Abstract
Massive calcification of the left atrium usually spares the interatrial septum, which provides a cleavage plane for surgical access to the mitral valve. Endoatriectomy with mitral valve replacement is the currently accepted corrective procedure because it affords maximum exposure while decreasing the risk of embolization and intraoperative hemorrhage. We describe a case in which the entire left atrium, including the septum, was thickly calcified and resembled a coconut shell. This condition prevented surgical correction of severe mitral stenosis. To our knowledge, this is the most severe case of left atrial calcification yet reported in the literature. Although it is not possible to establish preoperatively that the atrium is completely calcified and impossible to incise, when predisposing factors and evidence of complete transmural calcification are present, the surgeon should be aware of this possibility and should weigh carefully the decision to operate.
Key words: Calcinosis/complications, calcinosis/surgery, heart atrium/surgery, heart valve prosthesis, mitral valve stenosis/surgery, rheumatic heart disease/complications
Calcification of the left atrium was originally described in 1898. 1 Usually associated with rheumatic valvular disease, it is no longer considered a medical curiosity. In the less severe forms, calcification may involve the atrial appendage, the free wall of the left atrium, or the mitral valve apparatus. The most severe form heretofore described—“porcelain atrium”—has been reported infrequently; it involves the left atrial appendage, the atrial free wall, and the mitral valve apparatus. The interatrial septum is usually spared, and this provides surgical access to the mitral valve. We report a case of “coconut atrium,” in which dense calcification involved all areas of the left atrium, including the septum, and prevented surgical correction of severe mitral stenosis. This is, to our knowledge, the most severe case of left atrial calcification yet reported in the literature.
Case Report
A 67-year-old woman was 1st admitted to the cardiology service at our institution on 6 June 1997 with chronic atrial fibrillation and congestive heart failure (New York Heart Association functional class IV). Her medical history revealed a previous mitral commissurotomy via a right thoracotomy 26 years earlier for rheumatic mitral stenosis. More recently, she had been diagnosed with bronchiectasis, hyperlipidemia, and glucose intolerance. Chest radiography showed marked calcification of the left atrium. Transthoracic and transesophageal echocardiography demonstrated severe mitral stenosis, pulmonary artery pressure of 100 mmHg, and severe tricuspid insufficiency, and it confirmed the presence of calcification of the left atrium and mitral annulus (Fig. 1). The patient's condition improved upon medical therapy. She was offered mitral valve replacement with possible endoatriectomy, but she refused angiography and surgery. She went to another institution seeking percutaneous mitral valvuloplasty, but she was not accepted for the procedure because of calcification; once again, the patient was offered and declined mitral valve replacement. Subsequently, she was admitted several times to different hospitals for repeated episodes of congestive heart failure. On 24 August 1997, she was brought by ambulance to our emergency department with acute pulmonary edema. She was stabilized and again refused surgery. Five days later, she further decompensated and developed severe pulmonary edema and oliguria. At this point, she requested surgery. Limited coronary angiography, performed on an emergency basis, demonstrated minimal coronary artery stenoses. She was taken to the operating room for urgent surgery.
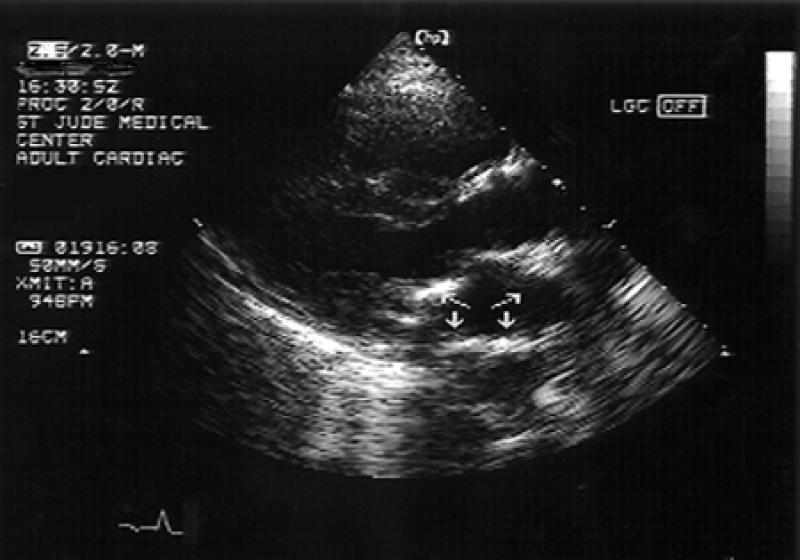
Fig. 1 Transesophageal echocardiography demonstrates the presence of dense transmural calcification of the mitral annulus (broken arrows) and the left atrial wall (solid arrows).
Surgical Technique
The heart was exposed through a median resternotomy. Cardiopulmonary bypass was established through aortic and bicaval cannulation, and the aorta was cross-clamped. The myocardium was protected with antegrade and retrograde induction of warm-blood cardioplegic solution, followed by intermittent cold retrograde infusions every 15 minutes, with continuous venting through the aortic root. Systemic hypothermia was maintained at 25 °C.
