Abstract
Thrombotic microangiopathy (TMA) is a syndrome of microangiopathic hemolytic anemia and thrombocytopenia with end-organ dysfunction. Although the advent of plasma exchange, immunosuppression, and complement inhibition has improved morbidity and mortality for primary TMAs, the management of secondary TMAs, particularly drug-induced TMA, remains less clear. TMA related to cancer drugs disrupts the antineoplastic treatment course, increasing the risk of cancer progression. Chemotherapeutic agents such as mitomycin-C, gemcitabine, and platinum-based drugs as well as targeted therapies such as antiangiogenesis agents and proteasome inhibitors have been implicated in oncotherapy-associated TMA. Among TMA subtypes, drug-induced TMA is less well-understood. Treatment generally involves withdrawal of the offending agent and supportive care targeting blood pressure and proteinuria reduction. Immunosuppression and therapeutic plasma exchange have not shown clear benefit. The terminal complement inhibitor, eculizumab, has shown promising results in some cases of chemotherapy-associated TMA including in re-exposure. However, the data are limited, and unlike in primary atypical hemolytic uremic syndrome, the role of complement in the pathogenesis of drug-induced TMA is unclear. Larger multicenter studies and unified definitions are needed to elucidate the extent of the problem and potential treatment strategies.
Keywords: chemotherapy, thrombotic microangiopathy, TMA, drug-induced TMA, DITMA, antineoplastics, cancer-associated TMA, gemcitabine-induced TMA, mitomycin-C-associated TMA, cisplatin induced TMA
Case Presentation
A 63-year-old woman with 2 years of stage IIIB serous ovarian carcinoma presented to nephrology clinic for evaluation of AKI. Cancer treatment included debulking surgery followed by adjuvant carboplatin/paclitaxel and then paclitaxel/bevacizumab. Six months before presentation, disease progression prompted treatment change to bevacizumab/gemcitabine, although one month ago, bevacizumab was discontinued due to new-onset difficult-to-control hypertension. Serum creatinine had increased from 0.8 mg/dl (3 months prior) to 2.2 mg/dl with new proteinuria of 8.6 g/g creatinine. Laboratory results revealed decreasing hemoglobin (8.4 g/dl from 12 g/dl) and platelet count (144×1000/µl). Physical examination was unremarkable. Urine sediment showed few granular casts. Complement(C)3 and C4 were normal. Haptoglobin was undetectable. Lactate dehydrogenase (705 U/L), reticulocyte count (3.11%), and fibrinogen (492 mg/dl) were elevated. Gemcitabine was discontinued, and the patient underwent a kidney biopsy. Biopsy revealed chronic thrombotic microangiopathy (TMA), acute tubular injury, and 10% interstitial fibrosis and tubular atrophy. Glomeruli were globally sclerotic except one with a fibrocellular crescent. Vessels had moderate-to-severe intimal sclerosis. The lamina rara interna layer of the glomerular basement membrane (GBM) was expanded. There were no immune complex deposits. Creatinine later improved (1.4 mg/dl at 2 months and 1.0 mg/dl at 6 months). Proteinuria decreased to 0.22 g/g creatinine.
Introduction
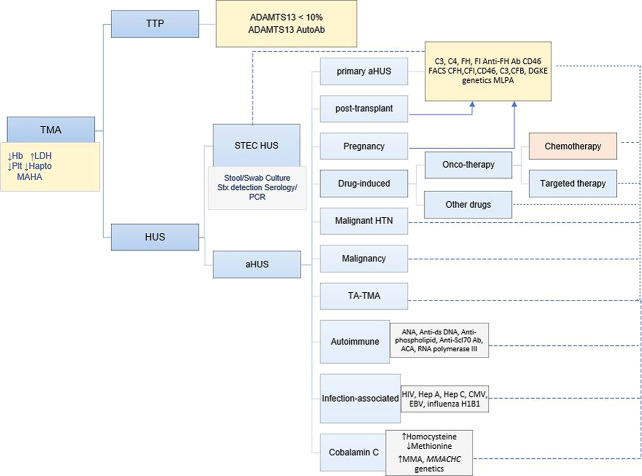
Chemotherapy offers curative treatment for early stage cancer and palliation for late-stage cancer but may have off-target effects including kidney toxicity. One such adverse effect is TMA which constitutes microangiopathic hemolytic anemia (MAHA), thrombocytopenia, intravascular thrombosis, and ischemia-induced end-organ damage. The first case of TMA was reported in 1924 by Moschcowitz who described a 16-year-old girl with acute paralysis, fever, petechial rash, MAHA, severe thrombocytopenia, and kidney dysfunction, culminating in neurologic deficits, coma, and death within days.1 Autopsy revealed widespread hyaline thrombi in kidney and heart capillaries. This disease, now known as thrombotic thrombocytopenic purpura (TTP), is one of the most extensively studied subtypes of TMA. Primary TMAs mainly include hereditary or acquired forms of TTP and primary atypical hemolytic uremic syndrome (aHUS). Their pathogeneses are well-understood, and their respective diagnosis and treatment are well-developed. Drugs (including chemotherapy), pregnancy, malignant hypertension, autoimmune rheumatic diseases, infection, transplant, and malignancy constitute the secondary TMAs (Figure 1).
Figure 1.
KDIGO TMA diagnostic algorithm. The classifications of TMA and corresponding laboratory diagnoses are presented. The dashed line represents possible utility but insufficient evidence to recommend this evaluation. ACA, anticentromere antibody; aHUS, atypical hemolytic uremic syndrome; ANA antinuclear antibody; anti-Scl-70, antitopoisomerase I antibody; CMV, cytomegalovirus; DGKE, diacylglycerol kinase ε; EBV, Epstein-Barr virus; FACS, florescence-activated cell sorting; Hb, hemoglobin; Hep, hepatitis; HUS, hemolytic uremic syndrome; LDH, lactate dehydrogenase; MAHA, microangiopathic hemolytic anemia; MLPA, multiplex ligation-dependent probe amplification; PCR, polymerase chain reaction; Plts, platelets; STEC-HUS, Shiga toxin E. coli HUS; Stx, Shiga toxin; TA-TMA, transplant-associated thrombotic microangiopathy; TTP, thrombotic thrombocytopenic purpura. Adapted from Goodship et al. with permission from Kidney International.2
The association between chemotherapy and TMA was recognized as early as 1971 when Liu et al. described AKI and MAHA in patients with advanced cancer treated with the alkylating agent mitomycin-C.3 Similar descriptions were reported subsequently, leading to the terms mitomycin-associated HUS, mitomycin-associated renal failure, or cancer-associated TMA.4 Other antineoplastics have since been associated with TMA.5–7 In this review, we explore the existing literature on the pathophysiology, diagnosis, therapeutic options, and prognosis of chemotherapy-associated TMA.
Epidemiology of Cancer-Associated TMA
Although HUS (1–3 in 100,000) and TTP (<1 in 100,000) are rare among the general population, an overall TMA incidence of 6%–15% has been reported among patients with cancer, reaching approximately 40% in the hematopoietic stem cell transplant (HSCT) setting.8,9 According to the most recent retrospective review of patients hospitalized with TMA by Bayer et al., secondary TMAs in general are much more common than primary TMAs.10 Following a three physician adjudication process, of 564 patients hospitalized for management of TMA across four major hospitals in France in a span of 7 years, most (94%) were attributed to a secondary cause of TMA. A cause was identified in 94% of these cases with malignancies making up 19% of the causes and drugs, 26%.10 The implicated drugs were calcineurin inhibitors (68%), gemcitabine (8%), and vascular endothelial growth factor inhibitors (3%). Of note, nearly half of the entire cohort had ≥2 causes, and 61% of those with malignancy-attributed TMAs were also on drugs that have been associated with TMA.
The incidence of drug-induced TMA (DITMA) in the general population and its contribution to chronic kidney disease is less well-known due to lack of unifying diagnostic criteria. A recent systematic review revealed that only 344 of approximately 1500 articles on DITMA had evaluable data; only 22 of 78 unique drug-TMA associations were deemed definite, and many reclassified as probable.11 However, DITMA is also likely underdiagnosed as it may present as renal-limited TMA, without systemic signs to aid diagnosis. Chemotherapy-associated TMA in particular may be on the rise with the increasing use of multidrug regimens and may be an underappreciated cause of chronic kidney disease in the cancer population where hematologic abnormalities are often attributed to myelosuppression delaying diagnosis.
Diagnosis of TMA
Clinical Presentation
Clinically, chemotherapy-induced TMA presents similarly to aHUS (Table 1). Patients may exhibit elevated creatinine, worsening or new-onset hypertension, proteinuria, and edema. Hypertension has been reported in 75%–90% of patients with chemotherapy-associated TMA.12 The proteinuria is often subnephrotic but can be in the nephrotic range (>3 g/d). Laboratory evaluation should include complete blood count with differential, lactate dehydrogenase (LDH), haptoglobin, and peripheral smear for schistocytes, although it must be noted that hematologic features of TMA are not always present in DITMA (Table 2).13,19 Haptoglobin is reduced because of binding to free hemoglobin and subsequent clearance by macrophages. LDH is often high secondary to tissue ischemia and cell lysis. The Coombs test is negative, consistent with intravascular hemolysis. Schistocytes result from red blood cell fragmentation within the microvasculature, and >1% or ≥2 per high power field is considered significant.34,35 Coagulation tests will be normal unlike in diffuse intravascular coagulation, which should be considered in patients with active malignancy. An important step in the diagnosis is to exclude TTP by measuring ADAMTS13 activity. Vitamin B12, methylmalonic acid, and homocysteine levels and if diarrhea, stool Shiga toxin and Escherichia coli analysis should also be pursued in the right clinical setting.
Table 1.
