Abstract
Objective
High tibial valgus osteotomy (HTO) is a widely accepted procedure indicated for varus knee with symptomatic osteoarthritis of the medial compartment. However, there is a lack of studies evaluating long term results of this procedure. The primary aim of this study was to evaluate the long‐term survival of opening wedge high tibial osteotomy (HTO) for isolated osteoarthritis in the medial compartment of the knee. The secondary objective was to identify independent predictors of conversion to total knee arthroplasty (TKA).
Methods
This is a long term retrospective study of 296 cases of open wedge HTOs performed at a single center (level of evidence IV) between January 2005 and August 2015. Opening wedge medial HTO was always performed after diagnostic arthroscopy. Eighty‐three percent of the population (233 patients, 247 procedures) was followed up at a mean 11.6 years (6–17) by telephone interview, to evaluate the possible conversion to TKA. Mean age at the index operation was 42.8 years (range 15–70) and most patients were male (70%). Associated procedures (e.g., platelet rich plasma supplementation, microfractures, meniscectomy, etc.) were carried out at the time of the HTO in 80 (32%) cases. Survival of HTO and its association with age, sex, body mass index, smoking habit, preoperative severity of varus deformity, cartilage status at surgery, and associated procedures were evaluated. Kaplan–Meier and Cox regression analyses were performed.
Results
Thirty‐three of the 247 HTOs (13.4%) were converted to knee replacement, with 86.6% of the original procedures surviving at a mean 12‐year follow‐up. Kaplan–Meier survival estimates at 17 years for HTO were 75.5% (95% confidence interval [CI] 66.7–84.3). There was significant difference (P < 0.001) in the 17‐year survival rate between obese (55.5%; 95% CI 35.3–75.6) and non‐obese (79.7%; 95% CI 70.1–89.2) patients. The determinants of conversion to knee arthroplasty detected at multivariate Cox regression analysis were body mass index, severity of cartilage degeneration in the medial compartment (Outerbridge grade), and age.
Conclusion
The long‐term survival of open wedge HTO for osteoarthritis in the medial compartment of the knee is satisfactory. The risk of conversion to TKA is significantly increased in obese patients. Advanced age and severity of pre‐existing cartilage damage may also contribute to the risk of conversion to TKA.
Keywords: Failure, High tibial osteotomy, Knee osteoarthritis, Open wedge, Predictors, Survival
The long‐term survival of open wedge HTO for osteoarthritis in the medial compartment of the knee is satisfactory. The risk of conversion to TKA is significantly increased in obese patients. Advanced age and severity of pre‐existing cartilage damage may also contribute to the risk of conversion to TKA.

Introduction
The treatment of osteoarthritis (OA) in the medial compartment of the knee in young, active patients is challenging. Varus malalignment implies an increased risk of progression of medial OA. 1 High tibial valgus osteotomy (HTO) is a widely accepted procedure indicated for varus knee with symptomatic OA or overload (e.g., after medial meniscectomy) of the medial compartment. 2 Although the widespread use of total knee arthroplasty (TKA) has led to a decline in HTO, this procedure has been recently shown to be cost‐effective compared to knee arthroplasty in patients aged 40–60 years with medial OA of the knee. 3 Indeed, the revision rate of TKA in younger, active patients is higher in comparison with older patients 4 , 5 , 6 , 7 due to high mechanical stress on the implant. Moreover, a significant number of younger patients reports dissatisfaction with the functional outcome after TKA. 8 , 9 , 10 , 11 HTO and unicompartmental knee arthroplasty (UKA) are two surgical options for medial unicompartmental knee OA. However, HTO is more indicated for younger patients with high physical activity requirements. Basic surgical techniques of HTO include lateral closing wedge osteotomy and medial opening osteotomy. Lateral closing wedge osteotomy is the historical approach, but it has been associated with a high complication rate in long‐term follow‐up. 12 HTO with medial opening has several advantages, including better collateral ligament tension, easier control of the degree of correction, minimal soft tissue dissection, and lower risk of nerve injury. However, it is unclear whether these advantages are reflected in a higher long‐term survival rate and what factors may influence the outcome of this procedure. 8 , 9 , 12 , 13 Indeed, the number of studies regarding the long‐term survivorship of open‐wedge HTOs is smaller than that of closing wedge HTOs because closing wedge HTOs were introduced earlier. 14 Furthermore, while there has been growing interest in the literature in identifying factors influencing the outcome of trauma surgery 15 and elective orthopedic surgery, 14 , 16 few data are available on determinants of long‐term survivorship of opening wedge HTO in large series of patients. 17 , 18 , 19
The aim of this study was precisely to evaluate the long‐term survival of opening wedge HTO for isolated OA in the medial compartment of the knee in a large series of patients. The secondary objective was to identify independent predictors of conversion to TKA. We hypothesized that multiple factors including age, the severity of cartilage damage in the medial compartment, and the degree of correction obtained with surgery may influence the long‐term survivorship of HTO.
