Abstract
Objective:
Childhood brain tumor (BT) survivors are at risk for working memory (WM) and processing speed (PS) deficits, which impact other cognitive domains. This study aimed to characterize WM, PS, and untimed mathematics calculation performance in pediatric BT survivors at least 2 years post-diagnosis, identify medical factors associated with deficits in mathematics, and examine whether WM and/or PS predict mathematics performance in this clinical sample.
Methods:
Retrospective data were gathered from 72 BT survivors between 7 and 21 years of age (M=13.64 y, SD= 4.01 y) for a clinical neuropsychological evaluation. All participants completed Wechsler measures of WM and PS and a measure of untimed mathematics calculation.
Results:
WM, PS, and the mathematics calculation were significantly lower than the normative mean. Math scores were not correlated with any of the examined medical factors. PS was negatively correlated with the Neurological Predictor Scale and positively correlated with age at diagnosis. Both WM and PS were associated with math outcomes and accounted for 30.4% and 19.2% of the variance, respectively.
Conclusions:
The findings indicate that WM and PS contribute to mathematics performance in pediatric BT survivors. Examining mathematics performance should be a part of clinical neuropsychological evaluations. Interventions to improve mathematics performance in this population should also focus on WM and compensatory strategies for slowed PS.
Keywords: mathematics, numerical skills, calculation, oncology
It is well documented that survivors of pediatric brain tumors are at risk for cognitive deficits attributable to disease and treatment factors that impact the Central Nervous System (CNS). These treatment factors include intrathecal chemotherapy, radiation therapy, and neurosurgery, particularly at younger ages when the brain is still developing.1 The Neurological Predictor Scale (NPS;2), a composite score that quantifies cancer-related treatments and neurological complications, is one way to conceptualize the risk factors for greater cognitive deficits in pediatric brain tumors. The NPS, which takes into account pertinent medical factors, including the history of hydrocephalus, seizures, endocrinopathies, and chemotherapy; the extent of and the number of neuro-surgeries; and the type of radiation therapy has been shown to predict cognitive outcomes, including academic achievement in pediatric brain tumor samples.3
Investigations of neurocognitive outcomes in survivors of brain tumors have produced 3 primary models that illustrate the relationship between cognitive skills and treatment. Palmer4 proposed that processing speed (PS) is the primary pathway for cognitive deficits in pediatric medulloblastoma survivors. Specifically, reduced PS impacts selective attention and working memory (WM), which have a downstream impact on overall intellectual functioning (IQ) and academic achievement. In contrast, Wolfe et al5 suggested that attention, WM, PS, and executive functions have an equal and interrelated impact on cognition. King et al6 suggested that the empirical model built upon these earlier theoretical models by demonstrating that PS was the core cognitive skill that negatively impacts other cognitive skills, such as attention and WM. While these models vary in terms of the initial cognitive domain impacted by cancer treatment, they all highlight the role of WM and PS as important underlying constructs that have a downstream impact on the development of other neurocognitive skills. Thus, it is reasonable to consider that these core constructs may be implicated in the math deficits observed in survivors of pediatric brain tumors.
In non-oncology samples, mathematics has been shown to be an academic skill that encompasses component skills such as the understanding of numerical concepts, computational abilities, and the aspects of cognitive proficiency, including math fact automaticity/fluency and WM (eg, holding information in mind to complete a problem).7–10 Cognitive proficiency can also impact the acquisition of math knowledge. For example, PS can affect the rate at which math problems can be solved.11,12 Not surprisingly, research with non-oncology samples has shown that WM and PS are important for math achievement.13–17
Given that WM and PS skills are primarily affected in pediatric brain tumor survivors and have a central role in mathematics skills in otherwise healthy individuals, this study broadly aimed to explore whether deficits in these cognitive domains may help explain high rates of math difficulties in children with a history of brain tumors. Specifically, this study investigated the relationship between working memory and PS on untimed mathematics performance among school-age children with a history of brain tumor treatment. This study aimed to (1) characterize the rates of impairment in WM, PS, and untimed mathematics skills in children referred for a neuropsychological evaluation and treated for a brain tumor; (2) identify medical factors associated with deficits in untimed math calculation; and (3) quantify the degree to which WM and PS contribute to mathematics performance in pediatric brain tumor survivors. It was hypothesized that pediatric brain tumor survivors would demonstrate normative weaknesses in WM, PS, and untimed math calculation; that specific treatment factors such as younger age at diagnosis and higher NPS score would be associated with worse math performance; and that deficits in WM and PS would predict math difficulties observed in this sample.
