ABSTRACT
The coronavirus disease 2019 (COVID-19) pandemic has psychological consequences such as increased risk of depression, anxiety, and stress problems, exacerbating human health disparities. This study aimed to analyze depression and its causes in COVID-19-recovered patients in Bangladesh. A cross-sectional study was conducted on COVID-19-recovered patients who attended follow-up visits after 14 days to 3 months at Dhaka Medical College Hospital (DMCH) and Dhaka North City Corporation Hospital (DNCCH), Dhaka, Bangladesh, from 1 January to 31 December 2021. Respondents were face-to-face interviewed with a semistructured questionnaire after written agreement. The Patient Health Questionnaire (PHQ-9) was used to assess respondents’ depression, and data were analyzed using SPSS version 23, with a P value of <0.05 indicating statistical significance. A total of 325 COVID-19-recovered patients aged from 15 to 65 years (mean, 44.34 ± 13.87 years) were included in this study, the highest proportion (23.1%) of them were aged 46 to 55 years, and the majority (61.5%) of them were male. There were 69.5% of respondents who had no signs of depression while 31% of them did have signs, with 26.7% being mildly depressed, 2.5% being extremely depressed, and 1.2% being severely depressed. Diabetes mellitus, hospitalization duration, social distancing, social media posts on COVID-19, loss of employment, family damage, and fear of reinfection were significantly associated with depression level of respondents. This study gives us a glimpse into the psychological health of COVID-19-recovered patients, and its findings highlight the imperative of alleviating their psychological anguish in Bangladesh.
IMPORTANCE The COVID-19 pandemic had a significant psychological impact on healthy populations, with increased depression, perceived stress, posttraumatic stress disorder, and insomnia reported. The COVID-19 pandemic affects people’s mental health by instilling fear of infection and depression. In the post-COVID-19 syndrome, depressive symptoms and clinically significant depression may have serious consequences for quality-of-life outcomes. To combat the spread of COVID-19, the Bangladesh government has implemented a number of measures, including lockdown, social distancing, self-isolation, and quarantine. Given the negative consequences, it is critical to investigate potential factors and mechanisms that may shed light on mental health improvement. The purpose of the study is to determine the level of depression in patients 3 months after recovering from acute COVID-19. The study’s findings highlight the need for COVID-19-infected people in Bangladesh to receive health education and interventions.
KEYWORDS: Bangladesh, COVID-19-recovered patients, depression, NIPSOM, PHQ-9 scale
INTRODUCTION
Since the dawn of 2020, the world has faced a pandemic caused by SARS-CoV-2, the highly contagious COVID-19 (1). Bangladesh has been suffering from this highly transmissible disease since March 2020 (2). The rapid spread of the disease in a wide variety of people makes them subject to varied degrees of panic, which makes it difficult to treat and rehabilitate them (3). According to earlier studies, viral respiratory infections are linked to chronic and acute psychological effects among the survivors including posttraumatic stress, insomnia, depression, anxiety, and even suicidality. After discharge, many of these patients’ mental disturbances persisted and continued for a long time (4, 5).
The COVID-19 pandemic has a significant psychological impact on healthy populations, with an increase in depression, perceived stress, posttraumatic stress, and insomnia being reported (6). The COVID-19 pandemic situation is fast-changing with worldwide case counts of crisis, suicide, domestic violence, mental disorder, anxiety, and depressive disorders (7). To combat the spread of COVID-19, the Bangladesh government has implemented a number of measures, including lockdown, social distancing, self-isolation, and quarantine (8). Besides, recent findings have demonstrated prevailing acute psychiatric symptoms among patients while being treated in isolation, lacking interaction with friends, family, or loved ones, being admitted to intensive care units (ICUs), and requiring mechanical ventilation (9). Extreme fear, when accompanied with social and economic implications (e.g., job loss, reduced earnings, relationship problems), has the potential to encourage individuals to engage in irrational thinking, which can lead to psychological discomfort (10).
