Abstract
Prior studies of cardiovascular health (CVH) disparities among immigrants of South Asian-origin in the United States (U.S.) have examined South Asians as one homogenous group, focused primarily on Indian-origin immigrants, and examined risk at the individual level. We present current knowledge and evidence gaps about CVH in the three largest South Asian-origin populations in the U.S.- Bangladeshi, Indian, and Pakistani- and draw on socioecological and lifecourse frameworks to propose a conceptual framework for investigating multilevel risk and protective factors of CVH across these groups. The central hypothesis is that CVH disparities among South Asian populations exist due to differences in structural and social determinants, including lived experiences like discrimination, and that acculturation strategies and resilience resources (e.g. neighborhood environment, education, religiosity, social support) ameliorate stressors to act as health protective factors. Our framework advances conceptualization of the heterogeneity and drivers of cardiovascular disparities in diverse South Asian-origin populations. We present specific recommendation to inform the design of future epidemiologic studies on South Asian immigrant health and the development of multilevel interventions to reduce CVH disparities and promote well-being.
Keywords: South Asian People, Cardiovascular Diseases, Immigrants, Social Determinants of Health
Introduction
People of South Asian-origin (Bangladeshi, Bhutanese, Indian, Maldivian, Nepalese, Pakistani, and Sri Lankan) account for almost a quarter of the world’s population, and the South Asian diaspora is one of the largest and most widespread across the globe [1]. Studies from Europe and North America have consistently shown that immigrants of South Asian-origin experience significant atherosclerotic cardiovascular disease (ASCVD) disparities, as evidenced by increased risk factor burden, higher hospitalization, and mortality rates compared with North-American White and European-origin populations [2–5].
Both the 2016 European prevention guidelines and 2018 American Heart Association/American College of Cardiology multi-society cholesterol guidelines now include South Asian ethnicity as a risk-enhancer when considering the initiation of statin therapy [6, 7]. However, South Asian is a broad label that encompasses the diverse populations of South Asia, and most certainly masks heterogeneity in cardiovascular risk. Moreover, use of this broad label and application in health research does not call attention to the structural and social factors that concentrate exposures and resources underlying cardiovascular disparities in minoritized communities.
The South Asian umbrella term includes people from Bangladesh, Bhutan, India, the Maldives, Nepal, Pakistan and Sri Lanka, and also members of the South Asian diaspora who migrated to other parts of the world, including the Caribbean, South America, Africa, Oceana, and Europe [1]. The people aggregated into the South Asian-origin category have diverse ethnic, linguistic, cultural, and religious backgrounds, as well as varied migration histories globally. Prior to 1947, the Indian subcontinent had been colonized by Britain for almost 200 years. In 1947, the Indian subcontinent was divided into 2 countries, India (a majority Hindu country) and Pakistan (a majority Muslim country). East Bengal, which was originally included in Pakistan, gained independence in 1971, and became Bangladesh. The division of the Indian subcontinent set off one of the largest forced migrations of people in history, and this event continues to shape the identity of South Asia creating displaced communities within and outside of South Asian nations [8]. Other South Asian countries, including Bhutan, Maldives, Nepal, and Sri Lanka have distinct political and economic histories which have also impacted migration and settlement patterns [9–11].
The South Asian population in the United States (U.S.) grew rapidly over the past decade, largely fueled by immigration (Table 1) [12]. Bangladeshis, Indians, and Pakistanis are the three largest South Asian groups in the U.S.; however, over the past decade, some of the smaller origin groups – such as Nepalese – experienced the fastest growth rates (Table 1) [13]. Approximately 70% of South Asian-origin people in the U.S. are first generation immigrants [12].
Table 1:
Largest South Asian origin groups in U.S. in 2010 and 2019
| Origin Group | Population | ||
|---|---|---|---|
|
| |||
| 2010 | 2019 | Percent Growth | |
| Bangladeshi | 147,000 | 208,000 | 41% |
| Bhutanese | 19,000 | 24,000 | 26% |
| Indian | 3,183,000 | 4,686,000 | 45% |
| Nepalese | 59,000 | 198,000 | 235% |
| Pakistani | 409,000 | 554,000 | 35% |
| Sri Lankan | 45,000 | 56,000 | 24% |
| Total | 3,862,000 | 5,726,000 | 48% |
Data are from the Pew Research Center.13
Current knowledge about CVH in immigrants from Bangladesh, India, and Pakistan
The majority of studies about ASCVD among South Asian communities in the U.S. have included predominantly Indian participants [14, 15]. For example, in the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study, the first federally-funded longitudinal cohort of South Asians in the U.S., 83% of participants are Indian immigrants (n=965); only 6% are from Pakistan and 0.5% are from Bangladesh (2% were born in the U.S., and the remaining 8% were born in other diaspora countries) [15]. The MASALA study has shown that South Asian Americans have a high prevalence of diabetes and hypertension [16], lower levels of physical activity, and more visceral adiposity and hepatic fat at a lower body mass index [17, 18], than non-Hispanic White, Black, Hispanic, and Chinese Americans. However, since 2010 when MASALA was established, the Pakistani and Bangladeshi populations have grown substantially in the U.S., and comprise 10% and 3% of South Asian immigrants, respectively [19]. Yet little is known about the health and wellbeing of these South Asian-origin people in the U.S., and how their health may differ from Indians.
