Abstract
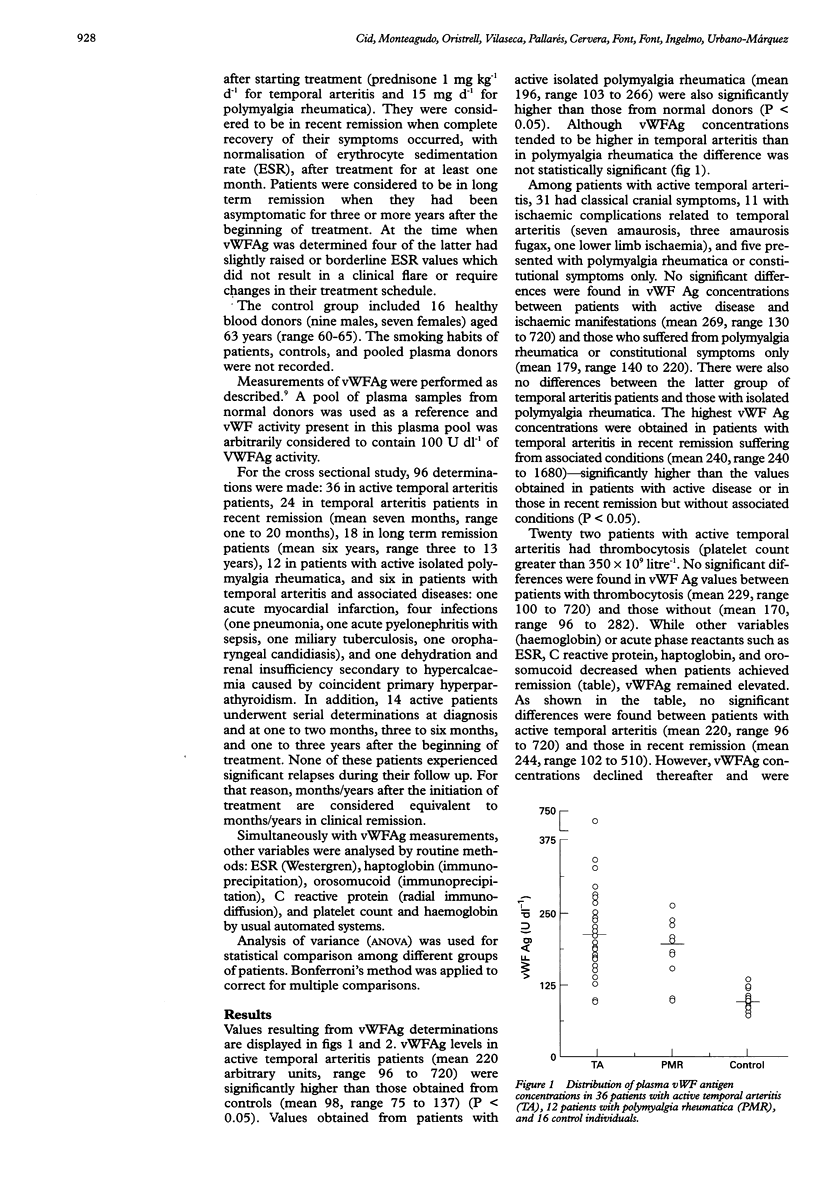
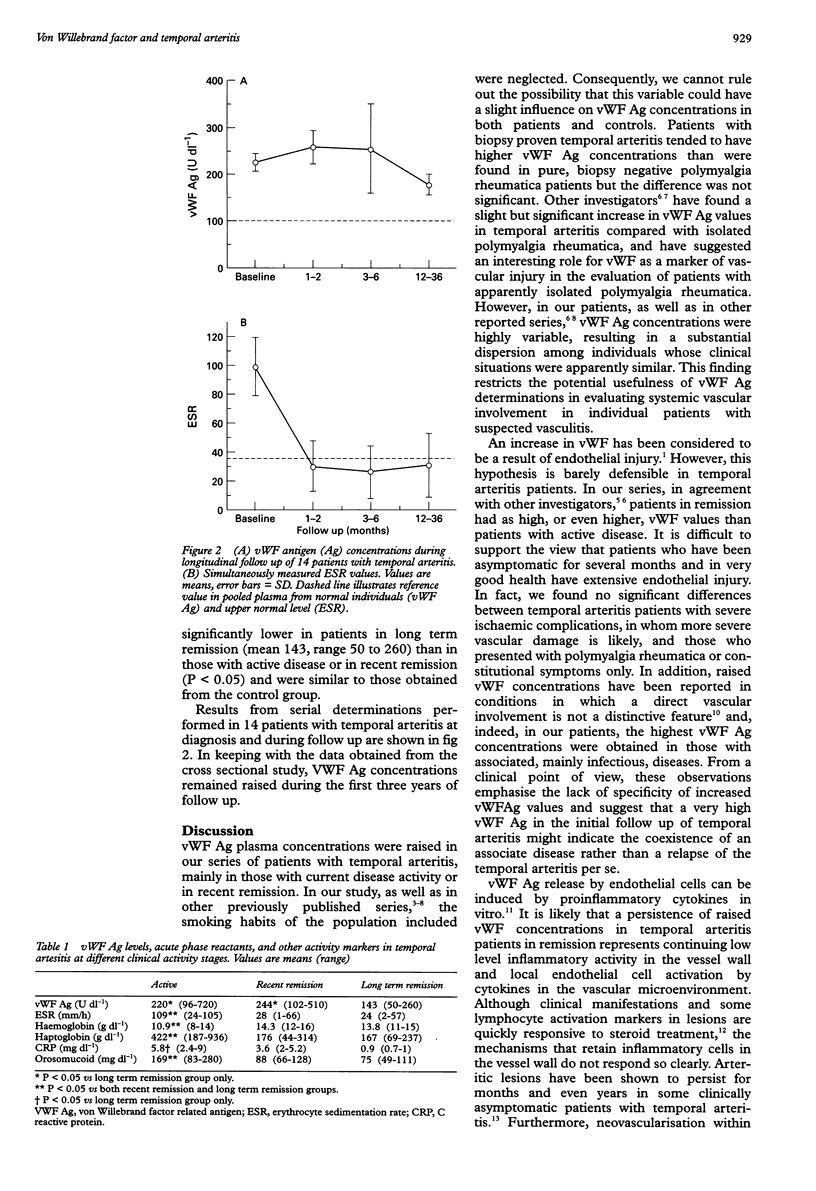
OBJECTIVE: To determine fluctuation in circulating von Willebrand factor (vWF) in the outcome of patients with temporal arteritis. METHODS: Plasma vWF antigen concentrations were measured in 65 patients with biopsy proven temporal arteritis at different disease activity stages, in 12 with isolated polymyalgia rheumatica, and in 16 controls. Fourteen temporal arteritis patients underwent serial determinations during the course of their disease. RESULTS: vWF concentrations were significantly raised in temporal arteritis (mean 220 [arbitrary units], range 96 to 720) and in polymyalgia rheumatica (mean 196, range 103 to 266) compared with healthy controls (mean 98, range 75 to 137) (P < 0.05). Although vWF values tended to be higher in temporal arteritis, no significant differences were found between temporal arteritis and polymyalgia rheumatica patients nor between temporal arteritis patients with ischaemic complications (mean 269, range 130 to 720) and those who presented with polymyalgia rheumatica or constitutional symptoms only (mean 179, range 140 to 220). The highest levels were obtained in patients with associated, mainly infectious, diseases (mean 631, range 240 to 1680). Raised vWF values found in active temporal arteritis patients (mean 220, range 96 to 720) persisted within the first two years after the beginning of treatment (mean 244, range 102 to 510) but tended to normalise in patients in long term remission (mean 143, range 50 to 260). CONCLUSIONS: Persistent elevation of vWF during early remission of temporal arteritis might represent an endothelial activation status induced by a remaining inflammatory microenvironment rather than a marker of endothelial cell injury. In long term remission, decreasing vWF concentrations might reflect progression of inflammatory lesions to a healing stage.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blann A. D. von Willebrand factor as a marker of injury to the endothelium in inflammatory vascular disease. J Rheumatol. 1993 Sep;20(9):1469–1471. [PubMed] [Google Scholar]
