Abstract
Background and Objectives
Developing high-value care models with limited resources for large populations of individuals with migraine requires advanced understanding of patient preferences for care delivery methods. In this study, we aimed to inform the development of migraine care models by assessing patient preferences for types of care delivery and determining differences based on migraine frequency and disability.
Methods
We analyzed unpublished data from a cross-sectional survey of 516 randomly selected individuals with migraine within a community practice associated with Mayo Clinic, Rochester, MN.
Results
Individuals with chronic migraine, compared with those with episodic migraine, were more likely to prefer a visit with a neurologist (p = 0.0005), synchronous telephone conference with primary care provider (PCP) and neurologist (p = 0.0102), and a written migraine action plan in the medical record (p = 0.0343). Compared with those with mild/no disability, individuals with moderate-to-severe disability were more likely to prefer a visit with a neurologist (p < 0.0001), synchronous video or telephone conference with PCP and neurologist (p < 0.0001), PCP communication with neurologist (p = 0.0099), electronic message to primary care team with access to neurologist (p = 0.0216), and written action plan in the medical record (p = 0.0011). Collectively, individuals most preferred telephone follow-up and least preferred communications with a nurse or pharmacist or generalized education (all p < 0.001).
Discussion
We observed differences in migraine care delivery preferences between migraine frequency and level of migraine disability. Observations support development of care pathways that include a written migraine action plan, primary care–neurology collaboration including nontraditional interactions, and prioritization of traditional neurology consultation for the most disabled patients.
Migraine is a chronic and disabling disorder that affects more than 1 billion people globally.1 The migraine population has limited access to care2 including the recent advances in migraine therapeutics3 that may reduce disability and improve quality of life. Primary care providers (PCPs)4 and general neurologists provide most migraine care, and both groups project future workforce shortages.5,6 Subspecialty headache centers have long wait times, with a recent study demonstrating wait lists for traditional face-to-face and video visits as long as 14 months.2
Novel models of care delivery such as electronic consultations7,8 and asynchronous and synchronous primary care-neurology collaboration8 are promising interventions that may improve access to specialty advice. Asynchronous collaboration may take the form of physician-to-physician electronic consultation or informal “curbside” consultations. Synchronous collaboration involves a real-time visit between the patient, PCP, and neurologist. While synchronous collaboration has long been used in the inpatient setting,9 it has been described in the outpatient setting in the Integrated Community Neurology model at Mayo Clinic, Rochester, MN, in which a general neurologist is colocalized into a primary care medical home.10 A pilot study of this model, in which the neurologist was allotted scheduled time for asynchronous and synchronous collaboration, demonstrated reductions in the need for face-to-face appointments and referrals to tertiary neurology thereby improving access for the most complex patients.8
Compared with episodic migraine (EM), chronic migraine (CM) is associated with substantially higher disability,11-13 missed work,11 and total costs.14,15 Disability, healthcare utilization, and direct costs increase along a continuum with the number of headache days experienced per month.16 In a previous study, we surveyed randomly selected adults with migraine from a population of patients in the Mayo Clinic (Rochester, MN) primary care health system and found that, compared with individuals with EM, individuals with CM reported higher levels of disability, lower levels of satisfaction with their care, and less satisfaction with access to both care and medical advice.17 Therefore, it is likely that individuals with different attack frequencies have different healthcare resource needs and that there may be differences in patient preference for various novel types of care delivery.
In this study, we present unpublished data from our prior survey17 and use these data to test the hypothesis that preferences for care delivery also differ based on migraine frequency and level of migraine-associated disability. We aim to better understand patient preferences regarding traditional and nontraditional approaches to delivery of care intended to improve access to care and shorten wait times.
Methods
Standard Protocol Approvals, Registrations, and Patient Consents
The Mayo Clinic Institutional Review Board granted an exception for written informed consent project (#17-004871).
Study Population
Study population selection and survey administration were described in our previous study.17 Key methods are summarized as follows. We identified 5,239 adult individuals with migraine within a total population of approximately 155,000 locally residing individuals with a designated PCP at Mayo Clinic, Rochester, MN. All patients were aged 18 years or older and had documentation of a migraine-specific ICD-9 or ICD-10 diagnosis code between May 1, 2014, and April 1, 2017. Of 5,239 eligible participants, 1,804 were randomly selected anticipating a 30% response rate and goal of 500 total respondents. A paper-based survey was mailed to participants. Because this study was designed after survey completion, a statistical power analysis was not calculated.
Measures
Electronic Medical Record and Registration
As previously described,17 patient demographic information was abstracted from the existing information located in the electronic health record. Migraine frequency was determined by patient report of headache days.
Individuals reporting more than 15 headache days per month for more than 3 months were categorized as those with CM and the remaining individuals were categorized as those with EM. Disability and quality of life were assessed using the Migraine Disability Assessment (MIDAS).18-20 Based on the total MIDAS score, survey respondents were categorized into 2 groups: no/minimal disability and moderate-to-severe disability.
