Synopsis
An umbilical vein varix is a rare fetal condition and is defined as a focal dilatation of the umbilical vein.
Keywords: antepartum assessment, diagnostic ultrasound, obstetric complication, ultrasound Doppler
1. INTRODUCTION
An umbilical vein varix is defined as focal dilatation of the umbilical vein. Most cases of fetal umbilical vein varix are reported to be intra‐abdominal. Extra‐abdominal or intra‐amniotic umbilical vein varix is rare, with only a few case reports published in the literature.
Adverse fetal complications have been reported, including compression and kinking of the umbilical cord, aneurysm rupture, and thrombosis inside the aneurysm.
Owing to the rarity of this condition, there are no specific guidelines for its management during pregnancy, especially follow‐up intervals, or at the time of delivery.
2. CASE REPORT
We present the case of a 39‐year‐old woman with her sixth pregnancy who was admitted to our department at 35+5 weeks of pregnancy. Her obstetrical history included four term vaginal deliveries and one spontaneous abortion at the fifth week of pregnancy. Her medical and family histories were normal.
This study was approved by the ethics committee of Nazareth Hospital EMMS and the patient gave her consent for us to publish our case findings.
Close prenatal surveillance was performed because of morbid obesity and gestational diabetes mellitus. The second‐trimester triple marker test revealed a 1/271 risk for trisomy 21; amniocentesis for karyotyping was recommended, but the woman refused to consent. An anomaly scan at 22 weeks of pregnancy was normal.
Routine ultrasound performed on admission (35+5 weeks) showed the fetus with a vertex presentation. The estimated fetal weight was 2830 g (62nd centile), with a normal biophysical profile. Focal intra‐amniotic dilatation of the umbilical vein was observed with a dimension of 28 × 33 mm in the transverse section but without turbulent flow within the varix. The umbilical artery, middle cerebral artery, and ductus venosus Doppler findings were normal. At 36+2 weeks a detailed ultrasound was performed, including fetal echocardiography, which was normal. However, the varix was enlarged to 40.4 × 28 mm in the transverse section (Figures 1 and 2), and turbulence in the varix was observed (Figures 3 and 4).
FIGURE 1.

Ultrasound image of 36 weeks gestation shows abnormal dilation of the umbilical vein (intra‐amniotic vein varix).
FIGURE 2.
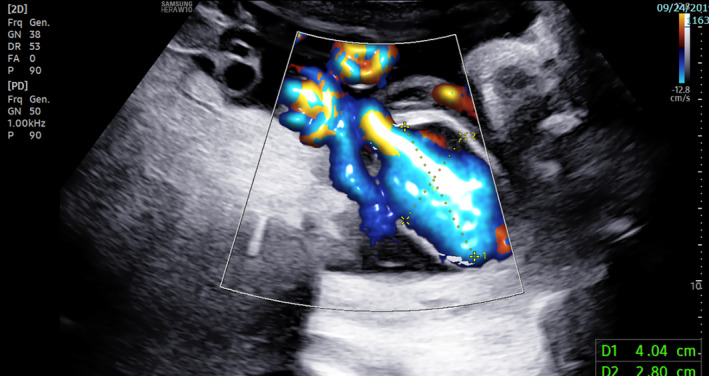
Ultrasonography image shows enlargement of the intra‐amniotic vein varix to 40.4 × 28 mm in the transverse section with color doppler.
FIGURE 3.
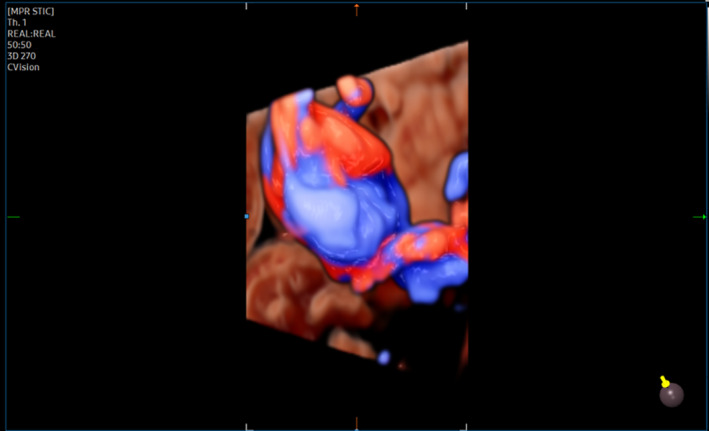
Three‐dimensional ultrasound imaging with color doppler shows turbulence flow in the intravascular area of the intra‐amniotic vein varix.
