Abstract
Background
The delivery of high quality care is a fundamental goal for health systems worldwide. One policy tool to ensure quality is the regulation of services by an independent public authority. This systematic review seeks to identify determinants of compliance with such regulation in health and social care services.
Methods
Searches were carried out on five electronic databases and grey literature sources. Quantitative, qualitative and mixed methods studies were eligible for inclusion. Titles and abstracts were screened by two reviewers independently. Determinants were identified from the included studies, extracted and allocated to constructs in the Consolidated Framework for Implementation Research (CFIR). The quality of included studies was appraised by two reviewers independently. The results were synthesised in a narrative review using the constructs of the CFIR as grouping themes.
Results
The search yielded 7,500 articles for screening, of which 157 were included. Most studies were quantitative designs in nursing home settings and were conducted in the United States. Determinants were largely structural in nature and allocated most frequently to the inner and outer setting domains of the CFIR. The following structural characteristics and compliance were found to be positively associated: smaller facilities (measured by bed capacity); higher nurse-staffing levels; and lower staff turnover. A facility’s geographic location and compliance was also associated. It was difficult to make findings in respect of process determinants as qualitative studies were sparse, limiting investigation of the processes underlying regulatory compliance.
Conclusion
The literature in this field has focused to date on structural attributes of compliant providers, perhaps because these are easier to measure, and has neglected more complex processes around the implementation of regulatory standards. A number of gaps, particularly in terms of qualitative work, are evident in the literature and further research in this area is needed to provide a clearer picture.
Introduction
The delivery of high quality care is a fundamental goal for health systems worldwide. Quality is variable, due to structural issues such as insufficient staffing levels [1], or process issues like poor cleaning practices [2], and can cause differences in outcome across health and social care providers such as high complication rates and poor patient experience [3].
Governments commonly introduce regulation to monitor the quality of goods and services. Regulated organisations/individuals must comply with prescribed standards. In health and social care, regulatory bodies typically license or authorise providers, and/or directly regulate the structures and processes of care through inspection, feedback or sanctions [4].
Regulation can be defined as: “sustained and focused control exercised by a public agency over activities which are valued by a community” [5]. The scope of regulation in health and social care differs depending on the setting and country. Principally, regulation centres on structural, process and outcome-related aspects of services. For example, in nursing homes (NH) in the United States, regulations cover inter alia resident rights, nursing services, infection control, physical environment and resident assessment [6].
There are important differences in how countries regulate health and social care. In one model the regulator is a publicly-funded, independent organisation which is aligned to a government ministry e.g. Healthcare Improvement Scotland [7]. There are also examples of regulatory authorities that are incorporated into government ministries e.g. Ministry of Long-Term Care (Ontario) [8].
In both examples above, the regulator has statutory powers of inspection and enforcement. A third approach is found in countries such as Australia where mandatory accreditation is performed by third-party organisations [9]. While having no statutory powers their role is akin to a regulator because any decision to not accredit can result in State sanctions [10]. This is distinct from other models of voluntary accreditation [11].
Regulatory compliance can be understood as “behavior fitting expectations communicated to regulatees regarding how the former should or should not behave in a given domain” [12]. This conceptualisation of compliance is markedly different to adhering to clinical guidelines or voluntary codes of practice. A feature of regulatory compliance is the mandatory requirement to comply with standards and rectify deficits.
There is a substantial literature on the structures (e.g. public/private ownership, facility size and staffing levels/competencies [13–16]) and processes (e.g. disposition towards regulation, normalisation of compliance within day-to-day operations [17, 18]) which determine compliance by health and social care organisations. This literature, not yet synthesised, is a distinct subset of the broader literature on determinants of quality because of the context and focus of regulation. Unlike most quality assessment initiatives, regulation involves consequences for the regulatee, and therefore introduces different motivations around implementation.
Regulators and regulatees would prefer that all interactions produced findings of compliance. Understanding the determinants of compliance is one way to increase this likelihood. Regulation can be regarded as a complex intervention and compliance equates to successful implementation. This allows for the use of implementation science concepts to better understand why some organisations fail to comply: “implementation science enables questions to be asked about whether, and if so how, an intervention can make a difference to a patient’s life or to the practice of a health care delivery team” [19]. The success of an innovation is contingent on a range of factors. For example, the attitudes and beliefs of staff towards an innovation can influence its implementation [20].
Several tools/frameworks have been developed in the field of implementation science. The Consolidated Framework for Implementation Research (CFIR) is one such framework [21]. The CFIR was developed by drawing together disparate existing theories on implementation to produce an “overarching typology–a list of constructs to promote theory development and verification about what works where and why across multiple contexts” [21]. The CFIR has been used previously as a framework for structuring and synthesising the results of systematic reviews [22].
There is a body of work critiquing the effectiveness of regulation (e.g. improving system performance [23]), but given that regulation exists, and that there is much effort put into compliance, it is legitimate to investigate this practice on its own terms. There has been no previous synthesis of the extensive literature which makes use of regulatory compliance as an outcome measure in health and social care settings. Moreover, little is known about the processes by which health and social care services manage regulatory encounters and how this impacts on compliance. Thus, the aim of this systematic review is to identify and describe determinants of regulatory compliance in health and social care services, and the broader phenomenon of attempting compliance. The focus of the review is on the regulation of organisations as there are existing evidence syntheses on the regulation of individual professionals [24, 25].
Methods
We performed a systematic review of studies that used qualitative, quantitative or mixed-methods approaches to identify determinants of compliance in health and social care services. We take regulation to mean any form of evaluation of quality and safety which is underpinned by sanctioning powers. Any literature focusing on the regulation of individual professionals (e.g. nurses) or on occupational health and safety (e.g. working hours) were outside scope. Determinants were anything associated with compliance and could be aspects of the organisation or the environment in which it is situated. Determinants may also be barriers or facilitators to successful implementation of regulatory requirements. In quantitative studies the outcome of interest was regulatory compliance and in qualitative studies this was also the phenomenon of interest. We interpreted regulatory compliance as any formal approval of the performance of a health or social care provider by the relevant regulator or accrediting agency. The review follows a published protocol which was not registered [26]. The methods applied are summarised in brief with additions to/deviations from the original protocol outlined.
Criteria for inclusion
The phenomena of interest were determinants of regulatory compliance in health and social care services.
Articles—either qualitative, quantitative or mixed-methods—were included if they:
Described factors or characteristics that were related to regulatory compliance. Specifically, this refers to regulations that are mandated by government or other state authorities. A wide range of constructs were considered for inclusion including, but not limited to, the following: service characteristics (size, location, model of care, ownership); organisational characteristics (culture, management/governance structure, maturity); service user characteristics (age, disability type, disease/illness); nature of regulatory engagement (punitive, adversarial, collaborative).
Discussed barriers or facilitators to regulatory compliance for health and social care services.
Were focused on quality of care in health and social care services and used regulatory compliance as an outcome measure.
Studies were excluded if they:
Analysed regulatory compliance in a field other than in a health or social care setting.
Analysed compliance with clinical guidelines or other evidence-based methods for managing care that were not underpinned by the potential for regulatory sanction where there was a failure to comply.
Used an outcome measure that was not equivalent to regulatory compliance in accordance with the definitions set out above. For example: adherence to voluntary standards or codes of conduct; where failure to comply does not result in regulatory sanctions of enforcement; compliance concerning individuals as opposed to organisations as is the case with regulations for specific health care professionals.
A search strategy using the CIMO (Context, Intervention, Mechanism, Outcome) framework was devised (S1 File). Searches were carried out on 22nd July 2022 on PubMed, MEDLINE, PsycINFO, CINAHL, SocINDEX and OpenGrey. Targeted web searches were conducted. The reference lists of any systematic reviews identified were searched for relevant material. In deviating from the protocol, we included the term ‘accreditation’ in the search terms to identify studies where accreditation was mandatory i.e. de facto regulation. There were no time or language restrictions. The reference lists of all included articles were hand-searched for additional relevant material. Forward citation searching of included articles was also conducted.
Screening and full-text review
All articles were imported into Covidence [27] and the title/abstract screened by two reviewers independently. Full-text review was carried out by PD.
Data extraction
Data extraction was performed by PD. LMK independently performed data extraction on 10% of articles for cross-check purposes. For all studies, the following data were extracted: full reference, study type, publication type, country, study aim(s), population/setting. The extraction of results data differed depending on the study design. For example, in studies reporting quantitative results, the variable name and its direction of association with compliance were extracted whereas for qualitative studies whole sentences or phrases were extracted.
Determinants expressed as composites (e.g. Medicaid occupancy multiplied by Medicaid rate) were omitted. We focused on determinants of overall compliance measures. Where not available, determinants of compliance with specific regulations were reported. We excluded variables acting as measures of quality (e.g. proportion of patients/residents with pressure sores; proportion of patients/residents subject to physical restraint), because of the likelihood of circular reasoning: in theory, quality is an outcome, rather than a determinant of compliance.
In qualitative and mixed-methods studies, anything mentioned as influential with respect to compliance activity, either negative or positive, was extracted for synthesis.
Analysis
We counted studies where a determinant was estimated and recorded the association with compliance in each case. In quantitative studies associations with compliance were recorded as ‘positive/negative/null’ for continuous or ordinal variables, ‘different/null’ for nominal variables (‘different’ denoting that one or more categories in the variable was positively or negatively associated with compliance). In qualitative studies the role of the relevant factor in influencing engagement with the regulatory process was noted.
Determinants were then coded to the most appropriate CFIR construct through an iterative and deliberative process among all three authors. PD first coded each determinant to the most appropriate CFIR construct (e.g. determinants related to facility size were coded to the structural characteristics construct in the inner setting domain), with reference to established definitions [21]. These data were then discussed jointly by PD and LMK in order to ensure that determinants were placed in the most appropriate construct. This process resulted in some determinants being moved to alternative constructs and also the creation of a category of ‘other’ within each domain. This was necessary due to the significant number of determinants that had no appropriate match in the CFIR (e.g. the survey tools used by inspectors had no equivalent match for a construct in the intervention characteristics domain).
PD, LMK and JPB subsequently discussed all coding with a particular emphasis on whether the determinant had relevance in the specific context of implementing regulations. For example, a determinant relating to the level of public/state funding made available for services was originally coded to the available resources construct in the inner setting domain. On reflection, we determined that this was not appropriate as the funding was not specifically related to implementing regulations. As such, this determinant was moved to ‘other’ in the inner setting domain. This process continued until all three authors agreed on the coding of each determinant. The analysis was also consistent with the application of the CFIR to post-implementation evaluation of innovations, where determinants are linked to outcomes i.e. compliance [21].
Quality appraisal
Quality appraisal of quantitative and qualitative studies used the Joanna Briggs Institute tools [28]; for mixed-methods studies we used the Mixed-Methods Appraisal Tool (MMAT) [29]. All grey literature were PhD theses and were appraised using the most appropriate Joanna Briggs Institute tool [28]. PD and FB (see acknowledgments) carried out quality appraisal independently and subsequently compared findings. Any disagreements were resolved by PD and FB jointly reviewing the respective studies and arriving at a consensus.
Results
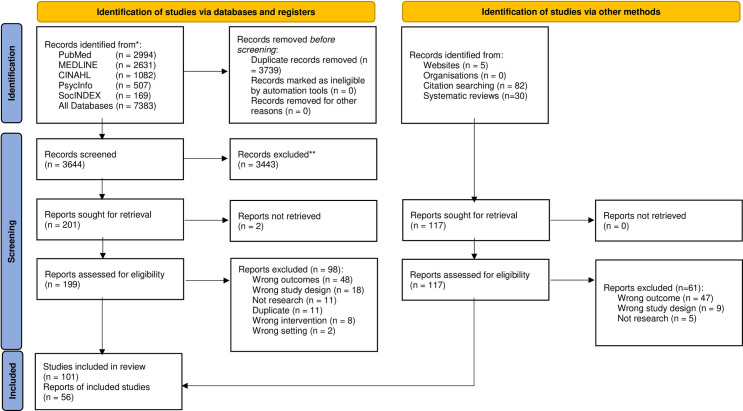
7,500 records were retrieved: 7,383 from electronic database searches and 117 from targeted web searches, reference searches and forward citation searching. Of the 7,383, 3,739 duplicates were removed. Title/abstract of 3,644 were screened, 3,443 did not meet inclusion criteria, leaving 201 for full-text review. All but two studies were retrieved, leaving 199 for full-text review. Upon full-text review, 98 were excluded leaving 101.
Of the 117 found by other means (i.e. targeted web searches, reference searches and forward citation searching), 61 were ineligible, leaving 56. The total number of studies in the review was 157 (See Fig 1 for PRISMA flow diagram, S1 Checklist for PRISMA checklist and S2 Table for full list of included studies). Characteristics of included studies are set out in Table 1.
Fig 1. PRISMA 2020 flow diagram: Determinants of regulatory compliance in health and social care services: A systematic review using the consolidated framework for implementation research.
Table 1. Characteristics of studies included in the systematic review.
| Publication type | n (%) |
| Journal Article | 137 (87.3) |
| Thesis | 19 (12.1) |
| Book Section | 1 (0.6) |
| Study setting | n (%) |
| Nursing Homes | 143 (91.1) |
| Hospitals | 7 (4.4) |
| Nursing/Care Homes | 2 (1.3) |
| Assisted-living facilities | 2 (1.3) |
| Nursing Home/Assisted-Living Facilities | 2 (1.3) |
| Pharmacies | 1 (0.6) |
| Study design | n (%) |
| Quantitative | |
| Cross-sectional/Observational | 140 (89.2) |
| Longitudinal | 3 (1.9) |
| RCT | 2 (1.3) |
| Experimental | 2 (1.3) |
| Qualitative | |
| Case study | 4 (2.5) |
| Ethnography | 1 (0.6) |
| Focus groups | 1 (0.6) |
| Mixed methods | 4 (2.5) |
| Country | n (%) |
| USA | 140 (89.2) |
| Australia | 9 (5.7) |
| Europe | |
| United Kingdom | 3 (1.9) |
| Denmark | 1 (0.6) |
| Portugal | 1 (0.6) |
| Netherlands | 1 (0.6) |
| China | 1 (0.6) |
| Saudi Arabia | 1 (0.6) |
Search parameters were configured to identify studies that specifically focused on compliance as an outcome. It is possible there is a body of literature on regulatees’ perspectives on regulation that were not included as there was no attempt to link these perspectives to compliance.
Quality appraisal
Quantitative studies
There were mixed findings in terms of the quality of quantitative studies (S1 File). Most followed best practice in terms of defining their samples, identifying and controlling for confounding factors, and using appropriate statistical methods. However, there were limitations evident in the use of self-reported measures (e.g. measurements of culture) and therefore it was not possible to be assured that these were objective.
Qualitative and mixed methods studies
Most qualitative and mixed methods studies were of good quality (S1 File). There was generally a congruence between the methods employed by the researchers and their objectives, data collection methods, analysis and interpretation of results. Common weaknesses in these studies tended to be a lack of reflexivity or the absence of a statement locating the authors culturally and theoretically in the research.
Mapping findings to the CFIR
We coded findings to all five CFIR domains. We coded findings to 19 of the 39 CFIR constructs, in addition to coding findings to an additional construct for ‘other’ in each of the five domains.
Intervention characteristics
This domain covers “aspects of an intervention that may impact implementation success, including its perceived internal or external origin, evidence quality and strength, relative advantage, adaptability, trialability, complexity, design quality and presentation, and cost” [30]. We coded nothing to four of the eight constructs in this domain: intervention source; trialability; design quality and packaging; cost. In total, 16 studies featured in this domain, see Table 2.
Table 2. Determinants coded to the intervention characteristics domain.
| Construct | Determinant |
|---|---|
| Intervention Source | No studies |
| Evidence Strength & Quality | “The sentiment seemed to be shared among others in the room, who laughed and nodded, and agreed that there was a tangible disconnect between their delivery of clinical care and the ratings and scores representing their care to the public“ “As one nurse manager put it in a meeting," … it’s not about the clinical management of sepsis, it’s about fully reporting the “cookbook” steps of the goal” “clinicians repeatedly defined metric compliance as distinct to their clinical practice or scientific expertise” [18] |
| Relative Advantage | “Rather than containing the worst aspects of corporate activity in this sector, regulation may serve to obscure what might be widespread routine forms of injurious activity through a veil of bureaucratic compliance” [31] |
| “During the discussion one of the participants (E8) mentioned that there are an estimated 3,000 non-licensed nursing homes in Portugal. “An inspection with a global closing order of all the illegal nursing homes would create an unsolvable problem: what would become of all the elderly who live there nowadays, who are roughly 25,000 to 30,000 people? There are simply not enough beds for so many people” (E8). Therefore, as mentioned by E5: “Unfortunately there is a lot of covering-up and impunity in Portugal” [32] | |
| Adaptability | “A mandate that requires clinicians to timestamp and document secondary tasks, just to ensure metric compliance, historically is not typical for ED workflow” [18] |
| Trialability | No studies |
| Complexity | “An internist involved in quality assurance, explained that clinicians and administrators agreed SEP-1 was so complex it would need its own meeting” “His explanation echoes accounts from research at other hospitals, which confirm unprecedented complexity contributing to SEP-1’s difficulty” [18] |
| Design Quality & Packaging | No studies |
| Cost | No studies |
| Other | Disapproving inspection teams [33] Inspection team characteristics [34–38] |
| Inspection survey tool [39, 40] Inspection team: cooperative [41] Inspection team: deterrence [41] Inspection team: persuasion and education [41] Inspection team viewed intervention as necessary [41] Inspection type [42] Perceived persuasive approach by regulator [43] Perceived punishment approach by regulator [43] Re-integrating inspection teams [33] Stigmatizing inspection teams [33] Tolerant inspection teams [33] Unannounced inspections [44] |
Evidence strength & quality
Stakeholders’ perceptions of the quality and validity of evidence supporting the belief that the innovation will have desired outcomes.
Hospital staff expressed scepticism that a regulatory rating reflected their own perception of quality: “The sentiment seemed to be shared among others in the room, who…agreed that there was a tangible disconnect between their delivery of clinical care and the ratings and scores representing their care to the public” [18].
Relative advantage
Stakeholders’ perception of the advantage of implementing the innovation versus an alternative solution.
In this instance, regulatory standards were the innovation to be implemented. Findings were coded here if they were concerned with advantages (or disadvantages) derived from complying. NH inspectors noted that enforcing closure of unauthorised NH would mean loss of bed capacity, thereby questioning the logic of implementing that solution [32]. The inspectors reasoned that turning a blind eye was somehow more desirable than the closure of thousands of beds [32]. In a participant observation study, regulators provided “a veil” of compliance to care providers who then leveraged this to attract service users [31]. Managers “reproved workers not on the basis of whether tasks had been completed, but according to whether files reflected regulatory standards” [31]. Thus, management perceived the advantage of good documentation—even going as far as to falsify records—in order to achieve compliance [31].
Adaptability
The degree to which an innovation can be adapted, tailored, refined, or reinvented to meet local needs.
This construct refers to how regulatory measures can be adapted to fit with existing work practices. In a qualitative study, the requirement for clinicians to document secondary tasks to ensure compliance was reported to be difficult to adapt to a hospital’s workflow [18]. Thus, it was challenging to comply because it created additional work or necessitated a work-around.
Complexity
Perceived difficulty of the innovation, reflected by duration, scope, radicalness, disruptiveness, centrality, and intricacy and number of steps required to implement.
A regulatory measure related to sepsis treatment procedures presented “unprecedented complexity”; study participants suggested it was so complex it required its own quality assurance meeting [18].
Other
Findings were placed in this section where they could not be coded to an appropriate construct but were considered relevant to this domain.
