Colorado Department of Public Safety. https://cdpsdocs.state.co.us/ors/docs/reports/2017_SB250-Rpt.pdf. Accessed 22 Nov 2021 [Google Scholar]
- 23.Colorado Department of Public Health and Environment (2019) RMEP Legislative brief final 2019: retail marijuana education program fact sheet—January 2019
- 24.Gourdet C, Giombi K, Kosa K, Wiley J, Cates S (2017) How four U.S. states are regulating recreational marijuana edibles. Int J Drug Policy 43:83–90. 10.1016/j.drugpo.2017.01.018 [DOI] [PubMed] [Google Scholar]
- 25.Wang G, Roosevelt G, Heard K (2013) Pediatric marijuana exposures in a medical marijuana state. JAMA Pediatr 167(7):630–633. 10.1001/jamapediatrics.2013.140 [DOI] [PubMed] [Google Scholar]
- 26.Wang G, Le Lait M, Deakyne S, Bronstein A, Bajaj L, Roosevelt G (2016) Unintentional pediatric exposures to marijuana in Colorado, 2009–2015. JAMA Pediatr 170(9):160971. 10.1001/jamapediatrics.2016.0971 [DOI] [PubMed] [Google Scholar]
- 27.Marijuana Enforcement Division (2016) Retail marijuana code. https://www.colorado.gov/pacific/sites/default/files/Retail%20Marijuana%20Rules%20through%2001302015.pdf. Accessed 22 Nov 2021
- 28.Brohl B, Kammerzell R, Koski W (2015) Colorado marijuana enforcement division: annual update. Colorado Department of Revenue Denver, Denver [Google Scholar]
- 29.Mehmedic Z, Chandra S, Slade D, Denham H, Foster S, Patel A, Ross S, Khan I, ElSohly M (2010) Potency trends of delta9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. J Forensic Sci 55(5):1209–1217. 10.1111/j.1556-4029.2010.01441.x [DOI] [PubMed] [Google Scholar]
- 30.Smart R, Caulkins J, Kilmer B, Davenport S, Midgette G (2017) Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington state. Addiction 112(12):2167–2177. 10.1111/add.13886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandra S, Radwan M, Majumdar C, Church J, Freeman T, ElSohly M (2019) New trends in cannabis potency in USA and Europe during the last decade (2008–2017). Eur Arch Psychiatry Clin Neurosci 269(1):5–15. 10.1007/s00406-019-00983-5 [DOI] [PubMed] [Google Scholar]
- 32.Wilson J, Freeman T, Mackie C (2019) Effects of increasing cannabis potency on adolescent health. Lancet Child Adolesc Health 3(2):121–128. 10.1016/S2352-4642(18)30342-0 [DOI] [PubMed] [Google Scholar]
- 33.Stogner J, Miller B (2015) Assessing the dangers of “dabbing”: mere marijuana or harmful new trend? Pediatrics 136(1):1–3. 10.1542/peds.2015-0454 [DOI] [PubMed] [Google Scholar]
- 34.Vergara D, Bidwell L, Gaudino R, Torres A, Du G, Ruthenburg T, deCesare K, Land D, Hutchison K, Kane N (2017) Compromised external validity: federally produced cannabis does not reflect legal markets. Sci Rep 7:46528. 10.1038/srep46528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Orens A, Light M, Rowberry J, Matsen J, Lewandowski B (2015) Marijuana equivalency in proportion and dosage: an assessment of physical and pharmacokinetic relationships in marijuana production and consumption in Colorado. Colorado Department of Revenue Denver, Denve: r [Google Scholar]
- 36.Bidwell L, Martin-Willett R, Karoly H (2021) Advancing the science on cannabis concentrates and behavioural health. Drug Alcohol Rev 40(6):900–913. 10.1111/dar.13281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meier M, Docherty M, Leischow S, Grimm K, Pardini D (2019) Cannabis concentrate use in adolescents. Pediatrics. 10.1542/peds.2019-0338 [DOI] [PubMed] [Google Scholar]
- 38.Colorado Department of Public Health and Environment (2020) Monitoring heatlh concerns related to marijuana in Colorado: 2020 report summary. Denver, CO [Google Scholar]
- 39.Tormohlen K, Brooks-Russell A, Ma M, Schneider K, Levinson A, Johnson R (2019) Modes of marijuana consumption among Colorado high school students before and after the initiation of retail marijuana sales for adults. J Stud Alcohol Drugs 80(1):46–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnson R, Brooks-Russell A, Ma M, Fairman B, Tolliver R, Levinson A (2016) Usual modes of marijuana consumption among high school students in Colorado . J Stud Alcohol Drugs 77(4):580–588. 10.15288/jsad.2016.77.580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mennis J, Stahler G (2020) Adolescent treatment admissions for marijuana following recreational legalization in Colorado and Washington. Drug Alcohol Depend 210:107960. 10.1016/j.drugalcdep.2020.107960 [DOI] [PubMed] [Google Scholar]
