Abstract
Involvement of the temporomandibular joint (TMJ) is common in juvenile idiopathic arthritis (JIA). TMJ arthritis can lead to orofacial symptoms, orofacial dysfunction, and dentofacial deformity with negative impact on quality of life. Management involves interdisciplinary collaboration. No current recommendations exist to guide clinical management. We undertook this study to develop consensus‐based interdisciplinary recommendations for management of orofacial manifestations of JIA, and to create a future research agenda related to management of TMJ arthritis in children with JIA. Recommendations were developed using online surveying of relevant stakeholders, systematic literature review, evidence‐informed generation of recommendations during 2 consensus meetings, and Delphi study iterations involving external experts. The process included disciplines involved in the care of orofacial manifestations of JIA: pediatric rheumatology, radiology, orthodontics, oral and maxillofacial surgery, orofacial pain specialists, and pediatric dentistry. Recommendations were accepted if agreement was >80% during a final Delphi study. Three overarching management principles and 12 recommendations for interdisciplinary management of orofacial manifestations of JIA were outlined. The 12 recommendations pertained to diagnosis (n = 4), treatment of TMJ arthritis (active TMJ inflammation) (n = 2), treatment of TMJ dysfunction and symptoms (n = 3), treatment of arthritis‐related dentofacial deformity (n = 2), and other aspects related to JIA (n = 1). Additionally, a future interdisciplinary research agenda was developed. These are the first interdisciplinary recommendations to guide clinical management of TMJ JIA. The 3 overarching principles and 12 recommendations fill an important gap in current clinical practice. They emphasize the importance of an interdisciplinary approach to diagnosis and management of orofacial manifestations of JIA.
INTRODUCTION
Temporomandibular joint (TMJ) arthritis is a frequent manifestation of juvenile idiopathic arthritis (JIA). TMJ arthritis often occurs early in the JIA disease course, and the inflammatory process and related orofacial signs and symptoms can persist into adulthood (1, 2, 3, 4, 5, 6, 7). Occasionally, TMJ arthritis is the only manifestation of JIA (8). Early TMJ arthritis may be asymptomatic, but many patients experience orofacial symptoms, orofacial dysfunction, and a decrease in quality of life as the disease progresses (1, 2, 3, 5, 6, 9, 10, 11, 12). In skeletally immature patients, TMJ arthritis can interfere with facial growth and development, resulting in dentofacial deformity (13, 14).
Management of the orofacial manifestations of TMJ arthritis requires an interdisciplinary care team which includes pediatric rheumatology, oral and maxillofacial surgery, orthodontics, radiology, pediatric dentistry, specialists in orofacial pain and jaw function, and others. In 2019, consensus‐based terminology specific to JIA‐associated TMJ arthritis was introduced (15). Standardization of terminology provides a platform for communication among the many healthcare providers involved in the integrative care of this condition, facilitates research, and may improve outcomes.
Management of TMJ arthritis varies widely in different regions and healthcare systems (16, 17); interdisciplinary consensus‐based recommendations to guide clinical decision‐making and standardize care are necessary. The objectives of this project were to develop interdisciplinary recommendations for management of orofacial manifestations of JIA and to create a future research agenda related to TMJ arthritis management in JIA.
MATERIALS AND METHODS
This study was conducted by a steering committee consisting of members of the Temporomandibular Joint Juvenile Arthritis Working Group (TMJaw), an international, interdisciplinary research network dedicated to the study of TMJ involvement in JIA. All task force members are experts in JIA‐associated TMJ arthritis within their respective professional fields. This study adheres to the consensus‐based terminology for JIA‐associated TMJ arthritis (15) (Table 1). Methodologic details are displayed in Figure 1.
Table 1.
Standardized, consensus‐based terminology for juvenile idiopathic arthritis (JIA)–associated temporomandibular joint (TMJ) arthritis*
| Terminology | Consensus‐based definition |
|---|---|
| TMJ arthritis | Active inflammation in the TMJ |
| TMJ involvement | Abnormalities presumed to be the result of TMJ arthritis |
| TMJ arthritis management | Diagnosis, treatment, and monitoring of TMJ arthritis and involvement |
| Dentofacial deformity | Abnormality in the growth, development, structure, and/or alignment of the facial bones and dentition |
| TMJ deformity | Abnormality in the growth, development, or structure of the osseous and/or soft tissue components of the TMJ |
| TMJ dysfunction | Physician‐reported functional examination abnormalities related to TMJ arthritis or involvement |
| TMJ symptoms | Patient or parent‐reported conditions related to TMJ arthritis or involvement |
The consensus‐based definitions are derived from ref. 15 (Stoustrup et al).
Figure 1.
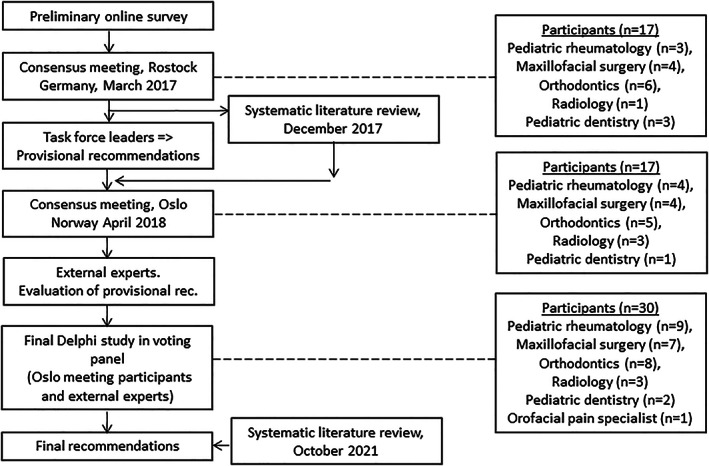
Outline of the consensus process for the development of interdisciplinary recommendations for the management of temporomandibular joint arthritis in children with juvenile idiopathic arthritis.
Prior to the first working group meeting, the steering committee distributed an online survey to TMJaw members using the Mentimeter survey system (Stockholm, Sweden) to determine the disciplines involved in the integrated care of orofacial manifestations of JIA within their healthcare systems. The core team (PS and MT) developed 4 standardized questions based on the online survey, and systematic reviews were performed to develop evidence‐based tables according to the modified Grading of Recommendations Assessment, Development and Evaluation (GRADE) method. An international TMJaw task force assembled in Rostock, Germany in March 2017 (17 participants representing 10 countries in Europe and North America), including representatives from each discipline represented in the initial survey. During the initial meeting, the project was outlined (Figure 1). Target populations for future recommendations were defined as 1) healthcare professionals involved in the integrative care of TMJ arthritis and related manifestations and 2) public health authorities and policy makers. Working groups of 3 to 5 members were formed, representing pediatric rheumatology, radiology, orthodontics, maxillofacial surgery, and pediatric dentistry. Working groups were provided with the 4 standardized questions and the literature search and asked to answer the predefined research questions (Table 2), and to recommend principles to guide clinical decision‐making and grade the evidence level for those principles.
Table 2.
Tasks relevant to the management of temporomandibular joint (TMJ) arthritis in patients with juvenile idiopathic arthritis (JIA) addressed by the working groups after the 2017 Rostock meeting*
| Working group tasks | |
|---|---|
| 1 | Define orofacial diagnostic/treatment strategies relevant for the management of JIA in the TMJ and the related conditions |
| 2 | Define indications for these management strategies (imaging, radiologic, clinical indications) |
| 3 | Define contraindications for these management strategies (imaging, radiologic, clinical indications) |
| 4 | Define, if relevant, specifications on how to conduct these management strategies |
Working groups were provided with these 4 predefined standardized research questions and a literature search and tasked with providing principles to guide clinical decision‐making and grade the evidence level for each principle.