In prior lethal viral epidemics, fear of death, loneliness, boredom, anxiety, sadness, social isolation, contagion, and (in severe situations) thoughts of suicide might result in long-term psychological repercussions among the general population (11). In the present COVID-19 pandemic, depression and anxiety problems are more activated. A recent systematic review reported that the pooled prevalence of depression and anxiety among COVID-19 patients was 45% and 47%, respectively (12).
Patients with COVID-19 have different degree of psychological pain such as anxiety and depression, which may worsen their prognosis by negatively affecting the patients’ immunity. As a result, clinically significant depression could have serious consequences for quality of life (13). Despite its increasing significance, present estimates on the prevalence of psychological distress, such as anxiety and depressive symptoms, among COVID-19 patients are uncertain (12).
In the aftermath of a natural disaster, a high rate of mental health suffering (i.e., a prevalence rate of 65% depression, much higher than rates reported elsewhere) was previously reported and appears to reflect the vulnerability of the Bangladeshi population to mental health suffering in a pandemic situation such as COVID-19 (14). During pandemics, public health officials and the media are more concerned with the biological and physical consequences of the outbreak than with mental health difficulties. With an increasing number of reports indicating that the COVID-19 outbreak is causing an increase in mental health burden, there have been greater calls for steps to improve mental health support for the public (15).
To date, scant findings on COVID-19 have been reported regarding the prevalence and associated factors of depression among COVID-19=recovered patients in Bangladesh. Therefore, this study aimed to comprehensively assess the level of depression and explore the factors associated with depressive symptoms 3 months after recovery from COVID-19 infection.
RESULTS
Sociodemographic characteristics of respondents.
This study comprised a total of 325 respondents, whose ages ranged from 15 to 65 years. The respondents’ mean age was 44.34 years, with standard deviation (SD) of ±13.87 years, and the highest proportion (23.1%) were between 46 and 55 years old. The majority of respondents (61.5%) were men, 75.7% were married, 92% were Muslims, 21.2% were graduates, 31.4% were business owners, 81.5% belonged to nuclear families, 61.5% resided in urban areas, 89.2% of them had only one family member who was financially contributing, 37% of respondents did not complete vaccination against COVID-19, and hypertension was found to be the most prevalent chronic disease (Table 1).
TABLE 1.
Sociodemographic characteristics of the respondents
| Characteristic | Frequency (f) | % |
|---|---|---|
| Age (yr) | ||
| 15–25 | 37 | 11.4 |
| 26–35 | 72 | 22.2 |
| 36–45 | 65 | 20.0 |
| 46–55 | 75 | 23.1 |
| 56–65 | 65 | 20.0 |
| 66–75 | 11 | 3.4 |
| Mean (±SD) | 44.34 ± 13.87 | |
| Sex | ||
| Male | 200 | 61.5 |
| Female | 125 | 38.5 |
| Marital status | ||
| Married | 246 | 75.7 |
| Single | 45 | 13.8 |
| Widowed | 31 | 9.5 |
| Separated | 2 | 0.6 |
| Divorced | 1 | 0.3 |
| Religion | ||
| Islam | 299 | 92.0 |
| Hinduism | 25 | 7.7 |
| Christianity | 1 | 0.3 |
| Educational qualification | ||
| Illiterate | 64 | 19.7 |
| Primary | 65 | 20.0 |
| Secondary | 55 | 16.9 |
| Higher secondary | 49 | 15.1 |
| Graduation | 69 | 21.2 |
| Postgraduation | 23 | 7.1 |
| Occupation | ||
| Government employee | 30 | 9.2 |
| Private employee | 51 | 15.7 |
| Businessperson | 102 | 31.4 |
| Homemaker | 81 | 24.9 |
| Student | 34 | 10.5 |
| Type of family | ||
| Nuclear family | 265 | 81.5 |
| Extended family | 60 | 18.5 |
| Residency | ||
| Urban | 200 | 61.5 |
| Rural | 125 | 38.5 |
| Income-earning family member(s) | ||
| Self or 1 | 290 | 89.2 |
| More than 1 | 35 | 10.8 |
| History of chronic disease | ||
| Diabetes mellitus | 91 | 28.0 |
| Cardiac disease | 20 | 6.2 |
| Asthma or COPDa | 66 | 20.3 |
| Kidney disease | 13 | 4.0 |
| Hypertension | 107 | 32.9 |
| History of vaccination against COVID-19 | ||
| Two doses completed | 205 | 63.1 |
| Not completed | 120 | 36.9 |
COPD, chronic obstructive pulmonary disease.
