Abstract
Food insecurity has disproportionately impacted Hispanic/Latinx households in the United States, specifically those with young children. Although the literature provides evidence of an association between food insecurity and adverse health outcomes in young children, minimal research has addressed the social determinants and related risk factors associated with food insecurity among Hispanic/Latinx households with children under three, a highly vulnerable population. Using the Socio-Ecological Model (SEM) as a framework, this narrative review identified factors associated with food insecurity among Hispanic/Latinx households with children under three. A literature search was conducted using PubMed and four additional search engines. Inclusion criteria consisted of articles published in English from November 1996 to May 2022 that examined food insecurity among Hispanic/Latinx households with children under three. Articles were excluded if conducted in settings other than the US and/or focused on refugees and temporary migrant workers. Data were extracted (i.e., objective, setting, population, study design, measures of food insecurity, results) from the final articles (n = 27). The strength of each article’s evidence was also evaluated. Results identified individual factors (i.e., intergenerational poverty, education, acculturation, language, etc.), interpersonal factors (i.e., household composition, social support, cultural customs), organizational factors (i.e., interagency collaboration, organizational rules), community factors (i.e., food environment, stigma, etc.), and public policy/societal factors (i.e., nutrition assistance programs, benefit cliffs, etc.) associated with a food security status of this population. Overall, most articles were classified as “medium” or higher quality for the strength of evidence, and more frequently focused on individual or policy factors. Findings indicate the need for more research to include a focus on public policy/society factors, as well as on multiple levels of the SEM with considerations of how individual and policy levels intersect and to create or adapt nutrition-related and culturally appropriate interventions to improve food security of Hispanic/Latinx households with young children.
Keywords: food security, early childhood, Hispanic/Latinx household, social determinants of health, risk factors, Socio-Ecological Model, low-income population
Statement of Significance.
Understanding factors contributing to food insecurity is an essential first step in addressing the negative impacts on US households with young children. Using the SEM framework, this narrative review provides an overview of the current state of knowledge about the factors associated with food insecurity, particularly in Hispanic/Latinx households with children under the age of 3 y. Recognizing how multiple factors intersect and impact the food security status of the most vulnerable households is pivotal for developing and/or adapting interventions and promoting policies that improve access and availability of adequate and nutritious foods to these families, contributing to health outcomes.
Introduction
Food insecurity is a critical public health issue affecting millions of households in the United States [1]. In 2020, an estimated 14.8% of households with children (13.8 million) met the US Department of Agriculture (USDA) Economic Research Service definition of food insecurity—“limited or uncertain availability of nutritionally adequate and safe foods, or limited or uncertain ability to acquire acceptable foods in socially acceptable ways [2].”
Historically, the reported prevalence of food insecurity of underrepresented groups in the US has been statistically higher than the national average for all US households [3]. In 2020, the rate of food insecurity was higher for Hispanic (17.2%) than for White, non-Hispanic (7.1%) households [4]. Similarly, across racial/ethnic groups, the prevalence of food insecurity in households with children under 6 was higher (15.3%) than the national average for all US households (10.5%) [5]. Hispanic/Latinx children were more than twice as likely to live in food-insecure households as White children [6].
Several studies have found that children under three living in food-insecure households have poorer overall health than children living in food-secure households [[7], [8], [9]]. For instance, infants and toddlers in these food-insecure households have an increased risk of developing congenital disabilities, anemia, cognitive problems, aggression, and anxiety [[10], [11], [12], [13]]. Thus, adequate and age-appropriate dietary intake in the first 1000 days of life is pivotal for a child’s growth and development [14].
Although the existing body of research provides evidence of an association between food insecurity and adverse health outcomes in young children, minimal research has been conducted to address the social determinants of health (SDOH) associated with food insecurity among Hispanic/Latinx households with children under age three [11, [15], [16], [17]]. SDOH refers to “conditions in the places where people live, learn, work, and play that affect a wide range of health and quality of life–risks and outcomes” [18]. SDOH can be grouped into five domains, including 1) economic stability, 2) education access and quality, 3) health care access and quality, 4) neighborhood and built environment, and 5) social and community context [18]. Food insecurity in the context of SDOH results from a combination of economic and social structural barriers, creating short and long-term effects on the health, and well-being of individuals living in these households [19].
Research has found that food-insecure households with young children are less likely to consume a nutrient-dense diet than food-secure households with young children, which has been associated with increased body weight, risk of chronic disease, and poor health outcomes [[20], [21], [22], [23], [24]]. Understanding the multiple levels of influence contributing to food security in Hispanic/Latinx households with young children is an essential first step to addressing the needs and barriers of US households with young children. The Socio-Ecological Model (SEM) has been previously applied to address the determinants of health associated with food insecurity and other health behaviors, including obesity and other chronic diseases [25, 26]. This model places the individual at the center of the ecosystem, providing an integrative framework to identify the multiple factors (i.e., innate characteristics and/or sociocultural environment) that contribute to food insecurity in Hispanic/Latinx households with young children [27].
This narrative review provides an overview of the determinants contributing to food insecurity among Hispanic/Latinx households with children <3 y old by applying the SEM. Only studies focused on documented Hispanic/Latinx caregivers living in US households were included in this review. Specific objectives of this narrative review include: 1) providing an overview of the current state of knowledge about factors associated with food insecurity among US Hispanic/Latinx households with children under the age of three based on the SEM; 2) classifying the strength of the evidence to identify predominant research gaps and future research directions to reduce food insecurity within this population; and 3) providing practice and policy-based recommendations for the development and evaluation of interventions that intend to reduce food insecurity of Hispanic/Latinx households with young children.
Methods
This narrative review consisted of a search of peer-reviewed scientific literature and a snowball search of the reference sections of retrieved articles to inform the criteria needed to address the review objectives. Additional online searches were conducted to identify reports and documents from organizations actively involved in advancing equitable access to nutritious food for underserved populations, specifically Hispanic/Latinx groups (e.g., UnidosUS, Urban Institute, Brookings, and Feeding America—Latino Hunger Research).
Before initiating the literature search, inclusion and exclusion criteria were defined to identify the articles of interest. Inclusion criteria consisted of articles published in English that examined food insecurity among Hispanic/Latinx households with children in the age range of 0 to 3 y old in the US. Studies published after November 1996 (i.e., the year when food security was defined at the World Food Summit) and available until May 4, 2022 were included [28]. Observational and experimental studies, including both qualitative and quantitative, were included if they explored or evaluated risk factors associated with food insecurity among Hispanic/Latinx households with young children. Articles were excluded if they were conducted outside the US and/or focused on undocumented immigrants, refugees, or temporary migrant workers. Research suggests experiences of the groups mentioned above differ from other Hispanic/Latinx groups [29, 30].
Research databases included PubMed, Cumulative Index to Nursing and Allied Health Literature, Web of Science, Google Scholar, and Google search engine. The search strategy was developed with support from the University of Florida librarian. Medical Subject Headings (i.e., MeSH terms in PubMed), Subject Headings (i.e., MH in Cumulative Index to Nursing and Allied Health Literature), and Research Area (i.e., SU in Web of Science) were identified and included in the search strategy. For instance, the search included MeSH-compliant keywords: Food Supply, Infant, Child, Preschool, and Infant Health. All other search terms related to “Food Security,” “Young Children,” and “Hispanic /Latinx” were searched under title and abstracts. Terms under “Contributed Factors” were only included in the search strategy for Web of Science to minimize limiting the research results. The final search strategy respective to each database is outlined in Supplemental Table 1. Google Scholar and Google engine searches were utilized to identify gray literature (i.e., reports and other documents published from relevant organizations and websites).
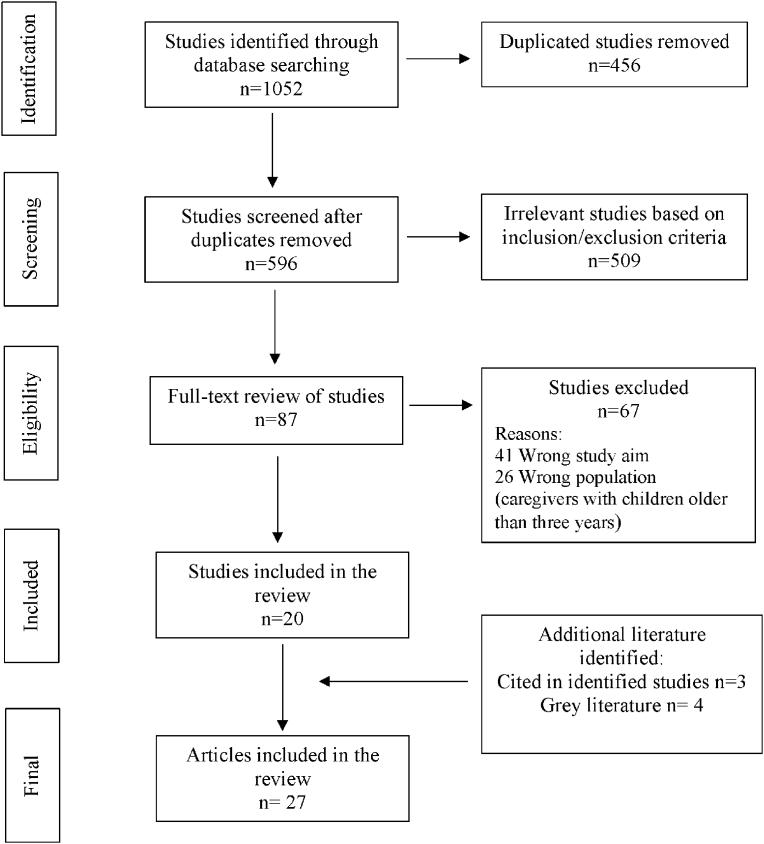
The search for this narrative review was conducted in May 2022 by one of the authors (EGV), resulting in an initial total of 1052 records. After duplicated search results were excluded using Covidence [31], a screening and data extraction tool, 596 articles were screened by one of the authors (EGV). Only 87 articles were selected for a full review, and 20 of these articles matched the inclusion criteria. Additional articles (n = 3) were identified by scanning the reference sections. Articles identified through gray literature (n = 4) search were also added to the review. Thus, a final total of 27 articles were included in this narrative review. Figure 1 provides a detailed summary of the sample selection process.
FIGURE 1.
Summary of the sample selection process.
