Abstract
Background and Objectives
Although the importance of pediatric-to-adult health care transition (HCT) has been recognized, individuals with childhood-onset neurologic conditions often encounter challenges during pediatric-to-adult HCT, and HCT benefits for this population remain elusive. We assessed the current HCT situation in individuals with childhood-onset neurologic conditions to develop an improved transition system that incorporates patient perspectives.
Methods
This cross-sectional study was conducted at the Tokyo Metropolitan Kita Medical and Rehabilitation Center for the Disabled from November 2020 to December 2020. We targeted adults with childhood-onset neurologic conditions who visited the Department of Internal Medicine and their families. Questionnaires provided to 127 patients asked them about their experiences with pediatric-to-adult HCT (i.e., educational opportunities regarding HCT during pediatric visits, difficulties in transition, and the merits/demerits of adult practice) and their families' perspectives regarding pediatric-to-adult HCT. We also reviewed the patients' medical records to examine the severity of their disabilities.
Results
Responses were collected from 111 patients (response rate: 87%). Most patients had both severe physical and intellectual disabilities, and approximately half had a physical disability level of Gross Motor Function Classification System V and a profound intellectual disability. Half of the respondents were not transitioned through pediatric-to-adult HCT by their pediatricians, and they visited adult departments by themselves without a formal referral process. They experienced difficulties during HCT, such as a lack of knowledge regarding adult health care providers and consultants. However, those who underwent HCT benefited from it in terms of their health, experience, and service use, such as age- and condition-appropriate care, seeing adult specialists, and the introduction of adult services. They also addressed challenges in managing appointments and having adult doctors understand their medical history. Nonetheless, they were not informed about diseases and medical and welfare resources for adulthood during pediatric visits and desired to discuss future plans with pediatricians.
Discussion
Systems that provide sufficient pediatric-to-adult HCT for individuals with childhood-onset neurologic conditions are required. Lifelong education for patients and families, training for pediatricians on HCT and neurologists on childhood-onset conditions and disabilities, and clinical practice and human resources that support patients and families are warranted.
Pediatric-to-adult health care transition (HCT) is a process that supports young people in their transition from family-centered pediatric care to person-centered adult health care. Structured HCT for young patients with chronic conditions potentially improves adherence to care, quality of life, and satisfaction with care.1 Transition programs for people with childhood-onset neurologic conditions exist,2,3 and the Japanese Society of Neurology recently issued a statement in 2022 indicating that neurologists should cooperate with pediatric-to-adult HCT for this population.4 However, certain disparities between pediatric and adult health care remain. Even if a patient could continue visiting a pediatrician as a young adult, when the patient grows older or their pediatrician relocates, they eventually need to consult doctors in the adult department without any educational preparation. Consequently, patients and their families encounter several challenges, for example, a lack of awareness regarding the management of appointments with multiple adult specialists due to previous experience involving the exclusive engagement of a single pediatrician who covered a wide range of medical problems. Adult practitioners may also be hesitant to entertain them because of their limited experience in treating people with childhood-onset diseases.5 As a result, patients are potentially lost to regular follow-up, leading to a deterioration of their conditions.6 Patient perspectives have recently become essential in assessing the outcomes of interventions.7,8 We have come to recognize the relevance of individuals' experiences of medical care, population health, and their perspectives regarding medical usage and costs (Triple Aim) in evaluating the effectiveness of transitional care.9 Therefore, we ought to incorporate patient perspectives in the development of systems that serve individuals with childhood-onset conditions who undergo HCT to adult medical care and provide them with adequate preparation.
The Tokyo Metropolitan Kita Medical and Rehabilitation Center for the Disabled is a comprehensive medical facility that was established in Tokyo in 1985. The hospital provides medical care, respite care, and rehabilitation for individuals with disabilities from childhood to adulthood. Most patients have childhood-onset neurologic conditions, such as cerebral palsy or epilepsy syndrome and profound intellectual and multiple disabilities (PIMD). On recognizing the importance of HCT, we have conducted regular in-hospital pediatrician-neurologist transition consultation meetings since 2019. We previously reported that adjustment of treatment, patient education, and promotion of community-based care are essential in pediatric-to-adult HCT for individuals with childhood-onset neurologic conditions.10 Further research is required to examine patients' and caregivers' satisfaction with post-HCT treatment, experience of patient education, and utilization of community-based care due to HCT.
Therefore, this study aimed to determine whether individuals with childhood-onset neurologic conditions experience benefits or challenges from HCT. In this study, we investigated the current status of HCT from the patients' perspectives using a self-administered questionnaire and review of medical records to build a transition system that incorporates patient input.
Methods
Study Sample
This cross-sectional study used a paper-based, structured, self-administered questionnaire provided at the Tokyo Metropolitan Kita Medical and Rehabilitation Center for the Disabled. Adult patients with childhood-onset neurologic conditions who visited the hospital's Department of Internal Medicine between November 17, 2020, and December 31, 2020, and their families were included in this study. These patients sought adult medical care. As all patients with childhood-onset neurologic conditions received a certain degree of pediatric care before visiting the hospital's Department of Adult Internal Medicine, we assumed that all study participants had undergone pediatric-to-adult HCT. We excluded those to whom we were unable to directly explain the nature of the study and those who had intellectual disabilities that rendered it difficult for them to personally consent to participate in the study and had no primary caregiver to accompany them to the hospital. The corresponding author (M.O.) recruited patients and their families for the study when they visited the hospital. Written consent was obtained from all patients or their families. When patients had severe intellectual disabilities, consent was obtained from their family members on their behalf. The questionnaires were subsequently distributed, and participants were asked to return them by mail or hand on completion. Where patients could not respond to questions owing to intellectual disabilities, primary caregivers (family members in all cases) were required to answer on their behalf.
Demographics of Patients With Childhood-Onset Neurologic Conditions
The questionnaire comprised questions on demographics, utilization of medical devices, living arrangements (i.e., living with family or alone), daily activities, and medical care and welfare service utilization as background information. In addition to the questionnaire survey, we reviewed the participants' medical records to examine their current medical conditions and treatments, such as diagnoses and prescriptions. To confirm the level of disability, 3 neurologists (M.O., C.T., and Y.M.) reviewed the patients' medical records. First, they independently graded physical and intellectual disability levels using the Gross Motor Function Classification System (GMFCS)11 and Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), respectively.12 Thereafter, disability levels were determined via discussion if any disagreements arose among neurologists.
