Abstract
Background and aims
Vaccination is the most powerful public health intervention proven to be safe and effective in the battle against the coronavirus disease-2019 (COVID-19) pandemic. Despite the potential therapeutic benefits of primer vaccine dosage regimens, public perceptions of COVID-19 vaccine booster dose (VBD) acceptance and hesitancy vary among various sub-group populations. This study investigates COVID-19 vaccine booster dose acceptance and compares the multi-dimensional potential factors influencing VBD acceptance and hesitancy among university teachers and the student community in Bangladesh.
Methods
This web-based cross-sectional study employed an anonymous, validated, and self-administered questionnaire. The questionnaire items were adopted from a theoretical analysis of the recent relevant literature. The questionnaire was deployed in an on-line-enabled format (Google form) and conveniently distributed to 685 teachers and 990 students between 15th June, 2022 and 15th August, 2022 which resulted in the participation of 1250 (505 teachers vs.745 students) total respondents (response rate 73.72% vs. 75.25%) from various universities in Bangladesh. A non-parametric analytical tool (binary logistic regression) was applied to rationalize the study objectives and a Chi-squared test was performed to estimate the booster- hesitant risky group.
Results
The pooled COVID-19 vaccine booster dose acceptance rates were 84.6% (95% CI 81.5─87.7) and 67.2% (95% CI 63.8─70.6) for teachers and students in the university academic community, respectively. In employing a binary logistic regression, this study revealed that out of twelve (12)multi-dimensional key predictors, “equal safety”, “risk-benefit ratio”, and “variant control” had a significant positive association with VBD acceptance in both sets (p = 0.000, p = 0.000, and p = 0.005, respectively). Varied effects were found for several predictors; post-vaccination “side effects” had a significant negative association (p = 0.020) and “community protection” had significant positive association (p = 0.034) with vaccine booster dose acceptance in the teachers community while these variables were insignificant in the students cohort. “Trust” had a highly significant positive association (p = 0.000);“communication” and “academic attainment” had significant positive associations (p = 0.033 and 0.024, respectively) with VBD acceptance in the students cohort, while these predictors were insignificant in the teachers community. Women were more likely to receive a third dose of the vaccine (OR = 1.4 vs. 0.9 between teacher and student model); however, no significant association between gender and booster vaccine acceptance was found in a comparative Chi-squared model. Therefore, statistically, the booster vaccine-hesitant risky group was not found to implicate the massive booster vaccine drive among the university academic community.
Conclusions
COVID-19 booster vaccine acceptability among the student cohort was slightly lower than pre-roll-out intent. The teacher community was more inclined to get booster vaccinated. Moreover, differences were found between the multi-dimensional potential factors associated with VBD acceptance among teachers and students in university settings. This study explicitly confirmed positive attitudes toward the safety, health benefits, and variants control of the COVID-19 VBD under any circumstances. Post-vaccination side effect concern was found to be a barrier to administering booster shots and a reason for booster skepticism. Tailored communication and health education interventions need to be adopted to improve the public awareness of booster vaccine consequences, and limit booster skepticism.
Introduction
For three years, the world has battled against the coronavirus disease 2019 (COVID-19) pandemic to protect human lives and adopt new normal lifestyles. The transmission of viral chains can be minimized through adopting host immunity [1] either by massive community vaccination or immunity acquired from previous infections [2]. Several prediction models have been applied and found useful; however, the burden of causalities during the COVID-19 pandemic due to high morbidity and mortality across countries was entirely unpredictable. Hence, the perceived strategy of cost–benefit analysis for achieving acquired immunity via natural infection was not favorable in this instance [3]. Since the disclosure of multiple genomes sequencing of the novel coronavirus as of January 2021, the scientific community has incorporated over 100 potential candidates into the COVID-19 vaccine platform [4]. Worldwide, these vaccines were widely in use by the middle of 2021 and were proven as the best effective therapeutic intervention to prevent coronavirus contaminations, hospitalizations, and unusual deaths [5–7].
Despite all the fortified public health efforts to advance COVID-19 vaccines, recent reports are increasingly documenting a decline in humoral immunity after six months of vaccination with a second dose; it has been increasingly reported that exposure to a new coronavirus variant arrival resulted in the emergence of repeated infection [8,9]. COVID-19 vaccine effectiveness dropped from 74.7% to 53.1% after a few months of nursing home resident vaccination [10]. Due to declining herd immunity and the probable arrival of new coronavirus variants, the World Health Organization (WHO) and scientists around the world decided to promote booster vaccination shots against COVID-19. Recent research reported 11.3-fold and 19.5-fold raised body defense against infection and severe illness among people by administering a COVID-19 booster shot five months after completing the two primer doses [11]. Although booster shots will at some point play a key role in the public health response by preventing infection, hesitancy to receive a booster shot emerged as a vaccination barrier among significant portions of South Asian people [12]. Previous research reported thatCOVID-19 primer vaccine acceptance has declined due to people’s doubtful attitudes toward receiving the vaccine. While the search for coronavirus vaccines was underway, these suspicious outlooks preventing vaccine acceptance were the major barrier to vaccine roll-out and were collectively known as vaccine hesitancy [13,14]. Concerns regarding vaccination hesitancy have intensified as a result of the COVID-19 epidemic. Consequently, it is imperative to decrease COVID-19 vaccine reluctance, which depends on comprehensive insight into its determinants, to mitigate the pandemic. In the current context, the acceptance of primer vaccinations has been shown to differ considerably among various sub-group populations with substantial regional variability [15]. Thus, the rapid roll-out of the third COVID-19 vaccine dose likely faces the same challenges, and low booster dose uptake would be a major hurdle to curbing new corona virus variant arrival globally.
The dynamic relationship between intention and final decision with respect to the COVID-19 booster is beginning to be evaluated in university settings [16–19] and other sub-group populations worldwide [20–26]. As of December 28, 2021, Bangladesh has begun to administer booster doses of the COVID-19 vaccine [27] in the wake of breakthrough infections, the arrival of new variants, and a decline in long-standing protection. Initially, health policy makers decided to boost front-liners and the elderly as a priority group for immunization through VBD. Among different sub-population groups, students are certainly vulnerable to coronavirus exposure due to their active lifestyles, reading in crowded settings, and a perception of disease invulnerability [28]. Moreover, the teacher community plays a significant role in educational attainment, particularly those teachers in boarding facilities. Recent studies have documented the substantial influence of teachers on student attitudes and behavior [29] and dynamic vaccine behaviors existing in a college setting [30]. Several observational studies conducted in Bangladesh to date have focused on COVID-19 vaccination events among diverse sub-group populations [31–38], including university students [39–43]. However; public readiness to accept the COVID-19 vaccine booster dose has rarely been studied in Bangladesh. Hence, we conducted a web-based cross-sectional comparative study focused on COVID-19VBDacceptance among two major and inter-related population sub-groups in Bangladesh. This study thus aimed to investigate COVID-19 VBD acceptance and compare the potential factors influencing VBD acceptance and hesitancy among university teachers and the student community in Bangladesh.
Materials and methods
We have deposited step-by-step descriptions of the study protocols on protocols.io (DOI: doi.org/10.17504/protocols.io.5jyl8jeq6g2w/v1) to enhance the reproducibility of study results.
