Abstract
Background
There is a lack of consensus about the effect of the COVID-19 pandemic on the mental health of children and adolescents. We aimed to compare rates of paediatric emergency department visits for attempted suicide, self-harm, and suicidal ideation during the pandemic with those before the pandemic.
Methods
For this systematic review and meta-analysis, we searched MEDLINE, Embase, and PsycINFO for studies published between Jan 1, 2020, and Dec 19, 2022. Studies published in English with data on paediatric (ie, those aged <19 years) emergency department visits before and during the COVID-19 pandemic were included. Case studies and qualitative analyses were excluded. Changes in attempted suicide, self-harm, suicidal ideation, and other mental-illness indicators (eg, anxiety, depression, and psychosis) were expressed as ratios of the rates of emergency department visits during the pandemic compared with those before the pandemic, and we analysed these with a random-effects meta-analysis. This study was registered with PROSPERO, CRD42022341897.
Findings
10 360 non-duplicate records were retrieved, which yielded 42 relevant studies (with 130 sample-estimates) representing 11·1 million emergency department visits for all indications of children and adolescents across 18 countries. The mean age of the samples of children and adolescents across studies was 11·7 years (SD 3·1, range 5·5–16·3), and there were on average 57·6% girls and 43·4% boys as a proportion of emergency department visits for any health reasons (ie, physical and mental). Only one study had data related to race or ethnicity. There was good evidence of an increase in emergency department visits for attempted suicide during the pandemic (rate ratio 1·22, 90% CI 1·08–1·37), modest evidence of an increase in emergency department visits for suicidal ideation (1·08, 0·93–1·25), and good evidence for only a slight change in self-harm (0·96, 0·89–1·04). Rates of emergency department visits for other mental-illness indications showed very good evidence of a decline (0·81, 0·74–0·89), and paediatric visits for all health indications showed strong evidence of a reduction (0·68, 0·62–0·75). When rates for attempted suicide and suicidal ideation were combined as a single measure, there was good evidence of an increase in emergency department visits among girls (1·39, 1·04–1·88) and only modest evidence of an increase among boys (1·06, 0·92–1·24). Self-harm among older children (mean age 16·3 years, range 13·0–16·3) showed good evidence of an increase (1·18, 1·00–1·39), but among younger children (mean age 9·0 years, range 5·5–12·0) there was modest evidence of a decrease (0·85, 0·70–1·05).
Interpretation
The integration of mental health support within community health and the education system—including promotion, prevention, early intervention, and treatment—is urgently needed to increase the reach of mental health support that can mitigate child and adolescent mental distress. In future pandemics, increased resourcing in some emergency department settings would help to address their expected increase in visits for acute mental distress among children and adolescents.
Funding
None.
Introduction
“Are the kids all right?” has been a repeated media headline and frequent discussion point during the COVID-19 pandemic. Stress, unpredictability, and disruptions can be precipitants of mental distress and psychiatric illness. During the pandemic, children and adolescents have had to endure repeated disruptions to schooling, social life, peer-group interactions, and extracurricular activities. Individual and family-level risk factors for paediatric mental distress have also increased during the pandemic, including increased screen time,1 reduced physical activity,2 and decreases in perceived connectedness to family and peers,3 as well as increases in family violence,4 parental depression and anxiety,5 parental alcohol consumption,6 parents losing jobs or facing disruptions, and caregiver death.7 In population-based samples, paediatric depression and anxiety8 and eating disorders9 have also been estimated to have increased during the pandemic.
Research in context.
Evidence before this study
We searched MEDLINE, Embase, and PsycINFO for studies published in English reporting COVID-19-related differences in paediatric (ie, those aged <19 years) emergency department visits for severe mental distress, including attempted suicide, self-harm, suicidal ideation, and other mental-illness indicators (eg, anxiety, depression, and psychosis) published between Jan 1, 2020, and Dec 19, 2022. The main search terms were related to mental health (eg, “suicidal behavio(u)r”, “psychological distress”), paediatric population groups (eg, “child” and “adolescent”), and coronavirus disease (eg, “COVID-19”). We found many independent studies comparing differences in emergency department visits for severe mental distress from periods before and during the COVID-19 pandemic, but no meta-analyses. Consequently, no cross-study quantitative estimate of COVID-19-related changes in child and adolescent psychiatric emergency department visits exists.
Added value of this study
To our knowledge, this systematic review and meta-analysis provides the first comprehensive synthesis of published studies reporting COVID-19-related changes in the absolute numbers of paediatric emergency department visits for attempted suicide, self-harm, suicidal ideation, and other mental-illness-related indicators. We included 42 studies representing 11·1 million unique paediatric emergency department visits for all indications across 18 countries. We found an overall reduction in paediatric emergency department visits during the COVID-19 pandemic (rate ratio 0·68, 90%CI 0·62–0·75), but we found good evidence that emergency department visits for suicide attempts increased (1·22, 1·08–1·37). Rates of emergency department visits for other mental-illness indications showed very good evidence of a decline (0·81, 0·74–0·89). We also found good evidence that the change in emergency department visits for suicidal ideation or attempt was larger for girls than for boys. Rates of self-harm increased among older children, but they decreased among younger children. By statistically pooling the available literature, this synthesis can more conclusively determine that indices of attempted suicide, self-harm, and suicidal ideation in children and adolescents have increased during the COVID-19 pandemic compared with before the pandemic.
Implications of all the available evidence
The COVID-19 pandemic represents a sociohistorical event with considerable implications for paediatric mental health. This study highlights the importance of, and need for, improved prevention strategies and greater sources of support for acute mental illness in children and adolescents.
Estimates of COVID-19-related change in indices of severe mental distress—including attempted suicide, self-harm, and suicidal ideation—have varied in the literature. Some authors report decreases in severe mental distress,10, 11, 12 or no clear change,13, 14, 15, 16 whereas others report increases among children and adolescents, especially adolescent girls.17, 18, 19, 20 Changes in emergency department presentations for severe mental distress have also evolved during the pandemic; initial reports suggested a decline from March to May, 2020, whereas increases were documented, especially among girls, in June to December, 2020.21 These discrepancies have fuelled confusion and have probably contributed to delays in public health and policy responses to address paediatric mental distress in the aftermath of the pandemic.22 Such delays are concerning, since pre-pandemic world data indicate that suicide was the third leading cause of death in adolescent girls aged 15–19 years and the fourth leading cause of death in adolescent boys aged 15–19 years.23 Moreover, there is evidence that suicidal ideation and self-harm were highly prevalent before the COVID-19 pandemic: one in seven adolescents aged 12–16 years reported that they had contemplated suicide,24 and one in six adolescents aged 13–18 years reported that they engaged in self-harm behaviour.25 More recent data indicate that one in three adolescent girls and one in seven adolescent boys had seriously considered attempting suicide in the past year, and rates of death by suicide in 13–17 year olds increased from July to December, 2020.26
To prepare and execute pandemic recovery policies adequately, and to determine resource allocation, explicit calls have been made to better understand the extent, severity, and pervasiveness of attempted suicide, self-harm, and suicidal ideation during the pandemic.22 Although numerous published studies compare differences in mental-illness-related emergency department visits before and during the COVID-19 pandemic, to our knowledge, no systematic review or meta-analysis exists. Thus, our primary objective was to conduct a systematic review and meta-analysis of the published literature to quantify pandemic-related changes in paediatric emergency department visits for attempted suicide, self-harm, and suicidal ideation. We focused primarily on these three emergencies because they represent the most severe, and potentially fatal, forms of mental distress. Research suggests that girls and adolescents are more likely to visit the emergency department for severe mental distress compared with boys and younger children.21, 25 Therefore, our secondary objective was to estimate whether COVID-19-related changes in rates of attempted suicide, self-harm, and suicidal ideation differed among sociodemographic moderators.
