Abstract
Purpose
Urologic chronic pelvic pain syndrome has attracted a lot of attention in the new century, and an increasing number of relevant studies have been published. Therefore, we performed a bibliometric analysis of these publications, hoping to show the current research hotspots and future research trends.
Methods
The articles on were selected from the Web of Science Core Collection. Countries, authors, references and keywords in the field were visualized and analyzed using CiteSpace and VOSViewer software.
Results
A total of 1014 articles on urologic chronic pelvic pain syndrome were identified, with “chronic pelvic pain syndrome” being the most common keyword, with a strong association with “interstitial cystitis” and “chronic prostatitis”. The hotspot of urologic chronic pelvic pain syndrome research has gradually shifted from chronic prostatitis / urologic chronic pelvic pain syndrome to cystitis/bladder pain syndrome over the past few years. Future research tends to focus on urologic chronic pelvic pain syndrome etiology, including oxidative stress and inflammation.
Conclusion
Research on urologic chronic pelvic pain syndrome is steadily growing. The United States has made the most prominent contribution in this area, and the share of China’s contribution is expected to grow further. The etiology of urologic chronic pelvic pain syndrome, including inflammation and oxidative stress, have been the focus of current research and developmental trends in the future research.
Keywords: bibliometric analysis, chronic pelvic pain syndrome, interstitial cystitis, chronic prostatitis, mechanisms, treatments
Introduction
Pain is a suffering experience of sensory, emotional, cognitive and social components related to tissue damage or potential tissue damage. To encourage doctors to listen to their patients and assess their suffering, pain has been called the fifth vital sign since 1996.1 Accordingly, in the past 20 years, people have paid more and more attention to urologic chronic pelvic pain syndrome (UCPPS), which encompasses two highly prevalent urologic chronic disorders—interstitial cystitis/bladder pain syndrome (IC/BPS) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).2 Because UCPPS is a heterogeneous disease both in presentation and pathophysiology, making characterization and reliable biomarker identification challenging,3 the diagnosis of UCPPS mainly depends on the symptoms dictated by patients currently, which mainly including chronic pain of pelvis, urogenital tract floor or external genitalia, generally accompanied by lower urinary tract symptoms.4 Studies have shown that UCPPS has a serious negative impact on patient quality of life, and patients with UCPPS may have a worse quality of life than those with end-stage renal disease.5 The prevalence of UCPPS has shown an increasing trend over the years, with community-based surveys reporting a prevalence of 8% in men, but estimates are that it can be as high as 11.5% in men under 50 years of age,5 and up to 7% of women were affected by IC/BPS.6,7 Although researchers have done a lot of basic and clinical exploration, the cause and effective treatment of UCPPS are still inconclusive.
Bibliometrics is a discipline that describes and analyzes the research trends and progress in a certain field, which began in 1969. It takes scientific literature as the research object, and quantitatively studies the characteristics and relationship between scientists and scientific literature by using statistical analysis, social network analysis and mathematical modeling.8 At the same time, visual co-citation analysis can explain the data more conveniently, show the data more comprehensively, and help to mine the internal relations among the data.9 Software is critical to scientific research: it helps scientists identify research questions, analyze data, visualize results, and disseminate knowledge. We have chosen Citespace and VOSviewer as our analysis tools in this research. Citespace pays attention to the strength of the relationship in terms of graphics and connections, while VOSviewer mainly constructs the relationship by distance.10 The two software have their own advantages and can play a complementary role.
This study aims to show the development status and structure, development frontier and evolution path of UCPPS in the form of knowledge mapping, and on this basis, selects the core literature in the field for reading, analysis and review, so as to provide new ideas for UCPPS study.
