Abstract
Chronic diseases disproportionately affect patients in low-income minority groups who traditionally use in-person healthcare services. COVID-19 disrupted their routines and limited options for people to receive care; this could exacerbate health inequities. The study examined telehealth chronic disease management among low-income minority groups. We used Florida Medicaid claims data from March to December 2020 and the American Consumer Survey to examine the study objectives. Data were analyzed using Linear and Logistic Regression. We retrieved claim records of 52,904 unique patients; 31,999 were female and 49% of the sample had at least one telehealth visit. Medicaid patients were 8% less likely to use telehealth and 21% more likely to have audio visits when compared to Medicare patients. The analyses suggest that Non-Hispanic Black patients and individuals with a lack of education experience significant health inequities. People with chronic obstructive pulmonary disease (5%) and heart failure (14%) were less likely to use telehealth than patients with diabetes. Telehealth will continue to be a health delivery option; thus we recommend that strategies are enacted to educate, and resources are provided to promote equity among Non-Hispanic Black patients. Without priority attention to people among low-income minority populations, health inequities will continue to plague this community.
Keywords: Telehealth, Health inequity, COVID19, Chronic disease management, Poverty, Medicaid
Introduction
Telehealth has been widely used over the past several years. As a chronic disease management tool, telehealth supports quality care and increases provider and patient engagement [1, 2]. Telehealth increases the opportunity for patient monitoring, treatment, and education. During the pandemic, telehealth was a principal means to provide healthcare when in-person services were limited. We witnessed unprecedented legislative and reimbursement support that encouraged telehealth use to protect providers and patients from the contagion [3]. As a result, the demand for telehealth increased; however, telehealth use trends were not similar among all populations [4, 5]. Ideally, we should have observed a continuity of chronic disease management among all populations during COVID-19. However, when in-person options for care were limited, chronic disease management decreased for people in low-income minority positions [5, 6].
Medicaid beneficiaries are of particular interest, as this public insurance program serves individuals in low-income positions who often experience high rates of chronic diseases and have unfavorable quality outcomes. Medicaid is a jointly supported federal and state healthcare insurance program for people who have incomes below the federal poverty level [7–9]. A growing body of evidence suggested that income is an important contributor to healthcare access and outcomes due to increased chronic ailments, decreased financial resources, and inadequate living conditions [10, 11]. Chronic diseases including diabetes, chronic obstructive pulmonary disease, and heart failure account for over 80% to the US medical costs and affect 48% of adults [12]. These ailments affect nearly 70% vulnerable communities; vulnerable communities include people who identify with low-income minority groups, have low educational attainment, and are over the age of 65 [11–15].
Medicaid enrollees are disproportionately affected by chronic diseases; thus the lack of telehealth use is concerning [11, 12, 16, 17]. Among online health communities for individuals with chronic disease, telehealth use during the first few weeks of COVID-19 among Medicaid recipients (5%) was lower when compared to Medicare (47%), and private insurance recipients (43%) [16]. Health inequities among minority populations are exacerbated by their inability to access and use health related information technologies; barriers are associated with income, education, race, and ethnicity [18–22]. Even when people in low-income minority positions had a laptop or computer and internet access, they were less likely to use it to receive healthcare services [6, 23, 24]. In addition, among racial and ethnic minorities who do use telehealth services, telehealth adherence was low [6, 25].
Through this research, we aim to contribute to the study of health inequity in telehealth use among Florida Medicaid beneficiaries diagnosed with chronic diseases. This study will improve our understanding of telehealth use among low-income minority populations who have diabetes, chronic obstructive pulmonary disease, and heart failure. We provide recommendations to successfully implement telehealth programs in this population.