Distribution of conditions of COVID-19-recovered patients.
One-fourth of 325 respondents (25.2%) had personal life interruptions and 78.2% had physical symptoms after COVID-19, primarily weakness (57%) and cough (31%). Of them, 4.3% were taking antidepressants, 1.2% had a family history of depression, 12% were hospitalized for more than 21 days, 10.8% needed ICU, and 12.3% were distressed due to social distancing. Also, 10.2% were affected by social media posts about COVID-19, 13% felt harmful to the family, 2.8% feared losing their jobs, 6.2% feared reinfection with COVID-19, and 29% had relatives or acquaintances who died from COVID-19 (Table 2).
TABLE 2.
Distribution of conditions of COVID-19-recovered patients (n = 325)
| Variable | Frequency | % |
|---|---|---|
| Interruption of personal life | 82 | 25.2 |
| Physical symptoms after recovery | 254 | 78.2 |
| Physical symptoms | ||
| Dyspnea | 63 | 19.4 |
| Weakness | 184 | 56.6 |
| Cough | 101 | 31.1 |
| Fatigue | 85 | 26.2 |
| Muscle pain | 30 | 9.2 |
| Palpitation | 45 | 13.8 |
| Taking antidepressant drug | 14 | 4.3 |
| Family history of depression | 4 | 1.2 |
| Duration of hospitalization (days) | ||
| 1–7 | 183 | 56.3 |
| 7–14 | 61 | 18.8 |
| 14–21 | 33 | 10.2 |
| More than 21 days | 39 | 12.0 |
| Needing ICU | 35 | 10.8 |
| Mental distress due to social distancing | 40 | 12.3 |
| Being affected by posts on social media about COVID-19 | 33 | 10.2 |
| Fear of being harmful to one’s family | 42 | 12.9 |
| Fear of losing job | 9 | 2.8 |
| Fear of reinfection with COVID-19 | 20 | 6.2 |
| Death of relative(s) or acquaintance(s) from COVID-19 | 93 | 28.6 |
Prevalence of depression.
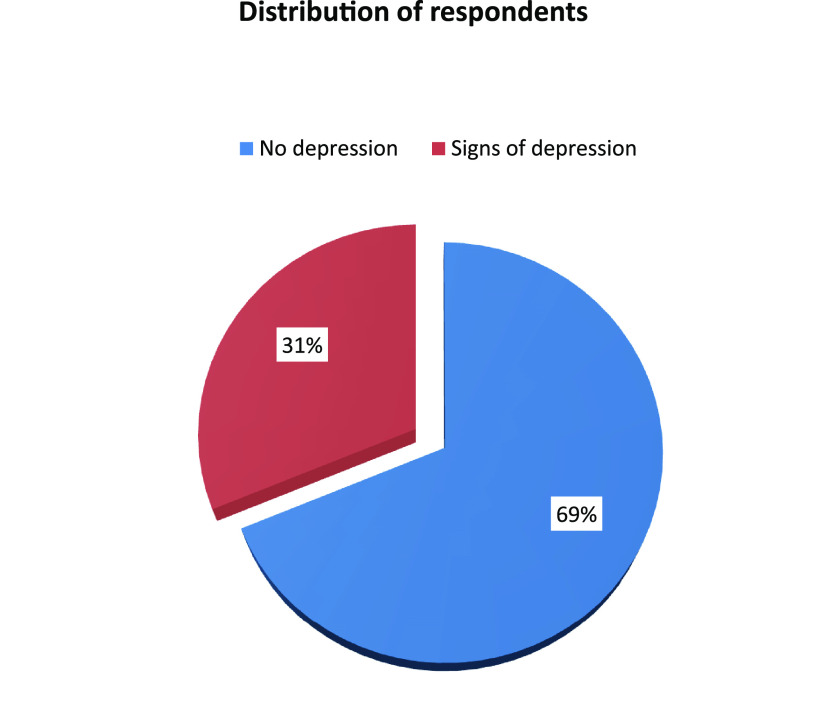
The prevalence of depression was assessed by a PHQ-9 scale comprising 9 items (Table 3) showing that about one-third of respondents (31%) had symptoms of depression (Fig. 1), whereas 87.8% of them were mildly depressed, 8.1% were moderately depressed, and 4.0% were severely depressed (Table 4).