Study design
This cross-sectional comparative study used a self-administered, anonymous, and validated multi-item questionnaire to rationalize the study’s outlined objectives. The questionnaire was deployed online using an online survey tool (Google forms) and conveniently sent to teachers and students in different public and private universities between 15thJune, 2022 and 15thAugust, 2022 using electronic collection methods (social media platform and emails) and following the STROBE guideline.
At the beginning of the questionnaire, the investigators incorporated a separate paragraph describing the study and terms of consent for participating. Hence, completion of the survey by a participant was considered indirect written consent. Permission to conduct this cross-sectional comparative study has been obtained from the “Ethical Review Committee” (ERC), Faculty of Biological Science and Technology, Jashore University of Science and Technology in Bangladesh. The detail research protocol was reviewed and evaluated by the ERC before the study began. Data were collected and analyzed anonymously, while no clinical intervention was applied to the subjects. Hence, the Ethical Review Committee of the university approved the study as exempt. There was no external funding.
Setting and participants
Teachers and students of government-sponsored (public) and non-government-sponsored (private) university settings in Bangladesh were the participants of this comparative analysis. No financial or in-kind reward was offered to participants who completed the survey. According to the latest census, 51 public and 108 private universities are approved by the University Grants Commission (UGC) in Bangladesh.
Participant’s inclusion criteria
The eligibility criteria for the participants were as follows: (i) understand and agree to the study objectives and provide anonymous data on COVID-19 booster vaccination, (ii) public and/or private university teachers in Bangladesh, and (iii) students currently studying in a Bangladeshi public or private university. This study did not harm participants, and participants were free to reject participation at any time of the study period.
Measures and survey instrument development
The theoretical concept of COVID-19 vaccine acceptance and hesitancy was conceptualized using recent systematic reviews conducted on the topic [15,44]. The questionnaire key items were adopted from a theoretical analysis of recent studies focusing onCOVID-19 booster consequences across countries[16–26]. Moreover, in-field expert consultation was conducted in formulating the primary questionnaire items. The questionnaire was constructed in the English language, highlighted multi-dimensional aspects of COVID-19 booster vaccination consequences, and was designed to take approximately 15 minutes to complete. Each item in the preliminary questionnaire was content- and face-validated by a panel of public health experts, which ensured the relevance and clarity of the questionnaire. Pilot testing (n = 10+10) was undertaken among the targeted population before administering the ultimate version of the questionnaire to validate the legitimacy and relevance of the instrument. The outcomes of the piloted research design were not taken into account for the final analysis.
The survey instrument assessed (1) socio-demographic characteristics of the respondents; (2) intention to uptake COVID-19 VBD; and (3) key factors influencing COVID-19 VBD acceptance and hesitancy. A non-parametric data analytical tool (binary logistic regression) was employed to analyze the association mode between predictor variables and the outcome variable with a 95% confidence interval (CI).
Survey administration
The convenience sampling technique was used for systematic data gathering from online survey tools. This process created a survey with the goal of collecting maximum insights from teacher and student samples for the purpose of developing quantitative variables of the attributes. Commencing with a basic description of the study goal and vision, the questionnaire also emphasized that enrollment was purely optional. Identities, birth dates, and personal information were not collected for the survey. Prior to completing the questionnaire form, all participants provided their informed authorization describing the study terms and objectives to participate willingly. Data integrity was maintained by ensuring anonymity throughout the study period and by requesting accurate responses and choices from participants. The online questionnaire was distributed among teachers and students in various universities, who were all, encouraged to participate; thus, a potential source of non-response bias was minimized.
Study variables
For the response variable of the study, we measured COVID-19 VBD acceptance as a binary variable (1 = Yes, 0 = No). Socio-demographic profiles of the respondents were also captured and expressed in suitable scale. In analyzing the data in the binary regression model, we investigated the impact of several socio-psychological and vaccine-related independent variables on the outcome response variable (VBD acceptance) dichotomized into 1 = Yes and 0 = No.
Study size
The following SurveyMonkey formula was used to calculate the least required sample size with a confidence interval of 95% (z score of 1.96) and a 5% margin of error.
Where N = population size, p = sample probability, e = margin of error (percentage in decimal form), z = z-score.
In general, the least required 500 data are recommended to conduct binominal regression analysis in observation studies with large sample size that characterize the parameters. Another formula is n = 100+50i where i stand for number of independent variables included into the analysis [45–47].We pre-tested data samples (n = 10+10) as a pilot test to examine the instrument’s clarity and to understand the average time spanned need for completing the survey.
Equations for binominal regression
Binominal regression equations are followings:
| (1) |
where y is the linear combination function.
| (2) |
here, P represented the probability of vaccine uptake intent and x indicated the vector of independent variable. If function of y is characterized as
| (3) |
Usually Eqs (2) and (3) is expressed and written as logit (P) or the log odd ratio as follows-
| (4) |
where logit(P) means log odd ratio.
Statistical methods
Descriptive statistics utilized weighted frequencies and percentages of the variables to analyze socio-demographic profiles and categorical variables. A non-parametric data analytical tool called binary logistic regression was employed to explore the pattern of association between explanatory variables and the response variable. All the key assumptions related to binary regression analysis were examined to adjust the model suitability. Assumptions of binary logistic analysis were tested. Raw data were inserted into Microsoft Excel version 10 and imported to Statistical Package for the Social Science (SPSS) software. IBM-SPSS version 25 (RRID: SCR_016479) was used for analyzing the data. In this study analysis, p<0.05 was considered statistically significant. The online survey denied the acceptance of incomplete survey responses; thus, no missing data were analyzed.
Results
Respondent’s characteristics
Table 1 displays comparative socio-demographic characteristics among teachers and students. We checked the eligibility criteria and confirmed participant inclusion accordingly through online survey restrictions. A lack of digital devices and limited internet access could be reasons for study non-participation. In total, 505 teachers and 745 students from various universities in Bangladesh were included for final analysis. Most of the teachers were 31–35 years or36-40 years in age range (20.8% and 20.5%, respectively), and 59.5% of students were youth-aged ranging from 21 to 25 years. Although the majorities (63.6%) of teachers were public university faculty, a significant portion 44.7% of students studied in private universities. However, Dhaka division had the highest count of both teachers and students (28.4% vs. 28.5%). Most teachers had completed two doses of vaccines, while this rate was slightly lower for students (91.5% vs. 61%). Appropriately, 29.6% female teachers and 48% female students participated from various universities. Most participants were Muslim by religion (79.4% vs.72.6%), while histories of COVID-19 positive results were (16.2% vs. 22.5%).
