Abstract
Climate change is upon us, and it will have a major effect on both kidney disease and the nephrology practice. But the converse is also true: our treatment of kidney disease has an effect on the climate. Much attention has focused on how rising temperatures can lead to acute and CKD and health exacerbations in patients with established kidney disease. Climate change is also associated with rising air pollution from wildfires and industrial wastes and infectious diseases associated with flooding and changing habitats, all of which heighten the risk of acute and CKD. Less well recognized or understood are the ways nephrology practices, in turn, contribute to still more climate change. Hemodialysis, although lifesaving, can be associated with marked water usage (up to 600 L per dialysis session), energy usage (with one 4-hour session averaging as much as one fifth of the total energy consumed by a household per day), and large clinical wastes (with hemodialysis accounting for one third of total clinical medicine–associated waste). Of note, >90% of dialysis occurs in highly affluent countries, whereas dialysis is much less available in the poorer countries where climate change is having the highest effect on kidney disease. We conclude that not only do nephrologists need to prepare for the rise in climate-associated kidney disease, they must also urgently develop more climate-friendly methods of managing patients with kidney disease.
Keywords: clinical nephrology, climate
Introduction
Nephrologists must be aware that, although climate change is leading to higher rates of kidney disease, the care and treatment of those patients itself contributes to yet more climate change. The US health care industry accounts for 10% of the nation’s greenhouse gas emissions, a disproportionate amount of which is presumed to come from the care of patients with kidney disease (1). The United States has a sizable percentage of the world’s patients on dialysis (785,883 prevalent patients in 2018), but only one study, by Sehgal et al., has investigated the environmental footprint of US nephrology care (2,3). Addressing the global climate crisis requires that the dialysis industry and nephrologists in the United States follow the example of the United Kingdom and set targets to reduce waste, water, and energy consumption (4). In this article, we review the effect of the climate crisis on kidney disease, discuss the implications of climate change for patients with CKD and kidney failure, and report the existing evidence regarding the effect of dialysis and nephrology services on climate.
Climate Change Causes More Kidney Disease
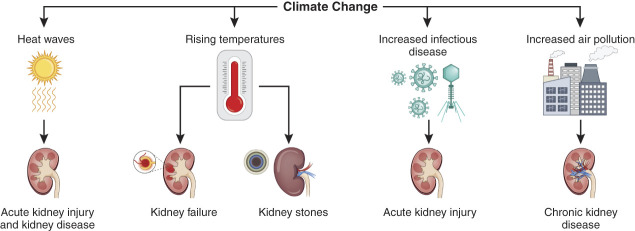
A growing literature shows that changing patterns of disease, water, and extreme weather events are linked to the development of kidney disease (5,6) (Figure 1). Not all populations are uniformly vulnerable to kidney disease. Unfortunately, the areas of the world most exposed to kidney complications of climate change are those least responsible for the current climate crisis. More worrisome, many of these regions have poor access to nephrology and dialysis services (7). Patients in the United States are no exception, becoming more at risk of extreme weather events such as hurricanes, floods, heat waves, and wildfires (8–11).
Figure 1.
Climate change mechanisms and their effect on the incidence and distribution of kidney disease. Created with BioRender.com.
AKI during extreme heat waves has been shown in geographically diverse locations over the past 30 years. AKI was recognized as an important cause of hospitalization as early as 1995 during a Chicago heat wave (12). In 2003 in Genoa, Italy, kidney failure was found to contribute to excess mortality among the elderly during an unprecedented heat wave that disproportionately affected the urban and elderly populations of Europe (13). Between 2000 and 2015, Brazil saw a higher risk of hospitalization from kidney disease of 0.9% for every 1° Celsius increase in daily mean temperature, which excessively affected the elderly (14). Heat waves also appear to lead to a disproportionate number of emergency department visits and hospitalizations for AKI in California; Black Americans may be particularly at risk (15). In total, 11% of agricultural workers working in hot and humid conditions in the United States will develop AKI by Kidney Disease Improving Global Outcomes (KDIGO) criteria after a work shift; and up to 33% of these will develop AKI on at least one workday (16,17). These studies raise the possibility that certain sectors of the population exposed to increasing temperatures may have recurrent subclinical or unrecognized injury.