Survey Questions
For a series of 13 questions, patients were asked, “How helpful would the following resources be to help manage your migraine headaches?” Resources addressed included attendance of educational seminars, phone call discussions with registered nurses, visits with PCPs, visits with neurologists, video or phone conferences with a neurologist while meeting with PCP, communication between PCP and a neurologist, ability to text message with a nurse, use of an online patient portal to communicate with PCP, pharmacist visits or phone calls, written action plans outlining treatment plans if usual treatments fail, phone follow-up on medication changes rather than clinic visits, and video conference visits rather than clinic visits. Patients responded using a Likert scale, a 5-point ordinal scale consisting of the response categories “not at all helpful,” “somewhat unhelpful,” “neither helpful nor unhelpful,” “somewhat helpful,” and “very helpful.”
Analysis
Total survey responses were summarized using frequencies and percentages for categorical and ordinal variables and median and ranges for continuous variables. We compared demographic and clinical characteristics of patient survey respondents with those of nonrespondents using chi-square tests for categorical variables and Wilcoxon rank sum tests for continuous variables. Of the respondents, we compared responses to the 13 ordinally scaled resource questions between patients with CM and EM and between patients with no/mild and moderate-to-severe disability using Cochran-Armitage tests for trend. We then combined all respondents together and ordered care delivery resources from most to least preferred based on mean ratings of the ordinally scaled questions. We formally compared differences in care delivery preferences across the 13 resources using a linear mixed modeling approach. Each participant contributed 13 observations to this analysis: 1 for each resource. Rating was fit as the outcome variable and resource as the predictor variable. We included a per-subject random intercept term with a compound symmetry variance-covariance matrix to account for within-subject correlations of ratings. This global test was followed by a series of 13 pairwise linear mixed modeling analyses