METHODS
Study Population and Inclusion Criteria
The study was approved by the Johns Hopkins University Institutional Review Board and in accordance with the Helsinki Declaration. Assessment data were gathered from a retrospective medical record review of all children referred for an outpatient clinical neuropsychological evaluation at Kennedy Krieger Institute between 2000 and 2021 after a brain tumor diagnosis and treatment at the Johns Hopkins Hospital. Participants were referred for neuropsychological evaluation by the neuro-oncology medical team (eg, neuro-oncologists, neuro-surgeons, radiation oncologists) or parents. Reasons for the referral included specific cognitive complaints (eg, memory, attention, PS, academics) or as per standard of care guidelines.18 Inclusion criteria for the the sample included age 6 years or older at the time of assessment, diagnosed with a brain tumor before 18 years of age, assessment completed at least 2 years postdiagnosis, completion of either the Wechsler Intelligence Scale for Children, Fourth/Fifth Edition (WISC-IV/V19,20;) or the Wechsler Adult Intelligence Scale, Fourth Edition (WAIS-IV21;), and a measure of untimed mathematics calculation. The Verbal Comprehension Index (VCI) was used as an untimed estimate of intellectual functioning instead of the Full Scale IQ (FSIQ), considering that several primary variables of interest (ie, WM and PS) are highly correlated with the FSIQ, and in fact are used to derive the FSIQ. Participants were excluded if they were on treatment at the time of the neuropsychological evaluation.
Medical Demographics
Neuroimaging reports were reviewed for tumor location (supratentorial, infratentorial, or midbrain). Medical (eg, age at diagnosis, time since diagnosis) and sociodemographic information (eg, race, sex) were extracted from the medical record. Medical severity was determined by calculating the NPS2 at the time of neuropsychological evaluation. This score is a continuous variable that serves as a cumulative index of neuro-oncology risk factors (eg, history of cranial radiation therapy, seizures, endocrine dysfunction). Scores were calculated after a medical record review. Scores range from 0 to 11, with higher scores denoting greater neurological risk.
Working Memory and Processing Speed
Intellectual outcomes were measured using either the WISC-IV/V19,20 or WAIS-IV (WAIS-IV21;) based on the patient’s age at the time of evaluation. For this study, the Working Memory Index (WMI) and Processing Speed Index (PSI) standard scores were used as measures of WM and PS, respectively. Standard scores have a mean of 100 and SD of 15.
Untimed Mathematic Calculation
Untimed math skills were examined using the Numerical Operations subtest from the Wechsler Individual Achievement Test, Third Edition (WIAT-III22) or the Math Computation subtest from the Kaufman Test of Educational Achievement, Third Edition (KTEA-323). Both of these subtests examine untimed math calculation skills. Given that the study was retrospective in nature, the children were administered different academic measures (WIAT-III or KTEA-3) in line with typical practice in this clinical neuropsychology setting. The total Math Calculation score was a composite of these 2 measures, which are strongly correlated with one another (r= 0.80;). Scores were calculated as standard scores, with a mean of 100 and SD of 15.
Statistical Analyses
Descriptive statistics were performed to characterize the medical, demographic, and neuropsychological features of the sample. The Kolmogorov-Smirnov Test was performed, and samples were normally distributed along the Math Calculation, WMI, and PSI scores. One-sample t tests were used to determine how the sample compared with the normative mean. Impairment was calculated using a 1.5 SD cut-off. Pearson or point-biserial correlations were used to investigate the association between demographic and medical factors (eg, sex, age at diagnosis, age at assessment, the time between diagnosis and assessment, NPS score) and mathematics performance. While not a central aim of this study, we also explored correlations between medical variables and WMI and PSI. A correlation was also performed to examine the relationship between WMI and PSI. Given the high collinearity between WMI and PSI (VIF =0.77), 2 separate linear regression models were performed to determine the extent to which WMI and PSI contributed to the math performance.
