Abstract
Objective
Although several prognostic models have been developed for patients who underwent hip fracture surgery, their preoperative performance was insufficiently validated. We aimed to verify the effectiveness of the Nottingham Hip Fracture Score (NHFS) for predicting postoperative outcomes following hip fracture surgery.
Methods
This was a single‐center and retrospective analysis. A total of 702 elderly patients with hip fractures (age ≥ 65 years old) who received treatment in our hospital from June 2020 to August 2021 were selected as the research participants. They were divided into the survival group and the death group based on their survival 30 days after surgery. The multivariate logistic regression model was used to identify the independent risk factors for the 30‐day mortality after surgery. The NHFS and American Society of Anaesthesiologists (ASA) grades were used to construct these models, and a receiver operating characteristic curve was plotted to assess their diagnostic significance. A correlation analysis was performed between NHFS and length of hospitalization and mobility 3 months after surgery.
Results
There were significant differences in the age, albumin level, NHFS, and ASA grade between both groups (p < 0.05). The length of hospitalization in the death group was longer than the survival group (p < 0.05). The perioperative blood transfusion and postoperative ICU transfer rates in the death group were higher than in the survival group (p < 0.05). The death group's incidence of pulmonary infections, urinary tract infections, cardiovascular events, pressure ulcers, stress ulcers with bleeding, and intestinal obstruction was higher than the survival group (p < 0.05). The NHFS and ASA III were independent risk factors for the 30‐day mortality after surgery, regardless of age and albumin level (p < 0.05). The area under the curve (AUC) of the NHFS and ASA grade for predicting the 30‐day mortality after surgery was 0.791 (95% confidence interval [CI] 0.709–0.873, p < 0.05) and 0.621 (95% CI 0.477–0.764, p > 0.05), respectively. The NHFS positively correlated with hospitalization length and mobility grade 3 months after surgery (p < 0.05).
Conclusion
The NHFS demonstrated a better predictive performance than the ASA score for the 30‐day mortality after surgery and positively correlated with the hospitalization length and postoperative activity limitation in elderly patients with hip fractures.
Keywords: Elderly Patients, Hip Fracture, Nottingham Hip Fracture Score, Outcomes
This study verified the performance of the NHFS in predicting the postoperative outcomes of 702 elderly patients undergoing hip fracture surgery. The NHFS had a significantly higher diagnostic accuracy than the American Society of Anesthesiologists (ASA) score for prediction of 30‐day postoperative mortality and was positively correlated with the hospitalization length and postoperative activity limitation.

Introduction
Hip fracture is one of the common fractures in the elderly. The incidence of these fractures in the elderly increases yearly as the population ages. 1 As recommended by experts, early surgical intervention should be performed for most of these cases. 2 However, such patients often suffer from various medical diseases due to advanced age and organ dysfunction, and perioperative complications occur frequently. The mortality of these patients during hospitalization is 3%–7%, and the mortality within 30 days after the occurrence of hip fractures is 3%–10%. 3 , 4 Performing a proper prediction of patients' surgical risk before surgery and accurate risk stratification and prognosis estimation may yield profound clinical significance for improving informed consent and medical safety. 3
Several mortality‐prediction tools have been developed to help identify patients at a high risk of mortality. Among these are the Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity, the Charlson Comorbidity Index, and the Nottingham Hip Fracture Score (NHFS). 5 The NHFS has shown the most promising results in predicting 30‐day mortality in hip fracture patients. 6
The NHFS is a British risk scoring system designed to predict 30‐day mortality in patients with hip fractures. It is based purely on objective parameters, including age, sex, malignancy, dementia, preoperative living status, hemoglobin levels, and predefined comorbidities. 3 The predefined comorbidities include cerebrovascular, cardiovascular, renal, and respiratory diseases. All factors included in the score are typically registered as part of admission documentation. It is calculated based on patient history upon admission, enabling its use as a screening method before the anesthetic assessment.
Although some risk models have demonstrated promising predictive performance, it is still unknown whether they are effective in clinical practice. Additionally, it is uncertain whether these risk models correlate with other indicators, such as hospitalization length and postoperative activity limitation. Most studies focused on the value of the NHFS and other methods in predicting the prognosis of postoperative mortality of hip fracture. At the same time, 7 their use in the preoperative risk assessment was seldom reported. Given this research gap, we performed this analysis to select the NHFS as a preoperative risk assessment in the elderly cohort with hip fracture. In this study, we aimed to 1) investigate the potential factors associated with the 30‐day mortality after surgery, 2) compare the predictive performance of the NHFS and ASA scores in our population, and 3) examine the correlation between the NHFS and clinical indicators.