FIGURE 4.
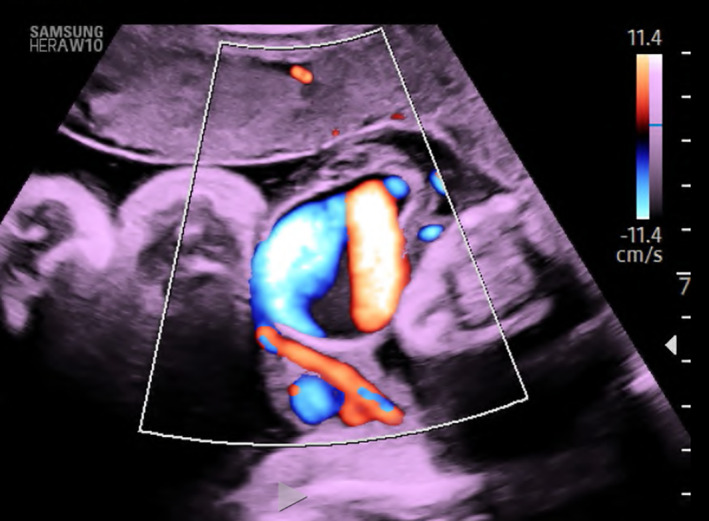
Ultrasound imaging with color doppler shows turbulence flow in the intravascular area of the intra‐amniotic vein varix.
As a result of the enlargement of the varix and the appearance of turbulent flow, we decided to deliver the premature baby after administration of betamethasone to the patient. After explaining the rarity of this finding and the lack of recommendations in the literature about the mode of delivery, the patient decided to deliver via cesarean section.
At 36+4 weeks, we performed a cesarean section and bilateral tubal ligation as requested. A healthy male baby was born, and the umbilical arterial pH was 7.36. The umbilical cord and placenta (Figures 5 and 6) were sent for histologic examination.
FIGURE 5.
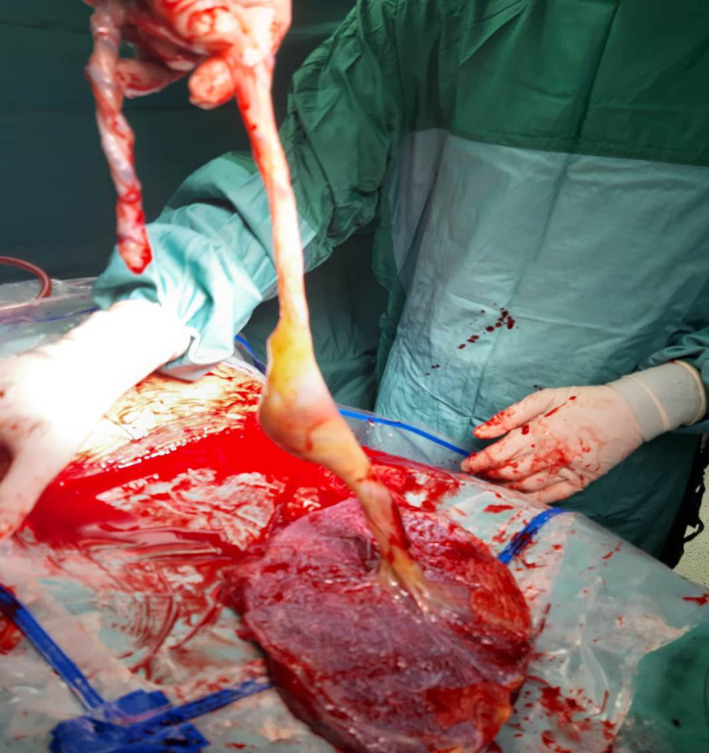
A photograph depicting a placenta with umbilical cord focal dilation.