HCT Experiences of Patients With Childhood-Onset Neurologic Conditions
To evaluate the HCT situation in individuals with childhood-onset neurologic conditions, the questionnaire included questions on patients' experiences with HCT. The HCT experience items were categorized into the following 3 sections:
Before transition: In the questionnaire, participants had to indicate (1) who referred the patient when they attempted to visit the adult department either in our hospital or in another hospital (primary pediatrician; other physicians, such as psychiatrists, among others; or no referral) and (2) the patient's age (years) at transition and time taken from the transition decision to implementation (months).
During transition: Participants had to indicate (1) whether they experienced any difficulties with HCT (yes or no) and, for those who answered yes, (2) the reasons for the difficulties on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree), using the following response options: “No information regarding adult health care providers,” “No information on who to consult regarding transition,” “Physician did not understand the patient's medical history,” “Physician did not understand the patient's and their family's feelings,” “Hesitation by the physician because of the disease,” “Hesitation by the physician because of the disability,” and “Treated like a child.” We dichotomized “strongly agree” and “agree” as “yes.”
After transition: Participants had to answer multiselect multiple-choice questions in response to the following items concerning (1) the benefits of adult practice: “Age- and condition-appropriate care,” “Ability to consult adult specialists,” “Health condition stabilized,” “Introduction to adult-service use,” “Ability to prepare for the future,” “Informed regarding current health condition and prognosis,” “Informed regarding adult services,” and “Few merits” and (2) the challenges of adult practice: “No challenges,” “Handling scheduled appointments in multiple departments,” “Difficulty in having doctors understand medical history,” “Burdensome to consult with a home doctor first when changes in health condition occurred,” “Difficulty in understanding doctor's explanation,” and “Shocked when you learned about your present health condition and prognosis.”
Patient Education Experiences of Individuals With Childhood-Onset Neurologic Conditions
As patient education is critical in developing self-management skills and decision making,13 we investigated patients' and families' experiences and knowledge related to the patients' health conditions. We developed questions concerning the provision of information by pediatricians to families regarding the patients' conditions based on the National Survey of Children's Health in the United States14 and Measure of Process of Care.15 Questionnaire items regarding patients' experiences in receiving information from pediatricians included the following: “Provision of a summary of their medical history,” “Treatment options,” “Long-term care plan,” “Merit/demerit of transition,” and “Services for adults with disabilities.” Questionnaire items regarding families' knowledge about patients' conditions included the following: “Effects of oral medication,” “The formal name of the disease,” “Ability to explain their medical history,” “Knowledge regarding the adverse effects of medication,” “Common complications of their primary disease,” “Natural history of the disease,” and “Symptoms requiring consultation with a doctor.” Participants' responses were based on a 5-point Likert sale, ranging from “strongly agree” and “agree” (categorized as “yes” in the analysis), “neutral,” and “disagree” and “strongly disagree” (categorized as “no/uncertain”), and we treated a missing response as a “no response.”
Patients' and Families' Opinions Toward HCT
