Abstract
The aim of this report is to illustrate the venous wall graft and to present the observations drawn from a large series of eyelid reconstructions performed with this method. Sixty-four patients underwent venous wall grafts, mostly after resection of invasive carcinomas of the eyelids and, in only one case, after traumatic injury. All patients had good functional and cosmetic results. The average follow-up time was 6.5 years. Few negligible complications were observed. Only two cases (3.1%) needed further surgical treatment. Vein graft is a reliable alternative to traditional procedures in replacing tarsus-conjunctival layer, achieving satisfactory results. A single surgical session is required, usually without complications.
Key words: Venous wall graft, Tarsus-conjunctival layer, Full-thickness reconstruction, Eyelid tumors
Introduction
Wide full-thickness reconstructions of the eyelids may be a complex and difficult procedure and at times with unsatisfactory results. The tarsus-conjunctival layer, surgically known as the posterior or interior lamella, represents the most difficult part to repair because of its highly specialized structure. Surgical therapy aims to achieve the best functional reconstruction of the thin, smooth, elastic layer getting a new interior lamella not remarkably different from the healthy eyelid. For this purpose, several methods have been proposed as recorded in many reviews.1,2 Each of those has its advantages and disadvantages although most of them are not usually satisfactory regarding the stiffness and thickness of the reconstructed eyelid. Furthermore, some methods need more than one surgical session. To overcome these problems, in 2008 we published our first results with a new method3 for reconstructing the tarsusconjunctival layer using a vein graft. Our aims were the following: i) to use an autologous graft made up by a layer of elastic dense connective tissue coated by a thin epithelium-like lining that is an anatomical structure comparable to the plate to be replaced; ii) to find a suitable structure to replace also the canthal apparatus; iii) to find a donor site capable of supplying large sized grafts, without functional and cosmetic impairment or discomfort for the patient; iv) to perform the whole reconstruction in only one surgical session.
Therefore, on the assumption that there would be some similarities between the tarsus- conjunctival layer and the vein wall, we believed that the superficial veins of the limbs could be suitable to replace the former. These vessels are propulsive veins, that means they are able to partly modify their size thanks to their store of smooth muscular cells and elastic fibers.4 This feature makes the middle layer of the vein functionally similar to the tarsus. Inside the vessels are lined with endothelium which, we hoped, could act as the conjunctival epithelium. Furthermore, the removal of a vein segment is irrelevant for the patient’s health and comfort and lastly the vein wall and the posterior lamella can have the same thickness. For these reasons we began testing the venous graft as a replacement for tarsusconjunctival layer in wide full-thickness reconstructions. First outcomes were encouraging so this method turned out to be a useful new reconstructive opportunity.
Herein we report our own experience in the surgical treatment of 64 wide full-thickness defects of the eyelids carried out by venous wall grafts.
Materials and methods
Sixty-three patients, 39 men and 24 women, aged from 52 to 88 (mean age 73.5) with malignant eyelid tumors were treated, using the venous wall graft, in the Dermatology Unit of Ospedale degli Infermi in Biella (Italy) from 1999 to 2015. Moreover, one 73-year-old man, who had been previously operated on elsewhere for traumatic injury on the upper eyelid, was treated for scarring which had damaged the cornea.
The tumors were 45 basal cell carcinomas, 8 squamous cell carcinomas, 4 Merkel cell carcinomas, 1 lentigo malignant melanoma and 5 adenocarcinomas arising either in the conjunctiva or in Meibomian glands.
The neoplasms were located in the lower eyelid in 54 patients (85.7%) and in the upper eyelid in 4 patients (6.3%); 7 patients also had medial canthus involvement (11.1%), 9 lateral canthus involvement (14.1%), whereas in 5 cases (7.9%) the tumors involved both eyelids. Further details are reported in Table 1.
Most patients (54=84.3%) were primarily treated in our department whereas 10 patients (15.6%) primarily treated elsewhere were admitted for recurrence of the tumor or for resulting discomfort (post-traumatic patient).
In all cases the ciliary margin was involved, and the resection exceeded one fourth of the eyelid length.
Tumor size ranged from 7 to 45 mm (mean 14). Radical excision with a safe healthy-tissue margin was always carried out. In every case the extent of resection depended on the size, location of the tumor and above all on its pathological feature, so consequently the width of the surgical defects ranged from 15 to 60 mm.