Materials and Methods
Data Collection
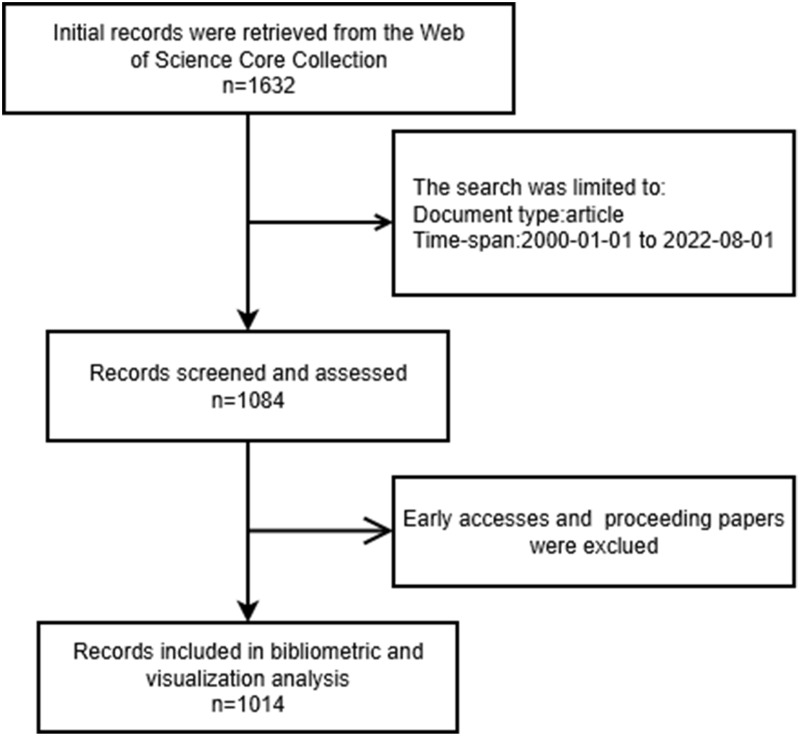
In order to collect comprehensive and authoritative articles, we chose Web of Science Core Collection as the data source. The search formula was set to TS = (“Urologic chronic pelvic pain syndrome” OR (“chronic pelvic pain” AND (“prostatitis” OR “Cystitis”))), and the timespan of the search were from January 1, 2000, to August 1, 2022. With limiting the type of literatures to be ‘Articles’, we retrieved 1084 articles. Then we excluded proceeding papers and early accesses, and finally got 1014 papers. ALL of these papers are exported as TXT files in the form of all records and references. The complete data acquisition process is illustrated in Figure 1.
Figure 1.
Flow chart for publications selection.
Data Analysis
All the data we collected in Web of Science Core Collection were imported into the Microsoft Excel 2019, Citespace and VOSviewer for visual analysis.
With the technical progress in the field of knowledge mapping, the existing information visualization techniques make knowledge mapping have the function of supporting multivariable, time-sharing and dynamic complex network analysis. Citespace and VOSviewer, as representative tools, are widely used to study the trends and evolvements of different disciplines.9,11 CiteSpace is based on the data normalization method of set theory for similarity measurement of knowledge units, and the similarity algorithm is used to obtain timezone and timeline within time slices, so that the process of knowledge evolution and the historical span of literature in a certain cluster can be clearly outlined in the time dimension to understand the development process and trend of the field.9,12 Vosviewer uses a probabilistic data normalization approach, providing various visualization views in the fields of keywords, co-authorship, co-organization, and co-authorship, including Network Visualization, Overlay, Visualization, and Density Visualization.11 In the form of display, We use Microsoft Excel 2019 to analyze annual publication trends, and CiteSpace and VosViewer software to analyze country and institutional distribution, author contributions, core journals, keyword and timezone viewer. These bibliometric studies based on scientific papers and citation data explore and predict the development characteristics and evolution law of UCPPS researches from different dimensions and perspectives.
Results
The Trend of Publication Outputs
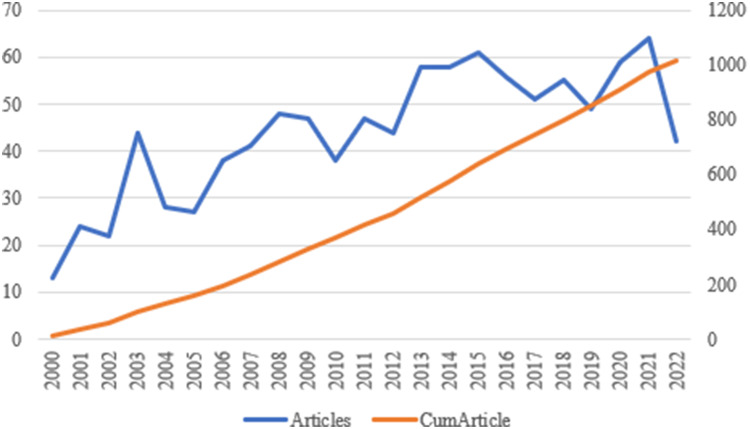
The number of publication outputs show the development trend in the research field. From January 2000 to August 2022, we searched 1014 valid literatures from Web of Science Core Collection. The 1014 papers used in this study were from 3086 authors at 1139 organizations in 52 countries and regions, published in 244 journals, and cited 11,793 citations from 3904 journals. We import the data collected from Web of Science Core Collection into Excel to get Figure 2, from which we can see that UCPPS has maintained a certain popularity in the past 20 years, especially after 2013, the number of articles has been kept at 50 per year, which indicates that UCPPS field has recently received more attention from researchers and become a new hot spot in the intersection of urology and pain disciplines.