Methodology
Datasets
The study was conducted in partnership with a State of Florida Medicaid Managed Care program; this agency provides managed care services primarily through Medicaid and Medicare Advantage Insurance Plans. The study period was from March 2020 to December 2020. At the patient level, the variables of interest in the data include insurance (Medicare, Medicaid, Dual Eligible: Medicaid and Medicare), modality (audio, video, in-person), demographics (age, gender), and diagnosis (diabetes, chronic obstructive pulmonary disease, heart failure). We examine the community level associations of socioeconomic factors with telehealth utilization; we retrieved data from American Community Survey Census [26]. The census data supported community (zip code) level analysis of the following variables: education, race, ethnicity, and employment status. Zip code is commonly used as a determinant of socioeconomic status, healthcare access, and healthcare quality [27, 28]. We retrieved demographic and socioeconomic data of people whose incomes were below the poverty level in the state of Florida from the American Consumer Survey.
Methods
Telehealth utilization (whether telehealth was used or not) was measured at the patient level. Categorical variables were created to stratify patients into groups by insurance, gender, age group, rural/urban area, and types of chronic disease. Zip codes were classified into urban or rural areas based on Rural–Urban Commuting Area Codes Data [29]. Multiple logistic regression was conducted to determine the odds ratios of patients in diverse groups utilizing telehealth services. To study the impacts of the socioeconomic variables on telehealth utilization at the community level, telehealth utilization was aggregated at the zip code level and calculated by the percentage of Medicaid patients who utilized telehealth in each zip code. Zip code telehealth utilization was then consolidated with the American Community Survey Census data and included individuals who were below poverty level. The consolidated data included 828 zip codes in the state of Florida. A linear regression analysis of the association of socioeconomic variables with zip code telehealth utilization was performed.
Results
We retrieved claim records of 52,904 unique patients, 31,999 females and 20,905 males. Among the patients in the study, 49% had one or more telehealth visits. Among the 49% of patients, 22,667 patients used video only for telehealth visits, 1020 patients used audio only for telehealth visits, and 2441 patients used video and audio for telehealth visits. A full description of the study sample is in Table 1. We performed a multiple logistic regression analysis to examine the odds of using telehealth by gender, age group, geographic area, and type of chronic disease (see Table 2). The number of visits of a patient was included in the logistic regression analysis to control its potential impact on the dependent variable, telehealth utilization. As shown in Table 3, the results suggest that Medicaid patients are 8% less likely to use telehealth, while patients that have both Medicare and Medicaid insurance are 7% more likely to use telehealth, as referenced to Medicare only patients. Male patients are 22% less likely to use telehealth, as referenced to females. Patients in the 45–64 age group are 69% more likely to use telehealth, as compared to the 65 + age group. Patients with chronic obstructive pulmonary disease are 5% less likely to use telehealth and patients with heart failure are 14% less likely to use telehealth, as compared to patients with diabetes. Furthermore, patients in rural areas are 43% less likely to use telehealth, as referenced to patients in urban areas. We conducted a multiple logistic regression analysis on video utilization (whether a patient had video visits). The results are shown in Table 3. It is worth noting that Medicaid enrollees are 12% less likely to have video visits than Medicare patients. Meanwhile, our logistic regression analysis on audio telehealth utilization suggests that Medicaid patients are 21% more likely to have audio visits than Medicare patients. The results suggest that among low-income populations, Non-Hispanic Black patients who are Medicaid enrollees experience inequity in telehealth use.
Table 1.
Characteristics of study sample used in the analysis
| Variables | Group: number of observations |
|---|---|
| Telehealth utilization (Whether a patient used telehealth during the study period) |
Yes: 26,128 used video only: 22,667 used audio only: 1020 used both video and audio: 2441 No: 26,776 |
| Insurance |
Medicare only: 16,099 Medicaid only: 26,127 Both Medicare and Medicaid: 10,678 |
| Gender |
Female: 31,999 Male: 20,905 |
| Age group |
Age 65 + : 31,434 Age 45–64: 17,579 Age 21–44: 3894 |
| Area |
Urban: 50,053 Rural: 2851 |
| Types of chronic disease |
Diabetes: 35,442 Chronic obstructive pulmonary disease: 13,566 Heart failure: 3896 |
Table 2.