CKD of unknown origin (CKDu) in agricultural workers was first recognized in El Salvador in 1990. CKDu, termed Mesoamerican nephropathy in Central America, is more common in men and was first described in young male sugar cane workers. It is characterized by kidney failure with minimal to no proteinuria in the absence of other traditional risk factors, such as diabetes and hypertension. Kidney biopsies show interstitial fibrosis, low-grade inflammation, tubular atrophy with glomerulosclerosis, and evidence of glomerular ischemia without overt vascular lesions (18). El Salvador, located on the Pacific coast of Central America, has some of the hottest regions in the Americas, and sugar cane workers are exposed to extreme heat while performing strenuous agricultural work. Although the top risk factor for developing CKDu in El Salvador is working in sugarcane, the second is working in hot temperatures (18,19). CKDu is the second leading cause of death in El Salvador and nearby Nicaragua (20).
Over the past three decades, CKDu has been described in agricultural workers in a variety of locations, including Mexico, Sri Lanka, India, Egypt, and Tunisia (21). In Sri Lanka, the epidemic of CKDu has occurred in the hottest areas of the country, the Northern Province, and in mostly male rice workers (22). In India, CKDu is affecting farmers in hot rural areas. In Uddanam, India, known for cashew and coconut farming, 13% of the population has CKD. In total, 73% of patients with CKD have CKDu and most of the patients are agricultural workers, matching the pattern seen in Central America and Sri Lanka (23). In Lebanon, heat exposure at work, such as that experienced by cooks and construction workers, was associated with a three-fold risk of dialysis among patients with kidney failure of undetermined origin (24). The common factors in these epidemics of CKDu are heat exposure, strenuous exercise, and volume depletion. On a planet with rising temperatures and increasing water shortages, this puts an increasing portion of the world’s population at risk of CKD and kidney failure.
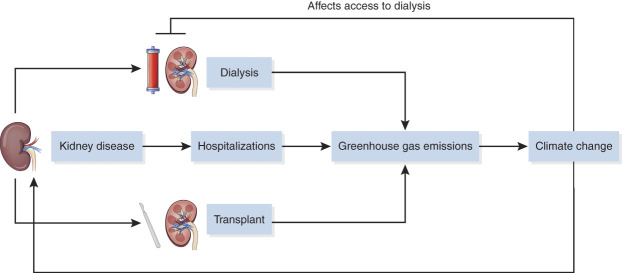
Beyond AKI and CKDu, climate change and rising temperatures are leading to higher rates and geographic redistribution of kidney stones and infectious diseases—both of which contribute to kidney disease (25,26). Kidney stones in the United States are most common in the southeastern region, but climate models predict a change in the geographic distribution of “the kidney stone belt” northward and westward (27). Infectious diseases traditionally restricted to specific geographic areas will spread, affecting populations with little or no immunity. Consequently, more people will develop AKI from these infectious diseases (28) (Figure 2).
Figure 2.
Relationship of climate change, infectious disease, and AKI.
Climate Change Affects Patients with Kidney Disease
As the number of extreme weather events increases, nephrologists and dialysis organizations need to plan for the provision of dialysis in the event of a natural disaster, including surges of patients and the influx of evacuees in neighboring centers.
During Hurricane Katrina, >5000 patients with kidney failure lived in the affected region. Patients who evacuated late or lived alone were much more likely to miss dialysis sessions; missing three treatments was associated with a risk for hospitalization (8). In a recent study, dialysis patients in the United States were observed to have a higher mortality in the 30 days after a storm (29). How hurricanes affect patients on dialysis cannot only be measured in mortality and missed dialysis, but also missed transplants. There was a 21% decline in kidney transplant services in the area a year after Katrina, leaving more patients dependent on dialysis because of the storm (30).
In the current coronavirus disease 2019 pandemic, patients on dialysis also are at risk during evacuations due to the crowding of people in evacuation facilities. Patients with kidney failure have a higher mortality from coronavirus disease 2019—approaching 25% (31)—so evacuating them to shelters puts them at particular risk.