Data and Methods
Subjects
A total of 702 elderly patients with hip fractures admitted to our hospital from June 2020 to August 2021 were selected as the subjects. Inclusion criteria: 1) patients ≥65 years old; 2) patients with hip fractures alone, including femoral neck fracture, intertrochanteric fracture, or subtrochanteric fracture; 3) patients with such fractures caused by low‐energy trauma; and 4) patients receiving surgical treatment of the hip fracture, including artificial hip replacement and intramedullary nail fixation. Exclusion criteria: 1) patients with old fractures (the duration from the onset to medical treatment > 3 weeks); and 2) patients having failed internal fixation or pathological fractures.
Patients were divided into the survival and the death groups based on their survival 30 days after surgery. The local medical research ethics committee approved the study (No. K2022‐002‐00), and the requirement of informed consents was waived due to the retrospective design.
The gender, age, body mass index, duration from onset to admission, duration from admission to surgical treatment, fracture type, and anesthesia mode of these patients were recorded before surgery.
Surgical Procedures
Intramedullary Nail Fixation Surgery
The patient was placed in the supine position under general anesthesia, and the proximal anti‐rotation intramedullary nail was applied. After abduction traction, the closed reduction was performed by adduction and internal rotation of 10° to 15° at a slow speed. The reduction effect was checked by C‐arm machine fluoroscopy (Cios Fusion, Simens Healthineers, Erlangen, Germany). The left and right incisions were made longitudinally above the greater trochanter. A guide wire was inserted into the medullary cavity through the median opening of the greater trochanter. Then, the main nail was disposed through the middle and lower 1/3 of the femoral neck. The helical blade was driven into the femoral head under the guidance of the guide device, and the C‐arm machine confirmed the ideal and locked. The distal guide needle was driven into the femoral head with a sight to check the active bleeding. After no active bleeding, the incision was rinsed repeatedly, then sutured layer by layer.
Artificial Hip Replacement
The patient was placed in a healthy lateral position with a hip joint, separating the muscles within the hip joint capsule incision as far as possible to keep the connection fracture piece of fascia tissue. The size of the rotor with steel was adjusted after reset by cutting the rotor to 1 cm in the small bone, from the femoral head to the handle of the acetabulum. The acetabular cup, which enlarges the pulp, was placed, followed by the prosthetic femoral head and handle. After implantation, the hip joint was reduced, and the joint tightness was tested. Ideally, the active bleeding was checked. After no active bleeding, the incision was rinsed repeatedly, then sutured layer by layer.
Observations of Prognostic Indicators
Indicators: 1) perioperative including surgical duration, intraoperative blood loss, length of hospitalization, perioperative blood transfusion, and postoperative intensive care unit (ICU) transfer; 2) complications during postoperative hospitalization, which include pulmonary infection, urinary system infection, cardiovascular events, new cerebral infarction, incision infection, intestinal obstruction, etc.; 3) the 30‐day mortality after surgery; 4) the mobility 3 months after surgery. Specifically, mobility can be divided into four grades, including grade 1 (patients can move around without the assistance of crutches), grade 2 (patients can conduct outdoor activities with the assistance of crutches), grade 3 (patients can conduct indoor activities and cannot conduct outdoor activities without the help of others) and grade 4 (patients cannot conduct functional activities with their lower limbs).
The NHFS values of all patients were calculated. The scoring criteria included age (≤ 65 years old, 0 points; 66–85 years old, 3 points; ≥ 86 years old, 4 points), gender (male, 1 point; female, 0 points), hemoglobin at admission (≤100 g/L, 1 point; ≥ 100 points), presence of any active malignant tumors within 20 years (yes, 1 point; no, 0 points), and the number of complications (≥2 complications, 1 point; ≤ 2 complications, 0 points).
Complications contained five chronic diseases, which can be recorded through medical history inquiry. These included cardiovascular diseases (myocardial infarction, angina pectoris, atrial fibrillation, valvular disease, and hypertension), cerebrovascular diseases (having been attacked by stroke or ischemic diseases), respiratory diseases (except for acute infection), kidney diseases, and diabetes.