TABLE 3.
Depression=related questions according to patient health questionnaire PHQ-9 (9 items) (n = 325)
| Attribute | No. (%) of respondents with frequency: |
|||
|---|---|---|---|---|
| Not at all | Several days | More than half of days | Nearly every day | |
| Little interest or pleasure in doing things | 244 (75.1) | 19 (5.8) | 27 (8.3) | 35 (10.8) |
| Feeling down or hopeless | 226 (69.5) | 51 (15.7) | 19 (5.8) | 29 (8.9) |
| Trouble falling or staying asleep or sleeping too much | 139 (42.8) | 74 (22.8) | 8 (2.5) | 104 (32) |
| Feeling tired or having little energy | 103 (31.7) | 81 (24.9) | 6 (1.8) | 135 (41.5) |
| Poor appetite or overeating | 149 (45.8) | 48 (14.8) | 6 (1.8) | 122 (37.5) |
| Feeling bad about oneself | 292 (89.8) | 11 (3.4) | 18 (5.5) | 4 (1.2) |
| Trouble concentrating | 283 (87.1) | 25 (7.7) | 3 (0.9) | 14 (4.3) |
| Moving or speaking slowly | 271 (83.4) | 44 (13.5) | 6 (1.8) | 4 (1.2) |
| Thoughts that one would be better off dead | 307 (94.5) | 6 (1.8) | 3 (0.9) | 9 (2.8) |
FIG 1.
Distribution of respondents according to signs of depression (n = 325).
TABLE 4.
Distribution of respondents according to level of depression (n = 99)
| Level of depression | Frequency (f) | % |
|---|---|---|
| Mild | 87 | 87.9 |
| Moderate | 8 | 8.1 |
| Severe | 4 | 4.0 |
Association of prevalence of depression with variables of respondent.
The variables of educational qualification, diabetes mellitus history, duration of hospitalization, distress due to social distancing, being affected by posts on social media about COVID-19, fear of job loss, feeling harmful to family members, fear of reinfection, taking an antidepressant drug, and interruption of personal life were significantly associated with the prevalence of depression (P < 0.05) (Table 5).
TABLE 5.