A study on attitudes to regulation reported that physicians who perceived a persuasive approach by regulators tended to be more compliant, as compared with a punishment approach [43]. Disapproving and re-integrating (i.e. respectful disapproval and then terminating disapproval through forgiveness upon improvement) inspection teams and compliance were positively associated whereas tolerant and stigmatizing teams were negatively associated [33]. Inspection teams that viewed intervention as necessary were positively associated with compliance, compared to three other types (cooperative; deterrence; persuasion & education) where there was a null association [41].
Inspection team characteristics (e.g. office base, team composition) and compliance was reported to be associated in all five studies that investigated these determinants [34–38]. The number of inspectors on a team was reported to have a null association with compliance [45]. Two studies investigated various tools used for inspection and both had an association with compliance [39, 40]. The type of inspection (e.g. inspections that mandated interviews with service users) was reported to be associated with compliance [42] whereas unannounced inspections were reported to have a null association when compared with announced [44].
Outer setting
The outer setting domain is defined as “external influences on intervention implementation including patient needs and resources, cosmopolitanism or the level at which the implementing organization is networked with other organizations, peer pressure, and external policies and incentives” [30]. Seventy-two studies were featured in the ‘peer pressure’ and ‘external policy and incentives’ constructs, as well as in ‘other’. No determinants were coded to two of four constructs in this domain: ‘cosmopolitanism’ or ‘needs and resources of those served by the organisation’, see Table 3.
Table 3. Determinants coded to the outer setting domain.
| Construct | Determinant |
|---|---|
| Needs & Resources of Those Served by the Organization | No studies |
| Cosmopolitanism | No studies |
| Peer pressure | Higher competition [13, 16, 46–63] Higher excess bed capacity in county [16, 64] Higher service demand [62] Nursing homes per population [64] Proportion of chains in region [55, 65, 66] Proportion of for-profit facilities [66] Proportion of hospital-based facilities [55, 66] Transparency (publication of star-rating) [53] |
| External Policy & Incentives | Higher state focus on infection prevention [67] Minimum staffing standard [68–70] More stringent nursing home administrator licensing criteria Ombudsman available [71–73] State-level mandatory overtime laws [46] States with certificate of need law [74] |
| Other | Ageing advocacy group influence [66] Democratic party controlled legislature (USA) [66] Governor’s institutional power [66] Higher local income [47, 50, 52, 59, 60, 62, 63, 66] Higher local unemployment [75] Higher mean age of service users [51, 66, 76] Higher population density [36, 46, 51, 62, 76–87] Higher proportion of African-American service users [13, 52, 76, 88, 89] Higher proportion of African-Americans residents in county [52] Higher proportion of Asian service users [52] Higher proportion of female service users [45, 51] Higher proportion of George W. Bush supporters in county [74] Higher proportion of Hispanic service users [13, 52, 89] Higher proportion of Hispanic residents in county [52] Higher proportion of married service users [45] Higher proportion of other non-White service users [13] Higher proportion of service users with dementia [14, 47, 49, 50, 54, 58, 59, 62, 63, 90–92] Higher proportion of service users with a disability [16, 45, 82] Higher proportion of service users with intellectual disability [49, 50, 54, 58, 59, 63, 92] Higher proportion of service users with incontinence needs [14, 54, 82, 90, 91, 93–97] Higher proportion of service users with mental illness [14, 47, 49, 50, 54, 57–59, 62, 63, 82, 90, 92–96, 98–102] Higher proportion of service users with obstructive bowel syndrome [82] Higher proportion of service users with high/complex care needs [14, 16, 46, 47, 49–52, 54, 58–64, 72, 82, 86, 90–97, 99, 103–110] Higher proportion of veterans [111] Higher proportion of White residents [51, 76, 112] Higher public funding [47–50, 55, 57–60, 63–66] Higher rate of religiosity [74] Individualistic state [74] Higher legislative professionalism [66] Nursing home industry influence [66] Moralistic state [66] State with Democratic Governor (USA) [55, 66] |
Peer pressure
Mimetic or competitive pressure to implement an innovation, typically because most or other key peer or competing organizations have already implemented or are in a bid for a competitive edge.
Market pressure was frequently studied and we mapped related determinants to this construct. This may occur in two ways: pressure to have better compliance rates than competitors in order to attract more clients; or pressure to match or exceed the compliance levels of peer organisations (e.g. a chain of hospitals owned by one corporation). Of 20 studies investigating competition, four reported high competition was positively associated with compliance [16, 57–59], four had a negative association [60–63], 11 reported a null association [13, 46–55]; one had a u-shaped finding where higher competition and monopoly were both positively associated whereas moderate competition was negatively associated [56].
Other studies investigated NH markets in a region. A higher proportion of chain NHs in a state and compliance was negatively associated in two studies [55, 65], a third reported a null association [66]. The proportion of for-profit [66] and/or hospital-based NHs [55, 66] and compliance had a null association. The number of NHs in a county per population and compliance had a null association [64]. Additional findings related to this construct included: publication of quality ratings, which we construed as increasing competitive pressure within local markets (null [53]), excess bed capacity in a county (positive [64]; null [16]) and higher service demand (positive [62]).
External policy and incentives
A broad construct that includes external strategies to spread innovations including policy and regulations (governmental or other central entity), external mandates, recommendations and guidelines, pay-for-performance, collaboratives, and public or benchmark reporting.
We interpreted this construct as relating to the regulatory environment, either via funding, legislative measures or quality improvement initiatives from external sources. In American states that had legislation/policies governing quality issues (e.g. minimum staffing standards [68–70] or infection control initiatives [67]) a ‘spillover’ effect was observed: service providers were more compliant with other regulations compared with states that had no such legislation/policies. Other findings included: presence of an ombudsman (positive [71]; null [72, 73]); stricter licensing criteria for NH managers (null [66]); mandatory overtime laws (negative [46]); and states with ‘certificate of need’ laws (positive [74]).
Other
Findings were placed in this section where they could not be coded to an appropriate construct but were still considered relevant to this domain.
Most of the material listed below relates to service user needs or the characteristics of a given population. We coded measures of service user case-mix to the ‘outer setting’ domain because, although case-mix is treated within the ‘inner setting’, it is a measure of the broader population being served.
In the context of people using services, 43 studies investigated the proportion of service users with needs that may require more care (e.g. dementia, incontinence, mental ill health) [14, 16, 45–47, 49–52, 54, 57–64, 72, 82, 86, 90–110, 113]. In general, higher proportions of such service users and compliance was negatively associated. For example, a higher proportion of service users with higher or more complex care needs (typically measured by case mix or activities of daily living scores) and compliance was reported to be positively associated in five studies [14, 58, 90, 93, 97], negatively in 18 studies [14, 16, 46, 47, 49, 60, 62, 82, 90–93, 96, 99, 104, 105, 108, 113], with 21 reporting a null association [50–52, 54, 59, 61, 63, 64, 72, 82, 86, 92–94, 96, 97, 103, 106, 107, 109, 110] (some studies investigated multiple different measures of care needs and reported different associations with compliance. Therefore, these studies appear across more than one of the above categories).
Higher mean age of service users and compliance was negatively associated in two [66, 76] of three studies. Studies also investigated service user ethnicity: higher proportion of white service users (positive [76]; null [51]); higher proportion of Asian service users (positive [52]); higher proportion of black service users (negative [76, 88]; null [13, 52, 89]); higher proportion of Hispanic service users (null [52, 89]; positive [13]); higher proportion of other non-white service users (positive [13]). Studies also reported on proportion of female service users (positive [45]; null [51]), proportion of married service users (positive [45]), and proportion of service users that were war veterans (negative [111]).
Other studies measured characteristics of the broader population served by a provider. Higher population density and compliance was positively associated in five studies [62, 76, 84, 85, 87], negatively in one [86], with ten finding a null association [36, 46, 51, 77–83]. Other material featuring in this construct were the proportion of elderly in the population (positive [50, 60, 74], negative [49, 55, 58, 63], null [47, 59]); higher per-capita/household income (positive [49, 66]; negative [46, 58]; null [47, 50, 52, 59, 60, 62, 63]) higher unemployment rates (positive [75]); higher rates of religiosity (positive [74]); higher proportions of African-Americans in a county (positive [52]); and higher proportions of Hispanics in a county (positive [52]).
Higher levels of public/state funding for services and compliance was positively associated in six studies [47, 50, 57, 58, 60, 114], negatively in one study [63] and seven studies reported no association [48, 49, 55, 59, 64–66].
Three studies from the United States examined political context such as having a Democratic party Governor (negative [55]; null [66]); a higher level of legislative professionalism [66]; the proportion of people that supported George W. Bush (positive [74]); having a Democratic-controlled legislature (negative [66]); or states designated as individualistic (positive [74]) or moralistic (null [74]). The presence of lobbying groups and compliance was reported to have a null association [66].
Inner setting
The majority of studies (n = 132) included at least one determinant coded to this domain (see Table 4). We coded no determinants to five out of 12 constructs: implementation climate–organisational incentives and rewards; implementation climate–goals and feedback; readiness for implementation; readiness for implementation–available resources; readiness for implementation–access to knowledge and information.
Table 4. Determinants coded to the inner setting domain.
| Construct | Determinant |
|---|---|
| Structural Characteristics | Continuing care retirement community [71, 92, 93] County medical care facility [106] Facility certification status [36] Facility certification type [78, 87] Facility provides skilled/specialist services [36, 62, 71, 80, 82, 91, 92, 95, 110, 115–117] For-profit facility [13, 16, 32, 35, 36, 45, 47–52, 54, 57–65, 71, 72, 74, 76, 80–87, 90–93, 95, 103, 104, 106, 108, 113, 115–123] Geographic location [13, 40, 45, 54, 61, 64, 79, 85, 87, 92, 94, 106, 117, 124, 125] Government-owned nursing home without a shared owner in hospital referral region [93] Higher number of years of facility in operation [45, 53, 93, 110, 115] Hospital-based facility [14, 16, 36, 61, 62, 71, 74, 78, 91, 93, 95, 104, 106, 126] Hospital participating in a clinical surgery registry [105] Larger size facility [13, 14, 16, 34–37, 45–47, 49–52, 54, 57–64, 71, 72, 74, 77, 78, 80–83, 85–87, 91–97, 105, 106, 108, 113, 114, 116–118, 120–124, 126–128] Level-1 trauma centre [105] Major teaching hospital [105] Model of ownership [62, 77, 78, 92, 96, 97, 107, 123, 126, 129, 130] Number of years organisation has engaged with accreditation [121] Nursing home co-location [127] Nursing home located near psychiatric hospital [102] Nursing home participating in community nursing home programme [111] Nursing home with shared owner of another nursing home in hospital referral region [93] Nursing home with specialist registration [110] Revenue source [78] Safety-net hospital status [105] “social workers and admission coordinators [in poorly-performing nursing homes as measured by compliance] were instructed to fill beds with Medicare residents before accepting Medicaid residents” [131] |
| Networks & Communications | Chain membership [13, 47, 49–52, 54, 58–63, 74, 76, 80, 82, 90, 92–96, 104, 106, 108, 113, 116, 122, 123, 132] Higher facility consultation with families [52, 76, 90, 116] Higher facility consultation with residents [71, 90, 116] Higher staff meeting frequency [133, 134] Higher use of information technology [81, 124, 134–136] Notification method for residents with potential infection [133] Nursing home has resident/family council [93] Nursing home is associated with other compliant facilities [137] Nursing homes that use a satisfaction survey [138] Process standardisation across chain [94] “In the historically high-performing nursing homes (NH1 and NH2), administrative and direct care staff used multiple modes of communication to care for residents and their families” [131] “In both homes, the flow of information, both hierarchically and laterally, was important to meeting resident needs quickly and thoroughly” [131] “In the low-performing nursing homes (NH3 and NH4), the conflicting message regarding the organizational mission, that is, the explicit (resident care) versus the implicit (economic viability and regulatory compliance), fragmented and confused staff” [131] “Problem resolution resulted in the creation of new forms, additional steps, problem intensification, and communication breakdown within and across disciplines and departments” [131] |
| Culture | Changing from non-profit to for-profit facility [139] Higher culture change focus [140, 141] Higher focus on reducing hospitalisation [133] Higher focus on patient-centred care [103, 108, 142, 143] Nursing home strategic focus [144] Organisational disposition towards regulation [41, 137] |
| Implementation Climate | |
| Tension for Change | More strict enforcement [53, 93, 115, 145–148] “participants expressed an awareness of the pressure they feel to reduce the overall reported rate to fulfill regulatory requirements and maintain or improve their star rating via the CMS public-reporting system to denote nursing home care quality” [149] |
| Compatibility | “The powerplan was stressed as the key to correct documentation and thereby improved compliance with the metric” “a coordinated, and inevitably, standardized approach to treating sepsis based on both policy requirements and clinical expertise. They also produce the documentation necessary for meeting and reporting on regulatory sepsis metrics” [18] |
| Relative Priority | Provider concern about regulatory enforcement [45] |
| Organizational Incentives & Rewards | No studies |
| Goals & Feedback | No studies |
| Learning Climate | “Staff across and within all disciplines [in high-performing nursing homes as measured by compliance] were involved in problem solving and decision making; staff were reminded that decision making and creativity improved with multiple perspectives” [131] |
| Readiness for Implementation | No studies |
| Leadership Engagement | Accredited facility [105, 118, 150–152] Higher ownership turnover [84] Receipt of a quality award [153] “In the high-performing homes, the leadership behaviors of the NHA and the DON created a clear, explicit, and coherent mission, a strong sense of purpose, for the organization….The importance of leadership relationship behaviors and the congruence of the stated and lived mission of the home were strikingly different between high- and low-performing homes” [131] |
| Available Resources | No studies |
| Access to Knowledge & Information | No studies |
| Other |
Staffing Higher administrative staffing [14, 54] Higher agency/contract staff levels [46, 143, 154, 155] Higher degree of nursing centralisation in a nursing home [36] Higher food-service staffing [156] Higher housekeeping staffing [14, 156] Higher infection control professional quality [134] Higher job satisfaction [157] Higher level of certified medication aide staffing [158] Higher level of staff training [91, 94, 110, 116, 133] Higher level of trainee nurse aides [158] Higher licensed practitioner/vocational nurse staffing [14, 47, 49–51, 54, 57–61, 63, 77, 81, 82, 93, 95, 108, 114, 123, 143, 156, 158] Higher nurse aide absenteeism [132] Higher nurse aide staffing [14, 15, 34, 36, 47, 49–51, 54, 57–61, 63, 81, 82, 93, 95, 108, 114, 123, 126, 127, 143, 156, 158, 159] Higher ratings for work effectiveness and practice environments in nursing homes [108, 120] Higher ratio of registered nurses as against other nurse and care staff [35, 57, 59, 97, 109, 113, 143, 160] Higher registered nurse staffing [14, 15, 35, 49–51, 54, 58, 59, 61, 63, 66, 93, 95, 96, 107–109, 113, 114, 122, 123, 127, 143, 154, 156, 158, 159, 161] Higher social services director caseload level [84] Higher specialist staffing [14, 34, 36, 57, 91, 116, 156, 162] Higher staff turnover [35, 52, 54, 76, 97, 133, 134, 143, 154, 160, 163–169] Higher staff workload [84, 133] Higher total nursing staff [35, 36, 47, 57, 60, 61, 72, 81, 83, 105, 107, 126, 158, 161, 164] Higher total staffing [52, 91, 94, 116, 122, 154] Nursing home meeting minimum staffing standard [60, 161] “Administrative leadership behaviors that fostered staff appreciation included routine practices such as having adequate staffing levels and resources to do the job (e.g., resident lifts); helping out on the floor by making beds, passing meal trays, and assisting residents when needed” [131] Financial Facilities that provided finances training, meetings or expert consultation related to infection control [133] Higher facility costs [64, 76, 82, 97, 106, 130, 170–173] Higher facility income [52, 64, 110, 172] Higher facility market share [174] Higher facility profitability [13, 51, 97, 175, 176] Higher staff salary levels [128] Higher proportion of private payers [62, 97, 116] Higher proportions of publicly-funded service-users [13, 14, 16, 35, 36, 46–52, 54, 57–59, 61, 62, 64, 66, 76, 77, 80, 82, 86, 87, 90–92, 95, 97, 104, 106, 107, 109, 110, 113, 114, 116] Admissions Accepts Medicaid admissions [35, 71, 80, 83, 115] Accepts Medicare admissions [71, 104] Higher admission rate [82, 96] Hospitals accepting critical access or rural referrals [86] Higher occupancy levels [16, 46, 47, 49–51, 54, 55, 57–61, 63–65, 82, 90–93, 95, 106, 110, 113, 119, 126, 154] Ownership Recently-acquired nursing homes [93, 177] Poor quality nursing homes that were acquired by a chain [177] Higher quality of acquiring nursing home chain [177] Infection control Additional job responsibilities for infection control staff Participation in infection control collaborative [133, 134] Types of resources used to determine and treat infection [133] Chains Physical plant standardisation across a nursing home chain [94] |
Structural characteristics
The social architecture, age, maturity, and size of an organization.
We construed this construct as including a wide range of organisational characteristics such as size, location, for-profit status and services provided.
Of the 15 studies that evaluated geographic location (comparing cities or regions), 14 reported compliance differed depending on location [13, 40, 45, 54, 61, 64, 79, 85, 87, 92, 94, 106, 117, 125]; one [124] reported a null association.
For-profit service providers and compliance were negatively associated in 29 studies [13, 16, 32, 45, 48, 52, 57, 60–62, 65, 72, 74, 76, 80, 84–87, 90–93, 104, 113, 115, 116, 119, 123], positively associated in seven [50, 58, 63, 81, 95, 117, 121], with a null association in 17 studies [35, 36, 47, 49, 51, 54, 59, 64, 71, 82, 83, 103, 106, 108, 118, 120, 122]. Aligned to the profit motive, in a qualitative study, staff in poorly-performing NHs (as measured by compliance) were instructed to prioritise the admission of people that attracted higher fees [131].
Larger facilities and compliance were negatively associated in 40 studies [13, 14, 16, 34–37, 46, 50–52, 54, 57, 58, 60–62, 64, 74, 77, 80, 82, 83, 86, 91–96, 106, 113, 114, 116, 117, 120, 122, 124, 127, 128]; three reported a positive association [59, 63, 71] and 16 a null association [45, 47, 49, 72, 78, 80, 81, 85, 87, 97, 105, 108, 118, 121, 123, 126] (one study [80] reported larger size NHs had a null association whereas larger size assisted-living facilities had a negative association, thereby represented in both columns). The longer a service was in operation was reported to be associated with poorer compliance in four of five studies [45, 53, 93, 110, 115]. Hospital-based NHs and compliance were positively associated in five studies [16, 62, 91, 93, 95], negatively in one [74], and there was no association in eight studies [14, 36, 61, 71, 78, 104, 106, 126].
There was no consistent association with compliance for facilities that provided a range of skilled/specialist services (positive [62, 71, 80, 82, 91, 116]; negative [62, 91, 92, 110, 115–117]; null [36, 62, 92, 95]). Assisted-living facilities with a nursing licence and compliance were negatively associated [80]; those with a mental health care licence positively associated [80]; and those providing memory care services had a null association [80]. Various models of facility ownership (e.g. publicly-owned, voluntary organisation or private corporation) and compliance were reported to be associated in five studies that investigated this determinant [78, 96, 123, 129, 130], whereas six reported a null association [62, 77, 92, 107, 126, 128].
