Abstract
Objective
Strong tendon grasping is vital to the success of a tenodesis operation. The purpose of this study was to evaluate the initial tendon‐fixation strength of the Lark‐Loop technique in arthroscopic suprapectoral biceps tenodesis and compare it with others commonly used techniques.
Methods
Thirty‐three porcine superficial flexor digitorum tendons were harvested from a local slaughterhouse and randomly divided into three groups to perform three tendon fixation techniques (Lasso‐Loop stich group, Lark‐Loop stich group or Krackow stich group; 11 tendons each group) with a No. 2 suture, respectively. Each tendon was pre‐tensioned in 5°N for 2 min and then cyclically loaded 5 to 30°N for 500 cycles to assess displacement. After cyclic loading, the tendon was loaded to ultimate tendon‐suture configuration failure at the rate of 1 mm/s. Finally, the mode of failure and the construct stiffness of the tendon were recorded and calculated.
Results
After cyclical loading, the displacement of the Lark‐Loop group was equivalent to the Krakow group (P > 0.9999) but significantly smaller than the Lasso‐Loop group (P = 0.0009). The ultimate load to failure for the Lark‐Loop was equivalent to the Krakow technique group (P = 0.1463) but significantly greater than the Lasso‐Loop group (P < 0.0001). The stiffness for the Lark‐Loop was equivalent to the Krakow group (P = 0.4718) but significantly greater than the Lasso‐Loop technique group (P < 0.0001). In the Lark‐Loop and Krackow group, all the tendons failed by suture breakage, while all the tendons failed by suture cutting through the tendon in the Lasso‐Loop technique group.
Conclusion
Lark‐Loop suture technique has biomechanical properties comparable to Krackow and superior to the Lasso‐Loop in terms of suture displacement, ultimate load to failure, and stiffness. Therefore, the Lark‐Loop suture fixation technique may be beneficial for arthroscopic biceps tenodesis.
Keywords: Arthroscopic, Biomechanics, Krackow, Lark‐Loop, Lasso‐Loop, Suprapectoral tenodesis
A safe tendon fixation is essential for the success of biceps tenodesis. Many fixation techniques used for arthroscopic suprapectoral biceps tenodesis can cause longitudinal splitting of the tendon, leading to failure of the construction and the tenodesis. This paper is to evaluate the initial tendon‐fixation strength of the Lark‐Loop technique in arthroscopic suprapectoral biceps tenodesis and compare it with other commonly used techniques. After a biomechanical test, we found that the Lark‐Loop suture fixation technique has biomechanical properties comparable to Krackow and superior to the Lasso‐Loop in terms of suture displacement, ultimate load to failure, and stiffness. Therefore, the Lark‐Loop suture fixation technique may be beneficial for arthroscopic biceps tenodesis.

Introduction
Lesions of the long head tendon of the biceps brachii (LHBT) are the common cause of anterior shoulder pain and flexion dysfunction, which seriously affecting patients' quality of life. 1 Surgical treatment is often required for LHBT lesions with conservative treatment failure. Among them, LHBT tenotomy and tenodesis are the common surgical treatment methods. 2 Tenotomy has the advantage of early functional exercise without immobilization, but there are complications of upper arm Popeye deformity (incidence rate of 10% to 58%). 3 Tenodesis can restore the anatomical length‐tension relationship of the biceps muscle, maintain its normal contour, and effectively reduce the incidence of complications such as upper arm Popeye deformity. 4
For LHBT tenodesis, due to the lack of consensus on the specific tenodesis methods, various research focused on the continuous improvement and development of existing tenodesis methods to obtain better biomechanical properties. As a result, many techniques have been introduced clinically, including open, mini‐open, and arthroscopic patterns. 5 , 6 , 7 Arthroscopic suprapectoral tenodesis at intertubercular groove tenodesis does not require additional surgical incisions, with less interference to the muscles and a similar postoperative pain relief effect compared to open surgery. Therefore, it is widely accepted by doctors and patients. 8 , 9 However, compared with open tenodesis, the upper arm Popeye deformity incidence is still higher with arthroscopic tenodesis. 10
In arthroscopic biceps tenodesis, the choice of suture technique is limited due to the space constraint in the joint. The simple stitch technique and the Lasso Loop technique with stronger tissue grasping ability are commonly utilized. 11 The Lasso‐Loop suture, designed by Lafosse et al. 12 in 2006, aims to improve tissue grip. Patzer et al 11 had proved that the Lasso‐Loop techniques achieved strong and secure tenodesis, which was equivalent to interference screws in LHBT tenodesis. But Kaback et al. 13 found that compared to the Krackow suture technique in human cadaveric LHBT tenodesis, the Lasso‐loop suture technique had showed significantly worse mean failure load and mean stiffness values. In addition, this suture technique cannot prevent longitudinally sawing tendons, which may eventually result in suture pull‐out and tenodesis failure and may be one of the main reasons for the still high incidence of upper arm Popeye deformity. 14 Although the classic Krackow suture technique shows superior biomechanical properties for biceps tendon fixation, it is not easy to complete under arthroscopy. 15 Therefore, secure tendon grasping ability of the suture techniques is critical for successful arthroscopic tenodesis in order to obtain a lower incidence of Popeye deformity of the upper arm with endoscopic fixation. The Lark‐Loop stitch, newly presented in 2022 by Zhou et al. 16 constructs a Lark's head knot, holding tendon tissue with the two suture ends piercing through the middle portion of the tendon. When tension is applied to the ends of the two suture, the Lark's head knot self‐tightening provides good tendon grip. In the meantime, the knot acts as a rip‐stop effect, restricting the suture sawing tendon and overcoming the failure of tenodesis. This suture structure is fully arthroscopically operable and tear‐resistant, allowing quick, easy, and safe tendon grasping. It is now used in arthroscopic proximal long‐head tenodesis. However, the biomechanical properties of the Lark‐Loop techniques need further study.
