Abstract
This article explores the potential of using systems methods for better conceptualizing the unexpected and complex sets of hurdles and opportunities that practicing psychologists frequently encounter. Examples are provided involving two distinct types of important clinical issues: 1) understanding how individuals maintain recovery from substance use disorders following treatment and 2) better understanding patients with chronic, unexplained post-viral illnesses. Traditional research methods used to explore these types of intricate social and medical issues have often lacked sophisticated dynamic systems-based perspectives, which could provide new insights into understanding how patient treatment gains can be maintained and how unexplained post-viral illnesses can be better understood. Our examples will demonstrate that systems-oriented approaches have the potential to provide psychologists unique opportunities to capture a fuller and richer depiction of a variety of clinical and community topics and thus provide new lenses that ultimately could provide better care for our patients.
The behavior of all our patients is deeply rooted in and affected by social environments, whether it is a child dealing with academic difficulties, a parent with a substance use disorder, or a community faced with unacceptable levels of violence. A systems perspective points us toward the realization that behavior is always embedded within ecological levels of analysis, including the person, group, organization, community, and society, and changes to one part of a system will affect other parts (Kelly, 2006). Failing to appreciate their influence on the individual can compromise our best intended interventions. In this article, we will illustrate how system perspectives can help clarify these types of complicated interactions that occur in the work of psychologists.
From its birth, the field of community psychology has dealt with systems, and its practitioners and theorists have tried to understand the bidirectional influence of the environment (and community-based structures) on individuals (Jason & Glenwick, 2016; Revenson & Seidman, 2002). Community psychology “theories” have often served primarily as orienting frameworks (Jason, Stevens, Ram, Miller, Beasley, & Gleason, 2016) that help to better understand these person-setting interactions and ecological layers of analysis. In clinical practice, recognizing these ecological issues provides a clearer insight on a vast number of clinical issues, such as non-compliance (e.g., as when a person released from prison or jail fails to attend therapy appointments due to unstable housing) (Substance Abuse and Mental Health Services Administration, 2017).
In this article, we provide several illustrative examples of efforts to capture the interrelationships of ecological levels of analysis, which we believe can ultimately lead to improved assessment and practice. We will show how systems analysis helps us to better describe, explain, and predict complex behaviors when treating a range of patients, including those with substance use disorders and those with unexplained post-viral disorders.
Dynamic Social Models in Recovery Settings
Our first example involves substance use disorder recovery homes, which often house residents with histories of chronic health conditions, homelessness, psychiatric comorbidity, and criminal justice involvement , who are thus at risk for contracting a number of diseases, including COVID-19. It is estimated that in the United States, recovery homes provide aftercare treatment to over 270,000 individuals with substance use disorders each year (Jason, Wiedbusch, et al., 2020). We have found that longer stays in these homes lead to better outcomes, particularly stays longer than 6 months (Jason, Olson, Ferrari, Majer, Alvarez, & Stout, 2007), and a systems perspective might help elucidate the reasons why some residents are able to stay longer and have more successful outcomes, which may help residents stay for longer periods of time.
Typically, issues like social support within a variety of naturalistic recovery communities have been addressed by assuming that the social environment is fixed over the timeframe of the study (Kingry-Westergaard & Kelly, 1990). This approach may make sense when the social environment in question changes on a much slower time scale than the individual behaviors and attitudes that comprise it - for instance, if the social environment in question is quite large (a city or country, sometimes even a neighborhood, or perhaps a highly structured, professionally-run treatment center). However, recovery house social environments tend to change more quickly in response to resident turnover, as well as individual change, because they are relatively small (7–10 individuals, generally) and highly interdependent by design, both socially and instrumentally (Polcin, Korcha, Bond, Galloway, & Lapp, 2010). Thus, to understand the role of social support in recovery homes, frameworks are required that allow both individual and social-ecological factors to change and affect each other over time.
Social Network Terminology
In studying whole social networks of recovery home residents, there are several terms that need to be operationally defined (Ripley et al., 2021). First, there are relationship patterns of bidirectionality, with each resident (ego) rating every other person in the house (alters). Each resident is referred to as a node and each relationship between the nodes of a dyad is referred to as an edge.Since each resident (ego) provides ratings on all other residents (alters), when working with whole networks, the raters may indicate different strengths of relationships, such that A’s rating of B is considered a different measure of the relationship than B’s rating of A (Marsden, 2011). Reciprocity measures the tendency for mutual (bidirectional) connection in a relationship whereas Density measures the interconnections in a related network(Wasserman & Faust, 1994). These are just a few examples of the types of dynamic, system-oriented measures that are possible with social network analysis (Jason, Guerrero, Lynch, Stevens, Salomon-Amend, & Light, 2020). Below we provide statistical approaches for analyzing these dynamic types of data.
Stochastic Actor Oriented Modeling
The Stochastic Actor Oriented Modeling (SAOM) framework (Snijders, van de Bunt & Steglich, 2010) was developed specifically for understanding social network systems like those that exist in classrooms or other group settings. The SAOM provides a framework for understanding both individual characteristics and the evolving structure of social networks in complex systems. The SAOM framework can be used to unpack mechanisms of social integration as they pertain to recovery from substance use disorders. This approach has been applied to studies of recovery homes (Doogan, Light, Stevens & Jason, 2019; Jason, Light, et al., 2013; Light et al., 2016; Stevens, Guerrero, Green, & Jason, 2018), carried out by a multidisciplinary team that included John Light, a sociologist with expertise in SAOM and social networks, Nathan Doogan, a social worker with expertise in SAOM and simulations, Ed Stevens, a community psychologists with interests in sense of community, Mike Stoolmiller, a statistician, and Leonard Jason, a clinical-community psychologist. We will now provide an example of using this dynamic approach to understanding the mechanisms of what occurs within recovery homes.
Oxford House Recovery Homes
Some recovery homes, such as Oxford Houses, provide comprehensive, self-governing social environments for residents (Oxford House Inc, 2021). There are over 3,000 of these houses in the US that are democratically run. Houses are rented, and residents are required to pay their fair share of expenses, abide by house rules, and remain abstinent from alcohol and illicit drugs. Though potentially augmented by non-resident family and friends, these recovery environments are often specifically intended to provide possibly difficult-to-find companionship for those attempting the perilous transition from early sobriety to self-sustaining, long-term recovery; companionship which, moreover, can model the motivation and methods required for this metamorphosis (Vaillant, 1995). It is reasonable to expect that residents comprise a significant portion of each other’s day-to-day social interactions —certainly as it relates to recovery, at the very least—and that whatever sobriety-reinforcing value this environment provides will be (in some way) dependent on social processes operating between and among the residents themselves. Because each house is a complete, or whole, network of relationships, it is possible to think of these social processes as a social network that co-evolves over time, along with changing resident characteristics such as recovery-related attitudes and behaviors. Thus, the ideas of recovery capital formation and access, ongoing abstinence, and personal recovery can be brought together in a conceptual and methodologically tractable way, by thinking of recovery homes as temporally evolving, multi-relational (multiplex) relationships which both affect and are affected by residents’ individual recovery progress. Below we give a concrete example of this approach with those with substance use disorders
System Approaches for Social Relationships within Recovery Homes
Representative research by our team includes a descriptive analysis of social networks within recovery homes (Jason, Guerrero, Lynch, Stevens, Salomon-Amend, & Light, 2020) yet interactions such as “friendship,” “willingness to lend money,” and “advice-seeking” might both enhance as well as impede the recovery outcomes of house residents. For example, Jason, Guerrero, Salomon-Amend, Lynch, Stevens, Light, Stoolmiller, and Doogan (2021) found the density of interpersonal ties involving willingness to loan money was positively associated with better individual outcomes (i.e., wages, social support, and self-esteem). In addition, Jason, Guerrero, Salomon-Amend, Lynch, Stevens, Light, and Stoolmiller (2021) found that higher density of advice-seeking was predictive of greater relapse. These results were surprising, inasmuch as one would normally expect advice-seeking to be beneficial.