- Cid M. C., Campo E., Ercilla G., Palacin A., Vilaseca J., Villalta J., Ingelmo M. Immunohistochemical analysis of lymphoid and macrophage cell subsets and their immunologic activation markers in temporal arteritis. Influence of corticosteroid treatment. Arthritis Rheum. 1989 Jul;32(7):884–893. [PubMed] [Google Scholar]
- Cid M. C., Grant D. S., Hoffman G. S., Auerbach R., Fauci A. S., Kleinman H. K. Identification of haptoglobin as an angiogenic factor in sera from patients with systemic vasculitis. J Clin Invest. 1993 Mar;91(3):977–985. doi: 10.1172/JCI116319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauchald P., Rygvold O., Oystese B. Temporal arteritis and polymyalgia rheumatica. Clinical and biopsy findings. Ann Intern Med. 1972 Dec;77(6):845–852. doi: 10.7326/0003-4819-77-6-845. [DOI] [PubMed] [Google Scholar]
- Federici A. B., Fox R. I., Espinoza L. R., Zimmerman T. S. Elevation of von Willebrand factor is independent of erythrocyte sedimentation rate and persists after glucocorticoid treatment in giant cell arteritis. Arthritis Rheum. 1984 Sep;27(9):1046–1049. doi: 10.1002/art.1780270912. [DOI] [PubMed] [Google Scholar]
- Mazzone D., Fichera A., Praticò G., Sciacca F. Factor VIII activity and factor VIII-related antigen in infants with viral bronchiolitis. N Engl J Med. 1984 Nov 8;311(19):1257–1258. doi: 10.1056/NEJM198411083111915. [DOI] [PubMed] [Google Scholar]
- Monteagudo J., Pereira A., Roig S., Reverter J. C., Ordinas A., Castillo R. Investigation of plasma von Willebrand factor and circulating platelet aggregating activity in mitomycin C-related hemolytic-uremic syndrome. Am J Hematol. 1990 Jan;33(1):46–49. doi: 10.1002/ajh.2830330109. [DOI] [PubMed] [Google Scholar]
