Abstract
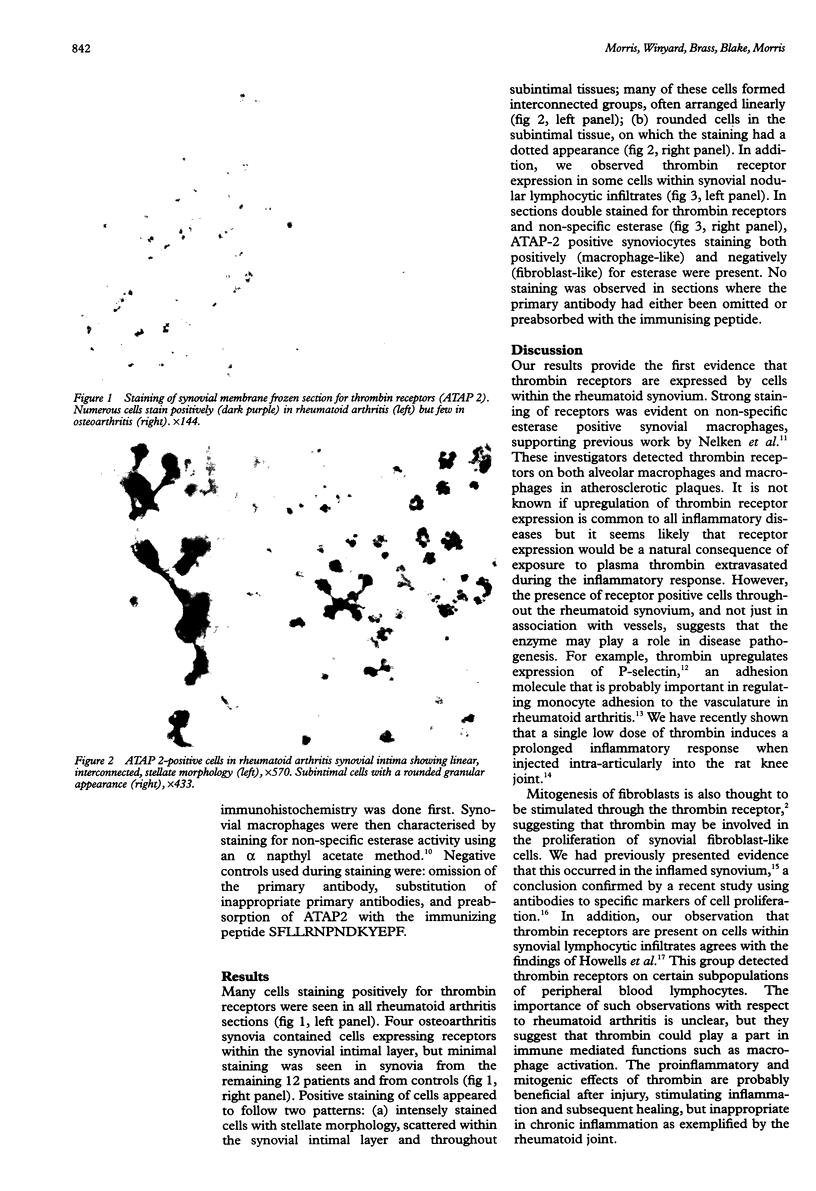
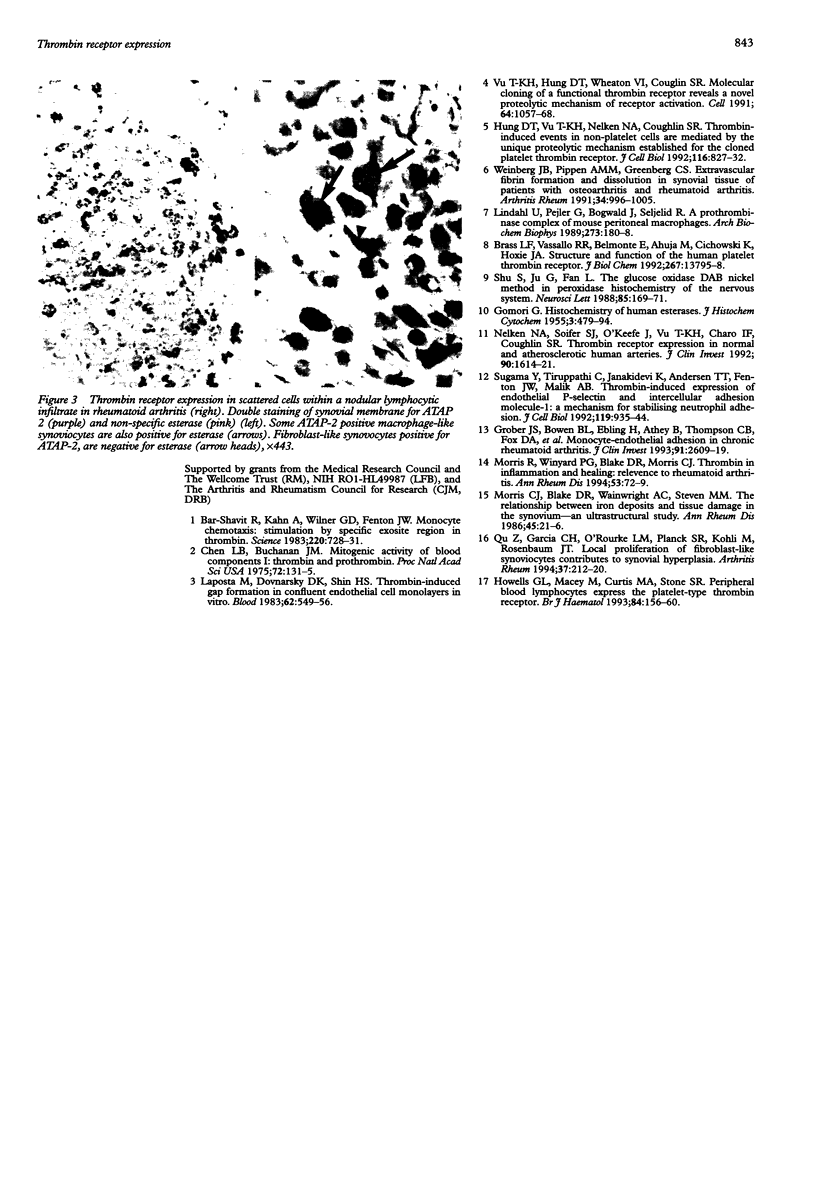
OBJECTIVE: To investigate the possibility that synovial cells might respond to thrombin in the inflamed human joint, using immunohistochemical detection of thrombin receptors. METHODS: Frozen sections of synovial membrane from 20 patients with rheumatoid arthritis, 16 with osteoarthritis, and four normal controls were stained using a monoclonal antibody to the human thrombin receptor. Sections were also double stained for both receptors and non-specific esterase. RESULTS: Receptor positive cells were present in rheumatoid synovia, with some cells also staining positively for non-specific esterase. In contrast, both osteoarthritic and normal synovia contained very few cells expressing receptors. CONCLUSIONS: Thrombin may mediate important pathological changes during chronic inflammatory joint disease.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bar-Shavit R., Kahn A., Wilner G. D., Fenton J. W., 2nd Monocyte chemotaxis: stimulation by specific exosite region in thrombin. Science. 1983 May 13;220(4598):728–731. doi: 10.1126/science.6836310. [DOI] [PubMed] [Google Scholar]
- Brass L. F., Vassallo R. R., Jr, Belmonte E., Ahuja M., Cichowski K., Hoxie J. A. Structure and function of the human platelet thrombin receptor. Studies using monoclonal antibodies directed against a defined domain within the receptor N terminus. J Biol Chem. 1992 Jul 15;267(20):13795–13798. [PubMed] [Google Scholar]
- Chen L. B., Buchanan J. M. Mitogenic activity of blood components. I. Thrombin and prothrombin. Proc Natl Acad Sci U S A. 1975 Jan;72(1):131–135. doi: 10.1073/pnas.72.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOMORI G. Histochemistry of human esterases. J Histochem Cytochem. 1955 Nov;3(6):479–484. doi: 10.1177/3.6.479. [DOI] [PubMed] [Google Scholar]