Descriptions of variables of linear regression analysis
| Variables | Definition | Mean (standard deviation) |
|---|---|---|
| Zipcode telehealth utilization | % of patients who utilized telehealth in a zip code | 48.85% (14.97%) |
| LessHighSchool | % with less than high school diploma among people below poverty in a zip code | 22.41% (11.69%) |
| Unemployed | % of unemployed among people below poverty in a zip code | 23.35% (13.04%) |
| Non-Hispanic Black | % of Black persons among people below poverty | 18.7% (17.39%) |
| Hispanic | % of Hispanic persons among people below poverty in a zip code | 25.12% (23.32%) |
| Non-Hispanic White | % of non-Hispanic White persons among people below poverty in a zip code | 51.81% (26.9%) |
Table 3.
Results of logistic regression analysis
| Variables | Odds ratio | Confidence Interval | P value | |
|---|---|---|---|---|
| (2.5%, 97.5%) | ||||
| Telehealth utilization (audio or video) | Insurance: referenced to Medicare only | |||
| Medicaid only | 0.92 | (0.88, 0.96) | < 0.01 | |
| Both | 1.07 | (1.01, 1.12) | < 0.02 | |
| Gender: referenced to Female | ||||
| Male | 0.78 | (0.76, 0.81) | < 0.01 | |
| Age group: referenced to 65 + | ||||
| Age 45–64 | 1.69 | (1.62, 1.76) | < 0.01 | |
| Age 21–44 | 1.6 | (1.49, 1.72) | < 0.01 | |
| Disease type: referenced to Diabetes | ||||
| Chronic obstructive pulmonary disease | 0.95 | (0.92, 0.99) | 0.03 | |
| Heart failure | 0.86 | (0.79, 0.92) | < 0.01 | |
| Area: referenced to urban | ||||
| Rural | 0.57 | (0.54, 0.64) | < 0.01 | |
| Video utilization |
Insurance: referenced to Medicare only Medicaid only |
|||
| Both | 0.88 | (0.84, 0.92) | < 0.01 | |
| 1.06 | (1.01, 1.12) | < 0.02 | ||
| Gender: referenced to Female | ||||
| Male | 0.78 | (0.76, 0.81) | < 0.01 | |
| Age group: referenced to 65 + | ||||
| Age 45–64 | 1.63 | (1.56, 1.70) | < 0.01 | |
| Age 21–44 | 1.56 | (1.45, 1.68) | < 0.01 | |
| Disease Type: referenced to Diabetes | ||||
| Chronic obstructive pulmonary disease | 0.94 | (0.90, 0.98) | < 0.01 | |
| Heart failure | 0.85 | (0.79, 0.91) | < 0.01 | |
| Area: referenced to Urban | ||||
| Rural | 0.61 | (0.56, 0.66) | < 0.01 | |
| Audio utilization |
Insurance: referenced to Medicare only Medicaid only |
|||
| Both | 1.21 | (1.06, 1.38) | < 0.01 | |
| 2.15 | (1.93, 2.40) | < 0.01 | ||
| Gender: referenced to female | ||||
| Male | 0.81 | (0.75, 0.87) | < 0.01 | |
| Age group: referenced to 65 + | ||||
| Age 45–64 | 2.49 | (2.30, 2.70) | < 0.01 | |
| Age 21–44 | 2.09 | (1.85, 2.38) | < 0.01 | |
| Disease Type: referenced to Diabetes | ||||
| Chronic obstructive pulmonary disease | 1.08 | (1.00, 1.17) | 0.04 | |
| Heart failure | 0.92 | (0.80, 1.06) | 0.25 | |
| Area: referenced to Urban | ||||
| Rural | 0.6 | (0.51, 0.71) | < 0.01 | |
As shown in Table 4, our linear regression analysis suggests that zip code telehealth utilization is negatively associated with the percentage of people with less than a high school diploma in a community. Thus, telehealth inequities exist among minority communities with low education levels. While unemployment rate has no statistically significant impact on zip code telehealth utilization, race and ethnicity are significant factors. Our results also suggest that in Florida, zip code telehealth utilization is positively associated with the percentage of Hispanic people in zip code, while the percentages of the Non-Hispanic Black and White populations show a negative association; Fig. 1 shows the distribution of telehealth use across the State of Florida.