The purpose of this study was to compare the displacement, ultimate load to failure, and stiffness between the Lark‐Loop technique and other common tendon suture techniques (including Krackow and Lasso‐Loop). Since the tendon‐suture interface is the weak link in tenodesis using anchors, it was hypothesized that the Lark‐Loop suture technique would provide better biomechanical results in terms of tendon‐suture fixation strength compared to the Lasso‐Loop suture technique. The study found that the elongation between the three groups (Lasso‐Loop, Lark‐Loop and Krackow) was no different.
Methods
Porcine superficial digital flexor tendons were chosen in this laboratory study, as these tendons were similar to human LHB in anatomic appearance and biomechanical properties. In addition, the superficial digital flexor tendons with a wide range of sources were considered an ideal substitute for limited cadaveric specimen resources. 14 , 17 All tendons were harvested from the forehoof of 6‐month‐old pigs after slaughtering in a local slaughterhouse. Since all the selected tendons for this study were harvested from porcine used for meat production instead research purposes, no animal ethics approval was required. The flow chart of the study and the parameters to be tested are described in Fig. 1. All the tendon specimens were harvested and isolated from 6‐ to 9‐month‐old pigs within an hour after slaughtering and were directly frozen at −20°C.
Fig. 1.
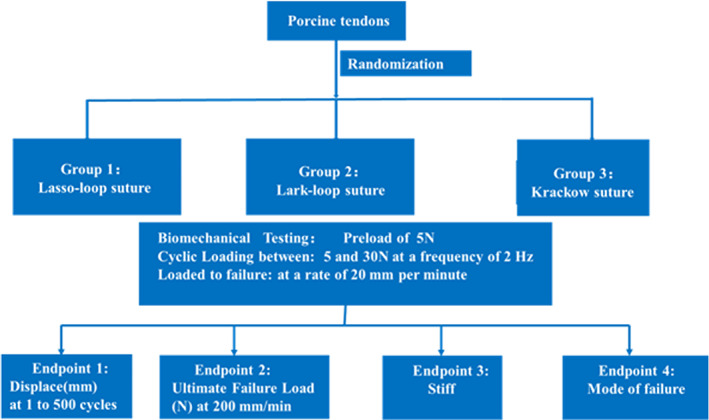
Study flow chart depicting the testing.
In total, 33 fresh frozen porcine superficial flexor tendons were randomly assigned to three groups (n = 11): Lasso‐Loop, n = 11, Lark‐Loop, n = 11, Krackow, n = 11. The tendons were stored at −20°C and thawed to room temperature 24 h in advance before the beginning of the experiment. Saline solution (0.9%) was periodically sprayed onto the surface of tendons to maintain moisture during preparation and testing. None of the tendons had degenerative or pathological changes.
Surgical Techniques
The 11 tendons in the Lasso‐Loop group were sutured with No. 2 FiberWire suture (Arthrex, Naples, FL, USA) according to the protocol of Lafosse et al. 12 the midportion of the No. 2 FiberWire suture is not completely passed through the tendon at the 1 cm from the distal end of the tendon. Then one end of the suture is passed back and threaded through the loop, hereby creating the Lasso‐Loop construct (Fig. 2A).
Fig. 2.
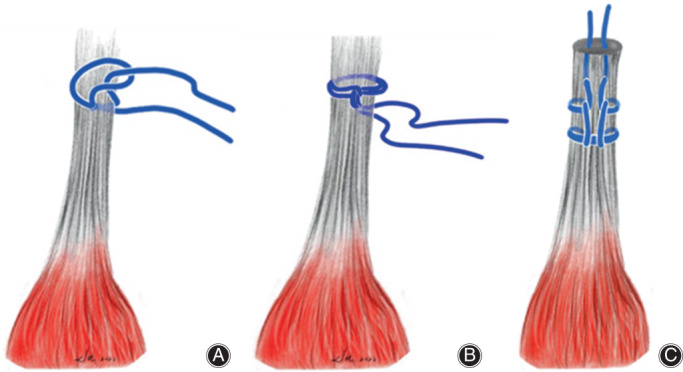
Illustration of Lasso‐Loop suture technique (A), Lark‐Loop suture technique (B) and Krakow suture technique (C).