Methods
Definitions of suicide-related outcomes
The terminology used to describe self-harm varies across settings and studies. Some studies apply self-harm as an umbrella term including all self-injurious behaviour regardless of suicidal intent; others reserve the term exclusively for non-suicidal self-injurious behaviour. As we were unable to examine the intent of self-harm at the level of individual participants, the outcome of self-harm was based on study-defined classifications and descriptions. Our definitions of suicide-related outcomes were consistent with approaches in other meta-analyses (appendix p 3).
Search strategy and selection criteria
We searched MEDLINE, Embase, and PsycINFO for English-language sources published between Jan 1, 2020, and May 17, 2022 (appendix p 4), and updated the search for studies on Dec 19, 2022. The search terms were related to mental health (eg, “suicidal behavio(u)r”, “psychological distress”), paediatrics (eg, “child” and “adolescent”), and coronavirus disease (eg, “COVID-19”); the full search strategy for MEDLINE is in the appendix (p 4; searches of Embase and PsycINFO were similar to that of MEDLINE). To identify additional studies, we hand-searched reference lists of included studies. This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.27 Retrieved studies were imported into Covidence software (Covidence; Melbourne, VIC, Australia) for title and abstract review. Studies were included if they reported emergency department visit data on attempted suicide, self-harm, or suicidal ideation, had data for before and during the COVID-19 pandemic, were for paediatric samples (ie, those aged <19 years), and were published in English. No lower age limit was applied to these inclusion criteria. Case studies and qualitative analyses were excluded. Titles and abstracts were reviewed by independent coders (SM, PP, JH, and BA; mean random agreement probability 92%). Full-text articles were reviewed by at least two independent coders (SM, PP, JH, and BA; mean random agreement probability 88%). Discrepancies were resolved via consensus between SM and PP.
The National Institute of Health Quality Assessment Tool for Observation Cohort and Cross-Sectional Studies was used to assess study quality. Studies were scored 0 (criterion unmet) or 1 (criterion met) for ten criteria and summed to derive a total score ranging from 0 to 10 (appendix p 6).
Data extraction and preparation
Summary data extracted from each study were the following: authors; year of publication; study characteristics (eg, country, setting, and duration of data collation); sample characteristics (eg, age, sex, race and ethnicity, and socioeconomic status); numbers of emergency department visits before and during the COVID-19 pandemic for attempted suicide, self-harm, and suicidal ideation; visits for other mental-illness-related reasons (eg, depression, anxiety, and psychosis; appendix p 5); total visits for any health reason (ie, mental or physical); and percentage differences or rate ratios (RRs) and their CIs associated with the onset of the COVID-19 pandemic (if the numbers of visits and time period for data collation were not reported). Data were extracted by two independent coders (PP and JH; intercoder agreement 87%) and discrepancies were resolved via consensus between the two coders.
Rates of emergency department visits before and during the COVID-19 pandemic were calculated by dividing the number of emergency department visits by the time period for data collation. RRs were calculated by dividing the rate during the COVID-19 pandemic by the pre-COVID-19 rate and were then log-transformed. RR SEs were calculated by taking the square root of the sum of the reciprocals of the absolute numbers of emergency department visits before and during the COVID-19 pandemic. When the RR but not the numbers of visits was reported in a study, the SE was derived from the CI of the ratio.
Data analysis
A random-effects meta-analysis model was prepared using the mixed-model procedure (Proc Mixed) in SAS OnDemand for Academics (version 9.4). In the primary meta-analysis, the dependent variable was the log of the sample-estimate RR. Sample-estimates were weighted by the inverse square of their SEs using the approach of Yang,28 in which the random effects were estimated by setting the residual variance to unity.
A single fixed effect represented the category of emergency department visits at five levels: attempted suicide, self-harm, suicidal ideation, other mental-illness-related indications, and total health visits for any reason. The random effects were study identity and sample-estimate identity within studies (with separate variances specified for each category of emergency department visit); this parsimonious random-effects model allowed for RRs to be similar within settings compared with differences between settings. The square root of the sum of study and sample-estimate variances provided the τ statistic as an estimate of heterogeneity preferable to the I 2 statistic; heterogeneity was also assessed by combining the τ and the uncertainty in the mean into a confidence (prediction) interval for the RR in any given individual setting.29, 30
There were insufficient study estimates with different values of a given moderator to include the moderator in an analysis with all category levels of emergency department visits. Sufficient data for meta-analysing the moderating effects of sex (ie, male and female) and geographical location (eg, North America and Europe) were obtained by combining counts for suicide attempts or suicidal ideation into a single measure of suicidal ideation or attempt. The only other effects that could be meta-analysed were the moderating associations between age and sex and changes in self-harm. For the moderation analysis by age, age was assumed to have a numeric linear effect, and the magnitude of the effect was evaluated by predicting and comparing the RRs for self-harm for ages 1 SD less than and 1 SD more than the mean age.31 For moderators with insufficient data for meta-analysis, we summarised the magnitude of rate changes from available studies.
The meta-analysed effects and heterogeneity (τ) were back-transformed to RRs. We predefined thresholds for interpreting confidence limits of large (<0·50), moderate (0·50 to <0·70), small (0·70 to <0·90), and slight (0·90 to <1·00) rate decreases, and slight (1·00 to <1·11), small (1·11 to <1·43), moderate (1·43 to <2·00), and large (≥2·00) rate increases. Thresholds for interpreting confidence limits of τ are the square root of those for rate increases. Further justification for thresholds is described in the appendix (p 8). Precision of estimation is expressed as 90% CIs, as favoured by Rothman.32 We inferred the magnitude of effects by interpreting the lower and upper confidence limits, which are consistent with an alpha of 0·05 (a maximum error rate of 5%) for rejection of significant and non-significant hypotheses.33 If the lower and upper limit of the 90% CI for a meta-analysed mean (or τ) was substantial and of opposite direction (ie, both positive and negative), the ratio was deemed unclear (failure to reject a substantial hypothesis); otherwise, the ratio was deemed to have adequate precision at the 90% level.33 The extent of overlap of the 90% CI with slight or substantial (ie, small, moderate, and large) values was used to assess the level of evidence33 for or against the magnitude of the ratio. The extent of overlap was estimated as the areas of the sampling distribution falling in substantial (ie, small, moderate, and large) and slight magnitudes. These areas represent the probabilities that the true ratio has those magnitudes in a Bayesian analysis in which the prior is non-informative.33 Thresholds for interpreting the probabilities for a given magnitude are provided in the appendix (p 8). This study was registered with PROSPERO, CRD42022341897.
Role of the funding source
There was no funder for this study.