Methods
Design, Participants, and Interventions
This retrospective study was based on 296 opening wedge HTOs performed between January 2005 and August 2015 at the institution of three of the authors (C.Z, V.I, S.N.), a large tertiary care hospital specialized in knee surgery. The local ethical committee confirmed that no ethical approval is required for this observational study. Inclusion criteria were: (i) medial compartment pain; (ii) varus angle between 5 and 15 degrees; and (iii) grade II‐III OA of the medial compartment as assessed by the Kellgren–Lawrence classification 20 on weight‐bearing anteroposterior radiographs. Exclusion criteria were: (i) bicompartmental or tricompartmental knee OA; (ii) abnormal anatomy of tibia; and (iii) previous knee or osteotomy surgery. Forty‐five patients (49 procedures) could not be followed up. Of these, 36 patients could not be traced and nine refused to participate in the study. Hence, the study group was limited to 233 patients and 247 procedures (83% of the total population). Patients' preoperative and operative data were obtained from surgical records and hospital files. Patients with a body mass index (BMI) over 30 were considered obese.
Radiographic Measurements
For preoperative planning, a full‐length anteroposterior radiograph of the weight‐bearing lower extremity was obtained. We used the Miniaci method 21 to plan the correction angle. The preoperative hip‐knee angle (HKA) was calculated on preoperative and postoperative radiographs. The aim of surgery was to achieve 5° tibiofemoral mechanical valgus in a one‐leg standing radiograph postoperatively. 22
Follow‐up Assessment
Telephone interviews were conducted to collect follow‐up data from all patients or, when necessary, from their relatives. All patients gave informed consent to participate in the study. Information was obtained on any operations on their knee after the HTO procedure, their nature, and the time interval since the index procedure. The mean length of follow‐up in the responders was 11.6 years (6–17). Table 1 summarizes the characteristics of patients.
TABLE 1.
Characteristics of the patients (n = 247)
| Mean ± SD or n (%) | Range | |
|---|---|---|
| Age at operation, years | 42.8 ± 14.1 | 15–70 |
| Age at follow‐up, years | 54.4 ± 15.0 | 21–86 |
| Sex | ||
| Female | 74 (30) | |
| Male | 173 (70) | |
| BMI, kg/m2 | 26.6 ± 4.3 | 19–47 |
| Smoking | ||
| No | 213 (86) | |
| Yes | 34 (14) | |
| Follow‐up, yr | 11.6 ± 3.5 | 6–17 |
| Preoperative radiographic HKA, degrees | 173.3 ± 2.0 | 170–178 |
Abbreviations: BMI, body mass index; HKA, hip knee angle; SD, standard deviation.