The excised tissue was immediately evaluated by frozen section examination. The eyelid reconstruction proceeded after confirmation of clear margins.
Once the tumor was radically removed, we harvested the selected portion of the superficial vein. The choice of the vessel was beforehand investigated using ultrasound, which enables the surgeon to choose carefully a suitable donor vein undamaged and without valves and branches. This one must be as smooth as possible to obtain the best contact with the eye-globe. With ultrasonography the thickness and diameter of the vein can also be determined so that the dimensions of the selected vessel fit the structure to be replaced. Moreover, ultrasound examination is important to assess the integrity of the deep venous system before compromising the superficial one.
In our case report the grafts were obtained in 52 patients (81.3%) from the anterior saphenous vein and in the other 12 patients (18.7%) from the forearm (cephalic or basilic vein). The prevalence of the lower limb as donor site is due to the advanced age of our patients who had thinner vessels on the forearm. The groin site was the preferred choice, except for a single patient where we were compelled to choose the distal third of the leg.
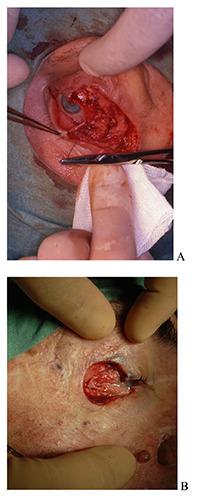
The graft was harvested through a short cutaneous incision; the vessel was blunt dissected to the necessary extent, clamped and tied at the extremes and then excised. The harvested tube was washed with saline solution, cut lengthwise to obtain a flat plate and inserted into the missing section of the posterior lamella placing the endothelium in contact with the bulbar conjunctiva. Through absorbable 7/0 suture the graft was fixed to the residual tarsus and the fascial plane (Figure 1). The stitches had to be placed away from the conjunctiva so that they would not protrude onto the internal surface, thereby preventing scratches on the cornea.
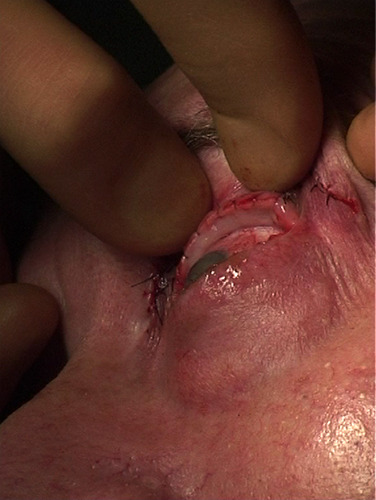
In 13 patients the venous grafts were also used to reconstruct the canthal tendon; in most cases the vein was sutured to the remaining, lateral or medial, stump but in 5 cases the whole lateral canthus was reconstructed. In these cases, the grafts were fixed directly to the orbital periosteum. The first two were realized with a couple of grafts, one for each eyelid, laterally sutured to each other and both to the Whitnall tubercle.5 (Figure 2A) Instead in the other three cases the canthal apparatus was obtained by folding a single graft in the shape of a sling and attaching the apex inside the orbital rim (Figure 2B).
The external lamella was reconstructed with various local flaps, preferring - when possible - myocutaneous flaps of orbicularis oculi muscle. For the upper eyelid, from the redundant skin, Burow triangle flap in 4 cases and advancement flap in 3 cases were used;6,7 Tenzel rotational flap was the solution in other 2 cases.8 For the lower eyelid 3 kinds of flaps were used as follows: Blaskovics rotational flap inferolaterally based in 34 cases,9 infero-medially based in 12 and Mustardé rotational cheek flap in 9 cases.10 In 5 cases there were also wide medial canthal defects that were repaired with various shapes of glabellar flaps.11,12 The flaps were sutured in standard layered fashion and, on the new edge, they were joined to the vein graft with few nonabsorbable stitches (Figure 3).
Eye occlusion dressing concluded the operation. Post-operative treatment consisted in systemic antibiotic therapy for 6 days and topical care with antibiotic ointment twice a day until the neovascularization of the graft which usually occurred within 5 days. No graft suffered vascular failure, but we could observe that the venous endothelium disappeared within 4 days, and it was replaced from day to day by the proliferation of the surrounding conjunctiva (Figure 4A,B). This process required different times depending on the surface sizes. However, it was always complete by the 14th day.