comparing each resource in turn with all other resources combined. This series of tests was performed in the spirit of Fisher protected least significant difference test; per-resource associations were not considered statistically significant in the absence of global significance. All statistical tests were 2-sided, and all data management and statistical analyses were performed using Statistical Analysis software, version 9.3 (Cary, NC) with statistical significance defined by p < 0.05.
Data Availability
Due to copyright restrictions, the paper survey will not be shared. Anonymized survey results data unpublished within this article will be made available by request from any qualified investigator.
Results
Demographics, Migraine Phenotype, and Disability and Quality of Life
Demographics, migraine phenotype, and disability and quality of life were previously reported.17 Survey response rate was 516/1,804 (30%). Survey respondents were older (median 47.4 vs 38.0 years, p < 0.0001) and more likely to be female (86.4% vs 79.9%, p = 0.001), married (66.1% vs 50.6%, p < 0.0001), and White (95.1% vs 84.3%, p < 0.0001) when compared with survey nonrespondents. Of all respondents, 110 (21%) were classified as those with CM, and 245 (52.2%) reported moderate-to-severe disability due to their migraines. MIDAS scores and age at onset of migraines were significantly different between CM and EM survey respondents. Patients with CM and EM did not differ according to age at survey response, sex, race, or marital status.
Migraine Frequency and Care Model Preferences
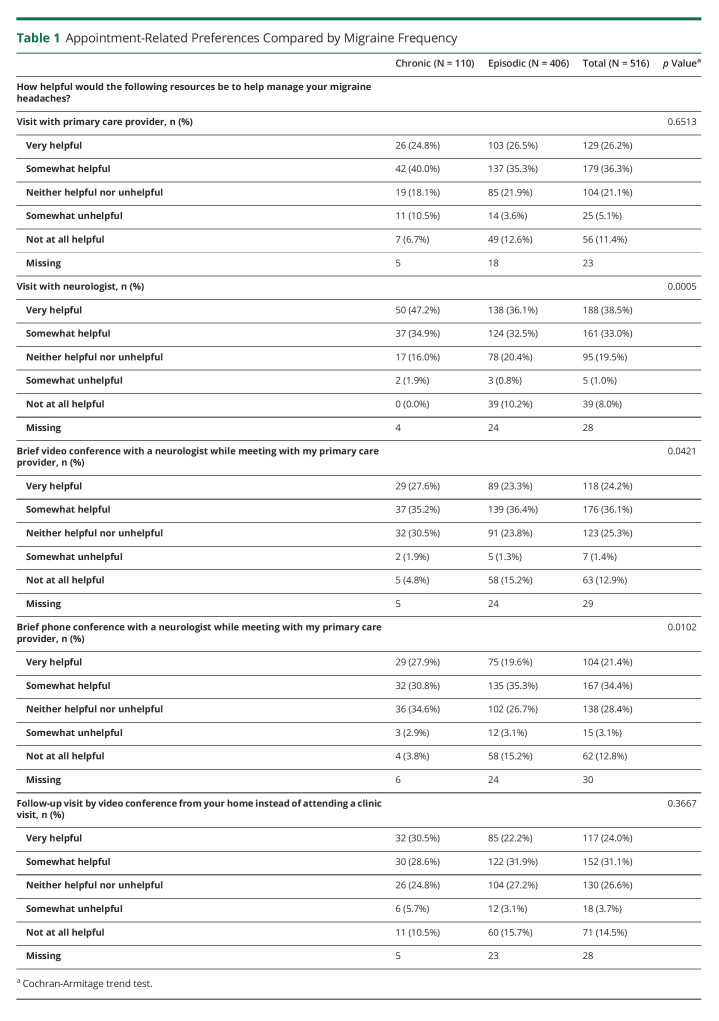
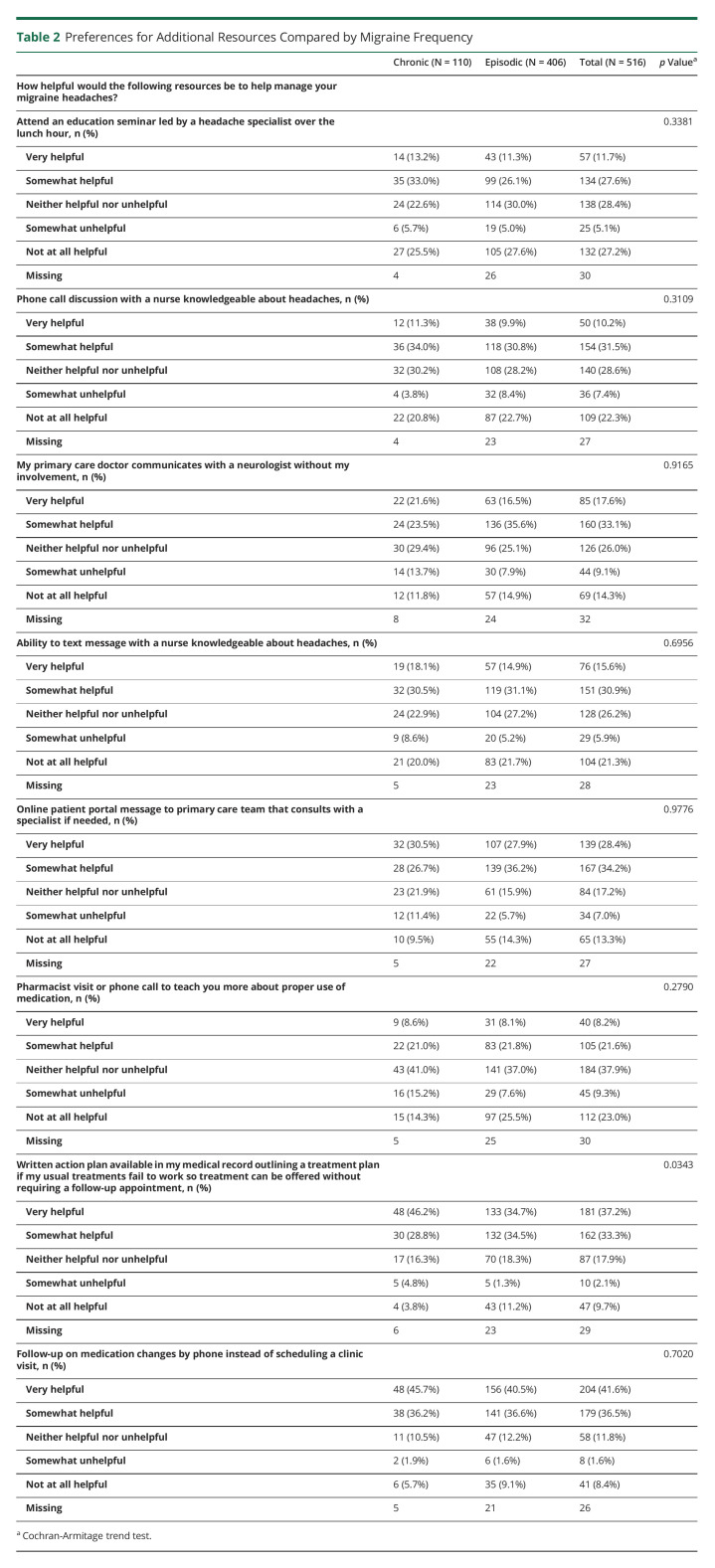
Appointment-related preferences compared by migraine frequency are reported in Table 1, and preferences for additional resources compared by migraine frequency are reported in Table 2. Compared with those with EM, respondents with CM were more likely to prefer a visit with a neurologist (p = 0.005), synchronous telephone conference between patient, PCP, and neurologist (p = 0.0102), synchronous video conference between patient, PCP, and neurologist (p = 0.0421), and a written migraine action plan in the medical record (p = 0.0343).
Table 1.
Appointment-Related Preferences Compared by Migraine Frequency
Table 2.