Statistical Processing
The measurement data were expressed as a percentage of cases. SPSS version 26.0 software (IBM Corp., Silicon Valley, CA, USA) was adopted for data analysis. The measurement data were subjected to a normality test, with the results expressed as mean ± standard deviation. Those conditions not aligned with the normal distribution were described with median and interquartile ranges. Moreover, the Student's t‐test was conducted. The Mann–Whitney U values were calculated to find potential miscalibration. The chi‐square test or Fisher's exact test was conducted to analyze the fit of the model. Both the NHFS and ASA classifications were subjected to logistic regression analysis to predict the 30‐day mortality after surgery. Variables were not adjusted in model 1 whereas age and albumin level at admission were adjusted in model 2. Subsequently, a receiver operating characteristic curve was plotted, and the area under curve (AUC) was calculated. The AUC with the value of 0.5–0.7 indicated poor diagnostic significance, that with the value >0.7–0.9 indicated medium diagnostic significance, and that with the value >0.9 indicated high diagnostic significance. Spearman correlation analysis was used to analyze the correlation related to grade data. p < 0.05 was considered as statistically significant.
Result
General Clinical Data
There were 684 cases in the survival group and 18 in the death group. Among them, the age (median [interquartile range]: 91.00 [83.50, 93.25] vs. 80.00 [73.00, 86.00]; p < 0.001), the NHFS (5.00 [5.00, 6.00] vs. 4.00 [3.00, 5.00]; p < 0.001), and the ASA (grade 3: 11.1% vs. 1.0%; p < 0.001) grades of the death group were higher than those of the survival group, while the albumin level at admission (36.60 [34.00, 39.08] vs. 40.20 [37.80, 42.60]; p < 0.001) in the death group was lower than that in the survival group. No significant difference in other baseline data. Please refer to Table 1. The representative images are shown in Figure 1.
Table 1.
Comparison of general clinical data between two groups
| Index | Survival group (n = 684) | Death group (n = 18) | Statistical values | p value |
|---|---|---|---|---|
| Gender [n(%)] | 0.951 | 0.329 | ||
| Male | 194 (28.4%) | 7 (38.9%) | ||
| Female | 490 (71.6%) | 11 (61.1%) | ||
| Age (years) | 80.00 (73.00, 86.00) | 91.00 (83.50, 93.25) | −4.004 | <0.001 |
| BMI (kg/m2) | 22.83 (20.03, 25.39) | 24.15 (20.57, 26.17) | −0.842 | 0.400 |
| Onset to admission (h) | 19.00 (7.00, 48.00) | 21.00 (5.75, 156.00) | −0.663 | 0.507 |
| Admission to surgery (d) | 0.00 (0.00,1.00) | 1.00 (0.00,1.00) | −0.532 | 0.594 |
| Number of comorbidities | 1.00 (0.00,2.00) | 1.00 (1.00,2.00) | −0.723 | 0.470 |
| Preoperative hemoglobin (g/L) | 121.00 (109.00, 133.00) | 117.00 (106.75, 132.00) | −0.624 | 0.533 |
| Preoperative albumin (g/L) | 40.20 (37.80, 42.60) | 36.60 (34.00, 39.08) | −3.734 | <0.001 |
| Fracture type [n(%)] | 0.156 | 0.693 | ||
| Femoral neck | 386 (56.4%) | 11 (61.1%) | ||
| Intertrochanteric and Subtrochanteric | 298 (43.6%) | 7 (38.9%) | ||
| Type of anesthesia [n(%)] | — | 0.617 | ||
| Local | 646 (94.4%) | 18 (100.0%) | ||
| General | 38 (5.6%) | 0 (0.0%) | ||
| NHFS | 4.00 (3.00, 5.00) | 5.00 (5.00, 6.00) | −4.937 | <0.001 |
| ASA grade [n (%)] | 15.884 | <0.001 | ||
| I | 489 (71.5%) | 9 (50.0%) | ||
| II | 188 (27.5%) | 7 (38.9%) | ||
| III | 7 (1.0%) | 2 (11.1%) |
Note: the data were expressed as median (interquartile range) or n (frequency).
Abbreviation: BMI: body mass index; NHFS: Nottingham Hip Fracture Score; ASA: American Society of Anaesthesiologists.
Figure 1.