The results of the working group were combined to guide the proposal of preliminary recommendations for diagnosis and management of TMJ arthritis. Three overarching consensus‐based principles were created. Additionally, specific preliminary recommendations were formulated for each of 5 relevant domains, including domains for diagnosis (domain I; n = 4), treatment of TMJ arthritis (domain II; n = 2), treatment of TMJ dysfunction and symptoms related to JIA (domain III; n = 3), treatment of arthritis‐related dentofacial deformity (domain IV; n = 2), and other orofacial aspects related to JIA (domain V; n = 1).
The preliminary recommendations were discussed at a subsequent task force meeting in Oslo, Norway in April 2018. The task force consisted of 17 participants representing 5 specialties (Figure 1). Subsequently, the overarching principles and provisional recommendations were refined using a task force–driven consensus process involving nominal group techniques and 2 Delphi iterations.
Following the Oslo meeting, external experts (n = 13) who were previously not involved in the process were invited to assess the content validity of the provisional recommendations. These experts were identified based on internationally recognized clinical expertise and general contribution to research and publications related to TMJ arthritis in JIA. The external experts were asked to comment on the provisional recommendations and suggest improvements. Feedback from this exercise was incorporated into the next round of recommendations.
As a final step, the participants from the Oslo meeting (n = 17) and the external experts (n = 13) formed a voting panel which completed 3 online Delphi iterations and agreed upon a final set of recommendations. Characteristics of the voting panel are in Figure 1. The members of the voting panel assessed the perceived strength of each recommendation (SoR) based on a visual analog scale (VAS) scale (0 = no SoR, 10 = great SoR). Recommendations receiving agreement from ≥80% of the voting panel members were accepted. The level of evidence (LoE) of each recommendation was assessed using the Oxford Centre for Evidence‐Based Medicine (OCEBM) level of evidence table (18).
All members of the voting panel were invited to formulate items for a future research agenda. During the Delphi iterations, the level of importance of each proposed research item was assessed using a 0–10‐point VAS (0 = not important, 10 = extremely important). Only items receiving a mean level of importance VAS score of ≥7 were included on the future research agenda.
An updated systematic literature review was conducted in October 2021 to determine if any new literature was identified supporting or contradicting each of the specific management recommendations. The new literature identified did not lead to any changes in the recommendations.
RESULTS
This process generated 3 overarching principles and 12 recommendations pertaining to the 5 following domains: domain I (diagnosis); domain II (treatment of TMJ arthritis, defined as active TMJ inflammation); domain III (treatment of TMJ dysfunction and symptoms); domain IV (treatment of arthritis‐related dentofacial deformity); and domain V (other related aspects) (Table 3). A full reference list for articles supporting the generation of each of the 12 recommendations is available in the Supplementary Material on the Arthritis & Rheumatology website at http://onlinelibrary.wiley.com/doi/10.1002/art.42338.
Table 3.
Recommendations for the management of temporomandibular joint (TMJ) arthritis and the related orofacial manifestations of juvenile idiopathic arthritis (JIA)
| Recommendations | Level of evidence* | SoR† | Agreement |
|---|---|---|---|
| Overarching principles | |||
| TMJ arthritis is a common finding in patients with JIA and standardized evaluation is recommended. | – | – | 100% |
| Goals of management are to 1) provide timely diagnosis of TMJ arthritis and TMJ involvement, 2) reduce TMJ inflammation, 3) reduce TMJ arthritis–related symptoms and dysfunction, 4) normalize dentofacial development, and 5) address dentofacial deformities. | – | – | 100% |
| Optimal TMJ arthritis management requires an interdisciplinary approach and longitudinal evaluation into adulthood regardless of the current TMJ disease activity. | – | – | 100% |
| Diagnosis | |||
| Contrast‐enhanced MRI is currently the best method to detect active TMJ arthritis. | 2 | 8.4 ± 2.1 | 94% |
| Patient (or proxy) history should be used to assess TMJ involvement. While often absent, orofacial symptoms should be regularly reassessed. A standardized approach is recommended. | 3 | 8.8 ± 2.2 | 100% |
| Clinical examination should be used to diagnose TMJ arthritis–related dysfunction; a standardized approach is recommended to monitor changes over time. | 3 | 8.5 ± 2.7 | 100% |
| All patients should be evaluated for dentofacial deformity; a standardized approach is recommended to monitor changes over time. | 3 | 8.9 ± 2 | 100% |
| Treatment of TMJ arthritis (active TMJ inflammation) | |||
| Optimal systemic treatment should be considered for active TMJ arthritis in patients with JIA. | 4 | 7.9 ± 2.4 | 90% |
| Skeletally immature patients: Intraarticular glucocorticoid injection is not recommended as first‐line management of TMJ arthritis in skeletally immature patients. Intraarticular glucocorticoids may be used cautiously in patients with refractory TMJ arthritis and orofacial symptoms. Repeated glucocorticoid injection is not recommended. | 2 | 8.3 ± 2.5 | 97% |
| Skeletally mature patients: Intraarticular glucocorticoid injection may be indicated in skeletally mature patients with active TMJ arthritis and orofacial symptoms. | 4 | 7.7 ± 2.4 | 87% |
| Treatment of TMJ dysfunction and symptoms | |||
| Occlusal splints and/or physical therapy may be beneficial in patients with orofacial symptoms and/or TMJ dysfunction. | 4 | 8.3 ± 2.2 | 100% |
| Intraarticular glucocorticoid injection may be indicated in arthritis‐induced refractory and symptomatic TMJ dysfunction, but is not recommended for first‐line management in skeletally immature patients (see recommendation 6). | 2 | 7.4 ± 2.7 | 87% |
| Intraarticular lavage (without steroid) may be beneficial for TMJ arthritis–related symptoms and dysfunction. Lavage without steroid can be used in both growing and skeletally mature patients. No additional effect of lavage with steroid injection has been reported. | 4 | 6.5 ± 2.6 | 90% |
| Treatment of arthritis‐related dentofacial deformity | |||
| Dentofacial orthopedics and orthodontics may improve facial development, occlusion, and function in skeletally immature patients. | 4 | 8.1 ± 2.5 | 100% |
| Skeletal surgery may be indicated in skeletally immature and skeletally mature patients with dentofacial deformities and quiescent/controlled TMJ arthritis. | 4 | 8.1 ± 2.4 | 97% |
| Other | |||
| Screening and monitoring of the oral cavity with a focus on dental decay, gingivitis, and ulcerations are recommended. | 3 | 6.5 ± 3.4 | 84% |
Level of evidence according to criteria from the Oxford Center of Evidence Based Medicine (1 = highest evidence level, 5 = lowest evidence level). MRI = magnetic resonance imaging.
Mean ± SD strength of recommendation (SoR) is based on a visual analog scale of 0–10, with 0 being no SoR and 10 being great SoR.
Level of evidence
The LoEs provided in the available literature with regard to support of these principles and recommendations varied, falling at either steps 2, 3, or 4 on the OCEBM level of evidence table (ranging from step 1 [highest LoE] to step 5 [lowest LoE]) (18); in general, the LoEs were low. Hence, this proposal should be regarded as conditional where the voting panel finds that the desirable effects outweigh the undesirable effects, but the members of the panel appreciate that uncertainties exist related to resources, settings, and costs (19, 20).