Table 1. Overview of socio-demographic profile of study participants (N = 505 vs.745).
| Variables | Teachers | Students | ||
|---|---|---|---|---|
| N | % | N | % | |
| Age distribution | ||||
| 16–20Years | 0 | 0 | 212 | 28.5 |
| 21–25Years | 0 | 0 | 443 | 59.5 |
| 26–30Years | 52 | 10.3 | 82 | 11.0 |
| 31–35 Years | 105 | 20.8 | 8 | 1.0 |
| 36–40 Years | 103 | 20.5 | 0 | 0 |
| 41–45 Years | 91 | 18.0 | 0 | 0 |
| 46–50 Years | 79 | 15.6 | 0 | 0 |
| 51–55 Years | 52 | 10.3 | 0 | 0 |
| 56–60 Years | 17 | 3.4 | 0 | 0 |
| 61–65 Years | 6 | 1.1 | 0 | 0 |
| University type | ||||
| Publicly funded | 321 | 63.6 | 412 | 55.3 |
| Privately funded | 184 | 36.4 | 333 | 44.7 |
| Others | 0 | 0 | 0 | 0 |
| Geographical distribution | ||||
| Dhaka | 151 | 28.4 | 212 | 28.5 |
| Rajshahi | 70 | 26.7 | 95 | 12.7 |
| Khulna | 94 | 21.3 | 121 | 16.3 |
| Chattogram | 49 | 5.7 | 82 | 11.0 |
| Mymensingh | 34 | 5.0 | 76 | 10.2 |
| Rangpur | 32 | 9.5 | 57 | 7.7 |
| Sylhet | 41 | 2.0 | 61 | 8.1 |
| Barishal | 34 | 1.3 | 41 | 5.5 |
| Gender | ||||
| Male | 356 | 70.5 | 387 | 52.0 |
| Female | 149 | 29.5 | 358 | 48.0 |
| Religion | ||||
| Muslim | 401 | 79.4 | 541 | 72.6 |
| Hindu | 99 | 19.6 | 182 | 24.4 |
| Others | 5 | 1.0 | 22 | 3.0 |
| Vaccination status | ||||
| Completed two doses | 462 | 91.5 | 455 | 61.1 |
| Received 1st dose | 36 | 7.1 | 209 | 28.1 |
| Not vaccinated yet | 7 | 1.4 | 81 | 10.8 |
| History of COVID-19 | ||||
| Corona infected previously | 82 | 16.2 | 188 | 22.5 |
| Booster dose acceptance | ||||
| Booster shot hesitancy | 78 | 15.4 | 244 | 32.8 |
| Intent to receive booster | 427 | 84.6 | 501 | 67.2 |
Results of descriptive statistics
Table 2 describes the descriptive results of the predictor variables and outcome variable in the study. The outcome event in this analysis was reported as‘COVID-19 vaccine booster dose acceptance’. The pooled COVID-19 VBD acceptance rate was 84.6%, 95% CI 81.5─87.7 in the teacher community and 67.2%, 95% CI 63.8─70.6 in the student cohort. The online survey barred acceptance of any incomplete survey instruments, so missing data were not produced by each variable of interest.
Table 2. Descriptive results of the variables.
| Variables | Teachers | Students | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| I Intend to accept COVID-19 booster dose anytime (Yes = 1, otherwise = 0) | 0.86 | 0.326 | 0.86 | 0.328 |
| Booster doses are similarly safe as were previous doses of COVID-19 vaccines (Yes = 1, otherwise = 0) | 0.78 | 0.404 | 0.82 | 0.398 |
| Booster doses will produce severe side effects (Yes = 1, otherwise = 0) | 0.56 | 0.498 | 0.59 | 0.498 |
| Booster shot has long effectiveness to protect COVID-19 (Yes = 1, otherwise = 0) | 0.92 | 0.314 | 0.86 | 0.328 |
| Effective communication on booster vaccine dose is necessary (Yes = 1, otherwise = 0) | 0.78 | 0.432 | 0.81 | 0.420 |
| Booster doses provide repeated protection against COVID-19 (Yes = 1, otherwise = 0) | 0.52 | 0.496 | 0.64 | 0.488 |
| The therapeutic benefit of booster doses overweigh the risk (Yes = 1, otherwise = 0) | 0.59 | 0.486 | 0.66 | 0.471 |
| I receive the vaccine’s booster dose on priority bases to protect the community people from COVID-19 infection (Yes = 1, otherwise = 0) | 0.45 | 0.421 | 0.46 | 0.425 |
| I trust that booster doses provides long-term herd immunity (Yes = 1, otherwise = 0) | 0.90 | 0.303 | 0.87 | 0.338 |
| Booster doses are required to control the arrival new coronavirus variants (Yes = 1, otherwise = 0) | 0.68 | 0.474 | 0.64 | 0.487 |
| I will receive booster to participate face-to face class at my university (Yes = 1, otherwise = 0) | 0.90 | 0.492 | 0.60 | 0.396 |
| I have adequate information about COVID-19 booster vaccine doses (Yes = 1, otherwise = 0) | 0.79 | 0.421 | 0.79 | 0.406 |
| Vaccination programs at regional, national, and global level encourage me to receive booster doses (Yes = 1, otherwise = 0) | 0.74 | 0.414 | 0.78 | 0.438 |
Model summary
Table 3 provides a model summary for both participant groups. The joint impact of all the predictor variables on the dependent variable was determined by using a Nagelkerke R squared test that explained the model summary.
Table 3. Comparative model summary.
| Model Summary | |||||
|---|---|---|---|---|---|
| -2 Log likelihood | Cox & Snell R square | Nagelkerke R square | |||
| Teachers | Students | Teachers | Students | Teachers | Students |
| 240.619a | 296.087a | 0.389 | 0.407 | 0.584 | 0.613 |
In Table 3, the result of a Cox–Snell R squared test indicates that the outcome variables (VBD acceptance) are given as (38.9%─58.4%) vs. (40.7%─61.3%) by the explanatory variables used in the teacher and student models, respectively, which are assumed to be good levels.
Goodness-of-model fit
The goodness-of-model fit of the model is explained by omnibus tests of model co-efficient and a Hosmer-Lemeshow test in Table 4. We evaluated the assumptions, and the result showed that the significance level (p-value) for the omnibus tests of model coefficients is significant (p<0.05), while it was insignificant (p>0.05) in Hosmer-Lemeshow tests for both studied models. These results indicate very good fitness of the study samples for the binary logistic regression.
Table 4. Omnibus tests of model coefficients and Hosmer-Lemeshow test.
| Omnibus tests of model coefficients | |||||||
| Chi-square | Significance level | ||||||
| Teachers | Students | Teachers | Students | ||||
| Step | 102.408 | 153.233 | 0.000 | 0.000 | |||
| Block | 102.408 | 153.233 | 0.000 | 0.000 | |||
| Model | 102.408 | 153.233 | 0.000 | 0.000 | |||
| Hosmer-Lemeshow test | |||||||
| Chi-square | Significance level | ||||||
| Teachers | Students | Teachers | Students | ||||
| 8.254 | 10.658 | 0.784 | 0.438 | ||||
Binary logistic regression analysis
Table 5 represents the comparative results of regression analysis. According to the regression models, out of twelve multi-dimensional predictors, “equal safety profile”, “risk–benefit ratio”, and “variant control” had a significant positive association with VBD acceptance in both sets (p = 0.000, p = 0.000, and p = 0.005, respectively). Varied effects were found for several predictors; post-vaccination “side effects” had a significant negative association and “community protection” had a significant positive association (p = 0.020 and p = 0.034, respectively) with vaccine booster dose acceptance in the teacher community, while these variables were insignificant in the student cohort. However, “trust” had a highly significant (p = 0.000) positive association and “communication” and “academic attainment” had a significant positive association (p = 0.033 and 0.024, respectively) with VBD acceptance in the student cohort, while these predictors were insignificant in the teacher community.