- 42.Substance Abuse and Mental Health Services Administration (2020) Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville [Google Scholar]
- 43.Rocky Mountain High Intensity Drug Trafficking Area (2020) The legalization of marijuana in Colorado: the impact. The Rocky Mountain HIDTA Training and Information Center Denver, Denver [Google Scholar]
- 44.Hasin D, Wall M, Keyes K, Cerda M, Schulenberg J, O’Malley P, Galea S, Pacula R, Feng T (2015) Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: Results from annual, repeated cross-sectional surveys. Lancet Psychiatry 2(7):601–608. 10.1016/S2215-0366(15)00217-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sarvet A, Wall M, Fink D, Greene E, Le A, Boustead A, Pacula R, Keyes K, Cerda M, Galea S, Hasin D (2018) Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction 113(6):1003–1016. 10.1111/add.14136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jones J, Jones K, Peil J (2018) The impact of the legalization of recreational marijuana on college students. Addict Behav 77:255–259. 10.1016/j.addbeh.2017.08.015 [DOI] [PubMed] [Google Scholar]
- 47.Vogel L (2018) What really happened after Colorado legalized marijuana? CMAJ 190(41):E1237–E1238. 10.1503/cmaj.109-5665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ghosh T, Vigil D, Maffey A, Tolliver R, Van Dyke M, Kattari L, Krug H, Reed J, Wolk L (2017) Lessons learned after three years of legalized, recreational marijuana: the Colorado experience. Prev Med 104:4–6. 10.1016/j.ypmed.2017.02.021 [DOI] [PubMed] [Google Scholar]
- 49.Popova L, McDonald E, Sidhu S, Barry R, Richers Maruyama T, Sheon N, Ling P (2017) Perceived harms and benefits of tobacco, marijuana, and electronic vaporizers among young adults in Colorado: implications for health education and research. Addiction 112(10):1821–1829. 10.im/add.13854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Silins E, Horwood L, Patton G, Fergusson D, Olsson C, Hutchinson D, Spry E, Toumbourou J, Degenhardt L, Swift W, Coffey C, Tait R, Letcher P, Copeland J, Mattick R (2014) Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry 1(4):286–293. 10.1016/S2215-0366(14)70307-4 [DOI] [PubMed] [Google Scholar]
- 51.Johnston L, Meich R, O’Malley P, Bachman J, Schulenberg J, Patrick M (2021) Monitoring the future national survey results on drug use, 1975–2020: 2020 Overview, key findings on adolescent drug use. Institute for Social Research, University of Michigan, Ann Arbor [Google Scholar]
- 52.Schuermeyer J, Salomonsen-Sautel S, Price R, Balan S, Thurstone C, Min S, Sakai J (2014) Temporal trends in marijuana attitudes, availability and use in Colorado compared to non-medical marijuana states: 2003–11. Drug Alcohol Depend 140:145–155. 10.1016/j.drugalcdep.2014.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stewart S, Bhatia D, Burns E, Sakai J, Martin L, Levinson A, Vaughn A, Li Y, James K (2020) Association of marijuana, mental health, and tobacco in Colorado. J Addict Med 14(1):48–55. 10.1097/ADM.0000000000000533 [DOI] [PubMed] [Google Scholar]
- 54.Hall K, Monte A, Chang T, Fox J, Brevik C, Vigil D, Van Dyke M, James K (2018) Mental health-related emergency department visits associated with cannabis in Colorado. Acad Emerg Med 25(5):526–537. 10.1111/acem.13393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang G, Davies S, Halmo L, Sass A, Mistry R (2018) Impact of marijuana legalization in Colorado on adolescent emergency and urgent care visits. J Adolesc Health 63(2):239–241. 10.1016/j.jadohealth.2017.12.010 [DOI] [PubMed] [Google Scholar]
- 56.Green B, Ritter C (2000) Marijuana use and depression. J Health Soc Behav 41(1):40–49 [PubMed] [Google Scholar]