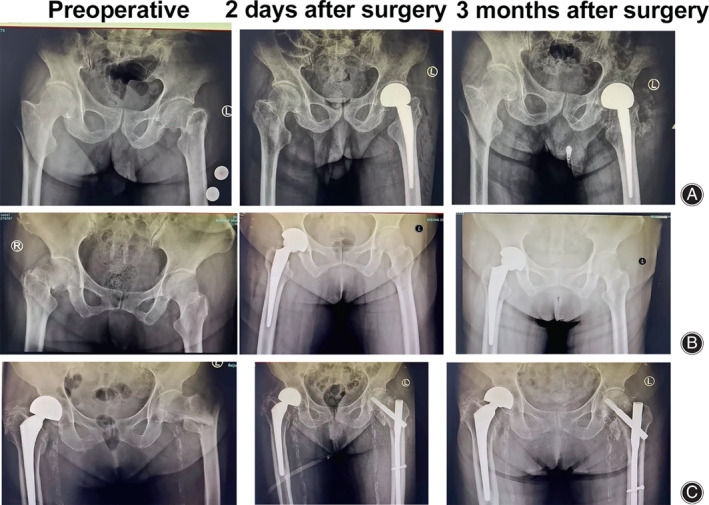
Representative images of three cases during different time points. (A) Case 1, male, 78 years old, was admitted to the hospital on August 5, 2021, with left hip pain caused by a fall for 10 days. Diagnosis: Fracture of the left femoral neck. Left artificial femoral head replacement was performed. (B) Case 2, a 76‐year‐old female, was admitted to the hospital on August 3, 2021, with right hip pain caused by a fall for one day. Diagnosis: Fracture of the right femoral neck. Right total hip replacement was performed. (C) Case 3, an 87‐year‐old female, was admitted to the hospital on August 5, 2021, with left hip pain caused by a fall injury for one day. Diagnosis: Left intertrochanteric fracture of femur. Open reduction and internal fixation with intramedullary nail were performed.
Perioperative Indicators
The length of hospitalization in the death group (6.00 [4.00, 14.75]) was longer than that in the survival group (4.00 [3.00, 5.00]) (p < 0.05); The perioperative blood transfusion rate and postoperative ICU transfer rate in the death group were higher than those in the survival group (66.7% vs. 17.5%; p < 0.05). Please refer to Table 2.
Table 2.
Comparison of perioperative indicators between two groups
| Index | Survival group (n = 684) | Death group (n = 18) | Statistical values | p value |
|---|---|---|---|---|
| Surgical duration (h) | 1.00 (1.00,1.00) | 1.00 (0.75,1.00) | −1.486 | 0.135 |
| Intraoperative blood loss (mL) | 200.00 (100.00,200.00) | 150.00 (100.00,200.00) | −0.136 | 0.891 |
| Length of hospitalization (d) | 4.00 (3.00,5.00) | 6.00 (4.00,14.75) | −3.298 | 0.001 |
| Perioperative blood transfusion [n(%)] | 9.252 | 0.002 | ||
| Yes | 253 (37.0%) | 13 (72.2%) | ||
| No | 431 (63.0%) | 5 (27.8%) | ||
| Postoperative ICU transfer [n(%)] | 27.719 | <0.001 | ||
| Yes | 120 (17.5%) | 12 (66.7%) | ||
| No | 564 (82.5%) | 6 (33.3%) |
Note: The data were expressed as median (interquartile range) or n (frequency).
Abbreviation: ICU: intensive care unit.
Comparison of Postoperative Complications Between Both Groups
Compared with the survival group, the incidence of pulmonary infection, urinary tract infection, cardiovascular events, pressure ulcers, stress ulcers with bleeding, and intestinal obstruction in the death group was higher. The difference between the two groups was statistically significant (p < 0.05 for all). Please refer to Table 3.
Table 3.
Comparison of postoperative complications between two groups
| Index [n(%)] | Survival group (n = 684) | Death group (n = 18) | Statistical values | p value |
|---|---|---|---|---|
| Pulmonary infection | 54 (7.9%) | 11 (61.1%) | 52.952 | <0.001 |
| Urinary system infection | 138 (20.2%) | 8 (44.4%) | 4.884 | 0.027 |
| Cardiovascular events | 23 (3.4%) | 6 (33.3%) | 32.571 | <0.001 |
| New cerebral infarction | 3 (0.4%) | 0 (0.0%) | — | 1.000 |
| Delirium | 12 (1.8%) | 2 (11.1%) | 3.798 | 0.051 |
| DVT | 83 (12.1%) | 3 (16.7%) | 0.046 | 0.830 |
| Pressure ulcer | 9 (1.3%) | 3 (16.7%) | 16.310 | <0.001 |
| Stress ulcer with Bleeding | 2 (0.3%) | 3 (16.7%) | — | <0.001 |
| Incision infection | 3 (0.4%) | 0 (0.0%) | — | 1.000 |
| Intestinal obstruction | 2 (0.3%) | 2 (11.1%) | — | 0.004 |
Note: the data were expressed as n (frequency).
Abbreviation: DVT: deep venous thrombosis.
Multivariate Logistic Regression Analysis of 30‐Day Death after Surgery
In terms of model 1, variables were not adjusted. The odds ratio of NHFS was 2.713 (1.698, 4.334), and that of ASA III was 15.524 (2.824, 85.332), both of which had statistical significance (p < 0.05). Regarding model 2, the age and albumin level at admission were adjusted. The odds ratio of NHFS was 2.017 (1.173, 3.470), and that of ASA III was 10.176 (1.643, 63.006), both of which had statistical significance (p < 0.05). Please refer to Table 4.