Association of level of depression with variables of respondent (n = 325)
| Association | Test value | P value |
|---|---|---|
| Sex of respondent | 3.081 | 0.379 |
| Educational qualification | 36.701 | 0.001 |
| History of diabetes mellitus | 13.005 | 0.003 |
| Duration of hospitalization | 19.520 | 0.007 |
| Mental distress due to social distancing | 28.881 | 0.001 |
| Being affected by posts on social media | 32.667 | 0.001 |
| Fear of losing job | 10.780 | 0.013 |
| Fear of being harmful to family members | 29.990 | 0.001 |
| Fear of further contamination | 13.715 | 0.003 |
| Receiving antidepressant drug | 11.550 | 0.006 |
| Interruption of personal life | 48.963 | 0.001 |
DISCUSSION
This study found that among 325 respondents, 31% had depression symptoms, with 26.8% exhibiting mild symptoms, 2.5% exhibiting moderate symptoms, and 1.2% exhibiting severe symptoms. Several studies were undertaken in Bangladesh following the commencement of COVID-19 to assess mental health, including depression. A cross-sectional study was conducted at the initial stage after the COVID-19 outbreak (from 1 June to 10 June 2020) among 1,146 Bangladeshi participants by Zubayer et al. (16), in which 47.2% of participants had depression, with 16.2% being mildly depressed, 20.4% moderately depressed, and 6.5% severely depressed, rates which were higher than those in this study. Another study, conducted by Das et al. (17), among 672 Bangladeshi people aged between 15 and 65 years from 15 April to 10 May 2020 reported a prevalence of depression of 38% with 24% being mildly depressed, 11% moderately depressed, and 3% severely depressed. Another study conducted among Bangladeshi students during the COVID-19 pandemic reported the prevalence rates of depression to be 46.9% (18). The increased prevalence of depression could be attributed to the virus’s ongoing transmission, the increasing number of new cases, the death of a loved one, and the fear of infection during the early stages of the COVID-19 outbreak, when individuals were challenged by mandatory quarantine, unexpected unemployment, and uncertainty associated with the outbreak (16, 18).
According to certain research, depressive symptoms were recorded at lower prevalence rates than in the present study, such as 16.5% of the Chinese population (19), 11.4% of Japanese people (20), 17.3% of Italians (3), 3.7% of Portuguese people (21), and 26% of Iranian people (22). Prevalence rates varied between studies, which could be explained by differences in government preparedness, the availability of medical supplies and facilities, the effective communication of information about COVID-19, or international/cultural variances affecting the psychological health of the general public (18).
According to the results of this study, the highest proportion (23.1%) of the respondents were between the ages of 46 and 55 years. This is because the risk of COVID-19-related illness and mortality increases with age (8). In some studies, individuals under the age of 45 had more adverse psychological symptoms during the pandemic (23, 24). This is consistent with our findings that about 54% of the participants were below 45 years of age. This finding could be explained in part by their role as family caregivers, who provide financial and emotional support to children and the elderly. Among the respondents, 61.5% were male, although females have been linked to mental health issues, but there were no significant sex differences (P = 0.379) in regard to depression in the current investigation (18, 25). Because of the COVID-19 condition, sex disparities in this study may be negated.
COVID-19 is highly contagious and can be passed from person to person (26). Therefore, individuals fear either having COVID-19 themselves or becoming asymptomatic carriers who spread the disease unknowingly to family and friends, contributing to psychiatric symptoms (21, 26). In line with previous studies, the present study also showed that fear of infection is significantly associated with depression (P = 0.001) (23, 27). That the death of a loved one leads to psychological problems, such as depression, is supported by the findings of the present study (26).
The present study showed that daily exposure to COVID-19-related news was significantly associated with overall mental health problems. Previous studies showed that people who were exposed to COVID-19-related news were more likely to develop psychiatric symptoms (23, 28). Moreover, symptoms of depression and anxiety among COVID-19 inpatients could increase due to uncertainty about the prognosis of the disease and the experience of adverse outcomes (16). Furthermore, side effects of COVID-19 medication and physical discomfort may also promote psychiatric problems among COVID-19 inpatients (28). This high prevalence of anxiety and depressive symptoms among Bangladeshi COVID-19 inpatients could be because of an inadequate health care system (8), shortage of beds, ICUs, and ventilators (16), treatment-related negligence in health care facilities (29), and less social interaction along with rampant circulation of misinformation on social and conventional media (30).