To obtain feedback from patients and their families regarding their experiences, we drew patients' and families' opinions regarding HCT. First, we questioned the optimal age for initiating discussions regarding transition and the appropriate age of transition and asked participants to indicate their age on the form. Furthermore, to determine the topics on which patients and families required further training and the training extent, we asked whether they desired further discussion regarding the following topics: “Prognosis and natural history of the disease,” “General information on the disease, such as treatment,” “Services for adults with disabilities,” “The reason for the selected treatment,” “Daily life of adults with disabilities,” and “Preparations required of parents before ceasing to take care of their children.” Participants' responses were based on a 5-point Likert sale, ranging from “strongly agree” and “agree” (categorized as “yes” in the analysis), “neutral,” and “disagree” and “strongly disagree” (categorized as “no/uncertain”), and we treated a missing response as a “no response.” Regarding desired systems that support pediatric-to-adult HCT, participants answered multiselect multiple-choice questions in response to the following items: “Coordinator/social worker,” “Transition center,” “Educational programs for patients and families from early childhood,” and “Transition visit for adolescents.”
Statistics
First, we described the demographics of the patients and their families. Second, we described the medical care and welfare services that the patients had received. Third, we described the participants' experiences with pediatric-to-adult HCT. Finally, we described the patient education status and elicited patients' and families' opinions regarding HCT. Analyses were performed using Stata/IC (version 16; STATA Corp, College Station, TX).
Standard Protocol Approvals, Registrations, and Patient Consents
This study was approved by the Institutional Review Boards of Tokyo Medical and Dental University (M2020-168) and Tokyo Metropolitan Kita Medical and Rehabilitation Center for the Disabled (2020-6). All the participants provided written informed consent.
Data Availability
Questionnaires and study data are available on request from the corresponding author (M.O.).
Results
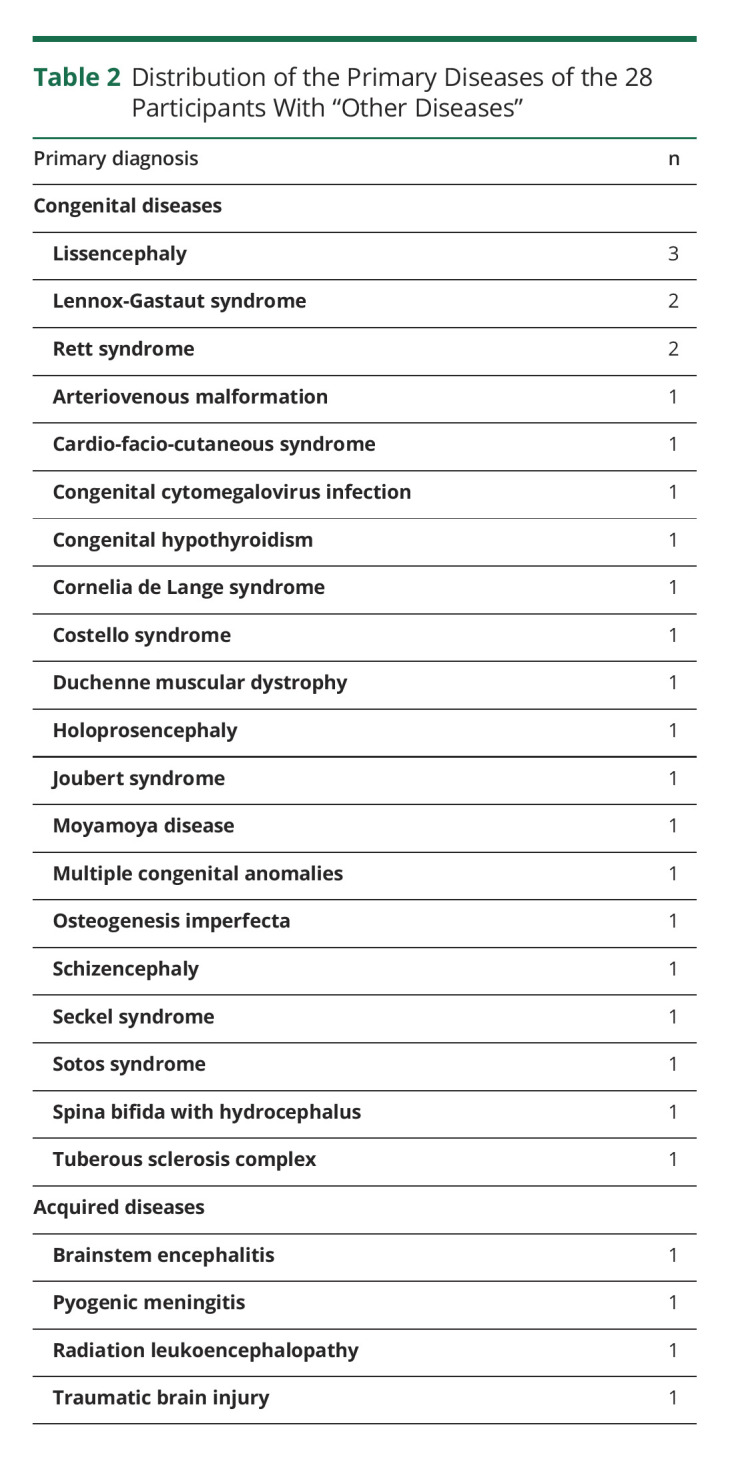
Between November 17, 2020, and December 31, 2020, 213 adult patients with childhood-onset neurologic conditions visited the Department of Internal Medicine. Of these patients, 133 patients were contacted in person. Therefore, we recruited 133 patients and their caregivers, 127 of whom eventually agreed to participate in this study. Finally, we collected completed questionnaires from 111 patients (response rate, 87.4%) (Table 1). The most frequent primary disease was cerebral palsy (CP) (36.9%). Approximately half of the participants had severe physical disability equivalent to GMFCS V (44.1%) and profound intellectual disability (52.3%) based on the DSM-5. Participants used medical devices at home, such as tube feeding (13.5%), and accessed various medical care and welfare services under the Japanese medical and welfare service systems.16 Table 2 shows the distribution of the “Other diseases” of the 28 participants mentioned in Table 1. Tables 1 and 2 reveal that study participants predominantly had congenital or genetic disorders.
Table 1.
Demographics, Medical Care, and Welfare Services of 111 Participants
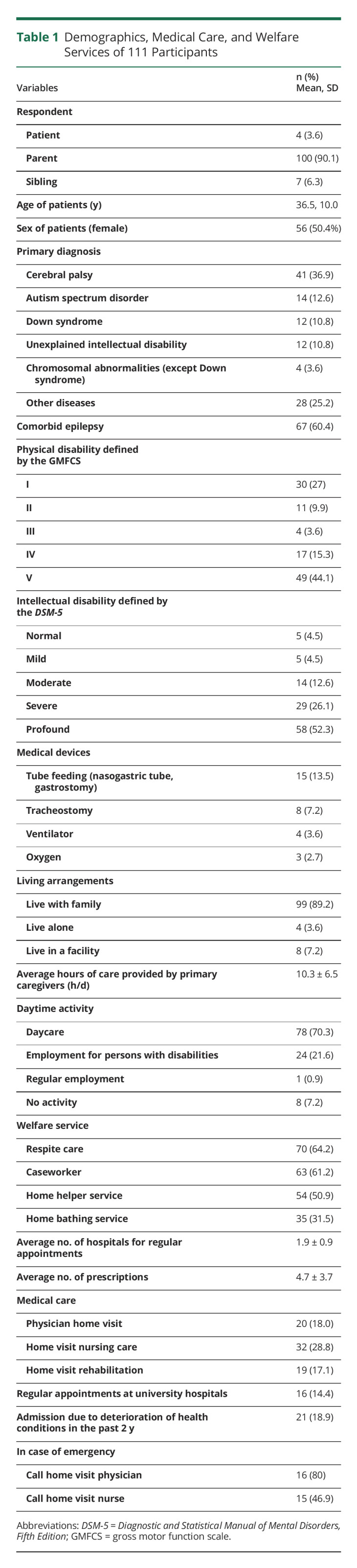
Table 2.
Distribution of the Primary Diseases of the 28 Participants With “Other Diseases”
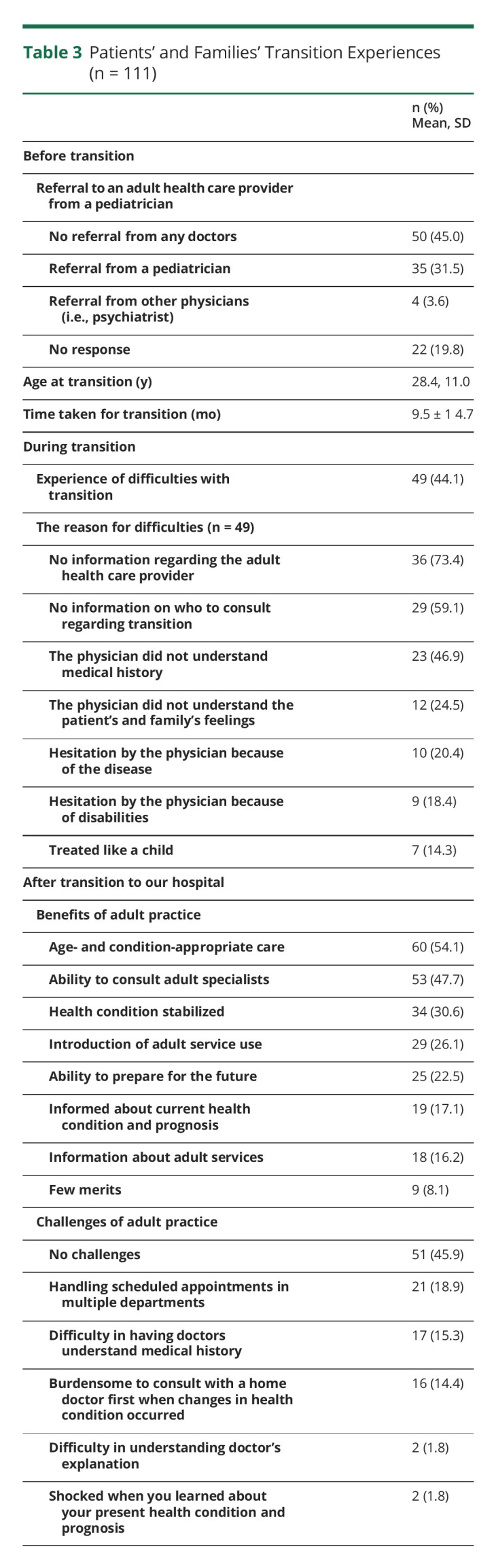
Patients' Experiences With Pediatric-to-Adult HCT
Table 3 summarizes the experience of patients and their families with pediatric-to-adult HCT. In terms of referral, one-third of the participants (31.5%) were referred by a pediatrician; nevertheless, approximately half (45.0%) did not receive any referral and visited the Department of Internal Medicine on their own accord. Approximately half (44.1%) of the patients experienced difficulties during transition. The difficulties were related to a lack of guidance on HCT, such as a lack of information regarding health care providers (73.4%) and on who to consult (59.1%); hesitation by adult practitioners due to patients' diseases (20.4%); and disabilities (18.4%). However, those who underwent HCT benefited from it in terms of their health, experience, and service use, such as age- and condition-appropriate care (54.1%), seeing adult specialists (47.7%), stabilized health condition (30.6%), and the introduction of adult services (26.1%). They also managed to address challenges such as handling scheduled appointments in multiple departments (18.9%), burdensome to consult with a home doctor first when changes in health condition occurred (14.4%), and having adult doctors understand their medical history (15.3%). These results suggest that pediatric care and adult practice are disintegrated when it comes to individuals with childhood-onset neurologic conditions, thus posing various challenges for patients and families during pediatric-to-adult HCT.