Table 4.
Results of linear regression analysis
| Variable | Coefficients | Standard error | t Stat | P value |
|---|---|---|---|---|
| LessHighSchool | − 0.21 | 0.05 | − 4.49 | < 0.01 |
| Unemployed | 0.02 | 0.04 | 0.62 | 0.53 |
| Non-Hispanic Black | − 0.05 | 0.03 | − 1.95 | 0.05 |
| Hispanic | 0.23 | 0.02 | 10.26 | < 0.01 |
| Non-Hispanic White | − 0.15 | 0.02 | − 7.09 | < 0.01 |
Fig. 1.
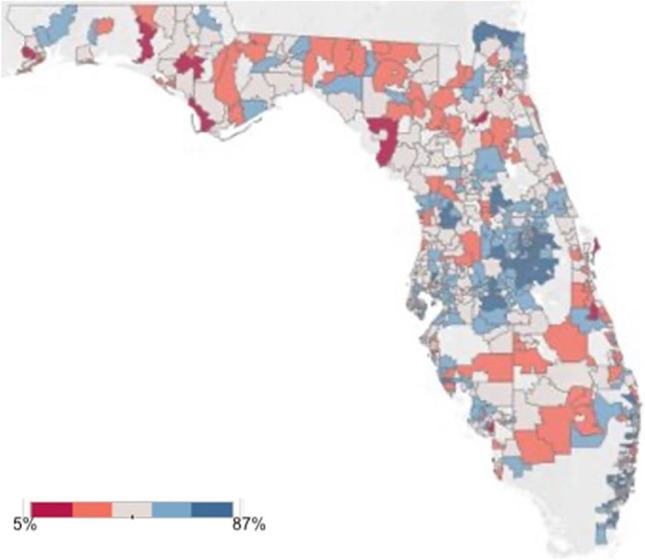
Percentage of Medicaid patients who utilized Telehealth
Discussion
Chronic Disease Management
We examined Medicaid recipients in the State of Florida and limited our study to patients who are diagnosed with diabetes, heart failure, and chronic obstructive pulmonary diseases. Our results suggest that Medicaid recipients were less likely to use telehealth than Medicare recipients. Given the qualifications for Medicaid in Florida, this finding is reasonable as people in lower income positions are associated with less resources and less access to telehealth. Research suggested that chronic disease management via telehealth and in-person care provide similar clinical outcomes, yet the lack of in-person options did not encourage telehealth use [17, 29, 30]. The pandemic decreased the options for people in vulnerable communities to receive care and adversely affected chronic disease management [17]. Chudasama et al. (2020) reported that 67% of providers perceived that the pandemic had a moderate to severe effect on chronic disease management; 45% of healthcare professionals offered only telephone support, 35% provided telephone and in-person, and 14% maintained only in-person care [15]. In resource-constrained settings, people without access to technology and were diagnosed with a chronic disease were either forced to seek in-person care, risking COVID-19 exposure, or delay care until urgent care was needed [31]. Studies reported that overall hospital readmissions related to chronic diseases decreased by 40–50% during COVID-19; however, mortality rate increased three-fold [32–34]. The complexity of chronic disease management and lack of health-related technology use highlights the adverse effects of the digital divide on healthcare access and outcomes.
Telehealth Inequities
Chronic disease management and telehealth use inequities are exacerbated by several factors such as geography, race, ethnicity, and education. Our study suggests that individuals in urban areas across public insurances were more likely to use telehealth than in rural areas. This aligns with other studies that suggested that Medicaid or Medicare enrollees who lived in urban areas were more likely than enrollees who lived in rural areas to access telehealth [35–38]. While telehealth provides a geographically location-friendly service that is beneficial to rural or remote populations, the benefits are not fully realized. Dowler and colleagues (2021) suggested that increased utilization in urban areas was partially due to the increased access to the internet and technology equipment [36]. Approximately 33% of people who lived in rural areas have limited access to telehealth technology [38]. Among people in these areas who do have access to telehealth, a study suggested that over 50% experienced internet interruptions during a telehealth visit [38].