- 57.Hammond C, Chaney A, Hendrickson B, Sharma P (2020) Cannabis use among US adolescents in the era of marijuana legalization: a review of changing use patterns, comorbidity, and health correlates. Int Rev Psychiatry 32(3):221–234. 10.1080/09540261.2020.1713056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Soler Artigas M, Sanchez-Mora C, Rovira P et al. (2020) Attention-deficit/hyperactivity disorder and lifetime cannabis use: genetic overlap and causality. Mol Psychiatry 25(10):2493–2503. 10.1038/s41380-018-0339-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kahn G, Wilcox H (2020) Marijuana use is associated with suicidal ideation and behavior among us adolescents at rates similar to tobacco and alcohol. Arch Suicide Res. 10.1080/13811118.2020.1804025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Clark R (1994) Marijuana use associated with first episode of psychiatric illness in an adolescent population. Am J Addict 3(1):67–71. 10.1111/j.1521-0391.1994.tb00228.x [DOI] [Google Scholar]
- 61.Hudak M, Severn D, Nordstrom K (2015) Edible cannabis-induced psychosis: intoxication and beyond. Am J Psychiatry 172(9):911–912. 10.1176/appi.ajp.2015.15030358 [DOI] [PubMed] [Google Scholar]
- 62.Rolland B, Geoffroy P, Jardri R, Cottencin O (2013) Aripiprazole for treating cannabis-induced psychotic symptoms in ultrahigh-risk individuals. Clin Neuropharmacol 36(3):98–99. 10.1097/WNF.0b013e3182908330 [DOI] [PubMed] [Google Scholar]
- 63.French L, Gray C, Leonard G et al. (2015) Early Cannabis use, polygenic risk score for schizophrenia and brain maturation in adolescence. JAMA Psychiat 72(10):1002–1011. 10.1001/jamapsychiatry.2015.1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hiemstra M, Nelemans S, Branje S, van Eijk K, Hottenga J, Vinkers C, van Lier P, Meeus W, Boks M (2018) Genetic vulnerability to schizophrenia is associated with cannabis use patterns during adolescence. Drug Alcohol Depend 190:143–150. 10.1016/j.drugalcdep.2018.05.024 [DOI] [PubMed] [Google Scholar]
- 65.Kendler K, Ohlsson H, Sundquist J, Sundquist K (2019) Prediction of onset of substance-induced psychotic disorder and its progression to schizophrenia in a Swedish ational sample. Am J Psychiatry 176(9):711–719. 10.1176/appi.ajp.2019.18101217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques T, Handley R, Luzi S, Russo M, Paparelli A, Butt A, Stilo S, Wiffen B, Powell J, Murray R (2009) High-potency cannabis and the risk of psychosis. Br J Psychiatry 195(6):488–491. 10.1192/bjp.bp.109.064220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Di Forti M, Sallis H, Allegri F et al. (2014) Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophr Bull 40(6):1509–1517. 10.1093/schbul/sbt181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Di Forti M, Marconi A, Carra E et al. (2015) Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case–control study. Lancet Psychiatry 2(3):233–238. 10.1016/S2215-0366(14)00117-5 [DOI] [PubMed] [Google Scholar]
- 69.Keller C, Chen E, Brodsky K, Yoon J (2016) A case of butane hash oil (marijuana wax)-induced psychosis. Subst Abus 37(3):384–386. 10.1080/08897077.2016.1141153 [DOI] [PubMed] [Google Scholar]
- 70.Murray R, Quigley H, Quattrone D, Englund A, Di Forti M (2016) Traditional marijuana, high-potency cannabis and synthetic cannabinoids: increasing risk for psychosis. World Psychiatry 15(3):195–204. 10.1002/wps.20341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pierre J, Gandal M, Son M (2016) Cannabis-induced psychosis associated with high potency “wax dabs.” Schizophr Res 172(1–3):211–212. 10.1016/j.schres.2016.01.056 [DOI] [PubMed] [Google Scholar]
- 72.Large M, Nielssen O (2017) Daily use of high-potency cannabis is associated with an increased risk of admission and more intervention after first-episode psychosis. Evid Based Ment Health 20(2):58. 10.1136/eb-2017-102630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pierre J (2017) Risk factors of increasingly potent cannabis: the joint effects of potency and frequency. Curr Psychiatry 16(2):15–20 [Google Scholar]
- 74.Rabin R, George T (2017) Understanding the link between cannabinoids and psychosis. Clin Pharmacol Ther 101(2):197–199. 10.1002/cpt.421 [DOI] [PubMed] [Google Scholar]
- 75.Bagot K, Milin R, Kaminer Y (2015) Adolescent initiation of cannabis use and early-onset psychosis. Subst Abus 36(4):524–533. 10.1080/08897077.2014.995332 [DOI] [PubMed] [Google Scholar]