Table 3.
Patients' and Families' Transition Experiences (n = 111)
Patient Education
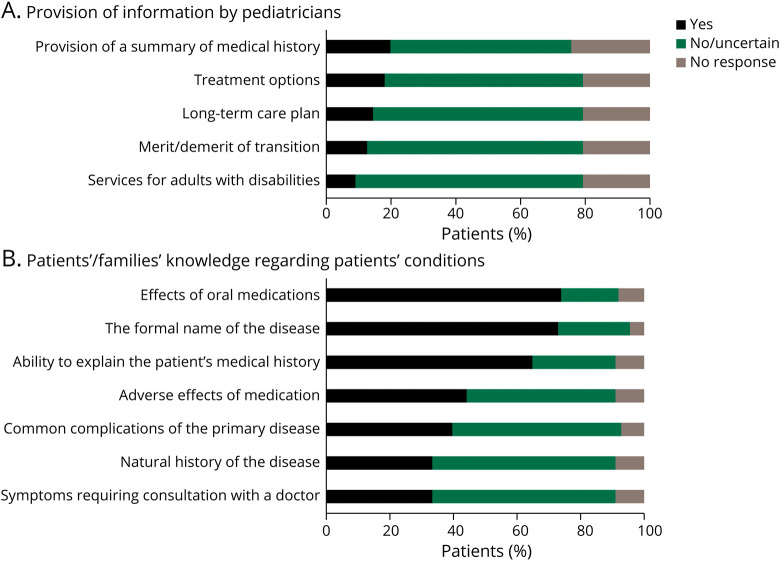
We asked the participants about their experiences with receiving information from their pediatricians (Figure 1A). Only 20% of the patients received a summary of their medical history and guidance for them and their families to make informed decisions regarding treatment options. Furthermore, less than 15% had discussions regarding long-term care plans and received information on pediatric-to-adult HCT.
Figure 1. Patient Education in Childhood-Onset Neurologic Conditions.
(A) Provision of information by pediatricians. Patients and their families were asked about their experiences with receiving information from their pediatricians. Their responses were based on a 5-point Likert scale; “strongly agree” and “agree” are denoted as “yes,” whereas “undecided,” “disagree,” and “strongly disagree” are denoted as “no/uncertain.” Where patients did not respond, their response is denoted as “no response.” (B) Patients' and families' knowledge regarding patients' conditions. Patients and families were asked whether they were aware of the patients' conditions using a 5-point Likert scale; “strongly agree” and “agree” are demoted as “yes,” whereas “undecided,” “disagree,” and “strongly disagree” are denoted as “no/uncertain.” Where patients did not respond, their response is denoted as “no response.”
We asked about the patients' and families' knowledge of their diseases (Figure 1B). Over 70% indicated that they understood the purpose of the prescribed drugs, knew the formal name of the disease, and could explain their medical history to others. However, more than half of them were unaware of typical complications, the natural history of the disease, or symptoms requiring consultation with a doctor.
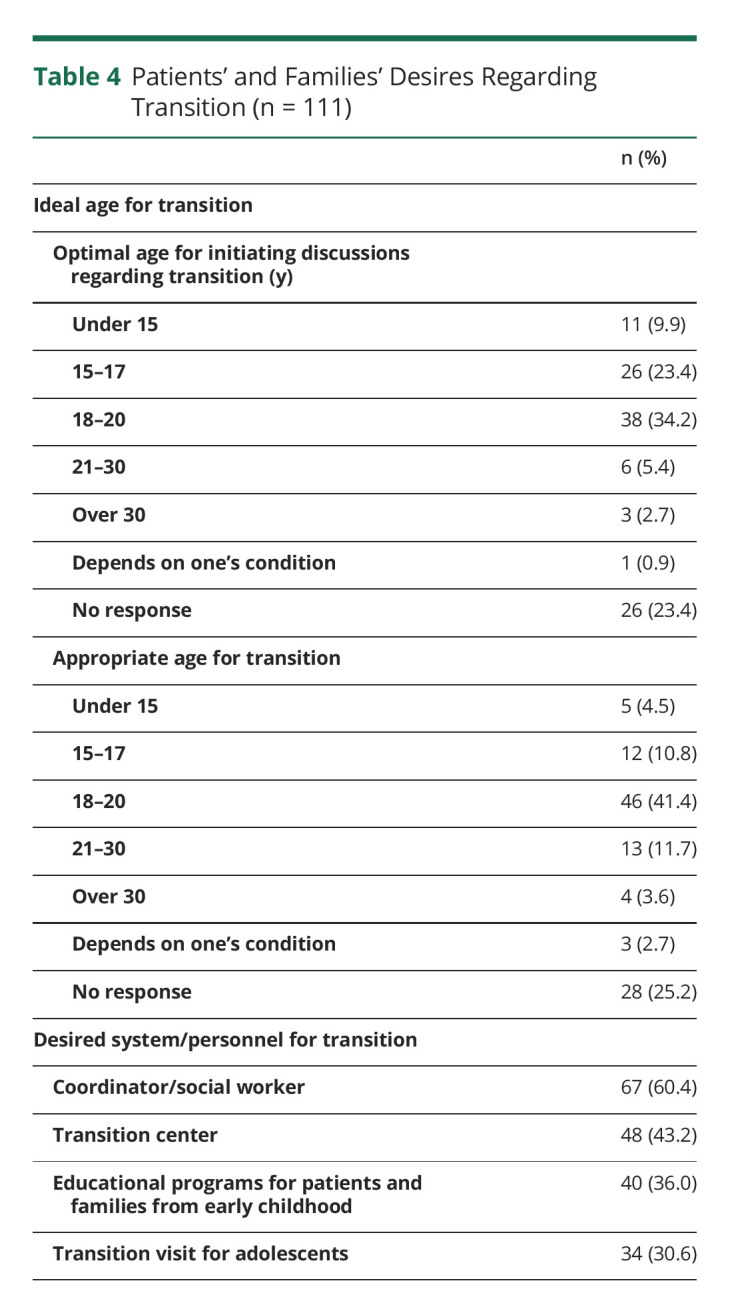
Patients' and Families' Opinions
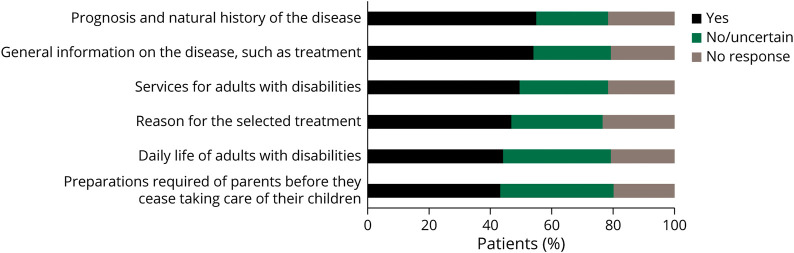
In terms of patients' and families' opinions, 40%–60% of patients/families indicated that they desired further discussion with pediatricians regarding their prognosis and the natural history of the disease, treatment, services, and preparations for the future (Figure 2). Regarding their current HCT experiences, we asked participants about their ideal age and desired system for transition (Table 4). One-third (34.2%) and one-fourth (23.4%) of the participants considered ages of 18–20 and 15–17 years to be optimal age for initiating discussions regarding transition, respectively. Furthermore, 41.4% indicated ages of 18 and 20 years to be appropriate timing for pediatric-to-adult HCT. In terms of the desired systems that support pediatric-to-adult HCT, patients and families desired the following: specialized coordinators to consult (60.4%), transition centers (43.2%), education programs for patients and families (46.0%), and specialized transition visits for adolescents (30.6%).
Figure 2. Topics on Which Families Desired Further Discussion With Pediatricians.
Patients and families were asked to indicate the topics related to their conditions on which they desired further training from pediatricians using a 5-point Likert scale; “strongly agree” and “agree” are denoted as “yes,” whereas “undecided,” “disagree,” and “strongly disagree” are denoted as “no/uncertain.” Where patients did not respond, their response is denoted as “no response.”
Table 4.
Patients' and Families' Desires Regarding Transition (n = 111)
Discussion
This study revealed the current status of pediatric-to-adult HCT in individuals with childhood-onset neurologic conditions. Most patients in this study had PIMD and received extensive medical care and welfare services via the community-based care system. Many of them had congenital disorders of a genetic background. We report here the extent to which pediatric-to-adult HCT has been beneficial or challenging to people with childhood-onset neurologic conditions and PIMD in Japan.