- Grober J. S., Bowen B. L., Ebling H., Athey B., Thompson C. B., Fox D. A., Stoolman L. M. Monocyte-endothelial adhesion in chronic rheumatoid arthritis. In situ detection of selectin and integrin-dependent interactions. J Clin Invest. 1993 Jun;91(6):2609–2619. doi: 10.1172/JCI116500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howells G. L., Macey M., Curtis M. A., Stone S. R. Peripheral blood lymphocytes express the platelet-type thrombin receptor. Br J Haematol. 1993 May;84(1):156–160. doi: 10.1111/j.1365-2141.1993.tb03039.x. [DOI] [PubMed] [Google Scholar]
- Hung D. T., Vu T. H., Nelken N. A., Coughlin S. R. Thrombin-induced events in non-platelet cells are mediated by the unique proteolytic mechanism established for the cloned platelet thrombin receptor. J Cell Biol. 1992 Feb;116(3):827–832. doi: 10.1083/jcb.116.3.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laposata M., Dovnarsky D. K., Shin H. S. Thrombin-induced gap formation in confluent endothelial cell monolayers in vitro. Blood. 1983 Sep;62(3):549–556. [PubMed] [Google Scholar]
- Lindahl U., Pejler G., Bøgwald J., Seljelid R. A prothrombinase complex of mouse peritoneal macrophages. Arch Biochem Biophys. 1989 Aug 15;273(1):180–188. doi: 10.1016/0003-9861(89)90177-x. [DOI] [PubMed] [Google Scholar]
- Morris C. J., Blake D. R., Wainwright A. C., Steven M. M. Relationship between iron deposits and tissue damage in the synovium: an ultrastructural study. Ann Rheum Dis. 1986 Jan;45(1):21–26. doi: 10.1136/ard.45.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris R., Winyard P. G., Blake D. R., Morris C. J. Thrombin in inflammation and healing: relevance to rheumatoid arthritis. Ann Rheum Dis. 1994 Jan;53(1):72–79. doi: 10.1136/ard.53.