Among minority groups, our study found that Hispanic patients were higher telehealth users when compared to Non-Hispanic Black and White patients. There is a lack of research that examines telehealth use among low-income minority groups with chronic diseases. Park et al.’s (2018) finding suggested that among underserved populations, Hispanics patients had a higher likelihood of using telehealth than Non-Hispanic Black patients but less than Non-Hispanic White patients; this study did not consider patients with chronic diseases [6]. Jain and colleagues (2021) suggested that Hispanic patients were lower utilizers of technology when compared to other racial and ethnic groups; however, this study did not consider socioeconomic position and chronic disease [39]. Further research is needed on cultural and racial factors that influence telehealth use among people in low income positions with chronic disease.
Education is an important factor in our study and has implications for health and digital literacy [40–43]. Education is critical for self-care management in chronic diseases and significantly affects health outcomes [42]. Banbury et al.’s (2020) study suggested that when literacy improved self-efficacy and self-care management improved and has the potential to favorably affect health outcomes [43]. However, the relationship between education and race is concerning for Non-Hispanic Black patients. A systemic review suggested that the literacy rates were lower for Non-Hispanic Black patients (38.3%), when compared to Hispanic (31.3%) and Non-Hispanic White patients (13.2%) [44]. Research suggested that Non-Hispanic Black patients in low-income positions have low educational attainments and were at higher risk for chronic diseases [44]. These trends should be noted by payers and providers with calls for strategic action to bolster educational efforts and access to resources.
Recommendations
While federal policies and modifications in reimbursement practices removed barriers to telehealth access use, these changes had little effect Medicaid beneficiaries [45]. Solutions that are not aligned with the health needs of the patient will contribute to health inequities that may be exacerbated by the digital divide. Based on the results of this study, we propose several recommendations. First, the public technology infrastructure among low-income and rural communities to access telehealth needs to be supported [46]. In the digital and information age, people who do not have access to the internet and technology will continue to experience health inequities. Secondly, we recommend educational programming that supports literacy among Non-Hispanic Black communities. Literacy is key to increasing outcomes in disease management programs; without digital and health literacy, telehealth utilization will continue to fall short [47, 48]. Meaningful use of technology that promotes literacy can lead to sustained progress in chronic disease management. Thirdly, it is critical that we develop a team-based approach that spans traditional, in-person care and telehealth delivery. A hybrid model of care empowers providers to shift between in-person and digital systems; this allows patients to engage with health-related technology and permits patient to become familiar with their healthcare team across platforms [49]. Telehealth can provide a holistic approach to improve access to healthcare services, yet without the readiness of the care recipient, digital health will complicate access to care [50].
Our results should be carefully considered. In this study, we examined patients with chronic conditions who are also in low-income positions using an administrative database; thus, it is subject to the limitations of administrative databases. We analyzed a specific population among Medicaid beneficiaries in the State of Florida. While this organization is one of the largest providers of Medicaid services in Florida, future studies should examine all Medicaid beneficiaries. It is also prudent to examine the resources of providers that serve low-income minority communities; providers may not have adequate resources to meet the complex social and medical needs of their community. By examining health inequities among low-income minority populations, we will be able to enact measures to mitigate health inequities in telehealth utilization from patient and provider perspectives.
Conclusion
Difficulties in accessing healthcare services are a long-standing challenge in the US healthcare system. Health inequities are delineated by race, ethnicities, geographic regions, socioeconomic status, and other social determinants of health. Inequities in access have considerable influence on quality of life and related outcomes. While there are considerable efforts to decrease inequities in healthcare access, events such as the proliferation of technology in healthcare and the global coronavirus pandemic of 2019 eclipse equity in access efforts. The challenges in telehealth utilization could become more problematic. Without patient engagement, vulnerable groups will suffer from health inequities that are exacerbated by digital access.
Author Contribution
CW contributed to the conception and the design of the study, interpretation of results, and drafting/revising of the work. DS contributed to the design of the study, interpretation, and analysis and revising of the data. All authors approved the final version of the manuscript.