Studies in South Asia and from several South Asian diaspora communities demonstrate that cardiovascular health (CVH, a combination of behavioral and clinical risk factors: diet, physical activity, tobacco, sleep, obesity, diabetes, hypertension, and dyslipidemia)[20] and ASCVD outcomes vary by country of origin. Among the five South Asian countries studied in the INTERHEART study, the highest prevalence of ASCVD risk factors was in Bangladesh [21, 22]. Emerging evidence from diaspora countries also show worse CVH in Bangladeshi and Pakistani people than in Indian people. For example, Pakistani and Bangladeshi immigrants in Canada have higher age-standardized incidence of a major cardiovascular event compared to Indian immigrants [4]. In both the United Kingdom (U.K.) and in Catalonia, Spain, poor CVH and ASCVD incidence are higher in Bangladeshi and Pakistani individuals compared to Indians [2, 5]. Preliminary data from the MASALA study showed that the unadjusted diabetes and obesity prevalence was higher in Pakistani participants compared to Indian participants [23]. However, clinical risk factors do not fully explain the elevated ASCVD risk observed among South Asians or the CVH disparities between South Asian subgroups. In the U.K. Biobank study, lower socioeconomic status among Bangladeshi and Pakistani participants compared to Indian participants partially explained subgroup differences in CVH among South Asians [5]. While health data on disaggregated South Asian national groups in the U.S. is sparse, the American Community Survey (Table 2) show wide gaps in educational attainment, income inequality, and English language proficiency between Bangladeshi, Indian, and Pakistani immigrants [13]. Few studies have been designed to look at across group differences and how multilevel determinants shape CVH exposures and outcomes among these populations. In 2021, the MASALA study received new funding to expand the current cohort to include people of Pakistani and Bangladeshi-origin to better define differences in CVH between the three largest South Asian-origin groups, and to determine how biopsychosocial and ecological characteristics may associate and interact with country of origin to influence cardiovascular disparities (Clinical Trial Identifier: NCT01207167).
Table 2:
Characteristics of Foreign-Born South Asians by subgroup in the U.S. (American Community Survey, 2017–19)*
| Bangladesh | Bhutan | India | Nepal | Pakistan | Sri Lanka | |
|---|---|---|---|---|---|---|
| % who have lived in US: | ||||||
| 0–10 years | 49 | 86 | 43 | 74 | 37 | 42 |
| More than 10 years (%) | 51 | 14 | 57 | 26 | 63 | 58 |
| Median household income | $58,600 | *** | $120,000 | $55,700 | $75,500 | $84,000 |
| % Living in poverty | 19 | 13 | 6 | 17 | 15 | 9 |
| Limited English proficiency, % | 45 | 64 | 23 | 52 | 33 | 21 |
| Educational attainment ≤high school, % | 35 | 75 | 16 | 43 | 28 | 21 |
| No health insurance, % | 12 | 9 | 5 | 14 | 9 | 9 |
Source: Pew Research Center analysis of 2017–2019 American Community Survey (IPUMS).13
Insufficient data to provide a reliable estimate.
Although the high prevalence of ASCVD in people of South Asian-origin overall may be bolstered in part by genetic variation, the patterns of genetic diversity within South Asians do not follow recently constructed national boundaries [24], and there is little evidence to support genetic heterogeneity as the main driver of differences in ASCVD between South Asian-origin groups [25]. The problem with aggregating all South Asians into a single category for ASCVD risk prediction is that this strategy signals a common genetic underpinning, masks intragroup cardiovascular health disparities, and disregards the social and structural inequities that drive health disparities. Studying the cardiovascular health of individual South Asian immigrant communities in the U.S. is a key opportunity to dispel the notion that racial or ethnic subgroup categories like “South Asian” are biological categories, and instead examine how heterogeneity in multilevel risk and protective factors underlie ASCVD disparities by country of origin and nativity. Critical knowledge gaps about the health of different South Asian populations limit public health and clinical efforts to achieve health equity in these rapidly growing immigrant populations.
Conceptual Framework
The broad construct of “South Asian” reflects a population with shared geographic, historic, cultural, and religious traditions. Yet this categorization obscures the dynamic nature of identity, as well as the tremendous heterogeneity in structural, social, and cultural factors that shape the lived experiences and health of the people who are categorized as South Asian. In the context of immigration, the term “South Asian” is not always meaningful because many first-generation immigrants will more strongly identify with their specific homeland or even national or sub-national language or regional group [26]. Given these variations, the term South Asian and what it represents must be clearly defined in epidemiologic research, and it is important to recognize similarities and differences between groups [27]. Attention to this heterogeneity in epidemiologic research requires not just sufficient sample sizes, but also integrating theories and concepts that can help identify root causes of CVH disparities among U.S. South Asian populations and provide deeper understanding of exposures and resources underlying differences in health outcomes.