RESULTS
Participants
Of the 117 patients initially identified, 45 did not meet the inclusion criteria. Please see the Figure 1 for a Consort diagram. Of note, the excluded participants did not significantly differ from included participants in WMI, PSI, or math calculation skills. For the current study, participants included 72 children, adolescents, and young adults between the ages of 7 and 21 years of age (Mean age at assessment = 13.7 y, SD=4.0 y). They were a mean average of 6.0 years postdiagnosis (SD=4.0 y). The majority of participants (48.6%) had a BT in the supratentorial region. Nearly all participants (84%) were treated with surgery, with less than half (40%) also receiving radiation therapy. The 11 patients who did not receive surgery were either monitored (n=5) or treated with chemotherapy (n=6). See Table 1 for sample demographics.
FIGURE 1.
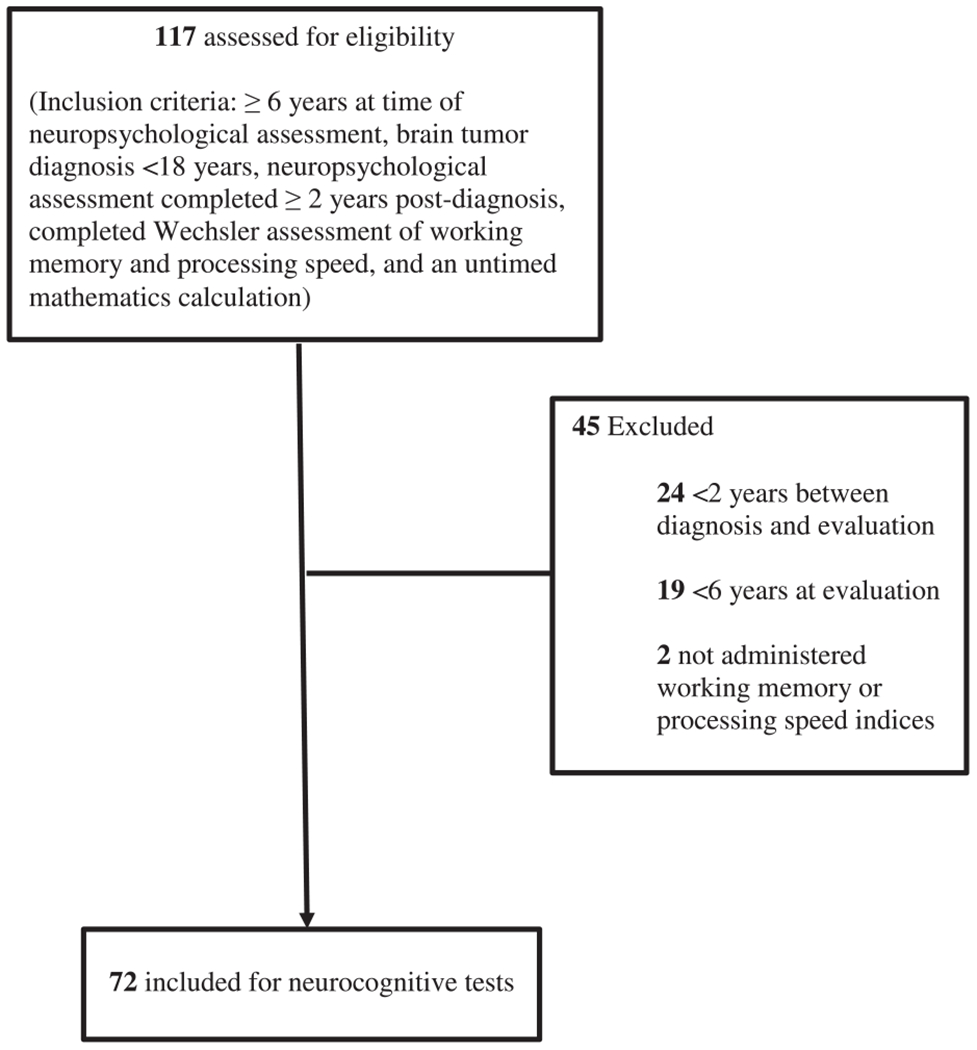
Consort diagram for inclusion and exclusion of study participants.
