Abstract
Background and Objectives:
Many highly capitated systems still pay physicians based on relative value units (RVUs) which may lead to excessive office visits. We reviewed electronic health records from the family medicine clinic panel members of 97 physicians and 42 residents to determine if a change from RVU to panel-based compensation influenced care delivery as defined by the number of office visits and telephone contacts per panel member per month.
Methods:
A retrospective analysis of the electronic health records of patients seen in four residency training clinics, ten community clinics, and four regional clinics was conducted. We assessed face-to-face care delivery and telephone call volume for the clinics individually and for the clinics pooled by clinic type from one year before to at least one year after the change.
Results:
Change in physician compensation was not found to have an effect on office visits or telephone calls per panel member per month when pooled by clinic categories. Some significant effects were seen in individual clinics without any clear patterns by clinic size or type.
Conclusions:
Change in physician compensation was not a key driver of care delivery in family medicine clinics. Understanding changes in care delivery may require looking at a broad array of system, physician, and patient factors.
Keywords: health care delivery, pay for performance
INTRODUCTION
Physician compensation is an important aspect of primary care clinic operations that has the potential to influence care delivery. Physicians who are paid more to deliver more services typically do so.1 This method of compensation rewards physicians who see a higher volume of patients and deliver a higher complexity of services. In some situations, this incentivizes desirable behavior, to deliver comprehensive care to patients in need. This method, however, has the potential to incentivize overutilization and inefficient care.2–4 In contrast, value-based or capitated health systems receive per-member-per-month payments that are not dependent on the patient coming into the office to receive care. A 2022 study of physician compensation arrangements in the US found that despite a move towards value-based reimbursement from payers, physician compensation remains largely based on volume-related incentives.5
While many advocate for a shift in physician compensation approaches,6,7 little is known about how a change to physician compensation impacts care delivery in outpatient primary care clinics. A 1990 Danish study8 showed that general practitioners who moved from a capitated system to part capitation, part fee-for-service compensation system, provided a larger number of contacts with patients (both telephone and face-to-face) with fewer referrals to specialists and hospitals.9 A 2021 study found no difference in the delivery of preventive services in salaried as compared to productivity-based or mixed compensation plans.10 Our previous work showed that a shift from compensation based on relative value units (RVUs) towards compensation based on panel size resulted in an increase in panel size for family physicians with variable changes in physician RVU productivity.11 Our other previous work has shown increased physician satisfaction and retention with a similar change in compensation structure.12 We did not find any literature exploring the impact of physician compensation changes on patient-level outcomes (number of visits and telephone calls per patient) rather than physician-level outcomes (RVUs per physician).
The purpose of this paper is to assess the impact of a change in family physician compensation on care delivery in the outpatient setting as measured by office visits and telephone call encounters per panel member per month, trended over time. We hypothesized that with this change in compensation, physicians would adopt a practice style in which patients are seen in the office less often and more care is provided via telephone.
METHODS
Setting
The University of Wisconsin-Madison (UW) Department of Family Medicine and Community Health (DFMCH) is one of the largest family medicine departments in the U.S., with sites in urban and rural communities throughout Wisconsin. The data analyzed in this study includes four residency training sites (42 residents and 32 faculty physicians), 10 community practices (52 physicians) in Dane County, WI and 4 regional sites (13 physicians) in nearby counties. Sources of revenue in these clinics in 2014 were 60% fee-for-service and 40% capitation. The DFMCH is part of UW Health, a public academic health system consisting of a school of medicine and public health, a nonprofit hospital, and a large multispecialty physician practice group. At the time of this study the health system was growing with no major changes to relationships to local payers. This project was considered exempt from human subject review under the quality improvement designation.
In 2013, based on the large capitated population relative to fee for service and an increasing focus on managing populations, as well as a realization that salaries had fallen behind the local market rates, the DFMCH abandoned its RVU-based physician compensation plan in favor of one based primarily on panel size.11 Physicians working at residency clinics adopted a plan in which 80% of their compensation was panel based and 20% was RVU based. The community and regional clinic faculty opted to allocate 50% to each of the two components. With the adoption of this new compensation structure, all but 2 physicians saw an increase in their salary, with an average increase of 23%.