In this study, the result showed that 78.2% of respondents had physical symptoms after recovery from COVID-19 and weakness (56.6%) was the most prevalent feature. However, a prospective cohort study among the Bangladeshi population reported that the incidence of post-COVID-19 syndrome was 46%, and other features included persistent cough (8.5%), postexertional dyspnea (7%), headache (3.4%), vertigo (2.3%), and sleep-related disorders (5.9%), rates which were lower than those in the present study (31). COVID-19 can cause acute respiratory syndrome with consequent release of proinflammatory cytokines, including interleukin-1β (IL-1β) and IL-6, from the respiratory tract. These cytokines were commonly found to be increased in major depressive disorder (32).
Due to the COVID-19 epidemic, we have had to make some adjustments to our regular schedule. Because of the substantial changes in everyday lives, in this study, 25.2% had suffered from interruption of regular personal life, which has led to concerns in other studies on mental health (3, 16, 23).
The Pearson chi-square test was used in this study to evaluate the association between depression and sociodemographic characteristics with factors related to COVID-19-recovered patients. According to the results, education qualification (P = 0.001), diabetes mellitus comorbidity (P = 0.001), receiving an antidepressant drug (P = 0.006), having fear of further contamination (P = 0.003), feeling of being harmful to family members (P = 0.001), fear of losing one’s job (P = 0.013), being affected by social media posts about COVID-19 (P = 0.001), mental distress due to social distancing (P = 0.001), and duration of hospitalization (P = 0.007) were statistically significantly related to depression (P = 0.001), a finding which is consistent with other researches (12, 13, 16). The current study highlights the necessity for reducing this psychological suffering in Bangladesh. Appropriate supportive programs and interventional approaches should be implemented in Bangladesh during the COVID-19 pandemic.
Limitations.
This study has a few limitations. First, for convenience data were collected from the patient during the COVID-19 recovery period, which could result in recall and selection bias. Second, the risk factors for depression were not able to be analyzed in association with the level of depression. Third, all the respondents in this study were sampled from two selected post-COVID units in Dhaka city, so the generalizability of this study was indeterminate and might not present the whole country’s situation during the COVID-19 pandemic.
Conclusion.
That the state of depression impacts COVID-19-recovered patients is undeniable. The study found that a significant portion of respondents reported mental health problems, with different levels of severity of depression. Most of the respondents were concerned about the presence of COVID-19-related symptoms, and fear of losing jobs, fear of reinfection, distress due to social distancing, etc., provoked depression in individuals. The findings of the study suggest the need for more targeted measures like health education intervention for people infected with COVID-19 in Bangladesh to accelerate progress in reducing the incidence of depression.
MATERIALS AND METHODS
Study design.
This cross-sectional study was conducted among COVID-19-recovered patients, who came for follow-up from 14 days up to 3 months after infection at the post-COVID unit of Dhaka Medical College Hospital (DMCH) and Dhaka North City Corporation Hospital (DNCCH), Dhaka, Bangladesh, from 1 January to 31 December 2021. Patients with known cases of depressive illness and other psychiatric disorders were excluded from this study.
Sampling and sample size.
A nonprobability convenience sampling method was used, and to estimate the required sample size, the prevalence for depression was set as 47.2% (16). So, the calculated sample size was 382, but because of the unfavorable COVID-19 scenario, it was possible to conduct interviews with only 325 respondents during the designated data collection period.
Ethical considerations.
Ethical approval for the study was granted by the Institutional Review Board (IRB) of National Institute of Preventive and Social Medicine (NIPSOM) with memo no. NIPSOM/IRB/2021/18 dated 13 December 2021. Written informed consent for participation was required for this study in accordance with national legislation and institutional requirements.
Data collection.
According to the specific objectives and after the pretest observation, a semistructured questionnaire was developed in English and then translated into Bengali using the selected variables. The respondents were advised of the title and purpose of the study, their anonymity, and voluntary participation in the study by ensuring privacy and confidentiality.
Data collection instrument.