TABLE 1.
Characteristics of the Brain Tumor Sample
| n (%) | Range | Mean (SD) | |
|---|---|---|---|
| Child sex | |||
| Male | 32 (44.4) | — | — |
| Female | 40 (55.6) | — | — |
| Child race | |||
| White | 46 (63.9) | — | — |
| Black | 11 (15.3) | — | — |
| Hispanic | 3 (4.2) | — | — |
| Asian | 3 (4.2) | — | — |
| Hawaiian | 1 (1.4) | — | — |
| Multi-racial | 3 (4.2) | — | — |
| Not reported | 3 (4.2) | — | — |
| Other | 2 (2.8) | — | — |
| Age at diagnosis (y) | — | 0.5-18.5 | 7.7 (5.0) |
| Age at evaluation (y) | — | 7.2-21.8 | 13.7 (4.0) |
| Time since diagnosis (y) | — | 2.0-16.2 | 6.0 (4.0) |
| NPS | — | 0-10 | 4.8 (2.4) |
| Tumor Location | |||
| Infratentorial | 35 (48.6) | — | — |
| Supratentorial | 18 (25.0) | — | — |
| Midbrain | 19 (26.4) | — | — |
| Lobule* | |||
| Frontal | 10 (13.9) | — | — |
| Parietal | 2 (2.8) | — | — |
| Temporal | 4 (5.6) | — | — |
| Occipital | 3 (4.2) | — | — |
| Midbrain | 19 (26.4) | — | — |
| Cerebellum | 35 (48.6) | — | — |
| Pathology | |||
| Astrocytoma | 16 (22.2) | — | — |
| ATRT | 1 (1.4) | — | — |
| Craniopharyngioma | 8 (11.1) | — | — |
| Ependymoma | 8 (11.1) | — | — |
| Gangliocytoma | 3 (4.2) | — | — |
| Glioma | 14 (19.4) | — | — |
| Germinoma | 4 (5.6) | — | — |
| Central Nervous System Neuroblastoma | 2 (2.8) | — | — |
| Medulloblastoma | 8 (11.1) | — | — |
| Meningioma | 1 (1.4) | — | — |
| Papilloma | 2 (2.8) | — | — |
| Pineoblastoma | 2 (2.8) | — | — |
| PNET | 3 (4.2) | — | — |
| Treatment Completed | |||
| Resection | 61 (84.7) | — | — |
| Chemotherapy | 38 (52.8) | — | — |
| Radiation | 29 (40.3) | — | — |
Value greater than 100% as one participant had multi-lobule involvement.
ATRT indicates Atypical Teratoid Rhabdoid Tumor; NPS, Neurological Predictor Scale score cumulative neuro-oncologic risk score based upon history of hydrocephalus, seizures, endocrinopathies, chemotherapy, extent and number of neuro-surgeries, and type of radiation therapy; PNET, Primitive neuroectodermal tumor.
Sample Performance and Rates of Impairment
Scores on neuropsychological measures (WMI, PSI, and math calculation) were below the normative mean (all P<0.05; Table 2). Of note, while the difference between sample performance and expected performance was statistically significant across all measures, only PSI was clinically significant and fell below the Average range (Standard Score=85.3). In a normal distribution, 6.7% of the population is anticipated to fall 1.5 SD below the mean. Within this study, participants were between 2 and 5 times that value, with 12.7% falling 1.5 SD below the mean on measures of untimed math calculation and WM. Even more (31.9%) participants fell 1.5 SD below the mean on PSI.
TABLE 2.
Working Memory, Processing Speed, and Math Calculation Performance in the Study Participants
| Mean (SD) | Range | Effect Size3 | % Impaired Observed | % Impaired Expected4 | Z-score5 | |
|---|---|---|---|---|---|---|
| WMI1 | 94.45 (15.50)** | 62-33 | 0.36 | 12.68 | 6.68 | 1.47 |
| PSI1 | 85.28 (14.84)*** | 53-117 | 0.98 | 31.88 | 6.68 | 4.74 |
| Math Calculation2 | 94.24 (15.41)** | 61-134 | 0.37 | 12.68 | 6.68 | 1.47 |
Working Memory Index from the Wechsler Intelligence tests.