Local anesthesia was preferred in 23 cases (21 lower, 2 upper) whilst 10 cases also needed sedation; 41 patients underwent general anesthesia.
The hospitalization time varied in relation to the patient’s state and the extent of plastic surgery (2-7 days).
Clinical follow-up was carried out one month after surgery and then every quarter for two years, afterwards twice a year. Imaging check-ups were required just in case of clinical doubt of recurrence. The average duration of follow-up was 6.5 years; the shortest 3 years. Eight patients (12.5%) broke off the follow-up at our hospital after a period ranging from 4 to 12 months, mostly because they were living far away.
Figure 1.

The vein graft is being sutured to the remaining tarsus and fascial plane.
Figure 2.
A) Two vein grafts, one for each eyelid, are laterally sutured to each other to reconstruct the canthal tendon. B) A single folded graft supplies the canthal tendon and the missing interior lamella of both eyelids.
Results
No graft suffered vascular failure. We did not come up against any intraoperative complication either in the orbital site or in the donor site. There were few postoperative complications. In a patient in prophylaxis with nadroparin calcium (38 antiXa IU/kg twice a day) after pulmonary embolism a hematoma appeared which led to a partial necrosis of the external lamella (Mustardé rotational flap). The cutaneous loss required a skin graft one month later. In one case some deep stitches came to the conjunctival surface 6 weeks after surgery leading to corneal abrasion. In this case the stitches were readily removed, and the keratopathy healed by means of antibiotic and corticosteroid ointments. We also noted 5 unexpected events in the new margins: 2 short notches and 3 granulomas.
No patient with epithelial or conjunctival neoplasm or Merkel cell carcinoma developed recurrence, but this was observed after 2 years in the L.M.Melanoma case. Fortunately, the lesion was very small, in situ and on the cheek, far away from the eyelid. The recurrence was excised, and, at the fifth year of follow-up, the patient is disease free. One patient with a wide recurrence of Meibomian gland carcinoma, previously operated on elsewhere, developed a submandibular lymph node metastasis three months later. He underwent radical neck dissection and radiotherapy. At the fifth year of follow-up the patient is disease free.
No patient complained about unsatisfactory cosmetic or functional outcomes.
Discussion
In our experience venous wall graft turned up to be suitable for replacing the interior lamella, both as regards the conjunctival layer and the tarsal plate. This adaptability is due to the architectural and histological similarities between the wall of propulsive vein and the tarsus-conjunctival plane. Basically, the interior lamella is composed of the conjunctiva, consisting of a thin epithelium, and the tarsus made of dense connective tissue with a certain amount of elastic fibers.13 Similarly, the wall of the propulsive vein is composed of an intimal layer of endothelium (1-2 rows of cells) and a middle layer of dense connective tissue with many elastic fibers and some smooth muscular cells.4,14 Moreover, the vein has an adventitial layer made of soft connective, rich in vasa vasorum, which can be removed by adventitiectomy, but it was usually preserved because the vasa vasorum could facilitate the revascularization of the graft.
This structural resemblance makes the venous graft suitable because of its smoothness, elasticity, pliability and thinness (about 2-3 mm in a medium-sized vein that is 5 mm in diameter) so it perfectly fits the globe without damaging the bulbar conjunctiva and the cornea.
Unexpectedly we found that the intima of the grafted vein does not survive for long; 48-96 hours after its harvest, it necrotizes and comes off. Even while the graft is devoid of intima, it does not cause any reaction on the eyeball, thanks to the extreme smoothness of its surface. Then within 2 weeks the graft is totally coated by the proliferation of the surrounding conjunctiva. Opportunely this replacement secures a renovated conjunctival epithelium with goblet cells differentiation in vivo. The presence of a complete and functional lining contributes to maintain a good lubrication so that no patients needed artificial tears beyond the early postoperative period, on the average 4 weeks. For these reasons, in one case, we also used a particularly thin venous graft without adventitia to fill in missing bulbar conjunctiva (Figure 5). The loss of the intimal layer makes the behavior of the venous graft similar to a graft of naked cartilage,15 or of fascia temporalis,16 or lata, but compared with the latter three, the vein wall is more adaptable, more congruous in thickness and more consistent (Figure 6A,B). Unlike the cartilage the vein graft is also very suitable for repairing the canthal tendons and what is more it has no limits in length like some fascial donor sites where the harvest often involves greater discomfort and side effects. Finally, the venous graft revascularization is more reliable and rapid, in our opinion thanks to the abundant vasa vasorum pool, so we did not find any problem that could be connected to vascular failure.