Features of drug-induced thrombotic microangiopathies
| ➢ Exposure to potentially causative drug in the past 21 days or chronic exposure |
| ➢ Renal dysfunction |
| • Elevated creatinine |
| • Proteinuria, often subnephrotic |
| ➢ New or worsening hypertension |
| ➢ MAHA |
| • Coombs negative hemolytic anemia |
| • Elevated LDH |
| • Undetectable haptoglobin |
| • Schistocytes: ≥2/HPF or >1% |
| ➢ Thrombocytopenia (<150k or 25% decline from baseline) |
| ➢ ADAMTS13 activity often low but >10% |
| ➢ Normal coagulation profile |
Clinical features of drug-induced thrombotic microangiopathies (DITMA) are shown.
MAHA, microangiopathic hemolytic anemia; LDH, lactate dehydrogenase; ADAMTS13, a disintegrin and metalloprotease with thrombospondin type 1 repeats, member 13.
Table 2.
Cases of common antineoplastic-associated thrombotic microangiopathies: clinical presentation, treatment, and outcomes
| Suspected Drug | Author, Year | N | Clinical Presentation | Duration, Cumulative Dose | Other Drugs | Renal Bx | Tx | Outcomes | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Hematologic Response | Renal Response | Overall Survival | ||||||||
| Chemotherapy (Type I) | ||||||||||
| Mitomycin-C | Liu, 19713 | 3 | 44–61 y/o, AKI, HTN, edema, proteinuria, ↓hgb, ↓plt, ↑LDH | 5–8 mo 105 mg/260 mg/275 mg | None | Yes | Supportive care + CS | Variable | None | 1 died (kidney failure), 2—disease progression |
| Lesesne, 19894 | 85 | Pulm edema (65%), MAHA (83), 35% no active cancer | 1–5 mo, All but 9, >60 mg | 5-FU, Adriamycin | No | CS (50), SPA (21), TPE (37), HD (28) | TPE—11/37 SPA—10/21 CS—18/50 |
10/28 requiring HD; others unclear | 52 died in 8 wk, 18 due to progression | |
| Wen, 200313 | 1 | 58 y/o, gastric ca, HTN, edema, AKI, + schistocytes, proteinuria 0.8 g/d, ↓hgb, ↓plt, ↑LDH | 10 mo, 100 mg | None | Yes | TPE + antiplatelets | No MAHA at baseline | CKD—Cr 4 mg/dl | Alive at 4 yr with no progression | |
| Shiiki, 199214 | 1 | 65 y/o gastric leiomyosarcoma, edema, HTN, mild AKI, proteinuria 0.8 g/day | 6 mo, 70 mg | None | Yes | Supportive care | Gradual recovery in anemia | Quick AKI recovery | Died in 1 year (progression) | |
| Gemcitabine | Daviet, 201915 | 120 | AKI (97%), edema (57%), HTN (62%), ↓hgb (96%), ↓plt (75%), sev AKI (27%), hematuria (23%), proteinuria (34%) 0.6–2.8 g/d | Median 210 d, 13 g/m2 | Unknown | 24% | D/c (100%), TPE (40%), FFP (21%), CS (15%), Eculizumab (5%), HD (28%) | 65% CR | 42%—some remission | Only known for 59 pts. 35% died—65% attributed to TMA |
| Izzedine, 2006 (Cases)12 | 3 | 30–78 y/o, dyspnea, edema, all ↓hgb, ↓plt, ↑LDH, 2–8g/d proteinuria, + rare schistos (2/3) | 6 mo (19.2 g) 3 g 27 g |
Pt 1: none Pt 2: platinum salt Pt 3: none |
All 3 | Pt 1: D/c + CS Pt 2: 30 x TPE, IVIg, CS → doxy (2 mo) Pt 3: D/c + CS + FFP |
Pt 1: CR in 3 mo Pt 2: >2-3 wk of doxy Pt 3: Over months |
1: PR) at 6 mo (Cr: 1.6 mg/dl; 2: CR 3: PR at 2 yr (1.3 mg/dl) |
1: alive at 3 mo 2: alive at 3 mo 3: alive until 2 yr (cancer progression) |
|
| Izzedine, 2006 (systematic review)12 | 56 (incl. above 3) | 26–78 y/o advanced GI, SCC lung, ovarian ca. HTN (42), proteinuria (36), hematuria (33), ↓hapto (23/26), Schistos (21/24); All - ↓hgb, ↓plt, ↑LDH, AKI | 0.5 d–19 mo, 22.48 (2–70) g | 4 previous MMC exposed | 21/56 | D/c (43), D/c alone (5), TPE (20), CS (8), FFP (4), IVIg (1), ↓dose (1) | — | 66% PR/CR, 34% CKD, 24% HD | Died at 16 (11–24 mo (cancer progression) | |
| Glezerman, 200916 | 29 | Schistocytes (21/24), ↓hapto (23/26), HTN (26), edema (21), hematuria and proteinuria (27) | 7.5 (2–34) mo | 9 prev MMC: (4/9 shortly before Gem) | 4/29 | Drug D/c only | — | 19—CR 3—PR/CKD 7—NR/ESKD |
— | |
| Murugapandian, 201517 | 1 | 74 y/o, HTN, uProt 2.4g/d,↓hgb, ↓plt, ↑LDH,+ schistos | 9.4 g | Previous Cis | Yes | Refractory to 5× TPE +CS → 1 g Rituximab | CR 1.5 mo after rituximab ×1 | PR (7.3 to 2 mg/dl) | Cancer progression, → hospice | |
| Ritchie, 201718 | 3 | 52–68 y/o, pancreatic adenoCa. Severe HTN, edema, MAHA, 0.77–2.7 g proteinuria | 2–6 cycles adjuvant Gem, 22 g, 21.1 g, 8 g | — | Yes (3/3) | Refractory to D/c+ 5–6 cyc TPE+CS (Pt 1 and 2) and D/c + CS (Pt 3) → Rituximab × 4 cycles | CR after one course of Rituximab | 1 had CR, 2 had PR in 1–2 mo | All alive for >1 yr | |
| Platinum-based Cisplatin |
Nishikubo, 202119 | 1 | 43 y/o, lymphoma, AKI, uPCR 6.5 g/g, microhematuria, ↓hgb, no MAHA | 100 mg | Gem (2.8 g), DEX | Yes | Cis and Gem d/c | No MAHA | CR (1 mo), uPCR 0.5 g/g | Alive, short follow-up (<1 mo) |
| Carboplatin | Walker, 198920 | 1 | 62 y/o F with medulloblastoma, ↓hgb, ↓plt, ↓hapto, ↑LDH, ↑vWF, +schistocytes, encephalopathy | 17 mo | None | Yes | D/c+ Supportive care + CS | No | Stable | Died within days due to TMA |
| Iams, 201321 | 1 | 57 y/o F, ER/PR/HER2 + breast ca, AKI, dyspnea, ↓hgb, ↓plt, ↓hapto, ↑LDH | 4 mo | Docetaxel, etoposide | No | D/c + TPE +CS | CR in 8 days | PR (8 days), CR (5 mo) | Alive at 9 wk | |
| Oxaliplatin | Saad, 202222 | 1 | 73 y/o F, met colon ca, jaundice, hematuria, oliguria hours after chemo infusion, ↓hgb, ↓plt, ↓hapto, ↑LDH | Hours after infusion | Bevacizumab, 5-FU/LC | No | D/c+TPE + CS + HD | MAHA resolved at day 7 | HD | Alive at 27 days |
| Fuentes-Lacouture, 202023 | 1 | 64 y/o F, met gall bladder ca, disorientation, ↓hgb, ↓plt, ↓hapto, ↑LDH, no AKI | Last dose 20 d ago | Capecitabine, previously Gem + CIS | No | D/c + Palliative care | NR | Preserved kidney function | Died at 17 d, palliative care | |
| Dahabreh, 200624 | 1 | 52 y/o M, adjuvant FOLFOX for stage C colorectal ca s/p resection, immediate urine discoloration, severe AKI, ↓hgb, ↓plt, ↓hapto, ↑LDH, +schistos | Hours after infusion (normal labs prior to infusion) | 5-FU/LC | No | D/c + CS + FFP | CR (15d) | PR (15 d), CR (1 mo) | Alive at 1 yr, disease free | |
| Bleomycin | Salhi, 202125 | 1 | 56 y/o lung ca—nonseminoma germ cell tumor, ARF, ILD, severe HTN, AKI, uPCR 2.2 g/g, microhematuria, MAHA | 2 mo | Cis and etoposide | Yes | D/c + TPE (d1-4) + HD (d2) + eculizumab (d 5, 13, 20) | Improved after eculizumab | NR | Died on day 25: bleomycin-attributed respiratory failure |
| Jackson, 198426 | 5 | Two 24 and 29 y/o M with (tumor free for 5–6 mo), sCr 2.2 and 7.9 mg/dl, Pt 1—Plt/Hct/LDH nml, + schistocytes, Pt 2—MAHA, Pt 3–5: 60–66 y/o oropharyngeal SCC, all s/p surgical resection, sCr 7.6–13.8 mg/dl, + MAHA | 1–4 courses Pt 1–2: last dose 3 and 4 mo ago Pt 3–5: last dose 1 d, 3 d, 2 mo ago |
Cis and vincristine/vinblastin | Yes (5/5) | Pt 1—BP control Pt 2—HD Pt 3–5: TPE and dialysis |
Pt 1–2: CR (unknown time to recovery) Pt 3–5: 2/3 improved |
PR (sCr 1.9) NR |
Pt 1 and 2—alive and tumor free at 3 and 7 yr Pt 3–5: died at day 14, 29 and 59—arrhythmia, GIB/resp. failure; and PNA |
|
| Chemotherapy (Type II) | ||||||||||
| VEGFi | Eremina, 200827 | 6 | Pt 1: 56 y/o HCC: HTN, uPCR 3.4, ↓plt, no MAHA. Pt 2: 74 y/o HCC: AKI, uPCR-2.7, no MAHA. Pt 3: 54 y/o BAC, AKI, uProt 160 mg/d, no MAHA. Pt 4: 62 y/o SCC: severe AKI, uPCR 0.5 g/g, hematuria. Pt 5: 61 y/o, AKI, uProt-4.6 g/d, ↓plt, ↓hgb, +schistos. Pt 6: 59 y/o ovarian ca, no MAHA, uProt-825 mg/d | Pt 1—24 doses, Pt 2— last 9 mo, Pt 3—4 doses, Pt 4—19 doses, Pt 5—12 doses, Pt 6–9 mo (29 doses) | Pt 1–3: None, Pt 4—Cis, Pt 5—Gem + erlotinib, Pt 6—none | Yes (6/6) | Pt 1—D/c only, Pt 2—D/c only, Pt 3—D/c only, Pt 4—D/c + CS + CYC, Pt 5—D/c + 5× TPE, Pt 6—Drug continued | Mild or no hematologic findings in 5/6 | 1: PR in 3 mo, 2: CR in 3 mo, 3: Unknown, 4: CR in 2 mo, 5: PR w TPE, 6: PR w Persistent but stable uProt | 1,2, 4: Alive, 3, 5, 6: Died (progression) |
| Morimoto, 202028 | 1 | 68 y/o, HTN, mild edema, uPCR 6.8 g/g, +hematuria, + granular casts | 3 doses, bevacizumab | Carboplatin, paclitaxel → Gem | Yes, Subendo IC deposits | CS → CS + MMF × 3 mo | NR in 3 mo, PR in 10 mo | PR in 10 mo | Alive at 10 mo, no progression | |
| Izzedine, 200629 | 1 | 59 y/o F, chemoresistant metastatic ovarian cancer, severe HTN, 16.6 g/L proteinuria, + hematuria | 2 doses of VEGF Trap | 5-FU, CPT-11 | Yes | D/c + TPE + CS | No reported hematologic abnormality | PR in 2 mo | Alive at 2 mo | |