FIGURE 6.
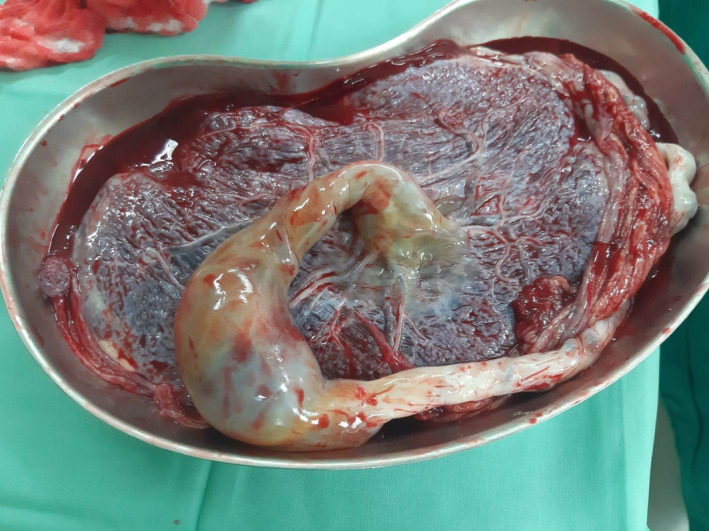
Umbilical cord with focal vein dilation of 60 mm in diameter.
Histopathologic examination showed a 43‐cm‐long, trivascular umbilical cord with focal vein dilatation of 60 mm diameter measured in the transverse section with central insertion to the placenta. The cross‐section of the placenta revealed intra‐placental infarcts with diffuse excess syncytial knots. The placenta had a diameter of 18 × 15 cm, with a maximum thickness of 4 cm and a weight of 662 g (Table 1).
TABLE 1.
Summary of published case reports of intra‐amniotic vein varix
| First author | GW at diagnosis | Delivery GW | Anomalies | Aneuploidy | UC length | Fetal outcome | Delivery |
|---|---|---|---|---|---|---|---|
| Ghosh (1984) 8 | 37 | 37 | NA | No | 100 | Stillbirth | Vaginal |
| Vesce (1987) 9 | 34 | 36 | No | No | 40 | Birth | CS |
| Schrocksnadel (1991) 10 | After delivery | term | NO | No | 70 | Stillbirth | NA |
| White (1994) 11 | 32 | 35 | SGA | NA | NA | Birth | NA |
| Shipp (1995) 12 | 24.5 | 34 | VSD, dilated SVC | NA | NA | Birth | NA |
| Vandevijver (2000) 13 | After delivery | 41 | No | NA | 50 | IUFD | Vaginal |
| Berg (2001) 14 | 34 | 34 | IUGR, Av fistula | Trisomy 18 | NA | Stillbirth | Vaginal |
| Cruise (2002) 15 | 24 | 32 | Klippel‐Trenaunay‐Weber syndrome | NA | NA | IUFD | NA |
| Zachariah (2004) 17 | After delivery | 41 | No | No | NA | Birth | Vaginal |
| Trobs (2012) 16 | 27 | 35 | DFG, SGA, and dilatation of left iliac vein | No | NA | Birth | CS |
| Akar (2012) 18 | 32 | TERM | No | NA | NA | Birth | CS |
| Kanenishi (2013) 7 | 35 | 35 | No | No | NA | Birth | CS |
| Jae hoon lee (2014) 2 | 34 | 35 | No | NA | 35 | Birth | CS |
| Deront‐bourdin (2014) 6 | 31 | 34 | No | NA | NA | Birth | CS |
| Schwaerzker (2016) 19 | 20 | 33 | SGA, omphalocele, anemia | no | NA | Birth | CS |
| Soriano (2015) 3 | 36 | 36 | NA | NA | NA | Birth | CS |
| Alessandro feola (2017) 1 | 39 | 39 | no | NA | 55 | IUFD | CS |
| Luis Humberto (2017) 4 | 38 | 38 | No | No | NA | IUFD | Vaginal |
| Yuuki Matsumoto (2019) 5 | 23 | 32 | No | No | NA | Birth | CS |
| The present study | 35.5 | 36.4 | No | No | 43 | Birth | CS |
Abbreviations: CS, Cesarean section; GW, gestational week; IUFD, intrauterine fetal death; IUGR, intrauterine growth restriction; NA, not announced; SGA, small for gestational age; SVC, superior vena cava; VSD, ventricular septal defect.