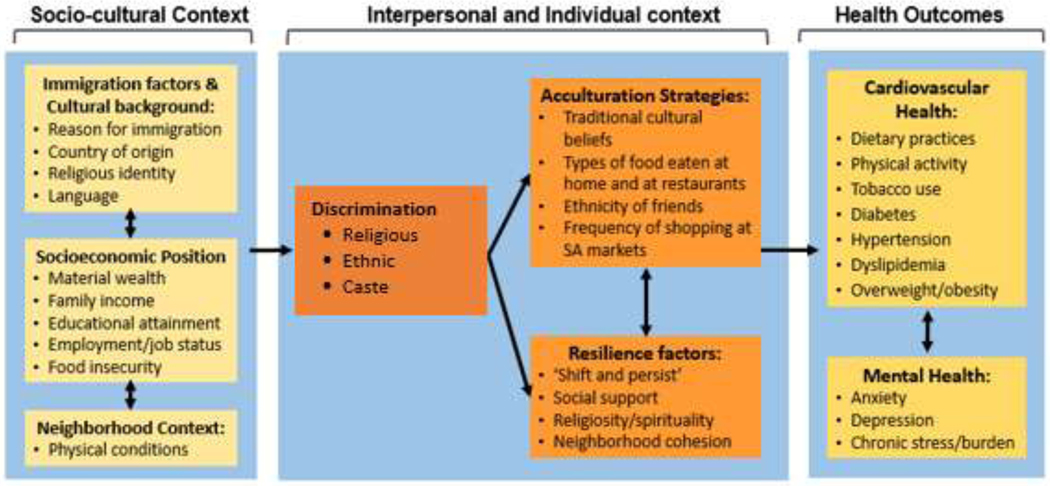
Theoretical and preliminary empiric evidence support the idea that heterogeneity in multilevel structural, social, cultural (hereafter referred to as socio-cultural), and psychological context shape differential risk exposures and resilience resources that produce health disparities among and between South Asian immigrants [28]. We conceptualized the structural and socio-cultural context as exerting independent effects on CVH, and also shaping the interpersonal and individual level factors that affect ASCVD development and outcomes in South Asian immigrants (Figure 1). This conceptual framework can guide the study and understanding of CVH among immigrants from Bangladesh, India, and Pakistan that is supported by: a) a biopsychosocial and ecological paradigm; and b) preliminary data from the MASALA study showing that acculturation strategies and resilience resources may be protective against CVD risk for some South Asian immigrants. Few have integrated these constructs into a broader framework that accounts for how biopsychosocial and ecological characteristics may associate and interact with country of origin to influence CVH, thus advancing the science of health disparities research.
Figure 1.
Conceptual Framework: Multilevel Drivers of Health Outcomes in South Asian Immigrants
Immigration, socioeconomic position, and neighborhood characteristics have direct and indirect influences on CVH
First generation South Asian immigrants undergo environmental, social, cultural, and psychological transitions that affect CVH [19]. They are also emigrating from home countries with substantial variation in socioeconomic indicators and CVD risk (Supplemental Table 1) [29–33]. Structural and socio-cultural determinants in the home and receiving country shape the exposures and resources that create CVH disparities, and they affect how immigrant populations experience and adjust in a new country. For example, immigrants from Bangladesh and Pakistan have more recent immigrant histories compared to immigrants from India, with different social networks and access to economic assets and educational resources. Table 2 shows sociodemographic data by South Asian population in the U.S. from a national survey, with notable differences in time in the U.S., economic resources, English language proficiency, educational attainment, and access to health care among subgroups [13, 34]. The proportion of immigrants from Bangladesh living in poverty is 19% compared to 6% of immigrants from India. Studies of South Asian people in the U.K. suggest that CVD risk and outcomes are patterned by socioeconomic position (SEP), with socioeconomic adversity being associated with worse CVH [35]. These data support a deeper investigation of how SEP, gender, and language intersect with country of origin to shape CVH among diverse South Asian immigrant populations.
Experiences of discrimination as an underexplored risk factor for CVD
Racism is a determinant of adverse health outcomes, but the contribution of racism and discrimination to CVH disparities among South Asian people has not been well studied [36]. Racism and discrimination against people of South Asian-origin has historical roots in the first wave of migration during the 1800s, codification of discriminatory laws prohibiting immigration by Indians in the Immigration Act of 1924, and anti-Indian sentiment and hate crimes during the 1980s [37]. Discrimination further intensified after September 11, 2001, when South Asians, mainly people identified as Muslim and Sikh, were targeted by hate and violence, including an escalation of state violence such as profiling, policing, surveillance, detention, and deportation [38]. In 2012, six worshippers were murdered when a gunman targeted a Sikh gurudwara (place of worship) in Wisconsin. Following the 2016 presidential election and passage of Executive Order 13780, “Protecting the Nation from Foreign Terrorist Entry into the United States,” which was felt to disproportionately target Muslim-majority countries, there was an increase in missed primary care appointments and increased emergency department visits among people from Muslim-majority countries living in Minneapolis-St. Paul, Minnesota [39]. In 2017, 50% of people identifying as Muslim reported that they have experienced some form of discrimination in the past twelve months [40]. Individuals from Bangladesh and Pakistan are predominantly Muslim and may have unique experiences with discrimination that impact their health outcomes in addition to being from the South Asian diaspora.
Since the COVID-19 pandemic spread globally, there has been a rise in anti-Asian racism. While much of this racism and violence has specifically targeted East and Southeast Asian people in the U.S., an online survey in late 2020 of 1,200 Indian Americans found that half reported experiences of discrimination, most often based on skin color. Indian Americans who were U.S.- born were more likely to perceive discrimination, and Muslim Indians reported the highest levels of religious discrimination [36]. Among Indian participants in MASALA, higher levels of self-reported discrimination were associated with greater psychological distress, including symptoms of anxiety and depression [41]. In a separate analysis, anxiety, depression, and chronic stress burden were independently associated with higher subclinical atherosclerosis in MASALA study participants, but it is unclear if these findings apply to different South Asian-origin groups [42].
Research in South Asia show links between caste discrimination and mental health and access to healthcare [43–45], but there is little or no exploration of how caste discrimination may operate to influence health among immigrant South Asians. Thus, the intersection of religion with country of origin and immigrant generation are important consideration when studying links between discrimination and health of South Asian-origin groups.