Surgical Technique
Diagnostic arthroscopy of the knee was routinely performed before tibial osteotomy to assess the severity of cartilage damage. Cartilage lesions were classified according to the Outerbridge classification. 23 After diagnostic arthroscopy, opening HTO was performed through a 6–8 cm skin incision, 2 cm medial to the tibial tuberosity and 2 cm below the joint line. The anterior fibers of the medial collateral ligament were detached. Guided by a Kirschner wire, a monoplanar opening wedge osteotomy was subsequently performed with an ascending bony cut starting at the medial edge of the tibia and directed toward the tibiofibular joint. The osteotomy was opened gradually using chisels and a spreader device. After reaching the expected tibial opening, the osteotomy was secured with a locking plate. The plates used in the study group included 197 VS Osteotomy Systems (Zimmer‐Biomet, Warsaw, IN, USA), 46 Puddu plates (Arthrex, Naples FL, USA), and 4 Tomofix plates (DePuy Synthes, Johnson & Johnson, New Brunswick, NJ, USA). An above‐the‐knee brace was prescribed at discharge, and full weight‐bearing was allowed at 4 weeks postoperatively.
Statistical Analysis
The Kaplan–Meier method was used to estimate the cumulative survival at 17 years after HTO in non‐obese and obese patients and the study group. Intergroup comparison was performed using a log‐rank test. We performed age‐adjusted univariate and multivariate Cox regression analysis to assess the effect of any explanatory variable on HTO survival. We included in the multivariate regression models all the explanatory variables that showed significant association (i.e., P ≤ 0.05) or a trend toward an association (i.e., P ≤ 0.10) with the outcome of interest in the univariate analysis. The following confounding or explanatory variables were tested as predictors of outcome: age, sex, BMI, smoking habit, postoperative varus correction, cartilage degeneration (Outerbridge grade) of the medial compartment, type of locking plate, and use of adjunctive procedures at surgery (i.e., microfractures, platelet rich‐plasma supplementation, meniscectomy). A P value < 0.05 was considered significant. Data were analyzed using SPSS (IBM SPSS, Chicago, IL, USA) version 26.0 software.
Results
General Results and Survivorship
The surgical data of the patients are summarized in Table 2. Thirty‐three of the 247 HTOs (13.4%) were converted to knee replacement during follow‐up, with 86.6% of the original procedures surviving at an average follow‐up of 11.6 years. Reasons for conversion of HTO to TKA were progression of knee osteoarthritis and/or loss of correction angle associated with increasing pain. Conversion occurred at a mean interval of 10.4 years (range, 4 to 16) from the index procedure. Thirty‐one HTO procedures were converted to TKA and 2 to UKA. Kaplan–Meier survival estimates at 17 years for HTO were 75.5% (95% confidence interval [CI] 66.7–84.3) (Fig. 1). The log‐rank test indicated a significant difference (p < 0.001) in the 17‐year survival rate of HTO between obese (55.5%; 95% CI 35.3–75.6) and non‐obese (79.7%; 95% CI 70.1–89.2) patients (Fig. 1).
TABLE 2.
Surgical data of patients
| Factor | Mean (range) or n (%) |
|---|---|
| Severity of cartilage degeneration in the medial compartment (Outerbridge grade) | |
| 0 | 0 (0) |
| 1 | 58 (24) |
| 2 | 43 (17) |
| 3 | 47 (19) |
| 4 | 99 (40) |
| Associated procedures | |
| None | 167 (68) |
| PRP supplementation | 32 (13) |
| Microfractures | 16 (6) |
| Partial meniscectomy | 10 (4) |
| PRP supplementation + microfractures | 8 (3) |
| Autologous chondrocyte implantation | 4 (2) |
| ACL procedures | 4 (2) |
| Microfractures + partial meniscectomy | 3 (1) |
| Partial meniscectomy + PRP supplementation | 2 (1) |
| Autologous chondrocyte implantation + PRP | 1 (0) |
| Postoperative radiographic HKA, degrees | 183.1 (180–190) |
| Surgical correction, degrees | 9.8 (5–20) |
Abbreviations: ACL, anterior cruciate ligament; HKA, hip knee angle; PRP, platelet rich plasma.
Fig. 1.