Table 4.
Multivariate logistic regression analysis of 30 days death after surgery
| Index | Model | OR (95%CI) | p value |
|---|---|---|---|
| NHFS | Model 1 | 2.713 (1.698,4.334) | <0.001 |
| Model 2 | 2.017 (1.173,3.470) | 0.011 | |
| ASA | Model 1 | ||
| I | 1.000 | ||
| II | 2.023 (0.743,5.510) | 0.168 | |
| III | 2.023 (0.743,5.510) | 0.002 | |
| Model 2 | |||
| I | 1.000 | ||
| II | 1.516 (0.54,4.244) | 0.429 | |
| III | 10.176 (1.643,63.006) | 0.013 |
Note: Model 1: variables were not adjusted; Model 2: age and albumin level at admission were adjusted.
The Diagnostic Validation of the NHFS and the ASA Grade in the 30‐Day Mortality after Surgery
The sensitivity, specificity, and AUC of the NHFS were 88.9%, 60.1%, and 0.791 (0.709, 0.873), respectively, all of which had statistical significance (p < 0.05). The sensitivity, specificity, and AUC of the ASA grade were 50.0%, 71.5%, and 0.621 (0.477, 0.764), respectively, all of which had no statistical significance (p > 0.05). Please refer to Table 5 and Figure 2. According to the data analysis, the diagnostic validity of NHFS is better than that of the ASA grade. Compared with male patients, the NHFS exhibited superior performance for predicting the occurrence of death events within 30 days after the hip surgery (Table 5).
Table 5.
The diagnostic significance of NHFS and ASA grade in the 30 days mortality after surgery
| Index | Sensitivity | Specificity | Cutoff | AUC | Lower limit | Upper limit | p value |
|---|---|---|---|---|---|---|---|
| Overall population | |||||||
| NHFS | 88.9% | 60.1% | 4.5 | 0.791 | 0.709 | 0.873 | <0.001 |
| ASA | 50.0% | 71.5% | 1.5 | 0.621 | 0.477 | 0.764 | 0.080 |
| Male | |||||||
| NHFS | 28.6% | 78.4% | 5 | 0.546 | 0.337 | 0.756 | 0.677 |
| ASA | 57.1% | 73.7% | 1 | 0.672 | 0.444 | 0.900 | 0.123 |
| Female | |||||||
| NHFS | 100.0% | 69.9% | 4 | 0.890 | 0.832 | 0.948 | <0.001 |
| ASA | 45.5% | 70.6% | 1 | 0.591 | 0.407 | 0.774 | 0.304 |
Abbreviation: AUC: area under the curve; NHFS: Nottingham Hip Fracture Score; ASA: American Society of Anaesthesiologists.
Figure 2.
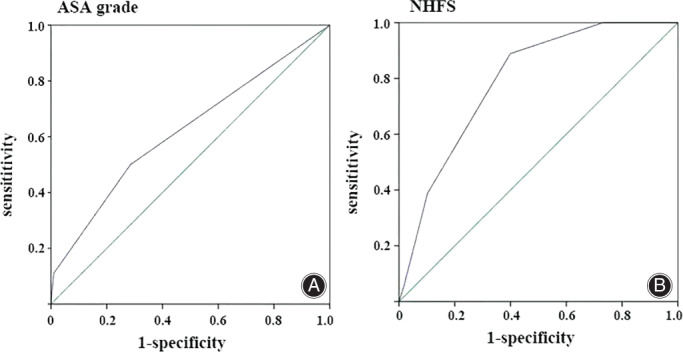
A ROC analysis of baseline ASA grade (A) and NHFS (B) in evaluating the effectiveness in the 30 days mortality after surgery.
Correlation Analysis of NHFS with the Length of Hospitalization and Mobility within 3 Months after Surgery
The NHFS was positively correlated with hospitalization length and mobility grade 3 months after surgery. The higher the NHFS, the longer the hospitalization (p = 0.001) and the worse the mobility (p < 0.001). Please refer to Table 6.
Table 6.
Correlation analysis of NHFS with length of hospitalization and mobility 3 months after surgery
| Index | Correlation coefficients | p value |
|---|---|---|
| Length of hospitalization | 0.121 | 0.001 |
| Mobility 3 months after surgery | 0.371 | <0.001 |
Abbreviation: NHFS: Nottingham Hip Fracture Score.