The baby was discharged without complications 6 days after birth and was normal at the 6‐month follow up.
3. DISCUSSION
We present a rare case of a fetus with an intra‐amniotic umbilical vein varix that was diagnosed and delivered in a late preterm infant with good perinatal outcomes.
Varix of the umbilical cord is a dilatation that can exist in any area across the umbilical cord or the hepatic part of the umbilical vein. It is a rare phenomenon with no known reasons. Doppler examination demonstrated turbulent flow within the aneurysm. Complications of the umbilical cord vein varix can cause fetal morbidity when thrombosis causes blockage of blood flow in the fetus and, consequently, fetal death.
To our knowledge, about 274 cases of fetal intra‐abdominal umbilical vein varix and 19 cases of intra‐amniotic umbilical vein aneurysms have been reported in the English‐language literature. Five of the 19 reported cases underwent vaginal delivery, including seven cases of intrauterine fetal death resulting from occlusion of the umbilical vein due to thrombosis and other anomalies.
The mean gestational age at the time of diagnosis of intra‐amniotic umbilical vein varix and time of delivery were 31+5 and 35 weeks of pregnancy, respectively.
Umbilical vein varix is also associated with congenital anomalies, cardiovascular anomalies, imperforate anus, congenital soft‐tissue disease (Klippel‐Trenaunay‐Weber syndrome), and trisomy 18.
In this case report, we describe an aneurysm of the umbilical cord vein that dilated rapidly during 4 days of follow up, with the appearance of turbulent flow. There are no guidelines in the literature regarding the follow up of these cases due to increased fetal morbidity, with few cases of fetal mortality described in previous studies. Therefore, we promoted delivery to avoid fetal death.
We suggest a close follow up, including fetal monitoring and ultrasound follow up, for signs of increased dilatation and the appearance of turbulent flow in the umbilical vein. The timing of delivery remains a challenging decision in the preterm period; however, we suggest considering delivery in late preterm infants in the presence of any suspicious signs that could cause fetal distress.
AUTHOR CONTRIBUTIONS
The study was designed and planned by Basel H. Nasser, Jimmy E. Jadaon, Yacoub Zakharian, and Daher Hamid, who also analyzed and interpreted the data, and wrote and revised the manuscript. All the authors read and approved the final manuscript.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
Nasser BH, Hamid D, Zakharian Y, Jadaon JE. Intra‐amniotic umbilical vein varix: A case report and review of the literature. Int J Gynecol Obstet. 2022;00:1‐5. doi: 10.1002/ijgo.14525
DATA AVAILABILITY STATEMENT
The data that supports the findings of this study are available in the supplementary material of this article.