Heat Waves
Hospitalizations and mortality from heat waves are potentially preventable. Recognizing vulnerable populations is essential to prevention. Advanced age, lower socioeconomic status, being non-White, and social isolation are all risk factors, and patients with CKD and kidney failure disproportionately reflect these risk factors. More specifically, elderly people with CKD are at substantial risk because of impairments in salt and water physiology, exacerbated by medications (32). Remigio et al. recently showed that urban patients on dialysis in the Northeast were at a higher risk of hospitalization and death during heat waves (9).
Air Pollutants
It has long been recognized that small particulate airborne pollutants are associated with higher rates of cardiovascular disease and a host of adverse pulmonary outcomes, but more recently, it has been suggested that particulate matter is associated with extra pulmonary disease and kidney disease specifically. In a cohort of US veterans, exposure to PM2.5 (particles with a mass median of aerodynamic diameter <2.5 μm) was associated with incident CKD, progression of CKD, and kidney failure (33). Most concerning, the risk of CKD begins well below the US Environmental Protection Agency's recommended level (12 mcg per m3), highlighting the need for improved air quality in the United States to protect public health. Patients on dialysis may be particularly susceptible to air pollutants because they are at elevated risk of cardiovascular disease. A recent study showed higher cardiovascular and all-cause mortality with ambient PM2.5 exposure in patients on dialysis, most pronounced in the elderly (34).
Environmental Effect of Dialysis: What We Know
Kidney disease and the need for dialysis are increasing worldwide. In 2010, an estimated 2.6 million people worldwide received dialysis, with an additional 2.3 million dying of kidney disease due to inadequate access. Around 93% of dialysis occurs in high- to upper-middle–income countries, with the highest number of patients in North America and Asia (7). Most patients receive hemodialysis, with a smaller percentage receiving peritoneal dialysis (PD) or transplant.
The environmental effect of dialysis alone is unknown, but we know the health care industry is a large emitter of greenhouse gas in the United States; because the United States has among the highest prevalence of patients on dialysis in the world, dialysis can be presumed to significantly contribute to this (35). The environmental effect of dialysis can be measured in three areas: water use, energy consumption, and waste management. The “carbon footprint” of dialysis can also be estimated.
Hemodialysis is an extremely water-hungry treatment. Water quality is essential to safe hemodialysis and depends on a sequence of purification and disinfection processes, which discard a large amount of unused water. Reverse osmosis (RO) machines are at the center of water treatment procedures in hemodialysis units and are very inefficient, often rejecting >50% of the water. This water is never in contact with a patient and does not pose a risk, but it is nonetheless discarded down the sewer. According to the Environmental Protection Agency, most US citizens use about 310 L of water a day (36), but a patient on dialysis requires one to two times this amount for a single treatment.
There have been successful efforts to reduce water usage in dialysis. In one Nephrocare center in France, water consumption was reduced from approximately 600 L per hemodialysis session to 300 L per session by updating the water system and decreasing the amount of rejected water (37). A dialysis facility in the United Kingdom was able to save 14,400 L per day of reject water by placing two RO in sequence. The reject water was collected from the first RO and used for the laundry room, while the second RO’s reject water was circulated back into the first RO system (38). But even with maximally efficient water treatment, dialysate flows of 500 ml per hour require 120 L for a 4-hour treatment, excluding priming or rinsing volumes. NxStage, which is widely used in the United States for home and in-hospital dialysis, does not rely on an RO and has lower dialysis flow rates, decreasing the obligatory water consumption. However, this is offset by an unknown amount of water required to prepare the prepackaged dialysis fluid and plastic bags that contain it. The Nxstage machine can be paired with a water treatment system, Pureflow SL, which produces pure water using deionization, thereby reducing the need to transport bags of dialysate (39). Unlike water treatment using reverse osmosis, deionization allows 100% of the source water to be used. The high water requirements of dialysis have renewed interest in sorbent technology, which allows dialysate effluent to be regenerated into pure water, dialysate, and returned to the patient. With sorbent technology, the amount of water per treatment could be reduced from 140 to <10 L (40,41).