In this study, we found that after HCT to the Department of Adult Internal Medicine, half of the patients and families appreciated adult practice, such as the ability to receive medical care appropriate for their condition and consult an adult specialist, and considered themselves not to have any challenges in visiting the department. Patients and families also considered themselves to be well informed about adult medical and welfare services and believed that their health conditions had stabilized after HCT. Our results regarding improved health conditions were consistent with those from a previous study on individuals with child-onset epilepsy syndrome, although the possibility of a natural improvement in health conditions and the emergence of newly developed antiepileptic drugs cannot be ruled out.17 Because our facility is dedicated to caring for individuals with disabilities from childhood to adulthood, we must consider that our adult medical providers are more accustomed to congenital and childhood-onset diseases than other facilities. Thus, the focus of the current study on posttransition can affect the study's uniqueness.
Despite the various advantages of HCT listed above, patients and their families still encounter challenges with HCT. Pediatric and adult care seemed fragmented, as exemplified by few referrals made from pediatricians to an adult practitioner or insufficient information from pediatrics regarding patients' illness. Families and patients were encumbered by a limited understanding or even hesitation among adult practitioners in relation to childhood-onset conditions and disabilities. Many adolescents with complex chronic conditions are lost to follow-up care or experience a gap in follow-up care.18 The discontinuation of care is related to patient-related medical factors, such as the nonrequirement of medications during referral from pediatric to adult care or milder disease severity, and health behavior, such as a history of missed appointments.19,20 In this study, it was not clear whether each participant required frequent medical care before HCT. To address this knowledge gap, further investigations are required to explore factors related to the discontinuation of care in individuals with childhood-onset neurologic conditions. Building a system that ensures the effective communication of patient medical history is of paramount importance in adult health care practice.
Adequate guidance and preparedness during pediatric care are required to assist patients with making comfortable transitions to the person-centered practice of adult health care. In this study, patients and families expressed confusion with the differences between pediatric and adult health care systems, such as the management of appointments. This confusion may be attributed to inadequate guidance and a shorter preparation time, that is, only 9.5 ± 14.7 months in this study, thus suggesting that discussion between pediatric care providers and patients regarding transition policy should commence at age 12–14, and preparation for an adult approach to care should be conducted at age 18.21 Our findings are consistent with those of previous studies in which a lack of HCT discussions among individuals with CP,22 dissatisfaction with parents,23 and a lack of coordination were cited.24,25 Further support, such as collecting information regarding adult practitioners or disease-specific readiness check assessments,26 may alleviate challenges encountered during the transition period.
No studies have yielded detailed reports on the age of HCT in patients with childhood-onset neurologic conditions in Japan. The timing of HCT among the participants in this study was 28.4 ± 11.0 years, which is later than that among patients from other countries with other childhood-onset diseases, such as congenital heart disease (22.4 ± 1.6 years),27 transplanted kidney (18.8 years),28 and type 1 diabetes (21.0 ± 2.6).29 Our results are consistent with previous findings, in which cognitive impairment in childhood and progressive disability with specific health care needs were related to a delayed transfer to adult care.30,31 Therefore, the introduction of HCT to patients with childhood-onset neurologic diseases needs to be initiated at an earlier age and afforded sufficient preparation time.