Table 5. Results of binary logistic regression analysis.
| Teachers community | |||||
|---|---|---|---|---|---|
| Variable | B | S.E. | Wald | Sig. | Exp(B) |
| Constant | 2.081 | 0.619 | 3.338 | 0.047 | 0.439 |
| Equal safety | 1.671** | 0.421 | 15.769 | 0.000 | 5.317 |
| Side effect | -0.424* | 0.520 | 1.799 | 0.020 | 1.711 |
| Effectiveness | 1.966 | 0.456 | 18.578 | 0.497 | 7.142 |
| Communication | 0.248 | 0.434 | 0.327 | 0.567 | 0.780 |
| Repeated immunity | 0.393 | 0.406 | 0.936 | 0.051 | 1.481 |
| Risk-benefit ratio | 0.265** | 0.390 | 0.462 | 0.000 | 1.303 |
| Community protection | 1.092* | 0.484 | 5.086 | 0.034 | 0.336 |
| Trust | 0.112 | 0.508 | 0.048 | 0.826 | 1.118 |
| Variant control | 0.214* | 0.307 | 0.876 | 0.039 | 2.346 |
| Academic attainment | -0.766 | 0.357 | 4.598 | 0.032 | 2.152 |
| Information | -0.298 | 0.421 | 0.501 | 0.479 | 0.742 |
| Vaccine justice | 0.568 | 0.421 | 0.956 | 0.785 | 1.121 |
| Students cohort | |||||
| Variable | B | S.E. | Wald | Sig. | Exp(B) |
| Constant | 2.819 | 0.585 | 10.077 | 0.024 | 0.262 |
| Equal safety | 1.297** | 0.364 | 12.723 | 0.000 | 3.659 |
| Side effect | 0.328 | 0.333 | 0.968 | 0.080 | 1.388 |
| Effectiveness | 1.108 | 0.391 | 8.027 | 0.065 | 3.030 |
| Communication | 0.987* | 0.331 | 8.886 | 0.033 | 2.684 |
| Repeated immunity | 0.613 | 0.322 | 3.615 | 0.057 | 1.845 |
| Risk-benefit ratio | 0.218** | 0.321 | 0.463 | 0.000 | 0.804 |
| Community protection | 1.509 | 0.498 | 9.194 | 0.982 | 4.523 |
| Trust | 1.021** | 0.320 | 2.147 | 0.000 | 2.833 |
| Variant control | 0.140* | 0.331 | 0.180 | 0.031 | 1.151 |
| Academic attainment | 2.045* | 0.657 | 5.561 | 0.024 | 1.021 |
| Information | -0.059 | 0.348 | 0.028 | 0.866 | 0.943 |
| Vaccine justice | 0.678 | 0.576 | 4.414 | 0.954 | 0.768 |
note:** = significant at <0.01 and ** = significant at <0.05.
Pearson’s Chi-squared test results
The following Table 6 represents the results of a Pearson’s Chi-squared test and odds ratio for VBD risky group estimation. The odds for accepting COVID-19 VBD were (1.5 vs. 0.9) between the models; however, Chi-squared test results revealed an insignificant (p>0.05) association between booster acceptance and gender. Hence, statistically, no group (female/male) was found to be a booster-hesitant risky group affecting country-wide booster vaccination implementation in near-real-time.
Table 6. Pearson’s Chi-squared test results in a comparative model.
| Teachers community | |||||||||||
| Chi-square tests | |||||||||||
| Value | Asymptotic significance (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | ||||||||
| Pearson chi-square | 2.406a | 0.121 | |||||||||
| Continuity correctionb | 1.981 | 0.159 | |||||||||
| Likelihood ratio | 2.411 | 0.121 | |||||||||
| Fisher’s exact test | 0.150 | 0.080 | |||||||||
| Linear-by-linear association | 2.401 | 0.121 | |||||||||
| N of valid cases | 505 | ||||||||||
|
Risk estimate |
Value | 95% Confidence Interval | |||||||||
| Lower | Upper | ||||||||||
| Odds ratio for gender: (Female / Male) | 1.466 | 0.886 | 2.770 | ||||||||
| For cohort I intend to accept vaccination anytime = No | 1.385 | 0.897 | 2.457 | ||||||||
| For cohort I intend to accept vaccination anytime = Yes | .848 | 0.886 | 1.015 | ||||||||
| N of valid cases | 505 | ||||||||||
| Students cohort | |||||||||||
| Chi-squared tests | |||||||||||
| Value | Asymptotic significance (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | ||||||||
| Pearson chi-square | 0.071a | 0.790 | |||||||||
| Continuity correctionb | 0.019 | 0.889 | |||||||||
| Likelihood ratio | 0.071 | 0.790 | |||||||||
| Fisher’s exact test | 0.801 | 0.444 | |||||||||
| Linear-by-linear association | 0.071 | 0.790 | |||||||||
| N of valid cases | 745 | ||||||||||
|
Risk estimate |
Value | 95% Confidence Interval | |||||||||
| Lower | Upper | ||||||||||
| Odds ratio for gender: (Female / Male) | 0.935 | 0.569 | 1.537 | ||||||||
| For cohort I intend to accept vaccination anytime = No | 0.943 | 0.610 | 1.457 | ||||||||
| For cohort I intend to accept vaccination anytime = Yes | 1.008 | 0.948 | 1.073 | ||||||||
| N of valid cases | 745 | ||||||||||
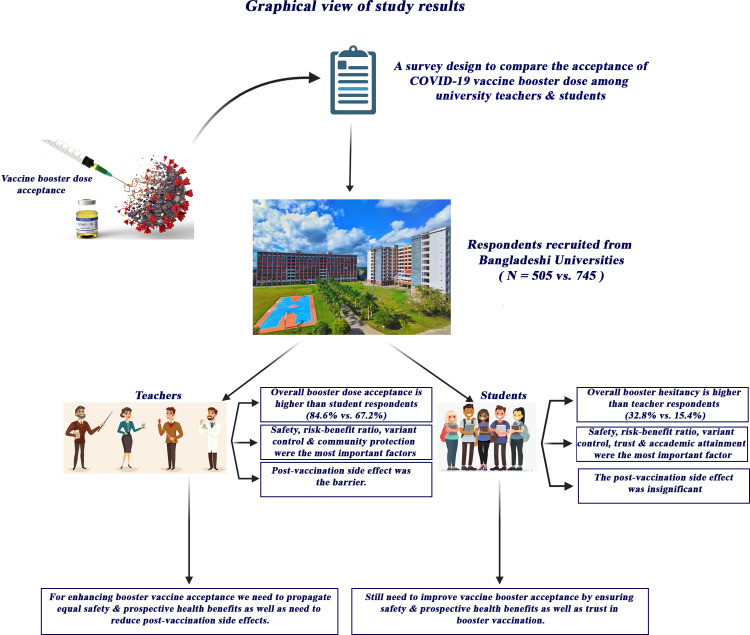
“Fig 1” displays a comparative graphical view of the potential factors influencing COVID-19 vaccine booster acceptance among university academic community in Bangladesh.
Fig 1. Graphical overview of the study outcomes.