Data and Variables
Data were extracted from the electronic health record (EHR) from 2012 to 2016 (Epic Systems Corporation, Verona, Wisconsin). We defined office visits as any face-to-face clinic encounter with a physician (including residents), physician assistant, or nurse practitioner. We defined telephone encounters as any telephone calls documented in the EHR, whether initiated by the patient or the clinic and whether handled by a physician, nurse practitioner, physician assistant, nurse, or medical assistant. In some cases, if there was more than one call regarding the same topic documented in the same encounter in the EHR, these encounters were counted as one encounter. During the study period our organization did not offer scheduled, billable telephone (Telehealth) encounters with patients in primary care, thus these visit types were not included in this study. At the start of our study less than 20% of family medicine patients had an active patient portal account, thus patient portal messages were excluded from our analysis based on the low volume of patient portal messages at that time. Clinic panel members were defined as patients who were assigned to a primary care physician at the clinic and had been seen anywhere within UW Health within the past three years.
Data Analysis
We performed a utilization analysis of office visits and telephone encounters trended over time for each of our family medicine clinics. DFMCH clinic visits and telephone encounters were stratified into two groups based on which compensation plan they adopted: residency clinics (80–20 panel-RVU) or community/regional clinics (50–50 panel-RVU). Utilization was recorded as office visits per panel member per month and telephone encounters per panel member per month. The study period began in January 2012 and ended in December 2016. We excluded a 6-month intervention phase-in after the roll out of physician compensation change. The physician compensation change occurred in January 2013 for residency and community clinics, and at later dates (between July 2013 and July 2014) for each of the regional clinics. We included data until the date of the next major system change (UW Health’s practice redesign) which occurred at a different time for each clinic but was at least one year after the physician compensation change at each site.
Statistical analysis was conducted in a two-stage process. In the first stage, the effects of the compensation plan deployment on each outcome were estimated for each clinic separately. For each clinic and each outcome, a time series linear model was used to predict the number of encounters per patient in that clinic’s patient panel per month. Seasonal and linear time trends were accounted for in the models. The effects of compensation plan deployment considered changes in level and/or in slope after deployment. After an initial model fit, observations with residuals greater than three standard deviations from the mean were assessed and found to represent error and thus were excluded and models were re-fit. Wald tests were used to assess significance of both change in level and in slope of compensation plan deployment. We note that both the overall level and the amplitude of month-to-month variability in response was quite heterogeneous across clinics. We did not feel that a single model comprising data from all clinics, even adjusting for clinic, would be adequate to capture this between-clinic heterogeneity. Therefore, we took the approach of fitting separate models to each clinic as if each clinic was its own individual intervention study. This represents the first stage.
The second stage utilized these individual clinic estimates in a pooled estimate across clinics. By analogy to meta-analysis, we combined the fitted model results across clinics to obtain overall effects on level and on slope, and jointly on the two parameters simultaneously. A visual representation of this statistical model is seen in Figure 1.
Figure 1.
Interrupted Time Series Study Design. Change in level = b2; change in slope (post minus pre) = b3.
RESULTS
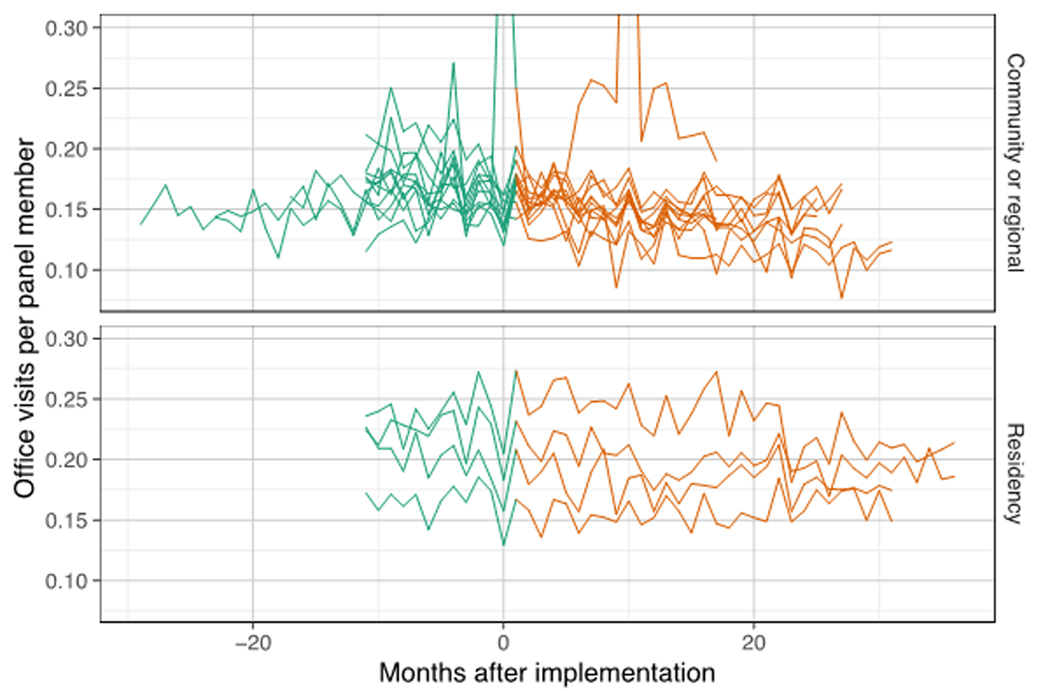
Office visits per panel member per month in the pooled data were not significantly impacted by the change in compensation for either the residency clinics or the community clinics/regional clinics (Figure 2). Neither the difference in the intercept (B2) nor the slopes (B3) were large or significant. Telephone calls per panel member per month were similarly unchanged in the pooled data with the implementation of the new compensation plan (Figure 3). There was no difference noted between residency clinics and community/regional clinics.