Energy consumption in hemodialysis has been incompletely studied. Energy use is dependent on both the method (home versus in-center) and machine. Energy consumption includes both the energy required to provide the treatment and the energy needed to maintain the building and transport patients and staff. Sehgal et al. found that electricity accounted for 27% of emissions in US dialysis facilities in Ohio, but the contributors to the energy use were unidentified (3). An Australian study to evaluate the cost-effectiveness of solar-assisted hemodialysis found the combination of a dialysis machine and RO system to require approximately 6 KwH per treatment (42). In comparison, the average household energy consumption in the United States is around 30 kWh per day (43). NxStage (with its lower flow rates) has a quarter of the energy demand (44), but a full accounting would require measuring the energy required to produce the dialysate and prepackaged dialysate bags.
Central RO units account for 60%–75% of the total energy consumed by in-center dialysis facilities. In a 12- and 15-chair unit in Australia, the average daily energy consumption was 271.5 and 325.0 kWh, equivalent to the energy required by a US household for 10 days (40). The environmental effect of energy consumption, of course, depends on the method of generation (e.g., coal versus solar), which have differing effects on climate. To mitigate the environmental effect of dialysis, facilities should focus on powering units with renewable energy, which promises to be both cost effective and environmentally responsible (42).
Dialysis units generate a large amount of both hazardous and general waste. Prepackaged dialysis supplies add to solid waste from dialyzers, tubing, syringes, and needles. Waste exposed to patients must be incinerated before disposal, creating significant emissions. A single hemodialysis session in the United Kingdom has been shown to generate 2.5 kg of clinical waste exposed to human tissue, of which 38% is plastic (45). Waste generated by dialysis units accounts for an estimated 30% of clinical waste in the United Kingdom (45).
The combined effect of water usage, energy consumption, and waste generation by different forms of hemodialysis can be better understood by documenting the carbon footprint of the different modalities. With this aim, Connor et al. measured the carbon footprint of home and in-center hemodialysis modalities in the United Kingdom. Traditional in-center hemodialysis 3× per week had a carbon footprint of 3.8 tons of CO2 annually, 20% of which was energy use. The carbon footprint of home hemodialysis using paired RO and hemodialysis machines ranged from a high of 7.9 tons to a low of 3.9 tons, depending on the frequency of the treatment. In comparison, Nxstage’s carbon footprint ranged from 1.8 to 2.1 tons for patients receiving five or six treatments per week. Nxstage had lower CO2 emissions attributed to energy (169 kg CO2 versus 796 kg CO2) (46). Given its lower environmental footprint, it may be able to be used at increased frequency before meeting the “break even” environmental effect of in-center hemodialysis.
A recent study in the United States measured the greenhouse gas emissions of 15 dialysis facilities belonging to a nonprofit dialysis organization. The largest contributors to emissions were patient and staff travel, electricity, and natural gas. Most notable was the large variation in emissions between facilities due to differences in transportation, natural gas, and water use (3). This study suggests that current facilities vary widely in their environmental footprint, and identifying best practices will help the community at large reduce its emissions. Further studies are needed to compare the carbon footprint of home and in-center hemodialysis, especially in the United States where patients and staff travel large distances by car and the public transportation infrastructure is limited.
Although there is a scarcity of studies evaluating the environmental effect of hemodialysis, there are even fewer for PD. Patients on continuous ambulatory PD use on average 10 L (4 × 2.5 L) per treatment. Although this is the most common method of dialysis worldwide, in the United States, most patients on PD are on cyclers and use significantly larger volumes than continuous ambulatory (CAPD). How much water is used to generate both the dialysate and its plastic bags is undocumented (but potentially knowable by the pharmaceutical manufacturers). The waste generated for CAPD has been reported at 1.7 kg per day, which (because CAPD is performed daily) makes it higher than that reported for hemodialysis (45). The only study looking at the carbon footprint of PD, by Chen et al., found packaging consumption accounted for more than 80% of the carbon footprint (47). Although the procedures of performing PD in China are significantly different than in the United States, making extrapolation difficult, one commonality is the large amount of packaging materials. The carbon footprint of 1400 kg CO2 annually per patient on PD in China is well below what has been measured for hemodialysis, but there were significant differences in methods (46–48).