| Izzedine, 201430 | 73 | 84% HTN, 70% hematuria, all proteinuria, ∼70% uProt > 1 g/d, ∼1/4 + schistos, drug: 1 | 1 wk–26 mo VEGFi (61), VEGF Trap (5), TKI (3) |
— | Yes, only intraglomerular | D/c (except 4) + antihypertensives | Mild or no hematologic findings | All improved with antihypertensive | 54 died at 12 mo (cancer progression) | |
| Proteasome inhibitor Bortezomib |
Van Keer, 201631 | 1 | 51 y/o M IgG k MM, skin lesions on chronic TPE, AKI, proteinuria 3.2 g/d, ↓hgb and plt, ↓hapto, + schisto | First episode: 4 wk (3 doses) Re-exposure: after three doses |
Thalidomide, DEX | Yes | TPE intensification and brief hold Required HD on re-exposure |
PR in 1 mo, unclear on rechallenge | First exposure: PR in 3 wk Re-exposure: PR in 2 mo |
Alive w/disease progression necessitating rechallenge in 8 mo |
| Carfilzomib | Rassner, 202132 | 2 | Pt 1—43 y/o M IgG k MM: dyspnea, malaise, fever, AKI, proteinuria 52 g/L, ↓hgb, LDH, hapto, 11% schisto Pt 2—59 y/o M IgG k MM: fever, proteinuria 6.2 g/d, ↓hgb, ↑LDH, ↓hapto, 42% schisto |
Day 2 of CFZ Fourth cycle of consolidation |
LEN x 2 → ASCT→42 d→recurrence →CFZ/LEN Elotuzumab/LEN |
No (2/2) | Pt 1: D/c + TPE (6 d) → wkly eculizumab×4 Pt 2: D/c + TPE (5 d) +CS→ eculizumab (4×900 mg/wk+1200 mg/2 wk×2) |
Pt 1: PR within days after eculizumab, CR (2 mo) Pt 2: CR after a few weeks |
Pt 1: Off HD- after fourth eculizumab, CR in 2 mo Pt 2: PR |
Pt 1: Alive at 1 yr, no progression Pt 2: Alive at 4 mo |
| Qaqish, 201633 | 2 | Pt 1—73 y/o M refractory MM: severe HTN, anuric AKI, not anemic, ↓plt, ↑LDH, + schisto Pt 2—72 y/o W relapsed MM, remote ASCT, nonoliguric AKI, ↓plt, ↓hgb, ↑LDH, + schisto |
2 cycles CFZ 6 cycles CFZ |
Previous BZ Previous BZ |
Yes (2/2) | Pt 1: D/c +TPE (4 d) + HD Pt 2: D/c + TPE (4 d) |
Pt 1: NR to TPE, Improved over a week off TPE Pt 2: NR to TPE, CR after 3 wk off TPE |
Pt 1: Off HD at 5 wk, PR (Cr1.6 mg/dl) Pt 2: CR after 9 mo |
Pt 1: Alive at 5 wk Pt 2: Alive at 9 mo |
|
Example published cases of type I (chemotherapy) and type II (targeted therapy) antineoplastics are presented along with therapeutics explored and outcomes where available. HTN, hypertension; LDH, lactate dehydrogenase; MAHA, microangiopathic hemolytic anemia; plts, platelets; 5‐FU, 5-fluorouracil; CS, corticosteroids; SPA, staphylococcal protein-A immunadsorption; TPE, therapeutic plasma exchange; HD, hemodialysis; GI, gastrointestinal; GEM, gemcitabine; Pt, patient; MM, multiple myeloma; CIS, cisplatin; PR, partial remission; TMA, thrombotic microangiopathy; uPCR, urine protein, creatinine ratio; vWF, von Willebrand factor; NR, no response; CPT-11, irinotecan; VEGFi, vascular endothelial growth factor inhibitor; VEGF-R, vascular endothelial growth factor receptor; VEGF-Trap, fully humanized recombinant fusion protein containing extracellular portions of VEGFR-1 and VEGFR-2; TKI, tyrosine kinase inhibitors; ASCT, autologous stem cell transplant; CFZ, carfilzomib; BZ, bortezomib; LEN, lenalidomide.
Histologic Findings
Kidney biopsy is useful for definitive diagnosis while excluding other etiologies for proteinuric AKI. It has diagnostic and prognostic implications and should be pursued when there is a clinical suspicion, particularly for kidney-limited TMA, as long as bleeding risk does not outweigh benefit. Biopsy may reveal alternative or concomitant diagnoses including antineoplastic-associated tubulointerstitial nephritis and glomerulonephritides, such as malignancy-associated minimal change disease or membranous nephropathy, although the frequency of co-occurrence of these findings is unknown.9 A kidney biopsy-associated bleeding risk score has been developed by Halimi et al. on the basis of a French national retrospective review of 52,138 patients who underwent a kidney biopsy which can assist with risk stratification.36 The presence of cancer (2+) and diagnosis of TMA at the time of biopsy (2+) were both one of 19 risk factors for major bleeding. This risk score notably also includes the presence of anemia (8+), thrombocytopenia (2+), and abnormal kidney function (4+). This score may be helpful after external validation as outcomes may be influenced by varying hospital practices and performers' expertise.
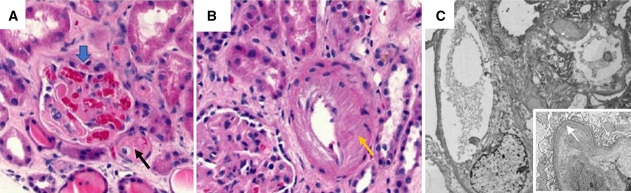
In acute TMA, histologic findings include thrombi or fragmented red cells in the mesangial space, mesangiolysis, swelling of endothelial cells, and occlusion of the endothelial lumen by thrombi (Figure 2). In chronic TMA, focal or global glomerulosclerosis, and duplication of the GBM, chronic intimal hyperplasia and intimal fibrosis may be observed. Glomerular cysts because of mesangiolysis have been specifically identified with mitomycin-C.14
Figure 2.
Histologic findings in a patient with gemcitabine-associated thrombotic microangiopathy. Shown here is a kidney biopsy from a patient with gemcitabine-induced TMA. H&E stained light microscopy evaluation showing (A) a glomerulus (wide blue arrow) with intraglomerular thrombi, mesangiolysis, entrapped intraglomerular thrombi, and a vessel (black arrow) with luminal occlusion and intimal thrombi, (B) vessel (yellow arrow) with intimal edema and sclerosis. Nine of 37 glomeruli were globally sclerotic. (C) Electron microscopy showing mesangiolysis, diffuse endothelial swelling, and duplication of the glomerular basement membrane with expansion of the lamina rara interna (white arrow).
Biomarkers
Hematologic evidence of intravascular hemolysis may not be present in less severe systemic hemolysis or kidney-limited TMA. Biomarkers may help in early diagnosis and intervention. Serum neutrophil gelatinase-associated lipocalin has been explored as a predictive tool for progression to renal replacement therapy in a cohort of 39 patients with STEC-HUS.37 However, endothelial markers may have a more useful role than tubular markers of injury in TMA. Elevated endothelial markers (e.g., thrombomodulin, plasminogen activator inhibitor-1, and soluble intercellular adhesion molecule-1) have been reported in transplant-associated TMA.38 Similarly, elevated thrombomodulin, tissue plasmin activator, and plasminogen activator inhibitor-1 have been reported in mitomycin-C–associated TMA.39 The utility of endothelial biomarkers for diagnosis of other types of TMA requires further study.
Genetic and functional complement pathway assessment may also be useful, but data on the utility of such studies are lacking.
Commonly Implicated Drugs in Chemotherapy-Associated TMA
Table 2 presents example cases of antineoplastics-associated TMA, including the suspected drug, management, and outcomes where available. The chemotherapeutic drugs most frequently associated with TMA are mitomycin-C and gemcitabine.
Mitomycin-C
The chemotherapeutic agent with the earliest reported association with TMA is mitomycin-C, a quinine antineoplastic isolated from Streptomyces caespitosus which inhibits DNA synthesis by crosslinking adenine and cytosine.5 In addition to direct endothelial toxicity, mitomycin promotes platelet aggregation through prostacyclin inhibition.40 TMA has been reported in 4%–15% of patients on mitomycin-C with mortality as high as 75% depending on overall cancer status.4 Although commonly reported within 4 weeks of the last dose, late-onset presentations of 6–12 months after initiation have been described.5,13,41 A 1989 US national registry of 85 patients with then-called cancer-associated HUS reported that 84 patients were treated with mitomycin-C, and all but nine had received doses exceeding 60 mg.4 A total cumulative dose exceeding 40–60 mg seems to be a major risk factor.5,42 Delayed bone marrow suppression is the most common toxicity, which may mask early TMA. Dyspnea was a common presenting symptom with noncardiogenic pulmonary edema reported in two thirds of 84 patients with mitomycin-associated TMA.4 Severe renal impairment requiring dialysis was reported in about 1/3 of the patients which recovered in approximately 36%.