Results
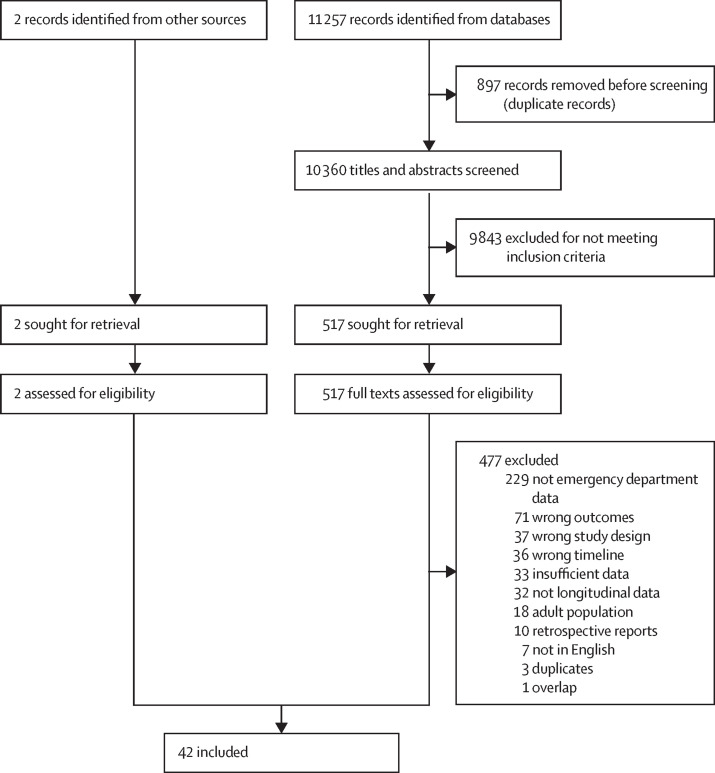
10 360 non-duplicate records were identified by our search, 517 full texts were reviewed, and 42 studies met full inclusion criteria (table 1 , figure 1 ). Sufficient data were reported across studies to derive 130 sample-estimate RRs (appendix pp 9–13). Funnel plots of sample-estimate SEs versus sample-estimates for the five categories of emergency department visits did not indicate substantial publication bias (appendix p 14).
Table 1.
Characteristics of the included studies
| Country | Visit categories |
Data collection periods |
||
|---|---|---|---|---|
| Before COVID-19 | During COVID-19 | |||
| Ashworth et al (2022)34 | UK | Suicidal ideation and self-harm | March, 2019, to March, 2020 | March, 2020, to March, 2021 |
| Berger et al (2022)35 | Switzerland | Suicidal ideation and self-harm | 2019 | 2020 |
| Bergmans and Larson (2021)36 | USA | Self-harm | 2015 to 2019 | 2020 |
| Bortoletto et al (2022)37 | Italy | Suicidal ideation | 2018 and 2019 | 2020 |
| Bothara et al (2021)38 | New Zealand | Suicidal ideation and self-harm | Feb 15 to March 18, 2020 | March 26 to April 28, 2020 |
| Bozzola et al (2022)39 | Italy | Suicidal ideation | March, 2019, to March, 2020 | March, 2020, to March, 2021 |
| Brewer et al (2022)40 | USA | Suicidal ideation | November, 2017, to August, 2019 | September, 2019, to June, 2021 |
| Broomfield et al (2021)41 | USA | Suicidal ideation | 2019 | 2020 |
| Bruns et al (2022)11 | Germany | Self-harm and suicide attempt | 2017 to 2019 | 2020 |
| Carison et al (2022)42 | Australia | Suicidal ideation | 2018 and 2019 | 2020 |
| Clavenna et al (2022)43 | Italy | Self-harm | 2019 | 2020 |
| Corrigan et al (2022)19 | Australia | Self-harm | 2015 to 2020 | 2020 |
| Cozzi et al (2022)44 | Italy | Suicide attempt | 2019 and 2020 | 2020 and 2021 |
| Davico et al (2021)45 | Italy | Suicidal ideation | 2019 | 2020 |
| DeLaroche et al (2021)13 | USA | Suicidal ideation | 2017 to 2019 | 2020 |
| Díaz de Neira et al (2021)46 | Spain | Suicidal ideation, self-harm, and suicide attempt | 2019 | 2020 |
| Edgcomb et al (2022)16 | USA | Suicidal ideation | 2019 | 2020 |
| Ferrando et al (2021)10 | USA | Suicidal ideation, self-harm, and suicide attempt | 2020 | 2020 |
| Gill et al (2021)14 | USA | Self-harm | 2017 to 2019 | 2020 |
| Gracia et al (2021)17 | Spain | Suicide attempt | 2019 | 2020 |
| Hill et al (2021)47 | USA | Suicidal ideation and suicide attempt | 2019 | 2020 |
| Hiscock et al (2022)20 | Australia | Self-harm | January, 2018, to March, 2020 | March, 2020, to October, 2020 |
| Ibeziako et al (2022)48 | USA | Suicidal ideation and suicide attempt | March, 2019, to February, 2020 | March, 2020, to February, 2021 |
| Kemerer et al (2021)49 | Ireland | Self-harm and suicide attempt | 2019 | 2020 |
| Kim et al (2022)50 | South Korea | Suicide attempt | 2018 to 2020 | 2020 |
| Kim et al (2022)15 | South Korea | Self-harm | 2019 | 2020 |
| Kirič et al (2022)51 | Slovenia | Suicidal ideation and suicide attempt | March to December, 2019 | March to December, 2020 |
| Llorca-Bofí et al (2022)52 | Spain | Suicidal ideation and suicide attempt | Jan 13 to March 14, 2020 | March 15 to June 20, 2020 |
| Mayne et al (2021)18 | USA | Suicidal ideation | 2019 | 2020 |
| McDonnell et al (2022)53 | Ireland | Self-harm | 2019 to 2020 | 2020 to 2021 |
| Miles and Zettl (2021)54 | USA | Suicidal ideation and suicide attempt | 2017 to 2019 | 2020 |
| Ougrin et al (2022)12 | Multiple* | Self-harm | March and April, 2019 | March and April, 2020 |
| Padela and Jyothish (2022)55 | UK | Self-harm and suicide attempt | 2019 | 2020 |
| Petruzzelli et al (2022)56 | Italy | Self-harm and suicide attempt | July to December, 2019 | July to December, 2020 |
| Ridout et al (2021)21 | USA | Suicidal ideation and suicide attempt | Jan 1 to March 9, 2019, and March 10 to Dec 15, 2019 | Jan 1 to March 9, 2020, and March 10 to Dec 15, 2020 |
| Rodd and Graudins (2021)57 | Australia | Self-harm | 2019 | 2020 |
| Shankar et al (2022)58 | USA | Self-harm | 2018 and 2019 | 2020 |
| Sokoloff et al (2021)59 | USA | Suicidal ideation | 2018 and 2019 | 2020 |
| Steeg et al (2021)60 | UK | Self-harm | 2019 | 2020 and 2021 |
| Sveticic et al (2021)61 | Australia | Self-harm | 2019 | 2020 |
| Wells et al (2022)62 | USA | Suicide attempt | March 15, 2017, to March 14, 2020 | March 15, 2020, to March 14, 2021 |
| Zhang et al (2022)63 | Canada | Self-harm | 2019 | 2020 |
The study by Ougrin et al (2022)12 incorporated patient-records data received from hospital emergency departments in ten countries: England, Scotland, Ireland, Austria, Italy, Hungary, Serbia, Türkiye, Oman, and the United Arab Emirates.
Figure 1.