An Excel spreadsheet was used to extract and organize data from the final articles (n = 27). Data were extracted by one of the authors (EGV) and included: study reference, aim and purpose, setting and population, study design, measures of food insecurity, primary findings, and strength of evidence (Table 1). The strength of evidence of each article was evaluated using a scoring system derived from a prior published report on systematic approaches to assess the strength of scientific evidence [32]. The scoring system was used to rate the quality of each article by the lead author (EGV) based on defined elements and domains identified for different types of studies, including systematic reviews, randomized controlled trials, observational studies, and studies of diagnostic tests [32]. For instance, when rating the quality of observational studies, the author (EGV) reviewed the following elements: comparability of subjects, exposure or intervention, outcome measurement, statistical analysis, and funding or sponsorship [32]. As indicated by West et al. [32], the report indicates that if a study contained ≥75% of the evaluated elements, it was rated high in quality. If a study met <75% but >25% of the evaluated elements, it was rated as medium in quality, and if a study contained <25% of the evaluated elements, it was rated low in quality.
TABLE 1.
Overview, main findings, and strength of evidence of peer-reviewed studies and gray literature: narrative review examining food insecurity among Hispanic/Latinx households with children under the age of three (n = 27)
| Reference | Aim/Purpose | Setting/Population | Study Design | Key Variables/Inclusion Criteria | Measure of Food Insecurity | Main Findings | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Abrams et al., 2020 [34] | Determine how the pandemic has affected families' food insecurity. | Families receiving care at FQHC clinics in Austin, Texas, US; (n = 200). | Qualitative | Food Insecurity COVID-19 Socio-Demographic Characteristics |
2-Item USDA Household Food Security Module/Screener |
|
High Limited generalizability |
| Arteaga et al., 2021 [49] | Examine the relationship between SNAP participation and infant well-child visits using state administrative data from Missouri’s Department of Social Services from January 2006 to July 2014 for >50,000 infant-mother dyads. | First-born children of low-income mothers aged 18 and older in Missouri participating in SNAP and Medicaid, (n = 51,551 children: infant-mother dyads). | Cross-sectional | Well-child visits Immunizations Months of SNAP participation Patterns of SNAP participation Child and mother demographic characteristics |
Not Applicable |
|
Medium Variable bias Analyses were descriptive and could not explore how SNAP may affect child-well visits. Limited generalizability. |
| Berg et al., 2013 [40] | Understand relationships between parent and child weight status, parental perceptions of weight, child feeding, food insecurity, and acculturation. | Hispanic parent-child (2–5 yrs.) dyads in southern California, US; (n = 85). | Cross-sectional | Parent And Child Weight Status Parental Perceptions of Weight Child Feeding Food Insecurity Acculturation |
The Household Food Insecurity Access Scale |
|
Low Small sample size Measure used for calculating BMI1 Cross-sectional data prevent the drawing of causal inferences. |
| Bermúdez-Millán et al., 2011 [35] | Understand the social determinants of health of Puerto Rican women, emphasizing the determinants likely to affect maternal health and pregnancy outcomes. | Puerto Rican women, pregnant or with young children in the cities of Hartford and Willimantic, Connecticut, US; (n = 29) | Qualitative | Self-Perceived Discrimination Based on Race/Ethnicity Poverty Food Insecurity Education Health Care Access and Treatment Physical Environment, Working Conditions |
Three Interview Guide Questions |
|
High Limited generalizability Some of the focus groups were conducted in Spanish, and others in English |
| Buscemi et al., 2011 [41] | Determine if food insecurity was a predictor of BMI percentile and to examine acculturation as a moderator. | Latino children ages 2–17 of both immigrant and nonimmigrant parents in Memphis, Tennessee, US; (n = 63). | Cross-sectional | Child Anthropometric Measures Parent Socio-Demographic Characteristics Parental Acculturation Food Insecurity |
The Core Food Security Measure |
|
Low A significant amount of food insecurity and acculturation data missing and not included in the analyses Cross-sectional data prevent the drawing of causal inferences. |
| Chavez et al., 2007 [42] | Examine ethnic differences in Latino child health services use and describe and compare health and nutrition attitudes and practices. | Mexican, Puerto Rican, or other Hispanic mothers of children ages 3–8 in Chicago, Illinois, US; (n = 320). | Cross-sectional | Food Insufficiency Acculturation Socio-Demographic Characteristics |
10-Item Radimer/Cornell Measure of Hunger and Food Insecurity NHANES III (Family Questionnaire And 24-h Recall) |
|
Medium Although the food insufficiency scales and questions used in this study had been validated, they were not validated for the Latino population Small sample size Cross-sectional data prevent the drawing of causal inferences. |
| Chilton et al., 2009 [43] | Investigate the risk of household food insecurity and reported fair or poor health among very young children who were US citizens and whose mothers were immigrants. | Mothers with children aged 0–3 in Minneapolis, Minnesota, US; (n = 19,275). | Cross-sectional | Child Anthropometric Measures Food Insecurity |
USDA 18-Item Food Security Scale |
|
Medium Recall bias, shared method bias, cultural differences Cross-sectional data prevent the drawing of causal inferences. |
| Denney et al., 2020 [44] | Understand if household characteristics within a residential context are important for household food insecurity. | Kindergarten-age children who live in 2,951 Census tracts in the US; (n = 8600). | Cross-sectional | Household Food Insecurity Child And Household Socio-Demographics Primary Caregiver Depression Level Household-Level Measures of Poverty |
USDA’s 18-Item Food Security Scale |
|
High Any possible benefits of contextual incongruence for household food security status might require a more extended period Cross-sectional data prevent the drawing of causal inferences. |
| Dhokarh et al., 2011 [45] | Examine associations between acculturation indicators and food insecurity and the influence of social networks and reciprocity on food insecurity. | Puerto Rican heads of the household with children between 12 and 36 mo of age in Hartford, Connecticut, US; (n = 200). | Cross-sectional | Food Insecurity Acculturation Social Networks and Reciprocity |
10-Item Radimer/Cornell Measure of Hunger and Food Insecurity |
|
Low Data was collected over 10 y. The main conclusion does not allow for the assessment of causality and the temporal sequence of events Cross-sectional data prevent the drawing of causal inferences. |
| Escobar et al., 2021 [58] | Examine the impact of COVID-19 on household and child food security in three preexisting, longitudinal, Latinx urban cohorts. | Hispanic mothers with young children in San Francisco, California, US; (n = 1875). | Research Report (not peer-reviewed) | Food Insecurity Food Assistance COVID-19 Symptoms |
USDA’s 18-Item Food Security Scale |
|
Not Applicable |
| Gonzalez, A. 2020 (Center for Primary Care: Harvard Medical School) [59] | Discuss how COVID-19 Exacerbates Food Insecurity in Latino Children & Families. | Latino young children and families in the US. | Report not peer-reviewed | Not Applicable | Not Applicable |
|
Not Applicable |
| Gross et al., 2019 [36] | Obtaining a better understanding of obesity-promoting infant-feeding beliefs, styles, and practices in the context of food insecurity. | Low-income Hispanic mother-infant pairs participating in an early childhood obesity prevention study at a large urban public hospital in New York City, New York, US; (n = 100). | Qualitative nested with a Randomized Controlled Trial | Food Insecurity Financial Pressures Infant And Toddler Feeding |
Interview Guides Informed by The Core Food Security Module–USDA |
|
Medium Limited generalizability The trial excluded the most marginalized families, including those with homelessness or severe mental illness. |
| Himmelgreen et al., 2000 [33] | Examine hunger and food insecurity among low-income Hispanics in Hartford, Connecticut, using the Radimer/Cornell Scale and the associations of specified variables (e.g., socio-demographics and food-assistance participation) with food insecurity. | Low-income Hispanic caretakers of children ≥1-y-old but younger than 6 y, recruited between July 19, 1995, and October 10, 1996, in Hartford, Connecticut, US; (n = 248). | Retrospective Cohort | Food Insecurity Food Stamps Run Out Before the End of The Month Caretaker Head of Household Child Enrollment in Preschool/Kindergarten Program Maternal Age Emergency Food Assistance |
10-Item Radimer/Cornell Measure of Hunger and Food Insecurity |
|
Low Data collected before national welfare reform changes (1995–1996) |
| Innella et al., 2016 [54] | Identify factors that influence obesity in Hispanic preschool children and factors needing further investigation. | N = 35 (articles) conducted in the US. | Integrative Review | Inclusion Criteria: Peer-Reviewed Articles Published between 2009–2014, With 50% Or More Of The Participants Either Parents/Caregivers of Preschool-Age Children or Preschool-Age Children And 50% Or More Participants Were Hispanic. |
Not Applicable |
|
Low Lack of detailed explanations about statistical significance in some of the quantitative studies |
| Johnson et al., 2020 [53] | Examine the association of neighborhood food environment and childhood weight status among 2–5 y old. | Black and Hispanic children aged 2–5 in Baltimore, Maryland, US; (n = 3724). | Retrospective Cohort | Body Mass Index Z-Score Healthy Food Availability Index WIC2 Store Availability Fast Food Availability Child Socio-Demographics |
Not Applicable |
|
Medium Limited generalizability |
| Kaiser et al., 2003 [46] | Examine the relationship between food insecurity and food supplies in Latino households. | Low-income Latino households with preschool children in six counties of California, US; (n = 274). | Cross-sectional | Food Insecurity Food Supplies Maternal And Child Body Mass Index Child Frequency of Food Consumption Mother’s Socio-Demographics |
USDA’s 18-Item Food Security Scale |
|
High Limited generalizability The list of the most reported food supplies by these Californian Latino families is very similar to that reported in the Chicago validation study Cross-sectional data prevent the drawing of causal inferences. |
| Kamdar et al., 2019 [47] | Examine the effects of food insecurity on a child’s body mass index through a complex series of pathways that involve parental feeding demandingness and responsiveness and child dietary quality. | Hispanic parent-preschooler (4–5 y) dyads in Houston, Texas, US; (n = 137). | Cross-sectional | Food Insecurity Parental Feeding Demandingness And Responsiveness Dietary Quality Maternal And Child Body Mass Index Acculturation |
6-Item Household Food Security Survey |
|
Medium Limited generalizability Self-report bias Cross-sectional data prevent the drawing of causal inferences. |
| Keith-Jennings et al., 2021 [56] | CBPP analysis of data from the Census Bureau’s ongoing Household Pulse Survey from April 2020 through late March 2021 | US Census population. | Report not peer-reviewed | Food Insecurity | Census Bureau’s Ongoing Household Pulse Survey from April 2020–March 2021 |
|
Not Applicable |
| Lindsay et al., 2009 [37] | Explore immigrant Latina mothers’ perceptions of factors that act as barriers to establishing their preschool-aged children's healthy eating and physical activity habits. | Latina mothers and their preschool-aged children in Boston, Massachusetts, US; (n = 51). | Qualitative | Barriers To Establishing Healthy Eating and Physical Activity Habits | Not Applicable |
|