The 1st attempt at exposure of the mitral valve was made through the left atrium behind the interatrial groove. The left atrial wall was completely calcified into the epicardium and could not be penetrated. The most distal half-centimeter of the right pulmonary veins was also calcified. When the dome of the left atrium was exposed between the superior vena cava and the aorta, it was found to be equally calcified. The right atrium was then opened and the interatrial septum exposed through a Dubost incision. The septum also showed complete transmural calcification. Further attempts to find an accessible area by probing all 3 areas with a scalpel were unsuccessful. Access to the mitral valve could not be achieved. A DeVega annuloplasty was performed to correct the tricuspid insufficiency. The patient was weaned from cardiopulmonary bypass by means of intra-aortic balloon counterpulsation and inotropic support. She died 48 hours later as a result of multiorgan system failure.
Discussion
Massive calcification of the left atrium predominantly affects women (74% of cases), 2 and is almost always associated with rheumatic mitral stenosis. At the time of diagnosis, most patients have experienced symptoms for an average of 17 to 20 years, 2 and almost all have atrial fibrillation, with an average duration of 10 years. 3 In more recent series, 4 most patients have previously undergone mitral valve operations.
Because of its potential to greatly complicate atriotomy, severe calcification of the left atrial wall should be anticipated prior to surgery. Particle embolization, difficult access to the mitral valve, and hemorrhage upon closure of the atriotomy are likely to occur. In most cases, an internal cast of calcium that does not involve much more than the endocardium can be removed by endoatriectomy. 3,4
Harthorne and coworkers 2 reviewed the literature in 1966 and added 16 cases of significant atrial calcification. The septum was spared in all cases. The most severe form of calcification of the left atrium reported up to the present time was found at operation and did involve the interatrial septum. 3 In this case, Ruvolo and colleagues were able to make one small incision behind the interatrial groove and then a transseptal incision, which made possible a total endoatriectomy and mitral valve replacement. The surgical mortality rate for this entity has been estimated as high as 25%. 2 Our patient had no spare area without calcification in the entire left atrium or the interatrial septum, and this dense transmural calcification resembled a coconut shell.
Difficulty in finding a cleavage plane for the atriotomy, hemorrhage following attempts at closure of the calcified atrial wall, and embolization can usually be circumvented by approaching the mitral valve through the right atrium and interatrial septum. Endoatriectomy both exposes the mitral valve and significantly reduces the risk of embolization. Because we were not aware of any previous cases in which the interatrial septum was completely calcified, we did not anticipate this situation.
Transesophageal echocardiography (TEE) enables excellent visualization of the left atrium because of the anatomic proximity of the esophagus. However, dense calcification of the atrial wall can prevent visualization of the interior of the chamber so that intracavitary thrombus and the septum cannot be seen. 5 Magnetic resonance imaging may demonstrate the presence of thrombus, but its ability to delineate universal septal calcification is suboptimal. Computed tomography (CT) demonstrates calcium well, but even with high-resolution techniques it does not reveal with certainty whether the septum is fully involved.
Although it is not possible to establish preoperatively that the atrium is completely calcified and impossible to incise, the surgeon should be aware of this possibility. If the predisposing factors are present (a woman with a long history of mitral stenosis), and if there is evidence of complete transmural calcification (i.e., the septum cannot be visualized by TEE and appears to be calcific by CT), the surgeon should suspect “coconut atrium” and should weigh carefully the decision to operate.
Footnotes
Address for reprints: Carlos Del Campo MD, Suite 195, 301 W. Bastanchury Rd., Fullerton, CA 92835
*RDCS = Registered Diagnostic Cardiac Sonographer; RVT = Registered Vascular Technologist; RT = Radiologic Technologist; CVT = Certified Vascular Technologist
References
- 1.Claude H, Levaditi P. Endocardite chronique a forme ulcereuse de la paroi auriculaire gauche avec infiltration calcaire consecutive. Bull Soc Anat Paris 1898;73:641.
- 2.Harthorne JW, Seltzer RA, Austen WG. Left atrial calcification. Review of the literature and proposed management. Circulation 1966;34:198–210. [DOI] [PubMed]
- 3.Ruvolo G, Greco E, Speziale G, Mercogliano D, Marino B. “Mold-like” calcification of the left atrium and of the pulmonary veins. Total endoatriectomy in a patient undergoing mitral valve replacement. Eur J Cardiothorac Surg 1994;8:54–5. [DOI] [PubMed]
- 4.Vallejo JL, Merino C, Gonzalez-Santos JM, Bastida E, Albertos J, Riesgo MJ, et al. Massive calcification of the left atrium: surgical implications. Ann Thorac Surg 1995;60:1226–9. [DOI] [PubMed]
- 5.Vilacosta I, Gomez J, Almeria C, Castillo JA, San Roman JA, Zamorano J, et al. Massive left atrial calcification: a limitation of transesophageal echocardiography. Am Heart J 1994;127:461–3. [DOI] [PubMed]