Study profile
Across the 42 studies, 11·1 million emergency department visits were recorded. The mean age of participants across studies was 11·7 years (SD 3·1, range 5·5–16·3). The average proportion of girls in a given study's total health emergency department visits was 57·6%, and that for boys was 43·4%. Pre-pandemic emergency department visits comparison dates ranged from early 2015 to 2020 (median 2019), and pandemic emergency department visits were from 2020 to 2021. Two (5%) studies reported data from Asia, 17 (40%) from Europe, 16 (38%) from North America, six (14%) from Australia or New Zealand, and one (2%) pooled data from multiple countries. The mean study quality score was 7·5 (range 5–9; appendix p 7).
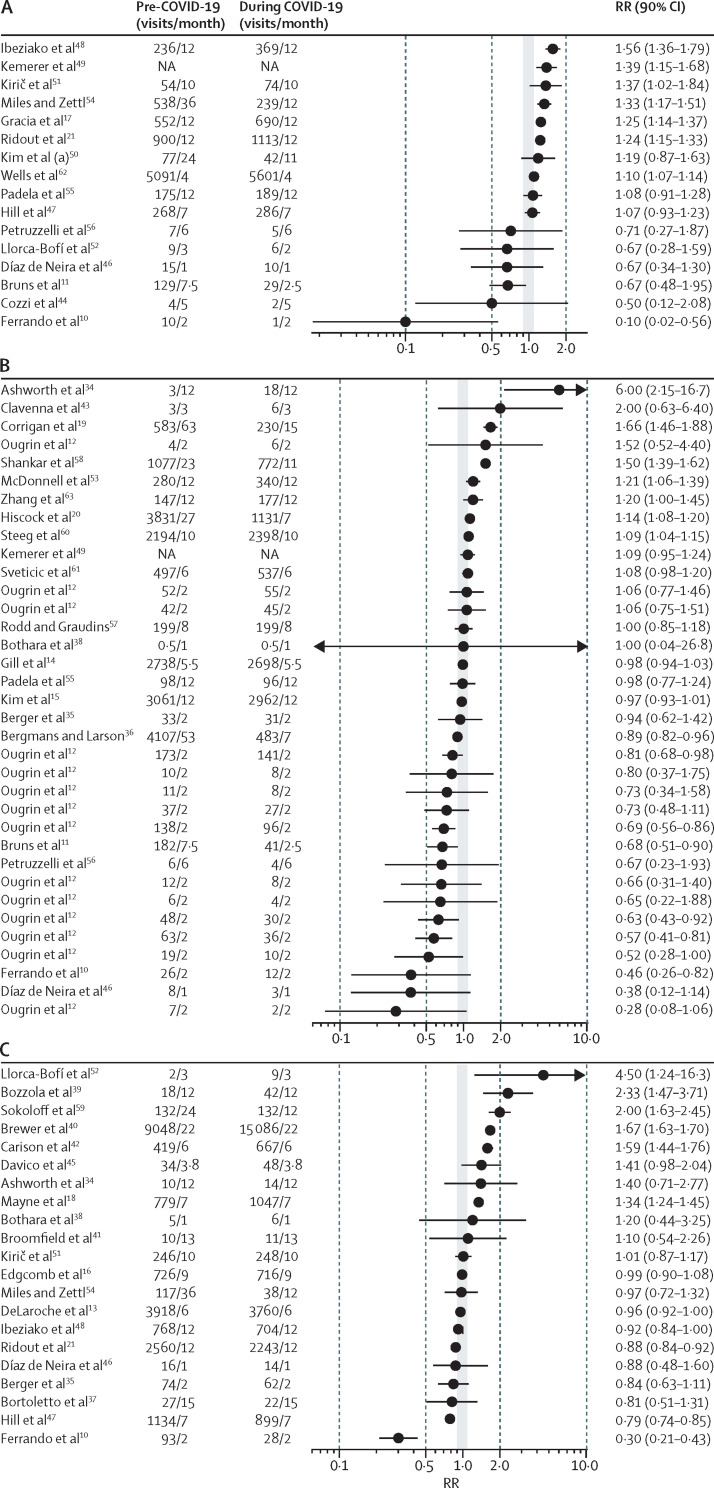
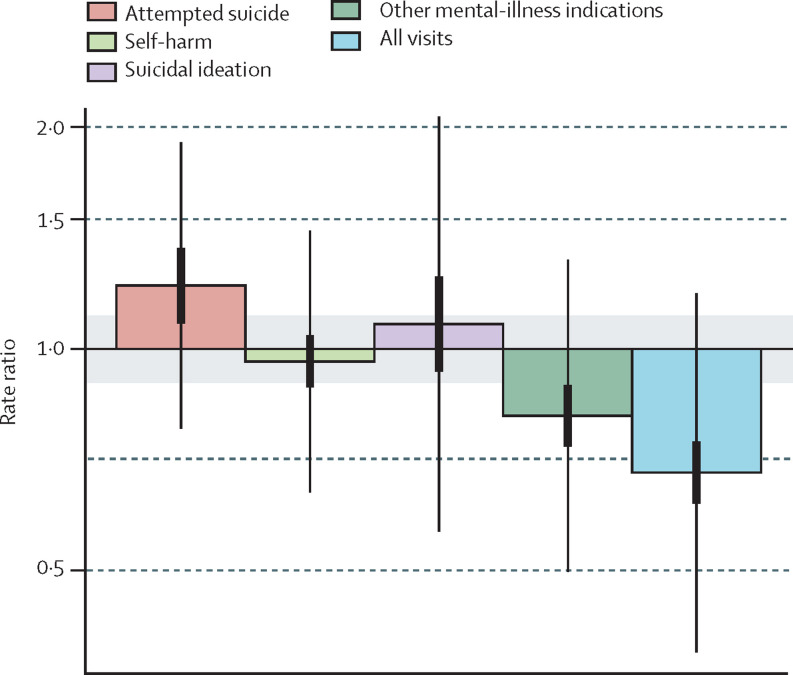
The results of the meta-analysis showed good evidence of an increase in emergency department visits during the COVID-19 pandemic for attempted suicide (RR 1·22, 90% CI 1·08–1·37; slight-to-small magnitude) and modest evidence of an increase for suicidal ideation (1·08, 0·93–1·25; slight-to-small magnitude; table 2 ; figure 2 ; figure 3 ). The uncertainty in the change for self-harm amounts to good evidence for a slight change, weak evidence for a reduction, and strong evidence against an increase (0·96, 0·89–1·04; small-to-slight magnitude). Emergency department visits for other mental-illness indications showed very good evidence of a reduction (0·81, 0·74–0·89; small magnitude), and visits for all indications showed strong evidence of a reduction (0·68, 0·62–0·75; small-to-moderate magnitude). In comparison with the reduction for all indications (including physical and mental health), there was strong evidence for relative increases in attempted suicide, self-harm, and suicidal ideation, and good evidence for a relative increase in the other mental-illness indications (appendix p 15).
Table 2.