Processing Speed Index from the Wechsler Intelligence tests.
Composite score of Wechsler Individual Achievement, Third Edition (WIAT-III) Numerical Operations and Kaufman Test of Educational Achievement, Third Edition (KTEA-3) Math Calculation subtests.
Expected rate of impairment based on a normal distribution.
Cohen’s d; small=.2, medium =.5, large =.8.
z-score ratio for the significance of the difference between % impaired observed and % impaired expected.
P<0.05.
P <0.01.
P <0.001.
Correlations with Neuropsychological and Medical Variables
Math calculation was positively correlated with WMI (n= 70, r=0.55, P<0.001) and PSI (n= 68, r=0.44, P<0.001), such that higher math performance was associated with stronger WM and PS outcomes. Math was not significantly correlated with NPS, age at diagnosis, age at evaluation, or time since evaluation (all P>.05) and thus not included in the regression model.
In exploring associations between medical variables and cognitive outcomes, PSI was negatively correlated with NPS (n= 68, r=−0.26, P= 0.03), such that faster PS was associated with a lower NPS score (a proxy for fewer neurocognitive risk factors). PSI was also positively correlated with age at diagnosis (n= 69, r=0.24, P= 0.04), such that older children at the time of diagnosis had faster PS abilities. WMI was not correlated with any of the medical variables examined.
Contributions to Math Calculation
There was high multicollinearity between WMI and PSI (VIF =−0.77). Thus, 2 linear regression models were performed to examine the contributions of WMI and PSI to math scores, respectively (Tables 3 and 4). The overall WMI regression model was significant F(1,68) = 29.77, P=0.000; WMI accounted for 30.4% of the variance in math calculation scores. The overall PSI regression model was also significant [F(1,66)= 15.66, P=0.000] and accounted for 19.2% of the variance in math calculation scores.
TABLE 3.
Prediction of Math Calculation by Working Memory and Processing Speed
| R2 Total | Unstandardized ß | |||
|---|---|---|---|---|
| ß | ß | P | ||
| Analysis 1: Math Calculation | ||||
| Working Memory | 0.566 | 0.552 | < 0.001 | |
| 0.304 | ||||
| Analysis 2: Math Calculation | ||||
| Processing Speed | 0.461 | 0.438 | < 0.001 | |
| 0.192 | ||||
TABLE 4.
Correlational Matrix of Neuropsychological Outcomes and Significant Medical Variables
| Math Calculation | WMI | PSI | NPS | |
|---|---|---|---|---|
| Math Calculation | ||||
| WMI1 | 0.55*** | — | — | — |
| PSI2 | 0.44*** | 0.50*** | — | — |
| NPS3 | −0.11 | −0.18 | −0.28*** | — |
| Age at Diagnosis | 0.01 | 0.13 | 0.26* | 0.18 |
P<0.05.
P <0.01.
P <0.001.
NPS indicates Neurologic Predictor Scale; PSI, Processing Speed Index; WMI, Working Memory Index.
DISCUSSION
This study had 3 aims: (1) to characterize rates of impairment in WM, PS, and untimed mathematics skills in children referred for a neuropsychological evaluation and treated for pediatric brain tumor; (2) to identify medical factors associated with deficits in untimed math calculation; and (3) to quantify the degree to which WM and PS contribute to mathematics performance in pediatric brain tumor survivors.
First, consistent with research on academic outcomes after the treatment for childhood cancer,24,25 mathematic calculation is an area of significant weakness in this population. In our sample, nearly 13% of participants had math calculation skills that fell at least 1.5 SD below the normative mean. WM and PS, which are core cognitive skills thought to be impacted by cancer treatment, were also areas of weakness, with 13 to 32% performing 1.5 SD below the mean, respectively. While we utilized data from patients at least 2 years out from diagnosis, other studies have shown that declines in cognitive functioning can emerge on standardized tests as early as 1 year after diagnosis.26
We also found that both WM and PS contributed to untimed mathematics calculation in childhood brain tumor survivors at least 2 years after diagnosis. It is possible that slower PS affects the speed with which information can be accessed from one’s long-term memory as well as the speed of problem-solving, thereby taxing one’s WM. Our findings are consistent with the theoretical models that have suggested that both WM and processing have a cascading effect on other cognitive and academic domains in pediatric BT survivors.4–6 Of note, this study did not examine causation, and our findings do not further elucidate the primary versus secondary core cognitive constructs impacted by cancer treatment. However, these findings are relevant given that cognitive rehabilitation studies have tended to focus on interventions that strengthen WM and/or mathematics skills in this population27,28 without considering the role of PS. Given that both WM and PS contribute to mathematics performance, these findings provide preliminary evidence that slowed PS may also be important when considering appropriate interventions.