Overarching principles
The 3 overarching principles represent a contemporary view on the management of TMJ arthritis and the related orofacial manifestations of JIA. These principles serve as a framework for the specific recommendations that follow.
Overarching principle A
TMJ arthritis is a common finding in patients with JIA and standardized evaluation is recommended. No population‐based studies exist on this matter. Estimates from non–population‐based studies (n > 100 participants) indicate that a substantial proportion of subjects with JIA have TMJ inflammation (termed “TMJ arthritis”), with prevalence ranging between 34% and 43% (1, 2, 3). The voting panels acknowledge that this estimate is subject to uncertainty due to methodologic differences, such as differences in patient populations. Other studies have reported >50% prevalence of TMJ arthritis in patients with JIA. However, these estimates mostly originated from studies with smaller sample sizes that included patients from the pre–biologic era, studies characterized by unspecified diagnostic MRI criteria, and studies in which patients with clinical and/or radiologic signs of previous TMJ arthritis (termed “TMJ involvement”) are also included in the estimates (21).
Overarching principle B
Goals of management are to 1) provide timely diagnosis of TMJ arthritis and TMJ involvement, 2) reduce TMJ inflammation, 3) reduce TMJ arthritis–related symptoms and dysfunction, 4) normalize dentofacial development, and 5) address dentofacial deformities. Timely diagnosis and resolution of TMJ inflammation are pivotal management objectives. Additionally, orofacial symptoms and dysfunction and dentofacial deformity that results from prior TMJ arthritis can persist and progress even after active arthritis has been managed. These sequelae have a significant negative impact on health‐related quality of life, and as such they must be equally included in management principles (9, 10, 11).
Overarching principle C
Optimal management of TMJ arthritis requires an interdisciplinary approach and longitudinal evaluation of patients from childhood into adulthood, regardless of their current TMJ disease activity. Interdisciplinary management is important for optimal patient outcomes, though it is recognized that the availability and expertise of providers and the accessibility of resources (e.g., government programs, health insurance) may vary by region and healthcare setting. The voting panel stresses the importance of implementing orofacial health evaluations in general JIA health assessments and the management of JIA.
Specific recommendations
Diagnosis and monitoring
Timely diagnosis is a critical first step in the management of TMJ arthritis and the related orofacial manifestations. Monitoring orofacial health in patients with TMJ involvement requires a standardized approach. No method of assessment can stand alone. Optimal TMJ monitoring should involve multiple modalities of assessment, including different aspects of patient history and clinical examination, patient‐reported outcomes, and imaging and radiology (15). Recommendations 1–4 (see below) refer to the diagnosis of TMJ arthritis and longitudinal monitoring of orofacial health.
Recommendation 1
Contrast‐enhanced magnetic resonance imaging (MRI) is currently the best method to detect active TMJ arthritis (LoE 2, mean ± SD SoR 8.4 ± 2.1). This recommendation specifies “active” TMJ inflammation to differentiate from TMJ involvement without active inflammation (Table 1) (15). The use of JIA‐specific TMJ MRI protocols and scoring systems is recommended (22, 23, 24, 25). It is recognized that the interpretation of MRI findings has an element of subjectivity and is influenced by the technique and equipment used for image capture, as well as by the expertise of the reader. Additional standardization of both image acquisition and interpretation is needed. It is stressed that the presence of a small amount of TMJ fluid and/or minor contrast enhancement may be considered a normal variation in a healthy TMJ, rather than a sign of active TMJ arthritis (26, 27, 28).
Ultrasonography is operator‐dependent and appears to have limited sensitivity to detect TMJ inflammation in patients with JIA (29, 30, 31, 32). Future research is needed to elucidate the role of ultrasonography in the diagnosis and monitoring of JIA and TMJ arthritis.
This recommendation is consistent with the 2019 interdisciplinary consensus‐based recommendation on the method of assessment of TMJ arthritis (15, 33). The voting panel acknowledges that accurate patient history (recommendation 2) and clinical orofacial examination (recommendation 3) may often precede imaging in the diagnostic sequence for TMJ arthritis.
Recommendation 2
Patient (or proxy) history should be used to assess involvement of the TMJ in JIA. While often absent, orofacial symptoms should be regularly reassessed. A standardized approach is recommended (LoE 3, mean ± SD SoR 8.8 ± 2.2). JIA‐specific tools such as the Childhood Health Assessment Questionnaire, the Juvenile Arthritis Disease Activity Score, and the Juvenile Arthritis Multidimensional Assessment Report are popular tools used for general disease assessment (34, 35, 36). However, because these tools provide limited or no assessment of the orofacial manifestations of JIA, TMJ and orofacial conditions may be overlooked.
Recommendation 3
Clinical examination should be used to diagnose TMJ arthritis–related dysfunction; a standardized approach is recommended to monitor changes over time (LoE 3, mean ± SD SoR 8.5 ± 2.7). Orofacial examination aids timely diagnosis and facilitates longitudinal monitoring of patients with existing TMJ involvement. While the use of orofacial examination alone for the diagnosis of TMJ involvement in JIA is limited, examination remains an important form of screening to inform the need for further diagnostic evaluation and serves as a low‐cost method for serial follow‐up. Additionally, orofacial examination improves the assessment of response to therapy and the evaluation of treatment options (33). A standardized orofacial examination approach that complies with consensus‐based standards is recommended (33). A consensus‐based JIA‐specific orofacial examination protocol was recently published (37).
Recommendation 4
All patients should be evaluated for dentofacial deformity; a standardized approach for evaluation is recommended to monitor changes in facial morphology over time (LoE 3, mean ± SD SoR 8.9 ± 2.0). Dentofacial deformity is a common complication of JIA. This occurs most frequently in patients who experience TMJ arthritis/involvement prior to reaching skeletal maturity (6, 38, 39). Assessment of facial morphology can be conducted during a clinical examination or by 3‐dimensional imaging and a conventional radiologic examination (15), in accordance with consensus‐based standards (33, 37). Progressive deviation in the mandibular morphology and facial profiles (e.g., mandibular asymmetry/retrognathia) of patients with JIA should prompt further radiographic examination and/or referral.
No protocol exists to guide decision‐making regarding the indications, timing, and frequency of TMJ imaging. Currently, radiologic evaluation of TMJ and facial morphology are variable and provider‐dependent. Assessment of TMJ and dentofacial deformities should adhere to consensus‐based standards (22, 40).
Treatment of TMJ arthritis (active TMJ inflammation)
Recommendations 5 and 6 (see below) refer to the management of TMJ inflammation (termed “TMJ arthritis”) (Table 1). Resolution of TMJ arthritis is considered a key component to optimal TMJ arthritis management.
Recommendation 5
The optimal systemic treatment should be considered for active TMJ arthritis in patients with JIA (LoE 4, mean ± SD SoR 7.9 ± 2.4). Longitudinal observational studies have reported a beneficial effect of systemic immunosuppressive therapy on TMJ arthritis, mandibular growth, and the progression of TMJ deformity (41, 42). The term “optimal” in this recommendation reflects the fact that the current level of evidence is insufficient to direct the administration of specific modalities. Empiric, early, and aggressive systemic treatment of TMJ arthritis is recommended, as this may reduce TMJ arthritis–related sequelae. Hence, TMJ disease status should be considered when determining the optimal systemic medical therapy to be used to treat all manifestations of JIA.