Medium Limited generalizability Recall bias, shared method bias, cultural differences |
| McCurdy et al., 2022 [50] | Examine the relationships between food security status, food parenting practices, and child eating behaviors in a predominately Hispanic, low-income sample of parents and preschool-aged children. | Hispanic, low-income parents and their preschool-aged (2–5y) children; (n = 66). | Cross-sectional | Food insecurity Food parenting practices Child eating behaviors Demographic and anthropometric characteristics |
2-Item USDA Household Food Security Module/Screener |
|
Medium The small sample size reduced the power to finding significant Associations Limited generalizability Cross-sectional data prevent the drawing of causal inferences. Self-report could have led to social desirability bias and measurement error |
| Nederveld et al. 2021 [39] | Understand the health behaviors of families with young children facing food insecurity in western Colorado. Specifically, parents on limited incomes use strategies to feed their children, their understanding of nutrition for their children, and the social factors contributing to or alleviating food insecurity. | Parents of young children from Mesa County, Colorado receiving WIC benefits–9 reported Latinx heritage (n = 20). | Qualitative | Strategies for families with food insecurity to navigate health behaviors in their social context | USDA’s 18-Item Food Security Scale |
|
Medium Limited generalizability Recall bias, shared method bias, cultural differences |
| Ochoa et al., 2017 [55] | Summarize and critically review the cross-sectional and longitudinal research conducted between 2005 and 2015 on key factors in the home environment of Latino children. | n = 7 (articles). | Narrative Review | Factors Within the Home Environment That Were Potential Factors Influencing Childhood Obesity Risk. | Not Applicable |
|
Medium Lack of detailed explanations about statistical significance in some of the studies |
| Pineros-Leano et al., 2019 [38] | Understand how Latina immigrant mothers make feeding decisions for their children using the Socio-Ecological Model. | Mothers from Latin American countries whose preschoolers were enrolled in WIC (n = 29). | Qualitative | Mother’s decision-making around feeding choices | Not applicable |
|
Medium Limited generalizability Recall bias, method bias (did not collect health status measures), cultural differences |
| Sharkey et al., 2013 [48] | Determine the prevalence of child hunger and identify protective and risk factors associated with hunger among children. | Mexican-origin mothers with children under the age of 5 in 44 colonias in two geographic areas in Texas (n = 470). | Cross-sectional | Individual, Economic, Family, And Community Resources Childhood Hunger |
12-Item Radimer/Cornell Measure of Hunger and Food Insecurity |
|
Medium Self-report bias Data did not attribute child hunger to specific children, or how the availability of food varied among household members Cross-sectional data prevent the drawing of causal inferences. |
| Schanzenbach et al., 2020 [57] | Describe levels and trends in food insecurity among households with children by the race/ethnicity of the adult respondent for the household. | Individuals who responded to Census Household Pulse Survey. | Rapid Research (Report not peer-reviewed) | Food Security Socio-Demographics |
Census Household Pulse Survey |
|
Not Applicable |
| Steimle et al., 2021 [52] | Investigates the implications of COVID-19 for families’ food insecurity and parent and child psychological distress and how receipt of food assistance programs may have buffered those effects. | Low-income families in rural Pennsylvania; Latinx 60.7% (N = 173–271). | Cross-sectional exploratory design (Longitudinal study) | Food insecurity Parent psychological distress Child psychological distress Food assistance usage Demographics |
Current Population Survey Food Security Supplement |
|
Medium Limited generalizability Interruption time-series approach Lack of randomization Cross-sectional data prevent the drawing of causal inferences. |
| Ventura et al. 2022 [51] | Describe WIC participants’ experiences with remote service delivery and recertification during the pandemic. | Mothers and infants who participated in a WIC-based intervention between June 2019–August 2020; (n = 246). | Cross-sectional study | Food Insecurity COVID-19 WIC participation (i.e., experiences with remote recertification and remote engagement services) Demographics |
USDA 6-item Household Food Security Screener |
|
High Recall bias Limited generalizability |
CBPP, Center on Budget and Policy Priorities; FQHC, Federally Qualified Health Centers; P-EBT, Pandemic Electronic Benefit Transfer; SES, socioeconomic status; SNAP, Supplemental Nutrition Assistance Program; WIC, The Special Supplemental Nutrition Program for Women, Infants, and Children.
This narrative review also utilized SEM as a framework to conceptualize the determinants of food insecurity among Hispanic/Latinx households with young children. The SEM consists of five levels of influence: individual, interpersonal, community, organizational, and policy, systems, or environment levels [27]. It provides a visual depiction of SDOH and other factors within the respective levels of influence that may impact the food security status of Hispanic/Latinx households with young children. As such, one of the authors (EGV) classified the SDOH identified in each peer-reviewed article and gray literature within the different levels of influence of the SEM (Table 2).
TABLE 2.
Levels of influence of the Socio-Ecological Model (SEM), social determinants of health, and corresponding peer-reviewed studies and gray literature examining food insecurity among Hispanic/Latinx households with children under the age of three
| Level of Influence Articles including at least one factor at SEM level, n) | Definition | Social Determinants of Health | Factors | Source |
|---|---|---|---|---|
| Individual (n = 21) | The first level identifies an individual’s biological components and personal history factors. These factors help predict an individual’s likelihood of becoming susceptible to a health condition or engaging in a particular health-related behavior. | Demographics Biological markers Psychological factors Knowledge Attitudes |
1. Education Level 2. Income Level 3. Marital Status 4. Language Proficiency 5. Acculturation Level 6. Nutrition Knowledge 7. Food and feeding preferences 8. COVID-19 fear |
1. Kaiser et al., 2003 [46] 2. Bermúdez-Millán et al., 2011 [35], Chavez et al., 2007 [42], Dhokarh et al., 2011 [45], Gross et al., 2019 [36], Innella et al., 2016 [54], Johnson et al., 2020 [53], Lindsay et al., 2009 [37], McCurdy et al. 2022 [50], Nederveld et al. 2021 [39], Ochoa et al., 2017 [55], Schanzenbach et al., 2020 [57] 3. Dhokarh et al., 2011 [45], Gross et al., 2019 [36] 4. Abrams et al., 2020 [34] 5. Buscemi et al., 2011 [41], Chilton et al., 2009 [43], Denney et al., 2020 [44], Gross et al., 2019 [36], Innella et al., 2015 [54], Pineros-Leano et al., 2019 [38] 6. Bermúdez-Millán et al., 2011 [35], Chavez et al., 2007 [42], Gross et al., 2019 [36], Himmelgreen et al., 2000 [33], Kaiser et al., 2003 [46], Kamdar et al., 2019 [47], Lindsay et al., 2009 [37], Ochoa et al., 2017 [55], Pineros-Leano et al., 2019 [38], Nederveld et al. 2021 [39] 7. Berg et al., 2013 [40], Buscemi et al., 2011 [41], Gross et al., 2019 [36], Pineros-Leano et al., 2019 [38], McCurdy et al. 2022 [50] 8. Abrams et al., 2020 [34] |
| Interpersonal (n = 11) | The second level examines an individual’s formal and informal social networks and social support systems. Social circles play an important role in influencing an individual’s behavior, as these relationships contribute to forming personal experiences and affect decision-making. | Social networks (family, friends, workgroup) Traditions Customs/Rituals |
1. Social networks (family and friends) 2. Culture/Customs |
1. Abrams et al., 2020 [34], Bermúdez-Millán et al., 2011 [35], Chavez et al., 2007 [42], Denney et al., 2020 [44], Dhokarh et al., 2011 [45], Gross et al., 2019 [36], Lindsay et al., 2009 [37], Nederveld et al. 2021 [39], Pineros-Leano et al., 2019 [38] 2. Gonzalez, A. 2020 [59], Pineros-Leano et al., 2019 [38] |
| Community (n = 4) | The third level explores the settings in which relationships occur. It primarily focuses on the relationships among organizations and institutions and how these can influence behavior at an individual or group level. This level of influence also emphasizes the environmental support within the community, including the built environment. | School Worksite Church Businesses Community centers Built environment Institutions |
1. Interagency collaboration 2. Organizational rules and procedures |
1. Keith-Jennings et al., 2021 [56] 2. Abrams et al., 2020 [34], Escobar et. al., 2021 [58], Keith-Jennings et al., 2021 [56], Steimle et al., 2021 [52] |
| Organizational (n = 11) | The fourth level focuses on the organizations or social institutions that create rules and regulations that affect the operation and management of services provided to individuals or groups. | Neighborhoods Organizations Societal institutions |
1. Food Environment 2. Stigma 3. Social capital |
1. Denney et al., 2020 [44], Gross et al., 2019 [36], Johnson et al., 2020 [53], Lindsay et al., 2009 [37], Ochoa et al., 2017 [55], Pineros-Leano et al., 2019 [38], Sharkey et al., 2013 [48], Ventura et al. 2022 [51] 2. Ochoa et al., 2018 [55], Ventura et al. 2022 [51] 3. Dhokarh et al., 2011 [45], Steimle et al., 2021 [52], Nederveld et al. 2021 [39] |
| Policy, Systems and Environment (n = 21) | The outermost level looks at the broad societal factors contributing to the climate of engaging in health-related behavior. It also focuses on the policies and laws that help regulate and support health practices. | Policies Regulations Federal/State laws Societal norms |
1. Supplemental programs 2. Benefit cliffs 3. Inequality of resources 4. Unemployment/Job opportunities/Minimum wage |
1. Abrams et al., 2020 [34], Bermúdez-Millán et al., 2011 [35], Chavez et al., 2007 [42], Chilton et al., 2009 [43], Dhokarh et al., 2011 [45], Gonzalez, A. 2020 [59], Gross et al., 2019 [36], Himmelgreen et al., 2000 [33], Kamdar et al., 2019 [47], Keith-Jennings et al., 2021 [56], Lindsay et al., 2009 [37], Sharkey et al., 2013 [48], Steimle et al., 2021 [52], Ventura et al. 2022 [51] 2. Himmelgreen et al., 2000 [33], Lindsay et al., 2009 [37], Ochoa et al., 2018 [55], Nederveld et al. 2021 [39] 3. Kaiser et al., 2003 [46], Keith-Jennings et al., 2021 [56], Lindsay et al., 2009 [37], Pineros-Leano et al., 2019 [38], Schanzenbach et al., 2020 [57] 4. Dhokarh et al., 2011 [45], Escobar et. al., 2020 [58], Gross et al., 2019 [36], Himmelgreen et al., 2000 [33], McCurdy et al. 2022 [50], Schanzenbach et al., 2020 [57], Steimle et al., 2021 [52] |
CURRENT STATUS OF KNOWLEDGE
A total of 27 studies met the criteria for this narrative review (see Table 1), with a retrospective cohort study published in 2000 being the earliest study included [33]. The literature included six qualitative studies [[34], [35], [36], [37], [38], [39]], 13 cross-sectional studies [[40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52]], two retrospective cohort studies [33, 53], one integrative review [54], one narrative review [55], and four reports [[56], [57], [58], [59]]. The target population for all the identified literature was low-income Hispanic or Latinx families or caregivers (i.e., mothers or fathers) with children under three and focused on the factors that influenced or exacerbated the household food security status. Based on the scoring system for the strength of evidence, a total of five articles [34, 35, 44, 46, 51] were classified as high quality; 13 articles [[36], [37], [38], [39], 42, 43, [47], [48], [49], [50], 52, 53, 55] as medium quality; and five articles [33, 40, 41, 45, 54] as low quality. Four articles [[56], [57], [58], [59]] did not fit the criteria to be scored for the strength of evidence as they were not systematic reviews, randomized clinical trials, observational studies, or diagnostic test studies.