- 76.Reed J, Hilkey S, Thorne J, English K (2021) Impacts of marijuana legalization in Colorado: a report pursuant to C.R.S. 24-33.4-516. Colorado Department of Public Safety Division of Criminal Justice, Office of Research and Statistics, Denver [Google Scholar]
- 77.Colorado Division of Criminal Justice Juvenile Diversion. https://dcj.colorado.gov/juvenile-diversion. Accessed 22 Nov 2021
- 78.Winder C et al. (2018) Juvenile diversion evaluation: youth served FY15-17. OMNI Institute, Denver [Google Scholar]
- 79.Volkow N, Baler R, Compton W, Weiss S (2014) Adverse health effects of marijuana use. N Engl J Med 370(23):2219–2227. 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McGraw M, Houser G, Galambos C, Wartchow E, Stillwell P, Weinman J (2018) Marijuana medusa: the many pulmonary faces of marijuana inhalation in adolescent males. Pediatr Pulmonol 53(12):1619–1626. 10.1002/ppul.24171 [DOI] [PubMed] [Google Scholar]
- 81.Perrine C, Pickens C, Boehmer T et al. (2019) Characteristics of a multistate outbreak of lung injury associated with e-cigarette use, or vaping—United States. MMWR Morb Mortal Wkly Rep 68(39):860–864. 10.15585/mmwr.mm6839e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schier J, Meiman J, Layden J et al. (2019) Severe pulmonary disease associated with electronic-cigarette-product use—interim guidance. MMWR Morb Mortal Wkly Rep 68(36):787–790. 10.15585/mmwr.mm6836e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Civiletto C, Aslam S, Hutchison J (2019) Electronic delivery (vaping) of cannabis and nicotine. StatPearls Publishing, Treasure Island, FL: [PubMed] [Google Scholar]
- 84.Duffy B, Li L, Lu S, Durocher L, Dittmar M, Delaney-Baldwin E, Panawennage D, LeMaster D, Navarette K, Spink D (2020) Analysis of cannabinoid-containing fluids in illicit vaping cartridges recovered from pulmonary injury patients: identification of vitamin e acetate as a major diluent. Toxics. 10.3390/toxics8010008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hartman R, Huestis M (2013) Cannabis effects on driving skills. Clin Chem 59(3):478–492. 10.1373/clinchem.2012.194381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Skelton K, Hecht A, Benjamin-Neelon S (2020) Recreational cannabis legalization in the US and maternal use during the preconception, prenatal, and postpartum periods. Int J Environ Res Public Health. 10.3390/ijerph17030909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Crume T, Juhl A, Brooks-Russell A, Hall K, Wymore E, Borgelt L (2018) Cannabis use during the perinatal period in a state with legalized recreational and medical marijuana: the association between maternal characteristics, breastfeeding patterns, and neonatal outcomes. J Pediatr 197:90–96. 10.1016/j.jpeds.2018.02.005 [DOI] [PubMed] [Google Scholar]
- 88.Wang G (2017) Pediatric concerns due to expanded cannabis use: unintended consequences of legalization. J Med Toxicol 13(1):99–105. 10.1007/s13181-016-0552-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dickson B, Mansfield C, Guiahi M, Allshouse A, Borgelt L, Sheeder J, Silver R, Metz T (2018) Recommendations from cannabis dispensaries about first-trimester cannabis use. Obstet Gynecol 131(6):1031–1038. 10.1097/A0G.0000000000002619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Committee on Obstetric Practice (2017) Marijuana use during pregnancy and lactation. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/10/marijuana-use-during-pregnancy-and-lactation. Accessed 22 Nov 2021 [Google Scholar]
- 91.One Chance to Grow Up. https://onechancetogrowup.org/policy/. Accessed 11 Nov 2021
- 92.ElSohly M, Mehmedic Z, Foster S, Gon C, Chandra S, Church J (2016) Changes in cannabis potency over the last 2 decades (1995–2014): analysis of Ln the United States. Biol Psychiatry 79(7):613–619. 10.1016/j.biopsych.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Di Marzo V, Piscitelli F (2015) The endocannabinoid system and its modulation by phytocannabinoids. Neurotherapeutics 12(4):692–698. 10.1007/s13311-015-0374-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hall W, Lynskey M (2016) Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction 111(10):1764–1773. 10.1111/add.13428 [DOI] [PubMed] [Google Scholar]
- 95.Marijuana Enforcement Division (2020) Colorado marijuana rules: 1 CCR 212–3. Department of Revenue, Denver [Google Scholar]