However, these studies failed to consider the characteristics of the advice giver. When we took this ecological dimension into consideration, we found that while greater advice-seeking is generally associated with negative outcomes, seeking advice from individuals who are more recovered tends to be beneficial. The SAOM framework involves a dyad-based conception of relationship formation, as well as the subsequent effects of those relationships that consider who, specifically, the relationship partner is. This example demonstrates the benefits of a systems approach to clearly understand the complex interpersonal dynamics that occur within these recovery homes. From a theoretical point of view, both network relationships and recovery behaviors can be conceptualized as mutually-interacting entities that co-evolve over time.
SAOM offers the advantage of separately estimating the contributions of selection and influence on the emergence of network autocorrelation; individuals may already be similar and tend to select others (e.g., as friends) like them, or the friendships may come first, with social influence leading to more similarity. Depending on the networks, behaviors, and populations involved, evidence of both selection and influence are commonly found in social groups, often simultaneously (Ripley et al., 2021).
In another example of our work, we reported evidence of a “selection” effect (Doogan et al., 2019), where residents with a high self-reported quality of life were more inclined to become friends with those with low quality of life and vice versa. This finding was consistent with the Oxford House model, which encourages friendship ties from more experienced residents to others most in need of such supports. We next found that when individuals with low recovery factor scores were situated in houses with at least one resident with high recovery factor scores, the scores of the low recovery factor resident increased in almost all cases (See Figure A for an example) (Jason Bobak, Islam, Guerrero, & Light, 2021). However, in one recovery home, where two individuals with low recovery factor scores did not increase their scores from Wave 1 to Wave 2 (both scores stayed at 1), there were few relationships or connections with the other residents who had higher recovery factor scorers (See Figure B). In other words, recovery can be enhanced when living in houses with high recovery factor residents, but it is also essential for the low recovery factor residents to have relationship ties with those residents who have more recovery; mere presence in the house with high recovery factor individuals might not be sufficient to observe positive recovery changes over time.
Figure A .
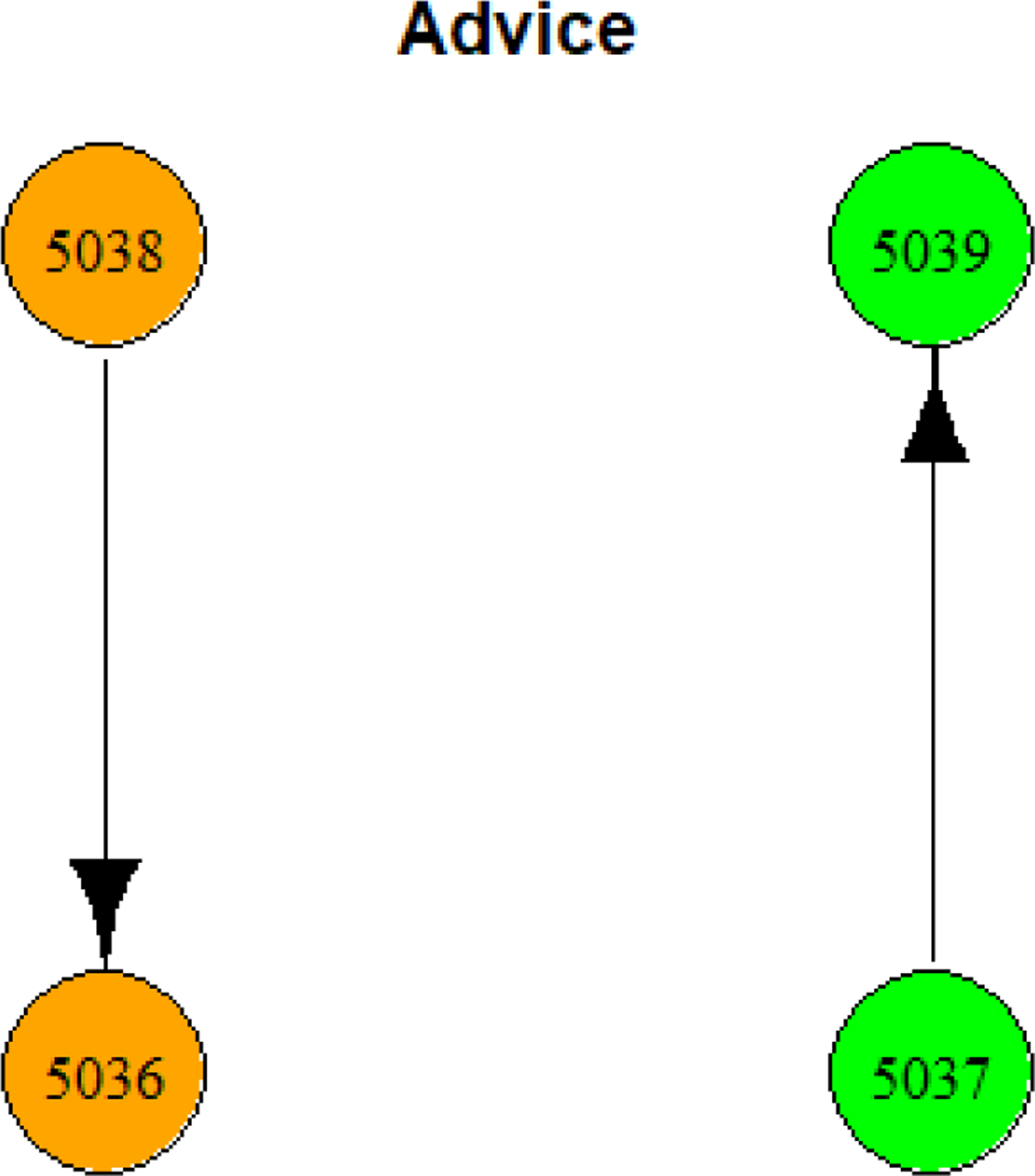
Few ties amongst members of house number 75 for seeking advice (Gold color designates low recovery score residents; Green color designates high recovery residents).