Funding
The authors did not receive support from any organization for the submitted work.
Data Availability
The data that support the findings of this study are available from but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission. Email corresponding author.
Code Availability
Not applicable.
Declarations
Ethics Approval
University IRB provided ethical approval.
Consent to Participate
Waiver of consent approved by the University IRB.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Keesara S, Jonas A, Schulman K. Covid-19 and health care’s digital revolution. New England J Med. 2020;382(23):82. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- 2.Hick JL, Biddinger PD. Novel coronavirus and old lessons—Health System for The Pandemic. N Engl J Med. 2020;382(20):55. doi: 10.1056/NEJMp2005118. [DOI] [PubMed] [Google Scholar]
- 3.Demeke HB, Merali S, Marks S, Pao LZ, Romero L, Sandhu P, Clark H, Clara A, McDow KB, Tindall E, Campbell S, Bolton J, Le X, Skapik JL, Nwaise I, Rose MA, Strona FV, Nelson C, Siza C. Trends in Use of Telehealth Among Health Centers During the COVID-19 Pandemic - United States, June 26-November 6, 2020. MMWR. Morb Mortal Wkly Rep. 2021;70(7):240–244. doi: 10.15585/mmwr.mm7007a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jnr BA. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):1–9. doi: 10.1007/s10916-020-01596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park J, Erikson C, Han X, Iyer P. Are state telehealth policies associated with the use of telehealth services among underserved populations? Health Aff. 2018;37(12):2060–2068. doi: 10.1377/hlthaff.2018.05101. [DOI] [PubMed] [Google Scholar]
- 7.Medicaid Planning. Retrieved from https://www.medicaidplanningassistance.org/medicaid-eligibility-florida/. Accessed 22 June 2022.
- 8.Federal Poverty Level,. Retrieved from https://www.healthcare.gov/glossary/federal-poverty-level-fpl/. Accessed 22 June 2022.
- 9.Florida Medicaid. Benefits. Retrieved from https://www.benefits.gov/benefit/1625. Accessed 22 June 2022.
- 10.Daniel-Robinson L & Moore JE. Innovation, and opportunities to address social determinants of health in Medicaid managed care. Institute for Medicaid Innovation, (2019);1–24.
- 11.Matthew P, Brodersen DM. Income inequality and health outcomes in the United States: An empirical analysis. Soc Sci J. 2018;55(4):432–442. doi: 10.1016/j.soscij.2018.05.001. [DOI] [Google Scholar]
- 12.Milani RV, Bober RM, Lavie CJ. The role of technology in chronic disease care. Prog Cardiovasc Dis. 2016;58(6):579–583. doi: 10.1016/j.pcad.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Shaw KM, Theis KA, Self-Brown S, Roblin DW, Barker L. Chronic disease disparities by county economic status and metropolitan classification, Behavioral Risk Factor Surveillance System, 2013. Prev Chronic Dis. 2016;13:E119. doi: 10.5888/pcd13.160088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doshi R, Aseltine RH, Sabina AB, et al. Interventions to improve management of chronic conditions among racial and ethnic minorities. J Racial Ethn Health Disparities. 2017;4:1033–1041. doi: 10.1007/s40615-017-0431-4. [DOI] [PubMed] [Google Scholar]
- 15.Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, Khunti K. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14(5):965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horrell LN, Hayes S, Herbert LB, MacTurk K, Lawhon L, Valle CG, Bhowmick A. Telemedicine use and health-related concerns of patients with chronic conditions during COVID-19: survey of members of online health communities. J Med Internet Res. 2021;23(2):e23795. doi: 10.2196/23795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hossain M, Dean EB, Kaliski D. Using administrative data to examine telemedicine usage among medicaid beneficiaries during the Coronavirus Disease 2019 Pandemic. Med Care. 2022;60(7):488–495. doi: 10.1097/MLR.0000000000001723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suphanchaimat R, Kantamaturapoj K, Putthasri W, Prakongsai P. Challenges in the provision of healthcare services for migrants: a systematic review through providers’ lens. BMC Health Serv Res. 2015;15(1):1–14. doi: 10.1186/s12913-015-1065-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: How COVID-19's telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83(5):e345–e346. doi: 10.1016/j.jaad.2020.