Preferences for Additional Resources Compared by Migraine Frequency
Migraine Disability and Care Model Preferences
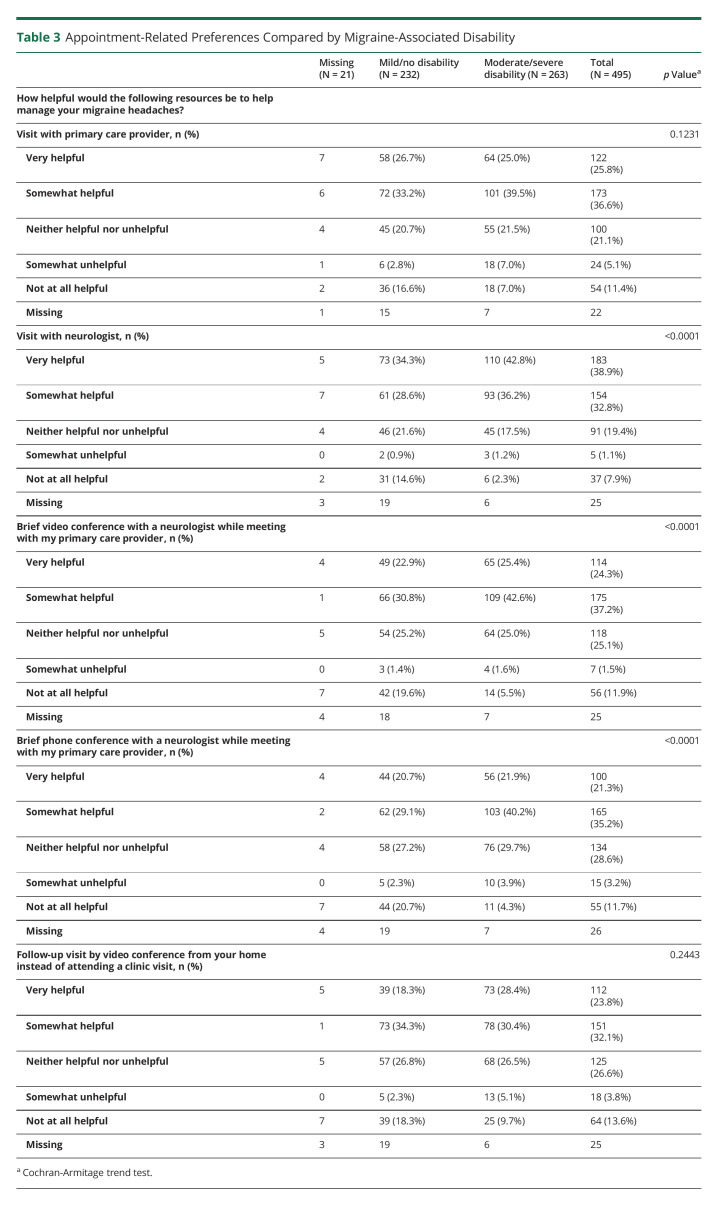
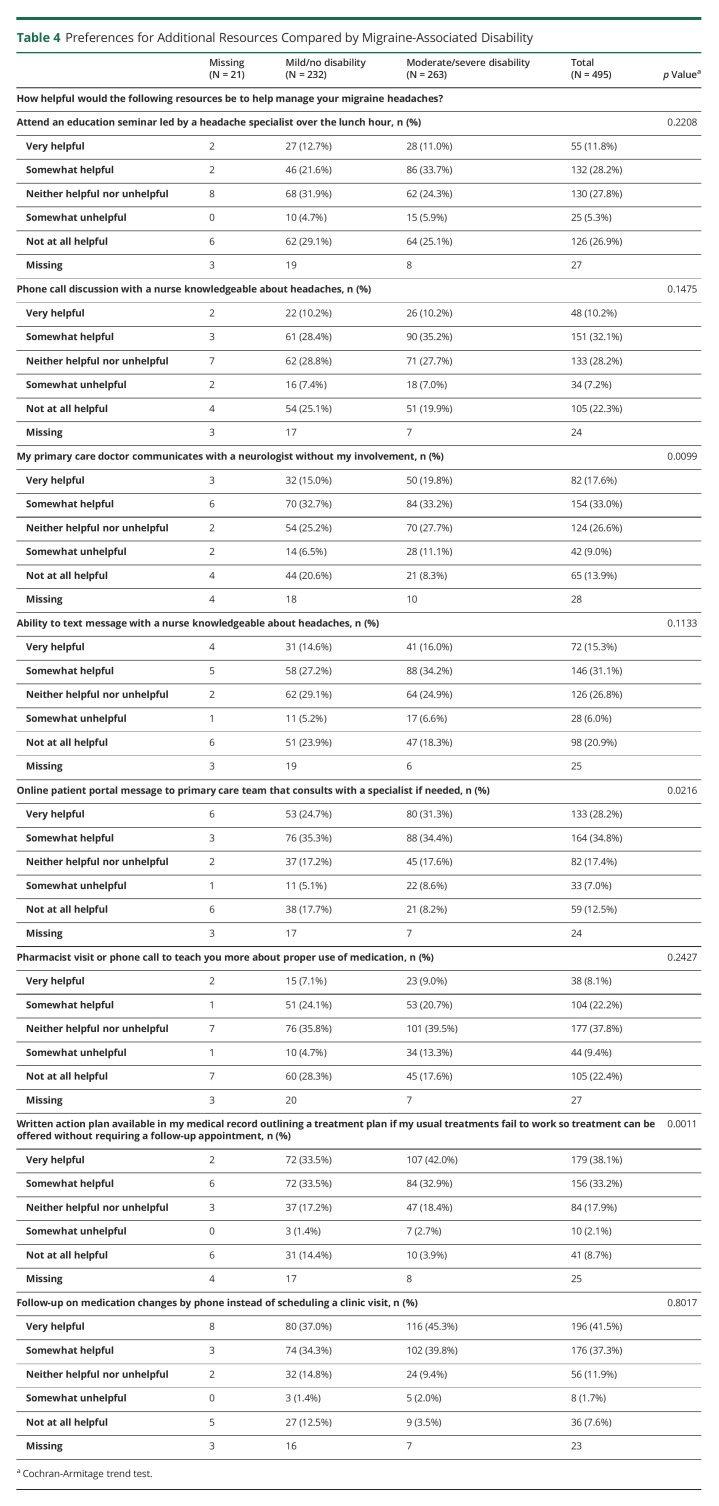
Appointment-related preferences compared by level of disability are summarized in Table 3, and preferences for additional resources compared by level of disability are summarized in Table 4. Compared with those with no/mild disability, respondents with moderate-to-severe disability were more likely to prefer a visit with a neurologist (p < 0.0001), synchronous video or telephone conference between patient, PCP, and neurologist (p < 0.0001 for each), asynchronous PCP communication with neurologist (p = 0.0099), electronic message to primary care team with access to neurologist (p = 0.0216), and a written action plan in the medical record (p = 0.0011).