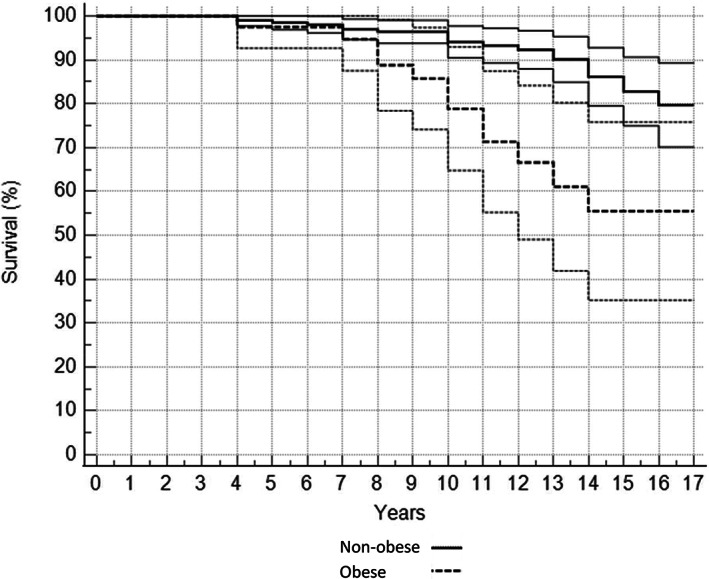
Kaplan–Meier survival curve and 95% Confidence Intervals comparing non‐obese (n = 207) with obese (n = 40) patients after HTO, with conversion to TKA being defined as failure
Outcome Predictors
When age‐adjusted univariate Cox regression analysis was used to examine the determinants of the conversion of HTO to knee replacement, age (hazard ratio (HR) = 1.06; 95% CI = 1.03–1.09; P < 0.001), BMI (HR = 1.12; 95% CI = 1.05 to 1.19; p = 0.001), and the severity of cartilage degeneration (Outerbridge grade)(HR = 2.09; 95% CI = 1.28 to 3.41; P = 0.003) were directly associated with this outcome. The determinants of conversion to knee arthroplasty detected at multivariate Cox regression analysis are shown in Table 3. BMI was the most influential predictor in the model. In the Outerbridge group 4, 23/99 knees (23.2%) were converted to knee arthroplasty, with a significantly higher failure rate than in the groups with less severe cartilage involvement (i.e., Outerbridge grade ≤3), where conversion occurred in 10/148 knees (6.8%) (P < 0.001). Only patients with an Outerbridge grade of 2 or greater required TKA, but no patient in Outerbridge group 1 was converted. Furthermore, only patients with an age at operation greater than 39 years and an age at follow‐up greater than 55 years were converted to TKA. No influence of sex, additional procedures performed at the time of surgery (microfracture, supplementation with platelet‐rich plasma, or meniscectomy), type of locking plate, or postoperative angle correction on HTO survival was detected.
TABLE 3.
Determinants of conversion to total knee arthroplasty at the multivariate Cox regression analysis
| Factor | HR (95% CI) | Chi‐square difference | p |
|---|---|---|---|
| Body mass index | 1.08 (1.01–1.15) | 17.27 | 0.024 |
| Severity of cartilage degeneration in the medial compartment (Outerbridge grade) | 1.84 (1.11–3.06) | 11.45 | 0.018 |
| Age | 1.04 (1.01–1.08) | 5.39 | 0.028 |
Abbreviations: CI, confidence interval; HR, hazard ratio.
Discussion
This study demonstrated that opening wedge HTO in the treatment of medial knee OA has an actual survival of 87% at a mean follow‐up of about 12 years and an estimated survival of 76% at 17 years. To the best of our knowledge, no previous study has reported the survival rate of opening wedge HTO in such a large cohort of patients with comparable long‐term follow‐up. Independent predictors for failure of HTO included older age, higher BMI, and the severity of cartilage deterioration in the medial compartment of the knee at surgery. The likelihood of conversion to knee replacement was higher in obese (i.e., BMI > 30) than in non‐obese subjects.