Recommendation 6a for skeletally immature patients
Intraarticular glucocorticoid injection is not recommended as the first‐line treatment for the management of TMJ arthritis in skeletally immature patients. Intraarticular glucocorticoids may be used cautiously in patients with refractory TMJ arthritis and orofacial symptoms. Repeated glucocorticoid injection is not recommended (LoE 2, mean ± SD SoR 8.3 ± 2.5).
Recommendation 6b for skeletally mature patients
Intraarticular glucocorticoid injection may be indicated in skeletally mature patients with active TMJ arthritis and orofacial symptoms (LoE 4, mean ± SD SoR 7.7 ± 2.4). Controversy prevails over the use of intraarticular glucocorticoid injections for the treatment of TMJ arthritis in growing patients (43). Longitudinal observational studies have demonstrated an antiinflammatory effect of intraarticular glucocorticoid injections in JIA patients with TMJ arthritis (44, 45). However, outcomes are variable and the effect is considered to be temporary and not curative (44, 45, 46, 47, 48). The voting panel stresses the importance of reducing inflammatory activity in the TMJ as early as possible to prevent signs and symptoms of TMJ arthritis, cartilage and bone tissue destruction, and growth inhibition. However, the side effects of TMJ intraarticular glucocorticoid injections are not yet fully understood. Recent research has suggested that the risks of the suppression of mandibular growth and/or the development of intraarticular calcifications may outweigh the antiinflammatory benefits of TMJ intraarticular glucocorticoid injection, particularly in skeletally immature patients (44, 45, 46, 49). A precautionary approach to the use of TMJ intraarticular glucocorticoid injection in skeletally immature patients is therefore recommended.
In skeletally mature patients, TMJ intraarticular glucocorticoid injections have been reported to have beneficial antiinflammatory effects without significant side effects (50). However, as in skeletally immature patients, the effects were temporary and not curative. The risk of side effects associated with TMJ intraarticular glucocorticoid injections in skeletally mature patients requires further investigation. At this point, TMJ intraarticular glucocorticoid injections may be used in skeletally mature patients with signs of TMJ arthritis on MRI and orofacial symptoms who have had an inadequate response to other treatment modalities (44, 50).
Treatment of TMJ symptoms and dysfunction
The relationship between the presence and severity of TMJ arthritis and the development of orofacial signs and symptoms is unclear (33, 51), because many patients with TMJ inflammation will not manifest orofacial symptoms. Conversely, orofacial signs/symptoms can progress in well‐treated patients without MRI evidence of TMJ inflammation (33, 51). A potential mechanistic model is that the sequelae of previous TMJ arthritis (e.g., TMJ deformity) may cause mechanical overloading of the TMJ during function. In turn, mechanical dysfunction can lead to orofacial signs and symptoms despite the absence of TMJ inflammation (52). The mechanism for the relationship between arthritis and symptoms requires further study. Given the dissociation between arthritic activity and orofacial signs and symptoms, it is essential to monitor and address TMJ‐related dysfunction and symptoms regardless of TMJ inflammatory status.
Recommendation 7
Occlusal splints and/or physical therapy may be beneficial in patients with orofacial symptoms and/or TMJ dysfunction (LoE 4, mean ± SD SoR 8.3 ± 2.2). Data from longitudinal observational case series have documented significant improvement in JIA‐related orofacial dysfunction and symptoms after treatment with oral splints, although the complete resolution of pain is rare (53, 54, 55). The design of the oral splint varied between studies (e.g., activators and flat stabilizing splints). Regardless of splint design, this treatment modality is considered reversible, safe, and of low cost in most healthcare settings (55). Oral splints also play a role in the treatment of dentofacial deformity (see recommendation 10).
No data exist regarding the effect of physiotherapy on JIA‐related orofacial signs and symptoms. Physiotherapy and jaw exercises are evidence‐based treatments for related conditions such as other temporomandibular dysfunctions, and can reasonably be extrapolated to patients with JIA‐related orofacial symptoms (56). The recommendation for the use of orofacial physiotherapy for JIA is solely based on empirical evidence and mechanism‐based reasoning (LoE 5). This is a subject of further study. In summary, splint therapy and physiotherapy are considered safe and reversible modalities for the management of orofacial signs and symptoms in JIA patients, and are therefore recommended despite a low level of evidence.
Recommendation 8
Intraarticular glucocorticoid injection may be indicated in arthritis‐induced refractory and symptomatic TMJ dysfunction, but is not recommended as first‐line management in skeletally immature patients (LoE 2, mean ± SD SoR 7.4 ± 2.7). Recommendation 8 relates to the role of TMJ intraarticular glucocorticoid injections in the management of TMJ symptoms and dysfunction in patients with refractory (active) TMJ arthritis, as opposed to recommendations 6a and b which relate to the management of TMJ inflammation. Longitudinal observational studies have demonstrated pain relief and improvement in TMJ function after intraarticular glucocorticoid injection to the TMJ (44, 45). Likewise, intraarticular glucocorticoid injection has been shown to decrease short‐term TMJ inflammation based on MRI (44, 45). However, as discussed earlier, the effects and the duration of the benefits of intraarticular glucocorticoid injections on the signs and symptoms of TMJ dysfunction are highly variable and temporary (44, 45, 46, 47, 48). The risk of side effects has been discussed above (see recommendations 6a and b).
Despite controversy regarding the use of TMJ intraarticular glucocorticoid injections, they are still indicated in specific circumstances (e.g., arthritis‐induced refractory and symptomatic TMJ dysfunction). The use of this treatment modality calls for special attention to the risks and benefits of the technique and to the level of skeletal maturity of the patient. Further study may help to clarify the role of this technique.
Recommendation 9
Intraarticular lavage (without steroids) may be beneficial for TMJ arthritis–related symptoms and dysfunction. Lavage without steroids can be used in both growing and skeletally mature patients. No additional effect of lavage with steroid injection has been reported (LoE 4, mean ± SD SoR 6.5 ± 2.6). In 2 prospective longitudinal case series, the effect of TMJ lavage (with or without steroid treatment) was studied in patients with MRI‐verified TMJ arthritis (44, 57). Temporary pain relief and improvement in TMJ function have been demonstrated, though outcomes are highly variable and benefits may be time‐limited. Complete resolution of orofacial signs and symptoms following this treatment is rare. The available literature indicates that there are limited benefits when steroids are added to the lavage procedure, and the addition of steroids is not routinely recommended (see recommendations 6 and 8). No severe side effects have been reported with TMJ lavage without steroid in JIA patients.
The limited evidence for this recommendation is acknowledged, and more evidence is needed to differentiate between the efficacy of the procedure compared to the placebo effect resulting from an operative intervention. This recommendation is made to provide clinicians with an option for the management of orofacial pain and dysfunction that has an improved safety profile in comparison to TMJ intraarticular glucocorticoid injection. Further studies are needed to determine the role of TMJ lavage in the management of JIA‐related TMJ arthritis.
Treatment of dentofacial deformity
TMJ arthritis impacts mandibular growth and development (38, 39, 40, 58). The severity of dentofacial deformity depends on the timing of the onset of TMJ arthritis in relation to growth trajectory and laterality (unilateral/bilateral). JIA‐induced dentofacial deformities can occur early in the disease course (6). As for orofacial signs and symptoms, the relationship between the severity of TMJ arthritis and the severity of dentofacial deformity is indirect and incompletely understood (6, 59). The severity of dentofacial deformity and the degree of skeletal maturity is a major factor in decision‐making with regard to disease management (38, 39, 58, 60, 61).