Table 3.
Appointment-Related Preferences Compared by Migraine-Associated Disability
Table 4.
Preferences for Additional Resources Compared by Migraine-Associated Disability
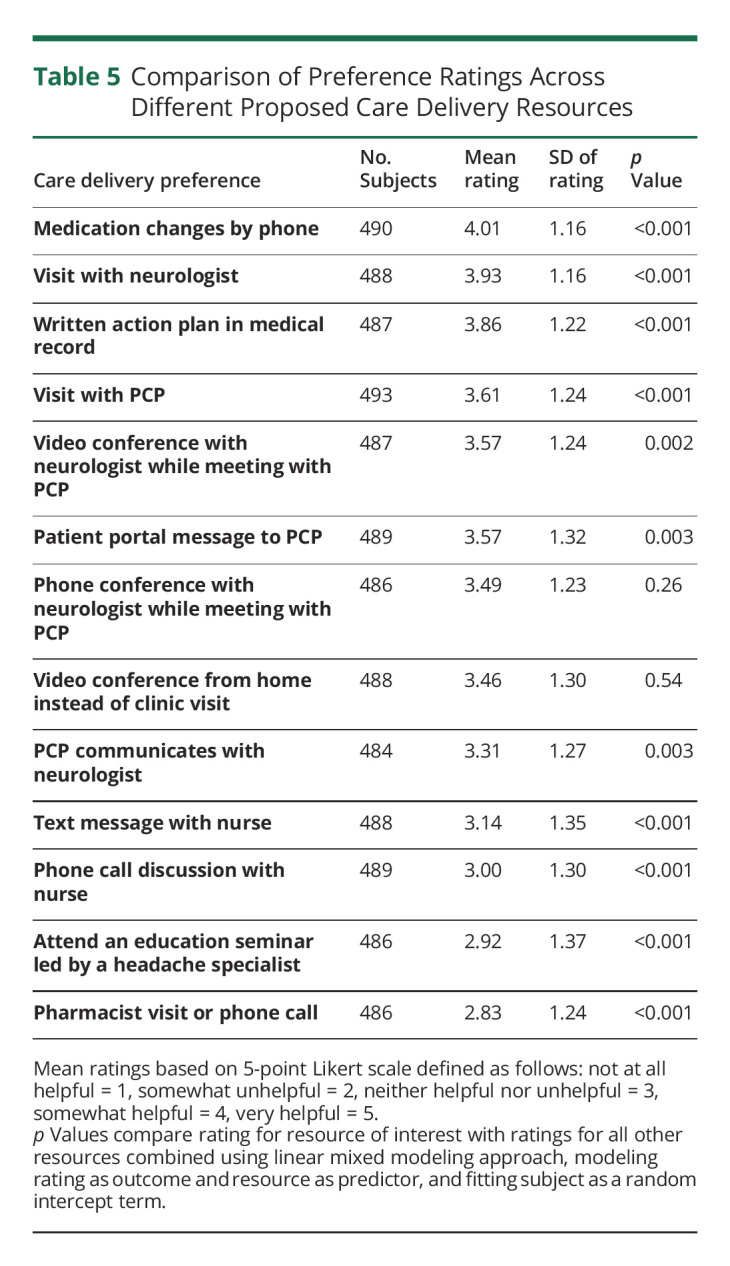
Patient Care Model Preference
The mean rating of collective care delivery preferences is reported in Table 5. The overall global test for differences in mean ratings across the 13 resources was highly significant (p < 0.0001), allowing us to explore per-resource associations. Collectively, respondents' highest preference was for telephone-follow up regarding medications (rather than requiring a clinic visit) with a mean (SD) rating of (4.01 [1.16]; p < 0.001). The second highest preference was a visit with a neurologist with a mean (SD) rating of (3.93 [1.16]; p < 0.001), followed by a written action plan in the medical record (3.86 [1.22]; p < 0.001). The least preferred care delivery model was contact with a pharmacist (2.83 [1.24]; p < 0.001), attending an educational seminar led by a specialist (2.92 [1.37]; p < 0.001), and ability to contact a nurse knowledgeable about headache by telephone (3.00 [1.30]; p < 0.001) or text message (3.14 [1.35]; p < 0.001).
Table 5.
Comparison of Preference Ratings Across Different Proposed Care Delivery Resources
Discussion
We observed that preferences for specific types of migraine care differ between individuals with EM and CM and between individuals with different levels of disability within a population of community patients associated with Mayo Clinic, Rochester, MN. The observations for those with CM and higher disability were relatively concordant as we expected. Patients with CM and higher disability were more likely than those with EM or no/mild disability to prefer care delivered by a neurologist including traditional face-to-face visits and nontraditional synchronous collaboration with PCPs; patients with moderate-to-severe disability were more likely than those with no/mild disability to prefer asynchronous collaboration with PCPs as well. Most patients regardless of migraine type preferred an option to follow-up through telephone and a written action plan with alternative treatment options if needed. We also found that collective preference was higher for options involving a physician or physician-driven plan and lower for nurse-driven or pharmacist-driven encounters or generalized educational opportunities.