In addition, specific medical variables were correlated with neuropsychological outcomes. Younger age at diagnosis was associated with slower PS—a finding that has been well documented in the pediatric oncology literature.29 Interestingly, NPS was associated with PS but not WM or mathematics. Our results may indicate that PS is more vulnerable than WM to medical factors such as hydrocephalus, seizures, cranial radiation, and chemotherapy, which are all captured by the NPS. In addition, our findings are consistent with previous work that showed NPS-predicted PS outcomes in pediatric oncology survivors more so than attention or working memory.30 Untimed math calculation was not associated with the medical variables examined in this sample, specifically NPS score, age at diagnosis, age at neuropsychological evaluation, or time since diagnosis. While this diverges from work by Kautiainen et al,3 who found an association between NPS and mathematical skills, it is consistent with Karlson et al31 who did not find a relationship between the NPS score (cancer diagnosis, age at diagnosis, age at evaluation, time since diagnosis, or sex) and mathematical skills. In their study, whole brain radiation dosimetry and referral sources predicted mathematics performance. This may suggest that there are nuances to CNS cancer treatment that impact patients and cognitive outcomes as well as individual risk and resiliency factors not captured by the NPS.
In light of these findings, several limitations warrant consideration. First, the relatively small sample size may have impacted our statistical power. This may explain why other well-documented risk factors (ie, younger age at diagnosis, NPS score) did not emerge as significant predictors. As a means of increasing sample size, this study included a heterogenous oncology population with respect to tumor pathology and treatment variables (type, intensity). Therefore, results cannot be generalized to any specific oncological condition. Inherent to retrospective clinical data, academic measures were based on clinician preference. While the different measures of untimed math calculation from the KTEA-3 and WIAT-III are highly correlated with one another, possible differences in norms between the test versions may exist. The test order may also have contributed to neuropsychological outcomes. Again, as these measures were administered as part of a clinical evaluation, the test order was not randomized. Thus, it is possible that participants were fatigued towards the end of testing, and the academic measures were possibly administered after many other neuropsychological measures. In addition, some data were not available, such as separated digit span forward and backward scores, that would better identify whether attention versus WM differentially impact math performance. An additional limitation of this study is the lack of information related to school absence. Children with a history of an oncology diagnosis have higher rates of school absence secondary to medical appointments, immunocompromised health status, and treatment side effects.32 While school absence can result in inconsistency or gaps in instruction, we cannot delineate the impact of school absence on mathematics performance in this clinical sample. Lastly, this was a clinically referred sample; thus, the results may not entirely generalize to a nonreferred, general treatment cohort.
There are many future directions that warrant discussion as well. Studies should consider the role of WM and PS on other speed-based academic skills, such as academic fluency, to determine if these core skills further predict timed measures. In addition, given that oral PS has been found to predict cognitive outcomes in pediatric BT survivors,30 it would be important to examine whether different types of speed (ie, oral, graphomotor) differentially predict academic skills in this population. Lastly, given the high rates of school absenteeism in pediatric oncology patients, studies should examine the role of school attendance on academic skills.
In summary, WM and PS, which are particularly vulnerable cognitive skills among pediatric brain tumor samples,4–6 contributed to math performance. The relationship between WM and PS and mathematics has been proposed both in typically developing populations33–35 and other medical populations,36,37 and has not been shown to contribute to outcomes in brain tumor samples. As such, cognitive treatments to address these core cognitive functions may reduce the risks of subsequent math difficulties. Examining mathematic calculation skills should be a part of clinical neuropsychological batteries when working with this population. In addition, interventions to improve mathematics performance in this population should also consider strategies to improve WM and compensatory strategies for slowed PS.