Figure B .
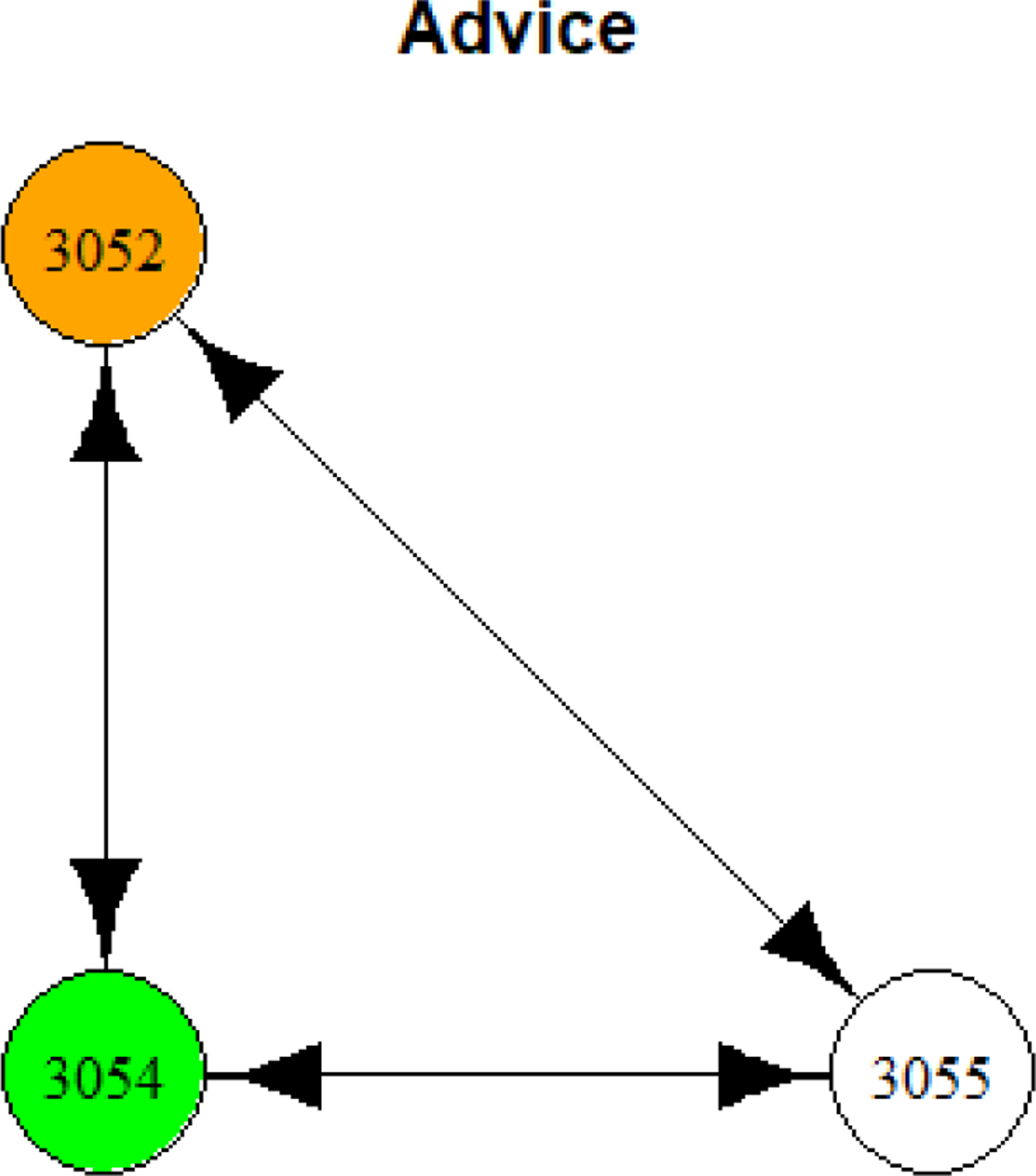
Strong interconnections amongst members of house number 49 for seeking advice (Gold color designates low recovery score resident; Green color designates high recovery resident, No color indicates resident with neither high or low recovery factor score).
Using this dynamic approach, there are a host of interesting but largely unexplored questions that could be answered which have considerable clinical significance. For example, what is the marginal value of associating with one vs two or more residents with higher recovery factor scores? It is not just the mentor, but the quality of the mentor’s recovery factor score. Our findings suggest that there are benefits when residents seek advice from those with more experience, strength, and hope or pursue relationships with those who have more of what they need for their sustained recovery. These are a few of the exploratory issues that can be examined. This is a unique approach to studying recovery house social dynamics that support abstinence and mediators of abstinence. The social network design provide a conceptually accurate way to represent recovery house social system dynamics in relation to residents’ progress towards self-sustaining recovery.
In sum, there is considerable evidence that social relationship dynamics affect individual recovery outcomes and vice versa. Understanding these complex processes is therefore key to understanding how recovery is promoted in these settings, why the residential experience seems to work for some but fail for others, and how this experience might be improved or broadened to other types of settings. By identifying mechanisms through which social environments affect health outcomes, this type of investigation can contribute to reducing unnecessary health care costs by improving the effectiveness of the residential recovery home system in the US and also restructuring and improving other community-based recovery settings. Housing instability is not only a problem for those with substance use disorders, but it is also a pressing issue for those in poverty, those with psychiatric conditions, those experiencing homelessness, and those with chronic health conditions (Housing Instability, 2022). Psychologists treat individuals with these conditions, and the systemic research reviewed above with recovery homes could serve as a model for how other intransigent mental health related conditions might be comprehensively approached.
Systems Approaches for Measuring Unexplained Neurological Illness
Systems analysis can shed light on coevolving dynamics within substance use recovery, and it can also provide a new lens through which to examine a complex, misunderstood post-viral illness. What has been commonly referred to as chronic fatigue syndrome (CFS), is a serious and complex illness often following a viral illness that affects many different body systems, and is characterized by cognitive impairment, post-exertional malaise, unrefreshing sleep, and often other disorders such as those of the autonomic nervous system (Komaroff, 2019). Many activists prefer the name Myalgic Encephalomyelitis (ME) and some refer to the illness as ME/CFS. Approximately 1.5 million people in the United States are estimated to have ME/CFS, resulting in substantial health care costs and productivity losses ((Jason & Mirin, 2021). Because of the current pandemic, a certain percentage of patients with COVID-19 have not recovered, and it is likely that many of these post-viral fatigue patients will be classified as having ME/CFS. Systems methods could be used to establish reliable and objective indicators of ME/CFS, which may help with diagnosis and legitimize evidence of impairment in patients.