- 96.Hathaway A, Callaghan R, Macdonald S, Erickson P (2009) Cannabis dependence as a primary drug use-related problem: the case for harm reduction-oriented treatment options. Subst Use Misuse 44(7):990–1008. 10.1080/10826080802494875 [DOI] [PubMed] [Google Scholar]
- 97.Robinson Z, Riggs P (2016) Cooccurring psychiatric and substance use disorders. Child Adolesc Psychiatr Clin N Am 25(4):713–722. 10.1016/jxhc.2016.05.005 [DOI] [PubMed] [Google Scholar]
- 98.Gillespie N, Neale M, Jacobson K, Kendler K (2009) Modeling the genetic and environmental association between peer group deviance and cannabis use in male twins. Addiction 104(3):420–429. 10.1111/j.1360-0443.2008.02457.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hayatbakhsh R, Williams G, Bor W, Najman J (2013) Early childhood predictors of age of initiation to use of cannabis: a birth prospective study. Drug Alcohol Rev 32(3):232–240. 10.1111/j.1465-3362.2012.00520.x [DOI] [PubMed] [Google Scholar]
- 100.Rogeberg O (2013) Correlations between cannabis use and IQ change in the Dunedin cohort are consistent with confounding from socioeconomic status. Proc Natl Acad Sci USA 110(11):4251–4254. 10.1073/pnas.1215678110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Levine A, Clemenza K, Rynn M, Lieberman J (2017) Evidence for the risks and consequences of adolescent cannabis exposure. J Am Acad Child Adolesc Psychiatry 56(3):214–225. 10.1016/j.jaac.2016.12.014 [DOI] [PubMed] [Google Scholar]
- 102.Fergusson D, Boden J (2008) Cannabis use and later life outcomes. Addiction 103(6):969–976. 10.1111/j.1360-0443.2008.02221.x [DOI] [PubMed] [Google Scholar]
- 103.Lynskey M, Glowinski A, Todorov A, Bucholz K, Madden P, Nelson E, Statham D, Martin N, Heath A (2004) Major depressive disorder, suicidal ideation, and suicide attempt in twins discordant for cannabis dependence and early-onset cannabis use. Arch Gen Psychiatry 61(10):1026–1032. 10.1001/archpsyc.61.10.1026 [DOI] [PubMed] [Google Scholar]
- 104.Grant J, Scherrer J, Lynskey M, Agrawal A, Duncan A, Haber J, Heath A, Bucholz K (2012) Associations of alcohol, nicotine, cannabis, and drug use/dependence with educational attainment: evidence from cotwin-control analyses. Alcohol Clin Exp Res 36(8):1412–1420. 10.1111/j.1530-0277.2012.01752.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Few L, Grant J, Nelson E et al. (2016) Cannabis involvement and nonsuicidal self-injury: a discordant twin approach. J Stud Alcohol Drugs 77(6):873–880. 10.15288/jsad.2016.77.873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jackson N, Isen J, Khoddam R, Irons D, Tuvblad C, Iacono W, McGue M, Raine A, Baker L (2016) Impact of adolescent marijuana use on intelligence: results from two longitudinal twin studies. Proc Natl Acad Sci USA 113(5):E500–508. 10.1073/pnas.1516648113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Meier M, Caspi A, Danese A, Fisher H, Houts R, Arseneault L, Moffitt T (2018) Associations between adolescent cannabis use and neuropsychological decline: a longitudinal co-twin control study. Addiction 113(2):257–265. 10.1111/add.13946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mackie C, Wilson J, Freeman T, Craft S, Escamilla De La Torre T, Lynskey M (2021) A latent class analysis of cannabis use products in a general population sample of adolescents and their association with paranoia, hallucinations, cognitive disorganisation and grandiosity. Addict Behav 117:106837. 10.1016/j.addbeh.2021.106837 [DOI] [PubMed] [Google Scholar]
- 109.Day N, Richardson G, Goldschmidt L, Robles N, Taylor P, Stoffer D, Cornelius M, Geva D (1994) Effect of prenatal marijuana exposure on the cognitive development of offspring at age three. Neurotoxicol Teratol 16(2):169–175. 10.1016/0892-0362(94)90114-7 [DOI] [PubMed] [Google Scholar]
- 110.Goldschmidt L, Day N, Richardson G (2000) Effects of prenatal marijuana exposure on child behavior problems at age 10. Neurotoxicol Teratol 22(3):325–336. 10.1016/s0892-0362(00)00066-0 [DOI] [PubMed] [Google Scholar]
- 111.Blackard C, Tennes K (1984) Human placental transfer of cannabinoids. N Engl J Med 311(12):797. 10.1056/NEJM198409203111213 [DOI] [PubMed] [Google Scholar]