Discussion
Main Findings
In this study, we explored the predictive value of the NHFS and ASA for 30‐day mortality in elderly patients undergoing hip surgery. The main findings can be summarized as follows: 1) the NHFS and ASA were independent risk factors for the 30‐day prognosis of elderly patients with hip fractures, which was irrelevant to the age and albumin level; 2) the NHFS exhibited superior prognostic value over the ASA in our population; 3) the NHFS positively correlated with hospitalization length and postoperative activity limitation at the 30‐day follow‐up. The present study suggested that the NHFS might be a useful preoperative tool in assessing the 30‐day death risk after hip surgery.
Prognosis Models for Patients with Hip Fractures
Hip fracture in the elderly is a major public health problem worldwide. Currently, it is recommended to identify those patients with high risks of surgery through risk assessment. 8 The application of an appropriate and effective scoring system to conduct a surgical risk assessment could assist clinicians in judging the surgical tolerance and risk and appropriate timing for surgery based on scientific data. It can also provide prognostic judgment for patients and their family members and improve informed consent. Currently, many scholars have established a preoperative risk assessment system for patients with hip fractures. The system mainly includes the ASA grade, the physiological and operative score for the enumeration of mortality and morbidity (POSSUM), the Portsmouth physiological and operative score for the enumeration of mortality and morbidity (P‐POSSUM), the surgical outcome risk tool (SORT), the NHFS, etc. Among them, the NHFS has received extensive recognition for its predictive effectiveness, and this assessment system has been adopted most frequently in clinical practice. 7 , 9 The NHFS was proposed for predicting the prognosis after hip fractures in the elderly, which includes age, gender, hemoglobin level at admission, mini‐mental state examination, preoperative living status, malignant tumors within 20 years, and complications. 2 , 3 , 4 This scoring system can reflect the preoperative physical condition of patients, and all variables can be obtained from their medical history at admission and routine examination. It is characterized by small subjectivity, fewer items, convenient collection, and simple calculation. Therefore, the NHFS is selected as the preoperative risk assessment tool in this study.
Recent Advances in the NHFS and ASA
It has been demonstrated in multiple studies that the NHFS can accurately predict the 30‐day mortality after surgery in elderly patients with hip fractures. 2 , 6 , 10 In this study, the effectiveness of the NHFS in predicting the 30‐day mortality after surgery was independently verified to assess whether there are differences among different indexes. Univariate analysis results suggest that the death group's age, the NHFS, and ASA grades are higher than those in the survival group. In contrast, the albumin level at admission in the death group is lower than that in the survival group. The multivariate analysis results suggest that the NHFS and ASA III are independent risk factors for mortality 30 days after surgery. The serum albumin level is recognized as a serum marker of malnutrition. As is demonstrated in some studies, the preoperative serum albumin level is closely related to the poor prognosis of elderly patients with hip fractures. 11 , 12 Therefore, model 2 is supplemented in multivariate logistic regression analysis, and age and albumin level at admission are adjusted. The results confirm that the NHFS and ASA III are still independent risk factors for the 30‐day mortality after surgery in elderly patients with hip fractures. In this study, patients with an ASA IV or above were recommended conservative therapy. Holt et al. 13 maintain that a higher ASA grade is closely related to the 30‐day mortality after surgery in elderly patients with hip fractures, which is consistent with the findings of this study.
The NHFS and ASA grades are adopted as predictors to construct models, and the receiver operating characteristic curve is plotted to assess their diagnostic significance for the 30‐day mortality after surgery. This result suggests that the NHFS has favorable predictive significance for the 30‐day mortality after surgery in elderly patients with hip fractures, which is superior to the ASA grade and can be used in clinical practice. The ASA grade is also commonly used in the preoperative assessment for elderly patients with hip fractures. However, this scoring system is subjective and easily influenced by the subjectivity of observers. Meanwhile, the NHFS is characterized by simplicity, reducing clinicians' subjective judgment.
Clinical Significance of Preoperative Assessment
Identifying those patients with high risks of surgery based on the NHFS contributes to formulating perioperative treatment and nursing schemes. In this study, the incidence of pulmonary infection and other complications in the death group was significantly higher than that in the survival group. In addition, the perioperative blood transfusion rate, postoperative ICU transfer rate, and hospitalization length in the death group were significantly higher than that in the survival group. This suggests that all postoperative complications may induce delayed rehabilitation and even increase postoperative mortality. Therefore, a prospective understanding of the prognosis of patients can not only lead to efficient doctor–patient communication but also provide a foundation for the formulation of individual‐based treatment schemes. Currently, most studies are limited to the analysis of the NHFS and mortality, and few studies focus on other important prognostic indicators. In this study, the NHFS is positively correlated with hospitalization length. Previous studies have also reported that increased NHFS is closely related to prolonged hospitalization stay. 14 The NHFS contains many components that can reflect poor physical condition, including advanced age, low hemoglobin level, cognitive impairment, complications, and the demand for other people's care before surgery. 15 All the above components can affect the recovery of these patients after surgery and increase the risk of complications. The postoperative complications could significantly influence the length of hospitalization. 16 Prolonged hospitalization would consume more medical resources and aggravate the economic burden on the family. Therefore, when performing a clinical assessment for a population with high risks of surgery, it is necessary to consider the balance between resource optimization and risk cognition.