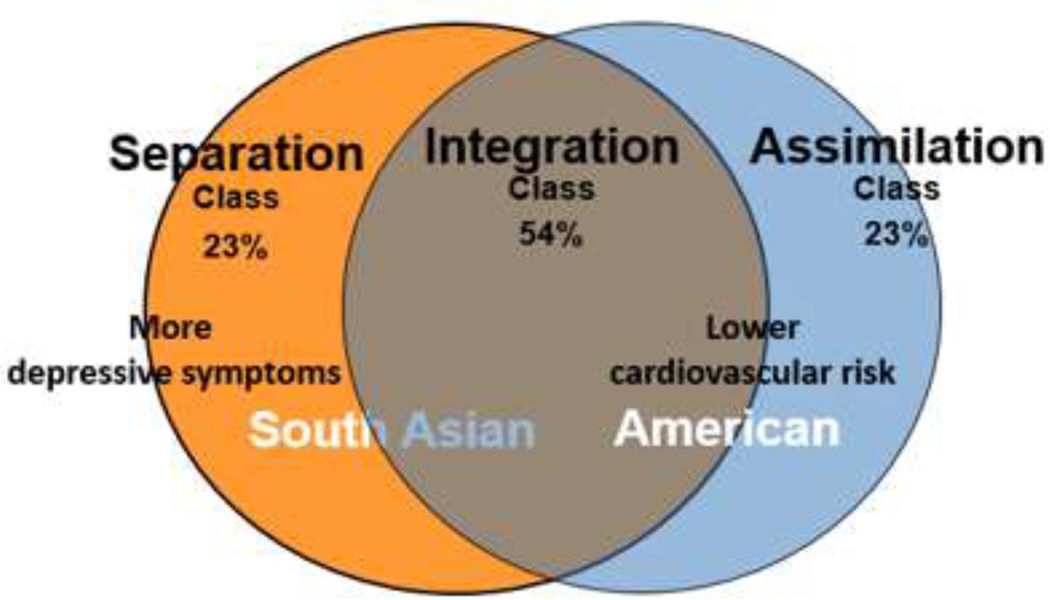
The acculturation process may vary across South Asian-origin groups and link to CVH
In addition to changes in social, economic, and structural context, immigration spurs acculturation, a process by which immigrants retain their cultural heritage and/or adopt the new receiving culture.[46] Many studies have found that acculturation is associated with health outcomes and behaviors in Hispanic and Asian-origin groups. In the MASALA cohort, different proxies for and measures of acculturation (i.e., years in the U.S., cultural beliefs) [47] were independently associated with diet, cardiovascular risk factors, and atherosclerosis [48–50]. For example, living in the U.S. for more years was associated with higher coronary artery calcium, and having a medium level of traditional beliefs, compared to high or low, was associated with less carotid atherosclerosis [48]. The acculturation process can also be understood as coping strategies that immigrants and other ethnic and racial groups use in order to adapt to their contextual circumstances in the U.S. [51]. Using this concept and latent class analysis, we previously identified three acculturation strategies (separation, integration, and assimilation) used by South Asian immigrants in the MASALA study [52]. We found that individuals using a separation strategy (preference for South Asian over U.S. culture) had more depressive symptoms than those who used an integration strategy (similar preference for both cultures) (Figure 2) [53]. Those who used an assimilation strategy (U.S. culture preference) had lower obesity, 2-hour glucose, visceral fat area, and higher HDL-cholesterol than those who used the separation strategy [50]. Hence, assimilation may be beneficial rather than harmful among some South Asian immigrant communities--a clear contrast from findings in other immigrant groups [54–57].
Figure 2.
Acculturation Strategies Derived in the MASALA study
Patterns of intermarriage may also shape acculturation and health outcomes. A study using 2008–2012 ACS data found that among foreign-born Asians, 8% of Sri Lankans, 7.7% of Pakistanis, and 5.4% of Asian Indians were in an interracial marriage [58]. Intermarriage patterns, which vary by country of origin, gender, socioeconomic status, and immigrant generation, could be another factor contributing to heterogeneity in CVH risk via socio-cultural and behavioral mechanisms.
The inconsistent association between acculturation and CVH in South Asian immigrants is not simply a measurement issue. Rather, the process and consequences of acculturation are confounded or moderated by other contextual factors, such as SEP, marriage and family, neighborhood race and ethnic composition, experiences of discrimination, and immigration policies [51]. Because there is variation in experiences of discrimination and the socio-cultural context of Bangladeshi, Indian, and Pakistani individuals in the U.S., there may be differences in the process and health consequences of acculturation. Many questions remain about heterogeneity in the process of acculturation, the context in which it occurs, and the potential CVH implications in diverse South Asian-origin groups.
Resilience resources as protective factors
While ethnicity, immigration factors, low SEP, and discrimination are recognized as risk enhancing factors, the factors that promote CVH, or resilience to CVD, among South Asians, have been underexplored. In its broadest conceptualization, resilience is defined as better than expected outcomes in the presence of exposure to risk [59]. Determinants of resilience include a host of environmental, interpersonal, and individual-level factors (Figure 1) that interact with one another to determine how one responds to stressful experiences. In the MASALA study cohort, perceptions of neighborhood social cohesion and social network size were associated with better CVH, including hypertension and subclinical atherosclerosis [60, 61]. In Indian individuals, having stronger traditional cultural beliefs and an active coping style attenuated the association of discrimination with worse mental health [41].
Several studies also show the protective effects of religiosity and spirituality in South Asian populations [62–64]. Questions related to religion tend to focus more on organizational aspects, while questions on spirituality tend to be about personal experiences outside the confines of institutional religion. In the MASALA study, which included mostly individuals who selfi-dentified as Hindu, followed by Muslim, Jain and Sikh, group prayer outside of religious services was associated with better self-rated health and mental health, along with lower anxiety and anger [65]. In addition, both theistic (closeness to God) and non-theistic religious and spiritual experiences (feeling connected to all of life), were also associated with better self-rated health and mental health outcomes [65]. Religious involvement may effect health through social mechanisms, including social networks, social capital, and cohesion, as well as through coping, values, beliefs, and norms [66]. It is unknown if the protective effects of religiosity are similar in different South Asian-origin groups, by religious denomination, type of congregant setting, gender, SEP, and immigrant generation. The potential of religious and spiritual practices and structures as a health protective factor remains underexplored in diverse South Asian groups.