Gemcitabine
A pyrimidine analog, gemcitabine promotes apoptosis of rapidly dividing cells by disrupting DNA synthesis. It is mostly renally excreted (98%), and the half-life of elimination depends on infusion length, ranging from 0.7 hours in infusions shorter than 70 minutes to 10.6 hours in infusions >70 minutes.43 The first gemcitabine-associated TMA was reported in 1994 in a phase II trial for pancreatic adenocarcinoma.44 Subsequent reports have estimated incidence ranging 0.015%–1.4%.12,45–47 Cumulative dosing >20,000 mg/m2 increases TMA risk, although TMA with single-dose or low-dose has been reported, particularly when used with other predisposing drugs.16,48 Prior treatment with mitomycin-C has been recognized as a risk factor.16 Gemcitabine has been associated with both dose-dependent and immune-mediated toxicity.49 There is often a long delay between TMA onset and initial drug exposure. TMA onset ranging from a few days to 34 months from initial exposure has been reported.12,16
The following chemotherapeutic agents have also been implicated in TMA but with an even rarer incidence.
Bleomycin
Like mitomycin, bleomycin is an antitumor antibiotic that disrupts DNA synthesis with a rarer association with TMA. Severe TMA with dialysis requirement, high mortality, and less reversibility is reported with bleomycin-associated TMA, although most (14 of 15 reported cases) were also receiving cisplatin and/or cisplatin and vinka alkaloid, confounding which drug played a causal role.25
Platinum-Based Agents
Cisplatin, oxaliplatin, and carboplatin are associated with varying degrees of tubular toxicity, electrolyte abnormalities, and, rarely, TMA. These agents bind to proteins and nucleic acids preventing DNA replication, causing cell cycle arrest and ATP depletion. TMA has been reported both alone and in combination with drugs such as gemcitabine and bleomycin.19–23,50–52 TMA occurrence within hours after infusion has been reported with oxaliplatin.22,24 Renal dysfunction was partially or completely reversed within few weeks in most cases.
Others (e.g., vincristine, adriamycin, and 5-fluorouracil [5-FU]) have also been implicated in fewer case reports almost always in the setting of concomitant or recent exposure with the abovementioned agents or antiangiogenic therapy.
Differential Diagnosis of TMA in the Patient on Chemotherapy
Depending on the chemotherapeutic agent, clinical history, and the type and extent of malignancy, even in the presence of biochemical findings suggesting TMA, differential diagnosis of AKI in the patient on chemotherapy should include the more common ischemic or nephrotoxin-induced acute tubular injury/necrosis, tumor burden–related urinary tract obstruction and in the right clinical setting, tumor lysis syndrome, interstitial nephritis, and glomerulonephritis.9
TMA in patients with cancer may result from either cancer or its treatment.5,9 Elucidating the etiology of TMA (Figure 1) requires comprehensive review of the patient's clinical presentation and medical history.
Type I oncotherapy-associated TMA: This represents chemotherapy-associated TMA. AKI with these agents is less likely to reverse and more likely to recur with re-exposure.9
Type II oncotherapy-associated TMA: Reports of targeted therapy-associated TMA are increasing. Frequently implicated drugs include the antiangiogenics vascular endothelial growth factor (VEGF) inhibitors and tyrosine kinase inhibitors.6,7,30,53 Cases of TMA in patients receiving the proteasome inhibitors bortezomib and carfilzomib also exist.32,33,54–57 Immunotherapy/immunotoxin-associated TMA has also been described.6,7 Although it is challenging to distinguish the causative agent in patients taking combinations with chemotherapies, TMA from VEGF-inhibitors tends to have milder hematologic features and exclusively intraglomerular findings.30
Cancer-associated TMA: TMA as a direct effect of cancer was historically considered rare, with cases usually occurring in association with mucinous adenocarcinoma.58,59 Recent data suggest that it may be a more common cause among TMAs. Malignancies were deemed the culprit in 19% of cases of TMA in a recent retrospective review of over 500 patients hospitalized with TMA.10 The top three implicated malignancies included adenocarcinoma (41%), acute leukemia (18%), and lymphoma (14%). The rest (3%–6%) were melanoma, urothelial carcinoma, multiple myeloma, and chronic lymphocytic leukemia. Half were taking at least one chemotherapeutic agent known to be associated with TMA making it difficult to ascertain whether cancer was the direct cause. In a 2012 review of 168 cancer-associated TMA cases, gastric cancer was the most common (26%), followed by prostate (21%), breast (15.5%), lung cancer (9.5%), and lymphoma (8.3%).8
Primary TMA: TTP from acquired or hereditary deficiency of ADAMTS13 (a disintegrin and metalloprotease with thrombospondin type 1 repeats, 13th member) which impairs von Willebrand factor (vWF) processing is a cause that must be excluded with the measurement of ADAMTS13 activity. An ADAMTS13 activity >10% excludes this diagnosis, important for therapeutic decisions. aHUS (complement-mediated TMA) may result from autoantibodies to complement factor H (CFH) or mutations in genes of complement regulatory proteins CFH and related proteins, CFI, membrane cofactor protein, thrombomodulin or mutations that activate the alternative pathway (CFB, C3). A genetic cause is not found in 40% of cases.60 Shiga toxin-associated HUS (STEC-HUS), which constitutes 90% of all HUS cases, should be considered in patients with diarrhea 4–6 days before presentation.61,62 Late-onset TMA associated with MMACHC mutation-induced cobalamin-C deficiency has also been reported.63
Hematopoietic stem cell transplant–associated TMA (TA-TMA): In patients with recent HSCT, TA-TMA may occur secondary to high-intensity conditioning regimen, radiation, calcineurin inhibitors, sirolimus, or graft versus host disease.64 An incidence of 10%–20% has been reported in allogeneic HSCT, with lower reported incidence in autologous HSCT.65
Pathogenesis of Chemotherapy-Associated TMA
The inciting event in TMA is believed to be endothelial injury from antibodies, circulating immune complexes, endotoxins, or drugs, leading to platelet aggregation and complement activation. The pathophysiology of DITMA likely involves multiple pathways. Vascular endothelial cells produce essential coagulation and platelet aggregation factors, such as vWF, prostacyclin, and thrombomodulin, whose balance is essential for endothelial integrity. Decreased prostacyclin, a potent platelet aggregation inhibitor, has been reported in DITMA.66,67 Two potential mechanisms of DITMA are described, such as immune mediated and nonimmune mediated. The latter is dose-dependent or duration-dependent endothelial injury leading to platelet aggregation and complement activation. Immune-mediated DITMA is associated with drug-induced antibody formation and drug-dependent binding to platelets and typically occurs within hours to approximately 21 days of exposure.11,68 Gemcitabine and oxaliplatin are believed to cause TMA through both immune and direct cytotoxic effects on the basis of timeline and therapeutic response.49,60,69
Genetic mutations may confer susceptibility to TMA. Less than 1% of DITMA has been associated with the presence of genetic mutations in the alternative pathway complement activating or regulatory proteins compared with 15%–60% of cases of malignant hypertension.10,60,70,71 However, the incidence in DITMA may be an underestimate as genetic studies are rarely pursued in cases when a drug is deemed responsible. The proteasome inhibitor carfilzomib has been associated with complement-mediated TMA through decreased CFH expression.55,72 A CFHR3-CFHR1 variant was reported in two of three patients with carfilzomib-induced TMA, although the clinical relevance of the heterozygous variant was unclear.55
Management of Chemotherapy-Associated TMA
The management of chemotherapy-associated TMA should involve discussions between oncology and nephrology including overall implications of discontinuing the suspected causative agent. Figure 3 presents the diagnosis and management of chemotherapy-associated TMA.
Figure 3.
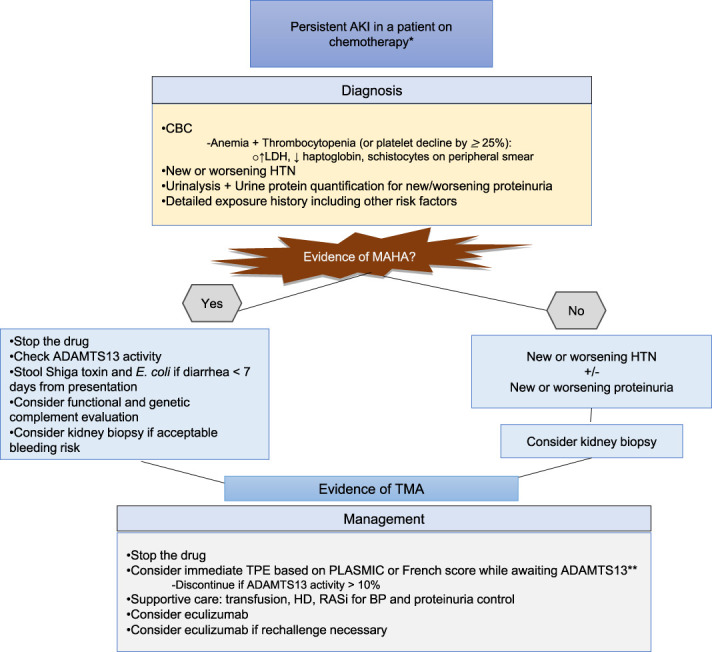
Proposed algorithm for evaluation of suspected chemotherapy-associated TMA. ADAMTS13, a disintegrin and metalloprotease with thrombospondin type 1 repeats, 13th member; BP, blood pressure; CBC, complete blood count; HTN, hypertension; MAHA, microangiopathic hemolytic anemia; RASi, renin angiotensin system inhibitor; TMA, thrombotic microangiopathy; TTP, thrombotic thrombocytopenic purpura. *Unexplained AKI, persistent despite volume optimization. **No proven benefit in cancer or chemotherapy-associated TMA. Consider only if etiology is uncertain or high index of suspicion for TTP.