In the present study, there was a relatively low mortality rate of hip fracture in the elderly within 30 days, while this rate was reported as 3%–10% in published literature. 3 , 4 There might be several reasons for this phenomenon. First, the included patients were milder in severity and had fewer comorbidities. We excluded those elderly patients who had old fractures, failed internal fixation, and pathological fractures. In addition, regional, ethnic, and hospital‐specific factors contribute to this disparity in mortality. Short‐term patient data, such as a 30‐day period, are susceptible to multiple factors from study design and execution.
In addition to the mortality and complications, daily mobility shall be incorporated into the prognosis assessment of hip fractures. It has been reported that the living ability of patients with hip fractures would decrease to a certain extent after surgery, and less than a third of patients can recover to the pre‐fracture state 1 year after surgery. 17 The analysis of Doherty et al. 18 found that the NHFS has a favorable performance profile in predicting the months following surgery. It can be found that the higher the NHFS, the worse the mobility. There is degraded tissue repair ability and body compensation ability for elderly patients. Further, these patients are often comorbid with many underlying diseases, thus more prone to induce complications after surgery, which is not conducive to their recovery. 19 , 20 Those patients with dementia or in need of other people's care before admission may be in worse physical condition and have decreased mobility to varying degrees. All these factors may affect fracture healing and functional recovery.
Limitations and Strengths
This study still has some limitations. It is a single‐center retrospective analysis, which may encompass selection bias and overlook some clinically significant data. Another limitation is that the sample size is too small. The sample size in most related studies is more than 1000 cases. Therefore, a multi‐center, large sample, and strictly designed clinical study is required for further exploration. The strength of this study was to demonstrate the superiority of NHFS versus the ASA in assessing the risk of 30‐day death in elderly patients undergoing hip surgery and identify the positive correlation of NHFS with hospitalization length and 30‐day limited activity after the surgery. These findings could be translated into the optimization of decision‐making and potential benefit in clinical outcomes.
Conclusion
The NHFS presents a favorable predictive significance for elderly patients with hip fractures for the 30‐day mortality after surgery. It exhibits a better performance than the ASA grade. Moreover, the NHFS is positively correlated with hospitalization length and postoperative activity limitation. Since the NHFS is characterized by simple calculation and higher objectivity and accuracy, it can be used as a screening tool at admission to guide clinicians to facilitate the perioperative decision‐making process. Individual‐based risk assessment and prognosis determination have considerable clinical significance for both improving the informed consent of patients and their family members and enhancing medical safety. Moreover, it is required to strengthen the monitoring of the population with high risks of surgery and actively prevent and cope with complications, which would contribute to prognosis improvement.
Ethics Statement
This study was conducted after garnering the informed consent of subjects and approved by the Ethics Committee of this hospital.
Conflict of Interest
The authors report no conflicts of interest in this work.
Funding Information
Beijing Hospitals Authority Youth Programme (code: QML20210405).
Authors' Contributions
Conception and design of the research: Zhao B, Sun LL. Acquisition of data: Sun LL, Liu ZW. Analysis and interpretation of the data: Sun LL, Wu H, Liu BC. Statistical analysis: Sun LL, Liu ZW, Wu H, Liu BC. Obtaining financing: None. Writing of the manuscript: Sun LL, Zhao B. Critical revision of the manuscript for intellectual content: Zhao B.
Acknowledgements
N/A.