Complicating issues surrounding this illness include the stigmatizing name (chronic fatigue syndrome), the absence of a consensus case definition among healthcare professionals and the research community, and variable rates of prevalence (Jason, Cotler, Bhatia, & Sunnquist, 2021). Key decisions regarding the name, case definition, epidemiology, and treatment were made many years ago within a sociopolitical context in which ME/CFS was assumed to be a psychologically-based problem (Jason et al., 1997). Some of the decisions may have been due, in part, to the predominance of female patients with this illness, whose medical complaints have historically been discredited by the predominantly male medical establishment (Richman & Jason, 2001). Many physicians and other healthcare professionals have continued to believe that individuals with this syndrome have a predominant psychiatric illness (Froehlich et al., 2021). Due to the stigmatizing controversy surrounding the name, etiology, and diagnostic criteria, people with the illness frequently face disbelieving attitudes from their doctors, family, and friends, with many experiencing profound losses in their support systems (Osler, 2006). As with many illnesses, the absence of a biological marker influences decision making among medical personnel, policy officials, and grant funders, concerning the legitimacy of research and treatment (Komaroff, 2019). Systems research that can help identity such a marker could have an enormous validating effect on how patients are currently being treated, and such work might also help those with comparable long-term symptoms of COVID-19.
Identifying Predisposing Immune Markers in ME/CFS
Present research suggests that there are probably several contributing factors that cause ME/CFS, complicating the study of this illness and the identification of biological markers (Lacerda, Geraghty, Kingdon, et al. 2019). In addition, studies of ME/CFS have focused on people who are already ill with the disease, but research occurring after illness onset can make it more difficult to distinguish causative factors from effects of the illness itself (Norris et al., 2017). In an effort to tackle this problem, a multi-disciplinary team of investigators (Leonard Jason, a community psychologist at DePaul, Jacob Furst, a computer scientist at DePaul, Matthew Sorenson, an immunologist within the nursing department at DePaul, and Ben Katz, an infectious disease physician at Northwestern Hospital) studied healthy college students over a four-year period to see if and when they developed Infectious Mononucleosis. Infectious Mononucleosis is caused by the Epstein-Barr virus, and is common among incoming college freshmen.. Infectious Mononucleosis is caused by the Epstein-Barr virus and is common among incoming college freshmen. Although Infectious Mononucleosis is a risk factor for subsequent ME/CFS, no prior study has followed a cohort of healthy individuals longitudinally to examine a possible linkage, along with other psychological and biological factors that may predict such progression.
In this longitudinal and prospective study, Jason, Cotler, Islam, Sunnquist, and Katz (2021) enrolled over 4,500 university students, about 5% of whom developed Infectious Mononucleosis over the course of their enrollment at university. The students who developed Infectious Mononucleosis were assessed for ME/CFS at a 6-month follow-up. Students who went on to develop severe ME/CFS were compared to students who were asymptomatic. Recent meta-analyses with ME/CFS samples, however, have found inconsistent immune system responses (Strawbridge et al., 2019). This could be due to differences in data collection methods or differences in immune reactions to the occurrence of Infectious Mononucleosis. We had obtained immune response biomarker data prior to illness onset. Rather than focusing on only individual pro and anti-inflammatory cytokines, we applied network analysis to the cytokine data in other ill and healthy groups, which had been diagnosed 6 months following Infectious Mononucleosis. Interrelationships among cytokines, conceived as networks, have been shown to provide further insights into the complex dynamics that would uncover dysregulations among those who develop severe ME/CFS following Infectious Mononucleosis.
We found that the severe ME/CFS group had significantly different network of cytokines when compared to controls. Figure C shows the cytokine associations among controls at baseline, which demonstrates a distinct pattern of two-family groupings of cytokines. In contrast, Figure D shows one network group of cytokine associations for severe ME/CFS. The differential nature of cytokine networks with the existence of one network family was most markedly different in those with severe ME/CFS, implying a pattern of distinct immunologic responsiveness with multiple connected pro and anti-inflammatory cytokines, whereas the controls show a more differentiated grouping of pro and anti-inflammatory cytokines. Network analyses provided us this unique opportunity to understand biological variables that might help investigators differentiate why certain individuals who get infected with Infectious Mononucleosis do not recover while others do; such findings could also have implications for the current COVID-19 pandemic (González-Hermosillo et al., 2021), as indicated below.
Figure C :
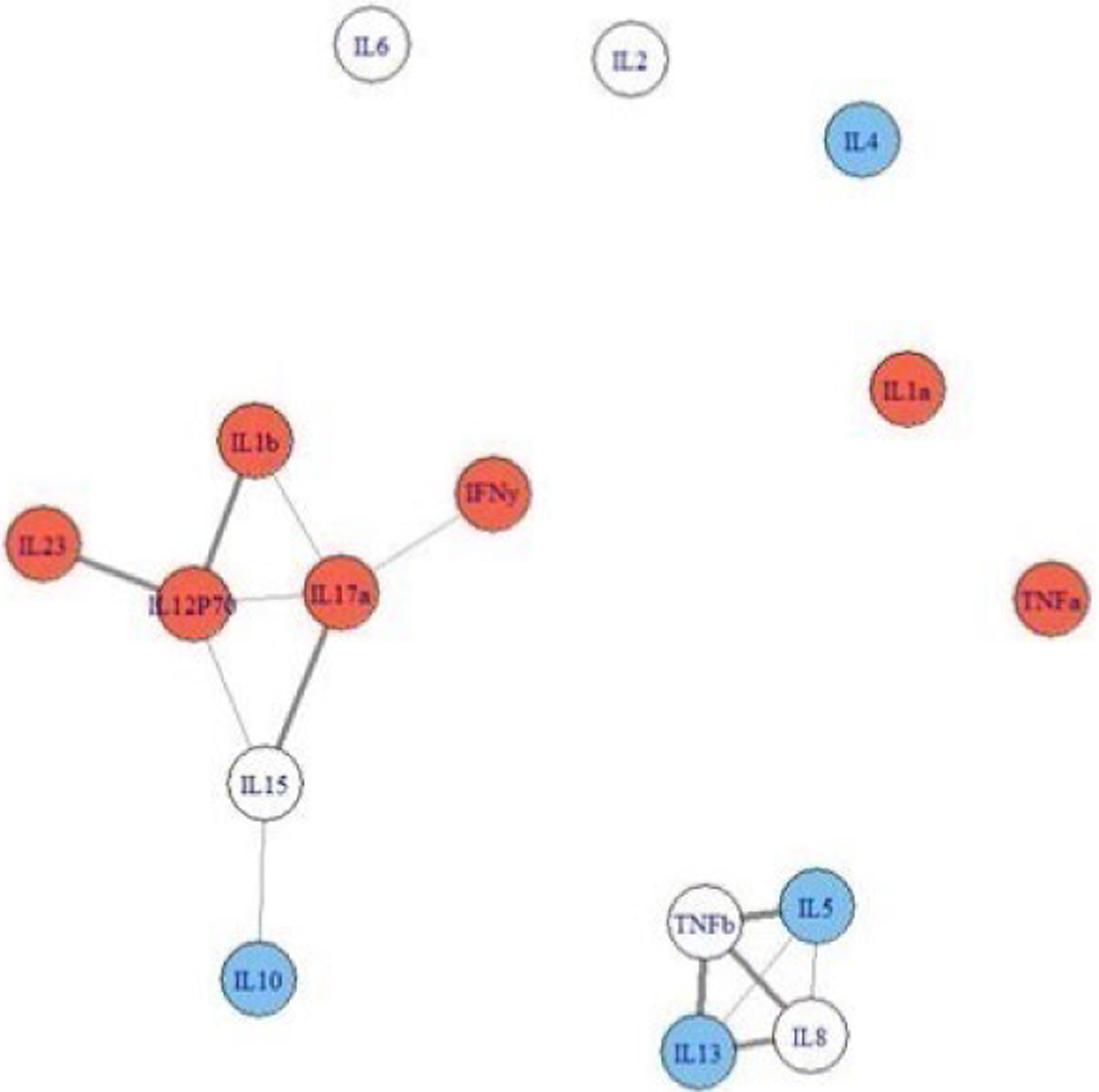
Cytokine Data for Controls. Cytokines colored red are pro-inflammatory, those colored blue are anti-inflammatory. Cytokines not colored have multi-purpose functions.