REFERENCES
- 1. Feola A, De Stefano N, La Sala F, Pietra BD. Umbilical vein varix rupture: a case report and review of the literature. Rom J Leg Med. 2017;25:256‐259. [Google Scholar]
- 2. Lee JH, Cho JH, Kwon HY, Park YW, Kim YH. A huge umbilical vein aneurysm: case report and a brief review of literatures describing umbilical vessel aneurysm. Korean J Perinatol. 2014;25(3):178‐183. [Google Scholar]
- 3. Soriano‐Lillo P, Padilla‐V B‐R, Variz CV. Extra‐abdominal umbilical vein varix. A case report clinic. Ginecol Obstet Mex. 2015;83:356‐362. [PubMed] [Google Scholar]
- 4. Contreras LHC, Al‐Maghrabi HA, Martínez SC. Extra abdominal umbilical vein varix causing stillbirth: a case report. Annals of Pathology and Laboratory Medicine. 2017;4(3):2394‐6983. [Google Scholar]
- 5. Matsumoto Y, Yanai A, Kamei S, Yamaguchi A, Nakamine H, Fujita K. A case report of umbilical vein varix with thrombosis: prenatal Ultrasonographic diagnosis and management. Hindawi Case Rep Obstet Gynecol. 2019;2019:4. Article ID 7154560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Deront‐Bourdin F, Blanquiot JL, Checchi C, Nataf S, Bongain A, Umbilical vein varix thrombosis. Gynecol Obstet Fertil. 2014;42(6):448‐450. doi: 10.1016/j.gyobfe.2014.01.018 [DOI] [PubMed] [Google Scholar]
- 7. Kanenishi K, Nitta E, Mashima M, et al. Hdlive imaging of intra‐amniotic umbilical vein varix with thrombosis. 2013;34(11):1110‐1112. doi: 10.1016/j.placenta.2013.08.008 [DOI] [PubMed] [Google Scholar]
- 8. Ghosh A, Woo JSK, MacHenry C, Wan CW, O'Hoy KM, Ma HK. Fetal loss from umbilical cord abnormalities—a difficult case for prevention. Europ J Obstest Gynec Reorid Biol. 1984;18:183‐198. [DOI] [PubMed] [Google Scholar]
- 9. Vesce F, Guerrini P, Perri G, Gavazzini L, Simonetti V. Ultrasonographic diagnosis of ectasia of the umbilical vein. J Clin Ultrasound. 1987;15:346‐349. [DOI] [PubMed] [Google Scholar]
- 10. Schrocksnadel H, Holbock E, Mitterschiffthaler G, Totsch M, Dapunt O. Thrombotic occlusion of an umbilical vein varix causing fetal death. Arch Gynecol Obstet. 1991;248:213‐215. [DOI] [PubMed] [Google Scholar]
- 11. White SP, Kofinas A. Prenatal diagnosis and management of umbilical vein varix of the intra‐amniotic portion of the um‐ bilical vein. J Ultrasound Med. 1994;13:992‐994. [DOI] [PubMed] [Google Scholar]
- 12. Shipp TD, Bromley B, Benacerraf BR. Sonographically detect abnormalities of the umbilical cord. Int J Gynaecol Obstet. 1995;48:179‐185. [DOI] [PubMed] [Google Scholar]
- 13. Vandevijver NMA, Hermans RHM, Schrander‐Stumpel CCTRM, Arends JW, Peeters LLH, Moerman PL. Aneurysm of the umbilical vein: case report and review of literature. Eur J Obstet Gynecol Reprod Biol. 2000;89:85‐87. [DOI] [PubMed] [Google Scholar]
- 14. Berg C, Giepel A, Germer U, Gloekner‐Hoffmann K, Gembruch U. Prenatal diagnosis of umbilical cord aneurysm in a fetus with trisomy18. Ultrasound Obstet Gynecol. 2001;17:79‐81. [DOI] [PubMed] [Google Scholar]
- 15. Cruise K, Rouse G. Klippel‐Trenaunay‐weber syndrome complicated by extrafetal umbilical vein varix. J Diagn Med Sonogr. 2002;18:317‐320. [Google Scholar]
- 16. Tröbs RB. Pseudotumerous enlargement of the umbilical cord owing to an intra‐amniotic varicosity associated with thrombocytopenia. Journal of Pediatric Surgery. 2012;47(9):1760‐1762. [DOI] [PubMed] [Google Scholar]
- 17. Zachariah M. Umbilical vein varix thrombosis: a rare pathology. J Obstet Gynaecol. 2004;24(5):581. [DOI] [PubMed] [Google Scholar]
- 18. Akar M. Prenatally diagnosed umbilical vein aneurysm with good prognosis. J Clin Ultrasound. 2012;40(6):368‐369. [DOI] [PubMed] [Google Scholar]
- 19. Schwärzler P. Prenatal Diagnosis of Large Intra‐ and Extra‐Abdominal Umbilical Vein Aneurysm Complicated by Occluded Perforation with a Successful Outcome. Ultraschall Med. 2016;37(4):338‐342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that supports the findings of this study are available in the supplementary material of this article.