In Japan, a person is legally an adult at age 18. It is quite rare for a young person with intellectual disabilities to assign an adult guardian when the young person's parents are still in good health. In addition, even if a guardian is appointed, adult guardians are primarily responsible for property management and various medical and welfare service contracts. Adult guardians are often not involved in providing medical consent. Therefore, in most cases, parents make medical decisions as they did when they had custody of the minor, and the medical institution in Japan accepts this situation. Consequently, whether the transition timing coincides with when the patient becomes an adult is not a concern in practice. However, there is a concern that parents' opinions may be too strongly reflected in the patient's postadult medical care.
Ideally, it would be desirable to have a discussion on the transition policy with the individual, their parents, and a multidisciplinary team (family, caregiver, primary care physician, case worker, nurse, rehabilitation specialist, and other adult guardians) before the individual reaches the age of an adult. After the individual becomes an adult, instead of only the parent making a medical decision, it would be sensible to have a multidisciplinary team involved in the process.
Patients and families believed that they had not been provided with sufficient pretransition information regarding their diseases and future treatment plans. A study on children with neurodevelopmental disorders revealed that health care professionals, including pediatricians, are parents' primary source of information regarding their children's diseases.32 However, parents seem dissatisfied with the knowledge they have gained because health care professionals appear to be too focused on medication and not on patients' conditions.32 This study revealed that patients and families were confident with their knowledge of effects of oral medication and formal name of the disease but not with that of the natural history of the disease or its complications. This lack of understanding of the natural history of the disease and its potential complications prevents patients and families from preparing adequately for transition to adult life. Strategies that maintain a favorable everyday life and well-being, such as acceptance or social engagement, are recommended for adult patients with chronic neurologic conditions; the approach reaches far beyond limitedly focused medical management.13 Furthermore, in the future, as new treatment options emerge, the prognosis of some childhood-onset neurologic diseases may improve.33 Therefore, lifelong patient education from childhood through adulthood may minimize mismatches in informational needs and empower patients to make appropriate decisions regarding their future.
In this study, parents understood that transition is necessary for the patient, and over half of the families considered 15–20 years to be the optimal age for discussing pediatric-to-adult HCT. Approximately half of the parents desired further discussion on the daily lives of adults with disabilities and on the preparations required of them before they cease taking care of their children. Open discussions among families, pediatricians, and adult practitioners regarding HCT are warranted. During the pediatric-to-adult HCT process, it may be ideal to have designated professionals, in addition to pediatricians or physicians, discuss their conditions and long-term care plans. Two-thirds of the participants desired consultation with a coordinator to facilitate HCT, whereas half desired a transition center, and these interventions may allow patients to receive advice from a third-party standpoint. Instructional programs for patients and families and HCT consultations for adolescents may supplement patient education, which is currently inadequate for regular outpatient visits.
Neurologists are typically accustomed to diagnosing conditions characterized by cognitive and motor dysfunction. Furthermore, a high rate of comorbid epilepsy was noted among participants in this study, as previously reported.34 Thus, adult neurologists can play a fundamental role in managing this population. However, adult neurologists are uncomfortable treating adults with childhood-onset conditions.35 We believe that there is a need for education about childhood-onset conditions and HCT among medical students, residents, and neurologists. In Japan, medical schools and junior residency programs provide opportunities to learn internal medicine and pediatrics independently but not transitional medicine.36,37 After completing junior residency, one must gain experience with the full range of neurologic disease cases during the training to become a board-certificated neurologist. These cases require childhood-onset neurologic diseases such as metabolic diseases or muscular dystrophies,38 but the number of cases and experience in managing HCT are limited in clinical practice. For lifelong learning for board-certificated neurologists, the Japanese Society of Neurology formed the Special Committee for Measures Against Transition from Pediatric to Adult Health Care in 2020 issuing a statement4 and started to provide seminars in annual meetings regarding management of people with childhood-onset neurologic conditions and HCT. In other countries, there are limited ways for residents and neurologists to gain knowledge about transitional medicine.35,39 As doctors' comfort in providing care for young adults with chronic illness of childhood is associated with experience in training with larger number of patients,40 implementing exposure to cases in medical schools, junior residency, and neurology training is urgent.
Most participants of the current study had severe disabilities. This study showed that some physicians were reluctant to care for patients because of their disabilities, which aligns with a previous report.41 One reason for the reluctance is that physicians had limited opportunities to learn about care of individuals with disabilities.42 Same as medical training on childhood-onset conditions, throughout medical training in Japan, there are no requirements for management of individuals with disabilities.36-38 Adequate education about disabilities will help physicians gain broader view about how disability affects patients' lives, their medical decision making, and how to support people with disabilities.43 Thus, improving transitional care in patients with childhood-onset neurologic conditions.
The primary disease of participants in the current study was quite heterogeneous and included many rare diseases, reflecting that rare diseases excessively affect the nervous system in children.44 In terms of self-management, a disease-specific transition program is desirable because each disease requires special attention.26 However, it may be challenging to implement a uniform program because there are a variety of symptoms and severity of the disability, even within the same disease.45 Therefore, in addition to disease-specific approach, conditions or disability-specific measures would be preferable. Furthermore, the number of patients at a single institution is limited due to the rarity of each disease; future analysis at the national registry level will be inevitable. The most common primary disease among the participants in this study was CP. As CP is an umbrella term, it will be necessary to include genetic testing and reevaluation of diagnosis to manage individuals with CP in the future.46,47
Although our study was based on a single hospital, some of its findings reflected the actual HCT situation facing individuals with childhood-onset neurologic conditions in Japan because the disparity between pediatric and adult practice is a common phenomenon.48 In this study, the response rate was as high as 87.4%, indicating a high level of interest in pediatric-to-adult HCT among the participants. However, this study has several limitations. First, we targeted adult patients who had already transitioned to an adult department. Adult patients and their families may not entirely recall the information their primary pediatricians imparted to them at a younger age, i.e., if any awareness was provided. Participants included older adults who had been accustomed to adult practice for a relatively long time after the transition. Future studies should recruit adult patients who still receive treatment in the pediatric department to examine their views on HCT. Second, we used self-reported measurements of the benefits and challenges of HCT and did not use validated or objective measurements. Therefore, certain information that potentially affects patients' and families' lives might have been overlooked. Studies are needed to examine patient knowledge, and satisfaction with adult care, among others, using validated and objective measurements. Finally, this study required that participants receive an in-person explanation of the nature of the study before giving their consent to participate in the study. Therefore, patients who had intellectual disabilities and lived in an institution away from their families may not have been included in this study. In addition, patients with unstable health conditions who visited the Department of Internal Medicine but needed urgent medical treatment and could not receive an explanation about the study due to time shortage may not have been included. Further nationwide studies are required to elucidate the HCT situation among patients with childhood-onset neurologic conditions and promote pediatric-to-adult HCT with adequate timing and support.