Figure 3.
Same case as Figure 1: feature of the reconstructed eyelid at the end of surgery
Figure 4.
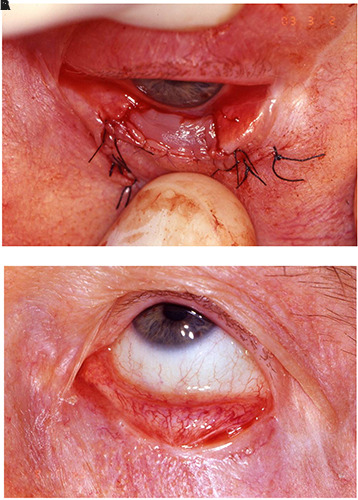
A) Feature of the vein graft just after surgery. B) one month later shows the proliferation of conjunctival epithelium over the vein graft.
Table 1.
Details collected from patients.
| Basal cell carcinoma |
Squamous cell carcinoma |
Conjunctival adenocarcinoma |
Meibomian gland carcinoma |
Merkel cell carcinoma |
Lentigo malignant melanoma |
Total | |
|---|---|---|---|---|---|---|---|
| Lower eyelid | 38 | 6 | 6 | 47 | |||
| Upper eyelid | 3 | 3 | |||||
| Lateral canthus + upper eyelid | 1 | 1 | |||||
| Medial canthus + lower eyelid | 4 | 4 | |||||
| Both canthi + lower eyelid | 1 | 1 | 1 | 3 | |||
| Lateral canthus + both eyelids | 3 | 1 | 1 | 5 | |||
| Total | 45 | 8 | 4 | 1 | 4 | 1 | 63 |
In our experience the dense connective tissue of the middle layer of the vein has proved to be an excellent replacement not only for the tarsus and the septal planes but also for the canthal apparatus. In 5 cases we anchored the graft to the periosteum, but it would also be possible to fix the vein directly to the bone using specific devices. Our proposed method saves every structure which has been left over after the tumor removal and does not involve other eyelid parts in the repair, the remaining ligamentous attachments of the canthi are spared. In fact, the venous wall graft never needs canthotomy.
The preoperative ultrasonography is essential in order to find a donor vein adequate in size and thickness as well as to assess the integrity of venous system in the limb and ensure that the donor vessel is devoid of branches, as straight as possible and undamaged. As regards the size, the venous graft can reach 16-22 mm in height in the anterior saphenous vein, that is about 6-8 mm in diameter at its proximal course. Therefore, with a vein graft it is possible to reconstruct the entire height of the upper eyelid. In length we can obtain whatever segment we need because, if we harvest the whole anterior saphenous vein, we will have at our disposal about 40 cm of vein. The average length of our harvests ranged from 6 to 24 cm.
Harvesting the vein, we must keep in mind that it is better for the graft to be slightly wider and longer than the palpebral loss because the grafted vein tends to contract in a manner compatible with its elasticity and the cicatricial retraction. In our cases we saw that the reconstructed eyelid became approximately 10% shorter. We did not observe any entropion in our patients and the depth of the recreated fornixes was always adequate in every case. In the same way no ectropion was noticed. Only in 2 cases we observed an incomplete eyelid closure with minimal lagophthalmos but no corneal damage. Thanks to its elasticity and thinness the venous graft does not impair the palpebral motility. Static parameters remained within physiological range: eyelid length ranged from 27 to 30 mm (mean 29.2). The results were long-term for the whole follow-up period.
Figure 5.

Two vein grafts are used to reconstruct both the lower eyelid and a portion of bulbar conjunctiva. The latter without adventitial layer.
Figure 6.
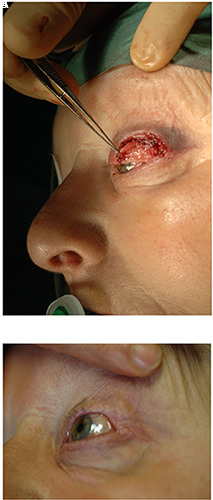
A) The interior lamella has just been repaired using a saphenous graft. B) One year after surgery.