Among other findings were: continuing care retirement communities (positive [92, 93]; null [71]); location beside a psychiatric hospital (negative [102]); county medical care facilities (null [106]); participation in a community NH program (negative [111]); teaching hospital status (negative [105]; null [86]); NH location (in the context of being co-located with various other types of services) was associated with compliance [127]; revenue source (null [78]); facility certification type was associated with compliance in one study [78] with a null association reported in another [87]; facilities in the United States designated as safety-net hospitals (i.e. serve all populations regardless of insurance status) (negative [105]); hospitals designated as level-1 trauma centres (negative [105]); hospitals participating in a clinical surgery registry (negative [105]); facility certification status (null [36]); facility proximity to a psychiatric hospital (negative [102]); nursing home shared ownership status (a form of public-private ownership) (positive [93]); and more organisational experience with the accreditation process (positive [121]).
Networks and communications
The nature and quality of webs of social networks, and the nature and quality of formal and informal communications within an organization.
Chain facilities and compliance had a negative association in 14 studies [13, 58–60, 62, 74, 80, 90, 95, 104, 113, 116, 122, 132], eight reported a positive association [47, 50, 63, 76, 93, 94, 96, 123] and nine a null association [49, 51, 52, 54, 61, 82, 92, 106, 108]. NHs that had a history of compliance were found to have effective communication practices, both hierarchically and laterally in a qualitative study: “administrative and direct care staff used multiple modes of communication to care for residents and their families” [131]. In contrast, poorly-performing nursing homes “confused staff” with conflicting messages regarding the service’s organisational mission and tension between providing resident care and ensuring economic viability [131].
A range of other factors were found to have no clear association with compliance: higher consultation with families (positive [76, 116]; negative [76]; null [52, 90]); higher consultation with NH residents (positive [116]; negative [90]; null [71]); NHs with family/resident councils (negative [93]); NHs that used a satisfaction survey (positive [138]); higher use of information technology (positive [81, 136]; null [124, 134, 135]); higher staff meeting frequency (negative [134]; null [133]); administrative/clinical standardisation across a nursing home chain (null [94]); facility methods for communicating potential IC issues (null [133]); maintaining a list of service users with infection (null [133]); and association with other compliant facilities (null [137]).
Culture
Norms, values, and basic assumptions of a given organisation.
In the context of our research question we interpreted this construct to refer to institutional culture with an obvious relevance to regulatory compliance. A study of motivational postures towards regulation reported that facilities adopting a posture of disengagement and compliance were negatively associated whereas those with a culture of resistance to regulation were positively associated with compliance [41]. The authors surmised that this seemingly incongruous finding may be explained by an interaction with the inspectors’ regulatory style [41]. Two further determinants in this study were reported as having a null association with compliance: a culture of capture (high degree of cooperation with regulators) and of managerial accommodation (where management were cooperative and accepted responsibility for implementation) [41]. A similar study measured the perspectives of senior managers in NHs in terms of whether they ‘believed in the standards’ or exhibited a ‘subculture of resistance”; both were positively associated with compliance [137].
Organisations with a higher patient-centred culture and compliance were positively associated in three studies [103, 108, 143], with a fourth reporting a null association [142]. NHs that had a “culture change” focus and compliance were positively associated in two studies [140, 141]. One study investigated whether a NH’s culture of cooperation with a regulator was associated with compliance (null [137]).
Other factors included a culture that focused on reducing hospitalisation for residents (negative [133]) and culture change brought on by converting from a non-profit to for-profit facility (negative [178]). The strategic focus of a NH (e.g. attracting clients through higher quality/lower costs) was associated with compliance [144].
Implementation climate–tension for change
The degree to which stakeholders perceive the current situation as intolerable or needing change.
We interpreted this construct as including studies that investigated organisational drivers for improved compliance or the urgency with which changes in compliance levels were considered necessary by organisations. A qualitative study on efforts to reduce anti-psychotic medication in NHs reported staff felt pressure to fulfil regulatory requirements and improve their publicly-reported quality level [149]. There were mixed findings on the stringency of regulators: three studies [53, 115, 147] reported stricter enforcement and compliance was positively associated, four negatively [93, 115, 145, 146], and one [148] reported a null association (one study [115] reported determinants in the positive and negative categories).
Implementation climate–compatibility
The degree of tangible fit between meaning and values attached to the innovation by involved individuals, how those align with individuals’ own norms, values, and perceived risks and needs, and how the innovation fits with existing workflows and systems.
We took compatibility to mean the degree to which a regulatory measure fits with pre-existing practices in an organisation. One qualitative study featured here, where the author reported compliance was improved because the regulatory metric was compatible with the electronic health record system enabling “a coordinated…standardized approach to treating sepsis based on both policy requirements and clinical expertise. They also produce the documentation necessary for meeting and reporting on regulatory sepsis metrics” [18].
Implementation climate–relative priority
Individuals’ shared perception of the importance of the implementation within the organization.
This construct relates the implementation of regulations to how important a goal it is for those charged with achieving compliance. One study investigated a range of issues relating to an organisation’s perception of regulation, their estimation of the likelihood of non-compliance being detected, and the perceived severity of regulatory sanctions [45]. The perceived severity of withholding a funding increase and compliance was negatively associated; the remaining factors in this study (e.g. probability of: prosecution/state detection/withdrawal of licence) had a null association [45].
Implementation climate–learning climate
A climate in which: 1. Leaders express their own fallibility and need for team members’ assistance and input; 2. Team members feel that they are essential, valued, and knowledgeable partners in the change process; 3. Individuals feel psychologically safe to try new methods; and 4. There is sufficient time and space for reflective thinking and evaluation.
The authors of one qualitative study on high- and low-performing nursing homes (as measured by compliance levels) reported that high-performing nursing homes were characterised by management who actively encouraged staff participation in decision-making [131].
Readiness for implementation–leadership engagement
Commitment, involvement, and accountability of leaders and managers with the implementation of the innovation.
Organisations where management submit to an external quality assessment (e.g. voluntary accreditation) were more likely to be compliant in all four studies that investigated this [150–153]. A fifth study investigated hospital accreditation by the Joint Commission (negative [105]) and the Commission on Cancer (null [105]). The authors of a qualitative study reported a difference in leadership behaviours when comparing high- and low-performing NHs: “the leadership behaviours of the NHA [Nursing Home Administrator] and the DON [Director of Nursing] created a clear, explicit, and coherent mission, a strong sense of purpose, for the organisation. The importance of leadership relationship behaviours and the congruence of the stated and lived mission of the home were strikingly different between high- and low-performing homes” [131].
Other
Findings were placed in this section where they could not be coded to an appropriate construct but were still considered relevant to this domain. For example, while many studies may have investigated whether staffing levels were associated with compliance, they did not investigate staffing that were specifically dedicated to implementing regulations or achieving compliance.
Other: Staffing. Of the 29 studies examining registered nurse staffing, 19 reported higher levels of this staff grade and compliance were positively associated [14, 35, 49–51, 58, 59, 61, 93, 95, 108, 113, 114, 123, 143, 156, 158, 159, 161], nine reported a null association [15, 54, 63, 66, 96, 109, 122, 127, 154] and one reported a negative association [107]. Likewise, total nurse staffing levels (all grades of nurse staff) and compliance were positively associated in eleven studies [35, 47, 57, 60, 81, 83, 107, 126, 158, 161, 164], with two finding a negative association [61, 83] and three a null association [36, 72, 105]. The results were similar for nurse aides/care assistants: 15 studies reported higher levels these staff and compliance were positively associated [14, 34, 36, 47, 49, 51, 59–61, 93, 95, 126, 127, 143, 156, 158], nine reported a null association [15, 54, 63, 81, 82, 108, 114, 123, 159] and three reported a negative association [50, 57, 58]. A higher ratio of registered nurses as against other nurse and care staff and compliance was positively associated in four studies [97, 109, 113, 143] with a null association in a further four [35, 57, 59, 160]. Higher levels of licensed practitioner/vocational nurses and compliance were positively associated in five [47, 49, 50, 67, 156], negatively in five [57–60, 77], and a null association reported in 13 [14, 51, 54, 61, 63, 81, 82, 93, 108, 114, 123, 143, 158].
Higher specialist staff levels (e.g. dietary professionals) and compliance were positively associated in five studies [14, 34, 91, 156, 162], negatively in one [116]; and null in two [36, 57] NHs meeting state criteria for minimum staffing and compliance were positively associated in two studies [60, 161].
Among other staffing-related determinants were the following: higher total staffing levels (positive [91, 116]; null [52, 94, 122, 154]); higher proportion of trained staff (positive [91, 133]; negative [116]; null [94, 110]); higher agency/contract staff levels (negative [46, 143, 155]; null [154]); higher administrative staff levels (positive [14]; null [54]); higher housekeeping staff levels (null [14, 156]); higher food-service staff levels (null [156]); higher infection control professional quality (measured by certification level and training attainment)(null [134]); higher levels of trainee nurse aides (null [158]); and higher levels of certified medication aide staffing (null [158]).
In a qualitative study, the authors found high-performing nursing homes (as measured by compliance levels) had leaders who made adequate resources available to allow staff do their job [131]. Higher staff workload was associated with poorer compliance in two studies [84, 133].
Of the 19 studies that assessed staff turnover, 16 reported high staff turnover and compliance was negatively associated [52, 54, 76, 119, 133, 143, 154, 160, 163–169, 179] and three reported no association [97, 133, 134] (one study [133] had two measures of turnover with different associations and is counted in both the negative and null columns). Higher job satisfaction and compliance had a null association in one study [157]; nurse-aide absenteeism and compliance was negatively associated [132]. Two studies found higher ratings for work effectiveness and practice environments in NHs and compliance were positively associated [108, 120]. The degree of nursing centralisation in a NH and compliance had a null association [36]. A higher social services director caseload level and compliance was negatively associated [84].
Other: Financial. The majority of studies listed in this section were literature from the United States. Higher costs (most of which were expressed as costs per patient day in a NH context) and compliance were negatively associated in six studies [64, 76, 82, 130, 171, 173], four reported a null association [97, 106, 171, 172], and one a positive association [170] (One study [171] had cost determinants in both the negative and null categories). Services with higher proportions of publicly-funded service-users and compliance also tended to be negatively associated (six positive [13, 47, 62, 76, 90, 109]; 21 negative [14, 16, 34, 48, 49, 52, 57, 58, 64, 77, 80, 90–92, 95, 97, 104, 110, 113, 114, 116]; 16 null [13, 35, 36, 46, 50–52, 54, 59, 61, 66, 82, 86, 87, 106, 107]) (some studies investigated multiple different types of public funding and reported different associations with compliance. Therefore, these studies appear across more than one of the above categories). Three studies investigated the proportion of private-payers (positive [62]; negative [116]; null [128]). Staff salary levels and compliance had a null association [97].
Four studies investigated facility profit level/margin (positive [51, 175]; negative [13]; null [97]). One study reported a u-shaped finding where average financial performance was positively associated with compliance whereas both high and poor financial performance were negatively associated [176]. Higher facility income and compliance was positively associated in two studies [52, 110], with two reporting a null association [64, 172]. Facilities that provided finances to attend infection control training and compliance were positively associated [133], whereas there was a null association when providing funding for infection control meetings or access to expert consultation on infection control [133]. Higher facility market share and compliance was reported to be positively associated [174].
Other: Admissions. NHs or assisted-living facilities accepting Medicaid (a public health insurance program in the United States for people on low incomes) admissions and compliance were positively associated in three studies [35, 71, 83], a fourth reported a negative association [115], and a fifth a null association [80]. NHs accepting Medicare (a health insurance program in the United States generally for those over 65 or with specific conditions) admissions and compliance were positively associated in two studies [71, 104]. NH admission rate and compliance had a null association in two studies [82, 96]. Hospitals accepting critical access or rural referrals and compliance had a null association [86]. Higher occupancy levels and compliance had no consistent direction of association in 28 studies (eight positive [16, 58, 59, 63, 93, 106, 119, 154]; nine negative [46, 55, 57, 60, 61, 65, 91, 95, 113]; 11 null [47, 49–51, 54, 64, 82, 90, 92, 110, 126]).
Other: Ownership. Recently-acquired NHs and compliance were reported to have a negative [177] and null [93] association. Compliance was reported to improve in poor quality NHs that were acquired by a chain [177]. Where a NH was acquired by a chain, higher quality chains were positively associated with compliance [177].
Other: Infection control. Participation in an infection control collaborative focused on reducing MRSA and compliance was positively associated [133]; while other infection control collaborations had a null association [133, 134]. The types of resources used to determine and treat infection and compliance had a null association [133]. A study of additional job responsibilities for infection control staff reported that being Director/Assistant Director of Nursing and compliance was negatively associated, all other roles were reported as having a null association [133].
Other: Chains. Physical plant standardisation across a nursing home chain and compliance was positively associated [94].
Characteristics of individuals
This domain reflects how “individuals’ beliefs, knowledge, self-efficacy, and personal attributes” may impact the implementation of regulations. We found no determinants that could be coded to two of the five constructs in this domain: knowledge and beliefs about the innovation, and individual stage of change. In total, seven studies–the lowest for any domain–investigated a determinant coded to this domain (see Table 5).
Table 5. Determinants coded to the characteristics of individuals domain.
| Construct | Determinant |
|---|---|
| Knowledge & Beliefs about the Innovation | No studies |
| Self-efficacy | Blocked legitimate opportunities to comply [137] |
| Individual Stage of Change | No studies |
| Individual Identification with Organization | Higher job commitment [132, 137, 157] |
| Other Personal Attributes | Directors of nursing having a higher emotional connection with inspectors [137] Higher level of task expectation (a measure of staff familiarity and clarity with their roles) [103] |
| Other | Higher staff empowerment [84] Ranking of infection control activities in order of how time-consuming each were [133] Senior managers’ perception of what is important in job knowledge [180] |
Self-efficacy
Individual belief in their own capabilities to execute courses of action to achieve implementation goals.
Studies were included in this construct if they examined perceptions of capacity to implement regulations and its relationship to successful compliance. When nursing home managers felt that legitimate means of achieving compliance were blocked by owners, this was negatively associated with compliance [137].
Individual identification with organisation
A broad construct related to how individuals perceive the organization, and their relationship and degree of commitment with that organization.
Higher job commitment and compliance was positively associated in two studies [132, 157] and had a null association in a third [137].
Other personal attributes
A broad construct to include other personal traits such as tolerance of ambiguity, intellectual ability, motivation, values, competence, capacity, and learning style.
Any studies which reported on miscellaneous personal attributes and their association with compliance were coded here. Directors of nursing having a higher emotional connection with inspectors and compliance was positively associated [137]. A higher level of task expectation (a measure of staff familiarity and clarity with their roles) and compliance was negatively associated [103].
Other
Findings were placed in this section where they could not be coded to an appropriate construct but were still considered relevant to this domain.
The degree to which staff felt empowered to do their job and compliance was positively associated [84]. A study of infection control attitudes among NH staff asked respondents to rank a range of activities in order of how time-consuming each were. The ranking of vaccination (negative [133]) and infection control policy development (positive [133]) as highly-time consuming and compliance was associated, the remainder having a null association. Senior managers’ perception of what is important in job knowledge (e.g. leadership; resident care; human resources) and compliance had a null association [180].
Process
The process domain refers to “stages of implementation such as planning, executing, reflecting and evaluating, and the presence of key intervention stakeholders and influencers including opinion leaders, stakeholder engagement, and project champions” [30]. No studies were coded to six of the 10 constructs within the domain: planning; engaging–opinion leaders; engaging–formally appointed internal implementation leaders; engaging–champions; engaging–external change agents; engaging–innovation participants. In total, 17 studies investigated a determinant coded here (see Table 6).
Table 6. Determinants coded to the process domain.
| Construct | Determinant |
|---|---|
| Planning | No studies |
| Engaging | |
| Opinion Leaders | No studies |
| Formally Appointed Internal Implementation Leaders | No studies |
| Champions | No studies |
| External Change Agents | No studies |
| Key Stakeholders | Physician represented on the infection control committees [133] “Administrative personnel made decisions without involving the staff or residents affected by the change…Administration handed down a solution, without input…the social work department director was distressed when she was not included in the problem solving and resolution of a survey deficiency” [131] |
| Innovation Participants | No studies |
| Executing | “The data analysis for this study revealed challenges from different non-clinical departments regarding pushing person centered care policies but showed little to no negative impact on annual state survey results. Most participants responded that the department had great annual survey results after achieving Eden Alternative certification” [181] “One physician explained that she orders blood cultures on every patient of hers that comes through the emergency room because the sepsis metric requires that immediate cultures are documented” [18] “The dynamics described in this article reveal that the formal aspects of caring—those enacted by regulatory authorities—are superseded by material conditions, which can lead standards to be enacted discursively but practically inactivated…What is uncovered in this study is that compliance with various standards becomes feigned by the corporation just as policing is performed by the so-called independent regulators…In the case of social care, it may be that the primary intention of regulation is to give credence to the overall system and the accumulation of private enterprises that takes place by establishing the appearance of regulatory effort coupled with an illusion of corporate compliance” [31] “Participants recognized that there were many potential benefits of antipsychotic medication reduction with four primary themes: (d) Improvement in the facility Quality Indicator score (regulatory compliance)” [149] |
| Reflecting & Evaluating | “Clinicians felt inundated with pressure and performance evaluations that tracked their compliance with the sepsis metric” [18] |
| Other | Availability of corporate training across a nursing home chain [94] Facility has a mechanism for providing hand hygiene feedback to staff [133] Formal staff teams [108] Hand hygiene product used in facility [133] Higher degree of managerial control [45, 137] Higher level of consensus leadership by Directors of Nursing [132] Higher levels of antibiotic prescribing in nursing homes [133] Higher levels of management autonomy [45] Higher quality senior managers [76, 103, 110, 118, 133] Higher scores on hand hygiene audits [182] Methods to determine service user infection [133] More time spent on infection control activities [133] Providing quality indicator outcome information to nursing home managers [183] Self-managed staff teams [108] Training methods used for infection control [133] |
Engaging–key stakeholders
Individuals from within the organization that are directly impacted by the innovation, e.g., staff responsible for making referrals to a new program or using a new work process.
In this construct, compliance can be influenced by how key individuals in an organisation are affected, or consulted with, during the ongoing process of implementing regulations. In a qualitative study, the compliance of NHs was poor where management were reported to make decisions without involving other staff and residents: “Administration handed down a solution, without input…the social work department director was distressed when she was not included in the problem solving and resolution of a survey deficiency” [131]. Including physicians on infection control committees and compliance was positively associated [133].
Executing
Carrying out or accomplishing the implementation according to plan.
We regarded this construct quite broadly and included determinants that described how an organisation carried out its functions and which could reasonably be argued to have some bearing on the implementation of regulations.
Four qualitative studies feature in this construct. One author argued that the execution of regulation is a façade that masks poor quality care; a form of performative compliance in which both the regulator and regulatee are complicit in providing false public assurance [31]. A second qualitative study described how a physician developed a work-around for a metric: “ordering blood tests ahead of a confirmed sepsis diagnosis to ensure she doesn’t fail the metric later if the patient becomes septic” [18]. Compliance was also achieved as a consequence of implementing another intervention such as a reduction in anti-psychotic medication or the implementation of a more person-centred care model in NHs [149, 181].
Reflecting and evaluating
Quantitative and qualitative feedback about the progress and quality of implementation accompanied with regular personal and team debriefing about progress and experience.
Studies that investigated how the provision of feedback or information on the implementation of regulations impacted the process of implementation were coded here. The author of a qualitative study reported clinicians felt overburdened with performance evaluations, ultimately developing work-arounds and “gaming the system” in order to worry less about meeting the metric [18].
Other
Findings were placed in this section where they could not be coded to an appropriate construct but were still considered relevant to this domain.