Recommendation 10
Dentofacial orthopedics and orthodontics may improve facial development, occlusion, and function in skeletally immature patients (LoE 4, mean ± SD SoR 8.1 ± 2.5). Observational studies have documented the benefits of dentofacial orthopedic appliances (oral splints) for the management of minor‐to‐moderate dentofacial deformities resulting from JIA (61, 62, 63, 64, 65). These splints are used in growing patients with the aim of supporting normal mandibular growth and occlusal development (52). Clinical evidence suggests that the optimal effect of this modality is achieved by initiating treatment early in the development of dentofacial deformity (65). Splints are used in conjunction with antiinflammatory therapies for active TMJ arthritis.
The use of oral splints may normalize minor‐to‐moderate dentofacial deformities and may have a preventative effect against the worsening of the deformity. This approach is therefore recommended for interceptive treatment of early dentofacial deformities in JIA (60, 61, 62, 64, 65). However, the availability of this treatment varies by region and healthcare setting. Other barriers exist and have been discussed elsewhere (52).
Little is known about the effects of orthodontic treatment with fixed orthodontic appliances (braces) in patients with JIA (61, 64, 66). However, orthodontic treatment is mainly considered as a modality to establish dental occlusion after the use of orthopedic appliances or in conjunction with surgical correction. Fixed appliance orthodontic treatment may also be used to correct minor malocclusions separately from orthopedic or surgical treatment. This is a subject for further recommendations from the TMJaw group.
Recommendation 11
Skeletal surgery may be indicated in skeletally immature and skeletally mature patients with dentofacial deformities and quiescent/controlled TMJ arthritis (LoE 4, mean ± SD SoR 8.1 ± 2.4). Surgical procedures aim to correct dentofacial deformities related to TMJ arthritis/involvement. The available surgical modalities have been systematically reviewed by Frid et al (67). There are 3 general surgical approaches, as follows: 1) mandibular distraction osteogenesis, 2) orthognathic surgery with TMJ preservation, and 3) TMJ reconstruction with autologous or alloplastic implants. A combination of these surgical modalities may be used. The current scientific evidence is scarce, and the choice of surgical approach varies widely. The selection of the surgical method used for the management of dentofacial deformity resulting from TMJ arthritis is influenced by the skeletal maturity of the patient, the level of TMJ inflammatory activity, the stability of the TMJ and dentofacial deformity, and the preference and experience of the surgeon (67). Resnick et al recently presented a consensus‐based algorithm for the management of dentofacial deformity resulting from JIA (60). The algorithm proposes a conceptual framework for an interdisciplinary approach involving the use of dentofacial orthopedic appliances and surgical management.
Other recommendation 12
Screening and monitoring of the oral cavity with a focus on dental decay, gingivitis, and ulcerations are recommended (LoE 3, mean ± SD SoR 6.5 ± 3.4). Recommendation 12 is directed toward the oral consequences of JIA and is not specifically for patients with TMJ arthritis/involvement. The impact of JIA on oral health was recently systematically reviewed by Skeie et al (68). The relationship between JIA and oral health conditions is not completely understood. However, there is evidence that periodontal disease (e.g., gingival inflammation, periodontitis) is more prevalent in patients with JIA compared to healthy controls (68, 69, 70). An association between JIA and dental caries has not been established (68). Little is known about the relationship between periodontal conditions and JIA (68, 69). Cross‐talk between the oral microbiota and the immune response has been suggested in the setting of rheumatoid arthritis, and periodontal pathogens have been considered a trigger of the autoimmune reaction in patients with rheumatoid arthritis (71, 72). The influence of the oral microbiota in the setting of JIA has only just begun to be investigated (73). Further investigation is needed before a bidirectional relationship between periodontal conditions and JIA can be established.
Future research agenda
A comprehensive research agenda was developed to provide a framework for future interdisciplinary research efforts. The full list of agenda items is provided in Table 4.
Table 4.
Proposal for a future research agenda on TMJ arthritis in patients with JIA*
| Future research agenda | Level of importance |
|---|---|
| Etiology and diagnosis of TMJ arthritis | |
| Identification of biomarkers for TMJ disease progression and treatment response | 8.7 |
| Effect of inflammation on facial growth | 8.6 |
| Differentiating JIA‐induced TMJ arthritis from idiopathic condylar resorption | 7.9 |
| Clinical diagnosis of TMJ arthritis | 7.6 |
| TMJ imaging | |
| Standardization of MRI assessment | 9.4 |
| Develop noninvasive diagnostic imaging techniques for young/noncooperative children | 7.9 |
| Systemic treatment of TMJ arthritis | |
| Prospective evaluation of systemic therapy on TMJ arthritis: methotrexate versus biologics as first‐line therapy | 8.2 |
| Orthopedic/orthodontic treatment of dentofacial deformity | |
| Effect of different types of orthopedic appliances (oral splints) for treatment of dentofacial deformity | 8.3 |
| Determine optimal developmental stage for initiation of orthopedic/orthodontic treatment with oral splints. | 7.7 |
| Surgical treatment of dentofacial deformity | |
| Prospective evaluation of surgical treatment modalities for arthritis‐related dentofacial deformity | 7.8 |
| Intraarticular treatment of TMJ arthritis | |
| Impact of intraarticular steroid on condylar growth | 7.9 |
| Study the effects of intraarticular administration drug therapy | 7.7 |
| Controlled randomized trial of intraarticular lavage and steroids versus intraarticular lavage alone versus control | 7.6 |
| Guidelines and protocols | |
| Develop an interdisciplinary management algorithm for TMJ arthritis management | 8.2 |
| Develop recommendations for monitoring orofacial health in JIA | 8.2 |
| Tutorial instruction video for standardized orofacial examination | 7.4 |
| Develop orofacial examination protocol for small children (2–5 years old) with JIA | 7.4 |
| Patient‐reported outcome | |
| Study quality of life of patients and families with JIA and TMJ arthritis | 8.4 |
| Study the burden of care for patients with TMJ arthritis/TMJ involvement/dentofacial deformity | 8 |
Levels of importance were assessed using a 10‐point visual analog scale, with 0 being not important and 10 being extremely important. See Table 3 for definitions.
DISCUSSION
These are the first interdisciplinary recommendations for the management of JIA‐related TMJ arthritis and the associated orofacial manifestations. Despite a lack of high‐level evidence, we created the 3 overarching principles and 12 recommendations outlined above to try to address the clinical questions clinicians are struggling with when treating patients with JIA‐associated TMJ arthritis. This article is considered to be a working document, with plans for revision as new evidence emerges. The 2021 American College of Rheumatology (ACR) guideline for the treatment of JIA was recently published and included therapeutic approaches for TMJ arthritis (74). Both the 2021 ACR guideline and the recommendations in this review caution against the use of intraarticular glucocorticoid injections in skeletally immature patients and the use of biologic DMARDs in patients who have had an insufficient response to synthetic DMARDs. In addition to the 2021 ACR treatment guideline, our recommendations include evidence not only for therapeutic approaches, but also for orthopedic devices, orthodontic devices, and surgical interventions for the management of JIA‐associated TMJ arthritis and the related manifestations.