Eleven tendons in the Lark‐Loop group were sutured with No. 2 FiberWire according to the protocol of Zhou et al. 16 First, the No. 2 FiberWire suture was folded in half to encircle the tendon, with the two suture strands threaded into the loop to construct a Lark's Head Knot 1 cm from the distal end of the tendon. Then a needle with the No. 2 FiberWire pierced through the mid‐center of the tendon, as a guiding suture. The piercing point is close to the Lark's Head Knot but on the side distal to the tendon stump. Subsequently, an overhand knot was tied tightly over the two suture strands of the Lark's Head Knot with the guiding suture, and the guiding suture was pulled out of the tendon to shuttle the two free strands of the Lark's Head Knot through the tendon. The Lark‐Loop construct was formed after removing the guiding suture and tensioning the working suture to remove excess suture within the tendon (Fig. 2B).
Eleven tendons in the Krackow group were sutured with No. 2 FiberWire suture according to the protocol of Deramo et al. 18 The first Krackow stitch was placed at 1 cm from the distal end of the tendon with two locking loops. The needle pitches were evenly maintained at 0.5 cm (Fig. 2C).
All the suture constructs were operated by the same experienced orthopedic surgeon for each tendon (Fig. 3).
Fig. 3.
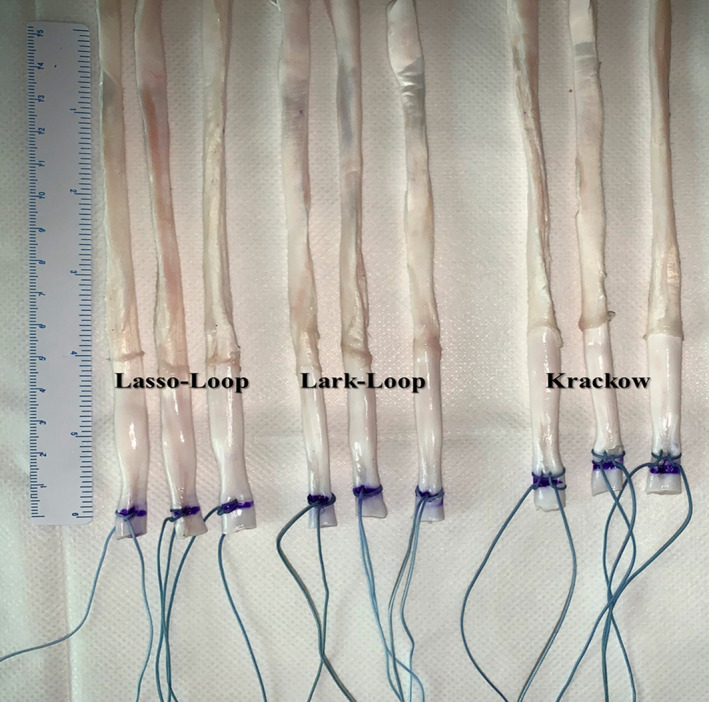
The suture techniques that we tested. From left to right: Lasso‐Loop suture technique; Lark‐Loop suture technique; Krakow suture technique.
Biomechanical Testing
The BOSE testing machine (ElectroForce 3500; Bose Corporation, ElectroForce Systems Group, Eden Prairie, MN, USA) was used to perform biomechanical testing (Fig. 4). First, each tendon was fixed at the sinusoid clamp and maintained at an equal 3 cm in length of the free tendon. Then, the two strands of the suture end were looped with 6‐throw square knots over the post of the adapter of the testing machine.
Fig. 4.
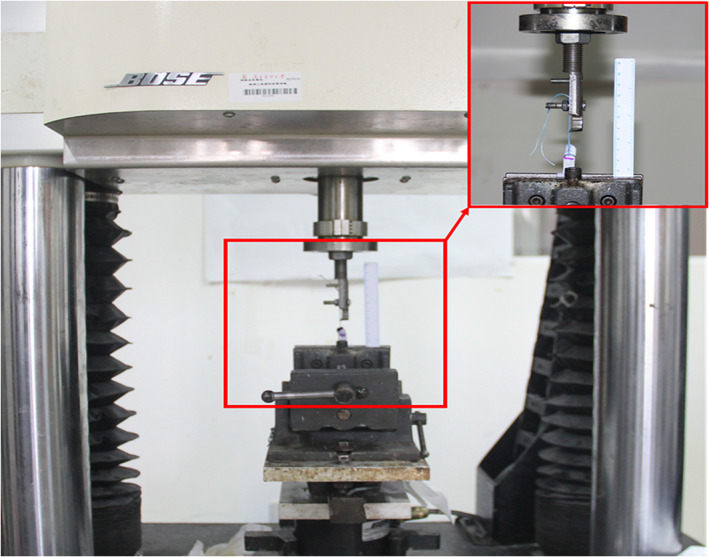
Test setting in the BOSE machine. The specimen was fixed in a custom‐made steel clip and the suture ends were knotted tightly on the corresponding clip, which allowed tensile loading to be performed along the long axis of the tendon in the testing machine. Test setting with Tendon and Lark‐Loop stitch, red box: magnification of suture construct and scales.