Figure 2 provides a visual representation of the identified factors associated with food insecurity for this population across the different levels of SEM. Table 2 provides a detailed explanation of the different levels of SEM, its corresponding determinants, and the factors identified in the articles of the review. For instance, if nutrition knowledge was indicated as an important factor related to food security, this finding was listed and described under the individual level of the SEM. Articles could be classified at multiple levels depending on if the study addressed >1 level of the SEM. Specifically, 21 articles included at least one focusing on the individual level, 11 at the interpersonal level, four at the community level, 11 at the institutional level, and 21 at the policy, system, or environmental level.
FIGURE 2.
Factors associated with food insecurity in Hispanic/Latinx households with children under the age of three by the different levels of the SEM framework.
The following summarizes the identified factors contributing to food insecurity in Hispanic/Latinx households with children under three by the different levels of SEM (i.e., individual, interpersonal, community, organizational, and policy, systems, or environment).
Individual factors contributing to food insecurity
Within the individual level of SEM, most articles (n = 10) were classified as medium in quality. These provided evidence on how income level [36, 37, 39, 42, 50, 53, 55], marital status [36], acculturation level [36, 38, 43], nutrition knowledge [[36], [37], [38], [39], 42, 47, 55], and food and feeding preferences [36, 38, 50] contribute to food insecurity in Hispanic/Latinx families with young children. Only four articles were rated high in quality and offered evidence on how education level [46], income level [35], language proficiency [34], nutrition knowledge [35, 60], and COVID-19 fear of exposure [34] contribute to food insecurity in these families. Similarly, five studies were rated low in quality providing evidence on how income level [45, 54], marital status [45], acculturation level [41, 54], nutrition knowledge [33], and food and feeding preferences [40, 41] contribute to food insecurity in this population.
Studies in this review reported that households with limited financial resources or low-income were unable to meet basic needs (i.e., rent, utilities, transportation, and medical care), with caregivers having to prioritize expenses, limit or restrict food intake for themselves or their children, and purchase lower-quality and less quantity of healthy foods [33, [35], [36], [37], 39, 42, 43, 45, 47, 54, 57, 58, 62]. For instance, one study mentioned that the frequency and amount of economic support individuals of Hispanic/Latinx households with young children provide to family members outside the US creates additional financial constraints [62] In addition, another study found within a scoping review found that despite experiencing precarious finances, families prioritized sending money “home” (i.e., outside of the US) because they felt their relatives were living in worse financial situations [63].
This narrative review also found other socio-demographic characteristics contributing to food insecurity among Hispanic/Latinx households with children under three. These factors included caregivers’ lower education level (i.e., obtaining less than a high school degree), lack of English language proficiency, marital status (i.e., single and/or one-parent household), and age of children (i.e., younger children require special attention and specific necessities) [34, 36, 45, 46, 62]. For instance, one study stated mothers become worried about purchasing formula for their infants when they are unable to breastfeed, suggesting additional physical, mental, and financial stressors related to providing adequate food for their young child [35].
Moreover, findings from a qualitative study also found pregnancy and infancy increased vulnerability to food insecurity within households because of changes in employment, physical environment limitations (i.e., store proximity), and new infant-related expenses (i.e., diapers, formula, and medical expenses) [36]. Similarly to the previous study, findings also indicated that the mothers rationed certain family members’ portion sizes and restricted the amount of self-perceived “expensive foods” (i.e., fruit, vegetables) during meals to afford infant formula and other healthy food items for their infants and toddlers [35, 36].
Furthermore, the lack of fundamental nutrition knowledge and food resource management in food-insecure Hispanic/Latinx households with children under three also poses a unique challenge to acquiring, storing, and preparing nutritious foods [35, 37, 38, 41, 42, 46]. Several studies within this review reported individuals having a difficult time accessing healthy foods as a result of not knowing where to access healthy and affordable foods and the preconception that healthy items, such as fresh produce, are considerably more expensive than foods with less nutritional value (i.e., junk food or fast food) [35, 37, 38, 41, 42, 46].
Finally, findings from this review show lower levels of acculturation also contribute to food insecurity among Hispanic/Latinx households with children under three [40, 41, 45, 54]. Acculturation is defined as “the process of cultural and psychological change that takes place as a result of contact between cultural groups and their members [64].” Research suggests that first and second-generation immigrants may have to balance the stress of keeping their cultural and ethnic identity, whereas adopting the traditions and customs of an unfamiliar cultural environment [40, 41, 45, 54]. This process makes decision-making challenging, impacting individuals’ ability to learn and practice health-related behaviors, whereas preserving cultural traditions related to food choices [65].
Interpersonal factors contributing to food insecurity
Although not as much evidence was found under the other levels of influence, most of the articles identified were rated as high or medium in quality. Within the interpersonal level of SEM, most articles (n = 5) were rated medium in quality. These provided evidence on how social networks [[36], [37], [38], [39], 42] and culture [38, 59] contribute to food insecurity in Hispanic/Latinx families with young children. Three articles were rated as high quality, showing how social networks contribute to food insecurity in these families. There were no articles rated as low quality within this level of influence. For instance, several studies in this review reported that social networks are an integral component of improving food security in Hispanic/Latinx underserved households with young children [[34], [35], [36], [37], 44, 45]. Social support networks, including extended family, friends, and neighbors, provided safety nets when household strategies proved insufficient to maintain food security [34, 36, 39]. As such, limited social support and feelings of isolation may negatively impact caregivers and their children’s lives [37].
Likewise, this review also identified cultural customs as a factor related to food insecurity in Hispanic/Latinx households with children under three. For instance, one study stated Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participants reported implementing cultural practices such as “giving tea” (i.e., bottle feeding herbal tea) to their infant instead of giving them breast milk or formula as recommended by the US. Dietary Guidelines for Americans [37]. The article stated that cultural beliefs, including the perception that noncultural foods have poor nutritional value compared with culturally appropriate foods, might be a barrier to food security and health [37]. As reported by the article, caregivers struggle to access cultural foods because of low availability and high prices. They are unaware of other nutritionally adequate and age-appropriate foods, including iron-fortified formulas [37]. Similarly, two additional studies suggested that intergenerational poverty (i.e., poverty that persists from one generation to the next) contributes to food insecurity in Hispanic/Latinx underserved households with young children [35, 38]. These articles indicated that a vicious cycle is often created as poverty creates food insecurity conditions, increasing the risk of physiological and mental issues in these families [35, 38].
Organizational factors contributing to food insecurity
Similar to the interpersonal level, only two articles qualified to be rated for strength of evidence within the organizational level of influence. These were ranked as high [34] or medium [52] quality and provided evidence of how organizational rules and procedures contribute to food insecurity in this population. Although, one article [56] provided evidence on how interagency collaboration contributes to food insecurity in Hispanic/Latinx families with young children, this was not rated as it did not fit the criteria utilized to rate the strength of evidence. For instance, parents of these households could not make it to regular business hours because of job scheduling conflicts [33, 59]. Likewise, shutdowns and social distancing policies resulting from COVID-19 added additional barriers limiting Hispanic/Latinx individuals living in food insecurity households from applying for or receiving food assistance benefits [37, 56].
In addition, one article found that Hispanic/Latinx households with children were hesitant to seek support in nonprofit organizations or societal institutions because of fear associated with the public charge rule (i.e., US immigrants classified as liable to become a public charge may be denied visas or permission to enter the country because of their disabilities or lack of economic resources) [34]. Finally, eligible families also reported having difficulty accessing P-EBT and other benefits because of problems with states identifying eligible children or communicating with eligible families [56]. The study reported a lack of communication among key organizations and agencies as a barrier to streamlining and improving access to benefits and services [56].
Community factors contributing to food insecurity
Within the community level of SEM, most articles were rated medium in quality (n = 8) providing evidence on how the food environment [[36], [37], [38], 48, 53, 55], stigma [55], and social capital [39, 52] contribute to food insecurity in Hispanic/Latinx families with young children. Two articles were rated high in quality within this level and offered evidence on the food environment [44, 51] and stigma [51]. Comparably, one article [45] was rated low in quality. It provided evidence on social capital being a contributor to food insecurity in this population. Specifically, proximity to food purchasing and distribution locations (i.e., supermarkets, grocery stores, emergency food pantries, etc.), including Supplemental Nutrition Assistance Program (SNAP) and WIC-eligible stores, have important impacts on healthy food availability and child dietary intake [37, 38, 44, 48, 53]. One study stated spatial inequality of resources is a big challenge for families to access fresh fruits and vegetables [44]. Previous literature supports this finding and has also found that areas that are poorer and/or comprise predominantly racial/ethnic minorities have fewer supermarkets than predominantly White and/or affluent neighborhoods, contributing to limited access to quality food sources in such communities [67].