Harvesting a vein segment means negligible damage in a healthy superficial venous network and not at all harmful if the harvest is carried out on the upper limb. For this reason, we must emphasize that we always examined firstly the forearm as a donor site and when the upper limb did not offer a suitable graft, we opted for the lower one (52 cases). Our first choice on the anterior saphenous vein was immediately below the femoral crossing. Only in one case our choice happened on the distal tract above the malleolus.
The venous graft does not need any tarsorrhaphy; but it is advisable to maintain eye occlusion dressing until the complete restoration of the conjunctival covering.
With the proposed method we avoided mutilations in important anatomical organs such as other eyelids, auricle, mouth, nose and fasciae which other reconstructions require.
We point out that our proposed method requires a single surgical session that, on average, takes 2 hours. The procedure does not require specific tools except for magnifying glasses.
Because of good functional and aesthetic results, paucity of complications and the absence of technical difficulties, we propose the venous wall graft for repairing wide, full-thickness defects of the eyelids after oncologic resection as well as consequence of burns, traumas and malformations.
Funding Statement
Funding: None.
References
- 1.Morales M, Ghaiy R, Itani K. Eyelid reconstruction. Selected Readings in Plastic Surgery 2010;11:1-43 [Google Scholar]
- 2.Mathijssen IM, van der Meulen JC. Guidelines for reconstruction of the eyelids and canthal regions. J Plast Reconstr Aesthet Surg 2010;63:1420– 33. [DOI] [PubMed] [Google Scholar]
- 3.Barbera C, Manzoni R, Dodaro L, et al. Reconstruction of the tarsus-conjunctival layer using a venous wall graft. Ophtal Plast Reconstr Surg 2008;24:352-56. [DOI] [PubMed] [Google Scholar]
- 4.Bucciante L. Histology of the venous wall. Symp Intern Morphol Istoch Paroi vasculaire. Fribourg 1965 Angiologica 1966;2:211-305 [Google Scholar]
- 5.Whitnall SE. Anatomy of the human orbit and accessory organs of vision. 2nd ed. London: Oxford University Press; 1932. [Google Scholar]
- 6.Gormley D.E. A brief analysis of the Burow’s wedge/triangle principle. J Dermatol Surg Oncol 1985;11:121-23. [DOI] [PubMed] [Google Scholar]
- 7.McGregor IA, Morgan G. Axial and random pattern flaps. Br J Plast Surg 1973;26:202-13. [DOI] [PubMed] [Google Scholar]
- 8.Tenzel RR, Steward WB. Eyelid reconstruction by the semicircle flap technique. Ophtalmology 1978;85:1164-69. [DOI] [PubMed] [Google Scholar]
- 9.Blaskovics L. About total reconstruction of lower eyelids. Z Augenheilk 1920;40:1-6 [Google Scholar]
- 10.Mustardé JC. Major reconstruction of the eyelids: functional and aesthetic considerations. Clin Plast Surg 1981;8:227-36. [PubMed] [Google Scholar]
- 11.Bertelmann E, Rieck P, Guthoff R. Medial canthal reconstruction by a modified glabellar flap. Ophtalmologica 2006;220:368-71. [DOI] [PubMed] [Google Scholar]
- 12.Meadows AE, Manners RM. A simple modification of the glabellar flap in medial canthal reconstruction. Ophtalmic Plast Reconstr Surg 2003; 19:313-15 [DOI] [PubMed] [Google Scholar]
- 13.Kersten R. Orbits, eyelids and lacrimal system: Section 7. In Purdy EP.American Academy of Ophtalmology Basic and Clinical Science Course. San Francisco: American Acad Ophtal; 2006:139. [Google Scholar]
- 14.Burton AC. Relation of structure to function of the tissues of the wall of the blood-vessels. Physiol Rev 1954;34: 619-42 [DOI] [PubMed] [Google Scholar]
- 15.Hashikawa K, Tahara S, Nakahara M, et al. Total lower lid support with auricular cartilage graft. Plast Reconstr Surg 2005;115:880-84 [DOI] [PubMed] [Google Scholar]
- 16.Holt JE, Holt GR, Van Kirk M. Use of temporalis fascia in eyelid reconstruction. Ophthalmology 1984;91:89-93. [DOI] [PubMed] [Google Scholar]