We cannot be sure there is an environmental benefit to PD. However, recent innovations in PD that reduce its carbon footprint include a PD system that produces pure water for dialysate and runs on solar power and methods to generate dialysate from tap water (49). Both of these innovations will reduce the need to transport bags of dialysis fluid to patients.
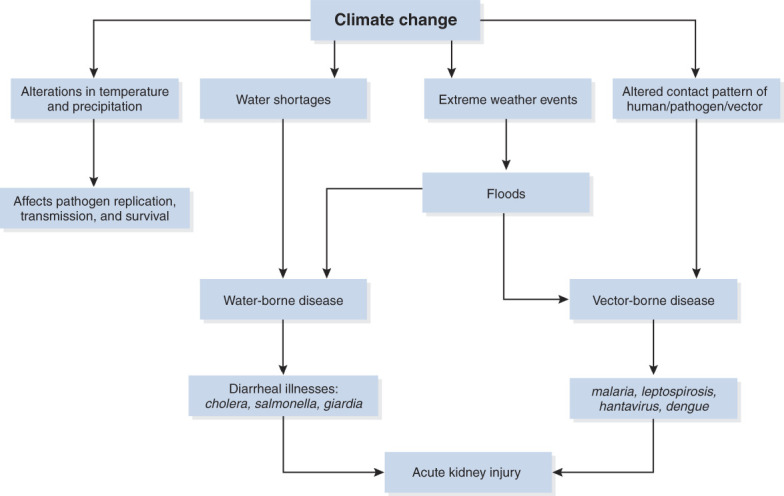
Transplant is presumed to be superior to PD and hemodialysis, but no studies have evaluated the carbon footprint of transplant. In 2017, almost 4000 patients received preemptive kidney transplants, saving the water, energy, and waste generated by dialysis; but what is the carbon footprint of the hospital, doctor visits, and pharmaceuticals needed to support our transplant centers? In a meeting abstract in 2016 at the American Transplant Congress, Grafals et al. reported they compared the environmental effect of hemodialysis, PD, and transplant for 15 years of kidney function. In their model, transplant reduced overall environmental effects by 96% compared with hemodialysis and 91% compared with PD (50) (Figure 3). These data counsel a new urgency to decrease barriers to transplant. Increasing access to transplant, more efficient organ donation, and championing living donors whenever possible can mitigate the carbon footprint of dialysis.
Figure 3.
Increased incidence of kidney disease leads to increased dialysis, hospitalizations, and transplant. These clinical activities contribute to greenhouse gas emissions. Climate change perpetuates kidney disease and affects access to dialysis. Created with BioRender.com.
In light of the environmental consequences of dialysis, nephrologists must redouble efforts to prevent and slow progression of CKD from increasing rates of obesity and diabetes. Public health measures to promote cycling and walking over car transportation, and initiatives to promote sustainable eating practices, have the combined benefits of improving public health and reducing global emissions (5).
Nephrologists should be aware of their own effect on climate. Medical directors of dialysis clinics must advocate to reduce waste, upgrade water systems, and implement clinic-specific practices to minimize energy consumption and adopt renewable energy. Physicians need to prepare patients for extreme weather and educate them about the risks from rising temperatures. Researchers need to explore the links between climate change and adverse health outcomes in patients with CKD and kidney failure. But we need not wait for the results of such studies to begin a concerted effort to reduce the carbon footprint of the dialysis industry.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Disclosures
R.J. Johnson reports having consultancy agreements with Horizon Pharmaceuticals; reports having ownership interest in Colorado Research Partners LLC (founder shares); reports receiving research funding from the National Institutes of Health and Veteran's Administration; reports receiving honoraria from Horizon Pharmaceutical and universities; reports having patents or patent applications on uric acid and fructose metabolism; reports receiving royalties from Comprehensive Clinical Nephrology (Elsevier) and Nature Wants Us to Be Fat (BenBella); and reports having stocks in XORTX Therapeutics. S.E. Young reports consultancy agreements with Horizon Therapeutics. The remaining author has nothing to disclose.
Funding
None.