Due to the low quality of available evidence, all recommendations are considered to be conditional to denote the uncertainty regarding the balance of benefits and harms (75). The proposed research agenda constitutes a framework for future interdisciplinary research efforts to improve the evidence of care. It is presented in the form of specific research questions to make the future research relevant and directly applicable to clinical practice. Future research should also focus on the burden of care and consider the cost‐effectiveness of the proposed diagnostic and treatment modalities. The proposed areas of study are suggestions and are not intended to exclude other research questions.
Optimal management of TMJ arthritis and the associated manifestations requires an interdisciplinary approach and should be recognized as an integrated part of contemporary JIA disease control. Management strategies should be individualized according to the specific JIA‐related orofacial manifestations of each patient. The voting panel highlights the importance of shared decision‐making involving patients, parents, and clinicians in defining targets of treatment and approaches to management. We acknowledge that management may vary by region and healthcare system. The voting panel hopes that the current recommendations help to facilitate a process for specialties to collaborate on local and national strategies for the management of TMJ arthritis and related orofacial manifestations. Furthermore, we hope that the current recommendations will increase attention to this common manifestation of JIA disease (1, 2, 5, 6).
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Drs. Stoustrup and Twilt had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Stoustrup, Resnick, Abramowicz, Pedersen, Twilt.
Acquisition of data
Stoustrup, Resnick, Abramowicz, Pedersen, Michelotti, Küseler, Koos, Verna, Nordal, Granquist, Halbig, Kristensen, Kaban, Arvidsson, Spiegel, Stoll, Lerman, Glerup, Defabianis, Frid, Alstergren, Cron, Ringold, Nørholt, Peltomaki, Larheim, Herlin, Peacock, Kellenberger, Twilt.
Analysis and interpretation of data
Stoustrup, Resnick, Abramowicz, Pedersen, Michelotti, Küseler, Koos, Verna, Nordal, Granquist, Halbig, Kristensen, Kaban, Arvidsson, Spiegel, Stoll, Lerman, Glerup, Defabianis, Frid, Alstergren, Cron, Ringold, Nørholt, Peltomaki, Larheim, Herlin, Peacock, Kellenberger, Twilt.
Supporting information
Disclosure Form
Appendix S1 Supplementary Material
Author disclosures are available at https://onlinelibrary.wiley.com/action/downloadSupplement?doi=10.1002%2Fart.42338&file=art42338‐sup‐0001‐Disclosureform.pdf.
REFERENCES
- 1. Cannizzaro E, Schroeder S, Müller LM, et al. Temporomandibular joint involvement in children with juvenile idiopathic arthritis. J Rheumatol 2011;38:510–5. [DOI] [PubMed] [Google Scholar]
- 2. Stoll ML, Sharpe T, Beukelman T, et al. Risk factors for temporomandibular joint arthritis in children with juvenile idiopathic arthritis. J Rheumatol 2012;39:1880–7. [DOI] [PubMed] [Google Scholar]
- 3. Von Schuckmann L, Klotsche J, Suling A, et al. Temporomandibular joint involvement in patients with juvenile idiopathic arthritis: a retrospective chart review. Scand J Rheumatol 2020;49:271–80. [DOI] [PubMed] [Google Scholar]
- 4. Arvidsson LZ, Smith HJ, Flato B, et al. Temporomandibular joint findings in adults with long‐standing juvenile idiopathic arthritis: CT and MR imaging assessment. Radiology 2010;256:191–200. [DOI] [PubMed] [Google Scholar]
- 5. Glerup M, Stoustrup P, Matzen LH, et al. Longterm outcomes of temporomandibular joints in juvenile idiopathic arthritis: 17 years of followup of a Nordic juvenile idiopathic arthritis cohort. J Rheumatol 2020;47:730–8. [DOI] [PubMed] [Google Scholar]
- 6. Stoustrup P, Glerup M, Bilgrau AE, et al. Cumulative incidence of orofacial manifestations in early juvenile idiopathic arthritis: a regional, three‐year cohort study. Arthritis Care Res (Hoboken) 2020;72:907–16. [DOI] [PubMed] [Google Scholar]
- 7. Weiss PF, Arabshahi B, Johnson A, et al. High prevalence of temporomandibular joint arthritis at disease onset in children with juvenile idiopathic arthritis, as detected by magnetic resonance imaging but not by ultrasound. Arthritis Rheum 2008;58:1189–96. [DOI] [PubMed] [Google Scholar]
- 8. Hugle B, Spiegel L, Hotte J, et al. Isolated arthritis of the temporomandibular joint as the initial manifestation of juvenile idiopathic arthritis. J Rheumatol 2017;44:1632–5. [DOI] [PubMed] [Google Scholar]
- 9. Frid P, Nordal E, Bovis F, et al. Temporomandibular joint involvement in association with quality of life, disability, and high disease activity in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken) 2017;69:677–86. [DOI] [PubMed] [Google Scholar]
- 10. Rahimi H, Twilt M, Herlin T, et al. Orofacial symptoms and oral health‐related quality of life in juvenile idiopathic arthritis: a two‐year prospective observational study. Pediatr Rheumatol Online J 2018;16:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carlsson AD, Wahlund K, Kindgren E, et al. Orofacial pain in juvenile idiopathic arthritis is associated with stress as well as psychosocial and functional limitations. Pediatr Rheumatol Online J 2019;17:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fischer J, Skeie MS, Rosendahl K, et al. Prevalence of temporomandibular disorder in children and adolescents with juvenile idiopathic arthritis: a Norwegian cross‐sectional multicentre study. BMC Oral Health 2020;20:282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stoustrup P, Traberg MS, Matzen LH, et al. Initial radiological signs of dentofacial deformity in juvenile idiopathic arthritis. Sci Rep 2021;11:13142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Von Bremen J, Ruf S. Juvenile idiopathic arthritis‐and now?: a systematic literature review of changes in craniofacial morphology. J Orofac Orthop 2012;73:265–76. [DOI] [PubMed] [Google Scholar]
- 15. Stoustrup P, Resnick CM, Pedersen TK, et al. Standardizing terminology and assessment for orofacial conditions in juvenile idiopathic arthritis: international, multidisciplinary consensus‐based recommendations. J Rheumatol 2019;46:518–22. [DOI] [PubMed] [Google Scholar]
- 16. Foeldvari I, Tzaribachev N, Cron RQ. Results of a multinational survey regarding the diagnosis and treatment of temporomandibular joint involvement in juvenile idiopathic arthritis. Pediatr Rheumatol Online J 2014;25;12:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kinard BE, Abramowicz S. Juvenile idiopathic arthritis practice patterns among oral and maxillofacial surgeons. J Oral Maxillofac Surg 2017;75:2333.e1–8. [DOI] [PubMed] [Google Scholar]
- 18. Howick J, Chalmers I, Glasziou P, et al. OCEBM Levels of Evidence Working Group . “The Oxford 2011 Levels of Evidence.” Oxford Centre for Evidence‐Based Medicine. URL: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. [Google Scholar]
- 19. Andrews J, Guyatt G, Oxman AD, et al. GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. J Clin Epidemiol 2013;66:719–25. [DOI] [PubMed] [Google Scholar]