Finally, psychological factors, such as positive coping and the psychological construct of “shift and persist” have been associated with inflammatory pathways and health outcomes in children and adults [67]. In MASALA, positive coping appeared to partially mitigate the effects of discrimination on health [41]. The shift-and-persist construct entails a combination of reframing stressors more positively while also enduring adversity by finding meaning in life and maintaining optimism. The shift-and-persist approach for dealing with adversity has not been examined among South Asian immigrants and could help identify psychological mechanisms that mitigate stressors associated with immigration and development of CVD. Thus, there is a need to study broader resilience factors in diverse South Asian populations, and if the types of resilience factors and health effects vary by country of origin, historical context, reasons for immigration. Incorporating resilience factors moves beyond a risk-based approach and recognizes the strengths and assets of immigrant communities as health protective factors.
Conclusions
There is a key knowledge gap regarding the heterogeneity of CVH among U.S. South Asian immigrants. Traditional clinical risk factors, like diabetes, hypertension, abdominal obesity, and physical inactivity contribute significantly to ASCVD risk in South Asian immigrants [5, 68]. Yet these established risk factors do not fully explain the higher CVD risk of South Asian individuals compared to people of non-Hispanic White or East Asian background, and there is a need for research on the biopsychosocial and ecological determinants of South Asian health. The conceptual framework proposed in this paper has informed the design of the MASALA expansion study to sequentially collect quantitative and qualitative data to investigate the heterogeneity of cardiovascular risk and resilience between and within Bangladeshi, Indian, and Pakistani immigrants in the U.S. This mixed-methods approach [69], where qualitative data are used to understand the lived experiences of South Asian immigrants and illuminate the complex determinants of CVH offers promise for the development of more effective interpersonal and community-level interventions to improve health.
Supplementary Material
Recommendations.
Key gaps remain in knowledge about the multilevel risks that cause CVH disparities, as well as protective factors that may mitigate them [70, 71]. The framework presented here expands current concepts of CVH disparities in U.S. South Asian immigrant populations and the role of structural, social, cultural, and psychological drivers as key mechanisms underlying differences among and between South Asian-origin subgroups.
Futures studies should:
Provide clarity on which South Asian groups are represented, how the term South Asian is being defined (for example, one or a mix of ancestry, geographical origin, birthplace, language, religion, migration history, name, or self-identity [72], and how this classification is operating to influence a health outcome;
Reconsider the use of “South Asian” ethnicity as a risk factor in health research and clinical care, and instead focus on how structural and social factors pattern risk exposures and resilience resources by national origin subgroup;
Include multilevel measures of resilience to identify components for resilience enhancing interventions that can promote cardiovascular health and wellness;
Recognize how social categories such as socioeconomic position, gender identity, and immigrant generation intersect with country of origin, and design studies with sufficient sample sizes to represent groups with intersectional identities in research;
Include the lived experience of South Asian Americans as empiric knowledge to be integrated with quantitative data. Mixed methods research that collects, analyzes, and interprets quantitative and qualitative data within one study can provide a diversity of perspectives, as well as insights into how people interpret complex phenomena, including the social and cultural context in which health is embedded [73].
The conceptual framework and recommendations we present can inform the design of future epidemiologic studies on South Asian immigrant health and the development of multilevel interventions to reduce CVH disparities and promote well-being.
Highlights.
Immigrants of South Asian origin experience cardiovascular disease disparities.
The category “South Asian” includes diverse populations and masks heterogeneity in health risk.
Structural and social determinants shape health disparities between South Asian immigrant subgroups.
A conceptual framework integrating structural and social determinants should be used to explain cardiovascular disparities between disaggregated South Asian subgroups.
Role of the funding source
NRK, AK, NI received funding from National Institutes of Health R01MD016071. The sponsor had no involvement in this review paper.
Namratha Kandula reports financial support was provided by National Institutes of Health. Alka Kanaya reports financial support was provided by National Institutes of Health. Nadia Islam reports financial support was provided by National Institutes of Health. Namratha Kandula reports a relationship with National Institutes of Health that includes: funding grants.
Abbreviations and acronyms:
- ASCVD
Atherosclerotic cardiovascular disease
- CVH
Cardiovascular health
- CVD
cardiovascular disease
- MASALA
Mediators of Atherosclerosis in South Asians Living in America study
- SEP
Socioeconomic position
- U.S
United States
- U.K.