Long‐Term Survivorship
Long‐term survival rates for HTO have been highly variable in previous studies. Koshino et al. 24 conducted a 15‐ to 28‐year follow‐up study of 75 closing wedge HTOs and found a survival of 95.1% at 10 years and 86.9% at 15 years. In another long‐term study, conducted by Akizuki et al., 25 a total of 94 patients were available for revision at an average of 16.4 years after lateral closing wedge osteotomy. The authors reported survival of 98% at 10 years and 90% at 15 years. Subsequent studies have shown lower long‐term survival rates for HTO. Hui et al. 26 evaluated 394 patients with a mean follow‐up of 12 years and estimated a survival probability of 79% at 10 years and 56% at 15 years for lateral closing wedge HTO. Also the comparative study by Polat et al. 27 reported a lower survival probability for HTO, 71.2% at 10 years and 60.1% at 15 years, regardless of the different surgical technique adopted. In contrast, a meta‐analysis by Kim et al. 14 indicated that the pooled survival rate was higher in opening wedge HTO than in closing wedge HTO at 10 years. Overall, the number of long‐term survival studies of opening wedge HTO and their sample size and follow‐up duration are notably lower than those of closing wedge HTO because closing wedge HTO was introduced earlier. Keenan et al., 17 in a retrospective study of 111 opening wedge HTOs, reported a conversion rate to TKA of 36% at a mean follow‐up of 6.3 years and a survival rate of 65% and 55% at 10 and 15 years, respectively. Primeau et al. 19 showed that the conversion rate of opening wedge HTO to TKA was 21% at 10 years. The multicenter study by Bouguennec et al. 28 reported a survival probability of 74% and 61% at 10 and 12 years, respectively, in HTO. Lastly, a small study by Lau et al. 29 with a median follow‐up of 13 years found a 87% 10‐year survival rate for medial opening wedge HTO. This wide range of different results can be explained by differences in the sample size and surgical technique of the studies, but mainly by their design and completion. However, although data in the literature on the survival rate with a follow‐up of more than 10 years for medial opening wedge HTO are limited, 14 our results concur with studies with shorter follow‐up that reported a 10‐year survival rate of 72% to 100%. 30
Outcome Predictors
Obesity
In the current study, obesity was the main independent predictor of HTO failure. Previous studies also indicated that BMI may affect cartilage regeneration after HTO 22 and represents an independent risk factor for reduced survivorship of the procedure. 18 , 19 , 25 , 26 , 28 In addition to the excessive and altered joint load transmission in subjects with high BMI, the effect of altered lipid metabolism and low‐grade inflammation and adipokines on the joint tissues of obese patients could play a pivotal role in the progression of OA, thus leading to reduced HTO survival. 31
Cartilage Damage
In our cohort of patients, the preoperative damage of articular cartilage was examined by arthroscopy at the time of osteotomy and the severity of involvement of medial compartment of the knee predicted failure of the procedure. Previous studies have indicated that the radiographic degree of OA in the medial compartment is a predictor of poor outcome. 18 , 19 , 28 , 29 One prior study that related the severity of cartilage damage assessed arthroscopically to the long‐term outcome of opening wedge HTO found that patients older than 40 years of age with advanced cartilage damage (Outerbridge 3–4) have a higher incidence of conversion to TKA. 32
Age
In the current study, older patients were significantly more likely to require conversion to TKA than younger patients. This result is in line with most previous long‐term studies that have shown a negative effect of increasing age on HTO survival. 17 , 18 , 19 , 26 , 32 , 33 Articular cartilage undergoes age‐related changes that increase the risk of knee OA and may limit tissue repair that occurs following HTO. 34
Associated Procedures
This study did not find significant effect of concomitant cartilage restoration techniques, including microfractures and/or platelet‐rich plasma supplementation, in increasing HTO survival. Theoretically, the improved load transmission through the knee achieved by osteotomy should allow for enhanced cartilage restoration in the medial compartment of the knee. In this context, the combination of biological procedures could stimulate post‐operative regeneration of articular cartilage or at least prevent the progression of medial OA. Cartilage restoration techniques and platelet‐rich plasma used in combination with HTO have been shown to be effective in improving function and relieving pain after surgery. 35 , 36 A previous literature review 35 also found that performing concomitant microfractures can potentially delay the need for TKA after HTO in the medium term. However, the analysis was limited by the heterogeneity of techniques used for HTO and cartilage restoration, as well as inconsistency of outcome measures in previous studies. Furthermore, long‐term survival has not been previously evaluated. 35 Further high‐quality data are needed to determine whether cartilage restoration procedures may actually be helpful in improving the long‐term HTO survival.