After informed written consent, the respondents were interviewed face to face with the questionnaire examining sociodemographic variables and the factors causing depression among them. The questionnaire was developed by using the patient health questionnaire (PHQ-9).
Level of depression.
PHQ-9 has nine different questions that assess the depressive symptoms of the respondents. The total score ranges from 0 to 27 points, where each question is scored from 0 to 3 depending on the answer: 0 (not at all), 1 (several days), 2 (half of the days), and 3 (nearly every day). To determine the state of depression, the total score was divided into four categories: cumulative scores of <10 indicate no depression, 10 to 15 indicate mild depression, 16 to 21 indicate moderate depression, and 22 to 27 indicate severe depression (17).
Statistical analysis.
Data processing and analysis were done using Statistical Package for Social Sciences (SPSS) version 23 according to objectives and variables. Frequency, percentage, mean, and standard deviation (SD) were used for descriptive statistics, chi-square (χ2) tests were carried out to assess the association of qualitative data with 95% confidence interval (CI), and a P value of <0.05 was considered statistically significant. Data are presented through tables and figures.
Data availability.
The original contributions presented in the study are included in the article; further inquiries can be directed to the corresponding author.
ACKNOWLEDGMENTS
We express our gratitude to all who participated and filled out the study.
We declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
K.K. was involved in setting up the study, data collection, and data analysis. N.F. drafted the manuscript. Both authors made comments on the different versions, added to the article, and approved the version that was submitted.
This work was not supported by any funding agency.
Contributor Information
Nasreen Farhana, Email: nas.farhana19@gmail.com.
Clinton J. Jones, Oklahoma State University
REFERENCES
- 1.World Health Organization (WHO). 2020. Coronavirus. https://www.who.int/health-topics/coronavirus#tab=tab_3. Accessed 15 November 2020.
- 2.Director General of Health Services (DGHS). 2020. Corona virus information. Ministry of Health and Family Welfare, Dhaka, Bangladesh. https://corona.gov.bd/. Accessed 13 November 2020.
- 3.Liu S, Yang L, Zhang C, Xiang Y-T, Liu Z, Hu S, Zhang B. 2020. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HC, Yoo SY, Lee BH, Lee SH, Shin HS. 2018. Psychiatric findings in suspected and confirmed Middle East respiratory syndrome patients quarantined in hospital: a retrospective chart analysis. Psychiatry Investig 15:355–360. doi: 10.30773/pi.2017.10.25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lam MH-B, Wing Y-K, Yu MW-M, Leung C-M, Ma RCW, Kong APS, So WY, Fong SY-Y, Lam S-P. 2009. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch Intern Med 169:2142–2147. doi: 10.1001/archinternmed.2009.384. [DOI] [PubMed] [Google Scholar]
- 6.Rajkumar RP. 2020. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr 52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sifat RI. 2020. Impact of the COVID-19 pandemic on domestic violence in Bangladesh. Asian J Psychiatr 53:102393. doi: 10.1016/j.ajp.2020.102393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anwar S, Nasrullah M, Hosen MJ. 2020. COVID-19 and Bangladesh: challenges and how to address them. Front Public Health 8:154. doi: 10.3389/fpubh.2020.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li W, Yang Y, Liu Z-H, Zhao Y-J, Zhang Q, Zhang L, Cheung T, Xiang Y-T. 2020. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci 16:1732–1738. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pakpour AH, Griffiths MD. 2020. The fear of COVID-19 and its role in preventive behaviors. J Concurr Disord 2:58–63. http://irep.ntu.ac.uk/id/eprint/39561. [Google Scholar]