United Kingdom
Footnotes
Author statement
Namratha Kandula: Conceptualization, Methodology, Writing-original draft preparation; Nadia Islam: Conceptualization and Writing-Reviewing and Editing; Alka Kanaya: Conceptualization and Writing-Reviewing and Editing; Writing Belinda Needham: Writing- Reviewing and Editing; Kiarri Kershaw: Writing- Reviewing and Editing; Lorna Thorpe: Writing- Reviewing and Editing; Edith Chen: Writing- Reviewing and Editing; Neil Zakai: Writing- Reviewing and Editing; Naheed Ahmed: Writing- Reviewing and Editing.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chatterji J, Washbrook DA: Routledge handbook of the South Asian diaspora. London; New York: Routledge; 2013. [Google Scholar]
- 2.Cainzos-Achirica M, Fedeli U, Sattar N, Agyemang C, Jenum AK, McEvoy JW, Murphy JD, Brotons C, Elosua R, Bilal U et al. : Epidemiology, risk factors, and opportunities for prevention of cardiovascular disease in individuals of South Asian ethnicity living in Europe. Atherosclerosis 2019, 286:105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah NS, Xi K, Kapphahn KI, Srinivasan M, Au T, Sathye V, Vishal V, Zhang H, Palaniappan LP: Cardiovascular and Cerebrovascular Disease Mortality in Asian American Subgroups. Circ Cardiovasc Qual Outcomes 2022, 15(5):e008651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tu JV, Chu A, Rezai MR, Guo H, Maclagan LC, Austin PC, Booth GL, Manuel DG, Chiu M, Ko DT et al. : The Incidence of Major Cardiovascular Events in Immigrants to Ontario, Canada: The CANHEART Immigrant Study. Circulation 2015, 132(16):1549–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel AP, Wang M, Kartoun U, Ng K, Khera AV: Quantifying and Understanding the Higher Risk of Atherosclerotic Cardiovascular Disease Among South Asian Individuals: Results From the UK Biobank Prospective Cohort Study. Circulation 2021, 144(6):410–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, De Ferranti S, Faiella-Tommasino J, Forman DE: 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology 2019, 73(24):e285–e350. [DOI] [PubMed] [Google Scholar]
- 7.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney M-T, Corrà U, Cosyns B, Deaton C: Guidelines: Editor’s choice: 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). European heart journal 2016, 37(29):2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bose S, Jalal Ayesha,: Modern South Asia: History, Culture, Political Economy, 4th edn. London; 2017. [Google Scholar]
- 9.Velamati M: Sri Lankan Tamil Migration and Settlement: Time for Reconsideration. India Quarterly 2009, 65(3):271–294. [Google Scholar]
- 10.Ibrahim Y, Rajapillai V, Scott S: Consuming conflict as Tamil consciousness: the case of second-generation British Sri Lankan Tamils. Journal of Ethnic and Migration Studies 2022, 48(5):1133–1151. [Google Scholar]
- 11.Mishra PB: Nepalese Migrants in the United States of America: Perspectives on their Exodus, Assimilation Pattern and Commitment to Nepal. Journal of Ethnic and Migration Studies 2011, 37(9):1527–1537. [Google Scholar]
- 12.South Asian Americans Leading Together: Demographic Snapshot of South Asians in the United States (2019). http://saalt.org/wp-content/uploads/2019/04/SAALT-Demographic-Snapshot-2019.pdf. In.; Accessed on 6/12/19.
- 13.Budiman A & Ruiz N, 2021. Key facts about Asian origin groups in the U.S., Pew Research Center. Retrieved from https://policycommons.net/artifacts/1526591/keyfacts-about-asian-origin-groups-in-the-us/2214831/ on 28 Jul 2022. CID: 20.500.12592/105wrx. [Google Scholar]
- 14.Jose PO, Frank AT, Kapphahn KI, Goldstein BA, Eggleston K, Hastings KG, Cullen MR, Palaniappan LP: Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol 2014, 64(23):2486–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanaya AM, Kandula N, Herrington D, Budoff MJ, Hulley S, Vittinghoff E, Liu K: Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study: Objectives, Methods, and Cohort Description. Clinical cardiology 2013, 36(12):713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanaya AM, Herrington D, Vittinghoff E, Ewing SK, Liu K, Blaha MJ, Dave SS, Qureshi F, Kandula NR: Understanding the high prevalence of diabetes in U.S. south Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes Care 2014, 37(6):1621–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah AD, Kandula NR, Lin F, Allison MA, Carr J, Herrington D, Liu K, Kanaya AM: Less favorable body composition and adipokines in South Asians compared with other US ethnic groups: results from the MASALA and MESA studies. Int J Obes (Lond) 2016, 40(4):639–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gujral UP, Vittinghoff E, Mongraw-Chaffin M, Vaidya D, Kandula NR, Allison M, Carr J, Liu K, Narayan KMV, Kanaya AM: Cardiometabolic Abnormalities Among Normal-Weight Persons From Five Racial/Ethnic Groups in the United States: A Cross-sectional Analysis of Two Cohort Studies. Ann Intern Med 2017, 166(9):628–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Demographic snapshot of South Asians in the United States, April 2019. [https://saalt.org/wp-content/uploads/2019/04/SAALT-Demographic-Snapshot-2019.pdf ]
- 20.Diaz CL, Shah NS, Lloyd-Jones DM, Khan SS: State of the Nation’s Cardiovascular Health and Targeting Health Equity in the United States A Narrative Review. Jama Cardiol 2021, 6(8):963–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J et al. : Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004, 364(9438):937–952. [DOI] [PubMed] [Google Scholar]
- 22.Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, Pandey MR, Haque S, Mendis S, Rangarajan S et al. : Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. Jama 2007, 297:286–294. [DOI] [PubMed] [Google Scholar]