Author Contributions
R.J. Johnson and S.E. Young conceptualized the review; R.J. Johnson provided supervision; L.J. Khoshnaw and S.E. Young were responsible for the visualization; S.E. Young wrote the original draft; and R.J. Johnson, L.J. Khoshnaw, and S.E. Young reviewed and edited the manuscript.
References
- 1.Eckelman MJ, Sherman J: Environmental impacts of the U.S. Health care system and effects on public health. PLoS One 11: e0157014, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States Renal Data System: 2020 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Available at: https://adr.usrds.org/2020. Accessed July 1, 2022 [Google Scholar]
- 3.Sehgal AR, Slutzman JE, Huml AM: Sources of variation in the carbon footprint of hemodialysis treatment. J Am Soc Nephrol 33: 1790–1795, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NHS England: Delivering a 'Net Zero' National Health Service. National Health Service England, United Kingdom, 2022 . [Google Scholar]
- 5.Barraclough KA, Blashki GA, Holt SG, Agar JWM: Climate change and kidney disease-threats and opportunities. Kidney Int 92: 526–530, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Johnson RJ, Wesseling C, Newman LS: Chronic kidney disease of unknown cause in agricultural communities. N Engl J Med 380: 1843–1852, 2019 [DOI] [PubMed] [Google Scholar]
- 7.Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, Zhao MH, Lv J, Garg AX, Knight J, Rodgers A, Gallagher M, Kotwal S, Cass A, Perkovic V: Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet 385: 1975–1982, 2015 [DOI] [PubMed] [Google Scholar]
- 8.Anderson AH, Cohen AJ, Kutner NG, Kopp JB, Kimmel PL, Muntner P: Missed dialysis sessions and hospitalization in hemodialysis patients after Hurricane Katrina. Kidney Int 75: 1202–1208, 2009 [DOI] [PubMed] [Google Scholar]
- 9.Remigio RV, Jiang C, Raimann J, Kotanko P, Usvyat L, Maddux FW, Kinney P, Sapkota A: Association of extreme heat events with hospital admission or mortality among patients with end-stage renal disease. JAMA Netw Open 2: e198904, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Remigio RV, Turpin R, Raimann JG, Kotanko P, Maddux FW, Sapkota AR, Liang X-Z, Puett R, He X, Sapkota A:. Assessing proximate intermediates between ambient temperature, hospital admissions, and mortality in hemodialysis patients. Environ Res 204: 112127, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xi Y, Kshirsagar AV, Wade TJ, Richardson DB, Brookhart MA, Wyatt L, Rappold AG: Mortality in US hemodialysis patients following exposure to wildfire smoke. J Am Soc Nephrol 31: 1824–1835, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Semenza JC, McCullough JE, Flanders WD, McGeehin MA, Lumpkin JR: Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med 16: 269–277, 1999 [DOI] [PubMed] [Google Scholar]
- 13.Conti S, Masocco M, Meli P, Minelli G, Palummeri E, Solimini R, Toccaceli V, Vichi M: General and specific mortality among the elderly during the 2003 heat wave in Genoa (Italy). Environ Res 103: 267–274, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Wen B, Xu R, Wu Y, de Sousa Zanotti Stagliorio Coêlho M, Hilario Nascimento Saldiva P, Guo Y, Li S: Association between Ambient Temperature and Hospitalization for Renal Diseases in Brazil during 2000–2015: A Nationwide Case-Crossover Study. Lancet Public Health Am 6: 100101, 2022 [DOI] [PMC free article] [PubMed]
- 15.Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, Trent R, English P: The 2006 California heat wave: Impacts on hospitalizations and emergency department visits. Environ Health Perspect 117: 61–67, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moyce S, Joseph J, Tancredi D, Mitchell D, Schenker M: Cumulative incidence of acute kidney injury in California’s agricultural workers. J Occup Environ Med 58: 391–397, 2016 [DOI] [PubMed] [Google Scholar]