Previous studies have reported that less than 5% of individuals with CM are able to successfully navigate all steps necessary to receive appropriate management of migraine,13 compared with 26.3% of those with EM.21 In our previous study, we found that individuals with CM had higher dissatisfaction with care delivery, access to care, and access to medical advice than did those with EM.17 The current observation that care model preferences differ as well suggests that the dissatisfaction in respondents with CM may be influenced by the use of traditional care models in groups with differing care delivery needs. Given the limited access to care using traditional healthcare delivery models, it is likely that individuals with a higher migraine frequency, and therefore greater healthcare needs, would have a greater proportion of their needs unmet.
We grouped individuals by lesser and greater levels of disability in addition to grouping by migraine frequency because while CM is associated with a higher level of disability,11,16,17,22 disability is not limited to the CM population. Migraine-related disability and poor quality of life for patients with frequent EM reporting 10–14 headache days per month is similar to that in individuals with CM.23 Indeed, disability, healthcare utilization, and direct costs have been demonstrated to increase with the number of migraine days experienced per month, including along a spectrum within the EM population.16
Consistent with expectation, while many of our patients had both CM and moderate-to-severe disability, 42.7% of our individuals with EM had moderate-to-severe disability as well. Also consistent with expectation, in this study, individuals with CM (compared with those with EM) and individuals with moderate-to-severe disability (compared with those with no/mild disability) had a significantly greater preference for greater healthcare access, including a visit with a neurologist, either face-to-face or synchronous with a PCP visit, and a written action plan in the chart to address treatment failures. Patients with moderate-to-severe disability (compared with those with no/mild disability) also had a significantly greater preference for asynchronous PCP-neurologist collaboration and electronic communication with a PCP team.
Recent government surveillance statistics demonstrated that 52.8% of appointments for migraine took place in primary care, vs 23.2% in specialty outpatient clinics24; yet studies have demonstrated that in the primary care setting, migraines are often underdiagnosed25 or treated in the absence of familiarity with management guidelines.26 Synchronous and asynchronous neurologist-PCP collaboration, when feasible, would be expected to potentially improve diagnosis and treatment by increasing access to specialist advice. Our findings suggest that patients may view these strategies favorably because most respondents indicated that synchronous and asynchronous neurologist-PCP collaboration would be helpful or very helpful. The feasibility of neurologist-PCP collaboration is currently limited in most smaller neurology practices but has been shown to be beneficial in an Integrated Community Neurology model8 and may ultimately have a role in the multispecialty practice environment.
These findings support continuing to offer electronic consultations and options for PCP-neurologist synchronous or asynchronous PCP-neurologist collaboration in our current integrated community neurology model at Mayo Clinic, Rochester, MN, as a strategy to improve access to specialty advice while prioritizing face-to-face visits for those with CM or disabling EM.8,10 Although prior studies of the integrated community neurology model included approximately 25% patients with headache, mostly migraine, the effect of electronic and curbside collaboration between PCPs and neurologists specifically on migraine outcomes requires further study.
Collectively, individuals in our study population had the highest preference for telephone follow-up on medication changes rather than requiring a clinic visit (78.1%). While this finding may partly reflect the convenience of a telephone discussion over a formal appointment, it may be influenced by the long wait times for return appointments and the wish to avoid the delay in the next step of management. Notably, the option for scheduling a video appointment rather than an in-person appointment, both of which are influenced by appointment availability, was substantially lower on the preference rank order (mean [SD] rating 3.46 [1.30] for video conference from home vs 4.01 [1.16] for telephone follow-up), suggesting that the wish to conduct follow-up from home is not the main driver. We hypothesize that patients endorsed this answer expecting that telephone calls may occur more expeditiously than clinical follow-up appointments. Patient triage mechanisms prioritizing appointments based on headache frequency and level of disability are supported by our findings.
Collective preference was also high (70.5%) for a written action plan in the medical record to address treatment failure, another care delivery option that is physician driven and may circumvent the wait for an available appointment. A migraine action plan has been developed for pediatric27,28 and adult29,30 patients but has not been studied in practice. Our survey supports the development of documented migraine care plans that include alternative treatment options that can be implemented easily through telephone or electronic follow-up guided by a neurologist.
Strengths of our study include the assessment of a large, random sample of a well-defined population of community patients who were likely to carry an accurate diagnosis of migraine with characteristics similar to other studies31 and with similar level of migraine disability along a spectrum. Our survey questions assessed novel nontraditional methods of care delivery in patients who received most of their care before the development of the Integrated Community Specialist Clinic in late 2014. Our findings may be applicable to community patients with migraine with similar access to primary and specialty care within a larger health care organization.