Figure D :
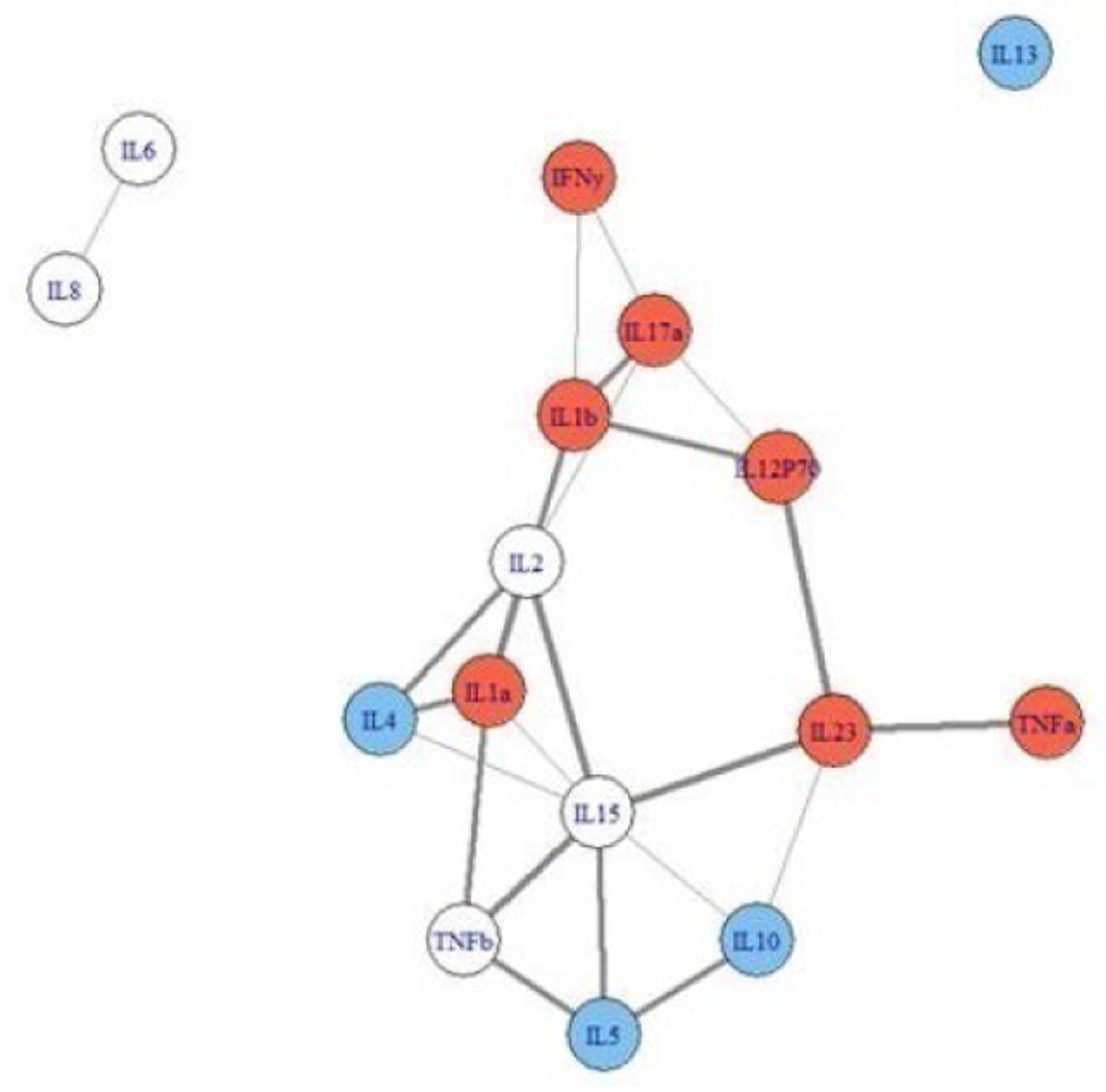
Cytokine Data at Baseline for Severe ME/CFS participants. Cytokines colored red are pro-inflammatory, those colored blue are anti-inflammatory. Cytokines not colored have multi-purpose functions.
For practicing psychologists, this type of work could help lay the groundwork for future prevention and intervention trials, based on the risk factors identified for development and maintenance of ME/CFS following Infectious Mononucleosis or other infections such as COVID-19 (Araja et al., 2021). Helping construct models with professionals from different disciplines in order to identify those likely to have persistent symptoms could provide enormous benefits. For example, psychologists could develop stress reduction techniques, and better sleep hygiene, exercise, and adequate water intake could be counseled at the onset of Infectious Mononucleosis or COVID-19. For those at risk for developing ME/CFS six months later or other post-viral illnesses like COVID-19, psychologists could participate in controlled trials of anxiolytics, medications to improve sleep (e.g., melatonin), or salt loading, and additionally, specific forms of supportive therapy or drugs to provide circulatory support (e.g., salt-retaining steroids) and autonomic modulation (e.g., beta blockers) may be contemplated.
Discussion
Our article demonstrates how systems research and community psychology can be applied in understanding complex behavioral phenomena, thus providing a useful perspective to practitioners. Maintaining recovery from addiction and better understanding a complex medical condition (ME/CFS) are used as illustrative examples. The article illustrates how one can approach the study of complex behavioral phenomena using a systems approach that is not often a part of practitioner training at the Ph.D. and Psy.D. level. Psychologists could seek advanced training in either General Systems Theory (von Bertalanffy, 1969) or biological systems such as in immunology (Coursera, 2022), or join multidisciplinary teams with scientists from medicine, computer science, and other disciplines. There are a growing number of institutions that are providing training and courses in translational science (National Center for Advanced Translational Sciences (2022), system dynamics (Washington University in St. Louis, 2022), social network analysis (Duke University, 2022) and SAOM (SIENA activities and workshops, 2022). The methods applied and illustrated in this article could stimulate others to apply the same approach to the study of chronic pain treatment, stress among caregivers of people with dementia, care of some SMI (seriously mentally ill) populations, and other circumstances that occur because problems in complex interacting systems do not easily lend themselves to simple testing of a variable or two. In other words, the orienting frameworks of community psychology can aid in developing and implementing solutions to complex psychological problems that often need a more ecological approach.