Figure 2.
Office Visits per Panel Member per Month
Figure 3.
Telephone Calls per Panel Member per Month
Some individual clinics had significant changes as can be seen in Figures 4 and 5. Out of sixteen total clinics, three had a significant increase in the number of office visits at six months after the change compared to baseline. Ten clinics had no change and no clinics had a significant decrease. Six clinics had a significant increase in office visits per member per month over time from six months after the compensation change to the end of data collection. Two clinics had a decrease and eight clinics had no change. With respect to telephone calls per panel member per month, four clinics had a significant drop in the level after the compensation change, two had a significant increase and ten were unchanged. Three clinics had an increase in the slope for telephone calls per panel member per month, two had a decrease and eleven had no significant difference.
Figure 4.
b2 and b3 Results for Office Visits per Panel Member per Month
Figure 5.
b2 and b3 Results for Telephone Calls per Panel Member per Month
DISCUSSION
A change from a physician compensation plan based on RVUs to one based primarily on panel size at UW DFMCH clinics was not found to impact care delivery as assessed by changes in pooled office visits and telephone calls per panel member per month. We had hypothesized that physicians may either consciously or subconsciously choose to provide more care via telephone and less via office visits in response to a change in financial incentives de-emphasizing in-person care as compared to non-face-to-face care, but our results did not confirm this hypothesis. This was in some ways unsurprising given that our previous study showed variable effects of a change in compensation model on RVU productivity for this physician group.11 The literature overall has yielded conflicting results in this regard with some studies showing a significant change in care delivery and others showing no significant change.
There are several possible reasons for our findings. First, our study may have been underpowered to detect an effect. Second, practice patterns may be deeply ingrained in physicians and not easily changed within the first year of implementation of a new compensation plan. Follow up studies after more years of experience working within this system could yield a different result though longer studies also are more susceptible to confounding from other changes that may occur in the healthcare system. In our case we ended data collection before the next major rollout of practice redesign at our organization. Another consideration is that if a physician wanted to make a change to their practice to emphasize non-face-to-face care, there may not be adequate clinic staff and protocols to support such a change. In addition, in the community and regional clinics there remains a significant portion of salary that is linked to RVU productivity such that the amount of productivity-based compensation was attenuated but not eliminated. Our results may also have been influenced by the significant heterogeneity of clinic types in our study, ranging from a small community clinic with two physicians to a large Federally Qualified Health Center with seven faculty physicians, 3 physician assistants and 12 residents.
There are several limitations to our study. Many patient, clinic and system factors may have influenced ways of seeking and receiving care from our system during our study period. There were several ongoing practice changes that occurred during the transition in our compensation model. For example, we have been implementing telephone triage protocols and medication refill protocols that likely influence how our patients seek advice from our practice whether it be in person or in non-face-to-face circumstances. Additionally, there were substantial changes in insurance starting in 2010 with the Affordable Care Act legislation.13 Preventive services were covered that hadn’t been covered previously, medication prescription costs changed, and accountable care organizations came into existence. The Health Insurance Marketplace began in October 2013, and by 2014, and many patients who were previously uninsured acquired some form of insurance. These insurance changes likely influenced how many of our patients were in capitated and fee-for-service insurance agreements and, as a result, how our primary care panel members accessed us for their primary care needs. While these complexities may limit the ability to separate out the impact of our compensation change from other aspects of our care delivery system we would also argue that primary care delivery is inherently complex and ever-changing. This study is a pragmatic real-world analysis and may be of assistance to those who seek to make similar changes in their own organizations. In particular this study of care delivery pre-pandemic was not impacted by the dramatic changes to healthcare delivery that have occurred as a result of the pandemic. It may offer some insights to health systems currently contemplating compensation plan changes and in some ways provide reassurance that major shifts were not seen in the first year after change.