Social capital (i.e., community events, church, and other community gatherings) also contributes to increasing food security among Hispanic/Latinx households with children under three [36, 45]. Community members and neighbors are meaningful connections for attaining resources [36, 45]. In some instances, neighbors and community centers serve to acquire food, either through transportation to sources or by delivering food. Accordingly, access to reliable and frequent public transit has been associated with increased food security among Hispanic/Latinx under-resourced households with young children [45]. Findings from this review suggest public transportation is often nonexistent within specific communities or operates minimally, creating an obstacle to accessing food [34, 36, 42]. Lack of transportation is an obstacle for various individuals, including families with young children, in different communities, forced to walk long distances to obtain food sources or wait long hours outside in several types of weather for public transportation [68, 69].
Finally, although supplemental food assistance programs protect against food insecurity in some households, research identified for this review found that some individuals refrain from using assistance because they may feel ashamed and/or embarrassed at food retail when using their benefits [[70], [71], [72]]. Thus, addressing the stigma associated with nutrition assistance and enhancing food equity should be considered when creating policies and strategies addressing existing barriers and increasing support for accessing food programs and implementing change systems.
Policy, systems, or environmental factors contributing to food insecurity
Finally, within the policy, systems, and environmental level of SEM, most articles were also rated medium in quality (n = 10). These provide evidence on how supplemental assistance programs [35, 37, 42, 47, 48, 52], benefit cliffs [37, 39, 55], inequality of resources [37, 38], and unemployment or low job opportunities [36, 50, 52] contribute to food insecurity in these families. Only four articles were classified as high in quality and provided evidence on supplemental assistance programs [34, 35] and inequality of resources [46]. Similar to the individual level of influence, this level contained one of the higher number of articles rated as low or not applicable for rating (n = 5) although, the majority of evidence was still rated as high or medium quality overall. These articles provided evidence on how supplemental assistance programs [33, 45, 56, 59], benefit cliffs [33], inequality of resources [56, 57], and unemployment or low job opportunities [33, 45, 57, 58] contribute to food insecurity in Hispanic/Latinx families with young children.
Limited research has explored the association between public policy and food insecurity in Hispanic/Latinx households with children under 3, specifically regarding policies aiming to improve food assistance and food distribution systems [73]. Nonetheless, this review reveals that caregivers of Hispanic/Latinx households with children under three, who receive government aid through SNAP and WIC benefits, believe the amount allocated per household is often not enough to feed all members of their household for the entire month [[34], [35], [36], 38, 42, 74]. In addition, results from these studies reported that given the limited amount of money allotted to purchase foods, families opt to buy affordable or low-price food items that are generally higher in calories and lower in nutritional value (i.e., high-fat and sugary foods) [[34], [35], [36], 38, 42, 48, 74].
Some studies from this review also reported the association between benefits cliffs and food insecurity among Hispanic/Latinx households with young children [33, 35, 42, 43, 49]. A “benefits cliff” is defined as when a person or household makes too much money to qualify for government benefits but not enough to sustain their household. The Welfare or Poverty Trap Theory, now referred to as a “benefits cliff,” argues that “poverty creates bad incentives that undermine motivations for and returns to investments that could reduce subsequent poverty.” Findings from this review align with another study that reported similar findings stating that individuals experiencing poverty or unemployment often also have limited economic incentives resulting from minimum wage and/or lack of income and have to find ways to stretch their money to meet basic needs [75]. Similarly, another study reported that even when individuals receive slightly higher earnings, they often also see a reduction in their net income because of economic inflation or other economic or social issues and cannot afford necessities without additional financial assistance [76].
A report included in this review found that Hispanic/Latinx families whose income was above SNAP’s income limits experienced difficulty affording food, stating that the requirements for eligibility had not been updated despite fluctuations in the economy [56]. Similarly, another study suggested that households that failed to renew SNAP benefits find it challenging to comply with the administrative burden associated with the process or are restricted by the demanding work obligations that limit their flexibility to keep appointments [49].
Similarly, findings from this review suggest the socioeconomic status of these households, often affected by high levels of unemployment, limited job opportunities, and eligibility requirements related to food and financial assistance, contribute to increased food insecurity levels [33, 36, 45, 57, 58]. One qualitative article mentioned a mother who described job loss as a “crisis,” explaining that unemployment often causes families to limit purchases to basic necessities [36].
Although this review did not focus on the contributing factors affecting Hispanic/Latinx households of undocumented immigrants, employment opportunities, and access to supplemental food assistance may depend on immigration status. Furthermore, studies from this review also identified that COVID-19 restrictions prevented many individuals from accessing secure and stable employment, consequently impacting their income status and contributing to food insecurity within this population [34, 52]
What is the current state of the evidence related to the contributing factors to food insecurity in Hispanic/Latinx households with children under the age of three based on the levels of the SEM?
Findings from this review reinforce evidence from previous literature suggesting that research has mainly focused on exploring the individual-level and policy-level factors contributing to food insecurity in this population [[77], [78], [79]]. For instance, various individual level factors (i.e., income level, education level, marital status, language proficiency, acculturation level, nutrition knowledge, and food preferences) were identified as contributors to food insecurity in Hispanic/Latinx households with young children [33, [35], [36], [37], 39, 42, 43, 45, 47, 54, 57, 58]. Further, some individual or interpersonal level factors are unique and more common in Hispanic/Latinx families compared with non-Hispanic families, including intergenerational poverty, the practice of sending funds to family outside the USA, thereby creating additional financial constraints, lack of English proficiency, lower education level (e.g., high school or less), higher likelihood of a single parent household, cultural customs and traditions impacting food access or choice, and limited social support if separated from family.
Similarly, articles focusing on policy-level factors mainly discussed barriers regarding eligibility and participation in federal assistance programs and unemployment-related issues [[34], [35], [36], 38, 42, 48, 74]. However, it is important to note that participation in federal assistance programs (policy-level factor) is likely also impacted by individual characteristics such as education level and lack of English proficiency, which is more common in Hispanic/Latinx families.
Moreover, this review supports prior research findings that report individual level factors such as limited financial resources or low-income as leading contributors to food insecurity [9, 61, [80], [81], [82], [83]]. For example, several studies within this review reported that the limited amount of money allocated for food often determines adequate access to and availability of higher quality and quantity of nutrient-dense foods (i.e., fruits, vegetables, protein foods, etc.) compared with ultra-processed foods (i.e., high in saturated and trans-fat, added sugar, and sodium) [36, 37, 42, 54, 57, 58]. Prior studies examining the association between household food insecurity and income level have reported that children living in under-resourced households consumed less nutrient-dense foods and were at a higher risk of developing diet-related health issues compared with households who were not low-income [9, 61, [80], [81], [82], [83]].
In addition, studies exploring other individual level factors contributing to the association between food insecurity and diet quality in early childhood have also reported the influence of lack of nutrition education (i.e., including food resource management knowledge and cooking skills) with a household’s supply of nutrient-dense foods (i.e., fruits and vegetables) [84, 85]. Several articles within this review reported the need to develop nutrition education interventions with basic nutrition content and topics related to food shopping, budgeting, meal planning, food preparation skills, and caregiver feeding guidelines [35, 36, 39, 40, 42, 45, 47, 48]. Food resource management training was also reported as a crucial component to foster the skills these families need to save money on groceries, reduce food waste, prevent worrying about running out of food, and increase self-confidence and self-efficacy in purchasing adequate foods for all household members at an affordable price [39, 86].
When considering interpersonal factors impacting food security in Hispanic/Latinx households with young children, this review found that social networks are important to accessing consistent, reliable transportation [[34], [35], [36], [37], 44, 45]. Prior research supports this finding suggesting individuals experiencing transportation challenges often feel they are inconveniencing others when asking for a ride to grocery stores and other food distribution locations [68, 87]. During the COVID-19 pandemic, families who relied on social networks to access transportation or childcare support could not utilize this niche as community support [34]. This new challenge added stress for caregivers in households who depended on these social networks to make ends meet for themselves and their children.
Although, one study found intergenerational poverty as a contributing interpersonal factor to food insecurity unique to underrepresented minorities, including Hispanic/Latinx households with children under three [35, 38], previous studies exploring the effects of intergenerational poverty suggest food insecurity can be grounded in other prior experiences across the life course and learning [88, 89]. Social and economic deprivation during childhood and adolescence can have a lasting effect on individuals, making it difficult for children who grow up in low-income families to escape poverty when they become adults. Interventions are needed to create community connections and health promotion opportunities to address the social, economic, and health risk factors associated with food insecurity. This is important while increasing knowledge, access, and consumption of healthy foods in families with young children [90].
Although the articles selected for this review frequently focused on the individual or policy-level factors associated with food security, other factors also significantly contribute to food insecurity in Hispanic/Latinx households with children under three. Findings from this review suggest that community-based organizations should work together more frequently to connect families to services and improve access to healthy and affordable foods [91, 92]. Instead, of competing initiatives, community organizations should strive to improve interagency communication and collaboration, rallying leaders around the common goal of reducing hunger and food insecurity within this population [91, 92]. In addition, organizations must deliver culturally and linguistically responsive services and resources to reduce existing gaps to build healthy and resilient communities [38, 44].
Previous research assessing low-income families has also found that the proximity of food or grocery stores is essential for purchasing food items for the household [93]. Therefore, if a neighborhood lacks stores with a vast supply of healthful food items and/or does not have eligible stores that accept WIC or SNAP benefits, household members are limited in the number of food-purchasing locations where affordable and healthy foods may be available to them. This is especially important for families with young children who may need infant formula or other age-appropriate foods. Many residents, therefore, rely on small corner stores and bodegas for most food purchases in neighborhoods that lack access to grocery stores [94, 95]. Unfortunately, these options often sell predominantly ultra-processed, nutrient-poor foods and little or no fresh produce [95, 96]. The spatial context, such as an individual’s environment, may help shape how a household copes with food insecurity, whether through altering shopping behavior, finding additional work opportunities, or seeking assistance [97]. Thus, strategies to expand healthy food offerings in under-resourced communities are needed to improve food security among Hispanic/Latinx households with children under three.
Overall, although the findings from this review examined several studies targeting Hispanic/Latinx households with children under three, prior research related to determinants of food insecurity has also focused on school-aged children and adolescents [8, 23]. Likewise, studies exploring the association between food insecurity and underrepresented racial and ethnic groups are limited and have focused on exploring factors associated with food insecurity within a specific or combination of racial and ethnic groups (i.e., African Americans, Asians, and Hispanics) [67, 98, 99]. This is relevant given several studies within this review found that low acculturation plays an important role in accessing healthy foods [40, 41, 45, 54]. Previous research suggests low acculturation in adults has been associated with lower language proficiency, socioeconomic status, and level of education, creating additional knowledge and communication barriers for individuals to access governmental and charitable assistance [67, 100, 101].