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang JE, Lai AY, Gupta A, Nguyen AM, Berry CA, Shelley DR. Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post-COVID era. Milbank Q. 2021;99(2):340–368. doi: 10.1111/1468-0009.12509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Durand MA, Yen RW, O’Malley J, Elwyn G, Mancini J. Graph literacy matters: Examining the association between graph literacy, health literacy, and numeracy in a Medicaid eligible population. PloS one. 2020;15(11):e0241844. doi: 10.1371/journal.pone.0241844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nouri S, Khoong EC, Lyles CR & Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catalyst Innovations in Care Delivery, (2020);1(3). 10.1056/CAT.20.0123
- 23.Mitchell UA, Chebli PG, Ruggiero L, Muramatsu N. The digital divide in health-related technology use: the significance of race/ethnicity. Gerontologist. 2019;59(1):6–14. doi: 10.1093/geront/gny138. [DOI] [PubMed] [Google Scholar]
- 24.Smith CB & Bhardwaj AS. Disparities in the use of telehealth during the COVID-19 pandemic (2020). 10.1200/JCO.2020.38.29
- 25.Wegermann K, Wilder JM, Parish A. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19, Digestive Diseases and Sciences, (2021);1–7. 10.1007/s10620-021-06842-5 [DOI] [PMC free article] [PubMed]
- 26.Bureau USC. Explore census data. Retrieved from https://data.census.gov/cedsci/. Accessed 26 Aug 2022.
- 27.Chen JT, Krieger N. Revealing the unequal burden of covid-19 by income, race/ethnicity, and household crowding: us county versus zip code analyses. J Public Health Manag Pract. 2021;27(1):S43–S56. doi: 10.1097/PHH.0000000000001263. [DOI] [PubMed] [Google Scholar]
- 28.Whaley CM, Pera MF, Cantor J, Chang J, Velasco J, Hagg HK, ... & Bravata DM. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA network open, (2020);3(11): e2024984-e2024984. 10.1001/jamanetworkopen.2020.24984 [DOI] [PMC free article] [PubMed]
- 29.Rural-urban commuting area codes. USDA ERS - rural-urban commuting area codes. Retrieved from https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx. Accessed 3 May 2022.
- 30.Hanlon Daines L, Campbell C, McKinstry B, Weller D, Pinnock H. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res. 2017;19(5):e172–e172. doi: 10.2196/jmir.6688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saqib MAN, Siddiqui S, Qasim M, Jamil MA, Rafique I, Awan UA, ... & Afzal MS. Effect of COVID-19 lockdown on patients with chronic diseases. Diab Metabol Syndr Clin Res Rev. 2020;14(6):1621–1623. 10.1016/j.dsx.2020.08.028 [DOI] [PMC free article] [PubMed]
- 32.Frankfurter C, Buchan TA, Kobulnik J, et al. Reduced rate of hospital presentations for heart failure during the COVID-19 pandemic in Toronto. Canada Can J Cardiol. 2020;36(10):1680–1684. doi: 10.1016/j.cjca.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jimenez-Blanco Bravo M, Cordero Pereda D, Sanchez Vega D, et al. Heart failure in the Time of COVID-19. Cardiol. 2020;145(8):481–484. doi: 10.1159/000509181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Almufleh A, Ahluwalia M, Givertz MM, et al. Short-term Outcomes in Ambulatory Heart Failure during the COVID-19 Pandemic: insights from Pulmonary Artery Pressure Monitoring. J Card Fail. 2020;26(7):633–634. doi: 10.1016/j.cardfail.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hwang EH, Guo X, Tan Y, Dang Y. Delivering healthcare through teleconsultations: implications for offline healthcare disparity. Inf Syst Res. 2022;33(2):515–539. doi: 10.1287/isre.2021.1055. [DOI] [Google Scholar]