- 17.Mix J, Elon L, Vi Thien Mac V, Flocks J, Economos E, Tovar-Aguilar AJ, Stover Hertzberg V, McCauley LA: Hydration status, kidney function, and kidney injury in Florida agricultural workers. J Occup Environ Med 60: e253–e260, 2018 [DOI] [PubMed] [Google Scholar]
- 18.Glaser J, Lemery J, Rajagopalan B, Diaz HF, García-Trabanino R, Taduri G, Madero M, Amarasinghe M, Abraham G, Anutrakulchai S, Jha V, Stenvinkel P, Roncal-Jimenez C, Lanaspa MA, Correa-Rotter R, Sheikh-Hamad D, Burdmann EA, Andres-Hernando A, Milagres T, Weiss I, Kanbay M, Wesseling C, Sánchez-Lozada LG, Johnson RJ: Climate change and the emergent epidemic of CKD from heat stress in rural communities: The case for heat stress nephropathy. Clin J Am Soc Nephrol 11: 1472–1483, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansson E, Mansourian A, Farnaghi M, Petzold M, Jakobsson K: An ecological study of chronic kidney disease in five Mesoamerican countries: Associations with crop and heat. BMC Public Health 21: 840, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.GBD 2019 Diseases and Injuries Collaborators : Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396: 1204–1222, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aguilar-Ramirez D, Raña-Custodio A, Villa A, Rubilar X, Olvera N, Escobar A, Johnson RJ, Sanchez-Lozada L, Obrador GT, Madero M: Decreased kidney function and agricultural work: A cross-sectional study in middle-aged adults from Tierra Blanca, Mexico. Nephrol Dial Transplant 36: 1030–1038, 2021 [DOI] [PubMed] [Google Scholar]
- 22.Wanigasuriya KP, Peiris-John RJ, Wickremasinghe R, Hittarage A: Chronic renal failure in North Central Province of Sri Lanka: An environmentally induced disease. Trans R Soc Trop Med Hyg 101: 1013–1017, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Tatapudi RR, Rentala S, Gullipalli P, Komarraju AL, Singh AK, Tatapudi VS, Goru KB, Bhimarasetty DM, Narni H: High prevalence of CKD of unknown etiology in Uddanam, India. Kidney Int Rep 4: 380–389, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doueihy C, Chelala D, Ossaili H, Hachem GE, Zeidan S, Ghoul BE, Aoun M: Occupational heat exposure as a risk factor for end-stage kidney disease: A case-control study. J Occup Environ Med 64: e103–e108, 2022 [DOI] [PubMed] [Google Scholar]
- 25.Romero V, Akpinar H, Assimos DG: Kidney stones: A global picture of prevalence, incidence, and associated risk factors. Rev Urol 12: e86–e96, 2010 [PMC free article] [PubMed] [Google Scholar]
- 26.Tasian GE Pulido JE Gasparrini A Saigal CS Horton BP Landis JR Madison R Keren R; Urologic Diseases in America Project : Daily mean temperature and clinical kidney stone presentation in five U.S. metropolitan areas: A time-series analysis. Environ Health Perspect 122: 1081–1087, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brikowski TH, Lotan Y, Pearle MS: Climate-related increase in the prevalence of urolithiasis in the United States. Proc Natl Acad Sci U S A 105: 9841–9846, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu X, Lu Y, Zhou S, Chen L, Xu B: Impact of climate change on human infectious diseases: Empirical evidence and human adaptation. Environ Int 86: 14–23, 2016 [DOI] [PubMed] [Google Scholar]
- 29.Blum MF, Feng Y, Anderson GB, Segev DL, McAdams-DeMarco M, Grams ME: Hurricanes and mortality among patients receiving dialysis. J Am Soc Nephrol 33: 1757–1766, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kopp JB, Ball LK, Cohen A, Kenney RJ, Lempert KD, Miller PE, Muntner P, Qureshi N, Yelton SA: Kidney patient care in disasters: Lessons from the hurricanes and earthquake of 2005. Clin J Am Soc Nephrol 2: 814–824, 2007 [DOI] [PubMed] [Google Scholar]