The tendon was pre‐loaded in tension with 5 N for 2 min. A purple dot was marked on each suture at the point where it pierced the tendon ends, as the maker indicated the displacement in pre‐tension and cyclical loading. The tendons were then cyclically loaded with tension from 5 to 30 N for 500 cycles at 2 Hz. 19 Elongation of the suture after cyclical loading was defined as the displacement in the distance between the purple marker after pre‐tension and cyclical loading, measured with an 8.9‐megapixel digital camera (EOS 60D; Canon, Tokyo, Japan). Displacement of the suture after cyclical loading was defined as the displacement in the distance between the purple marker after pre‐tension and cyclical loading, measured with image analysis software (ImageJ software, version 1.53j; National Institutes of Health, Bethesda, MD, USA). 14
After cyclical loading, all the tendons were loaded to failure at the rate of 1 mm/s. The ultimate failure load was defined as the maximum tensile force, and the failure types were also recorded (suture breakage, tendon rupture, and suture cutting through the tendon). Finally, the stiffness for each tendon‐suture construction is calculated in the linear region of the load–displacement curve.
Statistical Analysis
The sample size was estimated using a sample size analysis software, PASS 15 (NCSS, LLC. Kaysville, UT, USA), based on our preliminary experiment results regarding the displacement of the suture. In this initial experiment, nine tendons were randomly allocated to three groups (Lasso‐Loop 2.78 ± 0.52 mm, Lark‐Loop 2.10 ± 0.43 mm, Krackow 2.09 ± 0.41). The α and power (1‐β) were set as 0.05 and 0.80, respectively. Considering the possible specimen's loss during testing, 10% more samples were added in each group. Finally, the sample size of 11 specimens in each group and 33 in total was required.
Statistics analysis was conducted with SPSS Statistics for Windows, Version 25.0 (IBM Corp, Armonk, NY, USA). All the continuous outcomes were presented as mean ± standard deviation. The Kruskal‐Wallis test was used to compare the displacement, ultimate load to failure, and the stiffness. Statistical significance was set at a level of P < 0.05. Then, post hoc analysis with Mann–Whitney U‐test test with a Bonferroni correction was conducted for multiple comparisons between each suture group.
Result
Displacement
There were significant differences in displacement among the Lark‐Loop group (2.00 ± 0.50), Krakow group (1.95 ± 0.42 mm), and Lasso‐Loop group (2.91 ± 0.63 mm) (P = 0.0002). Furthermore, post hoc analysis after Bonferroni correction showed that there was no statistical difference between the Lark‐Loop group and the Krackow group (MD = 0.05, 95%CI: −0.52 to 0.61, P > 0.9999), but both were significantly less than the Lasso‐Loop group [(MD = 0.91, 95%CI: 0.35 to 1.47, P = 0.0009), (MD = 0.95, 95%CI: 0.39 to 1.5, P = 0.0005)] (Fig. 5A).
Fig. 5.
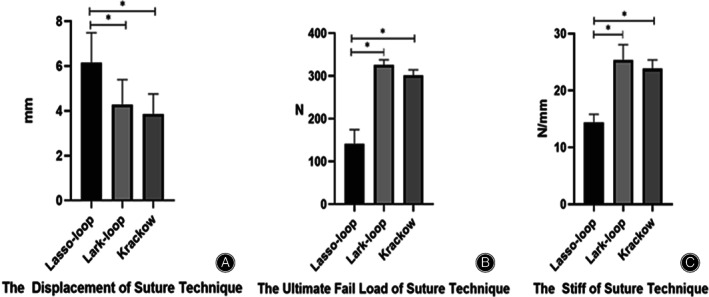
Displacement, ultimate load to failure, and stiffness (*, P < 0.05). After cyclic loading significant less displacement, a higher load to failure and stiffness was found in the Lark‐Loop suture technique group and Krakow suture technique group.
Ultimate Load to Failure
There were significant differences in ultimate load to failure among the Lark‐Loop group (325.89 ± 12.01°N), Krakow group (301.51 ± 13.17°N), and Lasso‐Loop group (141.51 ± 33.02°N) (P < 0.0001). Furthermore, post hoc analysis after Bonferroni correction showed that there was no statistical difference between the Lark‐Loop group and the Krackow group (MD = 24.47, 95%CI: −6.084 to 55.03, P = 0.1463), but both were significantly greater than the Lasso‐Loop group [(MD = −184.5, 95%CI: −215.0 to −153.9, p < 0.0001), (MD = −160.0, 95%CI: −190.6 to −129.4, P < 0.0001)] (Fig. 5B).