- Nordborg E., Andersson R., Tengborn L., Edén S., Bengtsson B. A. von Willebrand factor antigen and plasminogen activator inhibitor in giant cell arteritis. Ann Rheum Dis. 1991 May;50(5):316–320. doi: 10.1136/ard.50.5.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nusinow S. R., Federici A. B., Zimmerman T. S., Curd J. G. Increased von Willebrand factor antigen in the plasma of patients with vasculitis. Arthritis Rheum. 1984 Dec;27(12):1405–1410. doi: 10.1002/art.1780271211. [DOI] [PubMed] [Google Scholar]
- Olsson A., Elling P., Elling H. Serological and immunohistochemical determination of von Willebrand factor antigen in serum and biopsy specimens from patients with arteritis temporalis and polymyalgia rheumatica. Clin Exp Rheumatol. 1990 Jan-Feb;8(1):55–58. [PubMed] [Google Scholar]
- Paleolog E. M., Crossman D. C., McVey J. H., Pearson J. D. Differential regulation by cytokines of constitutive and stimulated secretion of von Willebrand factor from endothelial cells. Blood. 1990 Feb 1;75(3):688–695. [PubMed] [Google Scholar]
- Persellin S. T., Daniels T. M., Rings L. J., Kazmier F. J., Bowie E. J., Hunder G. G. Factor VIII-von Willebrand factor in giant cell arteritis and polymyalgia rheumatica. Mayo Clin Proc. 1985 Jul;60(7):457–462. doi: 10.1016/s0025-6196(12)60869-6. [DOI] [PubMed] [Google Scholar]
- Reidy M. A., Chopek M., Chao S., McDonald T., Schwartz S. M. Injury induces increase of von Willebrand factor in rat endothelial cells. Am J Pathol. 1989 Apr;134(4):857–864. [PMC free article] [PubMed] [Google Scholar]
- Woolf A. D., Wakerley G., Wallington T. B., Scott D. G., Dieppe P. A. Factor VIII related antigen in the assessment of vasculitis. Ann Rheum Dis. 1987 Jun;46(6):441–447. doi: 10.1136/ard.46.6.441. [DOI] [PMC free article] [PubMed] [Google Scholar]