Changes in child and adolescent emergency department visits expressed as ratios of rates during the COVID-19 pandemic to those before the pandemic
| Number of settings |
RR |
Heterogeneity ratio |
|||
|---|---|---|---|---|---|
| Mean (90% CI) | Magnitude* | τ (90% CI) | Magnitude† | ||
| Attempted suicide | 16 | 1·22 (1·08–1·37) | Slight-to-small increase | 1·26 (1·09–1·37) | Small to moderate |
| Self-harm | 39 | 0·96 (0·89–1·04) | Slight-to-small decrease | 1·26 (1·11–1·36) | Small to moderate |
| Suicidal ideation | 21 | 1·08 (0·93–1·25) | Slight-to-small increase | 1·43 (1·24–1·59) | Moderate to large |
| Other mental-illness indications | 24 | 0·81 (0·74–0·89) | Small decrease | 1·32 (1·19–1·42) | Small to large |
| All health indications | 34 | 0·68 (0·62–0·75) | Small-to-moderate decrease | 1·38 (1·27–1·47) | Moderate to large |
τ is the between-setting factor standard deviation. RR=rate ratio.
Magnitude thresholds for interpreting confidence limits of RR decreases: 0·90 to <1·00 slight; 0·70 to <0·90 small; 0·50 to <0·70 moderate; and <0·50 large. Thresholds for increases: 1·00 to <1·11 slight; 1·11 to <1·43 small; 1·43 to <2·00 moderate; ≥2·00, large.
Thresholds for interpreting confidence limits of τ are the square root of those for RR increases.
Figure 2.
Changes in child and adolescent emergency department visits for (A) attempted suicide, (B) self-harm, and (C) suicidal ideation expressed as ratios of rates during the COVID-19 pandemic to those before the pandemic
Ratios are plotted on a log axis. The grey area represents slight changes (RR 0·90 to <1·11). Vertical dashed lines indicate thresholds for large (0·10 to <0·50 or 2·00 to <10·00) and extremely large (<0·10 or ≥10·00) reductions and increases. Error bars represent 90% CIs. When numbers of visits are not reported (ie, NA for Kemerer and colleagues49), RRs and their corresponding CIs were extracted directly from the study. A value of 0·5 replaced counts of zero (ie, for Bothara and colleagues38). RR=rate ratio. NA=not applicable.
Figure 3.
Meta-analysed mean changes in child and adolescent emergency department visits expressed as ratios of rates during the COVID-19 pandemic to those before the pandemic
Ratios are plotted on a log axis. Grey area represents slight changes (rate ratio 0·90 to <1·11). Horizontal dashed lines indicate thresholds for reductions (moderate reduction 0·50 to <0·70; large reduction <0·50) and increases (moderate increase 1·43 to <2·00; large increase ≥2·00). Thick error bars represent 90% CIs for means and thin error bars represent 90% CIs for individual settings.
Each category of emergency department visit showed strong evidence of substantial heterogeneity (table 2). The resulting uncertainties in the changes in the rates of emergency department visits predicted in a given setting (thin error bars in figure 3) are considerably greater than those of the means (thick error bars).
In meta-analyses by sex, in five studies17, 18, 44, 48, 50 with ten study estimates there was good evidence that rates of emergency department visits for the combined measure of suicidal ideation or attempt increased during the COVID-19 pandemic among girls (RR 1·39, 90% CI 1·04–1·88; small-to-moderate magnitude; appendix p 16), whereas there was only modest evidence of an increase among boys (1·06, 0·92–1·24; slight-to-small magnitude). The comparison of these rates (girls:boys ratio 1·31, 90% CI 1·05–1·64; slight-to-moderate difference in magnitude) represents good evidence that the increase in suicidal ideation or attempt was greater for girls than for boys. In four studies19, 20, 38, 53 in which changes in rates of self-harm could be estimated for boys and girls, the difference between the sexes was inconclusive (appendix p 17).
Self-harm was the only indication for which there were sufficient data (14 study estimates across 11 studies10, 15, 19, 20, 35, 43, 46, 49, 53, 57, 60) to meta-analyse changes in emergency department visits by sample age. There was good evidence that rates of self-harm increased among older children (mean age 16·3 years [SD 1·0]), and modest evidence of a decrease among younger children (mean age 9·0 years [SD 1·0]) (appendix p 18). Rates of suicidal ideation or attempt at different ages were provided in only one study,21 in which there was good evidence that changes in emergency department visits for suicidal ideation or attempt differed only slightly between children and adolescents (appendix p 19).
One study18 in adolescents presented data from which to estimate the association between race and ethnicity and socioeconomic status and changes in suicidal ideation or attempt (appendix p 20). In that study, rates of suicidal ideation or attempt increased among White adolescents (RR 1·60, 90% CI 1·41–1·82; small-to-moderate magnitude), there was modest evidence of an increase among Black (1·12, 1·00–1·26; slight-to-small magnitude), Hispanic or Latinx (1·25, 0·94–1·67; slight-to-moderate magnitude), and Asian American (1·38, 0·95–2·00; slight-large magnitude) adolescents, and rates of suicidal ideation or attempt increased in all but the lowest socioeconomic group. There was one study20 from which to estimate the association between socioeconomic status and changes in self-harm; rates of self-harm only increased in the higher socioeconomic group (1·28, 1·18–1·39; small magnitude; appendix p 21).
The moderating effect of geographical region on changes in rate of emergency department visits for suicidal ideation or attempt was meta-analysed with 29 study estimates from 29 studies.10, 11, 13, 16, 17, 18, 21, 34, 35, 37, 38, 39, 40, 41, 42, 44, 45, 46, 47, 48, 49, 50, 51, 52, 54, 55, 56, 59, 62 There was good evidence of increased rates in samples from both North America (RR 1·27, 90% CI 1·04–1·53; slight-to-moderate magnitude)10, 13, 16, 18, 21, 40, 41, 47, 48, 54, 59, 62 and Europe (1·18, 0·99–1·41; slight-to-small magnitude).11, 17, 34, 35, 37, 39, 44, 45, 46, 49, 51, 52, 55, 56 A single study from Australia42 reported a moderate increase (1·59, 1·44–1·76). Further sample-estimates representing COVID-19-related changes in suicidal ideation or attempt in New Zealand38 (1·20, 0·44–3·25) and South Korea50 (1·19, 0·87–1·63) had small positive observed values but had unclear magnitudes.