A higher level of consensus leadership by Directors of Nursing and compliance was positively associated [132]. The availability of corporate training across a NH chain and compliance had a null association [94]. A higher degree of managerial control and compliance had positive [137] and null [45] associations in two different quantitative studies whereas higher levels of management autonomy and compliance were positively associated [45]. Having higher quality senior managers (as measured by educational attainment or years of experience) and compliance was positively associated in three studies [76, 103, 110], with two finding a null association [118, 133].
A study of infection control practices reported that, of five methods to determine resident infection, only one (using Centers for Disease Control definitions [184]) was positively associated with compliance, the remainder having a null association [133]. In the same study, whether a NH had a mechanism for providing hand hygiene feedback to staff, as well as the type of hand hygiene product used, and compliance, had null associations [133]. Training methods used for infection control, video-based training, face-to-face training and handouts/flyers and compliance all had null associations [133]. The time spent on infection control activities and compliance had a null association [133].
Self-managed staff teams and compliance were positively associated [108] whereas more formal staff teams had a null association [108]. Higher levels of antibiotic prescribing in nursing homes and compliance were negatively associated [133]. Higher scores on hand hygiene audits and compliance had a null association [182]. The provision of quality indicator outcome information to NH managers and compliance had a null association [183].
Discussion
The evidence base indicates that the following structural characteristics were positively associated with regulatory compliance: smaller facilities (as measured by bed capacity); higher nurse staffing levels; lower staff turnover. A facility’s geographic location was also strongly associated with compliance (Table 7). There was a paucity of evidence on the processes associated with successful implementation of regulations.
Table 7. Determinants of regulatory compliance where evidence is most consistent.
| Domain | Construct | Determinant | Associated* | Negative | Null | Positive |
|---|---|---|---|---|---|---|
| Inner setting | Other | Higher staff turnover | 16 | 3 | 0 | |
| Inner setting | Structural characteristics | Geographic location of facility | 13 | 1 | ||
| Inner setting | Structural characteristics | Larger size facility (bed number) | 40 | 16 | 3 | |
| Inner setting | Other | Higher total nursing staff | 2 | 3 | 11 | |
| Inner setting | Other | Higher registered nurse staffing | 1 | 9 | 19 |
* Denotes a nominal variable where a significant association was reported for one or more of those variables (e.g. federal states in Australia)
The evidence presented in this review was predominantly quantitative (n = 147, 94%), conducted in the United States (n = 140, 90%) and focused on NHs (n = 143, 91%). The observed focus on the structural attributes of compliant providers may be because these attributes were easier to measure and were available for quantitative analysis via routinely-collected data e.g. the Online Survey, Certification, And Reporting (OSCAR) database [185].
We find no other systematic review that has specifically focused on determinants of regulatory compliance in health and social care services. There are some reviews that used regulatory compliance as one of several outcome measures to evaluate associations between a specific structural or organisational characteristic (e.g. for-profit status [186] or service size [187] and quality). However, these studies were primarily interested in regulatory compliance as a proxy measure for quality while our review sought to identify structural or process determinants of compliance.
The processes that determined successful implementation of regulations (e.g. leadership engagement to ensure readiness for inspection) were much harder to map to routinely available data and were therefore harder to study. There were some CFIR constructs in the ‘process’ domain, which encompasses various stages of the implementation of an intervention such as ‘planning’, ‘engaging–innovation participants’ and ‘reflecting & evaluating’, to which we coded very few/no determinants. For example, we found no studies that investigated how organisations engaged in planning prior to the introduction of regulations.
We also coded few determinants to the ‘characteristics of individuals’ domain. Many of this domain’s constructs deal with the views, opinions and perceptions of individuals towards an intervention. Such constructs, by their nature, lend themselves to qualitative research in contrast to routinely available quantitative data. Therefore, our review reveals a clear gap in the evidence base and opportunities for future qualitative or mixed-methods studies on successful engagement with the regulatory process.
Facility characteristics
Our finding on facility size is in agreement with a similar review which investigated NH size and its relationship to quality [187]. Some have posited that staff attention and resources in larger facilities are directed towards health and quality of care outcomes at the expense of quality of life outcomes [188]. Larger facilities may also perform poorly with regard to broad quality measures (i.e. regulatory compliance) but better on individual quality indicators [187, 189]. Size may also interact with other facility characteristics that may impact on quality e.g. larger hospitals tend to be located in urban areas [190]. Facility size was also associated with staff turnover, where larger NHs have higher turnover, which may impact on quality [191]. We also found that high staff turnover was associated with compliance (see below).
Other studies have shown that for-profit facilities were associated with poorer compliance [186]; our findings are that 55% of studies reported a negative association. One explanation for the poorer performance may be that expenditures are minimised thereby resulting in fewer resources being directed towards care activities, which could in turn impact on compliance [186]. Not-for-profit facilities may be in a position to ‘cherry-pick’ clients (preferring people with minimal care needs and/or greater resources) whereas for-profit facilities may be more reliant on low-income clients with greater needs, thereby impacting on quality outcomes [74]. Higher process quality (e.g. leadership, training) in not-for-profit facilities may also be a mechanism through which higher quality is achieved [103].
Health service chains (mostly in the NH sector) have been the subject of considerable research with respect to quality, generally reporting a negative association [192–194]. We did not replicate this finding: 45% of studies in our review also reported a negative association but 26% reported a positive association and 29% a null association. Chain ownership accounts for varying proportions of the market across jurisdictions (e.g. in 2014, 64% of NHs were owned/operated by chains in the United Kingdom whereas the figure was 17% in Sweden and Canada) [192]. One possible explanatory mechanism is the association between chain status and lower rates of nurse staffing [16, 195], potentially impacting on a facility’s compliance capability. The pursuit of corporate interests may also diminish resources [196], thereby affecting compliance. Some have cautioned that the literature on chain facilities tends to treat all chains equally, whereas there may be important differences in terms of chain size and ownership [196].
The association between occupancy levels and quality is also a facility characteristic subject to much research [197–200]. High occupancy levels (typically regarded as >90%) and overcrowding in hospitals have been associated with higher mortality [198, 201] and higher incidence of healthcare associated infections [202]. We found no clear association between occupancy and compliance. This is surprising as lower occupancy has been associated with poorer financial performance in nursing homes [203] and higher use of antipsychotic medication [200], which one might expect to also impact compliance. Given most studies in our review were set in NHs, it may be that NH compliance levels are less sensitive to occupancy compared to hospitals.
Staffing
We find high staff turnover to be strongly associated with poorer compliance. A circular relationship may be evident here: poor quality care precipitates staff dissatisfaction and vice versa [191]. The high costs related to staff turnover [204] may impact on an organisation’s compliance levels. High turnover rates have also been associated with poor implementation of evidence-based practices [205], thereby providing another potential causal mechanism for poorer compliance.
There was robust evidence that higher nurse staffing levels are associated with higher compliance. This finding is concordant with previous studies investigating nurse staffing levels and quality in hospitals [206–209] and NHs [200, 210, 211], albeit that some report inconclusive findings [212]. Some studies draw a distinction with respect to nurse type, finding registered nurses had a greater impact on quality when compared with licensed vocational nurses [200, 207, 208], a finding replicated in our review. Higher nurse staffing levels may be associated with quality when measures were nurse-sensitive outcomes (e.g. cardiac arrest, unplanned extubation) [206]. Lower nurse staffing levels may result in frontline care being provided by less-qualified staff which impacts on quality [208]. Higher levels of registered nurse staffing have been associated with lower antipsychotic medication use in NHs [200], which is also often a quality measure subject to regulation in these settings [213, 214]. Potential interaction effects with other staff-related measures (e.g. turnover, agency staff) have led some to argue that simply measuring nurse staffing levels is insufficient in terms of explaining the relationship to quality [215].
Demographics
We find that the geographic location of a facility was strongly associated with compliance. Most studies that investigated this were interested in multiple other factors and were usually at national-level; the geographic location may have been different cities or states in America or Australia (as distinct from urban/rural or population density). It is likely that location was interacting with multiple other variables producing this association. One obvious explanation is inconsistent regulation, for which there is evidence across a range of industries [216–219]. The level of public funding available across regions can also differ substantially, thereby impacting the resources available for compliance [220, 221]. Geographic location is associated with health service availability [222], medically underserved populations [223] and NH use of antipsychotic medication [200], each of which may have implications for compliance.
Our findings indicate no clear association of service-users with more complex or resource-intensive needs, or populations with a more challenging profile (e.g. older, sicker or poorer) and compliance. This is somewhat surprising as there is evidence to suggest these populations have generally poorer access to quality healthcare. For example, facilities in severely-deprived neighbourhoods have lower staffing levels [224]. Moreover, greater resourcing is required for service users with higher acuity [225], which one might argue limits the resources available for compliance.
We found some evidence relevant to the processes by which implementation of regulations becomes ‘normalised’ within organisations. For example, the degree to which regulatory requirements were compatible with existing work practices was important [18]. Some studies in our review reported that habitually producing good documentation to substantiate regulatory compliance was also important (albeit that this was geared more towards ‘gaming the system’ as opposed to achieving the goals of regulation) [18, 31]. The above findings were echoed in studies relying on normalisation process theory (NPT) to evaluate implementation efforts. For example, in a study using NPT to evaluate the implementation of a regulatory intervention for individual doctors, the authors discussed how successful implementation was influenced by compatibility with existing practices and good documentation/record-keeping [226]. The process of interaction between regulator and regulatee also appears to influence the compliance outcome [33, 41, 137].
There was a very limited literature investigating behaviours of regulatory staff and their responses to varying levels of compliance. However, there was evidence that regulation was sometimes implemented poorly by regulators, thereby giving a false measure of compliance. For example, by inspectors effectively turning a blind eye [32], services finding workarounds [18], or the entire system of regulation representing a performative means by which to draw a veil over poor care practices [31]. There are two relevant issues here. Firstly, there are multiple examples in a range of industries where a public scandal erupts, implicating the regulator [227–229]. Poor implementation of regulations by a regulator (through mechanisms such as regulatory capture or incompetence) can have potentially serious consequences for the public good. Secondly, the circumvention of regulatory prescriptions (e.g. by workarounds or misleading documentation) is similar in nature to ‘ritualism’ [17]. Here, organisations engage in a subtle rejection of regulatory goals by ‘playing the game’ typified in the following example: “an Australian director of nursing…did not want to oppose an inspection team who ‘made a big heap out of ethnic diet’ under an Australian standard that requires sensitivity to cultural preferences for different types of food: ‘So we bought ethnic diet books…give it a foreign name and they’ll be happy’” [17]. This is compliance in name only and can mean that regulatory goals such as safety or person-centred care are not met.
There is an extensive literature on compliance theory which seeks to explicate compliance at the level of individuals, organisations and nation states across various regulated contexts such as tax [230, 231], transport [232, 233] and environmental protection [234, 235]. There are four conceptual themes that seek to explain compliance: “motives, organizational capacities and characteristics, regulation and enforcement, and social and economic environments (or institutions)” [236]. Motives include the pursuit of material (e.g. profit or limiting costs), emotional (fear of admonishment, anger) or normative (to act appropriately, do the right thing) goals [12]. Organisational capacity refers to the differences between organisations in terms of economic resources, knowledge and expertise [236]. Regulation and enforcement draws attention to the various strategies and styles adopted by regulators and how these influence compliance behaviour [236]. Finally, compliance can be affected by the wider environment (e.g. political, economic or social) such as when a regulator leverages public pressure through ‘naming and shaming’ [237].
There are two broad empirical approaches evident in the literature on compliance theory: objectivist and interpretive [236]. Objectivist efforts at explaining compliance test theories by regarding compliance as the dependent variable and seeking associations with specific independent variables. The interpretive school is more concerned with how compliance is socially constructed and contested: “The research task shifts from mapping ‘compliance’ and ‘noncompliance’…to describing and understanding a whole range of organizational perceptions of, and behavioural responses to, regulation” [236].
Within the literature on compliance theory (which we searched separately) we found very few studies that sought to describe determinants of compliance in organisations within whole industries (e.g. banking or manufacturing). Rather, studies tended to focus on individual organisations [238] or were ethnographies that described how organisations/people engaged with regulation [239]. One review of financial regulation sought to identify organisational determinants of compliance [240]. The only statistically significant finding related to ownership structure: firms with a high separation of ownership from control (the degree to which board and shareholder power are separated) and family-owned firms were associated with higher compliance [240].
The lack of wide-ranging reviews make it difficult to situate our study within the wider literature on compliance theory. Some reflection on our findings in the light of the four conceptual themes and two empirical approaches outlined above may be useful. The studies in our review were located mostly within the organisational capacities and characteristics conceptual theme. These were largely objectivist in nature and identified variables that may be associated with compliance (e.g. staff levels, local demographics). There were only small numbers of studies that could be described as relevant for each of the other themes: motives; regulation and enforcement; and environment. Thus, the interpretive approach (which often relies on qualitative means of enquiry [236]) was largely absent from our review, representing a significant gap in the literature.
Our findings, particularly those that are supported by findings of other reviews, have important implications. Several modifiable organisational characteristics such as facility size and nurse staffing levels merit attention by policy makers, particularly in the context of NH design.
The inequity highlighted in the finding of poorer compliance for service users with higher needs and less resources (although not reaching our >60% threshold) is another reminder of the importance of the socio-economic determinants of health [241]. This represents a real challenge for regulators because while these populations deserve parity in terms of care quality, regulatory sanctions could potentially further diminish quality by diverting time/resources away from care. Regulators may need to be cognisant of this issue, especially during times of economic uncertainty and pressure on public spending [242].
The design of regulatory interventions and their subsequent implementation could be informed by the application of implementation science. For example, regulatory impact analysis—an increasingly common process undertaken prior to the introduction of regulation [243]—could potentially benefit from identifying implementation barriers or facilitators.
There was an expectation on behalf of the authors that a larger number of qualitative studies would be found. There is an extensive field of qualitative enquiry on the implementation of other aspects of quality in health and social care such as clinical guidelines [244, 245], quality improvement initiatives [246, 247], patient feedback [248, 249], and professional regulation [250]. Moreover, the regulation and compliance literature is replete with qualitative studies of organisational responses to regulation, yet very few examine organisations working in health and social care [236]. The relative absence of studies on the implementation of regulatory standards and how this is linked to compliance is therefore puzzling and represents a gap in the literature. It may be the case that regulators are seen as a “remote disembodied agent” due to infrequent contact with managers and frontline staff, therefore being overlooked as a potential field of enquiry in implementation science [251].
Multiple avenues for future research arise from our findings. Firstly, the causal mechanisms for some determinants of compliance warrant deeper investigation across a range of contexts and settings. For example, while we find that larger facilities were associated with poorer compliance, some studies have found a positive association of quality and size [200, 252]. It may be that associations between facility size and quality differ depending on the quality measure assessed and further research may be able to address this matter.
Secondly, the ‘regulatory character’ of one setting/context can differ significantly to another: “findings from any one study need to be assessed in light of the particular jurisdiction and regulatory regime in question” [253]. Therefore, given the extensive body of research from the United States and in NHs, research focused on other countries and other settings could prove instructive.
Thirdly, the heavy focus on objectivist approaches could be complemented by more interpretive and qualitative research. For example, one may wish to understand how the behaviour of organisations (and individuals within those organisations) during regulatory encounters impacts on the compliance outcome, building on contemporary work in other settings [254].
Finally, there may be merit in exploring the utility of various implementation strategies that could potentially address barriers to regulatory compliance. For example, certain Expert Recommendations for Implementing Change (ERIC) strategies have been identified as most appropriate for addressing specific CFIR constructs [255]. Consideration of various implementation strategies could also inform a regulator’s approach to inspection and enforcement practices.
Strengths and limitations
A strength of this review is the application of a systematic, wide-ranging search that offered the best opportunity of identifying relevant literature. A published protocol guided the process and provided methodological rigour [26]. The authors are not aware of any other systematic review which focused specifically on regulatory compliance in health and social care services. In addition, the conceptualisation of regulation as an intervention, thereby facilitating use of the CFIR and implementation science more generally, is novel.
The ability to draw generalisable conclusions in this review is limited by the preponderance of literature focusing on NHs in the United States. Other settings like hospitals, and other jurisdictions, are relatively absent in the literature. A further weakness in the evidence base is the reliance on observational designs which means causal inferences have to be tentative. We also draw attention to the mixed quality of the included studies as a limitation. Many studies relied on self-reported measures which could not be objectively verified. For example, many studies involving nursing homes relied on staffing levels as reported in the OSCAR database, which has been shown to be inconsistent when compared with other data sources [256].
A further limitation of our review is the heterogeneity of regulations used across the included studies. The heterogeneity is found both among studies (e.g. where one may focus specifically on infection control and another may cover a broad basket of regulations) and also in the diversity of regulatory frameworks across jurisdictions. It is likely that determinants vary in their importance depending on the specific regulation in question and the nature (e.g. timeliness, use of sanctions) of the regulatory relationship. This limits our ability to generalise about the importance of different determinants of compliance.
We considered a number of framework options for structuring our review. While we considered other options such as Normalisation Process Theory [257] and the Practical Robust Implementation and Sustainability Model (PRISM) [258], we ultimately chose to use the CFIR as it provided a comprehensive framework that encompassed both organisational and individual-level implementation features.
One might question whether regulation was a good fit for study under implementation science and the CFIR. Regulation can hardly be regarded as an ‘innovation’—it is not new. Moreover, the ‘ongoing’ nature of regulation makes it different to other, more common, interventions which are perhaps time-limited [259, 260] or intended to be introduced and then subsumed (normalised) by an organisation [261, 262]. We encountered some coding difficulties with the CFIR, which perhaps reflects that initial implementation of an intervention and continuous quality assurance (i.e. regulation) are distinct. For example, organisations are required to implement and sustain regulatory standards on an ongoing basis, and have that monitored by a third-party (the regulator) at often random intervals. Such an intervention feature (i.e. sustainability and external evaluation) has no natural home within the CFIR. Nevertheless, we were satisfied that the CFIR provided a useful framework within which to evaluate regulation as an intervention.
There has been an acknowledgment that the CFIR has a blind spot in terms of implementation sustainability [263], indeed a revision to CFIR was recently published [264]. Discussions on CFIR utilisation in various contexts have also highlighted a need to differentiate between innovation and implementation outcomes [263]. In this review we regarded compliance as an implementation outcome: i.e. the degree to which organisations successfully implemented regulations. Similarly, we regarded determinants as constituting implementation determinants which predicted or explained actual implementation outcomes. Authors using the CFIR are encouraged to reflect on three questions which we have addressed in S1 Text.
Conclusion
This review sought to identify and describe determinants of regulatory compliance. The multiplicity of determinants identified illustrates how regulatory compliance is a complex and context-specific phenomenon. There were some structural characteristics of organisations that showed an association with compliance. It is difficult to draw conclusive causal relationships and further research should attempt to better understand these mechanisms.
Regarding regulation as an intervention and using the CFIR as a framework offered some useful insights into the structures and processes that produce compliance. The uneven distribution of determinants across the five CFIR domains demonstrates that the literature included in this review tends to draw on objectivist approaches.