Stiffness
There were significant differences in stiffness among the Lark‐Loop group (25.39 ± 2.68°N/mm), Krakow group (23.82 ± 1.67°N/mm), and Lasso‐Loop group (14.34 ± 1.49°N/mm) (P < 0.0001). Furthermore, post hoc analysis after Bonferroni correction showed that there was no statistical difference between the Lark‐Loop group and the Krackow group (MD = 1.571, 95%CI: −1.238 to 4.379, P = 0.4718), but both were significantly greater than the Lasso‐Loop group [(MD = −11.05, 95%CI: −13.86 to −8.24, P < 0.0001), (MD = −9.477, 95%CI: −12.29 to −6.67, P < 0.0001)] (Fig. 5C).
Failure Mode
In the Lark‐loop and Krackow group, all the tendons failed by suture breakage, while all the tendons failed by suture cutting through the tendon in the Lasso‐Loop group (Fig. 6).
Fig. 6.
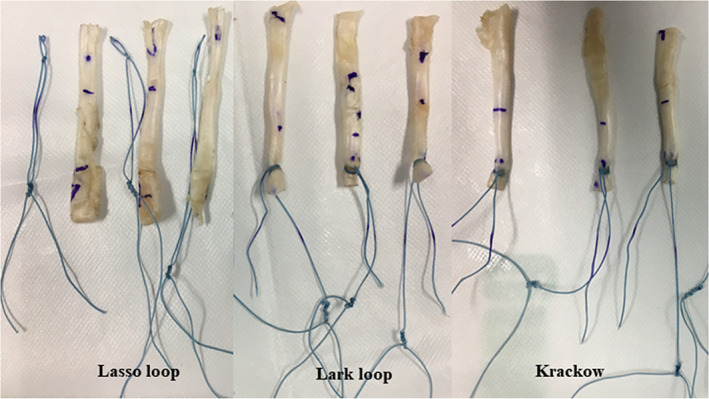
Mode of suture construct failure. The sutures were almost cut out from the tendons in Lasso‐Loop suture technique group; however, the sutures were broken in the Lark‐Loop suture technique group and Krakow suture technique group.
Discussion
In this study, the Lark‐Loop suture technique resulted in a statistically equivalent biomechanical profile to the Krackow suture technique, and a statistically superior biomechanical profile to the Lasso‐Loop suture technique. Compared with Lasso‐Loop technique, the Lark‐Loop technique demonstrated lesser displacement, stronger ultimate load to failure and, bigger stiff. This result indicates that the Lark‐Loop has comparable mechanical properties to the Krackow suture technique. However, the Krackow suture not only requires the surgeon to suture the tendon externally but also to puncture the tendon multiple times, which inevitably increases the operative time. On the contrary, Lark‐Loop tenodesis has identical advantages to Lasso‐Loop in that tenodesis can be done thoroughly by arthroscopy and requires only once piercing of the tendon.
All‐Arthroscopic Suprapectoral Biceps Tenodesis
Although some scholars believe that open subpectoral LHBT tenodesis is more reliable in treating LHBT lesions, more studies have shown that there were no significant differences in postoperative pain and function restoration between arthroscopy and open treatment. 20 , 21 Because arthroscopic surgery avoids additional incisions and deltoid dissection, it is widely welcomed by doctors and patients. In the last 10–15 years, all‐arthroscopic LHBT tenodesis has become the mainstream surgical approach for treating symptomatic LHBT lesions. 9 , 22 The Lasso‐Loop suture technique has a reliable clinical outcome and is currently the commonly used arthroscopic onlay tenodesis technique for LHBT tenodesis in the intertubercular groove. 23 , 24 , 25 , 26 Although the Lasso‐Loop suture technique is easy to operate under the arthroscope with a strong tissue grasping ability, according to recent biomechanical studies, the Lasso‐Loop suture technique shows biomechanical defects of uneven suture tendon load distribution. 12 , 15 At the same time, the suture can easily cut the tendon and causes fixation failure, resulting in inferior biomechanical results compared with other techniques. 14 Muller et al. have recently modified the Lasso‐Loop, although its maximum load, displacement, and stiffness have been improved to some extent. Still, most of the tendon‐suture constructs failed at suture cutting through the tendon, indicating that the safety of this fixation technique is still insufficient. 14 In this study, the biomechanical of Lasso‐Loop suture technique had also been researched. The maximum failure load and failure mode of it were consistent with their results above‐mentioned (about 150°N, longitudinal tendon cutting). Therefore, the insecurity of the Lasso‐Loop suture technique in biceps onlay tenodesis had been proved again.
Displacement, Ultimate Load to Failure and Stiffness in Different Studies
Displacement as a parameter of primary tenodesis stability has been evaluated by many researchers. The displacement of Lasso‐loop technique was 2.91 ± 0.63 mm in this study. It was higher compared to published literatures, the displacement of a range between 0.7 and 2.6 mm for Lasso‐Loop stitch biceps tenodesis has been reported. 27 , 28 , 29 However, the cyclic loading in these studies was 20 or 100 cycles. But in our study, the tendons were cyclically loaded for 500 cycles (currently recognized), before to be loaded to failure, which maybe one of reasons for higher displacement. Another reason to account for this situation may be due to different loads applied (5–20°N, Ponce et al.28; 5–50°N, Patzer et al. 29 ). Lower cyclic load also can obtain lower displacement. Although the displacement of the Lasso‐loop suture technique varies from study to study. But in this study, we can find that the displacement of Lasso‐loop suture technique was significantly higher than that of Lark‐Loop and Krackow suture techniques.