Discussion
One of the most powerful scientific interventions proven to limit several contagious infections and aid in the eradication of diseases is vaccination. The present investigation seeks to assess COVID-19 vaccine booster acceptance and compares multi-dimensional potential factors associated with booster acceptance and hesitancy among teachers and students in university settings. According to our results, the pooled booster vaccine acceptance rate was 84.6% vs. 67.2% for teachers and students, respectively. Appropriately, teachers are more likely to get booster vaccinated against COVID-19 infection. Despite general compliance with the common predictors, we found several differences in the factors associated with VBD acceptance and hesitancy. Equal safety, risk-benefit ratio, and variant control were common factors for VBD acceptance in both groups. Community protection and post-vaccination side effects concern were identified factors among the teacher’s community, while trust, communication, and academic attainment were identified among student cohorts.
Comparable challenges regarding misconceptions and beliefs about the acceptability of the COVID-19 booster vaccine for both adolescents and grownups were observed in the general community. Thus, determining the severity of this challenge and strategizing to lessen booster dose reluctance and get the university community immunized against the coronavirus is imperative. A study conducted on COVID-19 VBD acceptability amongst various sub-group populations reported that in Germany, 87.8% of university students and staff were willing to receive the VBD [16]. Similarly, 71% of adult Poles in Poland [48]; 74.5% of students and health professionals in Poland [17]; 75.3% and 72.7% of the university community in Italy and Belgium, respectively [18,19]; 62% of adult Americans [21]; and 71.3% of healthcare workers in the Czech Republic [49] have declared their willingness to accept the COVID-19 VBD. These results are consistent with our findings. However, low vaccine uptake intention or vaccine apprehension is a complex heterogeneous occurrence that has steadily increased in more than 90% of countries since 2014 [50]. Public acceptance and hesitance towards COVID-19 vaccine has been well-documented for a regularly scheduled dose regimen [15,51,52] as well as for COVID-19 VBD receptivity [22,53,54].
Numerous multi-dimensional psychological concerns have contributed to altered vaccine uptake decisions and determine actual vaccination behavior. The analysis of Roy et al. reported that the most common predictors of vaccine acceptance are safety and efficacy, in other words, trust in the vaccine, but also, at least in Asia, the influence of information, and side effects was significant [15]. Perceived vaccine safety and post-vaccination side effects concern have gradually become the most prominent predictors of primer dose COVID-19 vaccine behavior [51,55–57] as well as booster shot behavior [16,17,49,53].This study also observed that equal safety, risk–benefit ratio, and variant control had a positive association with VBD acceptance in both groups. The outcomes of our research also highlighted post-vaccination side effects as a significant predictor of COVID-19 VBD acceptance among teachers, while this was insignificant in the student set. Although no severe adverse effects were encountered [58,59], moderate side effects were reported during the administration of COVID-19 vaccines for elderly individuals and individuals with a co-morbid diagnosis. University students are youth-aged; adopt active lifestyles, and have faith in disease invulnerability, so the side effects factor is insignificant for this group. Both groups acknowledged that the perceived benefits of the booster dose outweigh the risks and that the booster shot is essential for controlling new variant arrival. However, in this regard, students argued that primer doses are sufficient to provide long-term protection. A recent study deduced that vaccine safety profile, variant control, and risk–benefit ratio were the principal predictive factors regarding VBD acceptance among the university community [17] and general population [22]. In our study, community protection was a significant predictor of VBD acceptance among the teachers, while academic attainment was significant among students. Since teachers are senior citizens, they hold roles of accountability for social and community care over students; hence, community protection has been recognized as an important concern among teachers. Adequate health protection for family members, the community, and patients have been identified as altruistic promoters of VBD acceptance [16]. Moreover, institutional or academic recommendation to uptake the third dose of the vaccine to attain face-to-face classes encourages student booster dose acceptance.
The findings of the present survey demonstrated that trust was an important predictor of booster dose decision among the student cohort. Trust was one of the key determinants of vaccine optimization because confidence regarding vaccine safety, side effects, and efficacy were critically influenced by the level of trust regarding vaccination [60–62]. Tailored and credible health communication has influenced positive health behaviors, guided decision-making, addressed concerns, and built trust in mass vaccination programs [63]. Communication provided by healthcare professionals and government spokes people has been crucial to building public trust for rapid vaccination turn-outs [64]. Higher levels of institutional trust are significantly associated with a greater willingness to uptake two primer vaccine doses [65] and a third booster dose [66]. A growing body of research has noted that receiving two doses provides only limited and short-lived protection against coronavirus infection with the arrival of new variants such as the omicron variant [67]. A study from Saudi Arabia in the first week of omicron spread showed that two-thirds of healthcare workers (HCWs) felt that vaccination was the best option to prevent further spread of the new omicron variant [68]. However, the utility of prospective vaccines to control new coronavirus variants depends on their public acceptance [69]. COVID-19 vaccine acceptance has varied substantially among students in different geographical locations, and numerous multi-dimensional factors are associated with students’ COVID-19 vaccine hesitancy [70]. We have included a large data sample to provide external validity of this study’s results. Substantial variations in respondents’ socio-demographic profiles and a large sample size provided much strength with which to predict the generalizability of the study findings toensureCOVID-19 VBD confidence and receptivity among the general population.
Implications
This comparative study has some practical implications for policy support, practices, and future research. This study largely benefits health policy makers, health stakeholders, and vaccine promoters in developing evidence-based booster dose promotional planning. Potential factors underlying booster vaccine acceptance and hesitancy would be functional in designing rigorous health interventions involving key messages delivered by community leaders and vaccine policy makers [71]. This study’s findings therefore provide support in overcoming barriers and propagating facilitators while enhancing teacher and student health engagement in a nationwide booster vaccine roll-out; thus, they may help governments to design a booster dose protocol accordingly. In terms of research, this study may act as scientific evidence for initiating further observational studies of COVID-19 vaccine booster acceptance by examining the association between vaccine hesitancy and other confounding variables. Since the pattern of COVID-19 vaccine reluctance can change over time [72], this study assists in the design of a long-term surveillance study for tracking the temporal changes in factors associated with COVID-19 vaccine booster decisions.
Strengths and limitations
This is the first study focusing onCOVID-19 booster vaccine acceptance, and it applies a new analytical approach to exploring the key determinants of booster vaccine acceptance and hesitancy among two important sub-group populations in university settings. The first strength of our study lies in the fact that its data encompassed people in age groups between 16 and 65 years old; another strength is that a thorough analysis was conducted. Health benefits apparently led participants to uptake VBD over the perceived risk; thus, prospective community benefits outweighing perceived risk have been established in receiving VBD. The significance of community protection over a perception of disease invulnerability was clearly demonstrated to accelerate booster vaccination acceptance. The identification of vaccination trust and academic attainment as a positive predictor for receiving a booster shot adds new value to the existing field of research. The electronic recruitment of participants and the online survey mode provide a rapid strategy with which to obtain a meaningful estimate of effect size and associated variability, which helps researchers to receive a large data sample quickly [73].
The following aspects may have contributed to specific research limitations. Firstly, since this survey was cross-sectional, the causal relationship between the investigated variables could not be validated. The results may be overestimated or underestimated based on self-reported feedback. Secondly, according to the sample size selection criteria, the sample size of our study was inadequate in comparison with the total population size. The electronic data collection mode created the possibility of a non-response bias for those who did not participate in this survey because the digital data collection procedure often fails to capture the depth of information which could have otherwise been possible using an in-person approach. Thirdly, human behavior is transformative and may be altered by changes to the perceived health risk, vaccine characteristics, and vaccine deployment. Fourthly, the sequential alteration of factors associated withCOVID-19 vaccine booster acceptance could still take place, and some additional confounding factors may lead to booster hesitancy that were not defined in this study. These limitations must be addressed in future studies on the topic. Finally, the perceptions to the new omicron and bivalent vaccines were not included in this study.