Other Factors
No effect of different locking plates on HTO survival was observed in this study. There are no data in the literature on the influence of different fixation devices on the long‐term outcome and survival of opening wedge HTO. However, biomechanical studies have shown that different locking plates have similar biomechanical properties and sufficient strength to ensure the healing of open wedge HTO. 37 , 38 In the current study, sex was not a risk factor for conversion of HTO to TKA. Previous studies have suggested that women have a higher risk for this event, 17 , 19 while others have not confirmed the relationship with sex 26 or even found that osteotomy failure is less frequent in the female sex. 28 The influence of sex on HTO survival requires further investigation.
Strength and Limitations
The most important strength of the present study is the survival analysis carried out in a large cohort of patients who had undergone opening wedge HTO many years earlier. The Kaplan–Meier analysis enabled meaningful calculation of failure rates despite different follow‐up times, while the Cox regression methodology allowed us to evaluate the effect of several factors on failure of HTO. The present study also has several shortcomings. First, it is limited by the retrospective nature of its design. In addition, the choice of using conversion to TKA as the only indicator of failure of HTO may have underestimated the rate of poor outcomes of the procedure. In fact, some patients, especially in older age, may refuse knee replacement despite the progression of knee OA after HTO. However, the conversion to TKA has been considered the primary endpoint in virtually all published papers reporting HTO survival. Furthermore, knee replacement is an unambiguous event that all patients may accurately recall. Another limitation of this study is that some potential predictors for survival of HTO, including duration of osteoarthritis and the patient's daily activity and physical demand, were not included in the Cox regression analysis. However, it would be difficult to retrospectively establish with sufficient accuracy what is the real ‘beginning’ of osteoarthritis, since symptoms usually do not reflect the severity of the degenerative process and patients are generally unable to recall precisely when symptoms started. We also recognize that physical demand might influence failure of HTO, but unfortunately our study protocol did not include any patient reported outcome neither specific information about patient's daily activity level.
Conclusion
The long‐term survival of open wedge HTO for OA in the medial compartment of the knee is satisfactory. However, the risk of conversion to TKA is significantly increased in obese patients. Advanced age and severity of pre‐existing cartilage damage may also contribute to the risk of conversion to TKA. These prognostic factors should be considered and discussed with patients when planning surgery for isolated medial compartment OA.
Author's Contribution
Conceptualization, A.G., L.F., C.Z.; Methodology, V.I., S.N.; Validation, C.Z., M.M.; Investigation, A.G., L.F.; Formal Analysis, A.C., M.M.; Writing ‐ Original Draft, A.G., L.F.; Writing ‐ Review & Editing, M.M, A.C.; Visualization A.C.; Supervision, C.Z., M.M.
Acknowledgments
Research included in this paper was partly completed at the IRCSS Sacro Cuore Don Calabria, Negrar (Verona, Italy) under the supervision of Dr.C. Zorzi and at the Department of Public Health at Università degli Studi di Napoli Federico II, Italy, under the supervision of Prof M. Mariconda. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Level of evidence: Retrospective case series (level IV).