In summary, physician compensation was not found to be a key driver of in-clinic versus non-face-to-face care delivery in our family medicine clinics. As compensation plans evolve to align with how practices are paid, it is important to understand what impact, if any, these changes have on care delivery.
Acknowledgements:
The authors wish to thank Peter Nordby and Mindy Smith for editorial support and comments on earlier drafts.
Financial Support:
This project was supported by the Health Innovation Program, the UW School of Medicine and Public Health from The Wisconsin Partnership Program, and the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research (UW ICTR) through the National Center for Advancing Translational Sciences (NCATS), grant 9 U54 TR000021 (previously grant 1 UL1 RR025011 from the National Center for Research Resources).
Footnotes
Conflict of Interest Disclosure: The authors have no conflicts of interest to disclose.
References
- 1.Brekke KR, Holmås TH, Monstad K, Straume OR. Do treatment decisions depend on physicians’ financial incentives? Journal of Public Economics. 2017;155:74–92. doi: 10.1016/j.jpubeco.2017.09.012 [DOI] [Google Scholar]
- 2.Gosden T, Forland F, Kristiansen IS, et al. Capitation, salary, fee-for-service and mixed systems of payment: effects on the behaviour of primary care physicians. Cochrane Database Syst Rev. 2000(3):CD002215. [DOI] [PMC free article] [PubMed]
- 3.Lyu H, Xu T, Brotman D, et al. Overtreatment in the United States. PLoS One. 2017;12(9):e0181970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell JM. Urologists’ use of intensity-modulated radiation therapy for prostate cancer. N Engl J Med. 2013;369(17):1629–1637. [DOI] [PubMed] [Google Scholar]
- 5.Reid RO, Tom AK, Ross RM, Duffy EL, Damberg CL. Physician Compensation Arrangements and Financial Performance Incentives in US Health Systems. JAMA Health Forum. 2022;3(1):e214634-e214634. doi: 10.1001/jamahealthforum.2021.4634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coleman DL, Joiner KA. Physician Incentive Compensation Plans in Academic Medical Centers: The Imperative to Prioritize Value. The American Journal of Medicine. 2021;134(11):1344–1349. doi: 10.1016/j.amjmed.2021.06.040 [DOI] [PubMed] [Google Scholar]
- 7.Epstein J. Transitioning to value-based physician compensation. Healthcare Financial Management. Vol 68; 2014:30–34. [PubMed] [Google Scholar]
- 8.Krasnik A, Groenewegen PP, Pedersen PA, et al. Changing remuneration systems: effects on activity in general practice. BMJ. 1990;300(6741):1698–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarma S, Devlin RA, Belhadji B, Thind A. Does the way physicians are paid influence the way they practice? The case of Canadian family physicians’ work activity. Health Policy. 2010;98(2–3):203–217. [DOI] [PubMed] [Google Scholar]
- 10.Ozkardes C, Harman JS. Physician Compensation Method Effects on Preventive Service Delivery. Journal of General Internal Medicine. 2022;37(2):480–481. doi: 10.1007/s11606-020-06580-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lochner J, Trowbridge E, Kamnetz S, Pandhi N. Family physician clinical compensation in an academic environment: moving away from the relative value unit. Fam Med. 2016;48(6):459–466. [PMC free article] [PubMed] [Google Scholar]
- 12.Trowbridge E, Bartels CM, Koslov S, Kamnetz S, Pandhi N. Development and Impact of a Novel Academic Primary Care Compensation Model. Journal of General Internal Medicine. 2015;30(12):1865–1870. doi: 10.1007/s11606-015-3410-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Health and Human Services. About the Affordable Care Act. https://www.hhs.gov/healthcare/about-the-aca/index.html. Accessed August 6, 2019.