Conclusions
The COVID-19immunization actions of the university academic community were evaluated when health policy makers launched a COVID-19vaccine into vaccination programs throughout the country. This study provided insight into the multi-dimensional determinants of booster acceptance among two academically influential groups in universities. Understanding opinions on COVID-19 booster vaccine acceptance and supporting the academic community’s booster vaccine readiness are thus critical for implementing large-scale booster vaccinations. Intention to receive the COVID-19 booster vaccine was slightly lower among students than teachers. This study deduced that several multi-dimensional potential factors were associated with VBD acceptance decisions, and differences were found between teachers and students regarding the potential factors of VBD acceptance. This study confirms the importance of a positive attitude toward the vaccine’s safety profile as were previous doses of COVID-19 vaccines, prospective health benefits, variant control, community protection, trust, health communication, and academic attainment for receiving a booster shot, while post-vaccination side effects concern was a barrier and primary reason for booster dose skepticism. Tailored communication and multi-disciplinary educational intervention must be adopted to improve public adherence and knowledge about booster vaccine consequences and limit booster skepticism.
Acknowledgments
Authors are greatly acknowledging to all surveyors contributed data collections from various universities in Bangladesh.
Reporting guidelines
Figshare: STROBE Checklist for:“Multi-dimensional potential factors influencing COVID-19 vaccine booster acceptance and hesitancy among university academic community in Bangladesh: a cross-sectional comparative study” DOI: 10.6084/m9.figshare.21896463.
No copy edited materials are contained in the Figure (Fig 1).
Abbreviations
- COVID-19
Coronavirus disease-2019
- VBD
Vaccine Booster Dose
- WHO
World Health Organization
- UGC
University Grants Commission
- SPSS
Statistical Package of Social Science
- LMICs
Low and middle-income countries
Data Availability
Publicly available at: Figshare: “Minimal Data Set-csv.” DOI: 10.6084/m9.figshare.21896451;"
Funding Statement
This research did not receive any specific support from funding agencies in the public, commercial, or not-for-profit sector.
References
- 1.Raina SK, Kumar R. Herd immunity in COVID-19: Needs de-emphasizing. Journal of Family Medicine and Primary Care. 2022. May 1;11(5):1595–7. doi: 10.4103/jfmpc.jfmpc_1852_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kadkhoda K. Herd immunity to COVID-19: alluring and elusive. Am J Clin Pathol. (2021) 155:471–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park M, Jit M, Wu JT. Cost-benefit analysis of vaccination: a comparative analysis of eight approaches for valuing changes to mortality and morbidity risks. BMC medicine. 2018. Dec;16(1):1–1. doi: 10.1186/s12916-018-1130-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson RM, Vegvari C, Truscott J, Collyer BS. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020;396(10263):1614–6. doi: 10.1016/S0140-6736(20)32318-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Korang S.K.; von Rohden E.; Veroniki A.A.; Ong G.; Ngalamika O.; Siddiqui F.; et al. Vaccines to prevent COVID-19: A living systematic review with Trial Sequential Analysis and network meta-analysis of randomized clinical trials. PLoS ONE 2022, 17, e0260733. doi: 10.1371/journal.pone.0260733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dagan N.; Barda N.; Kepten E.; Miron O.; Perchik S.; Katz M.A.; et al. BNT162b2 MRNA COVID-19 Vaccine in a Nationwide Mass Vaccination Setting. N. Engl. J. Med. 2021, 384, 1412–1423. doi: 10.1056/NEJMoa2101765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ndwandwe D.;Wiysonge C.S. COVID-19 vaccines. Curr. Opin. Immunol. 2021, 71, 111–116. doi: 10.1016/j.coi.2021.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lange B.; Gerigk M.; Tenenbaum T. Breakthrough Infections in BNT162b2-Vaccinated Health CareWorkers. N. Engl. J. Med.2021, 385, 1145–1146. doi: 10.1056/NEJMc2108076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levin EG, Lustig Y, Cohen C, Fluss R, Indenbaum V, Amit S, et al. Waning immune humoral response to BNT162b2 COVID-19 vaccine over 6 months. NEngl J Med. (2021) 385:e84. doi: 10.1056/NEJMoa2114583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nanduri, S.; Pilishvili, T.; Derado, G.; Soe, M.M.; Dollard, P.; Wu, H.; et al. Effectiveness of Pfizer-BioNTech and Moderna Vaccines in Preventing SARS-CoV-2 Infection Among Nursing Home Residents Before and During Widespread Circulation of the SARS-CoV-2 B.1.617.2 (Delta) Variant—National Healthcare Safety Network, 1 March–1 August 2021. MMWR Morb. Mort. Week. Rep. 2021, 70, 1163. [DOI] [PMC free article] [PubMed]
- 11.Bar-On Y.M.; Goldberg Y.; Mandel M.; Bodenheimer O.; Freedman L.; Kalkstein N.; et al. Protection of BNT162b2 Vaccine Booster against COVID-19 in Israel. NEJM N. Engl. J. Med. 2021, 385, 1393–1400. doi: 10.1056/NEJMoa2114255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lal PM, Shaikh OA, Vohra LI, Arif A, Ochani S, Ullah K. Increased burden of booster shots for COVID-19 amidst vaccine hesitancy in Pakistan. Annals of Medicine and Surgery. 2022. Sep 1;81:104360. doi: 10.1016/j.amsu.2022.104360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public health. 2021. May 1;194:245–51. doi: 10.1016/j.puhe.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: A longitudinal study. PloS one. 2021. Apr 16;16(4):e0250123. doi: 10.1371/journal.pone.0250123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roy DN, Biswas M, Islam E, Azam MS. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: A systematic review. PloS one. 2022. Mar 23;17(3):e0265496. doi: 10.1371/journal.pone.0265496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Attia S, Mausbach K, Klugar M, Howaldt HP, Riad A. Prevalence and Drivers of COVID-19 Vaccine Booster Hesitancy Among German University Students and Employees. Frontiers in public health. 2022;10. doi: 10.3389/fpubh.2022.846861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dziedzic A, Issa J, Hussain S, Tanasiewicz M, Wojtyczka R, Kubina R, et al. COVID-19 vaccine booster hesitancy (VBH) of healthcare professionals and students in Poland: Cross-sectional survey-based study. Frontiers in Public Health. 2022. Jul 25;10:938067. doi: 10.3389/fpubh.2022.938067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Folcarelli L, Miraglia del Giudice G, Corea F, Angelillo IF. Intention to receive the COVID-19 vaccine booster dose in a university community in Italy. Vaccines. 2022. Jan 19;10(2):146. doi: 10.3390/vaccines10020146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paridans M, Monseur J, Donneau AF, Gillain N, Husson E, Leclercq D, et al. The Dynamic Relationship between the Intention and Final Decision for the COVID-19 Booster: A Study among Students and Staff at the University of Liège, Belgium. Vaccines. 2022. Sep 6;10(9):1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdelmoneim SA, Sallam M, Hafez DM, Elrewany E, Mousli HM, Hammad EM, et al. COVID-19 vaccine booster dose acceptance: Systematic review and meta-analysis. Tropical Medicine and Infectious Disease. 