Our study had several limitations. The survey response rate was only 30%, which could have biased results if individuals with more or less severe symptoms were more likely to participate. We found that respondents and nonrespondents differed regarding age, sex, race, and marital status. However, respondents and nonrespondents did not differ by EM vs CM status, which reduces the likelihood of confounding by response. Because survey respondents were predominantly female (86.4%) and White (95.0%), the study population does not represent the population of patients with migraine as a whole. Because migraine-associated needs may differ across groups, our results cannot be generalized to all patients with migraine. A major future direction will be to assess healthcare delivery needs across more varied populations. This survey was conducted before the COVID-19 pandemic, which may have shifted patient preferences for care delivered through video telemedicine. We did not specifically assess patient preferences to communicate with a neurologist directly through electronic messaging. We also did not inquire about using a smartphone application to assess, monitor, or communicate the need for migraine care plan adjustments. We did not inquire using the direct terms of “electronic consultation” or “curbside consultation” because we were uncertain whether patients would recognize the terms vs using a general description of the interaction. We also did not assess the factors underlying patient preferences.
Further work is needed to understand whether our observations are similar in other migraine patient populations and whether they might differ by race and sex. Because the social determinants of health substantially influence health-related and quality-of-life outcomes, we plan to include these in future patient surveys.
Because survey participants have not undergone the full range of options presented, future directions include incorporation of perceived preferences into care delivery strategies and modification of strategies based on migraine frequency and disability. It is possible that preferences might change after patients directly experience different interventions. For example, the collective preference was generally low for nurse-driven or pharmacist-driven encounters and generalized educational opportunities, but it is not clear whether they would remain low with additional direct experience with these strategies. It will also be important to understand the challenges that may be introduced by preexisting preferences. Ultimately, we will aim to better understand how and if care models that are better aligned with patient preferences improve migraine frequency, associated disability, quality of life, and patient satisfaction with the implemented changes.
Our study suggests that clinical care preferences differ by migraine frequency and disability and that models should consider these preferences when attempting to improve access to specialty advice, ongoing care, and patient satisfaction. Patients with migraine in this study preferred physician-driven care, including options that decrease the need for face-to-face appointments. Preference was lower for nurse-driven and pharmacist-driven encounters and more generalized educational opportunities. Observations support continued development of care pathways that include primary care with formalized options for collaboration with a neurologist and that focus neurologist resources based on migraine frequency and disability. Last, outpatients indicated a strong desire for actionable written care plans with alternative treatment options and convenient options to change the care plan when needed.
Appendix. Authors
Study Funding
CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS) Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
Disclosure
The authors report no relevant disclosures. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
TAKE-HOME POINTS
→ Compared with patients with episodic migraine, those with chronic migraine have higher levels of disability, lower levels of satisfaction with their care, and less satisfaction with access to medical care and advice.
→ Patient preferences for specific methods of care delivery differ based on migraine frequency and level of migraine-associated disability.
→ Findings support development of care pathways that include a written migraine action plan, traditional and nontraditional primary care–neurology collaboration, and prioritization of formal neurology consultation for patients with the highest disability.
References
- 1.GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954-976. doi. 10.1016/S1474-4422(18)30322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wongsiriroj S, Grillo E, Levi S, et al. Management of migraine and the accessibility of specialist care: findings from an extended multinational survey (my migraine center survey). Neurol Ther. 2020;9(2):551-565. doi. 10.1007/s40120-020-00205-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao YJ, Ong JJY, Goadsby PJ. Emerging treatment options for migraine. Ann Acad Med Singap. 2020;49(4):226-235. doi. 10.47102/annals-acadmed.sg.2019255. [DOI] [PubMed] [Google Scholar]
- 4.Silberstein SD. Considerations for management of migraine symptoms in the primary care setting. Postgrad Med. 2016;128(5):523-537. doi. 10.1080/00325481.2016.1175912. [DOI] [PubMed] [Google Scholar]
- 5.Petterson SM, Liaw WR, Tran C, Bazemore AW. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035. Ann Fam Med. 2015;13(2):107-114. doi. 10.1370/afm.1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burton A. How do we fix the shortage of neurologists? Lancet Neurol. 2018;17(6):502-503. doi. 10.1016/s1474-4422(18)30143-1. [DOI] [PubMed] [Google Scholar]
- 7.Robblee J, Starling AJ. E-Consultation in headache medicine: a quality improvement pilot study. Headache. 2020;60(10):2192-2201. doi. 10.1111/head.13981. [DOI] [PubMed] [Google Scholar]