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelken N. A., Soifer S. J., O'Keefe J., Vu T. K., Charo I. F., Coughlin S. R. Thrombin receptor expression in normal and atherosclerotic human arteries. J Clin Invest. 1992 Oct;90(4):1614–1621. doi: 10.1172/JCI116031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Z., Garcia C. H., O'Rourke L. M., Planck S. R., Kohli M., Rosenbaum J. T. Local proliferation of fibroblast-like synoviocytes contributes to synovial hyperplasia. Results of proliferating cell nuclear antigen/cyclin, c-myc, and nucleolar organizer region staining. Arthritis Rheum. 1994 Feb;37(2):212–220. doi: 10.1002/art.1780370210. [DOI] [PubMed] [Google Scholar]
- Shu S. Y., Ju G., Fan L. Z. The glucose oxidase-DAB-nickel method in peroxidase histochemistry of the nervous system. Neurosci Lett. 1988 Feb 29;85(2):169–171. doi: 10.1016/0304-3940(88)90346-1. [DOI] [PubMed] [Google Scholar]
- Sugama Y., Tiruppathi C., offakidevi K., Andersen T. T., Fenton J. W., 2nd, Malik A. B. Thrombin-induced expression of endothelial P-selectin and intercellular adhesion molecule-1: a mechanism for stabilizing neutrophil adhesion. J Cell Biol. 1992 Nov;119(4):935–944. doi: 10.1083/jcb.119.4.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vu T. K., Hung D. T., Wheaton V. I., Coughlin S. R. Molecular cloning of a functional thrombin receptor reveals a novel proteolytic mechanism of receptor activation. Cell. 1991 Mar 22;64(6):1057–1068. doi: 10.1016/0092-8674(91)90261-v. [DOI] [PubMed] [Google Scholar]
- Weinberg J. B., Pippen A. M., Greenberg C. S. Extravascular fibrin formation and dissolution in synovial tissue of patients with osteoarthritis and rheumatoid arthritis. Arthritis Rheum. 1991 Aug;34(8):996–1005. doi: 10.1002/art.1780340809. [DOI] [PubMed] [Google Scholar]