Supportive Care
The management of chemotherapy-associated TMA also includes blood pressure management, transfusion, and dialysis as needed. Renin-angiotensin system inhibitors help reduce glomerular and systemic hypertension and high-grade proteinuria. Platelet transfusion is generally avoided in TMA in the absence of bleeding because it may worsen microvascular thrombosis.73 Platelet transfusion has been associated with higher odds of mortality (odds ratio, 4.22; 95% confidence interval, 2.36 to 7.60), although likely as a marker of illness severity rather than cause.10 Depending on the degree of kidney dysfunction, dialysis may also be necessary for clearance or volume management.
Therapeutic Considerations
Withholding the drug alone may not lead to hematologic or kidney recovery. Various treatment options have been explored in pursuit of clinical improvement with variable success. Caution must be employed in generalizing response given the possibility of publication bias with preferential reporting of successful case studies. Interpretation of which treatment provides benefit is difficult in many cases where multimodal treatments are used.
Therapeutic Plasma Exchange
The purpose of therapeutic plasma exchange (TPE) in the management of TMA is to remove vWF multimers, replenish ADAMTS13, and remove any potential autoantibodies. TPE has significantly improved mortality from TTP from uniformly fatal (90%–95%) to <20%.74,75 However, it has not been shown to improve outcomes in chemotherapy-associated TMA. TPE for chemotherapy (gemcitabine) is listed as category IV (i.e., ineffective) in the American Society for Apheresis guidelines (Grade_2C).76 Although few drugs, specifically the antiplatelet ticlopidine, have been associated with diminished ADAMTS13 activity, this association has not been reported for TMA-associated chemotherapeutics. Full/partial renal recovery was reported in 65% of 29 cases of gemcitabine-associated TMA with drug withdrawal alone, a better outcome than a cohort treated with TPE, although the latter had more severe disease requiring dialysis.16,77 Only 1/11 TPE-treated versus 3/4 TPE-untreated patients for bleomycin-associated TMA had hematologic and kidney recovery.25 In a large French national registry of 120 patients with gemcitabine-associated TMA, TPE did not improve outcomes compared with corticosteroids or eculizumab but had higher incidence of adverse events.15
It is reasonable to initiate TPE while awaiting ADAMTS13 when suspicion for TTP is high. The PLASMIC score (platelet count <30×103/µl, hemolysis, active cancer, solid organ/stem cell transplant, MCV <90 fL, INR <1.5, creatinine <2 mg/dl) may help risk stratify patients for the likelihood of severe TTP and urgent initiation of TPE while awaiting ADAMTS13 results.78,79 The French score, a simpler score which includes the presence of thrombocytopenia, serum creatinine, or detectable antinuclear antibody, also allows the prediction of likelihood of a low ADAMTS13.80 Although both had poor sensitivity and specificities in older than 60 years, the incorporation of degree of proteinuria was shown to improve the performance of both scores.81,82
Protein-A Immunoadsorption
This treatment has been explored on the basis of a hypothesis that circulating immune complexes may play a role in the pathogenesis of DITMA. Successful use of protein-A immunoadsorption has been reported in severe cases of mitomycin-C–associated TMA.83,84 It was associated with 30-day remission in 25 of 55 patients (53 mitomycin-C/5-FU and 2 cisplatin-associated TMA) defined as at least two of ≥50% LDH reduction, ≥50% platelets rise, ≥50% hemoglobin rise, and creatinine stabilization/improvement.84
Rituximab
There are reports of rituximab, an anti-CD20 monoclonal antibody, use in gemcitabine-associated TMA with positive results.17,18,85,86 Few case studies of patients treated with rituximab with TPE (2) or in cases deemed refractory to TPE and corticosteroids (3) are published with renal recovery reported in 3.17,18,85–87 Rituximab use in mitomycin-C–associated TMA has also been reported but with less positive results.83,88 In a 2019 French retrospective study of 564 patients hospitalized with TMA by Bayer et al., rituximab was used in 3% of the cohort but only 1 of 144 patients with drug-associated TMA.10
Complement Inhibition
Eculizumab, a monoclonal antibody against the near terminal complement C5 has improved mortality and renal recovery in aHUS.89 Its success in aHUS has motivated its use in chemotherapy-associated TMA. There have been case reports of renal recovery with eculizumab with sustained remission in bleomycin, gentamycin, and oxaliplatin-associated TMA including a case of rechallenge.90–95 The median dose was four infusions.96 Other complement blockers, such as the longer acting ravulizumab and the oral C5a receptor-blocker avacopan, have shown promise in aHUS/PNH and as glucocorticoid adjunct in severe ANCA-associated vasculitis, respectively.97–99 Ravulizumab was also found more cost-effective and noninferior to eculizumab with breakthrough hemolysis in phase III trials.97,98,100,101 A case report of its use in a gemcitabine-associated TMA refractory to rituximab/TPE describes improved TMA markers for 3 days before the patient succumbed to sepsis.102 An ongoing multicenter phase III clinical trial is investigating ravulizumab in secondary TMA (NCT04743804).
Other Potential Novel Therapeutics in the Management of TMA
The sodium-glucose cotransporter-2 inhibitor canagliflozin has prevented cisplatin-induced proximal tubular injury and endothelial dysfunction in animal models.103,104 The following have been investigated in other types of secondary TMA. Narsoplimab, a human monoclonal antibody targeting MASP-2 (mannan-binding lectin-associated serine protease-2), which is the effector enzyme of the lectin pathway of the complement system, has received an US Food and Drug Administration Breakthrough Therapy designation for the treatment of TA-TMA and a fast track designation for aHUS. Caplacizumab, a humanized nanobody (single-domain antibody) against the A1 domain of vWF multimers preventing interaction with platelet glycoprotein Ib-IX-IV, key step in microvascular thrombosis, has been associated with quicker platelet normalization and reduced days on plasmapheresis compared with placebo in acquired TTP.105 Prophylactic defibrotide (a fibrinolytic and endothelial stabilizer), which has been effectively used in veno-occlusive disease, has shown promise in a pilot study of 25 pediatric patients high-risk for TA-TMA (incidence 4% with prophylactic defibrotide versus 18%–40% in a similar population).106
Prognosis and Rechallenge in Chemotherapy-Associated TMA
TMA associated with chemotherapy carries a high risk of progression to CKD and mortality. Overall, chemotherapy-associated TMA seems to have more severe presentation and worse prognosis than targeted therapy-associated TMAs.30 Mortality rates of 15%–90% have been reported depending on underlying malignancy stage.9,12 Although rapid hematologic remission can be seen after drug discontinuation, kidney remission takes longer and is often incomplete (Table 2). Partial/complete remission was reported in about half of patients with gemcitabine-associated TMA after drug withdrawal, less for mitomycin, and aggressively treated bleomycin-associated TMA.12,25,26 Eculizumab has shown quicker recovery in some cases of chemotherapy-associated TMA.32,55,90,93–96 Poor prognostic factors for kidney recovery and overall survival include older age, underlying kidney disease, severe hypertension, higher extent and chronicity of kidney involvement at presentation, and advanced status of underlying malignancy.
Rechallenge
The chemotherapy agent that induced TMA may have the greatest anticancer benefit, and re-exposure to the same drug may become necessary in the setting of disease progression on other agents. There are few published reports of rechallenge, all with gemcitabine. Efe et al. recently published successful rechallenge with gemcitabine (cumulative dose 2000 mg/m2) with concomitant eculizumab in a young man with prior eculizumab-treated gemcitabine-associated TMA without evidence of recurrence.95 The patient's previous TMA was also treated with eculizumab with complete hematologic and partial renal response after six doses, but his cholangiocarcinoma progressed within 6 months of stopping gemcitabine despite trials of FU and oxaliplatin. Five cases of rechallenge in gemcitabine-associated TMA have been reported where follow-up data were available for 4, with no recurrence in 50%.15,16,107–109
Conclusion/Future Directions
Cancer therapy–associated TMA is a poorly understood but important cause of kidney disease in the cancer population. Its incidence is expected to rise as various cancers become chronic diseases with episodes of recurrence and increased use of existing and novel therapies including multidrug regimens. The pathogenesis and management of chemotherapy-associated TMA need further investigation. The management is challenging in the absence of diagnostic and treatment guidelines. Evidence is currently lacking to definitively recommend any treatment other than prompt discontinuation of the suspected drug. Complement inhibition may offer benefit in severe or refractory cases. Noninvasive diagnostic tools such as biomarkers of endothelial injury are worth exploration because they may assist with early diagnosis. Functional and genetic complement testing and exploring various treatments in randomized clinical trials may further guide evaluation and targeted management to improve outcomes.
Disclosures
A.A. Shirali reports the following: Consultancy: OnViv; and Other interests or relationships: ASN- member and early program faculty for 2021/2022. The remaining author has nothing to disclose.
Funding
None.
Author Contributions
Supervision: Anushree C. Shirali.
Visualization: Abinet M. Aklilu.
Writing – original draft: Abinet M. Aklilu.