- 23.Reddy NK, Kaushal V, Kanaya AM, Kandula NR, Gujral UP, Shah NS: Cardiovascular risk factor profiles in North and South Indian and Pakistani Americans: The MASALA Study. American Heart Journal 2022, 244:14–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Narasimhan VM, Patterson N, Moorjani P, Rohland N, Bernardos R, Mallick S, Lazaridis I, Nakatsuka N, Olalde I, Lipson M et al. : The formation of human populations in South and Central Asia. Science 2019, 365(6457). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang M, Menon R, Mishra S, Patel Aniruddh P, Chaffin M, Tanneeru D, Deshmukh M, Mathew O, Apte S, Devanboo Christina S et al. : Validation of a Genome-Wide Polygenic Score for Coronary Artery Disease in South Asians. Journal of the American College of Cardiology 2020, 76(6):703–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hall S, Rutherford J: Identity: Community, culture, difference. In.: Lawrence and Wishart; London; 1990. [Google Scholar]
- 27.Schmidt KJ: An Atlas and Survey of South Asian History. New York; 2015. [Google Scholar]
- 28.Bhatia S, Ram A: South Asian Immigration to United States: A Brief History Within the Context of Race, Politics, and Identity. In: Biopsychosocial Approaches to Understanding Health in South Asian Americans. edn. Edited by Perera MJ, Chang EC. Cham: Springer International Publishing; 2018: 15–32. [Google Scholar]
- 29.Monitoring progress on universal health coverage and the health-related Sustainable Development Goals in the WHO South-East Asia Region. In.: World Health Organization; 2021. [Google Scholar]
- 30.Magliano DJ, Fang M, Rooney M, Ogurtsova K, Boyko E, Selvin E: IDF diabetes atlas: global prevalence estimates of prediabetes for 2021 and projections for 2045. Diabetologia 2022, 65(Suppl 1):S95–S95. [Google Scholar]
- 31.Shams P, Hussain M, Karani S, Mahmood S, Hasan A, Siddiqi S, Virani SS, Samad Z: Can Sound Public Health Policies Stem the Tide of Burgeoning Epidemic of Cardiovascular Disease in South Asians? Curr Cardiol Rep 2021, 23(12):181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang HD, Abbas KM, Abbasifard M, Abbasi-Kangevari M, Abbastabar H, Abd-Allah F, Abdelalim A, Abolhassani H, Abreu LG, Abrigo MRM et al. : Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396(10258):1160–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao D: Epidemiological Features of Cardiovascular Disease in Asia. JACC Asia 2021, 1(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pew Research Center analysis of 2013–2015 American Community Survey (IPUMS). [https://www.pewresearch.org/topics/asian-americans/]
- 35.Bhopal R, Hayes L, White M, Unwin N, Harland J, Ayis S, Alberti G: Ethnic and socioeconomic inequalities in coronary heart disease, diabetes and risk factors in Europeans and South Asians. J Public Health Med 2002, 24(2):95–105. [DOI] [PubMed] [Google Scholar]
- 36.Social Realities of Indian Americans: Results From the 2020 Indian American Attitudes Survey - Carnegie Endowment for International Peace https://carnegieendowment.org/2021/06/09/social-realities-of-indian-americans-resultsfrom-2020-indian-american-attitudes-survey-pub-84667 Accessed on July 28, 2022.
- 37.Communities on Fire. From South Asian Americans Leading Together. [https://saalt.org/wp-content/uploads/2018/01/Communities-on-Fire.pdf]
- 38.Misra S, Tankasala N, Yusuf Y, Rao T, Paul A, Khan S, Singh S: Health Implications of Racialized State Violence Against South Asians in the USA. J Racial Ethn Health Disparities 2022, 9(1):1–8. [DOI] [PubMed] [Google Scholar]
- 39.Samuels EA, Orr L, White EB, Saadi A, Padela AI, Westerhaus M, Bhatt AD, Agrawal P, Wang D, Gonsalves G: Health Care Utilization Before and After the “Muslim Ban” Executive Order Among People Born in Muslim-Majority Countries and Living in the US. JAMA Network Open 2021, 4(7):e2118216-e2118216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Center. PR: U.S. Muslims Concerned About Their Place in Society, but Continue to Believe in the American Dream. In.; 2017.
- 41.Nadimpalli SB, Kanaya AM, McDade TW, Kandula NR: Self-reported discrimination and mental health among Asian Indians: Cultural beliefs and coping style as moderators. Asian Am J Psychol 2016, 7(3):185–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shah BM, Shah S, Kandula NR, Gadgil MD, Kanaya AM: Psychosocial Factors Associated with Subclinical Atherosclerosis in South Asians: The MASALA Study. J Immigr Minor Health 2016, 18(6):1317–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Komanapalli V, Rao D: The mental health impact of caste and structural inequalities in higher education in India. Transcult Psychiatry 2021, 58(3):392–403. [DOI] [PubMed] [Google Scholar]
- 44.Patel P, Das M, Das U: The perceptions, health-seeking behaviours and access of Scheduled Caste women to maternal health services in Bihar, India. Reprod Health Matters 2018, 26(54):114–125. [DOI] [PubMed] [Google Scholar]
- 45.Thapa R, van Teijlingen E, Regmi PR, Heaslip V: Caste Exclusion and Health Discrimination in South Asia: A Systematic Review. Asia Pac J Public Health 2021, 33(8):828–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berry JW: Psychology of acculturation. Nebr Symp Motiv 1989, 37:201–234. [PubMed] [Google Scholar]
- 47.Mukherjea A, Underwood KC, Stewart AL, Ivey SL, Kanaya AM: Asian Indian views on diet and health in the United States: importance of understanding cultural and social factors to address disparities. Family & community health 2013, 36(4):311–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kanaya A, Ewing S, Vittinghoff E, Herrington D, Tegeler C, Mills C, Kandula N: Acculturation and Subclinical Atherosclerosis among U.S. South Asians: Findings from the MASALA study. Journal of clinical and experimental research in cardiology 2014, 1(1). [PMC free article] [PubMed] [Google Scholar]