Data Availability Statement
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1. Wolf O, Mukka S, Ekelund J, Möller M, Hailer NP. How deadly is a fracture distal to the hip in the elderly? An observational cohort study of 11,799 femoral fractures in the Swedish Fracture Register. Acta Orthop. 2021;92:40–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tilkeridis K, Ververidis A, Kiziridis G, Kotzamitelos D, Galiatsatos D, Mavropoulos R, et al. Validity of Nottingham hip fracture score in different health systems and a new modified version validated to the Greek population. Med Sci Monit. 2018;24:7665–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Van Rijckevorsel VAJIM, Roukema GR, Klem TMAL, Kuijper TM, de Jong L, Dutch Hip Fracture Registry Collaboration . Validation of the Nottingham hip fracture score (NHFS) in patients with hip fracture: a prospective cohort study in the Netherlands. Clin Interv Aging. 2021;16:1555–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. De Jong L, Mal Klem T, Kuijper TM, Roukema GR. Validation of the Nottingham hip fracture score (NHFS) to predict 30‐day mortality in patients with an intracapsular hip fracture. Orthop Traumatol Surg Res. 2019;10:485–9. [DOI] [PubMed] [Google Scholar]
- 5. Jonsson MH, Bentzer P, Turkiewicz A, Hommel A. Accuracy of the physiological and operative severity score for the enUmeration of mortality and morbidity score and the Nottingham risk score in hip fracture patients in Sweden ‐ a prospective observational study. Acta Anaesthesiol Scand. 2018;62:1057–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Karres J, Heesakkers NA, Ultee JM, Vrouenraets BC. Predicting 30‐day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury. 2015;46:371–7. [DOI] [PubMed] [Google Scholar]
- 7. Pallardo Rodil B, Gómez Pavón J, Menéndez MP. Hip fracture mortality: predictive models. Med Clin (Barc). 2020;154:221–31. [DOI] [PubMed] [Google Scholar]
- 8. Dreinhöfer K. Hip fracture in the elderly: time to act. Dtsch Arztebl Int. 2020;117:51–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nelson MJ, Scott J, Sivalingam P. Evaluation of Nottingham hip fracture score, age‐adjusted Charlson comorbidity index and the physiological and operative severity score for the enumeration of mortality and morbidity as predictors of mortality in elderly neck of femur fracture patients. SAGE Open Med. 2020;8:2050312120918268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marufu TC, White SM, Griffiths R, Moonesinghe SR, Moppett IK. Prediction of 30‐day mortality after hip fracture surgery by the Nottingham hip fracture score and the surgical outcome risk tool. Anaesthesia. 2016;71:515–21. [DOI] [PubMed] [Google Scholar]
- 11. Bohl DD, Shen MR, Hannon CP, Fillingham YA, Darrith B, Della Valle CJ. Serum albumin predicts survival and postoperative course following surgery for geriatric hip fracture. J Bone Joint Surg Am. 2017;99:2110–8. [DOI] [PubMed] [Google Scholar]
- 12. Shi H, Na Q, Zhang X, Jiang X. Correlations between the levels of acute infection markers and serum albumin in elderly patients with hip fracture. Aging Clin Exp Res. 2017;29:435–41. [DOI] [PubMed] [Google Scholar]
- 13. Holt G, Smith R, Duncan K, Hutchison JD, Gregori A. Outcome after surgery for the treatment of hip fracture in the extremely elderly. J Bone Joint Surg Am. 2008;90:1899–905. [DOI] [PubMed] [Google Scholar]
- 14. Lisk R, Yeong K, Fluck D, Fry CH, Han TS. The ability of the Nottingham hip fracture score to predict mobility, length of stay and mortality in hospital, and discharge destination in patients admitted with a hip fracture. Calcif Tissue Int. 2020;107:319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Archunan MW, Subhash S, Attwood J, et al. Nottingham hip fracture score: does it predict mortality in distal femoral fracture patients? Cureus. 2021;13:e19139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Van den Belt L, van Essen P, Heesterbeek PJ, Defoort KC. Predictive factors of length of hospital stay after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23:1856–62. [DOI] [PubMed] [Google Scholar]
- 17. Pfeufer D, Grabmann C, Mehaffey S, Keppler A, Böcker W, Kammerlander C, et al. Weight bearing in patients with femoral neck fractures compared to pertrochanteric fractures: a postoperative gait analysis. Injury. 2019;50:1324–8. [DOI] [PubMed] [Google Scholar]
- 18. Doherty WJ, Stubbs TA, Chaplin A, et al. Prediction of postoperative outcomes following hip fracture surgery: independent validation and recalibration of the Nottingham hip fracture score. J Am Med Dir Assoc. 2021;22:663–669.e662. [DOI] [PubMed] [Google Scholar]
- 19. Hickson LJ, Farah WH, Johnson RL, Thorsteinsdottir B, Ubl DS, Yuan BJ, et al. Death and postoperative complications after hip fracture repair: dialysis effect. Kidney Int Rep. 2018;3:1294–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Malik AT, Quatman CE, Phieffer LS, Ly TV, Wiseman J, Khan SN. The impact of metabolic syndrome on 30‐day outcomes in geriatric hip fracture surgeries. Eur J Orthop Surg Traumatol. 2019;29:427–33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.