According to research, it takes an average of about 112 N to flex the elbow to 90° while holding a 1 kg weight. 30 Therefore, a tendon‐suture fixation is considered reliable when the ultimate load to failure is over 112°N. Theoretically, although the ultimate load to failure of the Lasso‐Loop suture techniques is inferior to the Lark‐Loop and the Krackow, Lasso‐Loop is still considered to provide relatively secure strength to maintain daily activities at zero. 11 , 28 However, in the follow‐up of LHBT tenodesis with Lasso‐Loop, it was found that the incidence of Popeye's sign was still high. 31 This shows that the daily load of the elbow flexion is far more than 1 kg, which requires a larger failure load to resist the force before the tendon‐to‐bone biological heal. The ultimate load to failure of the Lark‐Loop stitch is as high as 325 N, which is much better than that of the Lasso‐Loop. This is due to the Lark‐Loop stitch holding tendon tissue with the two suture ends piercing through the middle portion of the tendon. When tension is applied to the ends of the two sutures, the Lark‐Loop stitch self‐tightening provides good tendon grip. Therefore, we have reason to believe that this simple Lark‐Loop suture technique would be a safe and good choice for arthroscopic fixation of the long head of the biceps tendon.
Similarly, the stiffness of the Lasso‐Loop can be found in many literatures, however, values vary widely. Kaback et a.l 13 reported stiffness values of only 4.5°N/mm for the Lasso‐Loop stitch while Müller et al. 14 showed values of 13.1°N/mm for the Lasso‐Loop technique. The modified Lasso‐Loop stitch, 360Lasso‐Loop, had been modified to increase the stiffness of Lasso‐Loop technique. 14 After modifying, the stiffness value of Lasso‐Loop is increased to a certain extent (19.1°N/mm). In this study, the stiffness of Lark‐Loop suture technique also achieves a great improvement, and showed significant higher than of the Lasso‐Loop (25.39 ± 2.68°N/mm, 14.34 ± 1.49°N/mm).
The Sutures in the Lark‐Loop and Krackow Techniques
The Krackow suture is one of traditional methods to repair tendons. In order to determine whether the Lark‐Loop technique has similar biomechanical properties to the Krackow technique, the difference between the Lark‐Loop and Krackow techniques has also been compared. The data from this study showed the Lark‐Loop suture technique achieved biomechanical properties similar to the Krackow suture technique (displacement, ultimate load to failure and stiffness). Some may question that our Krackow stitching method is not the same as the classic Krackow method. Because the Krackow stitching technique here uses one suture with two locking loops on each side, while the classic one is one suture with three locking loops. However, as previously demonstrated, in the case of the Krackow technique with one suture, whether it is two locking loops, four locking loops or six locking loops, the maximum failure load does not change significantly. 32 According to the experience of many experienced clinicians, the more the tendon is sutured, the more the damage to the tendon, the more locking loops in the tendon, the greater the impact on the suture elongation, and ultimately leads to the failure of tendon‐bone fixation. 33 Therefore, we believe that Lark‐Loop technique has similar biomechanical properties to the classic Krackow technique.
Limitations and Strengths
Although the superior mechanical properties of the Lark Loop suture technique have been proven in vitro with porcine superficial flexor tendons in this study, there are some limitations to our experiments. First, due to the problematic source of cadavers, all the experiment subjects of our biomechanical tests were based on the model of the porcine superficial flexor tendons. Therefore, the porcine tendons are not fully representative of human tendons, and the mechanical results of this study should be interpreted with caution. However, several studies have also performed biomechanical testing using the porcine flexor digitorum superficialis tendon because it exhibits similar anatomical and biomechanical properties to the human biceps long head tendon. Second, the mechanical results at zero‐time in vitro cannot accurately represent the mechanical changes in the tendon‐to‐bone healing process under physiological conditions in vivo. Relevant animal research has been currently in progress to further verify the safety and superiority of this technology before promotion. Finally, this biomechanical study only analyzes the suture structure of suture and tendon, but does not combine with anchor under arthroscopy. In order to analyze this structure more accurately, it may be necessary to further study the combination of anchor fixation and related suture techniques.
Conclusion
The Lark‐Loop suture technique has better biomechanical properties in terms of tendon‐suture‐interface like the Krackow suture, and the Lark‐Loop suture technique has the same characteristics as the Lasso‐Loop suture technique, which is easy to operate under all arthroscopy. Therefore, this technique may be beneficial for arthroscopic fixation of the long head of the biceps tendon.