- 20. Andrews JC, Schünemann HJ, Oxman AD, et al. GRADE guidelines: 15. Going from evidence to recommendation‐determinants of a recommendation's direction and strength. J Clin Epidemiol 2013;66:726–35. [DOI] [PubMed] [Google Scholar]
- 21. Larheim TA, Doria AS, Kirkhus E, et al. TMJ imaging in JIA patients—An overview. Semin Orthod 2015;21:102–10. [Google Scholar]
- 22. Kellenberger CJ, Junhasavasdikul T, Tolend M, et al. Temporomandibular joint atlas for detection and grading of juvenile idiopathic arthritis involvement by magnetic resonance imaging. Pediatr Radiol 2018;48:411–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tolend M, Junhasavasdikul T, Cron RQ, et al. Discrete choice experiment on a magnetic resonance imaging scoring system for temporomandibular joints in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken) 2021;74:308–16. [DOI] [PubMed] [Google Scholar]
- 24. Tolend MA, Twilt M, Cron RQ, et al. Toward establishing a standardized magnetic resonance imaging scoring system for temporomandibular joints in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken) 2018;70:758–67. [DOI] [PubMed] [Google Scholar]
- 25. Tolend M, Doria AS, Meyers AB, et al. Assessing the reliability of the OMERACT juvenile idiopathic arthritis magnetic resonance scoring system for temporomandibular joints (JAMRIS‐TMJ). J Clin Med 2021;10:4047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Angenete OW, Augdal TA, Jellestad S, et al. Normal magnetic resonance appearances of the temporomandibular joints in children and young adults aged 2‐18 years. Pediatr Radiol 2018;48:341–9. [DOI] [PubMed] [Google Scholar]
- 27. Kottke R, Saurenmann RK, Schneider MM, et al. Contrast‐enhanced MRI of the temporomandibular joint: findings in children without juvenile idiopathic arthritis. Acta Radiol 2015;56:1145–52. [DOI] [PubMed] [Google Scholar]
- 28. Stoll ML, Guleria S, Mannion ML, et al. Defining the normal appearance of the temporomandibular joints by magnetic resonance imaging with contrast: a comparative study of children with and without juvenile idiopathic arthritis. Pediatr Rheumatol Online J 2018;16:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hechler BL, Phero JA, Van Mater H, et al. Ultrasound versus magnetic resonance imaging of the temporomandibular joint in juvenile idiopathic arthritis: a systematic review. Int J Oral Maxillofac Surg 2018;47:83–9. [DOI] [PubMed] [Google Scholar]
- 30. Muller L, Kellenberger CJ, Cannizzaro E, et al. Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: a pilot study comparing clinical examination and ultrasound to magnetic resonance imaging. Rheumatology (Oxford) 2009;48:680–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zwir LF, Terreri MT, do Amaral EC, et al. Is power Doppler ultrasound useful to evaluate temporomandibular joint inflammatory activity in juvenile idiopathic arthritis? Clin Rheumatol 2020;39:1237–40. [DOI] [PubMed] [Google Scholar]
- 32. Kirkhus E, Gunderson RB, Smith HJ, et al. Temporomandibular joint involvement in childhood arthritis: comparison of ultrasonography‐assessed capsular width and MRI‐assessed synovitis. Dentomaxillofac Radiol 2016;45:20160195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Stoustrup P, Twilt M, Spiegel L, et al. Clinical orofacial examination in juvenile idiopathic arthritis: International consensus‐based recommendations for monitoring patients in clinical practice and research studies. J Rheumatol 2017;44:326–33. [DOI] [PubMed] [Google Scholar]
- 34. Consolaro A, Ruperto N, Bazso A, et al. Development and validation of a composite disease activity score for juvenile idiopathic arthritis. Arthritis Rheum. 2009;61:658–66. [DOI] [PubMed] [Google Scholar]
- 35. Filocamo G, Consolaro A, Schiappapietra B, et al. A new approach to clinical care of juvenile idiopathic arthritis: the Juvenile Arthritis Multidimensional Assessment Report. J Rheumatol 2011;38:938–53. [DOI] [PubMed] [Google Scholar]
- 36. Ruperto N, Ravelli A, Pistorio A, et al. Cross‐cultural adaptation and psychometric evaluation of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ) in 32 countries. Review of the general methodology. Clin Exp Rheumatol 2001;19:S1–9. [PubMed] [Google Scholar]
- 37. Stoustrup P, Herlin T, Spiegel L, et al. Standardizing the clinical orofacial examination in juvenile idiopathic arthritis: an interdisciplinary, consensus‐based, short screening protocol. J Rheumatol 2020;47:1397–404. [DOI] [PubMed] [Google Scholar]
- 38. Fjeld MG, Arvidsson LZ, Smith HJ, et al. Relationship between disease course in the temporomandibular joints and mandibular growth rotation in patients with juvenile idiopathic arthritis followed from childhood to adulthood. Pediatr Rheumatol Online J 2010. 22;8:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fjeld MG, Arvidsson LZ, Stabrun AE, et al. Average craniofacial development from 6 to 35 years of age in a mixed group of patients with juvenile idiopathic arthritis. Acta Odontol Scand 2009;67:153–60. [DOI] [PubMed] [Google Scholar]
- 40. Stoustrup P, Iversen CK, Kristensen KD, et al. Assessment of dentofacial growth deviation in juvenile idiopathic arthritis: reliability and validity of three‐dimensional morphometric measures. PloS One 2018;13:e0194177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bollhalder A, Patcas R, Eichenberger M, et al. Magnetic resonance imaging followup of temporomandibular joint inflammation, deformation, and mandibular growth in juvenile idiopathic arthritis patients receiving systemic treatment. J Rheumatol 2020;47:909–16. [DOI] [PubMed] [Google Scholar]
- 42. Ince DO, Ince A, Moore TL. Effect of methotrexate on the temporomandibular joint and facial morphology in juvenile rheumatoid arthritis patients. Am J Orthod Dentofacial Orthop 2000;118:75–83. [DOI] [PubMed] [Google Scholar]
- 43. Resnick CM, Pedersen TK, Abramowicz S, et al. Time to reconsider management of the temporomandibular joint in juvenile idiopathic arthritis. J Oral Maxillofac Surg 2018;76:1145–6. [DOI] [PubMed] [Google Scholar]
- 44. Antonarakis GS, Blanc A, Courvoisier DS, et al. Effect of intra‐articular corticosteroid injections on pain and mouth opening in juvenile idiopathic arthritis with temporomandibular involvement: a systematic review and meta‐analysis. J Craniomaxillofac Surg 2020;48:772–8. [DOI] [PubMed] [Google Scholar]
- 45. Stoustrup P, Kristensen KD, Verna C, et al. Intra‐articular steroid injection for temporomandibular joint arthritis in juvenile idiopathic arthritis: a systematic review on efficacy and safety. Semin Arthritis Rheum 2013;43:63–70. [DOI] [PubMed] [Google Scholar]
- 46. Lochbühler N, Saurenmann RK, Müller L, et al. Magnetic resonance imaging assessment of temporomandibular joint involvement and mandibular growth following corticosteroid injection in juvenile idiopathic arthritis. J Rheumatol 2015;42:1514–22. [DOI] [PubMed] [Google Scholar]
- 47. Resnick CM, Vakilian PM, Kaban LB, et al. Quantifying the effect of temporomandibular joint intra‐articular steroid injection on synovial enhancement in juvenile idiopathic arthritis. J Oral Maxillofac Surg 2016;74:2363–9. [DOI] [PubMed] [Google Scholar]