There were only a small number of studies in this review that were qualitative and could be described as using an interpretive approach to understand compliance determinants. While such studies exist in other fields of regulation and compliance research, they are relatively absent in the context of health and social care and represent a gap in the literature.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(XLSX)
(DOCX)
(XLSX)
Acknowledgments
The authors wish to acknowledge the valuable contribution of Fiona Barry, University College Cork, Ireland in contributing to the quality assessment component of this systematic review.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This review comprises part of a PhD study funded by the Health Information and Quality Authority (Ireland). This research was conducted as part of the Structured Population health, Policy and Health-services Research Education (SPHeRE) programme (Grant No. SPHeRE/2019/1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hickey EC, Young GJ, Parker VA, Czarnowski EJ, Saliba D, Berlowitz DR. The effects of changes in nursing home staffing on pressure ulcer rates. Journal of the American Medical Directors Association. 2005; 6(1): 50–3. Available from: https://www.sciencedirect.com/science/article/pii/S1525861004000040. doi: 10.1016/j.jamda.2004.12.003 [DOI] [PubMed] [Google Scholar]
- 2.Kovach CR, Taneli Y, Neiman T, Dyer EM, Arzaga AJA, Kelber ST. Evaluation of an ultraviolet room disinfection protocol to decrease nursing home microbial burden, infection and hospitalization rates. BMC infectious diseases. 2017; 17(1): 1–8. Available from: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-017-2275-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, et al. Mortality after surgery in Europe: a 7 day cohort study. The Lancet. 2012; 380(9847): 1059–65. Available from: https://www.sciencedirect.com/science/article/pii/S0140673612611489. doi: 10.1016/S0140-6736(12)61148-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mukamel DB, Haeder SF, Weimer DL. Top-down and bottom-up approaches to health care quality: the impacts of regulation and report cards. Annual review of public health. 2014; 35: 477–97. Available from: https://www.annualreviews.org/doi/full/10.1146/annurev-publhealth-082313-115826. [DOI] [PubMed] [Google Scholar]
- 5.Selznick P. Focusing organisational research on regulation. In: Noll Roger G., (Ed). Regulatory policy and the social sciences. Berkeley: University of California Press; 1985. p. 363–8. [Google Scholar]
- 6.Centers for Medicare and Medicaid Services. Part 483—Requirements for States and Long Term Care Facilities 2022. Available from: https://www.ecfr.gov/current/title-42/chapter-IV/subchapter-G/part-483/subpart-B Accessed on: 4/11/2022
- 7.Healthcare Improvement Scotland. Inspecting and regulating care 2022. Available from: https://www.healthcareimprovementscotland.org/our_work/inspecting_and_regulating_care.aspx Accessed on: 25/7/2022
- 8.Ministry of Long-Term Care. Long-term care home quality inspection program: Ministry of Long-Term Care; 2022. Available from: https://www.health.gov.on.ca/en/public/programs/ltc/31_pr_inspections.aspx Accessed on: 25/7/2022
- 9.Australian Commission on Safety and Quality in Health Care. Assessment to the NSQHS Standards: Australian Commission on Safety and Quality in Health Care; 2022. Available from: https://www.safetyandquality.gov.au/standards/nsqhs-standards/assessment-nsqhs-standards Accessed on: 25/7/2022
- 10.Australian Commission on Safety and Quality in Health Care. Australian health service safety and quality accreditation scheme: Australian Commission on Safety and Quality in Health Care,; 2022. Available from: https://www.safetyandquality.gov.au/our-work/accreditation/australian-health-service-safety-and-quality-accreditation-scheme Accessed on: 25/7/2022
- 11.Shaw CD, Braithwaite J, Moldovan M, Nicklin W, Grgic I, Fortune T, et al. Profiling health-care accreditation organizations: an international survey. International Journal for Quality in Health Care. 2013; 25(3): 222–31. Available from: 10.1093/intqhc/mzt011. [DOI] [PubMed] [Google Scholar]
- 12.Etienne J. Compliance theory: A goal framing approach. Law & Policy. 2011; 33(3): 305–33. Available from: https://www.researchgate.net/profile/Julien_Etienne/publication/227647055_Compliance_Theory_A_Goal_Framing_Approach/links/5e47026f458515072d9db840/Compliance-Theory-A-Goal-Framing-Approach.pdf. [Google Scholar]
- 13.O’Neill C, Harrington C, Kitchener M, Saliba D. Quality of care in nursing homes: An analysis of relationships among profit, quality, and ownership. Medical care. 2003: 1318–30. Available from: https://www.jstor.org/stable/3768307. doi: 10.1097/01.MLR.0000100586.33970.58 [DOI] [PubMed] [Google Scholar]
- 14.Harrington C, Zimmerman D, Karon SL, Robinson J, Beutel P. Nursing home staffing and its relationship to deficiencies. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2000; 55(5): S278–S87. Available from: https://academic.oup.com/psychsocgerontology/article/55/5/S278/536413. [DOI] [PubMed] [Google Scholar]
- 15.Hyer K, Thomas KS, Branch LG, Harman JS, Johnson CE, Weech-Maldonado R. The influence of nurse staffing levels on quality of care in nursing homes. The Gerontologist. 2011; 51(5): 610–6. Available from: https://academic.oup.com/gerontologist/article/51/5/610/595828. doi: 10.1093/geront/gnr050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harrington C, Olney B, Carrillo H, Kang T. Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Services Research. 2012; 47(1pt1): 106–28. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3447240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Braithwaite J. The nursing home industry. Crime and Justice. 1993; 18: 11–54. [Google Scholar]
- 18.Winslow R. Failing the metric but saving lives: The protocolization of sepsis treatment through quality measurement. Social Science & Medicine. 2020; 253: 112982. Available from: https://www.sciencedirect.com/science/article/pii/S027795362030201X. doi: 10.1016/j.socscimed.2020.112982 [DOI] [PubMed] [Google Scholar]
- 19.Rapport F, Clay‐Williams R, Churruca K, Shih P, Hogden A, Braithwaite J. The struggle of translating science into action: foundational concepts of implementation science. Journal of evaluation in clinical practice. 2018; 24(1): 117–26. Available from: https://onlinelibrary.wiley.com/doi/pdf/10.1111/jep.12741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farahnak LR, Ehrhart MG, Torres EM, Aarons GA. The influence of transformational leadership and leader attitudes on subordinate attitudes and implementation success. Journal of Leadership & Organizational Studies. 2020; 27(1): 98–111. Available from: https://journals.sagepub.com/doi/pdf/10.1177/1548051818824529. [Google Scholar]
- 21.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science. 2009; 4(1): 1–15. Available from: https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan PS-f, Fang Y, Wong MC-s, Huang J, Wang Z, Yeoh EK. Using Consolidated Framework for Implementation Research to investigate facilitators and barriers of implementing alcohol screening and brief intervention among primary care health professionals: a systematic review. Implementation science. 2021; 16(1): 1–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bevan G, Hood C. What’s measured is what matters: targets and gaming in the English public health care system. Public administration. 2006; 84(3): 517–38. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1467-9299.2006.00600.x. [Google Scholar]
- 24.Browne J, Bullock A, Poletti C, Cserző D. Recent research into healthcare professions regulation: a rapid evidence assessment. BMC health services research. 2021; 21(1): 1–12. Available from: https://link.springer.com/article/10.1186/s12913-021-06946-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quick O. A scoping study on the effects of health professional regulation on those regulated. 2012. Available from: https://www.professionalstandards.org.uk/docs/default-source/publications/research-paper/study-on-the-effects-of-health-professional-regulation-on-those-regulated-2011.pdf.
- 26.Dunbar P, Browne JP, O’Connor L. Determinants of regulatory compliance in health and social care services: a systematic review protocol. HRB Open Research. 2021; 4. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8258703.3/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Covidence systematic review software. Melbourne, Australia: Veritas Health Innovation; 2022. [Google Scholar]
- 28.Joanna Briggs Institute. Critical Appraisal Tools [Online]. 2020. Available from: https://joannabriggs.org/critical-appraisal-tools Accessed on: 4/11/2022
- 29.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information. 2018; 34(4): 285–91. Available from: https://escholarship.mcgill.ca/downloads/v118rj210. [Google Scholar]
- 30.Safaeinili N, Brown‐Johnson C, Shaw JG, Mahoney M, Winget M. CFIR simplified: Pragmatic application of and adaptations to the Consolidated Framework for Implementation Research (CFIR) for evaluation of a patient‐centered care transformation within a learning health system. Learning health systems. 2020; 4(1): e10201. Available from: https://onlinelibrary.wiley.com/doi/pdf/10.1002/lrh2.10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greener J. Performative compliance and the state–corporate structuring of neglect in a residential care home for older people. Critical Criminology. 2019: 1–18. Available from: https://link.springer.com/article/10.1007/s10612-019-09467-3. [Google Scholar]
- 32.Gil AP. Quality procedures and complaints: nursing homes in Portugal. The Journal of Adult Protection. 2019; 21(2): 126–43. Available from: https://www.researchgate.net/profile/Ana-Gil-18/publication/331658790_Quality_procedures_and_complaints_nursing_homes_in_Portugal/links/5c925419a6fdccd4602cce2c/Quality-procedures-and-complaints-nursing-homes-in-Portugal.pdf. [Google Scholar]
- 33.Makkai T, Braithwaite J. Reintegrative shaming and compliance with regulatory standards. Criminology. 1994; 32(3): 361–85. [Google Scholar]
- 34.Smith KM, Thomas KS, Johnson S, Meng H, Hyer K. Dietary service staffing impact nutritional quality in nursing homes. Journal of Applied Gerontology. 2019; 38(5): 639–55. Available from: https://journals.sagepub.com/doi/abs/10.1177/0733464816688309. [DOI] [PubMed] [Google Scholar]
- 35.Dellefield ME. Organizational correlates of the risk-adjusted pressure ulcer prevalence and subsequent survey deficiency citation in California nursing homes. Research in Nursing & Health. 2006; 29(4): 345–58. Available from: https://www.academia.edu/download/49070947/nur.2014520160923-4657-1c1dzkz.pdf. doi: 10.1002/nur.20145 [DOI] [PubMed] [Google Scholar]
- 36.Dellefield ME. Predictors of quality of care in California nursing homes: University of California, Los Angeles; 1999. https://search.proquest.com/openview/86e20c088eb8f9071e9ee3135822c606/1?pq-origsite=gscholar&cbl=18750&diss=y [Google Scholar]
- 37.Flores C. The quality of care in residential care facilities for the elderly [Ph.D.]. Ann Arbor: University of California, San Francisco; 2007. https://sigma.nursingrepository.org/handle/10755/19343
- 38.Lee RH, Gajewski BJ, Thompson S. Reliability of the nursing home survey process: A simultaneous survey approach. The Gerontologist. 2006; 46(6): 772–9. Available from: https://academic.oup.com/gerontologist/article-abstract/46/6/772/584650. doi: 10.1093/geront/46.6.772 [DOI] [PubMed] [Google Scholar]
- 39.Lin MK, Kramer AM. The quality indicator survey: Background, implementation, and widespread change. Journal of Aging & Social Policy. 2013; 25(1): 10–29. Available from: https://www.tandfonline.com/doi/abs/10.1080/08959420.2012.705721. [DOI] [PubMed] [Google Scholar]
- 40.Delaney CM, Rafalson L, Fiedler RC, Hernick JI. Quality indicator survey versus traditional survey in New York State: a comparison of results from annual nursing home surveys. Journal of Aging & Social Policy. 2018; 30(2): 127–40. Available from: https://www.tandfonline.com/doi/abs/10.1080/08959420.2017.1406838. [DOI] [PubMed] [Google Scholar]
- 41.Braithwaite V, Braithwaite J, Gibson D, Makkai T. Regulatory styles, motivational postures and nursing home compliance. Law & Policy. 1994; 16(4): 363–94. [Google Scholar]
- 42.Spector WD, Drugovich ML. Reforming nursing home quality regulation: Impact on cited deficiencies and nursing home outcomes. Medical care. 1989: 789–801. [DOI] [PubMed] [Google Scholar]
- 43.Weske U, Boselie P, van Rensen E, Schneider M. Physician compliance with quality and patient safety regulations: The role of perceived enforcement approaches and commitment. Health services management research. 2019; 32(2): 103–12. Available from: https://journals.sagepub.com/doi/abs/10.1177/0951484818813324. [DOI] [PubMed] [Google Scholar]
- 44.Ehlers LH, Simonsen KB, Jensen MB, Rasmussen GS, Olesen AV. Unannounced versus announced hospital surveys: a nationwide cluster-randomized controlled trial. International Journal for Quality in Health Care. 2017; 29(3): 406–11. Available from: https://academic.oup.com/intqhc/article-pdf/29/3/406/24325405/mzx039.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Braithwaite J, Makkai T. Testing an expected utility model of corporate deterrence. Law & Society Review. 1991; 25: 7. Available from: https://www.academia.edu/download/39989026/Testing_An_Expected_Utility_Model_If_Cor20151113-6135-1rceo9d.pdf. [Google Scholar]
- 46.Lu SF, Lu LX. Do mandatory overtime laws improve quality? Staffing decisions and operational flexibility of nursing homes. Management Science. 2017; 63(11): 3566–85. Available from: https://www.researchgate.net/profile/Lauren-Lu-2/publication/307088031_Do_Mandatory_Overtime_Laws_Improve_Quality_Staffing_Decisions_and_Operational_Flexibility_of_Nursing_Homes/links/58d0075a92851c5009efd4da/Do-Mandatory-Overtime-Laws-Improve-Quality-Staffing-Decisions-and-Operational-Flexibility-of-Nursing-Homes.pdf. [Google Scholar]
- 47.Castle N, Wagner L, Ferguson J, Handler S. Hand hygiene deficiency citations in nursing homes. Journal of Applied Gerontology. 2014; 33(1): 24–50. Available from: https://www.academia.edu/download/44005338/24.full.pdf. doi: 10.1177/0733464812449903 [DOI] [PubMed] [Google Scholar]
- 48.White C. Medicare’s prospective payment system for skilled nursing facilities: Effects on staffing and quality of care. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2005; 42(4): 351–66. Available from: https://journals.sagepub.com/doi/pdf/10.5034/inquiryjrnl_42.4.351. [DOI] [PubMed] [Google Scholar]
- 49.Castle NG, Wagner LM, Ferguson-Rome JC, Men A, Handler SM. Nursing home deficiency citations for infection control. American Journal of Infection Control. 2011; 39(4): 263–9. Available from: https://www.sciencedirect.com/science/article/pii/S0196655311001118. doi: 10.1016/j.ajic.2010.12.010 [DOI] [PubMed] [Google Scholar]
- 50.Wagner LM, Mcdonald SM, Castle NG. Nursing home deficiency citations for physical restraints and restrictive side rails. Western Journal of Nursing Research. 2013; 35(5): 546–65. Available from: https://journals.sagepub.com/doi/abs/10.1177/0193945912437382. [DOI] [PubMed] [Google Scholar]
- 51.Sharma H, Xu L. Nursing home profit margins and citations for infection prevention and control. Journal of the American Medical Directors Association. 2021. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/pmc8079226/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Collier EJ. Quality of care & California nursing homes: The effects of staffing, organizational, resident and market characteristics [Ph.D]. San Francisco: University of California; 2008. https://search.proquest.com/openview/f69868ebcee935d3d3c828b16034eddf/1?pq-origsite=gscholar&cbl=18750
- 53.Hawks BA. The regulation of US nursing homes: An examination of state and federal tools and their effect on providers’ performance [Ph.D]. Washington D.C.: American University; 2018. https://www.proquest.com/docview/2115472636?pq-origsite=gscholar&fromopenview=true
- 54.Castle NG, Engberg J. Staff turnover and quality of care in nursing homes. Medical care. 2005: 616–26. Available from: https://www.jstor.org/stable/3768180. doi: 10.1097/01.mlr.0000163661.67170.b9 [DOI] [PubMed] [Google Scholar]
- 55.Harrington C, Mullan JT, Carrillo H. State nursing home enforcement systems. Journal of health politics, policy and law. 2004; 29(1): 43–74. Available from: https://www.researchgate.net/profile/Charlene-Harrington/publication/8673154_State_Nursing_Home_Enforcement_Systems/links/5673111d08aee7a427436e61/State-Nursing-Home-Enforcement-Systems.pdf. doi: 10.1215/03616878-29-1-43 [DOI] [PubMed] [Google Scholar]
- 56.Lu SF, Serfes K, Wedig G, Wu B. Does competition improve service quality? The case of nursing homes where public and private payers coexist. Management Science. 2021. Available from: https://pubsonline.informs.org/doi/abs/10.1287/mnsc.2020.3806. [Google Scholar]
- 57.Castle NG, Myers S. Mental health care deficiency citations in nursing homes and caregiver staffing. Administration and Policy in Mental Health and Mental Health Services Research. 2006; 33(2): 215–25. Available from: https://link.springer.com/article/10.1007/s10488-006-0038-2. [DOI] [PubMed] [Google Scholar]
- 58.Castle NG, Wagner LM, Ferguson JC, Handler SM. Nursing home deficiency citations for safety. Journal of Aging & Social Policy. 2010; 23(1): 34–57. Available from: https://www.tandfonline.com/doi/pdf/10.1080/08959420.2011.532011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McDonald SM, Wagner LM, Castle NG. Staffing-related deficiency citations in nursing homes. Journal of Aging & Social Policy. 2013; 25(1): 83–97. Available from: https://www.tandfonline.com/doi/abs/10.1080/08959420.2012.705696. [DOI] [PubMed] [Google Scholar]
- 60.Kim H. A longitudinal study of the relationship between nurse staffing and quality of care in nursing homes [Ph.D.]. New York: New York University; 2006. https://www.proquest.com/docview/304905820?parentSessionId=%2B7yLik2iwfFu1qXutBXZXZqWoL1IdyGnhyAO7dfZ5PI%3D&pq-origsite=summon&accountid=14504
- 61.Wesson KW, Donohoe KL, Patterson JA. CMS mega-rule update and the status of pharmacy-related deficiencies in nursing homes. Journal of Applied Gerontology. 2020: 1617–27. Available from: https://journals.sagepub.com/doi/abs/10.1177/0733464820967589. [DOI] [PubMed] [Google Scholar]
- 62.Konetzka RT, Yi D, Norton EC, Kilpatrick KE. Effects of Medicare payment changes on nursing home staffing and deficiencies. Health Services Research. 2004; 39(3): 463–88. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/pmc1361020/. doi: 10.1111/j.1475-6773.2004.00240.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Castle NG. Nursing home deficiency citations for abuse. Journal of Applied Gerontology. 2011; 30(6): 719–43. Available from: https://journals.sagepub.com/doi/abs/10.1177/0733464810378262. [DOI] [PubMed] [Google Scholar]
- 64.Nyman JA. Excess demand, the percentage of Medicaid patients, and the quality of nursing home care. Journal of Human Resources. 1988: 76–92. Available from: https://www.jstor.org/stable/145845. [Google Scholar]
- 65.Wang X, Gammonley D, Bender F. Civil money penalty enforcement actions for quality deficiencies in nursing homes. The Gerontologist. 2020; 60(5): 868–77. Available from: https://academic.oup.com/gerontologist/article-abstract/60/5/868/5685410. doi: 10.1093/geront/gnz180 [DOI] [PubMed] [Google Scholar]
- 66.Kelly CM, Liebig PS, Edwards LJ. Nursing home deficiencies: An exploratory study of interstate variations in regulatory activity. Journal of Aging & Social Policy. 2008; 20(4): 398–413. Available from: https://www.tandfonline.com/doi/abs/10.1080/08959420802131817. [DOI] [PubMed] [Google Scholar]
- 67.Cohen CC, Engberg J, Herzig CTA, Dick AW, Stone PW. Nursing homes in states with infection control training or infection reporting have reduced infection control deficiency citations. Infection Control & Hospital Epidemiology. 2015; 36(12): 1475–6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4658225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Park J, Stearns SC. Effects of state minimum staffing standards on nursing home staffing and quality of care. Health Services Research. 2009; 44(1): 56–78. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2669632. doi: 10.1111/j.1475-6773.2008.00906.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Matsudaira JD. Government regulation and the quality of healthcare—Evidence from minimum staffing legislation for nursing homes. Journal of Human Resources. 2014; 49(1): 32–72. Available from: http://jhr.uwpress.org/content/49/1/32.short. [Google Scholar]
- 70.Chen MM, Grabowski DC. Intended and unintended consequences of minimum staffing standards for nursing homes. Health economics. 2015; 24(7): 822–39. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/hec.3063. [DOI] [PubMed] [Google Scholar]
- 71.Cox CC, Eldridge-Houser J, Hasken J, Temme M. Relationship of facility characteristics and presence of an Ombudsman to Missouri long-term care facility state inspection report results. Journal of Elder Abuse & Neglect. 2011; 23(3): 273–88. Available from: https://www.tandfonline.com/doi/abs/10.1080/08946566.2011.584051. [DOI] [PubMed] [Google Scholar]
- 72.Cherry RL. Community presence and nursing home quality of care: the ombudsman as a complementary role. Journal of Health and Social Behavior. 1993; 34(4): 336–45. Available from: https://www.jstor.org/stable/2137371. [PubMed] [Google Scholar]
- 73.Nelson HW, Huber R, Walter KL. The relationship between volunteer long-term care ombudsmen and regulatory nursing home actions. The Gerontologist. 1995; 35(4): 509–14. Available from: https://academic.oup.com/gerontologist/article-abstract/35/4/509/568894. doi: 10.1093/geront/35.4.509 [DOI] [PubMed] [Google Scholar]
- 74.Amirkhanyan AA, Kim HJ, Lambright KT. Does the public sector outperform the nonprofit and for‐profit sectors? Evidence from a national panel study on nursing home quality and access. Journal of Policy Analysis and Management: The Journal of the Association for Public Policy Analysis and Management. 2008; 27(2): 326–53. [DOI] [PubMed] [Google Scholar]
- 75.Huang SS, Bowblis JR. Is the quality of nursing homes countercyclical? Evidence from 2001 through 2015. The Gerontologist. 2019; 59(6): 1044–54. Available from: https://academic.oup.com/gerontologist/article-abstract/59/6/1044/5211009. doi: 10.1093/geront/gny148 [DOI] [PubMed] [Google Scholar]
- 76.Singh DA. Influence of administrator and facility characteristics on nursing home performance [Ph.D]. Columbia: University of South Carolina; 1994. https://search.proquest.com/openview/1eb5ac608671ef4c2e763a2b9dba13a0/1?pq-origsite=gscholar&cbl=18750&diss=y
- 77.Towsley G, Beck S, Pepper G. Predictors of quality in rural nursing homes using standard and novel methods. Research in gerontological nursing. 2013; 6 2: 116–26. Available from: https://journals.healio.com/doi/abs/10.3928/19404921-20130114-02. [DOI] [PubMed] [Google Scholar]
- 78.Weisbrod BA, Schlesinger M. Public, private, nonprofit ownership and the response to asymmetric information: The case of nursing homes. The economics of nonprofit institutions: Studies in structure and policy: Oxford University Press; 1986. [Google Scholar]
- 79.Towsley GL. Quality care and financial viability of rural nursing homes [Ph.D]. Salt Lake City: The University of Utah; 2007.