References
- 1. Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Outcome after high tibial open‐wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2013;21:170–80. [DOI] [PubMed] [Google Scholar]
- 2. Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res. 2011;469:3443–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCormack DJ, Puttock D, Godsiff SP. Medial compartment osteoarthritis of the knee: a review of surgical options. EFORT Open Rev. 2021;6:113–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bayliss LE, Culliford D, Monk AP, Glyn‐Jones S, Prieto‐Alhambra D, Judge A, et al. The effect of pa‐ tient age at intervention on risk of implant revision after total replacement of the hip or knee: a population‐based cohort study. Lancet. 2017;389:1424–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Castagnini F, Sudanese A, Bordini B, Tassinari E, Stea S, Toni A. Total knee replacement in young patients: survival and causes of revision in a registry population. J Arthroplasty. 2017;32:3368–72. [DOI] [PubMed] [Google Scholar]
- 6. Lee BS, Kim TH, Bin SI, Kim JM, Kim H. Clinicoradiologic outcomes of medial open‐wedge high‐tibial osteotomy are equivalent in bone‐on‐bone and non‐bone‐on‐bone medial osteoarthritis. Arthroscopy. 2021;37:638–44. [DOI] [PubMed] [Google Scholar]
- 7. Piovan G, Farinelli L, Screpis D, Iacono V, Povegliano L, Bonomo M, et al. Distal femoral osteotomy versus lateral unicompartmental arthroplasty for isolated lateral tibiofemoral osteoarthritis with intra‐articular and extra‐articular deformity: a propensity score‐matched analysis. Knee Surg Relat Res. 2022;18(34):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Julin J, Jämsen E, Puolakka T, Konttinen YT, Moilanen T. Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow‐up study of 32,019 total knee replacements in the Finnish arthroplasty register. Acta Orthop. 2010;81:413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kort NP, van Raay JJAM, van Horn JJ. The Oxford phase III unicompartmental knee replacement in patients less than 60 years of age. Knee Surg Sports Traumatol Arthrosc. 2007;15:356–60. [DOI] [PubMed] [Google Scholar]
- 10. Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Jt Surg Am. 2003;85:1968–73. [DOI] [PubMed] [Google Scholar]
- 11. Smith WB 2nd, Steinberg J, Scholtes S, McNamara IR. Medial compartment knee osteoarthritis: age‐stratified cost‐effectiveness of total knee arthroplasty, unicompartmental knee arthroplasty, and high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25:924–33. [DOI] [PubMed] [Google Scholar]
- 12. Tunggal JAW, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy. Int Orthop. 2010;34:255–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lobenhoffer P, Agneskirchner JD. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2003;11:132–8. [DOI] [PubMed] [Google Scholar]
- 14. Kim JH, Kim HJ, Lee DH. Survival of opening versus closing wedge high tibial osteotomy: a meta‐analysis. Sci Rep. 2017;7:7296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pascarella R, Cerbasi S, Politano R, Balato G, Fantasia R, Orabona G, et al. Surgical results and factors influencing outcome in patients with posterior wall acetabular fracture. Injury. 2017;48:1819–24. [DOI] [PubMed] [Google Scholar]
- 16. Mariconda M, Andolfi C, Cerbasi S, Servodidio V. Effect of surgical correction of adolescent idiopathic scoliosis on the quality of life: a prospective study with a minimum 5‐year follow‐up. Eur Spine J. 2016;25:3331–40. [DOI] [PubMed] [Google Scholar]
- 17. Keenan OJF, Clement ND, Nutton R, Keating JF. Older age and female gender are independent predictors of early conversion to total knee arthroplasty after high tibial osteotomy. Knee. 2019;26:207–12. [DOI] [PubMed] [Google Scholar]
- 18. Li HB, Nie S, Lan M, Tang ZM, Liao XG. The risk factors for early conversion to total knee arthroplasty after high tibial osteotomy. Comput Methods Biomech Biomed Eng. 2020;19:1–7. [DOI] [PubMed] [Google Scholar]
- 19. Primeau CA, Birmingham TB, Leitch KM, Willits KR, Litchfield RB, Fowler PJ, et al. Total knee replacement after high tibial osteotomy: time‐to‐event analysis and predictors. Can Med Assoc J. 2022;194:E428–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kellgren JH, Lawrence JS. Radiological assessment of osteo‐arthrosis. Ann Rheum Dis. 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res. 1989;246:250–9. [PubMed] [Google Scholar]