Discussion
In this systematic review and meta-analysis of rates of child and adolescent visits to emergency departments, the evidence regarding attempted suicide and suicidal ideation indicates some of the adverse effects of the COVID-19 pandemic. Moderator analyses suggested that increases in suicidal ideation or attempt were more conclusive for girls than for boys, and that a conclusive increase in self-harm occurred only for older adolescents (aged around 16–17 years). We observed good evidence for a reduction in visits for all other mental-illness indications (eg, depression and psychosis) and strong evidence for a reduction in total emergency department visits for any health reason. In comparison with the reduction in total emergency department visits for any health reason, the findings reported in this study provide strong evidence for relative increases in attempted suicide, self-harm, and suicidal ideation during the COVID-19 pandemic. Commensurate with an accumulation of pandemic stressors,1, 2, 4, 5, 8, 9 there were decreases in access to various sources of support shown to prevent mental distress or mitigate its progression to severe outcomes. Together, these factors could have pushed children and adolescents, particularly girls and older adolescents, beyond their vulnerability thresholds.22
Several points are important to contextualise our findings. First, the decrease in the rate of emergency department visits for all indications is in line with data from the USA suggesting that there have been system-wide reductions in emergency department visits, especially early in the pandemic, for many condition-specific acute and chronic health problems.14 Reasons for such reductions include more watchful waiting of symptoms, shelter-in-place orders, and fear of COVID-19 infection.14 We also found a decrease in the absolute number of paediatric emergency department visits for other mental-illness-related indications. When this finding is paired with Canadian data showing that calls to crisis hotlines increased substantively, and that increases of 10–15% were observed in community-based mental health settings,64 it suggests that children and adolescents experiencing less acute (and potentially non-fatal) forms of mental distress during the COVID-19 pandemic could have used support outside of the emergency department to address their mental health needs. Our evidence of an increase in emergency department visits for suicide attempts and suicidal ideation during the pandemic is all the more notable when considered in the context of a system-wide reduction in emergency department visits for all indications.14
Second, the increase in the rate of visits for suicide-related outcomes could be due in part to a continuation of upward trends in rates of paediatric mental-illness-related issues that were well documented in the USA in the years before the pandemic.65 To contextualise this further, we calculated the upward trend in the rates for suicidal ideation or attempts pre-pandemic (studies used are listed in the appendix; p 22). We expressed the rates as factor increases per year, averaged the factors (via logs) for North American studies (mean 1·08 or 8% per year), then averaged this value with the value from the only European study (1·10) to give a mean of 1·09. The mean time between the midpoint of pre-COVID-19 and during-COVID-19 assessments of emergency department visits in the meta-analysed studies was 1·39 years, so on the assumption that the upward trend would have continued during the pandemic, the mean change in the rate of suicidal ideation or attempt in the meta-analysis due to the trend would have been a factor of 1·091·38=1·13 or 13%. If this trend applied equally to suicide attempts, self-harm, and suicidal ideation, the effect of the COVID-19 pandemic would reduce to slight changes or a small decrease for self-harm, but the change relative to all emergency department visits would still be substantial increases. Uncertainty in the trend will contribute to uncertainty in the adjusted RRs, but even a doubling of the trend (a factor of 1·132=1·28 or 28%) would leave reasonable evidence of relative increases due to the COVID-19 pandemic.
Third, substantial heterogeneity in the changes in rates was observed, indicating that, in some settings, the rates for each of the specific indications of suicide attempts, suicidal ideation, and self-harm did not increase or might even have reduced, whereas for others, they increased substantially. The specific settings in which rates showed evidence of substantial decreases and increases can be identified from the confidence limits for each indication and each study in the forest plot (figure 2) and in the appendix (pp 9–13).
Our moderator findings are consistent with pre-pandemic research observing a sex paradox of suicide, whereby girls are more likely to attempt suicide and engage mental health care, yet boys are more likely to die by suicide.66 In keeping with previous research, we found that girls were considerably more likely than boys to present to the emergency department (mean increase of 39% for girls vs 6% for boys) for severe mental distress during the pandemic. Moreover, self-harm increased in adolescents (mean increase of 18%) but decreased in younger children (mean decrease of 15%). As such, current findings support previous recommendations highlighting the need for sex and age specificity in youth suicide prevention interventions. These findings suggest that strategies for adolescent girls should focus on risk stratification among those receiving mental health care and presenting with self-harm behaviour, whereas strategies for boys should focus on increasing engagement with mental health services and addressing earlier prevention or intervention targets (ie, identifying and expressing emotion) in non-mental health, community settings.
Our finding of an increase of presentations with acute mental distress to emergency departments during the pandemic, concomitant with a decrease in general presentations for youth, implies that a greater proportion of the workload of emergency department staff was likely to comprise acute mental illness compared with before the pandemic. Research has found that even before the pandemic, paediatric care providers reported inadequate clinical training in mental-illness emergencies during residency.67 These findings suggest that an increase in multidisciplinary emergency department provider training, clinical capacity, and resources for managing acute psychiatric distress might be required in response to the changing landscape of emergency department care, should the changes observed in our meta-analysis be maintained over time.
Several limitations should be noted. First, data for this study are based on electronic health records capturing relevant diagnostic codes for presentation to the emergency department. As health records are based on individual clinician or organisational classifications, reporting is rarely standardised across sites, resulting in measurement error. Greater standardisation in data collection and reporting in this field is urgently needed to increase confidence in the generalisability of study results across settings. Second, this study does not identify the prevalence of suicidal thoughts and behaviour in the population more broadly, but rather presentation to the emergency department for these indications. Third, cross-study moderation analyses were limited to estimations of differences in rates of suicidal ideation or attempt by age and sex, and estimations of regional rates for samples from North America, Europe, and Australia. Due to the variability of reporting socioeconomic status and race and ethnicity data in individual studies, we were only able to assess such data reported in two studies. No individual study examined the effect of gender identity on changes in emergency department visits during the COVID-19 pandemic, which is a crucial avenue for future research. Fourth, 18 countries are represented in the analyses; however, most (>90%) were from North America, Europe, and Australia. The disproportionate focus on these continents is challenging for global generalisability, given that these regions only represent less than 10% of the world's population. Finally, only journal articles written in English were included.
This study provides good evidence of an exacerbation in severe mental distress and resultant emergency department presentations over the course of the COVID-19 pandemic among children and adolescents. Our findings are in line with pandemic-related research documenting population-level increases in paediatric mental illnesses such as depression and anxiety symptoms8 and eating disorders,9 as well as help-seeking behaviour.67 Thus, efforts to both understand and mitigate underlying factors associated with mental distress among children and adolescents are needed to inform prevention strategies. Our findings should also encourage health initiatives, clinical capacity, and targeted emergency department-provider training for managing acute psychiatric distress.
Data sharing
Data extracted and analysed in this study are fully reported in the appendix (pp 9–13). SAS code used to analyse these data can be made available from the corresponding author upon reasonable request.
Declaration of interests
TV has received honoraria for presentations related to youth suicide during the pandemic and is also the Chair of the COVID-19 Task Force and the Children and Schools working group for the Royal Society of Canada and is the President of the International Society for Research on Aggression. DJK has received grant funding related to research on youth suicide from the Canadian Institutes of Health Research, Sobey's Foundation, and SickKids Foundation in the past 36 months. All other authors declare no competing interests.
