In 1990, a 54-year-old man with hypertension and diabetes mellitus was admitted to our institution with an acute coronary syndrome. Coronary angiography (Figs. 1A and 2A) revealed prominent aneurysmal dilatation of the proximal portions of all major coronary arteries. He was treated medically with a calcium channel blocker and aspirin.
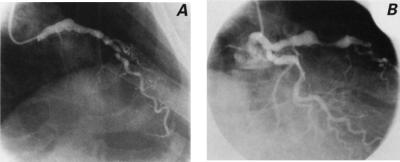
Fig. 1 A) Initial coronary angiogram of the left anterior descending (LAD) coronary artery shows proximal aneurysmal dilatation. The circumflex coronary artery was also aneurysmal but was not selectively injected on this frame. B) Coronary angiogram 8 years later shows increase of the aneurysmal dilatation of the LAD and long, tubular stenosis in its mid-portion. The proximal circumflex artery is ectatic.
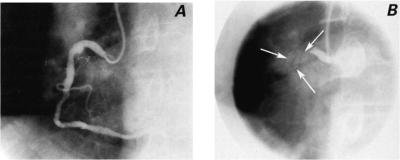
Fig. 2 A) Initial coronary angiogram of the right coronary artery (RCA) shows aneurysmal dilatation of the proximal segment. B) Coronary angiogram at presentation 8 years later shows the shadow (arrows), indicative of calcification, of a much larger proximal RCA aneurysm with thrombotic occlusion.
The patient did well for 8 years and experienced no angina pectoris until late 1998, when he presented to a local emergency center with typical ischemic pain and electrocardiographic changes consistent with acute inferior wall myocardial infarction. He received tissue plasminogen activator for thrombolysis and was then transferred to our institution. Upon arrival, he developed ventricular fibrillation and was immediately defibrillated. Coronary angiography (Figs. 1B and 2B) showed severe progression of his aneurysmal coronary artery dilatation. Additionally, there was focal stenosis of the left anterior descending artery and thrombotic occlusion at the site of a large, calcified proximal right coronary artery aneurysm. The patient received medical therapy and had an uneventful convalescence. Later, he was readmitted for elective aortocoronary bypass surgery, which was successful.
Aneurysmal coronary artery disease (CAD) is thought to occur in fewer than 5% of patients. 1 Reported incidence rates vary, depending on the angiographic criteria used to define the aneurysms. The most common cause of coronary artery aneurysm in the adult patient is atherosclerosis. Other causes include Kawasaki's disease, diagnostic or interventional coronary angiography, inflammatory and infectious arteritis, connective tissue disease, aortic dissection, tumor metastases, trauma, and congenital malformation.
A review of the recent English-language literature yielded no previous studies on the angiographic follow-up of atherosclerotic coronary aneurysms. Nevertheless, this entity merits consideration, since it carries potentially life-threatening complications, as in our patient. As the atherosclerosis progresses, the aneurysms enlarge, which can lead to myocardial ischemia, unstable coronary syndromes, and cardiac arrest.
The long-term prognosis and optimal management of these patients is not certain. The altered blood flow in aneurysmal segments is thought to predispose to thrombosis or embolism and subsequent ischemia or infarction. 2 However, a 1983 review of the Coronary Artery Surgery Study registry data found no difference between survival of patients who had coronary aneurysms and insignificant CAD and survival of patients who had no aneurysms in association with insignificant CAD. 2 Because of the relatively uncommon nature of these aneurysms, management of these patients has been based on anecdotal reports and experience and has included antiplatelet and anticoagulant medications. Nevertheless, it is generally agreed that coronary artery bypass surgery should be performed in patients who have aneurysmal disease concomitant with significant coronary stenosis.
Footnotes
Address for reprints: Virendra S. Mathur, MD, Department of Cardiology, Texas Heart Institute at St. Luke's Episcopal Hospital, 6624 Fannin Street, Suite 2480, Houston, TX 77030