Author Contributions
Min Zhou, Chuanhai Zhou and Dedong Cui designed the study and contributed to writing of the draft. Yi Long and Yan Yan contributed to data analysis and solved technical problems in software. Zhenze Zheng and Ke Meng contributed to data collection. Jinming Zhang participated in data extraction and analysis assistance. Jingyi Hou and Rui Yang participated in the design of this research and provided guidance and troubleshooting. All authors agree to be accountable for all aspects of the work. All authors read and approved the final manuscript. All authors contributed to the article and approved the submitted version.
Funding Information
This work was supported by the National Natural Science Foundation of China (NO. 81972067, 82002342) and the Fundamental Research Funds for the Central Universities, Sun Yat‐sen University (NO. 2020004).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Min Zhou, Chuanhai Zhou and Dedong Cui contributed equally to this work.
Contributor Information
Jingyi Hou, Email: houjy7@mail.sysu.edu.cn.
Rui Yang, Email: yangr@mail.sysu.edu.cn.
References
- 1. Chen RE, Voloshin I. Long head of biceps injury: treatment options and decision making. Sports Med Arthrosc Rev. 2018;26:139–44. [DOI] [PubMed] [Google Scholar]
- 2. Lalehzarian SP, Agarwalla A, Liu JN. Management of proximal biceps tendon pathology. World J Orthop. 2022;13:36–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wittstein JR, Queen R, Abbey A, Toth A, Moorman CT 3rd. Isokinetic strength, endurance, and subjective outcomes after biceps tenotomy versus tenodesis: a postoperative study. Am J Sports Med. 2011;39:857–65. [DOI] [PubMed] [Google Scholar]
- 4. Liu H, Song X, Liu P, Yu H, Zhang Q, Guo W. Clinical outcomes of arthroscopic Tenodesis versus Tenotomy for long head of the biceps tendon lesions: a systematic review and meta‐analysis of randomized clinical trials and cohort studies. Orthop J Sports Med. 2021;9:2325967121993805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schrock JB, Kraeutler MJ, Bravman JT. Comparison of clinical failure rates after 2 techniques of subpectoral mini‐open biceps Tenodesis: sequence and suture passage technique matter. Orthop J Sports Med. 2017;5:2325967117729356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Green JM, Getelman MH, Snyder SJ, Burns JP. All‐arthroscopic Suprapectoral versus open subpectoral Tenodesis of the long head of the biceps Brachii without the use of interference screws. Art Ther. 2017;33:19–25. [DOI] [PubMed] [Google Scholar]
- 7. Tu J, Xu B, Guo R. Open subpectoral vs. arthroscopic proximal biceps tenodesis: a comparison study of clinical outcomes. Exp Ther Med. 2020;19:428–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vellios EE, Nazemi AK, Yeranosian MG, Cohen JR, Wang JC, McAllister DR, et al. Demographic trends in arthroscopic and open biceps tenodesis across the United States. J Shoulder Elbow Surg. 2015;24:e279–85. [DOI] [PubMed] [Google Scholar]
- 9. Saltzman BM, Leroux TS, Cotter EJ, Basques B, Griffin J, Frank RM, et al. Trends in open and arthroscopic long head of biceps Tenodesis. HSS J. 2020;16:2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hurley DJ, Hurley ET, Pauzenberger L, Lim Fat D, Mullett H. Open compared with arthroscopic biceps Tenodesis: a systematic review. JBJS Rev. 2019;7:e4. [DOI] [PubMed] [Google Scholar]
- 11. Patzer T, Rundic JM, Bobrowitsch E, Olender GD, Hurschler C, Schofer MD. Biomechanical comparison of arthroscopically performable techniques for suprapectoral biceps tenodesis. Art Ther. 2011;27:1036–47. [DOI] [PubMed] [Google Scholar]
- 12. Lafosse L, Van Raebroeckx A, Brzoska R. A new technique to improve tissue grip: "the lasso‐loop stitch". Art Ther. 2006;22(1246):e1241–3. [DOI] [PubMed] [Google Scholar]
- 13. Kaback LA, Gowda AL, Paller D, Green A, Blaine T. Long head biceps tenodesis with a knotless cinch suture anchor: a biomechanical analysis. Art Ther. 2015;31:831–5. [DOI] [PubMed] [Google Scholar]
- 14. Muller S, Flury R, Zimmermann S, et al. The new LassoLoop360 degrees technique for biomechanically superior tissue grip. Knee Surg Sports Traumatol Arthrosc. 2019;27:3962–9. [DOI] [PubMed] [Google Scholar]