This article has examined the benefits of a systems-oriented methods approach in understanding two very different social and medical issues. The first example involves the mechanisms and maintenance of recovery from substance use disorders in community settings (e.g., recovery homes), and the other involves working with patients with ME/CFS to help reduce the stigma that surrounds the illness and discovering network-oriented biological markers. In prior work, qualitative methodological approaches have been used to establish cause-and-effect relationships to produce generalizable findings, but too often more simplistic linear methods have been used with few, if any, network analyses or bidirectional pathways that are more characteristic of systems. In an effort to move beyond the more traditional social and medical methods, we first explored dynamic systems-based methods that linked individuals’ recovery to relationship networks and recovery aspects of the house residents. We next examined networks of biological markers that could help account for formerly unexplained symptoms of ME/CFS. The studies illustrate how systems-oriented methods have the advantage of providing fresh insights for the complexities of both social and biological issues among individuals and their host settings.
In our first recovery home systems example, our work with social network analysis of Oxford Houses used SAOM (Snijders, van de Bunt, & Steglich, 2010) to capture social relationships and behavioral change. These methods are particularly good at modeling group processes of small groups, consisting of 5 to 10 people, that contain feedback loops. In contrast, in multilevel models, feedback loops cannot be modeled since no variable can be both a predictor and an outcome. In structural equation models, feedback loops can occur, but this approach is not naturally dynamic. An approach that does capture feedback loops - the Actor Partner Interaction Model (Kenny et al., 2002) - only focuses on dyads involving two people (e.g., an actor and a partner). However, dyads are usually embedded in a broader relational structure, and this approach therefore cannot measure more complex relationships such as transitivity, where a friend of a friend is likely to become a friend.
In our research with recovery homes, when utilizing traditional research methods, we noticed that higher rates of relapse occurred in recovery homes with more advice-seeking. To understand this type of relationship, it is necessary to understand how recovery home social dynamics and personal change interact to create desirable outcomes (e.g., sustained recovery) and problematic ones (e.g., early drop out). It was only when we examined the system dynamics of relationships more closely that we found advice-seeking with residents having higher recovery factor scorers was critical for positive changes to occur over time. In other words, recovery factor changes could occur for low recovery factor individuals, but context was also important, as those low recovery individuals needed to have relationships with those who had higher recovery. These types of investigations can help us better understand who benefits most and least from recovery houses, and this can have some important practical implications.
Psychologists with interests in treating those with substance use disorders will find that this systems research could lead to improvements in recovery outcomes for those participating in many types of residential aftercare settings, and it could increase the need for patient-centered education and planning for post-treatment transitions. This type planning must be connected to accessibility, availability, and affordability of aftercare residential resources. Overall, this argues that psychologists in their work might need to help develop a strongly networked continuum of care system that the patient evaluates as a critical, evidence-based choice influencing their likelihood of recovery. Factors that would facilitate better patient-centered planning, decision-making, and utilization of residential aftercare may include a focus on overall healthcare outcomes; a focus on systemic poor quality indicators, such as non-compliance and retreatment; and a focus on an individual’s total life-cycle costs related to alcohol and substance use disorders (Marchand et al., 2019). Barriers could include lack of awareness, lack of aftercare resources or services, lack of resources to help finance aftercare settings, and psychosocial impediments such as stigma (Substance Abuse and Mental Health Services Administration, 2016).
Our second topic involved a stigmatized post-viral illness known as ME/CFS. Difficulties in identifying biological markers have led to continued skepticism regarding the legitimacy of this illness. In interacting with patients with ME/CFS, it is important for psychologists to know that many patients dislike this term and prefer ME (Khazan, 2016). In addition, it is also important to be aware that the prevalence of females presenting with the disease tended to reduce credibility as a real medical condition by the male-dominated medical establishment (Richman & Jason, 2001). Psychologists need to recognize these issues in order to develop positive working relationships with patients with these types of unexplained illnesses.
One possible cause of ME/CFS and Long COVID could be fragments of viral genes triggering an immune overreaction or an immune system stuck in an overactive state (Islam, Cotler, & Jason, 2020). Our main finding involved networks of cytokines, as the pro and anti-inflammatory proteins in the blood of those who went on to develop severe ME/CFS following Infectious Mononucleosis had more centrality, or dense interconnected cytokine networks. More differentiated cytokine networks were seen for those at baseline who did not develop ME/CFS following Infectious Mononucleosis. Capturing patient characteristics prior to infection provided unique insights into predisposing factors, helping to answer why certain individuals develop ME/CFS. The use of networks that go beyond individual cytokine analyses can help us identify predisposing biological factors in the development and maintenance of symptoms, and thus lay the groundwork for a biological explanation of ME/CFS. In addition to identifying biological immune markers that could help legitimize patients with ME/CFS, psychologists have also used systems theory to identify irregularities within brain networks of these patients (Zinn et al., 2016). Such dysregulation evidence could be used by practicing psychologists to build rapport with patients who feel demoralized after experiencing skepticism of their illness by employers, friends and family members (Komaroff, 2021) who are not aware of these findings
Psychologists have many opportunities to work with those now suffering from post-viral illnesses. When Porter, Jason, Boulton, Bothne, and Coleman (2010) reviewed 70 complementary and alternative trials directed at treating patients with ME/CFS and FM, meditation emerged as the most promising candidate with nine of the ten meditation studies showing some overall beneficial effect. It is thought that the effects of meditation rely on the body’s ability to switch to alpha (resting) or theta brain-wave states, and during meditation the brain’s rhythm slows appreciably and endorphins are released (Goleman, & Davidson, 2017). Psychologists could use these types of mind-body techniques as a treatment for post-viral symptoms of fatigue and cognitive dysfunction (Centers for Disease Control and Prevention, 2019; Wise, Jantke, Brown, O’Connor, & Jason, 2015).
The use of systems methodology can involve collaborations with professionals from other disciplines. Most psychologists are not trained to analyze cytokines or to analyze complex network data, but our profession does value working with others with expertise and training in other fields. Such multidisciplinary projects have unique value for solving difficult clinical and community problems, and in addition, this type of what is called translational research is highly valued by funding agencies such as the National Institutes of Health for advancing knowledge in diagnostics, behavioral change and medical procedures (National Center for Advancing Translational Science, 2022).