- 8.Young NP, Elrashidi MY, Crane SJ, Ebbert JO. Pilot of integrated, colocated neurology in a primary care medical home. J Eval Clin Pract. 2017;23(3):548-553. doi. 10.1111/jep.12667. [DOI] [PubMed] [Google Scholar]
- 9.Demaerschalk BM, Levine SR. Telestroke: solid support for virtual acute stroke care. Neurology. 2016;87(13):1314-1315. doi. 10.1212/wnl.0000000000003166. [DOI] [PubMed] [Google Scholar]
- 10.Young NP, Burkholder DB, Philpot LM, McKie PM, Ebbert JO. Synchronous neurology-primary care collaboration in a medical home. Neurol Clin Pract. 2020;10(5):388-395. doi. 10.1212/cpj.0000000000000754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bigal ME, Serrano D, Reed M, Lipton RB. Chronic migraine in the population: burden, diagnosis, and satisfaction with treatment. Neurology. 2008;71(8):559-566. doi. 10.1212/01.wnl.0000323925.29520.e7. [DOI] [PubMed] [Google Scholar]
- 12.Lipton RB, Silberstein SD. Episodic and chronic migraine headache: breaking down barriers to optimal treatment and prevention. Headache. 2015;55(suppl 2):103123-122106. doi. 10.1111/head.12505_2. [DOI] [PubMed] [Google Scholar]
- 13.Dodick DW, Loder EW, Manack Adams A, et al. Assessing barriers to chronic migraine consultation, diagnosis, and treatment: results from the chronic migraine epidemiology and outcomes (CaMEO) study. Headache. 2016;56(5):821-834. doi. 10.1111/head.12774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Messali A, Sanderson JC, Blumenfeld AM, et al. Direct and indirect costs of chronic and episodic migraine in the United States: a web-based survey. Headache. 2016;56(2):306-322. doi. 10.1111/head.12755. [DOI] [PubMed] [Google Scholar]
- 15.Bloudek LM, Stokes M, Buse DC, et al. Cost of healthcare for patients with migraine in five European countries: results from the International Burden of Migraine Study (IBMS). J Headache Pain. 2012;13(5):361-378. doi. 10.1007/s10194-012-0460-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silberstein SD, Lee L, Gandhi K, Fitzgerald T, Bell J, Cohen JM. Health care resource utilization and migraine disability along the migraine continuum among patients treated for migraine. Headache. 2018;58(10):1579-1592. doi. 10.1111/head.13421. [DOI] [PubMed] [Google Scholar]
- 17.Young NP, Philpot LM, Vierkant RA, et al. Episodic and chronic migraine in primary care. Headache. 2019;59(7):1042-1051. doi. 10.1111/head.13543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart WF, Lipton RB, Kolodner K. Migraine disability assessment (MIDAS) score: relation to headache frequency, pain intensity, and headache symptoms. Headache. 2003;43(3):258-265. doi. 10.1046/j.1526-4610.2003.03050.x. [DOI] [PubMed] [Google Scholar]
- 19.Stewart WF, Lipton RB, Whyte J, et al. An international study to assess reliability of the Migraine Disability Assessment (MIDAS) score. Neurology. 1999;53(5):988-994. doi. 10.1212/wnl.53.5.988. [DOI] [PubMed] [Google Scholar]
- 20.Bigal ME, Rapoport AM, Lipton RB, Tepper SJ, Sheftell FD. Assessment of migraine disability using the migraine disability assessment (MIDAS) questionnaire: a comparison of chronic migraine with episodic migraine. Headache. 2003;43(4):336-342. doi. 10.1046/j.1526-4610.2003.03068.x. [DOI] [PubMed] [Google Scholar]
- 21.Lipton RB, Serrano D, Holland S, Fanning KM, Reed ML, Buse DC. Barriers to the diagnosis and treatment of migraine: effects of sex, income, and headache features. Headache. 2013;53(1):81-92. doi. 10.1111/j.1526-4610.2012.02265.x. [DOI] [PubMed] [Google Scholar]
- 22.Blumenfeld AM, Varon SF, Wilcox TK, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the International Burden of Migraine Study (IBMS). Cephalalgia. 2011;31(3):301-315. doi. 10.1177/0333102410381145. [DOI] [PubMed] [Google Scholar]
- 23.Torres-Ferrus M, Quintana M, Fernandez-Morales J, Alvarez-Sabin J, Pozo-Rosich P. When does chronic migraine strike? A clinical comparison of migraine according to the headache days suffered per month. Cephalalgia. 2017;37(2):104-113. doi. 10.1177/0333102416636055. [DOI] [PubMed] [Google Scholar]
- 24.Burch RC, Loder S, Loder E, Smitherman TA. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache. 2015;55(1):21-34. doi. 10.1111/head.12482. [DOI] [PubMed] [Google Scholar]
- 25.De Diego EV, Lanteri-Minet M. Recognition and management of migraine in primary care: influence of functional impact measured by the headache impact test (HIT). Cephalalgia. 2005;25(3):184-190. doi. 10.1111/j.1468-2982.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- 26.Minen MT, Loder E, Tishler L, Silbersweig D. Migraine diagnosis and treatment: a knowledge and needs assessment among primary care providers. Cephalalgia. 2016;36(4):358-370. doi. 10.1177/0333102415593086. [DOI] [PubMed] [Google Scholar]
- 27.Turner SB, Rende EK, Szperka CL, Hershey AD, Gelfand AA. The development of the pediatric migraine action plan (PedMAP). Headache. 2019;59(10):1671-1672. doi. 10.1111/head.13666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turner SB, Rende EK, Pezzuto T, et al. Pediatric migraine action plan (PedMAP). Headache. 2019;59(10):1871-1873. doi. 10.1111/head.13681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peretz AM, Minen MT, Cowan R, Strauss LD. Introducing the migraine action plan. Headache. 2018;58(2):195. doi. 10.1111/head.13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peretz AM, Minen MT, Cowan R, Strauss LD. Migraine action plan (MAP). Headache. 2018;58(2):355-356. doi. 10.1111/head.13255. [DOI] [PubMed] [Google Scholar]
- 31.Lipton RB, Manack Adams A, Buse DC, Fanning KM, Reed ML. A comparison of the chronic migraine epidemiology and outcomes (CaMEO) study and American migraine prevalence and prevention (AMPP) study: demographics and headache-related disability. Headache. 2016;56(8):1280-1289. doi. 10.1111/head.12878. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to copyright restrictions, the paper survey will not be shared. Anonymized survey results data unpublished within this article will be made available by request from any qualified investigator.