Contributors
SM and RDN, with input from DJK and TV, conceptualised and planned the study. SM managed and coordinated the research activity planning and execution. SM, PP, JMAH, and BA extracted the data. RDN and WGH reviewed the data, designed the methods, conducted the statistical analysis, and wrote up the results and appendices. SM and RDN prepared the first draft of the manuscript, with important contributions from DJK, TV, and NR. PP, JMAH, BA, SMD, and WGH critically reviewed and commented on the manuscript. PP, JMAH, and BA helped to prepare, create, and present the published work, specifically visualisation and data presentation. SM and RDN had oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team. All authors interpreted the results, commented on drafts of the manuscript, and approved the final version. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Supplementary Material
References
- 1.Madigan S, Eirich R, Pador P, McArthur BA, Neville RD. Assessment of changes in child and adolescent screen time during the COVID-19 pandemic: a systematic review and meta-analysis. JAMA Pediatr. 2022;176:1188–1198. doi: 10.1001/jamapediatrics.2022.4116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neville RD, Lakes KD, Hopkins WG, et al. Global changes in child and adolescent physical activity during the COVID-19 pandemic: a systematic review and meta-analysis. JAMA Pediatr. 2022;176:886–894. doi: 10.1001/jamapediatrics.2022.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosen ML, Rodman AM, Kasparek SW, et al. Promoting youth mental health during the COVID-19 pandemic: a longitudinal study. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Letourneau N, Luis MA, Kurbatfinski S, et al. COVID-19 and family violence: a rapid review of literature published up to 1 year after the pandemic declaration. EClinicalMedicine. 2022;53 doi: 10.1016/j.eclinm.2022.101634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Racine N, Hetherington E, McArthur BA, et al. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatry. 2021;8:405–415. doi: 10.1016/S2215-0366(21)00074-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nanos Research 25% of Canadians (aged 35–54) are drinking more while at home due to COVID-19 pandemic; cite lack of regular schedule, stress, and boredom as main factors. 2020. https://www.ccsa.ca/covid-19-and-increased-alcohol-consumption-nanos-poll-summary-report
- 7.Hillis S, N'konzi J-PN, Msemburi W, et al. Orphanhood and caregiver loss among children based on new global excess COVID-19 death estimates. JAMA Pediatr. 2022;176:1145–1148. doi: 10.1001/jamapediatrics.2022.3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agostino H, Burstein B, Moubayed D, et al. Trends in the incidence of new-onset anorexia nervosa and atypical anorexia nervosa among youth during the COVID-19 pandemic in Canada. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.37395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrando SJ, Klepacz L, Lynch S, et al. Psychiatric emergencies during the height of the COVID-19 pandemic in the suburban New York City area. J Psychiatr Res. 2021;136:552–559. doi: 10.1016/j.jpsychires.2020.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bruns N, Willemsen L, Stang A, et al. Pediatric intensive care unit admissions after adolescent suicide attempts during the pandemic. Pediatrics. 2022;150 doi: 10.1542/peds.2021-055973. [DOI] [PubMed] [Google Scholar]
- 12.Ougrin D, Wong BHC, Vaezinejad M, et al. Pandemic-related emergency psychiatric presentations for self-harm of children and adolescents in 10 countries (PREP-kids): a retrospective international cohort study. Eur Child Adolesc Psychiatry. 2022;31:1–13. doi: 10.1007/s00787-021-01741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeLaroche AM, Rodean J, Aronson PL, et al. Pediatric emergency department visits at US children's hospitals during the COVID-19 pandemic. Pediatrics. 2021;147 doi: 10.1542/peds.2020-039628. [DOI] [PubMed] [Google Scholar]
- 14.Gill PJ, Mahant S, Hall M, Berry JG. Reasons for admissions to US children's hospitals during the COVID-19 pandemic. JAMA. 2021;325:1676–1679. doi: 10.1001/jama.2021.4382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim S, Ro YS, Ko SK, et al. The impact of COVID-19 on the patterns of emergency department visits among pediatric patients. Am J Emerg Med. 2022;54:196–201. doi: 10.1016/j.ajem.2022.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edgcomb JB, Benson NM, Tseng CH, et al. Mental health-related emergency department visits among children during the early COVID-19 pandemic. Psychiatr Res Clin Pract. 2022;4:4–11. doi: 10.1176/appi.prcp.20210036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gracia R, Pamias M, Mortier P, Alonso J, Pérez V, Palao D. Is the COVID-19 pandemic a risk factor for suicide attempts in adolescent girls? J Affect Disord. 2021;292:139–141. doi: 10.1016/j.jad.2021.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mayne SL, Hannan C, Davis M, et al. COVID-19 and adolescent depression and suicide risk screening outcomes. Pediatrics. 2021;148 doi: 10.1542/peds.2021-051507. [DOI] [PubMed] [Google Scholar]
- 19.Corrigan C, Duke G, Millar J, et al. Admissions of children and adolescents with deliberate self-harm to intensive care during the SARS-CoV-2 outbreak in Australia. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.11692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hiscock H, Chu W, O'Reilly G, et al. Association between COVID-19 restrictions and emergency department presentations for paediatric mental health in Victoria, Australia. Aust Health Rev. 2022;46:529–536. doi: 10.1071/AH22015. [DOI] [PubMed] [Google Scholar]
- 21.Ridout KK, Alavi M, Ridout SJ, et al. Emergency department encounters among youth with suicidal thoughts or behaviors during the COVID-19 pandemic. JAMA Psychiatry. 2021;78:1319–1328. doi: 10.1001/jamapsychiatry.2021.2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korczak DJ, Madigan S, Vaillancourt T. Data divide—disentangling the role of the COVID-19 pandemic on child mental health and well-being. JAMA Pediatr. 2022;176:635–636. doi: 10.1001/jamapediatrics.2022.0791. [DOI] [PubMed] [Google Scholar]
- 23.US Centers for Disease Control and Prevention Youth risk behavior survey: data summary and trends report—2011–2021. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
- 24.Stallard P, Spears M, Montgomery AA, Phillips R, Sayal K. Self-harm in young adolescents (12–16 years): onset and short-term continuation in a community sample. BMC Psychiatry. 2013;13:328. doi: 10.1186/1471-244X-13-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bridge JA, Ruch DA, Sheftall AH, et al. Youth suicide during the first year of the COVID-19 pandemic. Pediatrics. 2023 doi: 10.1542/peds.2022-058375. published online Feb 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang M. Centre for multilevel modelling; London: 2003. A review of random effects modelling in SAS (release 8.2) [Google Scholar]
- 29.Higgins JPT. Commentary: heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008;37:1158–1160. doi: 10.1093/ije/dyn204. [DOI] [PubMed] [Google Scholar]
- 30.Borenstein M. In a meta-analysis, the I-squared statistic does not tell us how much the effect size varies. J Clin Epidemiol. 2022;152:281–284. doi: 10.1016/j.jclinepi.2022.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Gelman A. Scaling regression inputs by dividing by two standard deviations. Stat Med. 2008;27:2865–2873. doi: 10.1002/sim.3107. [DOI] [PubMed] [Google Scholar]
- 32.Rothman KJ. Oxford University Press; New York, NY: 2012. Epidemiology: an introduction. [Google Scholar]
- 33.Hopkins WG. Replacing statistical significance and non-significance with better approaches to sampling uncertainty. Front Physiol. 2022;13 doi: 10.3389/fphys.2022.962132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ashworth E, Provazza S, McCarthy M, Saini P. Children and young people presenting in a pediatric emergency department in north-west England in suicidal crisis: an exploratory case series study. Front Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.892939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berger G, Häberling I, Lustenberger A, et al. The mental distress of our youth in the context of the COVID-19 pandemic. Swiss Med Wkly. 2022;152 doi: 10.4414/smw.2022.w30142. [DOI] [PubMed] [Google Scholar]