- 80.June JW, Peterson L, Hyer K, Dobbs D. Implementation of an Emergency Power Rule: Compliance of Florida Nursing Homes and Assisted Living Facilities. Disaster medicine and public health preparedness. 2022: 1–4. Available from: https://www.cambridge.org/core/article/implementation-of-an-emergency-power-rule-compliance-of-florida-nursing-homes-and-assisted-living-facilities/70842AE156D93AF0F0AE78F9245A8789. doi: 10.1017/dmp.2022.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Alexander GL, Madsen RW. A report of information technology and health deficiencies in U.S. nursing homes. Journal of Patient Safety. 2017. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5955802/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Graber DR, Sloane PD. Nursing home survey deficiencies for physical restraint use. Medical care. 1995: 1051–63. Available from: https://www.jstor.org/stable/3766677. doi: 10.1097/00005650-199510000-00006 [DOI] [PubMed] [Google Scholar]
- 83.Trinkoff AM, Lerner NM, Storr CL, Yoon JM, Yang BK, Han K. Nursing staff availability and other facility characteristics in relation to assisted living care deficiencies. Journal of Nursing Regulation. 2019; 10(1): 21–7. Available from: https://www.journalofnursingregulation.com/article/S2155-8256(19)30079-1/fulltext. [Google Scholar]
- 84.Bonifas RP. Nursing home work environment characteristics: Associated outcomes in psychosocial care. Health Care Financing Review. 2008; 30(2): 19. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4195053/. [PMC free article] [PubMed] [Google Scholar]
- 85.Baldwin R, Chenoweth L, Dela Rama M, Liu Z. Quality failures in residential aged care in Australia: The relationship between structural factors and regulation imposed sanctions. Australasian Journal on Ageing. 2015; 34(4): E7–E12. Available from: http://hdl.handle.net/10453/36454. doi: 10.1111/ajag.12165 [DOI] [PubMed] [Google Scholar]
- 86.Terp S, Seabury SA, Axeen S, Pines JM, Lam CN, Arientyl V, et al. The association between hospital characteristics and emergency medical treatment and Labor Act citation events. Medical care. 2020; 58(9): 793–9. Available from: https://europepmc.org/articles/pmc8630639/bin/nihms1611652-supplement-supplement_4___doc___tif__pdf__etc__.docx. doi: 10.1097/MLR.0000000000001360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.June JW, Meng H, Dobbs D, Hyer K. Using deficiency data to measure quality in assisted living communities: A Florida statewide study. Journal of Aging & Social Policy. 2020; 32(2): 125–40. Available from: https://www.tandfonline.com/doi/abs/10.1080/08959420.2018.1563471. [DOI] [PubMed] [Google Scholar]
- 88.Chisholm L, Weech-Maldonado R, Laberge A, Lin F-C, Hyer K. Nursing home quality and financial performance: Does the racial composition of residents matter? Health Services Research. 2013; 48(6pt1): 2060–80. Available from: http://europepmc.org/articles/pmc3805666?pdf=render. doi: 10.1111/1475-6773.12079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Grabowski DC. The admission of blacks to high-deficiency nursing homes. Medical care. 2004: 456–64. Available from: https://www.jstor.org/stable/4640774. doi: 10.1097/01.mlr.0000124307.17380.df [DOI] [PubMed] [Google Scholar]
- 90.Hansen KE. Analyzing the effect of complaints, investigation of allegations, and deficiency citations on the quality of care in united states nursing homes (2007–2012) [Ph.D.]. Ann Arbor: University of South Florida; 2015. https://digitalcommons.usf.edu/cgi/viewcontent.cgi?article=6895&context=etd
- 91.Castle NG. Deficiency citations for physical restraint use in nursing homes. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2000; 55(1): S33–S40. Available from: https://academic.oup.com/psychsocgerontology/article-pdf/55/1/S33/9908782/S33.pdf. doi: 10.1093/geronb/55.1.s33 [DOI] [PubMed] [Google Scholar]
- 92.Jester DJ, Peterson LJ, Dosa DM, Hyer K. Infection control citations in nursing homes: Compliance and geographic variability. Journal of the American Medical Directors Association. 2021; 22(6): 1317–21. e2. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/pmc7834329/. doi: 10.1016/j.jamda.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pittman T. Care deficiencies and super-organization of American nursing homes in hospital referral region. Frontiers in Public Health. 2020; 8. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2020.582405/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kamimura A, Banaszak-Holl J, Berta W, Baum JA, Weigelt C, Mitchell W. Do corporate chains affect quality of care in nursing homes? The role of corporate standardization. Health Care Management Review. 2007; 32(2): 168–78. Available from: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.1075.6158&rep=rep1&type=pdf. doi: 10.1097/01.HMR.0000267794.55427.52 [DOI] [PubMed] [Google Scholar]
- 95.Castle NG. Nursing homes with persistent deficiency citations for physical restraint use. Medical care. 2002: 868–78. Available from: https://www.jstor.org/stable/3767576. doi: 10.1097/00005650-200210000-00005 [DOI] [PubMed] [Google Scholar]
- 96.Graber DR. The influence of nursing home characteristics and task environment on complaints and survey performance [Ph.D.]. Ann Arbor: The University of North Carolina at Chapel Hill; 1993. https://search.proquest.com/openview/27ecfb1fa44f3e91eb59cfc3d4240604/1?pq-origsite=gscholar&cbl=18750&diss=y
- 97.Munroe DJ. The influence of registered nurse staffing on the quality of nursing home care. Research in Nursing & Health. 1990; 13(4): 263–70. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/nur.4770130409. [DOI] [PubMed] [Google Scholar]
- 98.Jester DJ, Molinari V, Bowblis JR, Dobbs D, Zgibor JC, Andel R. Abuse and neglect in nursing homes: The role of serious mental illness. The Gerontologist. 2022. Available from: 10.1093/geront/gnab183. [DOI] [PubMed] [Google Scholar]
- 99.Castle NG, Longest BB. Administrative deficiency citations and quality of care in nursing homes. Health services management research. 2006; 19(3): 144–52. Available from: https://journals.sagepub.com/doi/abs/10.1258/095148406777888107. [DOI] [PubMed] [Google Scholar]
- 100.Li Y, Cai X, Cram P. Are patients with serious mental illness more likely to be admitted to nursing homes with more deficiencies in care? Medical care. 2011; 49(4): 397–405. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3784995/. doi: 10.1097/MLR.0b013e318202ac10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jester DJ, Hyer K, Bowblis JR. Quality concerns in nursing homes that serve large proportions of residents with serious mental illness. The Gerontologist. 2020; 60(7): 1312–21. Available from: 10.1093/geront/gnaa044. [DOI] [PubMed] [Google Scholar]
- 102.Rahman M, Grabowski DC, Intrator O, Cai S, Mor V. Serious mental illness and nursing home quality of care. Health Services Research. 2013; 48(4): 1279–98. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3703484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chesteen S, Helgheim B, Randall T, Wardell D. Comparing quality of care in non-profit and for-profit nursing homes: a process perspective. Journal of Operations Management. 2005; 23(2): 229–42. Available from: https://www.sciencedirect.com/science/article/pii/S0272696304001044. [Google Scholar]
- 104.Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein DU. Does investor ownership of nursing homes compromise the quality of care? American Journal of Public Health. 2001; 91(9): 1452–5. Available from: https://ajph.aphapublications.org/doi/pdfplus/10.2105/AJPH.91.9.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rajaram R, Chung JW, Kinnier CV, Barnard C, Mohanty S, Pavey ES, et al. Hospital characteristics associated with penalties in the centers for Medicare & Medicaid Services Hospital-Acquired Condition Reduction Program. Journal of the American Medical Association. 2015; 314(4): 375–83. Available from: 10.1001/jama.2015.8609. [DOI] [PubMed] [Google Scholar]
- 106.Holmes JS. Institutional form and the nursing home industry: Ownership effects on costs and quality [Ph.D.]. Ann Arbor: University of Michigan; 1992. https://search.proquest.com/openview/c12b90eb54038c5372d563fc3afb522d/1?pq-origsite=gscholar&cbl=18750&diss=y
- 107.Johnson-Pawlson J, Infeld DL. Nurse staffing and quality of care in nursing facilities. Journal of Gerontological Nursing. 1996; 22(8): 36–45. Available from: https://journals.healio.com/doi/abs/10.3928/0098-9134-19960801-11. [DOI] [PubMed] [Google Scholar]
- 108.Temkin-Greener H, Zheng NT, Cai S, Zhao H, Mukamel DB. Nursing home environment and organizational performance: association with deficiency citations. Medical care. 2010; 48(4): 357–64. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2925404/. doi: 10.1097/MLR.0b013e3181ca3d70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Moseley CB, Jones L. Registered nurse staffing and OBRA deficiencies in Nevada nursing facilities. Journal of Gerontological Nursing. 2003. Available from: https://journals.healio.com/doi/full/10.3928/0098-9134-20030301-10. [DOI] [PubMed] [Google Scholar]
- 110.Gage H, Knibb W, Evans J, Williams P, Rickman N, Bryan K. Why are some care homes better than others? An empirical study of the factors associated with quality of care for older people in residential homes in Surrey, England. Health & Social Care in the Community. 2009; 17(6): 599–609. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2524.2009.00861.x. [DOI] [PubMed] [Google Scholar]
- 111.Johnson CE, Weech-Maldonado R, Jia H, Reker D, Buchanan R, Laberge A. Characteristics of community nursing homes serving per diem veterans, 1999 to 2002. Medical Care Research and Review. 2007; 64(6): 673–90. Available from: https://journals.sagepub.com/doi/abs/10.1177/1077558707304740. [DOI] [PubMed] [Google Scholar]
- 112.Fennell ML, Feng Z, Clark MA, Mor V. Elderly Hispanics more likely to reside in poor-quality nursing homes. Health Affairs. 2010; 29(1): 65–73. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3825737. doi: 10.1377/hlthaff.2009.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kim H, Harrington C, Greene WH. Registered nurse staffing mix and quality of care in nursing homes: A longitudinal analysis. The Gerontologist. 2009; 49(1): 81–90. Available from: https://academic.oup.com/gerontologist/article-pdf/49/1/81/1563605/gnp014.pdf. doi: 10.1093/geront/gnp014 [DOI] [PubMed] [Google Scholar]
- 114.Castle NG, Engberg JB. Nursing home deficiency citations for medication use. Journal of Applied Gerontology. 2007; 26(2): 208–32. Available from: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.885.2837&rep=rep1&type=pdf. [Google Scholar]
- 115.Graf Schaffner ML. An exploratory study of boarding home sanctions and compliance in Washington State. Nursing Outlook. 2011; 59(6): 326–35. Available from: https://www.sciencedirect.com/science/article/pii/S0029655411001266. doi: 10.1016/j.outlook.2011.04.003 [DOI] [PubMed] [Google Scholar]
- 116.Castle NG. Citations and compliance with the Nursing Home Reform Act of 1987. Journal of Health & Social Policy. 2001; 13(1): 73–95. Available from: https://www.tandfonline.com/doi/abs/10.1300/J045v13n01_04. doi: 10.1300/j045v13n01_04 [DOI] [PubMed] [Google Scholar]
- 117.Ellis JM, Howe A. The role of sanctions in Australia’s residential aged care quality assurance system. International Journal for Quality in Health Care. 2010; 22(6): 452–60. Available from: https://academic.oup.com/intqhc/article-pdf/22/6/452/5055542/mzq055.pdf. [DOI] [PubMed] [Google Scholar]
- 118.Loescher SC. Analysis of the relationships between nursing home administrator’s types of learning and nursing home effectiveness [Ed.D.]. Auburn: Auburn University; 1994. https://search.proquest.com/openview/37a921ff9e43934795eb7b3e2b939654/1?pq-origsite=gscholar&cbl=18750&diss=y
- 119.Christensen C, Beaver S. Correlation between administrator turnover and survey results. The Journal of long term care administration. 1996; 24(2): 4–7. [PubMed] [Google Scholar]
- 120.Flynn L, Liang Y, Dickson GL, Aiken LH. Effects of nursing practice environments on quality outcomes in nursing homes. Journal of the American Geriatrics Society. 2010; 58(12): 2401–6. Available from: http://europepmc.org/articles/pmc3392023?pdf=render. doi: 10.1111/j.1532-5415.2010.03162.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Althumairi A, Alzahrani A, Alanzi T, Al Wahabi S, Alrowaie S, Aljaffary A, et al. Factors affecting compliance with national accreditation essential safety standards in the Kingdom of Saudi Arabia. Scientific reports. 2022; 12(1): 1–9. Available from: https://www.nature.com/articles/s41598-022-11617-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lee HY. Quality of care: Impact of nursing home characteristics [PhD]: University of California, San Francisco; 2009. https://escholarship.org/content/qt99r8k6gt/qt99r8k6gt.pdf
- 123.Kercado V. Relationship between nurse staffing and quality of care in Louisiana nursing homes [PhD.]. Minneapolis: Walden University; 2016. https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=3318&context=dissertations
- 124.Yu P, Jiang T, Hailey D, Ma J, Qian S. The contribution of electronic health records to risk management through accreditation of residential aged care homes in Australia. BMC medical informatics and decision making. 2020; 20(1): 58. Available from: 10.1186/s12911-020-1070-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Harrington C, Carrillo H. The regulation and enforcement of federal nursing home standards, 1991–1997. Medical Care Research and Review. 1999; 56(4): 471–94. Available from: https://journals.sagepub.com/doi/abs/10.1177/107755879905600405. [DOI] [PubMed] [Google Scholar]
- 126.Akinci F, Krolikowski D. Nurse staffing levels and quality of care in Northeastern Pennsylvania nursing homes. Applied Nursing Research. 2005; 18(3): 130–7. Available from: https://www.sciencedirect.com/science/article/pii/S0897189705000327. doi: 10.1016/j.apnr.2004.08.004 [DOI] [PubMed] [Google Scholar]
- 127.Lerner NB. The relationship between nursing staff levels, skill mix, and deficiencies in Maryland nursing homes. The health care manager. 2013; 32(2): 123–8. Available from: https://journals.lww.com/healthcaremanagerjournal/fulltext/2013/04000/The_Relationship_Between_Nursing_Staff_Levels,.4.aspx. doi: 10.1097/HCM.0b013e31828ef5f9 [DOI] [PubMed] [Google Scholar]
- 128.Riportella-Muller R, Slesinger DP. The relationship of ownership and size to quality of care in Wisconsin nursing homes. The Gerontologist. 1982; 22(4): 429–34. doi: 10.1093/geront/22.4.429 [DOI] [PubMed] [Google Scholar]
- 129.Harrington C, Ross L, Kang T. Hidden owners, hidden profits, and poor nursing home care. International Journal of Health Services. 2015; 45(4): 779–800. Available from: https://journals.sagepub.com/doi/abs/10.1177/0020731415594772. [DOI] [PubMed] [Google Scholar]
- 130.Holmes JS. The effects of ownership and ownership change on nursing home industry costs. Health Services Research. 1996; 31(3): 327. [PMC free article] [PubMed] [Google Scholar]
- 131.Forbes-Thompson S, Leiker T, Bleich MR. High-performing and low-performing nursing homes: a view from complexity science. Health Care Management Review. 2007; 32(4): 341–51. Available from: https://journals.lww.com/hcmrjournal/Fulltext/2007/10000/The_Power_of_Relationship_for_High_quality.00006.aspx. doi: 10.1097/01.HMR.0000296789.39128.f6 [DOI] [PubMed] [Google Scholar]
- 132.McKinney SH, Corazzini K, Anderson RA, Sloane R, Castle NG. Nursing home director of nursing leadership style and director of nursing-sensitive survey deficiencies. Health Care Management Review. 2016; 41(3): 224–32. Available from: https://www.jstor.org/stable/48516221. doi: 10.1097/HMR.0000000000000072 [DOI] [PubMed] [Google Scholar]
- 133.Herzig CT, Stone PW, Castle N, Pogorzelska-Maziarz M, Larson EL, Dick AW. Infection prevention and control programs in US nursing homes: results of a national survey. Journal of the American Medical Directors Association. 2016; 17(1): 85–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4696513/. doi: 10.1016/j.jamda.2015.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Stone PW, Herzig CTA, Agarwal M, Pogorzelska-Maziarz M, Dick AW. Nursing home infection control program characteristics, CMS citations, and implementation of antibiotic stewardship policies: A national study. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2018; 55. Available from: https://journals.sagepub.com/doi/pdf/10.1177/0046958018778636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hamann DJ, Bezboruah KC. Outcomes of health information technology utilization in nursing homes: Do implementation processes matter? Health Informatics Journal. 2020; 26(3): 2249–64. Available from: https://journals.sagepub.com/doi/pdf/10.1177/1460458219899556. [DOI] [PubMed] [Google Scholar]
- 136.Jiang T, Yu P, Hailey D, Ma J, Yang J. The impact of electronic health records on risk management of information systems in Australian residential aged care homes. Journal of medical systems. 2016; 40(9): 204. Available from: 10.1007/s10916-016-0553-y. [DOI] [PubMed] [Google Scholar]
- 137.Makkai T, Braithwaite J. Criminological theories and regulatory compliance. Criminology. 1991; 29(2): 191–220. [Google Scholar]
- 138.Nadash P, Hefele JG, Miller EA, Barooah A, Wang XJ. A national-level analysis of the relationship between nursing home satisfaction and quality. Research on Aging. 2019; 41(3): 215–40. Available from: https://journals.sagepub.com/doi/abs/10.1177/0164027518805001. [DOI] [PubMed] [Google Scholar]
- 139.Grabowski DC, Stevenson DG. Ownership conversions and nursing home performance. Health Services Research. 2008; 43(4): 1184–203. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2517264. doi: 10.1111/j.1475-6773.2008.00841.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Grabowski DC, O’Malley AJ, Afendulis CC, Caudry DJ, Elliot A, Zimmerman S. Culture change and nursing home quality of care. The Gerontologist. 2014; 54(Suppl_1): S35–S45. Available from: https://academic.oup.com/gerontologist/article-pdf/54/Suppl_1/S35/16786227/gnt143.pdf. doi: 10.1093/geront/gnt143 [DOI] [PubMed] [Google Scholar]
- 141.Grabowski DC, Elliot A, Leitzell B, Cohen LW, Zimmerman S. Who are the innovators? Nursing homes implementing culture change. The Gerontologist. 2014. a; 54(Suppl 1): S65–S75. Available from: https://academic.oup.com/gerontologist/article-pdf/54/Suppl_1/S65/2008716/gnt144.pdf. doi: 10.1093/geront/gnt144 [DOI] [PubMed] [Google Scholar]