- 22. Kumagai K, Akamatsu Y, Kobayashi H, Kusayama Y, Koshino T, Saito T. Factors affecting cartilage repair after medial opening‐wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25:779–84. [DOI] [PubMed] [Google Scholar]
- 23. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Jt Surg Br. 1961;43‐B:752–7. [DOI] [PubMed] [Google Scholar]
- 24. Koshino T, Yoshida T, Ara Y, Saito I, Saito T. Fifteen to twenty‐eight years' follow‐up results of high tibial valgus osteotomy for osteoarthritic knee. Knee. 2004;11:439–44. [DOI] [PubMed] [Google Scholar]
- 25. Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H. The long‐term outcome of high tibial osteotomy: a ten‐ to 20‐year follow‐up. J Bone Jt Surg Br. 2008;90:592–6. [DOI] [PubMed] [Google Scholar]
- 26. Hui C, Salmon LJ, Kok A, Williams HA, Hockers N, van der Tempel WM, et al. Long‐term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am J Sports Med. 2011;39:64–70. [DOI] [PubMed] [Google Scholar]
- 27. Polat G, Balcı Hİ, Çakmak MF, Demirel M, Şen C, Aşık M. Long‐term results and comparison of the three different high tibial osteotomy and fixation techniques in medial compartment arthrosis. J Orthop Surg Res. 2017;12:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bouguennec N, Mergenthaler G, Gicquel T, Briand C, Nadau E, Pailhé R, et al. Medium‐term survival and clinical and radiological results in high tibial osteotomy: factors for failure and comparison with unicompartmental arthroplasty. Orthop Traumatol Surg Res. 2020;106(8 S):S223–S30. [DOI] [PubMed] [Google Scholar]
- 29. Lau LCM, Fan JCH, Chung KY, Cheung KW, Man GCW, Hung YW, et al. Satisfactory long‐term survival, functional and radiological outcomes of open‐wedge high tibial osteotomy for managing knee osteoarthritis: minimum 10‐year follow‐up study. J Orthop Transl. 2020;26:60–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kuwashima U, Iwasaki K, Kurakazu I, Akasaki Y, Nakashima Y, Itoh M, et al. Effect of osteoarthritis severity on survival and clinical outcomes after high tibial osteotomy. Knee. 2021;29:441–7. [DOI] [PubMed] [Google Scholar]
- 31. Thijssen E, van Caam A, van der Kraan PM. Obesity and osteoarthritis, more than just wear and tear: pivotal roles for inflamed adipose tissue and dyslipidaemia in obesity‐induced osteoarthritis. Rheumatology. 2015;54:588–600. [DOI] [PubMed] [Google Scholar]
- 32. Orrego M, Besa P, Orrego F, Amenabar D, Vega R, Irribarra L, et al. (2020) medial opening wedge high tibial osteotomy: more than ten years of experience with Puddu plate technique supports its indication. Int Orthop. 2020;44:2021–6. [DOI] [PubMed] [Google Scholar]
- 33. Flecher X, Parratte S, Aubaniac JM, Argenson JN. A 12‐28‐year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res. 2006;452:91–6. [DOI] [PubMed] [Google Scholar]
- 34. Martin JA, Buckwalter JA. Roles of articular cartilage aging and chondrocyte senescence in the pathogenesis of osteoarthritis. Iowa Orthop J. 2001;21:1–7. [PMC free article] [PubMed] [Google Scholar]
- 35. Kahlenberg CA, Nwachukwu BU, Hamid KS, Steinhaus ME, Williams RJ 3rd. Analysis of outcomes for high tibial osteotomies performed with cartilage restoration techniques. Arthroscopy. 2017;33:486–92. [DOI] [PubMed] [Google Scholar]
- 36. Zhang Q, Xu W, Wu K, Fu W, Yang H, Guo JJ. Intra‐articular pure platelet‐rich plasma combined with open‐wedge high tibial osteotomy improves clinical outcomes and minimal joint space width compared with high tibial osteotomy alone in knee osteoarthritis: a prospective study. Arthroscopy. 2022;38:476–85. [DOI] [PubMed] [Google Scholar]
- 37. Watanabe K, Kamiya T, Suzuki D, Otsubo H, Teramoto A, Suzuki T, et al. Biomechanical stability of open‐wedge high tibial osteotomy: comparison of two locking plates. Open J Orthop. 2014;4:257–62. [Google Scholar]
- 38. Diffo Kaze A, Maas S, Waldmann D, Zilian A, Dueck K, Pape D. Biomechanical properties of five different currently used implants for open‐wedge high tibial osteotomy. J Exp Orthop. 2015;2:14. [DOI] [PMC free article] [PubMed] [Google Scholar]