- 36.Bergmans RS, Larson PS. Suicide attempt and intentional self-harm during the earlier phase of the COVID-19 pandemic in Washtenaw County, Michigan. J Epidemiol Community Health. 2021;75:963–969. doi: 10.1136/jech-2020-215333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bortoletto R, Di Gennaro G, Antolini G, et al. Sociodemographic and clinical changes in pediatric in-patient admissions for mental health emergencies during the COVID-19 pandemic: March 2020 to June 2021. Psychiatry Res Commun. 2022;2 doi: 10.1016/j.psycom.2022.100023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bothara RK, Raina A, Carne B, et al. Paediatric presentations to Christchurch Hospital emergency department during COVID-19 lockdown. J Paediatr Child Health. 2021;57:877–882. doi: 10.1111/jpc.15347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bozzola E, Ferrara P, Spina G, et al. The pandemic within the pandemic: the surge of neuropsychological disorders in Italian children during the COVID-19 era. Ital J Pediatr. 2022;48:126. doi: 10.1186/s13052-022-01324-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brewer AG, Doss W, Sheehan KM, Davis MM, Feinglass JM. Trends in suicidal ideation-related emergency department visits for youth in Illinois: 2016–2021. Pediatrics. 2022;150 doi: 10.1542/peds.2022-056793. [DOI] [PubMed] [Google Scholar]
- 41.Broomfield A, Rodd I, Winckworth L. Paediatric mental health presentations prior to, and during, the COVID-19 pandemic. Arch Dis Child. 2021;106(suppl 1):A283–A284. [Google Scholar]
- 42.Carison A, Babl FE, O'Donnell SM. Increased paediatric emergency mental health and suicidality presentations during COVID-19 stay at home restrictions. Emerg Med Australas. 2022;34:85–91. doi: 10.1111/1742-6723.13901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clavenna A, Zanini A, Pelucchi M, et al. Trend of emergency department accesses for mental disorders by adolescents during the pandemic period. Pediatr Emerg Care. 2022;38:e1233–e1235. doi: 10.1097/PEC.0000000000002686. [DOI] [PubMed] [Google Scholar]
- 44.Cozzi G, Blasutig F, De Nardi L, Giangreco M, Barbi E, Amaddeo A. The first winter of social distancing improved most of the health indexes in a paediatric emergency department. Acta Paediatr. 2022;111:1027–1033. doi: 10.1111/apa.16271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Davico C, Marcotulli D, Lux C, et al. Impact of the COVID-19 pandemic on child and adolescent psychiatric emergencies. J Clin Psychiatry. 2021;82 doi: 10.4088/JCP.20m13467. [DOI] [PubMed] [Google Scholar]
- 46.Díaz de Neira M, Blasco-Fontecilla H, García Murillo L, et al. Demand analysis of a psychiatric emergency room and an adolescent acute inpatient unit in the context of the COVID-19 pandemic in Madrid, Spain. Front Psychiatry. 2021;11 doi: 10.3389/fpsyt.2020.557508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147 doi: 10.1542/peds.2020-029280. [DOI] [PubMed] [Google Scholar]
- 48.Ibeziako P, Kaufman K, Scheer KN, Sideridis G. Pediatric mental health presentations and boarding: first year of the COVID-19 pandemic. Hosp Pediatr. 2022;12:751–760. doi: 10.1542/hpeds.2022-006555. [DOI] [PubMed] [Google Scholar]
- 49.Kemerer B, Casey S, McClelland I, Barrett E. The impact of COVID-19 on mental health presentations to Temple Street Children's University Hospital emergency department. Ir J Med Sci. 2021;190:S145–S146. [Google Scholar]
- 50.Kim MJ, Paek SH, Kwon JH, Park SH, Chung HJ, Byun YH. Changes in suicide rate and characteristics according to age of suicide attempters before and after COVID-19. Children (Basel) 2022;9:151. doi: 10.3390/children9020151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kirič B, Leben Novak L, Lušicky P, Drobnič Radobuljac M. Suicidal behavior in emergency child and adolescent psychiatric service users before and during the 16 months of the COVID-19 pandemic. Front Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.893040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Llorca-Bofí V, Adrados-Pérez M, Sánchez-Cazalilla M, et al. Urgent care and suicidal behavior in the child and adolescent population in a psychiatric emergency department in a Spanish province during the two COVID-19 states of alarm. Rev Psiquiatr Salud Ment. 2022 doi: 10.1016/j.rpsm.2022.03.003. published online June 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McDonnell T, Conlon C, McNicholas F, et al. Paediatric hospital admissions for psychiatric and psychosocial reasons during the first year of the COVID-19 pandemic. Int Rev Psychiatry. 2022;34:128–139. doi: 10.1080/09540261.2022.2061840. [DOI] [PubMed] [Google Scholar]
- 54.Miles J, Zettl R. 44.9 Impact of the COVID-19 pandemic on suicide attempts and suicidal ideations in youth. J Am Acad Child Adolesc Psychiatry. 2021;60:S240. [Google Scholar]
- 55.Padela M, Jyothish D. Mental health attendances to the emergency department by children and young people—a comparison between pre-pandemic and pandemic years. Arch Dis Child. 2022;107(suppl 2):A412–A413. [Google Scholar]
- 56.Petruzzelli MG, Furente F, Colacicco G, et al. Implication of COVID-19 pandemic on adolescent mental health: an analysis of the psychiatric counseling from the emergency room of an Italian university hospital in the years 2019–2021. J Clin Med. 2022;11 doi: 10.3390/jcm11206177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rodd N, Graudins A. Did the COVID-19 ‘lockdown’ in Melbourne, Australia influence adolescent deliberate self-poisoning (DSP) and mental-health presentations to a metropolitan hospital network? J Med Toxicol. 2021;17:147. [Google Scholar]
- 58.Shankar LG, Habich M, Rosenman M, Arzu J, Lales G, Hoffmann JA. Mental health emergency department visits by children before and during the COVID-19 pandemic. Acad Pediatr. 2022;22:1127–1132. doi: 10.1016/j.acap.2022.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sokoloff WC, Krief WI, Giusto KA, et al. Pediatric emergency department utilization during the COVID-19 pandemic in New York City. Am J Emerg Med. 2021;45:100–104. doi: 10.1016/j.ajem.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Steeg S, Bojanić L, Tilston G, et al. Temporal trends in primary care-recorded self-harm during and beyond the first year of the COVID-19 pandemic: time series analysis of electronic healthcare records for 2·8 million patients in the Greater Manchester Care Record. EClinicalMedicine. 2021;41 doi: 10.1016/j.eclinm.2021.101175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sveticic J, Stapelberg NJ, Turner K. Suicide prevention during COVID-19: identification of groups with reduced presentations to emergency departments. Australas Psychiatry. 2021;29:333–336. doi: 10.1177/1039856221992632. [DOI] [PubMed] [Google Scholar]
- 62.Wells JM, Rodean J, Cook L, et al. Injury-related pediatric emergency department visits in the first year of COVID-19. Pediatrics. 2022;150 doi: 10.1542/peds.2021-054545. [DOI] [PubMed] [Google Scholar]
- 63.Zhang EWJ, Davis A, Finkelstein Y, Rosenfield D. The effects of COVID-19 on poisonings in the paediatric emergency department. Paediatr Child Health. 2022;27(suppl 1):S4–S8. doi: 10.1093/pch/pxab100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mitchell RHB, Ani C, Cyr C, et al. Near-fatal self-harm among Canadian adolescents. Can J Psychiatry. 2022;67:598–607. doi: 10.1177/07067437211058602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang J, Sumner SA, Simon TR, et al. Trends in the incidence and lethality of suicidal acts in the United States, 2006 to 2015. JAMA Psychiatry. 2020;77:684–693. doi: 10.1001/jamapsychiatry.2020.0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McMahon EM, Keeley H, Cannon M, et al. The iceberg of suicide and self-harm in Irish adolescents: a population-based study. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1929–1935. doi: 10.1007/s00127-014-0907-z. [DOI] [PubMed] [Google Scholar]
- 67.Green C, Leyenaar JK, Turner AL, Leslie LK. Competency of future pediatricians caring for children with behavioral and mental health problems. Pediatrics. 2020;146 doi: 10.1542/peds.2019-2884. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data extracted and analysed in this study are fully reported in the appendix (pp 9–13). SAS code used to analyse these data can be made available from the corresponding author upon reasonable request.