Research gaps and future directions
Future research should further explore the identified factors unique to Hispanic/Latinx households with children under three that contribute to food insecurity. These factors include examples such as intergenerational poverty, lower education level, lack of English proficiency, household composition, cultural traditions, social support, self-perceived stigma, or hesitancy in accepting government benefits, and administrative burden of applying for benefits.
In addition, culturally sensitive and linguistically appropriate nutrition education and food assistance resources and services are needed for Hispanic/Latinx families with young children. As previously mentioned, acculturation and language barriers have been associated with food insecurity. Although some existing resources and services are translated into other languages, including Spanish, there is a need to improve and expand access to and availability of culturally sensitive and linguistically appropriate information [59]. Previous research has found that improved cultural competence and sensitivity also increase the level of connectedness and trust within the community [38, 44]. Thus, developing culturally responsive approaches that promote financial management, reduce the stigma associated with participation in nutrition assistance programs, and assist families in applying for food assistance should be considered an essential step toward improving food and nutrition security in this population.
Furthermore, novel, and adapted strategies should consider the unique needs and characteristics of Hispanic/Latinx population subgroups based on country of origin or geographic location. Based on the findings from the articles selected for this review, groups from different countries of origin (i.e., Mexico, Puerto Rico, etc.) expressed different needs and barriers to food insecurity [35, 38, 42, 45, 74]. Previous research has found that tailoring interventions to the unique characteristics and needs of target groups within the population also contributes to the positive integration of community members and improved diet-related behaviors [38, 44, [102], [103], [104]].
Future state and federal economic policies should also evaluate long-term eligibility means-tested benefit programs, particularly food assistance programs, to reduce poverty and mitigate food insecurity in this population. Although low-income Hispanic/Latinx families believe food assistance programs are essential for mitigating the effects of food insecurity, these programs are not always available or utilized because of the associated stigma, current policy restrictions, and eligibility limitations (i.e., immigration status, benefits cliffs, income limits, etc.). Although the majority of articles reviewed contained medium or high-quality evidence, even when examining them by SEM level, future research should focus on exploring the policy, systems, and environmental factors contributing to food security in this population given the potential larger scale impact and that some of the studies focused on this level of the SEM were ranked low with regards of strength of evidence, or were reports found in gray literature.
Finally, research should explore the interplay among factors impacting food security across multiple levels of influence (i.e., policy, community, organizational, interpersonal, and individual) rather than only one influence level. Exploring the determinants at multiple levels of influence can help inform and improve existing practices and policy-based strategies addressing access to age-appropriate and nutritionally adequate foods for all members of the households, specifically for children under three, and promoting health equity [73, 77, 105]. For instance, future research could evaluate how culturally and linguistically appropriate nutrition and food resource management education, interagency community collaborations to connect families to all eligible resources and services, and policy change to reduce the burden to apply for benefits and increase benefit amount, impacts household food security in Hispanic/Latinx families with young children.
Limitations
Although this narrative review highlights the need to strengthen the current body of literature on food insecurity among Hispanic/Latinx underserved households with children under three, some of the studies selected for this review lack consistency in evaluation tools to measure food insecurity, including different modes of analysis (i.e., quantitative vs. qualitative) and target specific groups within the Hispanic/Latinx community which hinders generalization of results. For instance, this review was limited to US states where research excluded risk factors associated with food insecurity among migrant workers and undocumented immigrants living in Hispanic/Latinx households. Further, because this was a narrative review with a specific review process, a second reviewer was not included in the process, potentially introducing bias. Finally, although this narrative review rated the strength of the evidence of each article, additional elements should be included in the grading system, including the quantity and consistency of the evidence provided in the selected studies [32].
In conclusion, although the associations between food security and early childhood have been previously studied, additional research and policy considerations are still needed to understand the barriers and opportunities that affect minority populations, specifically Hispanic/Latinx households with children under three. Using the SEM as a framework, this review revealed that most of the articles included factors at the individual (i.e., education level, income level, socioeconomic status, acculturation level, nutrition knowledge/skills, etc.) or factors at the policy, systems or environmental levels (i.e., supplemental nutrition programs, benefits cliffs, etc.) of the SEM with the less research at the community level or containing all SEM levels. Further, more than half of the articles in the review were rated at the “medium” level of evidence indicating that more research and rigor may be needed.
Recommendations include developing or adapting culturally and linguistically appropriate interventions for Hispanic/Latinx families with young children at multiple levels of the SEM to improve food security. This will require commitment from key stakeholders, thought leaders, and collaborations across communities, organizations, sectors, and public policy.
Author disclosures
The authors report no conflicts of interest.
Acknowledgments
The authors’ responsibilities were as follows—EGV completed the search and review process, retrieved and reviewed articles, extracted data, interpreted results, wrote the initial manuscript draft, and revised the final version; ARM conceptualized the topic, assisted with major revisions and edits; ARM, KPG, and MAM assisted the previously cited author in designing the structure of the manuscript and in reviewing the final content, and all authors read and approved the final manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.advnut.2022.12.001.
Funding
The authors reported no funding received for this study.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Nutrition and Healthy Eating . Office of Disease Prevention and Health Promotion; Washington, DC: 2021. U.S. Department of Health and Human.https://health.gov/healthypeople/objectives-and-data/browse-objectives/nutrition-and-healthy-eating [Internet] [date updated, date cited] [Google Scholar]
- 2.Coleman-Jensen A., Rabbitt M.P., Gregory A.C., Singh A. U.S. Department of Agriculture, Economic Research Service [Internet]; 2021. Household Food Security in the United States in 2020.https://www.ers.usda.gov/webdocs/publications/102076/err-298.pdf?v=2916.7 [date updated, date cited] [Google Scholar]
- 3.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolfson J.A., Leung C.W. Food insecurity and COVID-19: disparities in early effects for US adults. Nutrients. 2020;12(6) doi: 10.3390/nu12061648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez C., Crowder S.L., Rodriguez M., Redwine L., Stern M. Food insecurity and the Hispanic population during the COVID-19 pandemic. Ecol Food Nutr. 2021;60(5):548–563. doi: 10.1080/03670244.2021.1974014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rabbitt M., Smith M., Coleman-Jensen A. Amber Waves; Washington DC: 2016. Food insecurity and Hispanic diversity. 2015–06. [Google Scholar]
- 7.Ke J., Ford-Jones E.L. Food insecurity and hunger: a review of the effects on children’s health and behaviour. Paediatr Child Health. 2015;20(2):89–91. doi: 10.1093/pch/20.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Larson N.I., Story M.T. Food insecurity and weight status among U.S. children and families: a review of the literature. Am J Prev Med. 2011;40(2):166–173. doi: 10.1016/j.amepre.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 9.Schmeer K.K., Piperata B.A. Household food insecurity and child health. Matern Child Nutr. 2017;13(2) doi: 10.1111/mcn.12301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carmichael S.L., Yang W., Herring A., Abrams B., Shaw G.M. Maternal food insecurity is associated with increased risk of certain birth defects. J Nutr. 2007;137(9):2087–2092. doi: 10.1093/jn/137.9.2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skalicky A., Meyers A.F., Adams W.G., Yang Z., Cook J.T., Frank D.A. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J. 2006;10(2):177–185. doi: 10.1007/s10995-005-0036-0. [DOI] [PubMed] [Google Scholar]
- 12.Howard L.L. Does food insecurity at home affect non-cognitive performance at school? A longitudinal analysis of elementary student classroom behavior. Econ Educ Rev. 2011;30(1):157–176. [Google Scholar]
- 13.Whitaker R.C., Phillips S.M., Orzol S.M. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–e868. doi: 10.1542/peds.2006-0239. [DOI] [PubMed] [Google Scholar]
- 14.Cusick S.E., Georgieff M.K. The role of nutrition in brain development: the golden opportunity of the “first 1000 days.”. J Pediatr. 2016;175:16–21. doi: 10.1016/j.jpeds.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benjamin Neelon S.E., Burgoine T., Gallis J.A., Monsivais P. Spatial analysis of food insecurity and obesity by area-level deprivation in children in early years settings in England. Spat Spatiotemporal Epidemiol. 2017:1–9. doi: 10.1016/j.sste.2017.07.001. Edition 23. Netherlands: Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson A.D., Markowitz A.J. Associations between household food insecurity in early childhood and children’s kindergarten skills. Child Dev. 2018;89(2):e1–17. doi: 10.1111/cdev.12764. [DOI] [PubMed] [Google Scholar]
- 17.Brown A.G.M., Esposito L.E., Fisher R.A., Nicastro H.L., Tabor D.C., Walker J.R. Food insecurity and obesity: research gaps, opportunities, and challenges. Transl Behav Med. 2019;9(5):980–987. doi: 10.1093/tbm/ibz117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Office of Disease Prevention and Health Promotion . U.S. Department of Health and Human Services; Washington, DC: 2021. Social Determinants of Health.https://health.gov/healthypeople/objectives-and-data/social-determinants-health Internet. date updated, date cited. [Google Scholar]
- 19.Banks A.R., Bell B.A., Ngendahimana D., Embaye M., Freedman D.A., Chisolm D.J. Identification of factors related to food insecurity and the implications for social determinants of health screenings. BMC Public Health. 2021;21(1):1410. doi: 10.1186/s12889-021-11465-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanson K.L., Connor L.M. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr. 2014;100(2):684–692. doi: 10.3945/ajcn.114.084525. [DOI] [PubMed] [Google Scholar]
- 21.Murthy V.H. Food insecurity: a public health issue. Public Health Rep. 2016;131(5):655–657. doi: 10.1177/0033354916664154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hartline-Grafton H., Dean O. Food Research & Action Center; 2017. The Impact of Poverty, Food Insecurity, and Poor Nutrition on Health and Well-Being.https://frac.org/wp-content/uploads/hunger-health-impact-poverty-food-insecurity-health-well-being.pdf Internet. [date updated, date cited] [Google Scholar]
- 23.Gundersen C., Ziliak J.P. Food Insecurity And Health Outcomes. Health Aff (Millwood) 2015;34(11):1830–1839. doi: 10.1377/hlthaff.2015.0645. [DOI] [PubMed] [Google Scholar]
- 24.Gross R.S., Mendelsohn A.L. Food insecurity during early childhood: marker for disparities in healthy growth and development. Pediatrics. 2019;144(4) doi: 10.1542/peds.2019-2430. [DOI] [PubMed] [Google Scholar]
- 25.Gallegos D., Eivers A., Sondergeld P., Pattinson C. Food insecurity and child development: a state-of-the-art review. Int J Environ Res Public Health. 2021;18(17):8990. doi: 10.3390/ijerph18178990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pereira M.M.C.E., Padez C.M.P., Nogueira H.G.D.S.M. Describing studies on childhood obesity determinants by Socio-Ecological Model level: a scoping review to identify gaps and provide guidance for future research. Int J Obes (Lond). 2019;43(10):1883–1890. doi: 10.1038/s41366-019-0411-3. [DOI] [PubMed] [Google Scholar]
- 27.Glanz K., Rimer B.K., Viswanath K. Fifth Edition. Jossey-Bass/Wiley; 2015. Health Behavior: Theory, Research, and Practice. [Google Scholar]
- 28.Pinstrup-Andersen P. Food security: definition and measurement. Food Secur. 2009;1(1):5–7. [Google Scholar]
- 29.Carballo M., Nerukar A. Migration, refugees, and health risks. Emerg Infect Dis. 2001;7(3 Suppl):556–560. doi: 10.3201/eid0707.017733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holmes S.M. An ethnographic study of the social context of migrant health in the United States. PLOS Med. 2006;3(10):e448. doi: 10.1371/journal.pmed.0030448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Covidence systematic review software Melbourne [Internet]. Australia: Veritas Health Innovation. [date updated, date cited] www.covidence.org.