Our study established the pediatric-to-adult HCT experiences of individuals with childhood-onset neurologic conditions and severe physical and intellectual disabilities. Our findings suggest that systems and staff that support HCT and lifelong education for patients and families are warranted.
Acknowledgment
The authors thank the patients, and their families, who participated in this study as well as the hospital staff who contributed to data collection. In addition, they thank the members of the Department of Global Health Promotion, Tokyo Medical and Dental University, for their valuable contributions to this study.
Appendix. Authors
Study Funding
This study was supported by the Ministry of Health, Labour and Welfare (Health and Labour Science Research Grants, Program Grant Number: 21FC1015).
Disclosure
All authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
TAKE-HOME POINTS
→ Individuals with childhood-onset neurologic conditions benefited from pediatric-to-adult health care transition (HCT) regarding their health conditions and service use, despite experiencing difficulties during the HCT period and challenges in adult practice.
→ Systems and staff that support HCT and lifelong education for patients and families are warranted.
→ Medical training about childhood-onset neurologic conditions for physicians and neurologists is urgent.
References
- 1.Schmidt A, Ilango SM, McManus MA, Rogers KK, White PH. Outcomes of pediatric to adult health care transition interventions: an updated systematic review. J Pediatr Nurs. 2020;51:92-107. 10.1016/j.pedn.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Chabrol B, Milh M. Transition from paediatric to adult care in adolescents with neurological diseases and handicap. Rev Neurol (Paris). 2020;176(1-2):37-42. doi. 10.1016/j.neurol.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Camfield PR, Andrade D, Camfield CS, et al. How can transition to adult care be best orchestrated for adolescents with epilepsy? Epilepsy Behav. 2019;93:138-147. doi. 10.1016/j.yebeh.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 4.Ogata K, Mochizuki Y, Saito T, et al. Perspective on transition from pediatric to adult health care for patients with neurological disease: current situation and issues [in Japanese]. Rinsho Shinkeigaku. 2022;62(4):261-266. doi. 10.5692/clinicalneurol.cn-001676. [DOI] [PubMed] [Google Scholar]
- 5.Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88(8):1064-1073. doi. 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 6.Tolentino JTG. Cerebral palsy. In: Pilapil M, DeLaet DE, Kuo AA, Peacock C, Sharma N, eds. Care of Adults with Chronic Childhood Conditions: A Practical Guide: Springer; 2016:67-85. [Google Scholar]
- 7.Ronen GM, Rosenbaum PL, Streiner DL. Patient perspectives in pediatric neurology: a critical shift in the paradigm of outcome measurement. Dev Med Child Neurol. 2022;64(2):149-155. 10.1111/dmcn.14954. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine (US). Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century: National Academies Press (US); 2001. [PubMed] [Google Scholar]
- 9.Prior M, McManus M, White P, Davidson L. Measuring the “triple aim” in transition care: a systematic review. Pediatrics. 2014;134(6):e1648-e1661. doi. 10.1542/peds.2014-1704. [DOI] [PubMed] [Google Scholar]
- 10.Osako M, Takeuchi C, Mochizuki Y. Transition from pediatric to adult health care in patients with childhood-onset neurological disease : clinical practice for individuals with intellectual and physical disability. Neurol Ther. 2021;38(2):112-122. 10.15082/jsnt.38.2_112. [DOI] [Google Scholar]
- 11.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 2008;39(4):214-223. doi. 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 12.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5: American Psychiatric Association; 2013. [Google Scholar]
- 13.Audulv A, Hutchinson S, Warner G, Kephart G, Versnel J, Packer TL. Managing everyday life: self-management strategies people use to live well with neurological conditions. Patient Educ Couns. 2021;104(2):413-421. doi. 10.1016/j.pec.2020.07.025. [DOI] [PubMed] [Google Scholar]
- 14.United States Census Bureau. National survey of children's health [online]. www.census.gov/programs-surveys/nsch.html. Accessed July 8, 2022.
- 15.King S, King G, Rosenbaum P. Evaluating health service delivery to children with chronic conditions and their families: development of a refined measure of processes of care (MPOC−20). Child Health Care. 2004;33(1):35-57. doi. 10.1207/s15326888chc3301_3. [DOI] [Google Scholar]
- 16.Bureau of Social Welfare, Public Health, Tokyo Metropolitan Government. Social welfare and public health in Tokyo [online]. fukushihoken.metro.tokyo.lg.jp/english/about/pamphlet.html. Accessed July 8, 2022.
- 17.Kwack DW, Lee H, Lee R, Kim DW. Treatment outcome following the transition to adult epilepsy care in childhood-onset epilepsy. Seizure. 2022;96:43-45. doi. 10.1016/j.seizure.2022.01.015. [DOI] [PubMed] [Google Scholar]
- 18.Skogby S, Bratt EL, Johansson B, Moons P, Goossens E. Discontinuation of follow-up care for young people with complex chronic conditions: conceptual definitions and operational components. BMC Health Serv Res. 2021;21(1):1343. doi. 10.1186/s12913-021-07335-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harbison AL, Grady S Jr, Chi K, Fernandes SM. Provision of transition education and referral patterns from pediatric cardiology to adult cardiac care. Pediatr Cardiol. 2016;37(2):232-238. doi. 10.1007/s00246-015-1267-5. [DOI] [PubMed] [Google Scholar]
- 20.Goossens E, Bovijn L, Gewillig M, Budts W, Moons P. Predictors of care gaps in adolescents with complex chronic condition transitioning to adulthood. Pediatrics. 2016;137(4):e20152413. doi. 10.1542/peds.2015-2413. [DOI] [PubMed] [Google Scholar]
- 21.The National Alliance to Advance Adolescent Health. Six core elements of health care transition 2.0 [online]. gottransition.org/providers/index.cfm. Accessed July 8, 2022.