2022. Oct 13;7(10):298. doi: 10.3390/tropicalmed7100298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yadete T, Batra K, Netski DM, Antonio S, Patros MJ, Bester JC. Assessing acceptability of COVID-19 vaccine booster dose among adult Americans: A cross-sectional study. Vaccines. 2021. Dec 2;9(12):1424. doi: 10.3390/vaccines9121424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lounis M, Bencherit D, Rais MA, Riad A. COVID-19 Vaccine Booster Hesitancy (VBH) and Its Drivers in Algeria: National Cross-Sectional Survey-Based Study. Vaccines. 2022. Apr 15;10(4):621. doi: 10.3390/vaccines10040621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bendezu-Quispe G, Caira-Chuquineyra B, Fernandez-Guzman D, Urrunaga-Pastor D, Herrera-Añazco P, Benites-Zapata VA. Factors Associated with Not Receiving a Booster Dose of COVID-19 Vaccine in Peru. Vaccines. 2022. Aug;10(8):1183. doi: 10.3390/vaccines10081183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paul E, Fancourt D. Predictors of uncertainty and unwillingness to receive the COVID-19 booster vaccine: An observational study of 22,139 fully vaccinated adults in the UK. The Lancet Regional Health-Europe. 2022. Mar 1;14:100317. doi: 10.1016/j.lanepe.2022.100317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saddik B, Al-Bluwi N, Shukla A, Barqawi H, Alsayed HA, Sharif-Askari NS, et al. Determinants of healthcare workers perceptions, acceptance and choice of COVID-19 vaccines: A cross-sectional study from the United Arab Emirates. Human vaccines & immunotherapeutics. 2022. Jan 31;18(1):1–9. doi: 10.1080/21645515.2021.1994300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harapan H, Sallam M, Fathima R, Kusuma HI, Anwar S, Nalapraya WY, et al. Willingness to Pay (WTP) for COVID-19 Vaccine Booster Dose and Its Determinants in Indonesia. Infectious Disease Reports. 2022. Dec;14(6):1017–32. doi: 10.3390/idr14060101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bdnews24.com. Bangladesh rolls out COVID vaccine booster doses. January 13, 2023. Available at:https://bdnews24.com/bangladesh/bangladesh-rolls-out-covid-vaccine-booster-doses?fbclid =IwAR1N4iZNdTHc1dKutFfsLmhlW2WnCctUzQoyR7x5QMN-RA8pA2TgNaHmy-M.
- 28.Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, et al. Attitudes toward COVID-19 vaccines in Chinese college students. International journal of biological sciences. 2021;17(6):1469. doi: 10.7150/ijbs.58835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blazar D, Kraft MA. Teacher and teaching effects on students’ attitudes and behaviors. Educational evaluation and policy analysis. 2017. Mar;39(1):146–70. doi: 10.3102/0162373716670260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen Y, Zhang MX, Lin XQ, Wu H, Tung TH, Zhu JS. COVID-19 vaccine hesitancy between teachers and students in a college, a cross-sectional study in China. Human Vaccines & Immunotherapeutics. 2022. Jun 11:2082171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hossain MB, Alam MZ, Islam MS, Sultan S, Faysal MM, Rima S, et al. COVID-19 vaccine hesitancy among the adult population in Bangladesh: A nationwide cross-sectional survey. PloS one. 2021. Dec 9;16(12):e0260821. doi: 10.1371/journal.pone.0260821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee C, Holroyd TA, Gur-Arie R, Sauer M, Zavala E, Paul AM, et al. COVID-19 vaccine acceptance among Bangladeshi adults: understanding predictors of vaccine intention to inform vaccine policy. Plos one. 2022. Jan 13;17(1):e0261929. doi: 10.1371/journal.pone.0261929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abedin M., Islam M. A., Rahman F. N., Reza H. M., Hossain M. Z., Hossain M. A., et al. Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS One. 2021; 16(4), e0250495 doi: 10.1371/journal.pone.0250495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ali M, Hossain A. What is the extent of COVID-19 vaccine hesitancy in Bangladesh? A cross-sectional rapid national survey. BMJ open. 2021. Aug 1;11(8):e050303. doi: 10.1136/bmjopen-2021-050303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Banik R, Islam M, Pranta MU, Rahman QM, Rahman M, Pardhan S, et al. Understanding the determinants of COVID-19 vaccination intention and willingness to pay: findings from a population-based survey in Bangladesh. BMC Infectious Diseases. 2021. Dec;21(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patwary MM, Bardhan M, Disha AS, Hasan M, Haque MZ, Sultana R, et al. Determinants of COVID-19 vaccine acceptance among the adult population of Bangladesh using the health belief model and the theory of planned behavior model. Vaccines. 2021. Nov 25;9(12):1393. doi: 10.3390/vaccines9121393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roy DN, Huda MN, Azam MS. Factors influencing COVID-19 vaccine acceptance and hesitancy among rural community in Bangladesh: a cross-sectional survey based study. Human Vaccines & Immunotherapeutics. 2022. May 6:1–9. doi: 10.1080/21645515.2022.2064685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roy DN, Hossen M, Ferdiousi N, Azam M. Potential factors influencing COVID-19 vaccine acceptance and hesitancy among Bangladeshi people: a cross-sectional study. VirusDisease. 2022. Aug 13:1–0. doi: 10.1007/s13337-022-00775-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hossain M. E., Islam M. S., Ghose T. K., Jahan H., Chakrobortty S., Hossen M. S., et al. COVID-19 vaccine acceptability among public university students in Bangladesh: Highlighting knowledge, perceptions, and attitude. Human vaccines & immunotherapeutics, 2020; 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roy DN, Azam MS, Biswas M, Islam E. Potential factors influencing COVID-19 vaccine acceptance and hesitancy among university students in Bangladesh: A cross-sectional comparative study. Epidemiology & Infection. 2022. Dec 20:1–20. doi: 10.1017/S0950268822001820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hoque AF, Huq S, Abdullah-Al-Shoeb M, Mishu MA, Azad MA. Awareness and likelihood of accepting COVID-19 vaccines among the university students of Bangladesh. International Journal of Public Health. 2022. Jun;11(2):558–65. [Google Scholar]
- 42.Roy DN, Hossen MM, Biswas M, Islam E, Azam MS. Factors influencing COVID-19 vaccine acceptance and hesitancy among pharmacy students in Bangladesh: a cross-sectional study. F1000Research. 2022. Nov 24;11(1379):1379. [Google Scholar]
- 43.Rahman MM, Chisty MA, Alam MA, Sakib MS, Quader MA, Shobuj IA, et al. Knowledge, attitude, and hesitancy towards COVID-19 vaccine among university students of Bangladesh. PloS one. 2022. Jun 27;17(6):e0270684. doi: 10.1371/journal.pone.0270684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Renzi E, Baccolini V, Migliara G, Bellotta C, Ceparano M, Donia P, et al. Mapping the Prevalence of COVID-19 Vaccine Acceptance at the Global and Regional Level: A Systematic Review and Meta-Analysis. Vaccines. 2022. Sep 7;10(9):1488. doi: 10.3390/vaccines10091488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(2):1373–1379. doi: 10.1016/s0895-4356(96)00236-3 [DOI] [PubMed] [Google Scholar]