ACKNOWLEDGMENTS
The authors thank the patients and their contribution to this study, as well as the clinicians in the Kennedy Krieger Institute Department of Neuropsychology.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Ris MD, Noll RB. Long-term neurobehavioral outcome in pediatric brain-tumor patients: Review and methodological critique. J Clin Exp Neuropsychol. 1994;16:21–42. [DOI] [PubMed] [Google Scholar]
- 2.Micklewright JL, King TZ, Morris RD, et al. Quantifying pediatric neuro-oncology risk factors: development of the neurological predictor scale. J Child Neurol. 2008;23:455–458. [DOI] [PubMed] [Google Scholar]
- 3.Kautiainen RJ, Na SD, King TZ. Neurological predictor scale is associated with academic achievement outcomes in long-term survivors of childhood brain tumors. J Neurooncol. 2019;142:193–201. [DOI] [PubMed] [Google Scholar]
- 4.Palmer SL. Neurodevelopmental impact on children treated for medulloblastoma: a review and proposed conceptual model. Dev Disabil Res Rev. 2008;14:203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wolfe KR, Madan-Swain A, Kana RK. Executive dysfunction in pediatric posterior fossa tumor survivors: a systematic literature review of neurocognitive deficits and interventions. Dev Neuropsychol. 2012;37:153–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.King TZ, Ailion AS, Fox ME, et al. Neurodevelopmental model of long-term outcomes of adult survivors of childhood brain tumors. Child Neuropsychol. 2019;25:1–21. [DOI] [PubMed] [Google Scholar]
- 7.Fürst AJ, Hitch GJ. Separate roles for executive and phonological components of working memory in mental arithmetic. Mem Cognit. 2000;28:774–782. [DOI] [PubMed] [Google Scholar]
- 8.Geary DC. Learning disabilities in arithmetic: Problem-solving differences and cognitive deficits. Handbook Learn Disabil. 2003;1:199–212. [Google Scholar]
- 9.Imbo I, Vandierendonck A. The role of phonological and executive working memory resources in simple arithmetic strategies. European J Cognit Psychol. 2007;19:910–933. [Google Scholar]
- 10.Imbo I, Vandierendonck A, De Rammelaere S. The role of working memory in the carry operation of mental arithmetic: Number and value of the carry. Q J Exp Psychol. 2007;60:708–731. [DOI] [PubMed] [Google Scholar]
- 11.Fuchs LS, Fuchs D, Stuebing K, et al. Problem solving and computational skill: Are they shared or distinct aspects of mathematical cognition? J Educ Psychol. 2008;100:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geary DC. Mathematical disabilities: cognitive, neuropsychological, and genetic components. Psychol Bull. 1993;114:345. [DOI] [PubMed] [Google Scholar]
- 13.Bull R, Espy KA, Wiebe SA. Short-term memory, working memory, and executive functioning in preschoolers: Longitudinal predictors of mathematical achievement at age 7 years. Dev Neuropsychol. 2008;33:205–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Child AE, Cirino PT, Fletcher JM, et al. A cognitive dimensional approach to understanding shared and unique contributions to reading, math, and attention skills. J Learn Disabil. 2019;52:15–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mabbott DJ, Bisanz J. Computational skills, working memory, and conceptual knowledge in older children with mathematics learning disabilities. J Learn Disabil. 2008;41:15–28. [DOI] [PubMed] [Google Scholar]
- 16.Peng P, Namkung J, Barnes M, et al. A meta-analysis of mathematics and working memory: Moderating effects of working memory domain, type of mathematics skill, and sample characteristics. J Educ Psychol. 2016;108:455. [Google Scholar]