- 11.Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. 2009. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry 31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, Huang E, Zuo QK. 2021. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci 1486:90–111. doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Renaud-Charest O, Lui LMW, Eskander S, Ceban F, Ho R, Di Vincenzo JD, Rosenblat JD, Lee Y, Subramaniapillai M, McIntyre RS. 2021. Onset and frequency of depression in post-COVID-19 syndrome: a systematic review. J Psychiatr Res 144:129–137. doi: 10.1016/j.jpsychires.2021.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mamun MA, Hossain MS, Griffiths MD. 2022. Mental health problems and associated predictors among Bangladeshi students. Int J Ment Health Addict 20:657–671. doi: 10.1007/s11469-019-00144-8. [DOI] [Google Scholar]
- 15.Ho CS, Chee CY, Ho RC. 2020. Mental health strategies to combat the psychological impact of coronavirus disease 2019 (COVID-19) beyond paranoia and panic. Ann Acad Med Singap 49:155–160. doi: 10.47102/annals-acadmedsg.202043. [DOI] [PubMed] [Google Scholar]
- 16.Zubayer AA, Rahman ME, Islam MB, Babu SZD, Rahman QM, Bhuiyan MRAM, Khan MKA, Chowdhury MAU, Hossain L, Habib RB. 2020. Psychological states of Bangladeshi people four months after the COVID-19 pandemic: an online survey. Heliyon 6:e05057. doi: 10.1016/j.heliyon.2020.e05057. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Das R, Hasan MR, Daria S, Islam MR. 2021. Impact of COVID-19 pandemic on mental health among general Bangladeshi population: a cross-sectional study. BMJ Open 11:e045727. doi: 10.1136/bmjopen-2020-045727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. 2020. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dai L-L, Wang X, Jiang T-C, Li P-F, Wang Y, Wu S-J, Jia L-Q, Liu M, An L, Cheng Z. 2020. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang Shelter Hospital in Wuhan, China. PLoS One 15:e0238416. doi: 10.1371/journal.pone.0238416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ueda M, Stickley A, Sueki H, Matsubayashi T. 2020. Mental health status of the general population in Japan during the COVID-19 pandemic. Psychiatry Clin Neurosci 74:505–506. doi: 10.1111/pcn.13105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newby JM, O’Moore K, Tang S, Christensen H, Faasse K. 2020. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS One 15:e0236562. doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vahedian-Azimi A, Moayed MS, Rahimibashar F, Shojaei S, Ashtari S, Pourhoseingholi MA. 2020. Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic. BMC Psychiatry 20:402. doi: 10.1186/s12888-020-02804-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. 2020. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One 15:e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang Y, Zhao N. 2020. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moghanibashi-Mansourieh A. 2020. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr 51:102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, Choo FN, Tran B, Ho R, Sharma VK, Ho C. 2020. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zolotov Y, Reznik A, Bender S, Isralowitz R. 2022. COVID-19 fear, mental health, and substance use among Israeli university students. Int J Ment Health Addict 20:230–236. doi: 10.1007/s11469-020-00351-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Islam MS, Sujan MSH, Tasnim R, Sikder MT, Potenza MN, van Os J. 2020. Psychological responses during the COVID-19 outbreak among university students in Bangladesh. PLoS One 15:e0245083. doi: 10.1371/journal.pone.0245083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al-Zaman MS. 2020. Healthcare crisis in Bangladesh during the COVID-19 pandemic. Am J Trop Med Hyg 103:1357–1359. doi: 10.4269/ajtmh.20-0826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zarocostas J. 2020. How to fight an infodemic. Lancet 395:676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahmud S, Mohsin M, Khan IA, Mian AU, Zaman MA. 2021. Knowledge, beliefs, attitudes and perceived risk about COVID-19 vaccine and determinants of COVID-19 vaccine acceptance in Bangladesh. PLoS One 16:e0257096. doi: 10.1371/journal.pone.0257096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Conti P, Ronconi G, Caraffa A, Gallenga C, Ross R, Frydas I, Kritas S. 2020. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by coronavirus-19 (COVID-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents 34:327–331. doi: 10.23812/CONTI-E. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article; further inquiries can be directed to the corresponding author.