References
- 1.Moschcowitz E. An acute febrile pleiochromic anemia with hyaline thrombosis of the terminal arterioles and capillaries. Am J Med. 1952;13(5):567–569. doi: 10.1016/0002-9343(52)90022-3 [DOI] [PubMed] [Google Scholar]
- 2.Goodship THJ Cook HT Fakhouri F, et al. Atypical hemolytic uremic syndrome and C3 glomerulopathy: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) controversies conference. Kidney Int. 2017;91(3):539–551. doi: 10.1016/j.kint.2016.10.005 [DOI] [PubMed] [Google Scholar]
- 3.Liu K, Mittelman A, Sproul EE, Elias EG. Renal toxicity in man treated with mitomycin C. Cancer. 1971;28(5):1314–1320. doi: [DOI] [PubMed] [Google Scholar]
- 4.Lesesne JB Rothschild N Erickson B, et al. Cancer-associated hemolytic-uremic syndrome: analysis of 85 cases from a national registry. J Clin Oncol. 1989;7(6):781–789. doi: 10.1200/JCO.1989.7.6.781 [DOI] [PubMed] [Google Scholar]
- 5.Grangé S, Coppo P. Thrombotic microangiopathies and antineoplastic agents. Nephrol Ther. 2017;13:S109–S113. doi: 10.1016/j.nephro.2017.01.016 [DOI] [PubMed] [Google Scholar]
- 6.Blake-Haskins JA, Lechleider RJ, Kreitman RJ. Thrombotic microangiopathy with targeted cancer agents. Clin Cancer Res. 2011;17(18):5858–5866. doi: 10.1158/1078-0432.CCR-11-0804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Troxell ML, Higgins JP, Kambham N. Antineoplastic treatment and renal injury: an update on renal pathology due to cytotoxic and targeted therapies. Adv Anat Pathol. 2016;23(5):310–329. doi: 10.1097/PAP.0000000000000122 [DOI] [PubMed] [Google Scholar]
- 8.Lechner K, Obermeier HL. Cancer-related microangiopathic hemolytic anemia: clinical and laboratory features in 168 reported cases. Medicine. 2012;91(4):195–205. doi: 10.1097/MD.0b013e3182603598 [DOI] [PubMed] [Google Scholar]
- 9.Izzedine H, Perazella MA. Thrombotic microangiopathy, cancer, and cancer drugs. Am J Kidney Dis. 2015;66(5):857–868. doi: 10.1053/j.ajkd.2015.02.340 [DOI] [PubMed] [Google Scholar]
- 10.Bayer G von Tokarski F Thoreau B, et al. Etiology and outcomes of thrombotic microangiopathies. Clin J Am Soc Nephrol. 2019;14(4):557–566. doi: 10.2215/CJN.11470918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Nouri ZL, Reese JA, Terrell DR, Vesely SK, George JN. Drug-induced thrombotic microangiopathy: a systematic review of published reports. Blood. 2015;125(4):616–618. doi: 10.1182/blood-2014-11-611335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Izzedine H Isnard-Bagnis C Launay-Vacher V, et al. Gemcitabine-induced thrombotic microangiopathy: a systematic review. Nephrol Dial Transplant. 2006;21(11):3038–3045. doi: 10.1093/ndt/gfl507 [DOI] [PubMed] [Google Scholar]
- 13.Wen MC, Ho WL, Chen CH. Mitomycin C-induced renal insufficiency: a case report. Kaohsiung J Med Sci. 2003;19(6):317–320. doi: 10.1016/S1607-551X(09)70479-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shiiki H Dohi K Nishioka H, et al. Glomerular tuft ballooning in mitomycin-C-induced renal impairment. Virchows Arch A Pathol Anat Histopathol. 1992;420(6):545–551. doi: 10.1007/BF01600261 [DOI] [PubMed] [Google Scholar]
- 15.Daviet F Rouby F Poullin P, et al. Thrombotic microangiopathy associated with gemcitabine use: presentation and outcome in a national French retrospective cohort. Br J Clin Pharmacol. 2019;85(2):403–412. doi: 10.1111/bcp.13808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glezerman I, Kris MG, Miller V, Seshan S, Flombaum CD. Gemcitabine nephrotoxicity and hemolytic uremic syndrome: report of 29 cases from a single institution. Clin Nephrol. 2009;71(02):130–139. doi: 10.5414/CNP71130 [DOI] [PubMed] [Google Scholar]
- 17.Murugapandian S Bijin B Mansour I, et al. Improvement in gemcitabine-induced thrombotic microangiopathy with rituximab in a patient with ovarian cancer: mechanistic considerations. Case Rep Nephrol Dial. 2015;5(2):160–167. doi: 10.1159/000435807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ritchie GE, Fernando M, Goldstein D. Rituximab to treat gemcitabine-induced hemolytic–uremic syndrome (HUS) in pancreatic adenocarcinoma: a case series and literature review. Cancer Chemother Pharmacol. 2017;79(1):1–7. doi: 10.1007/s00280-016-3123-6 [DOI] [PubMed] [Google Scholar]
- 19.Nishikubo M Shimomura Y Hiramoto N, et al. Reversible renal-limited thrombotic microangiopathy due to gemcitabine-dexamethasone-cisplatin therapy: a case report. BMC Nephrol. 2021;22(1):175. doi: 10.1186/s12882-021-02386-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walker RW, Rosenblum MK, Kempin SJ, Christian MC. Carboplatin-associated thrombotic microangiopathic hemolytic anemia. Cancer. 1989;64(5):1017–1020. doi: [DOI] [PubMed] [Google Scholar]
- 21.Iams W, Beckermann KE, Neff AT, Mayer IA, Abramson VG. Thrombotic microangiopathy during docetaxel, trastuzumab, and carboplatin chemotherapy for early-stage HER2+ breast cancer: a case report. Med Oncol. 2013;30(2):568. doi: 10.1007/s12032-013-0568-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saad R, Hannun A, Temraz S, Finianos A, Zeenny RM. Oxaliplatin-induced thrombotic microangiopathy: a case report. J Med Case Rep. 2022;16(1):110. doi: 10.1186/s13256-022-03309-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fuentes-Lacouture MC, Barrera-Garavito EC. Oxaliplatin-induced thrombotic microangiopathy in a patient with stage IV gallbladder carcinoma: primary association or multiple hits? Case Rep Oncol. 2020;13(3):1191–1195. doi: 10.1159/000510307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dahabreh I, Tsoutsos G, Tseligas D, Janinis D. Hemolytic uremic syndrome following the infusion of oxaliplatin: case report. BMC Clin Pharmacol. 2006;6(1):5. doi: 10.1186/1472-6904-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salhi S, Ribes D, Faguer S. Complement C5 inhibition reverses bleomycin-induced thrombotic microangiopathy. Clin Kidney J. 2021;14(4):1275–1276. doi: 10.1093/ckj/sfaa101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jackson AM. Thrombotic microangiopathy and renal failure associated with antineoplastic chemotherapy. Ann Intern Med. 1984;101(1):41. doi: 10.7326/0003-4819-101-1-41 [DOI] [PubMed] [Google Scholar]
- 27.Eremina V Jefferson JA Kowalewska J, et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med. 2008;358(11):1129–1136. doi: 10.1056/NEJMoa0707330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morimoto M, Arai T, Matsuura M, Ono Y. Bevacizumab-associated glomerular microangiopathy that occurred after postoperative chemotherapy for ovarian cancer. CEN Case Rep. 2021;10(1):6–11. doi: 10.1007/s13730-020-00504-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Izzedine H, Brocheriou I, Deray G, Rixe O. Thrombotic microangiopathy and anti-VEGF agents. Nephrol Dial Transplant. 2007;22(5):1481–1482. doi: 10.1093/ndt/gfl565 [DOI] [PubMed] [Google Scholar]
- 30.Izzedine H Escudier B Lhomme C, et al. Kidney diseases associated with anti-vascular endothelial growth factor (VEGF): an 8-year observational study at a single center. Medicine. 2014;93(24):333–339. doi: 10.1097/MD.0000000000000207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Keer J, Delforge M, Dierickx D, Peerlinck K, Lerut E, Sprangers B. Renal thrombotic microangiopathy associated with the use of bortezomib in a patient with multiple myeloma. Case Rep Hematol. 2016;2016:1–5. doi: 10.1155/2016/6020691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rassner M Baur R Wäsch R, et al. Two cases of carfilzomib‐induced thrombotic microangiopathy successfully treated with Eculizumab in multiple myeloma. BMC Nephrol. 2021;22(1):32. doi: 10.1186/s12882-020-02226-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qaqish I, Schlam IM, Chakkera HA, Fonseca R, Adamski J. Carfilzomib: a cause of drug associated thrombotic microangiopathy. Transfus Apher Sci. 2016;54(3):401–404. doi: 10.1016/j.transci.2016.03.002 [DOI] [PubMed] [Google Scholar]
- 34.Zini G d’Onofrio G Erber WN, et al. 2021 update of the 2012 ICSH Recommendations for identification, diagnostic value, and quantitation of schistocytes: impact and revisions. Int J Lab Hematol. 2021;43(6):1264–1271. doi: 10.1111/ijlh.13682 [DOI] [PubMed] [Google Scholar]
- 35.Burns ER, Lou Y, Pathak A. Morphologic diagnosis of thrombotic thrombocytopenic purpura. Am J Hematol. 2004;75(1):18–21. doi: 10.1002/ajh.10450 [DOI] [PubMed] [Google Scholar]
- 36.Halimi JM Gatault P Longuet H, et al. Major bleeding and risk of death after percutaneous native Kidney biopsies: a French nationwide cohort study. Clin J Am Soc Nephrol. 2020;15(11):1587–1594. doi: 10.2215/CJN.14721219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vetter F Beneke J Menne J, et al. Serum neutrophil gelatinase-associated lipocalin (NGAL) in patients with Shiga toxin mediated haemolytic uraemic syndrome (STEC-HUS). Thromb Haemost. 2014;111(02):365–372. doi: 10.1160/TH13-05-0387 [DOI] [PubMed] [Google Scholar]