- 31.Hsu CM, Weiner DE, Aweh G, Miskulin DC, Manley HJ, Stewart C, Ladik V, Hosford J, Lacson EC, Johnson DS, Lacson E, Jr: COVID-19 Among US dialysis patients: Risk factors and outcomes from a national dialysis provider. Am J Kidney Dis 77: 748–756.e1, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O: Heat stress in older individuals and patients with common chronic diseases. CMAJ 182: 1053–1060, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z: Particulate matter air pollution and the risk of incident CKD and progression to ESRD. J Am Soc Nephrol 29: 218–230, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xi Y, Richardson DB, Kshirsagar AV, Wade TJ, Flythe JE, Whitsel EA, Peterson GC, Wyatt LH, Rappold AG: Effects of short-term ambient PM2.5 exposure on cardiovascular disease incidence and mortality among U.S. hemodialysis patients: A retrospective cohort study. Environ Health 21: 33, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eckelman MJ, Huang K, Lagasse R, Senay E, Dubrow R, Sherman JD: Health care pollution and public health damage in the United States: An update. Health Aff (Millwood) 39: 2071–2079, 2020 [DOI] [PubMed] [Google Scholar]
- 36.Dieter CA, Maupin MA, Caldwell RR, Harris MA, Ivahnenko TI, Lovelace JK, Barber NL, Linsey KS: Estimated Use of Water in the United States in 2015: U.S. Geological Survey Circular 1441. Reston, VA, USGS, 2018 [Google Scholar]
- 37.Bendine G, Autin F, Fabre B, Bardin O, Rabasco F, Cabanel JM, Chazot C: Haemodialysis therapy and sustainable growth: A corporate experience in France. Nephrol Dial Transplant 35: 2154–2160, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Connor A, Milne S, Owen A, Boyle G, Mortimer F, Stevens P: Toward greener dialysis: A case study to illustrate and encourage the salvage of reject water. J Ren Care 36: 68–72, 2010 [DOI] [PubMed] [Google Scholar]
- 39.NxStage Medical Inc : Therapy Handbook: NxStage Hemodialysis Treatment, Lawrence, MA, NxStage Medical, Inc., 2019 [Google Scholar]
- 40.Barraclough KA, Agar JWM: Green nephrology. Nat Rev Nephrol 16: 257–268, 2020 [DOI] [PubMed] [Google Scholar]
- 41.Vanholder R, Agar J, Braks M, Gallego D, Gerritsen KGF, Harber M, Noruisiene E, Pancirova J, Piccoli GB, Stamatialis D, Wieringa F: The European Green Deal and nephrology: A call for action by the European Kidney Health Alliance (EKHA). Nephrol Dial Transplant gfac160, 2022 [DOI] [PubMed] [Google Scholar]
- 42.Agar JW, Perkins A, Tjipto A: Solar-assisted hemodialysis. Clin J Am Soc Nephrol 7: 310–314, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.U.S. Energy Information Administration: U.S. Energy Information Administration (EIA), 2010 to 2021. Available at: http://www.eia.gov/. Accessed October 21, 2022
- 44.Connor A, Lillywhite R, Cooke MW: The carbon footprint of a renal service in the United Kingdom. QJM 103: 965–975, 2010 [DOI] [PubMed] [Google Scholar]
- 45.Hoenich NA, Levin R, Pearce C: Clinical waste generation from renal units: Implications and solutions. Semin Dial 18: 396–400, 2005 [DOI] [PubMed] [Google Scholar]
- 46.Connor A, Lillywhite R, Cooke MW: The carbon footprints of home and in-center maintenance hemodialysis in the United Kingdom. Hemodial Int 15: 39–51, 2011 [DOI] [PubMed] [Google Scholar]
- 47.Chen M, Zhou R, Du C, Meng F, Wang Y, Wu L, Wang F, Xu Y, Yang X: The carbon footprints of home and in-center peritoneal dialysis in China. Int Urol Nephrol 49: 337–343, 2017 [DOI] [PubMed] [Google Scholar]
- 48.Lim AE, Perkins A, Agar JW: The carbon footprint of an Australian satellite haemodialysis unit. Aust Health Rev 37: 369–374, 2013 [DOI] [PubMed] [Google Scholar]
- 49.Foo MWY, Htay H: Innovations in peritoneal dialysis. Nat Rev Nephrol 16: 548–549, 2020 [DOI] [PubMed] [Google Scholar]
- 50.Grafals M, Sanchez R: The Environmental Impact of Dialysis vs Transplantation. In: 2016 American Transplant Congress. Boston, MA, 2016