- 32.West S., King V., Carey T.S., Lohr K.N., McKoy N., Sutton S.F., et al. Agency for Healthcare Research and Quality; 2002. Systems to rate the strength of scientific evidence: Summary. AHRQ evidence report summaries. [PMC free article] [PubMed] [Google Scholar]
- 33.Himmelgreen D.A., Pérez-Escamilla R., Segura-Millán S., Peng Y.K., Gonzalez A., Singer M., et al. Food insecurity among low-income Hispanics in Hartford, Connecticut: implications for public health policy. Hum Organ. 2000;59(3):334–342. [Google Scholar]
- 34.Abrams S.A., Avalos A., Gray M., Hawthorne K.M. High level of food insecurity among families with children seeking routine care at federally qualified health centers during the coronavirus disease 2019 pandemic. J Pediatr X. 2020;4 doi: 10.1016/j.ympdx.2020.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bermúdez-Millán A., Damio G., Cruz J., D’Angelo K., Segura-Pérez S., Hromi-Fiedler A., et al. Stress and the social determinants of maternal health among Puerto Rican women: a CBPR approach. J Health Care Poor Underserved. 2011;22(4):1315–1330. doi: 10.1353/hpu.2011.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gross R.S., Mendelsohn A.L., Arana M.M., Messito M.J. Food insecurity during pregnancy and breastfeeding by low-income Hispanic mothers. Pediatrics. 2019;143(6) doi: 10.1542/peds.2018-4113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lindsay A.C., Sussner K.M., Greaney M.L., Peterson K.E. Influence of social context on eating, physical activity, and sedentary behaviors of Latina mothers and their preschool-age children. Health Educ Behav. 2009;36(1):81–96. doi: 10.1177/1090198107308375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pineros-Leano M., Tabb K., Liechty J., Castañeda Y., Williams M. Feeding decision-making among first generation Latinas living in non-metropolitan and small metro areas. PLOS ONE. 2019;14(3) doi: 10.1371/journal.pone.0213442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nederveld A., Phimphasone-Brady P., Marshall B., Bayliss E. Attitudes and knowledge regarding health-promoting behavior in families facing food insecurity. Pers Med. 2021;25:21. doi: 10.7812/TPP/21.011. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berg J., Tiso S., Grasska M., Tan E., Chowdhury Y., Zender R., Knudtson M. Obesity, parent perceptions, child feeding, and food security in first generation Hispanic families. Calif J Health Promot. 2013;11(3):86–92. [Google Scholar]
- 41.Buscemi J., Beech B.M., Relyea G. Predictors of obesity in Latino children: acculturation as a moderator of the relationship between food insecurity and body mass index percentile. J Immigr Minor Health. 2011;13(1):149–154. doi: 10.1007/s10903-009-9263-6. [DOI] [PubMed] [Google Scholar]
- 42.Chávez N., Telleen S., Kim Y.O. Food insufficiency in urban Latino families. J Immigr Minor Health. 2007;9(3):197–204. doi: 10.1007/s10903-006-9032-8. [DOI] [PubMed] [Google Scholar]
- 43.Chilton M., Black M.M., Berkowitz C., Casey P.H., Cook J., Cutts D., et al. Food insecurity and risk of poor health among US-born children of immigrants. Am J Public Health. 2009;99(3):556–562. doi: 10.2105/AJPH.2008.144394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Denney J.T., Brewer M., Kimbro R.T. Food insecurity in households with young children: A test of contextual congruence. Soc Sci Med. 2020;263 doi: 10.1016/j.socscimed.2020.113275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dhokarh R., Himmelgreen D.A., Peng Y.K., Segura-Pérez S., Hromi-Fiedler A., Pérez-Escamilla R. Food insecurity is associated with acculturation and social networks in Puerto Rican households. J Nutr Educ Behav. 2011;43(4):288–294. doi: 10.1016/j.jneb.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaiser L.L., Melgar-Quinoñez H., Townsend M.S., Nicholson Y., Fujii M.L., Martin A.C., et al. Food insecurity and food supplies in Latino households with young children. J Nutr Educ Behav. 2003;35(3):148–153. doi: 10.1016/s1499-4046(06)60199-1. [DOI] [PubMed] [Google Scholar]
- 47.Kamdar N., Hughes S.O., Chan W., Power T.G., Meininger J. Indirect effects of food insecurity on body mass index through feeding style and dietary quality among low-income Hispanic preschoolers. J Nutr Educ Behav. 2019;51(7):876–884. doi: 10.1016/j.jneb.2019.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sharkey J.R., Dean W.R., Nalty C.C. Child hunger and the protective effects of Supplemental Nutrition Assistance Program (SNAP) and alternative food sources among Mexican-origin families in Texas border colonias. BMC Pediatr. 2013;13:143. doi: 10.1186/1471-2431-13-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arteaga I., Hodges L., Heflin C. Giving kids a boost: the positive relationship between frequency of SNAP participation and infant’s preventative health care utilization. SSM Popul Health. 2021;15 doi: 10.1016/j.ssmph.2021.100910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McCurdy K., Gans K.M., Risica P.M., Fox K., Tovar A. Food insecurity, food parenting practices, and child eating behaviors among low-income Hispanic families of young children. Appetite. 2022;169 doi: 10.1016/j.appet.2021.105857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ventura A.K., Martinez C.E., Whaley S.E. WIC participants’ perceptions of COVID-19-related changes to WIC recertification and service delivery. J Community Health. 2022;47(2):184–192. doi: 10.1007/s10900-021-01026-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Steimle S., Gassman-Pines A., Johnson A.D., Hines C.T., Ryan R.M. Understanding patterns of food insecurity and family well-being amid the COVID-19 pandemic using daily surveys. Child Dev. 2021;92(5):e781–e797. doi: 10.1111/cdev.13659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnson K.A., Jones-Smith J., Curriero F.C., Cheskin L.J., Benjamin-Neelon S.E., Perin J., et al. Low-income black and Hispanic children’s neighborhood food environments and weight trajectories in early childhood. Acad Pediatr. 2020;20(6):784–792. doi: 10.1016/j.acap.2019.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Innella N., Breitenstein S., Hamilton R., Reed M., McNaughton D.B. Determinants of obesity in the Hispanic preschool population: an integrative review. Public Health Nurs. 2016;33(3):189–199. doi: 10.1111/phn.12215. [DOI] [PubMed] [Google Scholar]
- 55.Ochoa A., Berge J.M. Home environmental influences on childhood obesity in the latino population: a decade review of literature. J Immigr Minor Health. 2017;19(2):430–447. doi: 10.1007/s10903-016-0539-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Keith-Jennings B., Nchako C., Llobrera J. The Center on Budget and Policy Priorities; Washington, DC: 2021. Number of Families Struggling to Afford Food Rose Steeply in Pandemic and Remains High, Especially Among Children and Households of Color. [Google Scholar]
- 57.Schanzenbach, D. W., & A. Pitts. (2020, July 9). Food Insecurity during COVID-19 in households with children: Results by racial and ethnic groups. Institute for Policy Research Rapid Research Report. https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-9-july-2020-by-race-ethnicity.pdf.