- 38.Lia G, Giaccone L, Leone S, Bruno B. Biomarkers for early complications of endothelial origin after allogeneic hematopoietic stem cell transplantation: do they have a potential clinical role? Front Immunol. 2021;12:641427. doi: 10.3389/fimmu.2021.641427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nagaya S Wada H Oka K, et al. Hemostatic abnormalities and increased vascular endothelial cell markers in patients with red cell fragmentation syndrome induced by mitomycin C: vascular Endothelial Cell Injuries in RCFS Induced by Mitomycin C. Am J Hematol. 1995;50(4):237–243. doi: 10.1002/ajh.2830500404 [DOI] [PubMed] [Google Scholar]
- 40.Hassan AA, Kroll MH. Acquired disorders of platelet function. Hematology. 2005;2005(1):403–408. doi: 10.1182/asheducation-2005.1.403 [DOI] [PubMed] [Google Scholar]
- 41.Cantrell JE, Phillips TM, Schein PS. Carcinoma-associated hemolytic-uremic syndrome: a complication of mitomycin C chemotherapy. J Clin Oncol. 1985;3(5):723–734. doi: 10.1200/JCO.1985.3.5.723 [DOI] [PubMed] [Google Scholar]
- 42.Garcia G, Atallah JP. Antineoplastic agents and thrombotic microangiopathy. J Oncol Pharm Pract. 2017;23(2):135–142. doi: 10.1177/1078155216628324 [DOI] [PubMed] [Google Scholar]
- 43.National Center for Biotechnology Information. PubChem Compound Summary for CID 60750, Gemcitabine. Accessed September 10, 2022. https://pubchem.ncbi.nlm.nih.gov/compound/Gemcitabine [Google Scholar]
- 44.Casper ES Green MR Kelsen DP, et al. Phase II trial of gemcitabine (2,2?-difiuorodeoxycytidine) in patients with adenocarcinoma of the pancreas. Invest New Drugs. 1994;12(1):29–34. doi: 10.1007/BF00873232 [DOI] [PubMed] [Google Scholar]
- 45.Leal F, Macedo LT, Carvalheira JBC. Gemcitabine-related thrombotic microangiopathy: a single-centre retrospective series. J Chemother. 2014;26(3):169–172. doi: 10.1179/1973947813Y.0000000122 [DOI] [PubMed] [Google Scholar]
- 46.Humphreys BD Sharman JP Henderson JM, et al. Gemcitabine-associated thrombotic microangiopathy. Cancer. 2004;100(12):2664–2670. doi: 10.1002/cncr.20290 [DOI] [PubMed] [Google Scholar]
- 47.Zupancic M, Shah PC, Shah-Khan F, Nagendra S. Gemcitabine-associated thrombotic thrombocytopenic purpura. Lancet Oncol. 2007;8(7):634–641. doi: 10.1016/S1470-2045(07)70203-6 [DOI] [PubMed] [Google Scholar]
- 48.De Smet D, Jochmans K, Neyns B. Development of thrombotic thrombocytopenic purpura after a single dose of gemcitabine. Ann Hematol. 2008;87(6):495–496. doi: 10.1007/s00277-007-0429-9 [DOI] [PubMed] [Google Scholar]
- 49.Reese JA Bougie DW Curtis BR, et al. Drug-induced thrombotic microangiopathy: experience of the Oklahoma registry and the BloodCenter of Wisconsin: drug-induced TMA. Am J Hematol. 2015;90(5):406–410. doi: 10.1002/ajh.23960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muto J, Kishimoto H, Kaizuka Y, Kinjo M, Higashi H, Kishihara F. Thrombotic microangiopathy following chemotherapy with S-1 and cisplatin in a patient with gastric cancer: a case report. In Vivo. 2017;31(3):439–441. doi: 10.21873/invivo.11080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Curtis BR Kaliszewski J Marques MB, et al. Immune-mediated thrombocytopenia resulting from sensitivity to oxaliplatin. Am J Hematol. 2006;81(3):199–201. doi: 10.1002/ajh.20516 [DOI] [PubMed] [Google Scholar]
- 52.Jodele S Dandoy CE Myers K, et al. High-dose carboplatin/etoposide/melphalan increases risk of thrombotic microangiopathy and organ injury after autologous stem cell transplantation in patients with neuroblastoma. Bone Marrow Transpl. 2018;53(10):1311–1318. doi: 10.1038/s41409-018-0159-8 [DOI] [PubMed] [Google Scholar]
- 53.Yin Q Guo N Zhou X, et al. Regorafenib-induced renal-limited thrombotic microangiopathy: a case report and review of literatures. BMC Nephrol. 2022;23(1):112. doi: 10.1186/s12882-021-02656-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nguyen MN, Nayernama A, Jones SC, Kanapuru B, Gormley N, Waldron PE. Proteasome inhibitor‐associated thrombotic microangiopathy: a review of cases reported to the FDA adverse event reporting system and published in the literature. Am J Hematol. 2020;95(9):E218–E222. doi: 10.1002/ajh.25832 [DOI] [PubMed] [Google Scholar]
- 55.Portuguese AJ, Lipe B. Carfilzomib-induced aHUS responds to early eculizumab and may be associated with heterozygous CFHR3-CFHR1 deletion. Blood Adv. 2018;2(23):3443–3446. doi: 10.1182/bloodadvances.2018027532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gosain R Gill A Fuqua J, et al. Gemcitabine and carfilzomib induced thrombotic microangiopathy: eculizumab as a life-saving treatment. Clin Case Rep. 2017;5(12):1926–1930. doi: 10.1002/ccr3.1214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lodhi A, Kumar A, Saqlain MU, Suneja M. Thrombotic microangiopathy associated with proteasome inhibitors. Clin Kidney J. 2015;8(5):632–636. doi: 10.1093/ckj/sfv059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Neverauskaite-Piliponiene G Cesas K Pranys D, et al. Fatal pulmonary tumour thrombotic microangiopathy in patient with ovarian adenocarcinoma: review and a case report. BMC Cardiovasc Disord. 2022;22(1):1. doi: 10.1186/s12872-021-02434-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.de Nattes T Moreau-Grangé L Vezzosi D, et al. Adrenocortical carcinoma complicated by renal thrombotic microangiopathy, a case-series. BMC Nephrol. 2020;21(1):35. doi: 10.1186/s12882-020-1703-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Palma LMP, Sridharan M, Sethi S. Complement in secondary thrombotic microangiopathy. Kidney Int Rep. 2021;6(1):11–23. doi: 10.1016/j.ekir.2020.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tarr PI. Shiga toxin-associated hemolytic uremic syndrome and thrombotic thrombocytopenic purpura: distinct mechanisms of pathogenesis. Kidney Int. 2009;75:S29–S32. doi: 10.1038/ki.2008.615 [DOI] [PubMed] [Google Scholar]
- 62.Zheng XL, Sadler JE. Pathogenesis of thrombotic microangiopathies. Annu Rev Pathol Mech Dis. 2008;3(1):249–277. doi: 10.1146/annurev.pathmechdis.3.121806.154311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lemoine M François A Grangé S, et al. Cobalamin C deficiency induces a typical histopathological pattern of renal arteriolar and glomerular thrombotic microangiopathy. Kidney Int Rep. 2018;3(5):1153–1162. doi: 10.1016/j.ekir.2018.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Epperla N Li A Logan B, et al. Incidence, risk factors for and outcomes of transplant‐associated thrombotic microangiopathy. Br J Haematol. 2020;189(6):1171–1181. doi: 10.1111/bjh.16457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Elsallabi O, Bhatt VR, Dhakal P, Foster KW, Tendulkar KK. Hematopoietic stem cell transplant-associated thrombotic microangiopathy. Clin Appl Thromb Hemost. 2016;22(1):12–20. doi: 10.1177/1076029615598221 [DOI] [PubMed] [Google Scholar]
- 66.Remuzzi G Rossi E Misiani R, et al. Prostacyclin and thrombotic microangiopathy. Semin Thromb Hemost. 1980;6(04):391–394. doi: 10.1055/s-2007-1005110 [DOI] [PubMed] [Google Scholar]
- 67.Zakarija A, Bennett C. Drug-induced thrombotic microangiopathy. Semin Thromb Hemost. 2005;31(6):681–690. doi: 10.1055/s-2005-925474 [DOI] [PubMed] [Google Scholar]
- 68.Aster RH, Bougie DW. Drug-induced immune thrombocytopenia. N Engl J Med. 2007;357(6):580–587. doi: 10.1056/NEJMra066469 [DOI] [PubMed] [Google Scholar]
- 69.Abou‐Ismail MY, Kapoor S, Citla Sridhar D, Nayak L, Ahuja S. Thrombotic microangiopathies: an illustrated review. Res Pract Thromb Haemost. 2022;6(3):e12708. doi: 10.1002/rth2.12708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Timmermans SAMEG Abdul-Hamid MA Potjewijd J, et al. C5b9 formation on endothelial cells reflects complement defects among patients with renal thrombotic microangiopathy and severe hypertension. J Am Soc Nephrol. 2018;29(8):2234–2243. doi: 10.1681/ASN.2018020184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang Y Yang C Zhou X, et al. Association between thrombotic microangiopathy and activated alternative complement pathway in malignant nephrosclerosis. Nephrol Dial Transplant. 2021;36(7):1222–1233. doi: 10.1093/ndt/gfaa280 [DOI] [PubMed] [Google Scholar]
- 72.Blasco M Martínez‐Roca A Rodríguez‐Lobato LG, et al. Complement as the enabler of carfilzomib‐induced thrombotic microangiopathy. Br J Haematol. 2021;193(1):181–187. doi: 10.1111/bjh.16796 [DOI] [PubMed] [Google Scholar]
- 73.Benhamou Y Baudel JL Wynckel A, et al. Are platelet transfusions harmful in acquired thrombotic thrombocytopenic purpura at the acute phase? experience of the French thrombotic microangiopathies reference center: platelet Transfusion in Thrombotic Thrombocytopenic Purpura. Am J Hematol. 2015;90(6):E127–E129. doi: 10.1002/ajh.23997 [DOI] [PubMed] [Google Scholar]
- 74.von Baeyer H. Plasmapheresis in thrombotic microangiopathy-associated syndromes: review of outcome data derived from clinical trials and open studies. Therapher Dial. 2002;6(4):320–328. doi: 10.1046/j.1526-0968.2002.00390.x [DOI] [PubMed] [Google Scholar]
- 75.Rock GA Shumak KH Buskard NA, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. N Engl J Med. 1991;325(6):393–397. doi: 10.1056/NEJM199108083250604 [DOI] [PubMed] [Google Scholar]