- 36.Dowler S, Crosbie K, Thompson S, Drucker E, Jackson C. Telemedicine utilization trends during the COVID-19 public health emergency. North C Med J. 2021;82(4):255–258. doi: 10.18043/ncm.82.4.255. [DOI] [PubMed] [Google Scholar]
- 37.Bauerly BC, McCord RF, Hulkower R, Pepin D. Broadband access as a public health issue: the role of law in expanding broadband access and connecting underserved communities for better health outcomes. J Law Med Ethics. 2019;47(2):39–42. doi: 10.1177/1073110519857314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khoong EC, Butler BA, Mesina O, Su G, DeFries TB, Nijagal M, Lyles CR. Patient interest in and barriers to telemedicine video visits in a multilingual urban safety-net system. J Am Med Inform Assoc. 2021;28(2):349–353. doi: 10.1093/jamia/ocaa234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jain V, Al Rifai M, Lee MT, Kalra A, Petersen LA, Vaughan EM, ... & Virani SS. Racial and geographic disparities in internet use in the US among patients with hypertension or diabetes: implications for telehealth in the era of COVID-19. Diabetes Care, (2021);44(1): e15-e17. :10.2337/dc20-2016 [DOI] [PMC free article] [PubMed]
- 40.Mechanic D, Tanner J. Vulnerable people, groups, and populations: societal view. Health Aff. 2007;26(5):1220–1230. doi: 10.1377/hlthaff.26.5.1220. [DOI] [PubMed] [Google Scholar]
- 41.Mariga L, McConkey R, Myezwa H. Inclusive Education in Low-Income Countries: A resource book for teacher educators, parent trainers and community development. In: African Books Collective. Cape Town, South Africa: Disability Innovations Africa; 2014.
- 42.Lindsay Kobayashi C, Andrew S. Social isolation, loneliness, and health behaviors at older ages: longitudinal cohort study. Ann Behav Med. 2018;52(7):582–593. doi: 10.1093/abm/kax033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Banbury A, Nancarrow S, Dart J, Gray L, Dodson S, Osborne R, Parkinson L. Adding value to remote monitoring: co-design of a health literacy intervention for older people with chronic disease delivered by telehealth-The telehealth literacy project. Patient Educ Couns. 2020;103(3):597–606. doi: 10.1016/j.pec.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 44.Stormacq C, Van den Broucke S, Wosinski J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integr Rev Health Promot Int. 2019;34(5):e1–7. doi: 10.1093/heapro/day062. [DOI] [PubMed] [Google Scholar]
- 45.Cook BL, Trinh NH, Li Z, Hou SSY, Progovac AM. Trends in racial-ethnic disparities in access to mental health care. Psychiatr Serv. 2017;68(1):9–16. doi: 10.1176/appi.ps.201500453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wayne K, Hynes M. Remotely connected?: A comparative analysis of the development of rural broadband infrastructure and initiatives. In: Service Provision and Rural Sustainability. London, UK: Routledge; 2018. p. 142–161.
- 47.Shan R, Sarkar S, Martin SS. Digital health technology and mobile devices for the management of diabetes mellitus: state of the art. Diabetol. 2019;62(6):877–887. doi: 10.1007/s00125-019-4864-7. [DOI] [PubMed] [Google Scholar]
- 48.Clare CA. Telehealth and the digital divide as a social determinant of health during the COVID-19 pandemic. Netw Model Anal Health Inf Bioinforma. 2021;10(1):1–3. doi: 10.1007/s13721-021-00300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chin MH. Uncomfortable truths—what covid-19 has revealed about chronic-disease care in America. N Engl J Med. 2021;385(18):1633–1636. doi: 10.1056/NEJMp2112063. [DOI] [PubMed] [Google Scholar]
- 50.Johnson KF, Mahan LB. Interprofessional collaboration and telehealth: Useful strategies for family counselors in rural and underserved areas. Fam J. 2021;28(3):215–224. doi: 10.1177/1066480720934378. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission. Email corresponding author.
Not applicable.