- 17.Willcutt EG, Petrill SA, Wu S, et al. Comorbidity between reading disability and math disability: Concurrent psychopathology, functional impairment, and neuropsychological functioning. J Learn Disabil. 2013;46:500–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walsh KS, Noll RB, Annett RD, et al. Standard of care for neuropsychological monitoring in pediatric neuro-oncology: Lessons from the Children’s Oncology Group (COG). Pediatr Blood Cancer. 2016;63:191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wechsler D. Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV). San Antonio, TX: Pearson; 2003. [Google Scholar]
- 20.Wechsler D. Wechsler Intelligence Scale for Children, Fifth Edition (WISC-V). San Antonio, TX: Pearson; 2014. [Google Scholar]
- 21.Wechsler D. Wechsler Adult Intelligence Scale, Fourth Edition (WAIS-IV). San Antonio, TX: Pearson; 2008. [Google Scholar]
- 22.Wechsler D. Wechsler Individual Achievement Test, Third Edition. San Antonio, TX: Pearson; 2009. [Google Scholar]
- 23.Kaufman AS, Kaufman NL. Kaufman Test of Educational Achievement, Third Edition (KTEA-3). Bloomington, MN: NCS Pearson; 2014. [Google Scholar]
- 24.Kaemingk KL, Carey ME, Moore IM, et al. Math weaknesses in survivors of acute lymphoblastic leukemia compared to healthy children. Child Neuropsychol. 2004;10:14–23. [DOI] [PubMed] [Google Scholar]
- 25.Moore IMK, Hockenberry MJ, Krull KR. Cancer-related cognitive changes in children, adolescents and adult survivors of childhood cancers. Semin Oncol Nurs. 2013;29:248–259. [DOI] [PubMed] [Google Scholar]
- 26.Moxon-Emre I, Bouffet E, Taylor MD, et al. Impact of craniospinal dose, boost volume, and neurologic complications on intellectual outcome in patients with medulloblastoma. J Clin Oncol. 2014;32:1760–1768. [DOI] [PubMed] [Google Scholar]
- 27.Mabbott DJ, Penkman L, Witol A, et al. Core neurocognitive functions in children treated for posterior fossa tumors. Neuropsychology. 2008;22:159. [DOI] [PubMed] [Google Scholar]
- 28.Moore IM, Hockenberry MJ, Anhalt C, et al. Mathematics intervention for prevention of neurocognitive deficits in childhood leukemia. Pediatr Blood Cancer. 2012;59:278–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krull KR, Hardy KK, Kahalley LS, et al. Neurocognitive outcomes and interventions in long-term survivors of childhood cancer. J Clin Oncol. 2018;36:2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Semmel ES, Quadri TR, King TZ. Oral processing speed as a key mechanism in the relationship between neurological risk and adaptive functioning in survivors of pediatric brain tumors. Pediatr Blood Cancer. 2020;67:e28575. [DOI] [PubMed] [Google Scholar]
- 31.Karlson CW, Sarver DE, Raiker JS, et al. The contribution of neurocognitive functions to academic and psychological outcomes in pediatric cancer: A latent profile analysis. Child Neuropsychol, . (2020);26:881–899. [DOI] [PubMed] [Google Scholar]
- 32.French AE, Tsangaris E, Guger S, et al. School attendance in childhood cancer survivors. J Clin Oncol. 2011;29(15_suppl):9581–9581. [Google Scholar]
- 33.LeFevre J-A, DeStefano D, Coleman B, et al. Mathematical cognition and working memory. In: Campbell JID, ed. Handbook of Mathematical Cognition. London, England: Psychology Press; 2005:361–377. [Google Scholar]
- 34.Mazaheri M, Zhanoori F. The role of cognitive factors of attention, processing speed and working memory in predicting math learning disorder in primary school children. J Educ Psychol Stud. 2021;18:171–187. [Google Scholar]
- 35.Raghubar KP, Barnes MA, Hecht SA. Working memory and mathematics: a review of developmental, individual difference, and cognitive approaches. Learn Individ Differ. 2010;20:110–122. [Google Scholar]
- 36.Peterson RK, Williams S, Janzen L. Cognitive correlates of math performance in school-aged children with sickle cell disease and silent cerebral infarcts. Arch Clin Neuropsychol. 2021;36:465–474. [DOI] [PubMed] [Google Scholar]
- 37.Richard AE, Hodges EK, Heinrich KP. Visual attention and math performance in survivors of childhood acute lymphoblastic leukemia. Arch Clin Neuropsychol. 2018;33:1015–1023. [DOI] [PubMed] [Google Scholar]