- 46.Hsieh FY, Bloch DA, Larsen MD. A simple method of sample size calculation for linear and logistic regression. Statist Med. 1998;17(14):1623–1634. doi: [DOI] [PubMed] [Google Scholar]
- 47.Bujang MA, Sa’at N, Bakar TM. Sample size guidelines for logistic regression from observational studies with large population: emphasis on the accuracy between statistics and parameters based on real life clinical data. The Malaysian journal of medical sciences: MJMS. 2018. Jul;25(4):122. doi: 10.21315/mjms2018.25.4.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rzymski P, Poniedziałek B, Fal A. Willingness to receive the booster COVID-19 vaccine dose in Poland. Vaccines. 2021. Nov 5;9(11):1286. doi: 10.3390/vaccines9111286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Klugar M, Riad A, Mohanan L, Pokorná A. COVID-19 vaccine booster hesitancy (VBH) of healthcare workers in Czechia: National cross-sectional study. Vaccines. 2021. Dec 6;9(12):1437. doi: 10.3390/vaccines9121437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lane S.; MacDonald N.E.; Marti M.; Dumolard L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. doi: 10.1016/j.vaccine.2018.03.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Al-Jayyousi GF, Sherbash MA, Ali LA, El-Heneidy A, Alhussaini NW, Elhassan ME, et al. Factors influencing public attitudes towards COVID-19 vaccination: A scoping review informed by the socio-ecological model. Vaccines. 2021. Jun;9(6):548. doi: 10.3390/vaccines9060548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Saigí-Rubió F, Eguia H, Espelt A, Macip S, Bosque-Prous M. Hesitation about coronavirus vaccines in healthcare professionals and general population in Spain. Plos one. 2022. Dec 1;17(12):e0277899. doi: 10.1371/journal.pone.0277899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yoshida M, Kobashi Y, Kawamura T, Shimazu Y, Nishikawa Y, Omata F, et al. Factors Associated with COVID-19 Vaccine Booster Hesitancy: A Retrospective Cohort Study, Fukushima Vaccination Community Survey. Vaccines. 2022. Mar 26;10(4):515. doi: 10.3390/vaccines10040515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jairoun AA, Al-Hemyari SS, El-Dahiyat F, Jairoun M, Shahwan M, Al Ani M, et al. Assessing public knowledge, attitudes and determinants of third COVID-19 vaccine booster dose acceptance: current scenario and future perspectives. Journal of Pharmaceutical Policy and Practice. 2022. Dec;15(1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccines. 2022. Jan 12;10(1):110. doi: 10.3390/vaccines10010110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pires C. Global Predictors of COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines. 2022. Aug 18;10(8):1349. doi: 10.3390/vaccines10081349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Oche OM, Adamu H, Yahaya M, Illo HG, Danmadami AM, Ijapa A, et al. Perception and willingness to accept COVID-19 Vaccines: A cross-sectional survey of the general population of Sokoto State, Nigeria. Plos one. 2022. Dec 1;17(12):e0278332. doi: 10.1371/journal.pone.0278332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khaleduzzaman HM, Mishu NJ. Frequency of Side Effects after First Dose of Vaccination against COVID-19 Among the People of Bangladesh. European Journal of Medical and Health Sciences. 2021. May 17;3(3):22–4. [Google Scholar]
- 59.Parvej MI, Sultana S, Tabassum M, Mannan SE, Ahmed F. Determinants of COVID-19 vaccine acceptance and encountered side-effects among the vaccinated in Bangladesh. Asian Pacific Journal of Tropical Medicine. 2021. Aug 1;14(8):341. [Google Scholar]
- 60.Getachew D, Yosef T, Solomon N, Tesfaye M, Bekele E. Predictors of unwillingness to receive COVID-19 vaccines among Ethiopian Medical students. Plos one. 2022. Nov 2;17(11):e0276857. doi: 10.1371/journal.pone.0276857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Quinn SC, Parmer J, Freimuth VS, Hilyard KM, Musa D, Kim KH. Exploring communication, trust in government, and vaccination intention later in the 2009 H1N1 pandemic: results of a national survey. Biosecurity and bioterrorism: biodefense strategy, practice, and science. 2013. Jun 1;11(2):96–106. doi: 10.1089/bsp.2012.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: A cross-sectional study from Jordan. Plos one. 2021. Apr 23;16(4):e0250555. doi: 10.1371/journal.pone.0250555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gori D, Reno C, Remondini D, Durazzi F, Fantini MP. Are We Ready for the Arrival of the New COVID-19 Vaccinations? Great Promises and Unknown Challenges Still to Come. Vaccines. 2021. Feb;9(2):173. doi: 10.3390/vaccines9020173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nature medicine. 2021. Feb;27(2):225–8. doi: 10.1038/s41591-020-1124-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rego RT, Ngugi AK, Sophie Delius AJ, Luchters S, Kolars JC, Irfan FB, et al. COVID-19 vaccine hesitancy among non-refugees and refugees in Kenya. PLOS Global Public Health. 2022. Aug 24;2(8):e0000917. doi: 10.1371/journal.pgph.0000917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lin Y, Huang Z, Xu X, Du W, Alias H, Hu Z, et al. Multi-dimensional psychosocial factors influencing the willingness to receive a COVID-19 vaccine booster: A survey among the public in Mainland China. Human Vaccines & Immunotherapeutics. 2022. Sep 24:2126667. doi: 10.1080/21645515.2022.2126667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gram MA, Emborg HD, Schelde AB, Friis NU, Nielsen KF, Moustsen-Helms IR, et al. Vaccine effectiveness against SARS-CoV-2 infection or COVID-19 hospitalization with the Alpha, Delta, or Omicron SARS-CoV-2 variant: A nationwide Danish cohort study. PLoS medicine. 2022. Sep 1;19(9):e1003992. doi: 10.1371/journal.pmed.1003992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Temsah MH, Aljamaan F, Alenezi S, Alhasan K, Alrabiaah A, Assiri R, et al. SARS-COV-2 omicron variant: exploring healthcare workers’ awareness and perception of vaccine effectiveness: a national survey during the first week of WHO variant alert. Frontiers in Public Health. 2022;10. doi: 10.3389/fpubh.2022.878159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. doi: 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Roy DN, Hossen MM, Biswas M, Islam E, Azam MS. Prevalence of COVID-19 vaccine hesitancy in students: A global systematic review. F1000Research. 2022. Aug 12;11(928):928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee KW, Gew LT, Siau CS, Peh SC, Chia YC, Yacob S, et al. COVID-19 vaccine hesitancy and its associated factors in Malaysia. PloS one. 2022. Sep 1;17(9):e0266925. doi: 10.1371/journal.pone.0266925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xiao J, Cheung JK, Wu P, Ni MY, Cowling BJ, Liao Q. Temporal changes in factors associated with COVID-19 vaccine hesitancy and uptake among adults in Hong Kong: Serial cross-sectional surveys. Lancet Reg Health West Pac. 2022. Mar 29;23:100441. doi: 10.1016/j.lanwpc.2022.100441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kirkby HM, Wilson S, Calvert M, Draper H. Using e-mail recruitment and an online questionnaire to establish effect size: A worked example. BMC Medical Research Methodology. 2011. Dec;11(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Publicly available at: Figshare: “Minimal Data Set-csv.” DOI: 10.6084/m9.figshare.21896451;"