- 49.Gadgil MD, Kandula NR, Kanaya AM: Acculturation is Associated with Dietary Patterns in South Asians in America. J Immigr Minor Health 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Al-Sofiani ME, Langan S, Kanaya AM, Kandula NR, Needham BL, Kim C, Vaidya D, Golden SH, Gudzune KA, Lee CJ: The relationship of acculturation to cardiovascular disease risk factors among U.S. South Asians: Findings from the MASALA study. Diabetes Res Clin Pract 2020, 161:108052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alegria M: The challenge of acculturation measures: what are we missing? A commentary on Thomson & Hoffman-Goetz. Soc Sci Med 2009, 69(7):996–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Needham BL, Mukherjee B, Bagchi P, Kim C, Mukherjea A, Kandula NR, Kanaya AM: Acculturation Strategies Among South Asian Immigrants: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. J Immigr Minor Health 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Needham BL, Mukherjee B, Bagchi P, Kim C, Mukherjea A, Kandula NR, Kanaya AM: Acculturation Strategies and Symptoms of Depression: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. J Immigr Minor Health 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Reed D, McGee D, Cohen J, Yano K, Syme SL, Feinleib M: Acculturation and coronary heart disease among Japanese men in Hawaii. Am J Epidemiol 1982, 115(6):894–905. [DOI] [PubMed] [Google Scholar]
- 55.Hazuda HP, Haffner SM, Stern MP, Eifler CW: Effects of acculturation and socioeconomic status on obesity and diabetes in Mexican Americans. The San Antonio Heart Study. Am J Epidemiol 1988, 128(6):1289–1301. [DOI] [PubMed] [Google Scholar]
- 56.Gordon-Larsen P, Harris KM, Ward DS, Popkin BM, National Longitudinal Study of Adolescent H: Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med 2003, 57(11):2023–2034. [DOI] [PubMed] [Google Scholar]
- 57.Kandula NR, Diez-Roux AV, Chan C, Daviglus ML, Jackson SA, Ni H, Schreiner PJ: Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA). Diabetes Care 2008, 31(8):1621–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang P, Bohm-Jordan M: Patterns of Interracial and Interethnic Marriages among Foreign-Born Asians in the United States. Societies 2018, 8(3). [Google Scholar]
- 59.Tummala-Narra P: Conceptualizing trauma and resilience across diverse contexts: A multicultural perspective. Journal of aggression, maltreatment & trauma 2007, 14(1-2):33–53. [Google Scholar]
- 60.Lagisetty PA, Wen M, Choi H, Heisler M, Kanaya AM, Kandula NR: Neighborhood Social Cohesion and Prevalence of Hypertension and Diabetes in a South Asian Population. J Immigr Minor Health 2016, 18(6):1309–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shah NS, Huffman MD, Khan SS, Schneider JA, Siddique J, Kanaya AM, Kandula NR: Association of social network characteristics with cardiovascular health and coronary artery calcium in South Asians: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. Oral abstract presented at American Heart Association Epi/Lifestyle Council meeting, March, 2020. 2020. [Google Scholar]
- 62.Kent BV, Davidson JC, Zhang Y, Pargament KI, VanderWeele TJ, Koenig H, Underwood LG, Krause N, Kanaya AM, Tworoger SS et al. : Religion and Spirituality among American Indian, South Asian, Black, Hispanic/Latina, and White Women in the Study on Stress, Spirituality, and Health. J Sci Study Relig 2021, 60(1):198–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kent BV, Stroope S, Kanaya AM, Zhang Y, Kandula NR, Shields AE: Private religion/spirituality, self-rated health, and mental health among US South Asians. Qual Life Res 2020, 29(2):495–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stroope S, Kent BV, Zhang Y, Kandula NR, Kanaya AM, Shields AE: Self-Rated Religiosity/Spirituality and Four Health Outcomes Among US South Asians: Findings From the Study on Stress, Spirituality, and Health. J Nerv Ment Dis 2020, 208(2):165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stroope S, Kent BV, Zhang Y, Spiegelman D, Kandula NR, Schachter AB, Kanaya A, Shields AE: ‘Mental health and self-rated health among U.S. South Asians: the role of religious group involvement’. Ethn Health 2022, 27(2):388–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shapiro E: A Protective Canopy: Religious and Social Capital as Elements of a Theory of Religion and Health. J Relig Health 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen E, McLean KC, Miller GE: Shift-and-Persist Strategies: Associations With Socioeconomic Status and the Regulation of Inflammation Among Adolescents and Their Parents. Psychosom Med 2015, 77(4):371–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kanaya AM, Vittinghoff E, Lin F, Kandula NR, Herrington D, Liu K, Blaha M, Budoff MJ: Incidence and Progression of Coronary Artery Calcium in South Asians Compared With 4 Race/Ethnic Groups. J Am Heart Assoc 2019, 8(2):e011053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aspers P, Corte U: What is Qualitative in Qualitative Research. Qual Sociol 2019, 42(2):139–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Volgman AS, Palaniappan LS, Aggarwal NT, Gupta M, Khandelwal A, Krishnan AV, Lichtman JH, Mehta LS, Patel HN, Shah KS et al. : Atherosclerotic Cardiovascular Disease in South Asians in the United States: Epidemiology, Risk Factors, and Treatments. A scientific statement from the American Heart Association. Circulation 2018, 138:e1–e34. [DOI] [PubMed] [Google Scholar]
- 71.Stronks K, Snijder MB, Peters RJG, Prins M, Schene AH, Zwinderman AH: Unravelling the impact of ethnicity on health in Europe: the HELIUS study. BMC Public Health 2013, 13(1):402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bhopal R: Glossary of terms relating to ethnicity and race: for reflection and debate. J Epidemiol Community Health 2004, 58(6):441–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ram A, Dave SS, Lancki N, Moran M, Puri-Taneja A, Mammen S, Kanaya AM, Kandula NR: Social influence of adult children on parental health behavior among South Asian immigrants: findings from the MASALA (Mediators of Atherosclerosis in South Asians Living in America) study. Ethn Health 2022, 27(3):639–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.