In this article, we have suggested that systems research and theory can be applied to the real world settings of practicing psychologists, particularly those in clinical settings (e.g., medical centers, private practice, community mental health). Psychologists can integrate systems concepts into their work to conceptualize cases and better understand dynamics of their clients through capturing what is occurring within their social environments as well as within biological markers in their blood. Systems theory and research can improve client care and outcomes by better diagnosing problems in the different levels of analysis as well as developing more sophisticated treatment approaches that include these different ecological factors. Systems-oriented methods are increasingly being utilized by social scientists and mental health and community-based professionals, and they could contribute to the further maturation of intervention development, application, and evaluation. By utilizing a wide array of systems-oriented methods that are theoretically sound and empirically valid, psychologists have the ability to ask and answer important clinical questions, whose investigations will be meaningful and beneficial to the patients and communities in which they work.
Public Significance Statement.
Systems research and community psychology can be applied in understanding complex behavioral phenomena. It thus provides a useful perspective to practitioners in assisting with solutions to psychological or societal problems.
Acknowledgments
The authors appreciate the funding provided by the National Institute of Neurological Disorders and Stroke (project number NS111105) and the National Institute on Alcohol Abuse and Alcoholism (grant number AA022763).
References
- Araja D, Berkis U, Lunga A, & Murovska M (2021). Shadow Burden of Undiagnosed Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) on Society: Retrospective and Prospective—In Light of COVID-19. Journal of Clinical Medicine, 10(14), 3017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Bertalanffy L (1969). General Systems Theory, George Braziller, New York. [Google Scholar]
- Centers for Disease Control and Prevention (2019). Treatment of ME/CFS Available at: https://www.cdc.gov/me-cfs/treatment/index.html
- Coursera (2022) Fundamentals of Immunology: T Cells and Signaling Available at: https://www.coursera.org/lecture/immunologyfundamentalstcellssignaling/information-transfer-T9qeF
- Doogan NJ, Light JM, Stevens EB, & Jason. LA (2019). Quality of life as a predictor of social relationships in Oxford House. Journal of Substance Abuse Treatment, 101, 79–87. PMCID: PMC6557298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duke University (2022). Duke Network Analysis Center Available at: https://sites.duke.edu/dnac/training/
- Froehlich L, Hattesohl DBR Jason LA, Scheibenbogen C, Behrends U, Thoma M (2021). Medical care situation of people with Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome in Germany. Medicina, 57, 646. 10.3390/medicina57070646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Hermosillo JA, Martínez-López JP, Carrillo-Lampón SA, Ruiz-Ojeda D, Herrera-Ramírez S, Amezcua-Guerra LM, & Martínez-Alvarado M.d.R. (2021). Post-Acute COVID-19 Symptoms, a potential Link with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A 6-Month Survey in a Mexican Cohort. Brain Science, 2021, 11, 760. 10.3390/brainsci11060760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goleman D, & Davidson RJ (2017). Altered Traits: Science Reveals How Meditation Changes Your Mind, Brain, and Body Avery, New York, NY, 2017 [Google Scholar]
- Housing Instability (2022). The Healthy People 2020 Social Determinants of Health topic area. Office of Disease Prevention and Health Promotion Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/housing-instability
- Islam MF, Cotler J, & Jason LA Post-Viral Fatigue and COVID-19: Lessons from past epidemics. Fatigue: Biomedicine, Health & Behavior,2020; 8(2), 61–69. 10.1080/21641846.2020.1778227 [DOI] [Google Scholar]
- Jason LA, Cotler J, Bhatia S, & Sunnquist M (2021). Chronic illness: The case of Chronic Fatigue Syndrome-Myalgic Encephalomyelitis. In Ragin DF & Keenan JP (Eds.). Handbook of Research Methods in Health Psychology New York: Routledge. [Google Scholar]
- Jason LA, Cotler J, Islam M, Sunnquist M, & Katz BK (in press). Risks for developing ME/CFS in college students following Infectious Mononucleosis: A prospective cohort study. Clinical Infectious Diseases, 73(11), e3740–e3746, 10.1093/cid/ciaa1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA & Glenwick DS (Eds.). (2016). Handbook of Methodological Approaches to Community-Based Research: Qualitative, Quantitative, and Mixed Methods New York, NY: Oxford University Press. [Google Scholar]
- Jason LA, Guerrero M, Lynch G, Stevens E, Salomon-Amend M, & Light JN (2020). Recovery home networks as social capital. Journal of Community Psychology, 48, 645–657. 10.1002/jcop.22277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Guerrero M, Salomon-Amend M, Lynch G, Stevens E, Light JM, & Stoolmiller M (2021). Advice seeking and loaning of money related to relapse in recovery homes. Journal of Community & Applied Social Psychology, 31, 39–52 10.1002/casp.2486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Guerrero M, Salomon-Amend M, Lynch G, Stevens EB, Light JN, Stoolmiller M, & Doogan NJ (2021). Network measures of advice-seeking and resource sharing are related to well-being in recovery homes. International Journal of Drug Policy, 92, 10.1016/j.drugpo.2020.102970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Light JM, Stevens EB, & Beers K (2014). Dynamic social networks in recovery homes. American Journal of Community Psychology, 53, 324 –334. 10.1007/s10464-013-9610-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Lynch G, Bobak T, Light JM, & Doogan NJ (in press). Dynamic interdependence of advice seeking, loaning, and recovery characteristics in recovery homes. Journal of Human Behavior in the Social Environment . 10.1080/10911359.2021.1947930 [DOI] [PMC free article] [PubMed]
- Jason LA, & Mirin AA (2021). Updating the National Academy of Medicine ME/CFS prevalence and economic impact figures to account for population growth and inflation. Fatigue: Biomedicine, Health & Behavior, 9(1), 9–13. 10.1080/21641846.2021.1878716 [DOI] [Google Scholar]
- Jason LA, Olson BD, Ferrari JR, Majer JM, Alvarez J, & Stout J (2007). An examination of main and interactive effects of substance abuse recovery housing on multiple indicators of adjustment. Addiction, 102, 1114–1121. PMCID: PMC2976482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Olson BD, & Foli K (2008). Rescued lives: The Oxford House approach to substance abuse New York, NY: Routledge. [Google Scholar]
- Jason LA, Richman JA, Friedberg F, Wagner L, Taylor RR, & Jordan KM (1997). Politics, science, and the emergence of a new disease: The case of Chronic Fatigue Syndrome. American Psychologist, 52, 973–983. PMID:9301342 [DOI] [PubMed] [Google Scholar]
- Jason LA, Stevens E, Ram D, Miller SA, Beasley CR, Gleason K, (2016). Theories in the field of community psychology. Global Journal of Community Psychology Practice, 7(2), pages 1–27. Retrieved Day/Month/Year, from (http://www.gjcpp.org/). [Google Scholar]