- 76.Padmanabhan A Connelly‐Smith L Aqui N, et al. Guidelines on the use of therapeutic Apheresis in clinical practice—evidence‐based approach from the writing committee of the American Society for Apheresis: the eighth special issue. J Clin Apher. 2019;34(3):171–354. doi: 10.1002/jca.21705 [DOI] [PubMed] [Google Scholar]
- 77.Gore EM, Jones BS, Marques MB. Is therapeutic plasma exchange indicated for patients with gemcitabine-induced hemolytic uremic syndrome? J Clin Apher. 2009;24(5):209–214. doi: 10.1002/jca.20213 [DOI] [PubMed] [Google Scholar]
- 78.Bendapudi PK Hurwitz S Fry A, et al. Derivation and external validation of the PLASMIC score for rapid assessment of adults with thrombotic microangiopathies: a cohort study. Lancet Haematol. 2017;4(4):e157–e164. doi: 10.1016/S2352-3026(17)30026-1 [DOI] [PubMed] [Google Scholar]
- 79.Li A, Khalighi PR, Wu Q, Garcia DA. External validation of the PLASMIC score: a clinical prediction tool for thrombotic thrombocytopenic purpura diagnosis and treatment. J Thromb Haemost. 2018;16(1):164–169. doi: 10.1111/jth.13882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Coppo P Schwarzinger M Buffet M, et al. Predictive features of severe acquired ADAMTS13 deficiency in idiopathic thrombotic microangiopathies: the French TMA reference center experience. PLoS One. 2010;5(4):e10208. doi: 10.1371/journal.pone.0010208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fage N Orvain C Henry N, et al. Proteinuria increases the PLASMIC and French scores performance to predict thrombotic thrombocytopenic purpura in patients with thrombotic microangiopathy syndrome. Kidney Int Rep. 2022;7(2):221–231. doi: 10.1016/j.ekir.2021.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liu A Dhaliwal N Upreti H, et al. Reduced sensitivity of PLASMIC and French scores for the diagnosis of thrombotic thrombocytopenic purpura in older individuals. Transfusion. 2021;61(1):266–273. doi: 10.1111/trf.16188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kasper S, Neurath MF, Huber C, Theobald M, Scharrer I. Protein A immunoadsorption therapy for refractory, mitomycin-C-associated thrombotic microangiopathy. Transfusion. 2007;47(7):1263–1267. doi: 10.1111/j.1537-2995.2007.01266.x [DOI] [PubMed] [Google Scholar]
- 84.Snyder HW Mittelman A Oral A, et al. Treatment of cancer chemotherapy-associated thrombotic thrombocytopenic purpura/hemolytic uremic syndrome by protein A immunoadsorption of plasma. Cancer. 1993;71(5):1882–1892. doi: [DOI] [PubMed] [Google Scholar]
- 85.Bharthuar A Egloff L Becker J, et al. Rituximab-based therapy for gemcitabine-induced hemolytic uremic syndrome in a patient with metastatic pancreatic adenocarcinoma: a case report. Cancer Chemother Pharmacol. 2009;64(1):177–181. doi: 10.1007/s00280-008-0900-x [DOI] [PubMed] [Google Scholar]
- 86.Gourley BL, Mesa H, Gupta P. Rapid and complete resolution of chemotherapy-induced thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS) with rituximab. Cancer Chemother Pharmacol. 2010;65(5):1001–1004. doi: 10.1007/s00280-010-1258-4 [DOI] [PubMed] [Google Scholar]
- 87.Ryu H Kang E Park S, et al. A case of gemcitabine-induced thrombotic microangiopathy in a urothelial tumor patient with a single kidney. Kidney Res Clin Pract. 2015;34(4):237–240. doi: 10.1016/j.krcp.2015.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hausberg M, Felten H, Pfeffer S. Treatment of chemotherapy-induced thrombotic microangiopathy with eculizumab in a patient with metastatic breast cancer. Case Rep Oncol. 2019;12(1):1–6. doi: 10.1159/000495031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Legendre CM Licht C Muus P, et al. Terminal complement inhibitor eculizumab in atypical hemolytic–uremic syndrome. N Engl J Med. 2013;368(23):2169–2181. doi: 10.1056/NEJMoa1208981 [DOI] [PubMed] [Google Scholar]
- 90.Burns ST, Damon L, Akagi N, Laszik Z, Ko AH. Rapid improvement in gemcitabine-associated thrombotic microangiopathy after a single dose of eculizumab: case report and review of the literature. Anticancer Res. 2020;40(7):3995–4000. doi: 10.21873/anticanres.14393 [DOI] [PubMed] [Google Scholar]
- 91.Facchini L Lucchesi M Stival A, et al. Role of eculizumab in a pediatric refractory gemcitabine-induced thrombotic microangiopathy: a case report. J Med Case Rep. 2017;11(1):209. doi: 10.1186/s13256-017-1373-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Krishnappa V Gupta M Shah H, et al. The use of eculizumab in gemcitabine induced thrombotic microangiopathy. BMC Nephrol. 2018;19(1):9. doi: 10.1186/s12882-018-0812-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rogier T Gerfaud-Valentin M Pouteil-Noble C, et al. [Clinical efficacy of eculizumab as treatment of gemcitabine-induced thrombotic microangiopathy: a case report]. La Revue de Médecine Interne 2016;37(10):701–704. doi: 10.1016/j.revmed.2015.12.027 [DOI] [PubMed] [Google Scholar]
- 94.Schulte-Kemna L Reister B Bettac L, et al. Eculizumab in chemotherapy-induced thrombotic microangiopathy. Clin Nephrol Case Stud. 2020;8(01):25–32. doi: 10.5414/CNCS109836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Efe O, Goyal L, Galway A, Zhu AX, Niles JL, Zonozi R. Treatment of gemcitabine-induced thrombotic microangiopathy followed by gemcitabine rechallenge with eculizumab. Kidney Int Rep. 2021;6(5):1464–1468. doi: 10.1016/j.ekir.2021.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Grall M Daviet F Chiche NJ, et al. Eculizumab in gemcitabine-induced thrombotic microangiopathy: experience of the French thrombotic microangiopathies reference centre. BMC Nephrol. 2021;22(1):267. doi: 10.1186/s12882-021-02470-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rondeau E Scully M Ariceta G, et al. The long-acting C5 inhibitor, Ravulizumab, is effective and safe in adult patients with atypical hemolytic uremic syndrome naïve to complement inhibitor treatment. Kidney Int. 2020;97(6):1287–1296. doi: 10.1016/j.kint.2020.01.035 [DOI] [PubMed] [Google Scholar]
- 98.Tanaka K Adams B Aris AM, et al. The long-acting C5 inhibitor, ravulizumab, is efficacious and safe in pediatric patients with atypical hemolytic uremic syndrome previously treated with eculizumab. Pediatr Nephrol. 2021;36(4):889–898. doi: 10.1007/s00467-020-04774-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jayne DRW, Merkel PA, Schall TJ, Bekker P. Avacopan for the treatment of ANCA-associated vasculitis. N Engl J Med. 2021;384(7):599–609. doi: 10.1056/NEJMoa2023386 [DOI] [PubMed] [Google Scholar]
- 100.Wang Y Johnston K Popoff E, et al. A US cost-minimization model comparing ravulizumab versus eculizumab for the treatment of atypical hemolytic uremic syndrome. J Med Econ. 2020;23(12):1503–1515. doi: 10.1080/13696998.2020.1831519 [DOI] [PubMed] [Google Scholar]
- 101.O’Connell T, Buessing M, Johnson S, Tu L, Thomas SK, Tomazos I. Cost-utility analysis of ravulizumab compared with eculizumab in adult patients with paroxysmal nocturnal hemoglobinuria. Pharmacoeconomics. 2020;38(9):981–994. doi: 10.1007/s40273-020-00929-z [DOI] [PubMed] [Google Scholar]
- 102.MacDougall KN, Schwartz B, Harewood J, Bukhari Z, Neculiseanu E. A case of gemcitabine-induced thrombotic microangiopathy treated with ravulizumab in a patient with stage IV pancreatic cancer. Cureus. 2021;13(1):e13031. doi: 10.7759/cureus.13031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Park CH Lee B Han M, et al. Canagliflozin protects against cisplatin-induced acute kidney injury by AMPK-mediated autophagy in renal proximal tubular cells. Cell Death Discov. 2022;8(1):12. doi: 10.1038/s41420-021-00801-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhang Y Nakano D Guan Y, et al. A sodium-glucose cotransporter 2 inhibitor attenuates renal capillary injury and fibrosis by a vascular endothelial growth factor–dependent pathway after renal injury in mice. Kidney Int. 2018;94(3):524–535. doi: 10.1016/j.kint.2018.05.002 [DOI] [PubMed] [Google Scholar]
- 105.Scully M Cataland SR Peyvandi F, et al. Caplacizumab treatment for acquired thrombotic thrombocytopenic purpura. N Engl J Med. 2019;380(4):335–346. doi: 10.1056/NEJMoa1806311 [DOI] [PubMed] [Google Scholar]
- 106.Higham CS Shimano KA Melton A, et al. A pilot trial of prophylactic defibrotide to prevent serious thrombotic microangiopathy in high‐risk pediatric patients. Pediatr Blood Cancer. 2022;69(5):e29641. doi: 10.1002/pbc.29641 [DOI] [PubMed] [Google Scholar]
- 107.Flombaum CD, Mouradian JA, Casper ES, Erlandson RA, Benedetti F. Thrombotic microangiopathy as a complication of long-term therapy with gemcitabine. Am J Kidney Dis. 1999;33(3):555–562. doi: 10.1016/S0272-6386(99)70194-0 [DOI] [PubMed] [Google Scholar]
- 108.Walter RB, Joerger M, Pestalozzi BC. Gemcitabine-associated hemolytic-uremic syndrome. Am J Kidney Dis. 2002;40(4):e16.1–e16.6. doi: 10.1053/ajkd.2002.35758 [DOI] [PubMed] [Google Scholar]
- 109.Turner JL, Reardon J, Bekaii-Saab T, Cataland SR, Arango MJ. Gemcitabine-associated thrombotic microangiopathy: response to complement inhibition and reinitiation of gemcitabine. Clin Colorectal Cancer. 2017;16(2):e119–e122. doi: 10.1016/j.clcc.2016.09.004 [DOI] [PubMed] [Google Scholar]