- 48. Stoustrup P, Kristensen KD, Küseler A, et al. Temporomandibular joint steroid injections in patients with juvenile idiopathic arthritis: an observational pilot study on the long‐term effect on signs and symptoms. Pediatr Rheumatol Online J 2015;13:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Stoll ML, Amin D, Powell KK, et al. Risk factors for intraarticular heterotopic bone formation in the temporomandibular joint in juvenile idiopathic arthritis. J Rheumatol 2018;45:1301–7. [DOI] [PubMed] [Google Scholar]
- 50. Frid P, Augdal TA, Larheim TA, et al. Efficacy and safety of intraarticular corticosteroid injections in adolescents with juvenile idiopathic arthritis in the temporomandibular joint: a Norwegian 2‐year prospective multicenter pilot study. Pediatr Rheumatol Online J 2020;18:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kristensen KD, Stoustrup P, Küseler A, et al. Clinical predictors of temporomandibular joint arthritis in juvenile idiopathic arthritis: a systematic literature review. Semin Arthritis Rheum 2016;45:717–32. [DOI] [PubMed] [Google Scholar]
- 52. Stoustrup P, Pedersen TK, Nørholt SE, et al. Interdisciplinary management of dentofacial deformity in juvenile idiopathic arthritis. Oral Maxillofac Surg Clin North Am 2020;32:117–34. [DOI] [PubMed] [Google Scholar]
- 53. Isola G, Ramaglia L, Cordasco G, et al. The effect of a functional appliance in the management of temporomandibular joint disorders in patients with juvenile idiopathic arthritis. Minerva Stomatol 2017;66:1–8. [DOI] [PubMed] [Google Scholar]
- 54. Portelli M, Matarese G, Militi A, et al. Temporomandibular joint involvement in a cohort of patients with Juvenile Idiopatic Arthritis and evaluation of the effect induced by functional orthodontic appliance: clinical and radiographic investigation. Eur J Paediatr Dent 2014;15:63–6. [PubMed] [Google Scholar]
- 55. Stoustrup P, Kristensen KD, Kuseler A, et al. Management of temporomandibular joint arthritis‐related orofacial symptoms in juvenile idiopathic arthritis by the use of a stabilization splint. Scand J Rheumatol 2014;43:137–45. [DOI] [PubMed] [Google Scholar]
- 56. Lindfors E, Arima T, Baad‐Hansen L, et al. Jaw exercises in the treatment of temporomandibular disorders: an international modified delphi study. J Oral Facial Pain Headache 2019;33:389–98. [DOI] [PubMed] [Google Scholar]
- 57. Olsen‐Bergem H, Bjørnland T. A cohort study of patients with juvenile idiopathic arthritis and arthritis of the temporomandibular joint: outcome of arthrocentesis with and without the use of steroids. Int J Oral Maxillofac Surg 2014;43:990–5. [DOI] [PubMed] [Google Scholar]
- 58. Arvidsson LZ, Fjeld MG, Smith HJ, et al. Craniofacial growth disturbance is related to temporomandibular joint abnormality in patients with juvenile idiopathic arthritis, but normal facial profile was also found at the 27‐year follow‐up. Scand J Rheumatol 2010;39:373–9. [DOI] [PubMed] [Google Scholar]
- 59. Stoustrup PB, Ahlefeldt‐Laurvig‐Lehn N, Kristensen KD, et al. No association between types of unilateral mandibular condylar abnormalities and facial asymmetry in orthopedic‐treated patients with juvenile idiopathic arthritis. Am J Orthod Dentofacial Orthop 2018;153:214–23. [DOI] [PubMed] [Google Scholar]
- 60. Resnick CM, Frid P, Norholt SE, et al. An algorithm for management of dentofacial deformity resulting from juvenile idiopathic arthritis: results of a multinational consensus conference. J Oral Maxillofac Surg. 2019;77:1152.e1–33. [DOI] [PubMed] [Google Scholar]
- 61. Von Bremen J, Ruf S. Orthodontic and dentofacial orthopedic management of juvenile idiopathic arthritis: a systematic review of the literature. Orthod Craniofac Res 2011;14:107–15. [DOI] [PubMed] [Google Scholar]
- 62. Farronato G, Carletti V, Maspero C, et al. Craniofacial growth in children affected by juvenile idiopathic arthritis involving the temporomandibular joint: functional therapy management. J Clin Pediatr Dent 2009;33:351–7. [DOI] [PubMed] [Google Scholar]
- 63. Isola G, Ramaglia L, Cordasco G, et al. The effect of a functional appliance in the management of temporomandibular joint disorders in patients with juvenile idiopathic arthritis. Minerva Stomatol 2017;66:1–8. [DOI] [PubMed] [Google Scholar]
- 64. Kjellberg H, Kiliaridis S, Thilander B. Dentofacial growth in orthodontically treated and untreated children with juvenile chronic arthritis (JCA). A comparison with Angle Class II division 1 subjects. Eur J Orthod 1995;17:357–73. [DOI] [PubMed] [Google Scholar]
- 65. Stoustrup P, Kuseler A, Kristensen KD, et al. Orthopaedic splint treatment can reduce mandibular asymmetry caused by unilateral temporomandibular involvement in juvenile idiopathic arthritis Eur J Orthod 2013;35:191–8. [DOI] [PubMed] [Google Scholar]
- 66. Abate A, Cavagnetto D, Rusconi FM, et al. Safety and effects of the rapid maxillary expander on temporomandibular joint in subjects affected by juvenile idiopathic arthritis: a retrospective study. Children (Basel) 2021;8:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Frid P, Resnick C, Abramowicz S, et al. Surgical correction of dentofacial deformities in juvenile idiopathic arthritis: a systematic literature review. Int J Oral Maxillofac Surg 2019;48:1032–42. [DOI] [PubMed] [Google Scholar]
- 68. Skeie MS, Gil EG, Cetrelli L, et al. Oral health in children and adolescents with juvenile idiopathic arthritis: a systematic review and meta‐analysis. BMC Oral Health 2019;19:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Grevich S, Lee P, Leroux B, et al. Oral health and plaque microbial profile in juvenile idiopathic arthritis. Pediatr Rheumatol Online J 2019;17:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Merle CL, Hoffmann R, Schmickler J, et al. Comprehensive assessment of orofacial health and disease related parameters in adolescents with juvenile idiopathic arthritis: a cross‐sectional study. J Clin Med 2020;9:513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Hussain SB, Botelho J, Machado V, et al. Is there a bidirectional association between rheumatoid arthritis and periodontitis? A systematic review and meta‐analysis. Semin Arthritis Rheum 2020;50:414–22. [DOI] [PubMed] [Google Scholar]
- 72. Potempa J, Mydel P, Koziel J. The case for periodontitis in the pathogenesis of rheumatoid arthritis [review]. Nat Rev Rheumatol 2017;13:606–20. [DOI] [PubMed] [Google Scholar]
- 73. Frid P, Baraniya D, Halbig J, et al. Salivary oral microbiome of children with juvenile idiopathic arthritis: a Norwegian cross‐sectional study. Front Cell Infect Microbiol 2020;10:602239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Onel KB, Horton DB, Lovell DJ, et al. American College of Rheumatology Guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for oligoarthritis, temporomandibular joint arthritis, and systemic juvenile idiopathic arthritis. Arthritis Rheumatol 2022;74:553–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. World Health Organization . WHO handbook for guideline development, 2nd ed; 2014. URL: https://apps.who.int/iris/handle/10665/145714.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure Form
Appendix S1 Supplementary Material