- 142.Jogerst GJ, Daly JM, Dawson JD, Peek-Asa C, Schmuch G. Iowa nursing home characteristics associated with reported abuse. Journal of the American Medical Directors Association. 2006; 7(4): 203–7. Available from: https://www.academia.edu/download/40503891/Iowa_Nursing_Home_Characteristics_Associ20151130-6016-18hspnm.pdf. doi: 10.1016/j.jamda.2005.12.006 [DOI] [PubMed] [Google Scholar]
- 143.Castle NG. The influence of consistent assignment on nursing home deficiency citations. The Gerontologist. 2011. a; 51(6): 750–60. Available from: https://academic.oup.com/gerontologist/article-pdf/51/6/750/2446563/gnr068.pdf. doi: 10.1093/geront/gnr068 [DOI] [PubMed] [Google Scholar]
- 144.Laberge A. An examination of strategic group membership and technology in the nursing home industry [Ph.D.]. Ann Arbor: University of Florida; 2009. https://search.proquest.com/openview/f7c39abfdc9ac5202a96681137316157/1?pq-origsite=gscholar&cbl=18750
- 145.Castle NG, Engberg J. An examination of special focus facility nursing homes. The Gerontologist. 2010; 50(3): 400–7. Available from: https://academic.oup.com/gerontologist/article-pdf/50/3/400/1544443/gnq008.pdf. doi: 10.1093/geront/gnq008 [DOI] [PubMed] [Google Scholar]
- 146.Bell E, Robinson A, Barnett T. Building policy and service theory from nursing home inspection results: Qualitative Comparative Analysis. International Journal on Disability and Human Development. 2013; 12(1): 77–86. Available from: https://www.degruyter.com/document/doi/10.1515/ijdhd-2012-0119/html. [Google Scholar]
- 147.Wang X, Xuan Z, Storella TH, Zhou X. Determinants of non-prescription antibiotic dispensing in Chinese community pharmacies from socio-ecological and health system perspectives. Social Science & Medicine. 2020; 256: 113035. Available from: https://www.sciencedirect.com/science/article/pii/S0277953620302549. doi: 10.1016/j.socscimed.2020.113035 [DOI] [PubMed] [Google Scholar]
- 148.Klopfenstein K, Lockhart C, Giles-Sims J. Do high rates of OSCAR deficiencies prompt improved nursing facility processes and outcomes? Journal of Aging & Social Policy. 2011; 23(4): 384–407. Available from: https://www.tandfonline.com/doi/abs/10.1080/08959420.2011.605667. doi: 10.1080/08959420.2011.605667 [DOI] [PubMed] [Google Scholar]
- 149.Simmons SF, Bonnett KR, Hollingsworth E, Kim J, Powers J, Habermann R, et al. Reducing antipsychotic medication use in nursing homes: A qualitative study of nursing staff perceptions. The Gerontologist. 2018; 58(4): e239–e50. Available from: https://academic.oup.com/gerontologist/article-pdf/58/4/e239/25138914/gnx083.pdf. doi: 10.1093/geront/gnx083 [DOI] [PubMed] [Google Scholar]
- 150.Williams SC, Morton DJ, Braun BI, Longo BA, Baker DW. Comparing public quality ratings for accredited and nonaccredited nursing homes. Journal of the American Medical Directors Association. 2017; 18(1): 24–9. Available from: 10.1016/j.jamda.2016.07.025. [DOI] [PubMed] [Google Scholar]
- 151.Wagner LM, McDonald SM, Castle NG. Impact of voluntary accreditation on deficiency citations in U.S. nursing homes. The Gerontologist. 2012. a; 52(4): 561–70. Available from: https://academic.oup.com/gerontologist/article-pdf/52/4/561/1805648/gnr136.pdf. [DOI] [PubMed] [Google Scholar]
- 152.Wagner LM, McDonald SM, Castle NG. Joint commission accreditation and quality measures in US nursing homes. Policy, Politics, & Nursing Practice. 2012; 13(1): 8–16. Available from: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.905.7706&rep=rep1&type=pdf. [DOI] [PubMed] [Google Scholar]
- 153.Castle N, Olson D, Shah U, Hansen K. Do recipients of an association-sponsored quality award program experience better quality outcomes compared with other nursing facilities across the United States? Journal of Applied Gerontology. 2018; 37(11): 1368–90. Available from: https://journals.sagepub.com/doi/abs/10.1177/0733464816665205. [DOI] [PubMed] [Google Scholar]
- 154.Allan S, Vadean F. The association between staff retention and English care home quality. Journal of Aging & Social Policy. 2021: 1–17. Available from: https://kar.kent.ac.uk/75795/1/Assoc_Stf_Ret_CHQ_Accepted.pdf. doi: 10.1080/08959420.2020.1851349 [DOI] [PubMed] [Google Scholar]
- 155.Bourbonniere M, Feng Z, Intrator O, Angelelli J, Mor V, Zinn JS. The use of contract licensed nursing staff in U.S. nursing homes. Medical Care Research and Review. 2006; 63(1): 88–109. Available from: https://jdc.jefferson.edu/cgi/viewcontent.cgi?article=1025&context=nursfp. doi: 10.1177/1077558705283128 [DOI] [PubMed] [Google Scholar]
- 156.Bowblis JR, Roberts AR. Cost-effective adjustments to nursing home staffing to improve quality. Medical Care Research and Review. 2020; 77(3): 274–84. Available from: https://journals.sagepub.com/doi/abs/10.1177/1077558718778081. [DOI] [PubMed] [Google Scholar]
- 157.Holecek T, Dellmann-Jenkins M, Curry D. Exploring the influence of the regulatory survey process on nursing home administrator job satisfaction and job seeking. Journal of Applied Gerontology. 2010; 29(2): 215–30. Available from: https://journals.sagepub.com/doi/abs/10.1177/0733464808321886. [Google Scholar]
- 158.Yoon JM, Trinkoff AM, Galik E, Storr CL, Lerner NB, Brandt N, et al. Nurse staffing and deficiency of care for inappropriate psychotropic medication use in nursing home residents with dementia. Journal of Nursing Scholarship. 2022. Available from: https://sigmapubs.onlinelibrary.wiley.com/doi/abs/10.1111/jnu.12776. [DOI] [PubMed] [Google Scholar]
- 159.Lin H. Revisiting the relationship between nurse staffing and quality of care in nursing homes: An instrumental variables approach. Journal of health economics. 2014; 37: 13–24. Available from: https://www.sciencedirect.com/science/article/pii/S0167629614000629. doi: 10.1016/j.jhealeco.2014.04.007 [DOI] [PubMed] [Google Scholar]
- 160.Lerner NB, Johantgen M, Trinkoff AM, Storr CL, Han K. Are nursing home survey deficiencies higher in facilities with greater staff turnover. Journal of the American Medical Directors Association. 2014; 15(2): 102–7. Available from: https://www.sciencedirect.com/science/article/pii/S1525861013005276. doi: 10.1016/j.jamda.2013.09.003 [DOI] [PubMed] [Google Scholar]
- 161.Kim H, Kovner C, Harrington C, Greene W, Mezey M. A panel data analysis of the relationships of nursing home staffing levels and standards to regulatory deficiencies. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009. a; 64B(2): 269–78. Available from: http://europepmc.org/articles/pmc2655170?pdf=render. doi: 10.1093/geronb/gbn019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Vongxaiburana E, Thomas KS, Frahm KA, Hyer K. The social worker in interdisciplinary care planning. Clinical Gerontologist. 2011; 34(5): 367–78. Available from: https://www.tandfonline.com/doi/abs/10.1080/07317115.2011.588540. [Google Scholar]
- 163.Castle NG. Administrator turnover and quality of care in nursing homes. The Gerontologist. 2001. a; 41(6): 757–67. Available from: https://academic.oup.com/gerontologist/article-abstract/41/6/757/555763. doi: 10.1093/geront/41.6.757 [DOI] [PubMed] [Google Scholar]
- 164.Loomer L, Grabowski DC, Yu H, Gandhi A. Association between nursing home staff turnover and infection control citations. Health Services Research. 2022; 57(2): 322–32. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/1475-6773.13877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kennedy KA. Is nurse aide retention associated with nursing home quality? [PhD]: Miami University; 2021. https://etd.ohiolink.edu/apexprod/rws_etd/send_file/send?accession=miami1618591173416498&disposition=inline
- 166.Castle NG, Hyer K, Harris JA, Engberg J. Nurse aide retention in nursing homes. The Gerontologist. 2020; 60(5): 885–95. Available from: https://academic.oup.com/gerontologist/article-abstract/60/5/885/5796922. doi: 10.1093/geront/gnz168 [DOI] [PubMed] [Google Scholar]
- 167.Harvey D. Nursing home administrator turnover and quality of care: A quantitative study [D.M.]. Ann Arbor: University of Phoenix; 2014. https://search.proquest.com/openview/3f707b4e4bb90a5787e0fb8dbcabccc1/1?pq-origsite=gscholar&cbl=18750
- 168.Antwi YA, Bowblis JR. The impact of nurse turnover on quality of care and mortality in nursing homes: Evidence from the great recession. American Journal of Health Economics. 2018; 4(2): 131–63. Available from: https://www.journals.uchicago.edu/doi/abs/10.1162/ajhe_a_00096. [Google Scholar]
- 169.Donoghue C, Castle NG. Voluntary and involuntary nursing home staff turnover. Research on Aging. 2006; 28(4): 454–72. Available from: https://journals.sagepub.com/doi/abs/10.1177/0164027505284164. [Google Scholar]
- 170.Troyer JL. Cross-subsidization in nursing homes: Explaining rate differentials among payer types. Southern Economic Journal. 2002; 68(4): 750–73. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/j.2325-8012.2002.tb00457.x. [Google Scholar]
- 171.Stevenson DG, Spittal MJ, Studdert DM. Does litigation increase or decrease health care quality?: a national study of negligence claims against nursing homes. Medical care. 2013; 51(5): 430–6. Available from: https://pubmed.ncbi.nlm.nih.gov/23552438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Christianson JB. Long-term care standards: enforcement and compliance. Journal of health politics, policy and law. 1979; 4(3): 414–34. doi: 10.1215/03616878-4-3-414 [DOI] [PubMed] [Google Scholar]
- 173.Studdert DM, Spittal MJ, Mello MM, O’Malley AJ, Stevenson DG. Relationship between quality of care and negligence litigation in nursing homes. New England Journal of Medicine. 2011; 364(13): 1243–50. Available from: https://www.nejm.org/doi/full/10.1056/nejmsa1009336. [DOI] [PubMed] [Google Scholar]
- 174.Ballou JP. The role of the not-for-profit firm in the mixed industry: Three empirical analyses of the long-term care and hospital industries [Ph.D.]. Ann Arbor: Northwestern University; 2000. https://search.proquest.com/openview/e354c8e2e52942dcfdd2ffc26fcf4b20/1?pq-origsite=gscholar&cbl=18750&diss=y
- 175.Weech-Maldonado R, Pradhan R, Dayama N, Lord J, Gupta S. Nursing home quality and financial performance: Is there a business case for quality? INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2019; 56: 004695801882519. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6376502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Oetjen RM, Zhao M, Liu D, Carretta HJ. Nursing home safety: does financial performance matter? Journal of health care finance. 2011; 37(3): 51. Available from: https://vbn.aau.dk/ws/portalfiles/portal/42005647/JHCF_Winter10_1.pdf#page=53. [PubMed] [Google Scholar]
- 177.Banaszak-Holl J, Berta WB, Bowman DM, Baum JAC, Mitchell W. The rise of human service chains: antecedents to acquisitions and their effects on the quality of care in US nursing homes. Managerial and Decision Economics. 2002; 23(4–5): 261–82. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/mde.1065. [Google Scholar]
- 178.Grabowski DC, Stevenson DG. Ownership conversions and nursing home performance. Health Services Research. 2008; 43(4): 1184–203. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18355255. doi: 10.1111/j.1475-6773.2008.00841.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Donoghue C, Castle NG. Organizational and environmental effects on voluntary and involuntary turnover. Health Care Management Review. 2007; 32(4): 360–9. Available from: https://journals.lww.com/hcmrjournal/FullText/2007/10000/Organizational_and_environmental_effects_on.8.aspx. doi: 10.1097/01.HMR.0000296791.16257.44 [DOI] [PubMed] [Google Scholar]
- 180.Fabbri MA. Factors that influence an administrator’s perception of what they consider important in job knowledge and how those perceptions impact quality of care [Ph.D.]. Ann Arbor: Capella University; 2006. https://search.proquest.com/openview/ae770195fcea82080ac521e9690558f6/1?pq-origsite=gscholar&cbl=18750&diss=y
- 181.George K. Exploring the challenges non-clinical departments encounter during eden alternative implementation. Minneapolis: Walden University; 2019. https://search.proquest.com/openview/d00f65afa64dfc47b5f9b29126e424a4/1?pq-origsite=gscholar&cbl=18750&diss=y [Google Scholar]
- 182.Mumford V, Greenfield D, Hogden A, Debono D, Gospodarevskaya E, Forde K, et al. Disentangling quality and safety indicator data: a longitudinal, comparative study of hand hygiene compliance and accreditation outcomes in 96 Australian hospitals. BMJ Open. 2014; 4(9): e005284. Available from: http://bmjopen.bmj.com/content/4/9/e005284.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Castle NG. Providing outcomes information to nursing homes: can it improve quality of care? The Gerontologist. 2003; 43(4): 483–92. Available from: https://academic.oup.com/gerontologist/article-abstract/43/4/483/592297. doi: 10.1093/geront/43.4.483 [DOI] [PubMed] [Google Scholar]
- 184.Centers for Disease Control. National Healthcare Safety Network (NHSN) 2022. Available from: https://www.cdc.gov/nhsn/index.html Accessed on: 4/11/2022
- 185.Feng Z, Katz PR, Intrator O, Karuza J, Mor V. Physician and nurse staffing in nursing homes: The role and limitations of the Online Survey Certification and Reporting (OSCAR) system. Journal of the American Medical Directors Association. 2005; 6(1): 27–33. Available from: https://www.sciencedirect.com/science/article/pii/S152586100400009X. doi: 10.1016/j.jamda.2004.12.008 [DOI] [PubMed] [Google Scholar]
- 186.Comondore VR, Devereaux P, Zhou Q, Stone SB, Busse JW, Ravindran NC, et al. Quality of care in for-profit and not-for-profit nursing homes: systematic review and meta-analysis. Br Med J. 2009; 339. Available from: https://www.bmj.com/content/339/bmj.b2732.long. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Baldwin R, Chenoweth L, dela Rama M, Wang AY. Does size matter in aged care facilities? A literature review of the relationship between the number of facility beds and quality. Health Care Management Review. 2017; 42(4): 315–27. Available from: https://journals.lww.com/hcmrjournal/FullText/2017/10000/Does_size_matter_in_aged_care_facilities__A.5.aspx. doi: 10.1097/HMR.0000000000000116 [DOI] [PubMed] [Google Scholar]
- 188.Shippee TP, Henning-Smith C, Kane RL, Lewis T. Resident- and Facility-Level Predictors of Quality of Life in Long-Term Care. The Gerontologist. 2013; 55(4): 643–55. Available from: 10.1093/geront/gnt148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Spangler D, Blomqvist P, Lindberg Y, Winblad U. Small is beautiful? Explaining resident satisfaction in Swedish nursing home care. BMC health services research. 2019; 19(1): 1–12. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-019-4694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Smith JG, Plover CM, McChesney MC, Lake ET. Isolated, small, and large hospitals have fewer nursing resources than urban hospitals: Implications for rural health policy. Public Health Nursing. 2019; 36(4): 469–77. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6635079/. doi: 10.1111/phn.12612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Castle NG, Engberg J. Organizational characteristics associated with staff turnover in nursing homes. The Gerontologist. 2006; 46(1): 62–73. Available from: https://academic.oup.com/gerontologist/article/46/1/62/566756. doi: 10.1093/geront/46.1.62 [DOI] [PubMed] [Google Scholar]
- 192.Harrington C, Jacobsen FF, Panos J, Pollock A, Sutaria S, Szebehely M. Marketization in long-term care: a cross-country comparison of large for-profit nursing home chains. Health services insights. 2017; 10: 1178632917710533. Available from: https://journals.sagepub.com/doi/pdf/10.1177/1178632917710533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Anderson R, Weeks H, Hobbs B, Webb J. Nursing home quality, chain affiliation, profit status and performance. Journal of Real Estate Research. 2003; 25(1): 43–60. Available from: 10.1080/10835547.2003.12091100. [DOI] [Google Scholar]
- 194.Aguiar-Díaz I, Ruiz-Mallorquí MV, González-López Valcarcel B. Nursing homes: Affiliation to large chains, quality and public & private collaboration. Healthcare. 2022; 10(8): 1431. Available from: https://www.mdpi.com/2227-9032/10/8/1431/pdf. doi: 10.3390/healthcare10081431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Hsu AT, Berta W, Coyte PC, Laporte A. Staffing in Ontario’s long-term care homes: differences by profit status and chain ownership. Canadian Journal on Aging/La Revue canadienne du vieillissement. 2016; 35(2): 175–89. Available from: https://www.cambridge.org/core/journals/canadian-journal-on-aging-la-revue-canadienne-du-vieillissement/article/staffing-in-ontarios-longterm-care-homes-differences-by-profit-status-and-chain-ownership/FB64E7D75C7F108BC008DC1CDB50DACC. doi: 10.1017/S0714980816000192 [DOI] [PubMed] [Google Scholar]
- 196.You K, Li Y, Intrator O, Stevenson D, Hirth R, Grabowski D, et al. Do nursing home chain size and proprietary status affect experiences with care? Medical care. 2016; 54(3): 229. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4752885/. doi: 10.1097/MLR.0000000000000479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Castle NG, Liu D, Engberg J. The association of Nursing Home Compare quality measures with market competition and occupancy rates. Journal for Healthcare Quality. 2008; 30(2): 4–14. doi: 10.1111/j.1945-1474.2008.tb01129.x [DOI] [PubMed] [Google Scholar]
- 198.Kuntz L, Mennicken R, Scholtes S. Stress on the ward: Evidence of safety tipping points in hospitals. Management Science. 2015; 61(4): 754–71. Available from: http://helsetjenesteaksjonen.no/V01/wp-content/uploads/2015/02/kuntz.pdf. [Google Scholar]
- 199.Keegan AD. Hospital bed occupancy: more than queuing for a bed. Medical journal of Australia. 2010; 193(5): 291–3. Available from: https://onlinelibrary.wiley.com/doi/abs/10.5694/j.1326-5377.2010.tb03910.x. [DOI] [PubMed] [Google Scholar]
- 200.Cioltan H, Alshehri S, Howe C, Lee J, Fain M, Eng H, et al. Variation in use of antipsychotic medications in nursing homes in the United States: A systematic review. BMC Geriatrics. 2017; 17(1): 32. Available from: 10.1186/s12877-017-0428-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Sprivulis PC, Da Silva JA, Jacobs IG, Jelinek GA, Frazer AR. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Medical journal of Australia. 2006; 184(5): 208–12. Available from: https://onlinelibrary.wiley.com/doi/abs/10.5694/j.1326-5377.2006.tb00203.x. doi: 10.5694/j.1326-5377.2006.tb00416.x [DOI] [PubMed] [Google Scholar]