- Jason LA, Zinn ML, & Zinn MA (2015). Myalgic Encephalomyelitis: Symptoms and biomarkers. Current Neuropharmacology, 13(5), 701–734. 10.2174/1570159X13666150928105725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson H (2006). Osler’s Web. Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic Penguin Press. [Google Scholar]
- Kelly JG (2006). Becoming ecological: An exploration into community psychology Oxford, England: Oxford University Press [Google Scholar]
- Kenny DA, Mannetti L, Pierro A, Livi S, & Kashy DA (2002). The statistical analysis of data from small groups. Journal of Personality and Social Psychology, 83, 126–137. 10.1037/0022-3514.83.1.126 [DOI] [PubMed] [Google Scholar]
- Khazan O (2016, Oct. 8). The tragic neglect of Chronic Fatigue Syndrome. The Atlantic, Available at: https://www.theatlantic.com/health/archive/2015/10/chronic-fatigue-patients-push-for-an-elusive-cure/409534/
- Kingry-Westergaard C, & Kelly JG (1990). A contextualist epistemology for ecological research. In Tolan P, Keys C, Chertok F, & Jason L (Eds.) Researching community psychology. Issues of theory and methods (pp.23–31). Washington, DC: American Psychological Association. [Google Scholar]
- Komaroff AL (2019). Advances in Understanding the Pathophysiology of Chronic Fatigue Syndrome. Journal of the American Medical Association. E1–E2. [DOI] [PubMed]
- Komaroff AL (2021). Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: When Suffering Is Multiplied. Healthcare (Basel, Switzerland), 9(7), 919. 10.3390/healthcare9070919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komaroff AL, & Buchwald DS (1998). Chronic Fatigue Syndrome: An Update. Annual Review of Medicine, 49(1), 1–13. 10.1146/annurev.med.49.1.1 [DOI] [PubMed] [Google Scholar]
- Light JM, Jason LA, Stevens EB, Callahan S, & Stone A (2016). A mathematical framework for the complex system approach to group dynamics: The case of recovery house social integration. Group Dynamics: Theory, Research, and Practice, 20(1), 51–64. PMCID: PMC4821464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacerda EM, Geraghty K, Kingdon CC et al. A logistic regression analysis of risk factors in ME/CFS pathogenesis. BMC Neurol 19, 275 (2019). 10.1186/s12883-019-1468-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsden PV (2011). Survey methods for network data. The SAGE handbook of social network analysis, 25, 370–388. [Google Scholar]
- Marchand K, Beaumont S, Westfall J, MacDonald S, Harrison S, Marsh DC,…. Oviedo-Joekes E (2019). Conceptualizing patient-centered care for substance use disorder treatment: findings from a systematic scoping review. Substance Abuse Treatment, Prevention, and Policy 14, 37. 10.1186/s13011-019-0227-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Advancing Translational Science (2022). National Center for Advancing Translational Science Available at : https://ncats.nih.gov/index.php
- Norris T, Collin SM, Tilling K, Nuevo R, Stansfeld SA, Sterne JAC, et al. (2017). Natural course of chronic fatigue syndrome/myalgic encephalomyelitis in adolescents. Arch Dis Child . 19. doi: 10.1136/archdischild-2016-311198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Øksendal B (2010). Stochastic Differential Equations: An Introduction with Applications Springer. [Google Scholar]
- Polcin DL, Korcha R, Bond J, Galloway G, & Lapp W (2010). Recovery from addiction in two types of sober living houses: 12-month outcomes. Addiction Research and Theory, 18, 442–455. Available at: 10.3109/16066350903398460 [DOI] [Google Scholar]
- Porter N, Jason LA, Boulton A, Bothne N, & Coleman B (2010). Alternative medical interventions used in the treatment and management of myalgic encephalomyelitis/chronic fatigue syndrome and fibromyalgia. Journal of Alternative and Complementary Medicine, 16(3): 235–249. [DOI] [PubMed] [Google Scholar]
- Revenson TA, & Seidman E (2002). Looking backward and moving forward: Reflections on a quarter century of community psychology. In Revenson TA, D’Augelli AR, French SE, Hughes DL, Livert D, Seidman E,… Yoshikawa H (Eds.), A quarter century of community psychology: Readings from the American Journal of Community Psychology (pp. 3–31). New York, NY: Kluwer Academic/Plenum. [Google Scholar]
- Richman JA & Jason LA (2001). Gender biases underlying the social construction of illness states: The case of chronic fatigue syndrome. Current Sociology 49, 15–29. doi: 10.1177/0011392101049003003 [DOI] [Google Scholar]
- Ripley RM, Snijders TAB, Boda Z, Voros A, & Preciado P (2021). Manual for SIENA (version May 11 2021). Oxford: University of Oxford. Retrieved from http://www.stats.ox.ac.uk/siena/
- SIENA activities and workshops (2022). Lectures, workshops, courses Available at: https://www.stats.ox.ac.uk/~snijders/siena/siena_events.htm
- Snijders TAB, van de Bunt GG, & Steglich CEG (2010). Introduction to stochastic actor based models for network dynamics. Social Networks, 32, 44 – 60. 10.1016/j.socnet.2009.02.004 [DOI] [Google Scholar]
- Stevens E, Guerrero M, Green A, & Jason LA (2018). Relationship of hope, sense of community, and quality of life. Journal of Community Psychology, 46, 567–574. doi: 10.1002/jcop.21959. PMCID: PMC6086495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strawbridge R, Sartor ML, Scott F, & Cleare AJ (2019) Inflammatory proteins are altered in chronic fatigue syndrome – A systematic review and meta analysis. Neuroscience & Biobehavioral Reviews 107, 69–83. 10.1016/j.neubiorev.2019.08.011 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2017). Guidelines for Successful Transition of People with Mental or Substance Use Disorders from Jail and Prison: Implementation Guide. (SMA)-16-4998 Rockville, MD: Substance Abuse and Mental Health Services Administration. Available at: https://store.samhsa.gov/sites/default/files/d7/priv/sma16-4998.pdf [Google Scholar]
- Substance Abuse and Mental Health Services Administration ((2016). Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health [Internet] Washington (DC): US Department of Health and Human Services; CHAPTER 6, HEALTH CARE SYSTEMS AND SUBSTANCE USE DISORDERS. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424848/ [PubMed] [Google Scholar]
- Vaillant GE (1995). The natural history of alcoholism: Paths to recovery Cambridge, MA: Harvard University Press. [Google Scholar]
- Zinn ML, Zinn MA, & Jason LA (2016). Intrinsic functional hypoconnectivity in core neurocognitive networks suggests central nervous system pathology in patients with Myalgic Encephalomyelitis: A pilot study. Applied Psychophysiology and Biofeedback, 41(3), 283–300. 10.1007/s10484-016-9331-3 [DOI] [PubMed] [Google Scholar]
- Washington University in St. Louis (2022). System Science for Social Impact Available at: https://systemsscienceforsocialimpact.wustl.edu/workshop-tracks/
- Wasserman S, & Faust K (1994). Social Network Analysis: Methods and Applications Cambridge, UK: Cambridge University Press. [Google Scholar]
- Wise S, Jantke R, Brown A, O’Connor K, & Jason LA (2015). Functional level of patients with chronic fatigue syndrome reporting use of alternative vs. traditional treatments. Fatigue: Biomedicine, Health & Behavior, 3, 235–240. PMCID: PMC4830425 [DOI] [PMC free article] [PubMed] [Google Scholar]