- 15. Acosta J, Rinaldi JM, Guth JJ, Akhavan S. The loop 'n' tack knot: biomechanical analysis of a novel suture technique for proximal biceps Tenodesis. Orthop J Sports Med. 2020;8:2325967120952315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhou M, Zhou CH, Zhang JM, Yi L, Guo J, Hou JY, et al. The lark loop used for proximal biceps Tenodesis: an all‐arthroscopic technique. Arthrosc Tech. 2022;11:e1195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Domnick C, Wieskotter B, Raschke MJ, et al. Evaluation of biomechanical properties: are porcine flexor tendons and bovine extensor tendons eligible surrogates for human tendons in in vitro studies? Arch Orthop Trauma Surg. 2016;136:1465–71. [DOI] [PubMed] [Google Scholar]
- 18. Deramo DM, White KL, Parks BG, Hinton RY. Krackow locking stitch versus nonlocking premanufactured loop stitch for soft‐tissue fixation: a biomechanical study. Art Ther. 2008;24:599–603. [DOI] [PubMed] [Google Scholar]
- 19. Agarwalla A, Puzzitiello RN, Leong NL, Shewman EF, Verma NN, Romeo AA, et al. A biomechanical comparison of two arthroscopic suture techniques in biceps tenodesis: whip‐stitch vs. simple suture techniques. J Shoulder Elbow Surg. 2019;28:1531–6. [DOI] [PubMed] [Google Scholar]
- 20. Abraham VT, Tan BH, Kumar VP. Systematic review of biceps Tenodesis: arthroscopic versus open. Art Ther. 2016;32:365–71. [DOI] [PubMed] [Google Scholar]
- 21. Harris JD. Editorial Commentary: Open Versus Arthroscopic Biceps Tenodesis—You Choose. Art Ther. 2016;32:372–3. [DOI] [PubMed] [Google Scholar]
- 22. Erickson BJ, Jain A, Cvetanovich GL, Nicholson GP, Cole BJ, Romeo AA, et al. Biceps Tenodesis: an evolution of treatment. Am J Orthop (Belle Mead NJ). 2017;46:E219–23. [PubMed] [Google Scholar]
- 23. Meraner D, Sternberg C, Vega J, Hahne J, Kleine M, Leuzinger J. Arthroscopic tenodesis versus tenotomy of the long head of biceps tendon in simultaneous rotator cuff repair. Arch Orthop Trauma Surg. 2016;136:101–6. [DOI] [PubMed] [Google Scholar]
- 24. Hufeland M, Kolem C, Ziskoven C, Kircher J, Krauspe R, Patzer T. The influence of suprapectoral arthroscopic biceps tenodesis for isolated biceps lesions on elbow flexion force and clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2017;25:3220–8. [DOI] [PubMed] [Google Scholar]
- 25. Fang JH, Dai XS, Yu XN, Luo JY, Liu XN, Zhang MF, et al. Lesions of the long head of the biceps tendon concomitant with rotator cuff tears: Tenotomy or subpectoral mini‐open Tenodesis? A comparative short to mid‐term follow‐up study. Orthop Surg. 2019;11:857–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ihsan Kilic A, Hapa O, Ozmanevra R, Demirhan Demirkiran N, Gursan O. Biceps tenodesis combined with rotator cuff repair increases functional status and elbow strength. J Orthop Surg (Hong Kong). 2021;29:23094990211056978. [DOI] [PubMed] [Google Scholar]
- 27. Hapa O, Barber FA, Sunbuloglu E, Kocabey Y, Sarkalkan N, Baysal G. Tendon‐grasping strength of various suture configurations for rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2011;19:1749–54. [DOI] [PubMed] [Google Scholar]
- 28. Ponce BA, Hosemann CD, Raghava P, Tate JP, Eberhardt AW, Lafosse L. Biomechanical evaluation of 3 arthroscopic self‐cinching stitches for shoulder arthroscopy: the lasso‐loop, lasso‐mattress, and double‐cinch stitches. Am J Sports Med. 2011;39:188–94. [DOI] [PubMed] [Google Scholar]
- 29. Patzer T, Santo G, Olender GD, Wellmann M, Hurschler C, Schofer MD. Suprapectoral or subpectoral position for biceps tenodesis: biomechanical comparison of four different techniques in both positions. J Shoulder Elbow Surg. 2012;21:116–25. [DOI] [PubMed] [Google Scholar]
- 30. Ryu JH, Pedowitz RA. Rehabilitation of biceps tendon disorders in athletes. Clin Sports Med. 2010;29:229–46. vii‐viii. [DOI] [PubMed] [Google Scholar]
- 31. Uschok S, Herrmann S, Pauly S, Perka C, Greiner S. Combined arthroscopic tenodesis of the long head of biceps and rotator cuff repair in antero‐superior cuff tears. Arch Orthop Trauma Surg. 2016;136:1273–9. [DOI] [PubMed] [Google Scholar]
- 32. McKeon BP, Heming JF, Fulkerson J, Langeland R. The Krackow stitch: a biomechanical evaluation of changing the number of loops versus the number of sutures. Art Ther. 2006;22:33–7. [DOI] [PubMed] [Google Scholar]
- 33. Hahn JM, Inceoglu S, Wongworawat MD. Biomechanical comparison of Krackow locking stitch versus nonlocking loop stitch with varying number of throws. Am J Sports Med. 2014;42:3003–8. [DOI] [PubMed] [Google Scholar]