- 202.Kaier K, Mutters N, Frank U. Bed occupancy rates and hospital-acquired infections—should beds be kept empty? Clinical Microbiology and Infection. 2012; 18(10): 941–5. Available from: https://www.sciencedirect.com/science/article/pii/S1198743X14610909. doi: 10.1111/j.1469-0691.2012.03956.x [DOI] [PubMed] [Google Scholar]
- 203.Weech-Maldonado R, Lord J, Pradhan R, Davlyatov G, Dayama N, Gupta S, et al. High Medicaid nursing homes: Organizational and market factors associated with financial performance. Inquiry: The Journal of Health Care Organization, Provision, and Financing. 2019; 56: 0046958018825061. Available from: https://journals.sagepub.com/doi/abs/10.1177/0046958018825061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Waldman JD, Kelly F, Arora S, Smith HL. The shocking cost of turnover in health care. Health Care Management Review. 2010; 35(3): 206–11. Available from: https://journals.lww.com/hcmrjournal/Fulltext/2010/07000/The_shocking_cost_of_turnover_in_health_care.2.aspx. doi: 10.1097/HMR.0b013e3181e3940e [DOI] [PubMed] [Google Scholar]
- 205.Woltmann EM, Whitley R, McHugo GJ, Brunette M, Torrey WC, Coots L, et al. The role of staff turnover in the implementation of evidence-based practices in mental health care. Psychiatric Services. 2008; 59(7): 732–7. Available from: https://ps.psychiatryonline.org/doi/abs/10.1176/ps.2008.59.7.732. [DOI] [PubMed] [Google Scholar]
- 206.Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Medical care. 2007: 1195–204. Available from: https://www.jstor.org/stable/40221602. doi: 10.1097/MLR.0b013e3181468ca3 [DOI] [PubMed] [Google Scholar]
- 207.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. New England Journal of Medicine. 2002; 346(22): 1715–22. Available from: https://www.nejm.org/doi/full/10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 208.Lankshear AJ, Sheldon TA, Maynard A. Nurse staffing and healthcare outcomes: a systematic review of the international research evidence. Advances in Nursing Science. 2005; 28(2): 163–74. Available from: https://journals.lww.com/advancesinnursingscience/Fulltext/2005/04000/Nurse_Staffing_and_Healthcare_Outcomes__A.00008.aspx. doi: 10.1097/00012272-200504000-00008 [DOI] [PubMed] [Google Scholar]
- 209.Penoyer DA. Nurse staffing and patient outcomes in critical care: a concise review. Critical care medicine. 2010; 38(7): 1521–8. Available from: https://journals.lww.com/ccmjournal/Fulltext/2010/07000/Nurse_Staffing_and_Patient_Outcomes.00002.aspx. doi: 10.1097/CCM.0b013e3181e47888 [DOI] [PubMed] [Google Scholar]
- 210.Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: a systematic review. International journal of nursing studies. 2011; 48(6): 732–50. Available from: https://www.sciencedirect.com/science/article/pii/S0020748911000538. doi: 10.1016/j.ijnurstu.2011.02.014 [DOI] [PubMed] [Google Scholar]
- 211.Bostick JE, Rantz MJ, Flesner MK, Riggs CJ. Systematic review of studies of staffing and quality in nursing homes. Journal of the American Medical Directors Association. 2006; 7(6): 366–76. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16843237. doi: 10.1016/j.jamda.2006.01.024 [DOI] [PubMed] [Google Scholar]
- 212.Backhaus R, Verbeek H, van Rossum E, Capezuti E, Hamers JP. Nurse staffing impact on quality of care in nursing homes: a systematic review of longitudinal studies. Journal of the American Medical Directors Association. 2014; 15(6): 383–93. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24529872. doi: 10.1016/j.jamda.2013.12.080 [DOI] [PubMed] [Google Scholar]
- 213.Bowblis JR, Crystal S, Intrator O, Lucas JA. Response to regulatory stringency: the case of antipsychotic medication use in nursing homes. Health economics. 2012; 21(8): 977–93. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/hec.1775. [DOI] [PubMed] [Google Scholar]
- 214.Maker Y, McSherry B. Regulating restraint use in mental health and aged care settings: Lessons from the Oakden scandal. Alternative Law Journal. 2019; 44(1): 29–36. Available from: https://journals.sagepub.com/doi/full/10.1177/1037969X18817592. [Google Scholar]
- 215.Castle NG, Engberg J. The influence of staffing characteristics on quality of care in nursing homes. Health Services Research. 2007; 42(5): 1822–47. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17850522. doi: 10.1111/j.1475-6773.2007.00704.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Agarwal S, Lucca D, Seru A, Trebbi F. Inconsistent regulators: Evidence from banking. The Quarterly Journal of Economics. 2014; 129(2): 889–938. Available from: https://academic.oup.com/qje/article-abstract/129/2/889/1867167. [Google Scholar]
- 217.Boyd A, Addicott R, Robertson R, Ross S, Walshe K. Are inspectors’ assessments reliable? Ratings of NHS acute hospital trust services in England. Journal of health services research & policy. 2017; 22(1): 28–36. Available from: https://journals.sagepub.com/doi/abs/10.1177/1355819616669736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Tuijn SM, Robben PB, Janssens FJ, Van Den Bergh H. Evaluating instruments for regulation of health care in the Netherlands. Journal of evaluation in clinical practice. 2011; 17(3): 411–9. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2753.2010.01431.x. [DOI] [PubMed] [Google Scholar]
- 219.Läikkö-Roto T, Mäkelä S, Lundén J, Heikkilä J, Nevas M. Consistency in inspection processes of food control officials and efficacy of official controls in restaurants in Finland. Food Control. 2015; 57: 341–50. Available from: https://www.sciencedirect.com/science/article/pii/S0956713515002327. [Google Scholar]
- 220.Agarwal A, Marks L. Variations in medicaid payment rates for radiation oncology. International journal of radiation oncology, biology, physics. 2018; 102(3): e411. Available from: https://www.sciencedirect.com/science/article/pii/S0360301619302573. [DOI] [PubMed] [Google Scholar]
- 221.Miller DC, Gust C, Dimick JB, Birkmeyer N, Skinner J, Birkmeyer JD. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Affairs. 2011; 30(11): 2107–15. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4003905/. doi: 10.1377/hlthaff.2011.0783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, Larson EH. Geographic variation in the supply of selected behavioral health providers. American journal of preventive medicine. 2018; 54(6, Supplement 3): S199–S207. Available from: https://www.sciencedirect.com/science/article/pii/S0749379718300059. doi: 10.1016/j.amepre.2018.01.004 [DOI] [PubMed] [Google Scholar]
- 223.Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care—the growing importance of the community health center. New England Journal of Medicine. 2010; 362(22): 2047–50. Available from: https://www.researchgate.net/profile/Eli-Adashi/publication/43351796_Health_Care_Reform_and_Primary_Care_-_The_Growing_Importance_of_the_Community_Health_Center/links/0046352bc6c894d0c5000000/Health-Care-Reform-and-Primary-Care-The-Growing-Importance-of-the-Community-Health-Center.pdf. doi: 10.1056/NEJMp1003729 [DOI] [PubMed] [Google Scholar]
- 224.Falvey JR, Hade EM, Friedman S, Deng R, Jabbour J, Stone RI, et al. Severe neighborhood deprivation and nursing home staffing in the United States. Journal of the American Geriatrics Society. Available from: https://agsjournals.onlinelibrary.wiley.com/doi/abs/10.1111/jgs.17990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Harrington C, Dellefield ME, Halifax E, Fleming ML, Bakerjian D. Appropriate nurse staffing levels for US nursing homes. Health services insights. 2020; 13: 1178632920934785. Available from: https://journals.sagepub.com/doi/abs/10.1177/1178632920934785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Tazzyman A, Ferguson J, Boyd A, Bryce M, Tredinnick-Rowe J, Price T, et al. Reforming medical regulation: a qualitative study of the implementation of medical revalidation in England, using Normalization Process Theory. Journal of health services research & policy. 2020; 25(1): 30–40. Available from: https://journals.sagepub.com/doi/abs/10.1177/1355819619848017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Oakes P. Crash: what went wrong at winterbourne view? Journal of Intellectual Disabilities. 2012; 16(3): 155–62. Available from: https://journals.sagepub.com/doi/full/10.1177/1744629512449095. [DOI] [PubMed] [Google Scholar]
- 228.Bhaskar K, Flower J, Sellers R. Financial failures and scandals: From Enron to Carillion: Routledge; 2019. [Google Scholar]
- 229.Haines F.. Globalization and regulatory character: regulatory reform after the Kader Toy Factory Fire: Routledge; 2019. [Google Scholar]
- 230.Braithwaite V, Murphy K, Reinhart M. Taxation threat, motivational postures, and responsive regulation. Law & Policy. 2007; 29(1): 137–58. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1467-9930.2007.00250.x. [Google Scholar]
- 231.Feld LP, Frey BS. Tax compliance as the result of a psychological tax contract: The role of incentives and responsive regulation. Law & Policy. 2007; 29(1): 102–20. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1467-9930.2007.00248.x. [Google Scholar]
- 232.Gao J, Zhao J. Normative and image motivations for transportation policy compliance. Urban studies. 2017; 54(14): 3318–36. Available from: https://journals.sagepub.com/doi/abs/10.1177/0042098016664829. [Google Scholar]
- 233.Poulter DR, Chapman P, Bibby PA, Clarke DD, Crundall D. An application of the theory of planned behaviour to truck driving behaviour and compliance with regulations. Accident analysis & prevention. 2008; 40(6): 2058–64. Available from: https://www.sciencedirect.com/science/article/pii/S0001457508001796. doi: 10.1016/j.aap.2008.09.002 [DOI] [PubMed] [Google Scholar]
- 234.Gezelius SS. Do norms count? State regulation and compliance in a Norwegian fishing community. Acta Sociologica. 2002; 45(4): 305–14. Available from: https://journals.sagepub.com/doi/abs/10.1177/000169930204500404. [Google Scholar]
- 235.Van Snellenberg T, van de Peppel R. Perspectives on compliance: non‐compliance with environmental licences in the Netherlands. European Environment. 2002; 12(3): 131–48. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/eet.292. [Google Scholar]
- 236.Parker C, Nielsen VL. Introduction. In: Parker C, Nielsen VL, (Eds.). Explaining compliance: Business responses to regulation. Cheltenham: Edward Elgar Publishing; 2011. [Google Scholar]
- 237.Van Erp J. Naming and shaming in regulatory enforcement. In: Parker C, Nielsen VL, (Eds.). Explaining compliance: Business responses to regulation. Cheltenham: Edward Elgar Publishing; 2011. p. 322. [Google Scholar]
- 238.May PJ. Compliance motivations: Perspectives of farmers, homebuilders, and marine facilities. Law & Policy. 2005; 27(2): 317–47. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1467-9930.2005.00202.x. [Google Scholar]
- 239.Gilad S. Institutionalizing fairness in financial markets: Mission impossible? Regulation & Governance. 2011; 5(3): 309–32. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1748-5991.2011.01116.x. [Google Scholar]
- 240.Bajo E, Bigelli M, Hillier D, Petracci B. The determinants of regulatory compliance: An analysis of insider trading disclosures in Italy. Journal of Business Ethics. 2009; 90(3): 331–43. Available from: https://link.springer.com/article/10.1007/s10551-009-0044-x. [Google Scholar]
- 241.Palmer RC, Ismond D, Rodriquez EJ, Kaufman JS. Social determinants of health: future directions for health disparities research. American Public Health Association; 2019. p. S70–S1. doi: 10.2105/AJPH.2019.304964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Dowling E. The care crisis: What caused it and how can we end it?: Verso Books; 2022. [Google Scholar]
- 243.Francesco FD. Diffusion of regulatory impact analysis among OECD and EU member states. Comparative Political Studies. 2012; 45(10): 1277–305. Available from: https://journals.sagepub.com/doi/abs/10.1177/0010414011434297. [Google Scholar]
- 244.Chimeddamba O, Peeters A, Ayton D, Tumenjargal E, Sodov S, Joyce C. Implementation of clinical guidelines on diabetes and hypertension in urban Mongolia: a qualitative study of primary care providers’ perspectives and experiences. Implementation science. 2015; 10(1): 1–11. Available from: https://implementationscience.biomedcentral.com/articles/10.1186/s13012-015-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Song Y, Ballesteros M, Li J, García LM, de Guzmán EN, Vernooij RW, et al. Current practices and challenges in adaptation of clinical guidelines: a qualitative study based on semistructured interviews. BMJ Open. 2021; 11(12): e053587. Available from: https://bmjopen.bmj.com/content/11/12/e053587.abstract. doi: 10.1136/bmjopen-2021-053587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Sommerbakk R, Haugen DF, Tjora A, Kaasa S, Hjermstad MJ. Barriers to and facilitators for implementing quality improvements in palliative care–results from a qualitative interview study in Norway. BMC palliative care. 2016; 15(1): 1–17. Available from: https://link.springer.com/article/10.1186/s12904-016-0132-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Leggat SG, Balding C. A qualitative study on the implementation of quality systems in Australian hospitals. Health services management research. 2017; 30(3): 179–86. Available from: https://journals.sagepub.com/doi/abs/10.1177/0951484817715594. [DOI] [PubMed] [Google Scholar]
- 248.Mou D, Sisodia RC, Castillo-Angeles M, Ladin K, Bergmark RW, Pusic AL, et al. The surgeon’s perceived value of patient-reported outcome measures (PROMs): an exploratory qualitative study of 5 different surgical subspecialties. Annals of surgery. 2022; 275(3): 500–5. Available from: https://www.ingentaconnect.com/content/wk/sla/2022/00000275/00000003/art00016. doi: 10.1097/SLA.0000000000004253 [DOI] [PubMed] [Google Scholar]
- 249.Dainty KN, Seaton B, Laupacis A, Schull M, Vaillancourt S. A qualitative study of emergency physicians’ perspectives on PROMS in the emergency department. BMJ Quality & Safety. 2017; 26(9): 714–21. Available from: https://qualitysafety.bmj.com/content/26/9/714.abstract. doi: 10.1136/bmjqs-2016-006012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Zulman DM, Damschroder LJ, Smith RG, Resnick PJ, Sen A, Krupka EL, et al. Implementation and evaluation of an incentivized Internet-mediated walking program for obese adults. Translational behavioral medicine. 2013; 3(4): 357–69. Available from: https://academic.oup.com/tbm/article-abstract/3/4/357/4562886. doi: 10.1007/s13142-013-0211-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Gray GC, Silbey SS. The other side of the compliance relationship. In: Parker C, Nielsen VL, (Eds.). Explaining compliance: Business responses to regulation. Cheltenham: Edward Elgar Publishing; 2011. [Google Scholar]
- 252.Carter MW, Porell FW. Variations in hospitalization rates among nursing home residents: The role of facility and market attributes. The Gerontologist. 2003; 43(2): 175–91. Available from: 10.1093/geront/43.2.175. [DOI] [PubMed] [Google Scholar]
- 253.Haines F. Facing the compliance challenge: Hercules, Houdini or the Charge of the Light Brigade? In: Parker C, Nielsen VL, (Eds.). Explaining compliance: Business responses to regulation. Cheltenham: Edward Elgar Publishing; 2011. [Google Scholar]
- 254.Nielsen HØ, Nielsen VL. Different encounter behaviors: Businesses in encounters with regulatory agencies [Pre-print]. Regulation & Governance. 2022. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/rego.12455. [Google Scholar]
- 255.Waltz TJ, Powell BJ, Fernández ME, Abadie B, Damschroder LJ. Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implementation science. 2019; 14(1): 42. Available from: 10.1186/s13012-019-0892-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Kash BA, Hawes C, Phillips CD. Comparing Staffing Levels in the Online Survey Certification and Reporting (OSCAR) System With the Medicaid Cost Report Data: Are Differences Systematic? The Gerontologist. 2007; 47(4): 480–9. Available from: 10.1093/geront/47.4.480. [DOI] [PubMed] [Google Scholar]
- 257.Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC medicine. 2010; 8(1): 1–11. doi: 10.1186/1741-7015-8-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.McCreight MS, Rabin BA, Glasgow RE, Ayele RA, Leonard CA, Gilmartin HM, et al. Using the Practical, Robust Implementation and Sustainability Model (PRISM) to qualitatively assess multilevel contextual factors to help plan, implement, evaluate, and disseminate health services programs. Translational behavioral medicine. 2019; 9(6): 1002–11. Available from: 10.1093/tbm/ibz085. [DOI] [PubMed] [Google Scholar]
- 259.Toropova A, Björklund C, Bergström G, Elinder LS, Stigmar K, Wåhlin C, et al. Effectiveness of a multifaceted implementation strategy for improving adherence to the guideline for prevention of mental ill-health among school personnel in Sweden: a cluster randomized trial. Implementation science. 2022; 17(1): 23. Available from: 10.1186/s13012-022-01196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Szewczyk Z, Reeves P, Kingsland M, Doherty E, Elliott E, Wolfenden L, et al. Cost, cost-consequence and cost-effectiveness evaluation of a practice change intervention to increase routine provision of antenatal care addressing maternal alcohol consumption. Implementation science. 2022; 17(1): 14. Available from: 10.1186/s13012-021-01180-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Leon N, Lewin S, Mathews C. Implementing a provider-initiated testing and counselling (PITC) intervention in Cape town, South Africa: a process evaluation using the normalisation process model. Implementation science. 2013; 8(1): 97. Available from: 10.1186/1748-5908-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Pope C, Halford S, Turnbull J, Prichard J, Calestani M, May C. Using computer decision support systems in NHS emergency and urgent care: ethnographic study using normalisation process theory. BMC health services research. 2013; 13(1): 111. Available from: 10.1186/1472-6963-13-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Damschroder LJ, Reardon CM, Opra Widerquist MA, Lowery J. Conceptualizing outcomes for use with the Consolidated Framework for Implementation Research (CFIR): the CFIR Outcomes Addendum. Implementation science. 2022; 17(1): 7. Available from: 10.1186/s13012-021-01181-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implementation science. 2022; 17(1): 75. Available from: 10.1186/s13012-022-01245-0. [DOI] [PMC free article] [PubMed] [Google Scholar]