- 58.Escobar M., Mendez A.D., Encinas M.R., Villagomez S., Wojcicki J.M. High food insecurity in Latinx families and associated COVID-19 infection in the Greater Bay Area, California. BMC Nutr. 2021;7(1):23. doi: 10.1186/s40795-021-00419-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.González A. Center for Primary Care: Harvard Medical School; 2020. COVID-19 Exacerbates Food Insecurity in Latino Children & Families.https://info.primarycare.hms.harvard.edu/blog/covid-food-insecurity-latino Internet. [July 23rd, 2020 Accessed: 13 Apr 2022] [Google Scholar]
- 60.Kaiser L.L., Melgar-Quiñonez H.R., Lamp C.L., Johns M.C., Sutherlin J.M., Harwood J.O. Food security and nutritional outcomes of preschool-age Mexican-American children. J Am Diet Assoc. 2002;102(7):924–929. doi: 10.1016/s0002-8223(02)90210-5. [DOI] [PubMed] [Google Scholar]
- 61.Gross R.S., Mendelsohn A.L., Gross M.B., Scheinmann R., Messito M.J. Material hardship and internal locus of control over the prevention of child obesity in low-income Hispanic pregnant women. Acad Pediatr. 2016;16(5):468–474. doi: 10.1016/j.acap.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Maynard M., Dean J., Rodriguez P.I., Sriranganathan G., Qutub M., Kirkpatrick S.I. The experience of food insecurity among immigrants: a scoping review. J Int Migr Integr. 2019;20(2):375–417. [Google Scholar]
- 63.Quandt S.A., Shoaf J.I., Tapia J., Hernández-Pelletier M., Clark H.M., Arcury T.A. Experiences of Latino immigrant families in North Carolina help explain elevated levels of food insecurity and hunger. J Nutr. 2006;136(10):2638–2644. doi: 10.1093/jn/136.10.2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Berry J.W. Psychology Press/Erlbaum Taylor & Francis; United Kingdom: 2005. Acculturation. Culture and human development: The importance of cross-cultural research for the social sciences; pp. 291–302. [Google Scholar]
- 65.Monterrosa E.C., Frongillo E.A., Drewnowski A., de Pee S., Vandevijvere S. Sociocultural influences on food choices and implications for sustainable healthy diets. Food Nutr Bull. 2020;41(2_suppl):59S–73S. doi: 10.1177/0379572120975874. [DOI] [PubMed] [Google Scholar]
- 67.Myers A.M., Painter M.A. Food insecurity in the United States of America: an examination of race/ethnicity and nativity. Food Sec. 2017;9(6):1419–1432. [Google Scholar]
- 68.Keller H.H., Dwyer J.J.M., Senson C., Edwards V., Edward G. A Social ecological perspective of the influential factors for food access described by low-income seniors. J Hunger Environ Nutr. 2007;1(3):27–44. [Google Scholar]
- 69.Andress L., Fitch C. Juggling the five dimensions of food access: perceptions of rural low income residents. Appetite. 2016;105:151–155. doi: 10.1016/j.appet.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 70.Bertmann F.M., Barroso C., Ohri-Vachaspati P., Hampl J.S., Sell K., Wharton C.M. Women, infants, and children cash value voucher (CVV) use in Arizona: a qualitative exploration of barriers and strategies related to fruit and vegetable purchases. J Nutr Educ Behav. 2014;46(3 Suppl):S53–S58. doi: 10.1016/j.jneb.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 71.Haynes-Maslow L., Auvergne L., Mark B., Ammerman A., Weiner B.J. Low-income individuals’ perceptions about fruit and vegetable access programs: a qualitative study. J Nutr Educ Behav. 2015;47(4):317–324. doi: 10.1016/j.jneb.2015.03.005. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Quandt S.A., Arcury T.A., Early J., Tapia J., Davis J.D. Household food security among migrant and seasonal Latino farmworkers in North Carolina. Public Health Rep. 2004;119(6):568–576. doi: 10.1016/j.phr.2004.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Seligman H.K., Berkowitz S.A. Aligning programs and policies to support food security and public health goals in the United States. Ann Rev Public Health. 2019;40:319. doi: 10.1146/annurev-publhealth-040218-044132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sharkey J.R., Dean W.R., Johnson C.M. Association of household and community characteristics with adult and child food insecurity among Mexican-Origin Households in Colonias along the Texas-Mexico border. Int J Equity Health. 2011;10:19. doi: 10.1186/1475-9276-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lubbers M.J., García H.V., Castaño P.E., Molina J.L., Casellas A., Rebollo J.G. Relationships stretched thin: social support mobilization in poverty. Ann Am Acad Polit Soc Sci. 2020;689(1):65–88. [Google Scholar]
- 76.Stahel A.W. Why are the rich getting richer while the poor stay poor? Real-World Econ Rev. 2020;93:113–131. [Google Scholar]
- 77.Fleischhacker S., Parks C.A., Yaroch A.L. Addressing food insecurity in the United States: the role of policy, systems changes, and environmental supports. Transl Behav Med. 2019;9(5):827–836. doi: 10.1093/tbm/ibz131. [DOI] [PubMed] [Google Scholar]
- 78.Keenan G.S., Christiansen P., Hardman C.A. Household food insecurity, diet quality, and obesity: an explanatory model. Obesity (Silver Spring) 2021;29(1):143–149. doi: 10.1002/oby.23033. [DOI] [PubMed] [Google Scholar]
- 79.Brown A.F., Ma G.X., Miranda J., Eng E., Castille D., Brockie T., et al. Structural interventions to reduce and eliminate health disparities. Am J Public Health. 2019;109(S1):S72–S78. doi: 10.2105/AJPH.2018.304844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bronte-Tinkew J., Zaslow M., Capps R., Horowitz A., McNamara M. Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. J Nutr. 2007;137(9):2160–2165. doi: 10.1093/jn/137.9.2160. [DOI] [PubMed] [Google Scholar]
- 81.Frank D.A., Neault N.B., Skalicky A., Cook J.T., Wilson J.D., Levenson S., et al. Heat or eat: the Low Income Home Energy Assistance Program and nutritional and health risks among children less than 3 years of age. Pediatrics. 2006;118(5):e1293–e1302. doi: 10.1542/peds.2005-2943. [DOI] [PubMed] [Google Scholar]
- 82.Metallinos-Katsaras E., Sherry B., Kallio J., Hernandez D.C., Jacknowitz A., Park K., et al. Food insecurity is associated with overweight in children younger than 5 years of age. J Am Diet Assoc. 2009;109(10):1790–1794. doi: 10.1016/j.jada.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 83.Hernandez D.C., Jacknowitz A. Transient, but not persistent, adult food insecurity influences toddler development. J Nutr. 2009;139(8):1517–1524. doi: 10.3945/jn.109.105593. [DOI] [PubMed] [Google Scholar]
- 84.Hoisington A., Shultz J.A., Butkus S. Coping strategies and nutrition education needs among food pantry users. J Nutr Educ Behav. 2002;34(6):326–333. doi: 10.1016/s1499-4046(06)60115-2. [DOI] [PubMed] [Google Scholar]
- 85.Simmet A., Depa J., Tinnemann P., Stroebele-Benschop N. The dietary quality of food pantry users: a systematic review of existing literature. J Acad Nutr Diet. 2017;117(4):563–576. doi: 10.1016/j.jand.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 86.Pooler J.A., Morgan R.E., Wong K., Wilkin M.K., Blitstein J.L. Cooking matters for adults improves food resource management skills and self-confidence among low-income participants. J Nutr Educ Behav. 2017;49(7):545–553. doi: 10.1016/j.jneb.2017.04.008. e1. [DOI] [PubMed] [Google Scholar]
- 87.Andress L. Using a social ecological model to explore upstream and downstream solutions to rural food access for the elderly. Cogent Med. 2017;4(1) [Google Scholar]
- 88.Chilton M., Chyatte M., Breaux J. The negative effects of poverty & food insecurity on child development. Indian J Med Res. 2007;126(4):262–272. [PubMed] [Google Scholar]
- 89.Harper C., Marcus R., Moore K. Enduring poverty and the conditions of childhood: lifecourse and intergenerational poverty transmissions. World Dev. 2003;31(3):535–554. [Google Scholar]
- 90.Jarrott S.E., Cao Q., Dabelko-Schoeny H.I., Kaiser M.L. Developing intergenerational interventions to address food insecurity among pre-school children: a community-based participatory approach. J Hunger Environ Nutr. 2021;16(2):196–212. [Google Scholar]
- 91.Macias T. Working toward a just, equitable, and local food system: the social impact of community-based agriculture. Soc Sci Q. 2008;89(5):1086–1101. [Google Scholar]
- 92.Plough A.L. Building a culture of health: a critical role for public health services and systems research. Am Public Health Assoc. 2015;105:S150–S152. doi: 10.2105/AJPH.2014.302410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gittelsohn J., Laska M.N., Andreyeva T., Foster G., Rose D., Tester J., et al. Small retailer perspectives of the 2009 women, infants and children program food package changes. Am J Health Behav. 2012;36(5):655–665. doi: 10.5993/AJHB.36.5.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dannefer R., Williams D.A., Baronberg S., Silver L. Healthy bodegas: increasing and promoting healthy foods at corner stores in New York City. Am J Public Health. 2012;102(10):e27–31. doi: 10.2105/AJPH.2011.300615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.O'Malley K., Gustat J., Rice J., Johnson C.C. Feasibility of increasing access to healthy foods in neighborhood corner stores. J Commun Health. 2013;38(4):741–749. doi: 10.1007/s10900-013-9673-1. [DOI] [PubMed] [Google Scholar]
- 96.DeMartini T.L., Beck A.F., Kahn R.S., Klein M.D. Food insecure families: description of access and barriers to food from one pediatric primary care center. J Community Health. 2013;38(6):1182–1187. doi: 10.1007/s10900-013-9731-8. [DOI] [PubMed] [Google Scholar]
- 97.Allard S.W., Wathen M.V., Danziger S.K. The spatial context of food assistance: examining local food assistance environment in the context of SNAP. J Hunger Environ Nutr. 2021:1–20. [Google Scholar]
- 98.Hernandez D.C., Reesor L.M., Murillo R. Food insecurity and adult overweight/obesity: gender and race/ethnic disparities. Appetite. 2017;117:373–378. doi: 10.1016/j.appet.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 99.Bartfeld J.S., Ryu J.-H., Wang L. Local characteristics are linked to food insecurity among households with elementary school children. J Hunger Environ Nutr. 2010;5(4):471–483. [Google Scholar]
- 100.Kamimura A., Jess A., Trinh H.N., Aguilera G., Nourian M.M., Assasnik N., et al. Food insecurity associated with self-efficacy and acculturation. Popul Health Manag. 2017;20(1):66–73. doi: 10.1089/pop.2015.0179. [DOI] [PubMed] [Google Scholar]
- 101.Pérez-Escamilla R. Dietary quality among Latinos: is acculturation making us sick? J Am Diet Assoc. 2009;109(6):988–991. doi: 10.1016/j.jada.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hammons A.J., Hannon B.A., Teran-Garcia M., Barragan M., Villegas E., Wiley A., et al. Effects of culturally tailored nutrition education on dietary quality of Hispanic mothers: a randomized control trial. J Nutr Educ Behav. 2019;51(10):1168–1176. doi: 10.1016/j.jneb.2019.06.017. [DOI] [PubMed] [Google Scholar]
- 103.Evans A., Chow S., Jennings R., Dave J., Scoblick K., Sterba K.R., Loyo J. Traditional foods and practices of Spanish-speaking Latina mothers influence the home food environment: implications for future interventions. J Am Diet Assoc. 2011;111(7):1031–1038. doi: 10.1016/j.jada.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 104.Broyles S.L., Brennan J.J., Burke K.H., Kozo J., Taras H.L. Cultural adaptation of a nutrition education curriculum for Latino families to promote acceptance. J Nutr Educ Behav. 2011;43(4 Suppl 2):S158–S161. doi: 10.1016/j.jneb.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bleich S.N., Moran A.J., Vercammen K.A., Frelier J.M., Dunn C.G., Zhong A., et al. Strengthening the public health impacts of the Supplemental Nutrition Assistance Program through policy. Ann Rev Public Health. 2020;41:453–480. doi: 10.1146/annurev-publhealth-040119-094143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.