- 22.Blackman JA, Conaway MR. Adolescents with cerebral palsy: transitioning to adult health care services. Clin Pediatr (Phila). 2014;53(4):356-363. doi. 10.1177/0009922813510203. [DOI] [PubMed] [Google Scholar]
- 23.Pin TW, Chan WL, Chan CL, et al. Clinical transition for adolescents with developmental disabilities in Hong Kong: a pilot study. Hong Kong Med J. 2016;22(5):445-453. doi. 10.12809/hkmj154747. [DOI] [PubMed] [Google Scholar]
- 24.Bindels-de Heus KGCB, van Staa A, van Vliet I, Ewals FVPM, Hilberink SR. Transferring young people with profound intellectual and multiple disabilities from pediatric to adult medical care: parents' experiences and recommendations. Intellect Dev Disabil. 2013;51(3):176-189. doi. 10.1352/1934-9556-51.3.176. [DOI] [PubMed] [Google Scholar]
- 25.Stevenson CJ, Pharoah POD, Stevenson R. Cerebral palsy: the transition from youth to adulthood. Dev Med Child Neurol. 2008;39(5):336-342. doi. 10.1111/j.1469-8749.1997.tb07441.x. [DOI] [PubMed] [Google Scholar]
- 26.Warschausky S, Kaufman JN, Schutt W, Evitts M, Hurvitz EA. Health self-management, transition readiness and adaptive behavior in persons with cerebral palsy or myelomeningocele. Rehabil Psychol. 2017;62(3):268-275. doi. 10.1037/rep0000157. [DOI] [PubMed] [Google Scholar]
- 27.Hergenroeder AC, Moodie DS, Penny DJ, et al. Functional classification of heart failure before and after implementing a healthcare transition program for youth and young adults transferring from a pediatric to an adult congenital heart disease clinics. Congenit Heart Dis. 2018;13(4):548-553. 10.1111/chd.12604. [DOI] [PubMed] [Google Scholar]
- 28.Kosola S, Ylinen E, Finne P, Rönnholm K, Ortiz F. Implementation of a transition model to adult care may not be enough to improve results: national study of kidney transplant recipients. Clin Transpl. 2019;33(1):e13449. 10.1111/ctr.13449. [DOI] [PubMed] [Google Scholar]
- 29.Jones MR, Robbins BW, Augustine M, et al. Transfer from pediatric to adult endocrinology. Endocr Pract. 2017;23(7):822-830. doi. 10.4158/EP171753.OR. [DOI] [PubMed] [Google Scholar]
- 30.Geenen SJ, Powers LE, Sells W. Understanding the role of health care providers during the transition of adolescents with disabilities and special health care needs. J Adolesc Health. 2003;32(3):225-233. doi. 10.1016/s1054-139x(02)00396-8. [DOI] [PubMed] [Google Scholar]
- 31.Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics. 2005;115(1):112-120. doi. 10.1542/peds.2004-1321. [DOI] [PubMed] [Google Scholar]
- 32.Ahmed R, Borst JM, Yong CW, Aslani P. Do parents of children with attention-deficit/hyperactivity disorder (ADHD) receive adequate information about the disorder and its treatments? A qualitative investigation. Patient Prefer Adherence. 2014;8:661-670. doi. 10.2147/ppa.S60164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morris G, Schorge S. Gene therapy for neurological disease: state of the art and opportunities for next-generation approaches. Neuroscience. 2022;490:309-314. doi. 10.1016/j.neuroscience.2022.03.010. [DOI] [PubMed] [Google Scholar]
- 34.Jokiranta E, Sourander A, Suominen A, Timonen-Soivio L, Brown AS, Sillanpää M. Epilepsy among children and adolescents with autism spectrum disorders: a population-based study. J Autism Dev Disord. 2014;44(10):2547-2557. doi. 10.1007/s10803-014-2126-6. [DOI] [PubMed] [Google Scholar]
- 35.Oskoui M, Wolfson C. Treatment comfort of adult neurologists in childhood onset conditions. Can J Neurol Sci. 2012;39(2):202-205. doi. 10.1017/s0317167100013238. [DOI] [PubMed] [Google Scholar]
- 36.Ministry of Health Labour and Welfare, Japan. Objectives, strategies, and evaluation in residency training [online]. mhlw.go.jp/stf/newpage_03924.html. Accessed October 29, 2022.
- 37.Ministry of Education Culture, Sport, Science and Technology, Japan. Model core curriculum for medical education [online]. mext.go.jp/b_menu/shingi/chousa/koutou/033-2/toushin/1383962.htm. Accessed October 29, 2022.
- 38.Japanese Society of Neurology. Neurology specialist training curriculum (case requirements) [online]. neurology-jp.org/news/pdf/curriculum_case.pdf. Accessed October 29, 2022.
- 39.Tirol FG, Kumar A. Resident training in transitioning youth with epilepsy into adult care. J Child Neurol. 2021;36(1):60-64. doi. 10.1177/0883073820953010. [DOI] [PubMed] [Google Scholar]
- 40.Okumura MJ, Heisler M, Davis MM, Cabana MD, Demonner S, Kerr EA. Comfort of general internists and general pediatricians in providing care for young adults with chronic illnesses of childhood. J Gen Intern Med. 2008;23(10):1621-1627. doi. 10.1007/s11606-008-0716-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boyce DM, Devinsky O, Meskis MA. Barriers to transition from pediatric to adult care for patients with Dravet syndrome: a focus group study of caregivers. Epilepsy Behav. 2020;109:107096. doi. 10.1016/j.yebeh.2020.107096. [DOI] [PubMed] [Google Scholar]
- 42.Iezzoni LI, Long-Bellil LM. Training physicians about caring for persons with disabilities: Nothing about us without us. Disabil Health J. 2012;5(3):136-139. doi. 10.1016/j.dhjo.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 43.Lagu T, Haywood C, Reimold K, De Jong C, Walker Sterling R, Iezzoni LI. “I Am not the doctor for you”: physicians' attitudes about caring for people with disabilities. Health Aff (Millwood). 2022;41(10):1387-1395. doi. 10.1377/hlthaff.2022.00475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee CE, Singleton KS, Wallin M, Faundez V. Rare genetic diseases: nature's experiments on human development. iScience. 2020;23(5):101123. doi. 10.1016/j.isci.2020.101123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peron A, Canevini MP, Ghelma F, Di Marco F, Vignoli A. Healthcare transition from childhood to adulthood in tuberous sclerosis complex. Am J Med Genet C Semin Med Genet. 2018;178(3):355-364. doi. 10.1002/ajmg.c.31653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaufmann WE. Neurogenetics in child neurology: redefining a discipline in the twenty-first century. Curr Neurol Neurosci Rep. 2016;16(12):103. doi. 10.1007/s11910-016-0703-0. [DOI] [PubMed] [Google Scholar]
- 47.Shevell M. Cerebral palsy to cerebral palsy spectrum disorder. Neurology. 2019;92(5):233-235. doi. 10.1212/WNL.0000000000006747. [DOI] [PubMed] [Google Scholar]
- 48.Michihata N, Matsui H, Fushimi K, Yasunaga H. Clinical features of adult patients admitted to pediatric wards in Japan. J Adolesc Health. 2015;57(4):421-424. doi. 10.1016/j.jadohealth.2015.07.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Questionnaires and study data are available on request from the corresponding author (M.O.).