Figure 2.
Trends of UCPPS publications over the past 22 years.
The Analysis of Distribution and Collaboration Relationship of Countries/Regions
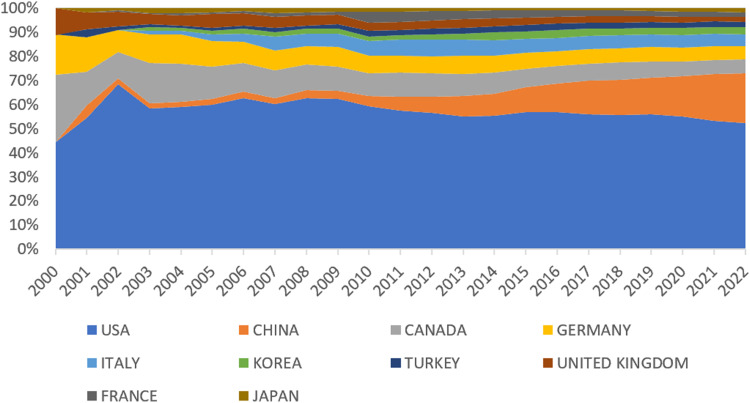
The address information of the authors of the article contains the institution where each author is located and its corresponding country, which can be used to analyze the geographical distribution of the authors of the paper. It can be seen from Figure 3 that developed countries such as Europe and the United States occupy a dominant position in the production of UCPPS research papers. Among them, the United States, as the first country that began to pay attention to this field, has the largest number of related papers, accounting for nearly 50% of the total, that is, about one-second of UCPPS papers contain at least one American author, indicating that the United States produces knowledge on this topic. Contribute the most. China followed closely, ranking second, with a cumulative output of more than 147 papers, accounting for 14.5% of the world’s total. The third place for the number of papers is Canada, with a total of about 93 papers (7.8%). Followed by developed countries in Europe and East Asia such as Italy, Germany, the United Kingdom, South Korea and Japan. It is worth noting that Turkey, a Middle East country, also has a relatively bright performance in UCPPS research, with more than 30 papers, accounting for about 3.1%.
Figure 3.
The top 10 most active countries/regions.
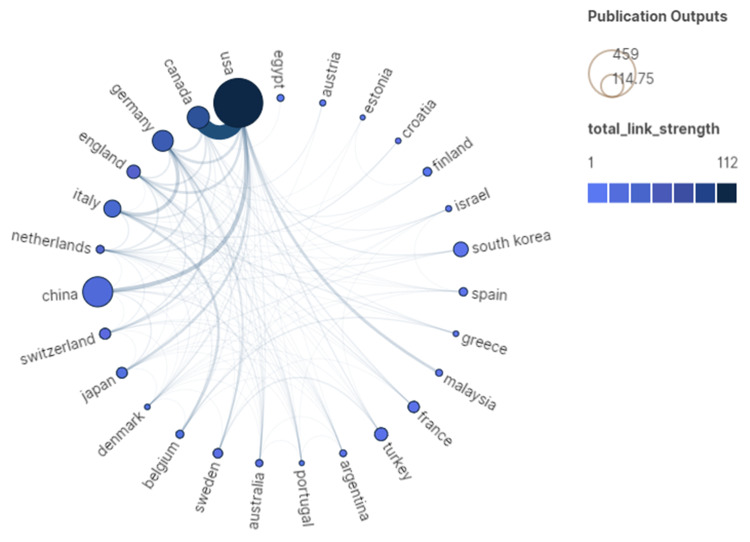
The development of communication technology and the process of economic globalization have promoted the increasing internationalization of scientific research. In the global UCPPS research, the cooperation between countries is becoming more and more frequent, and the proportion of international cooperative papers is increasing year by year. Figure 4 shows the partnership and the intensity of cooperation between the individual countries, “total link strength” represents the number of papers produced by inter-country collaboration. From the perspective of “total link strength”, the United States is the core force in the current international cooperation network of UCPPS, which had the strongest collaboration with Canada. But in terms of centrality (Table 1), Germany tops the list. Although its publication outputs are not so much, it occupies an important position in the cooperation network and has a high degree of cooperation. In addition, Canada, England, Australia, Egypt, Argentina, China, and Italy also have many cooperative relationships. Among them, although China has the second most outputs and a large number of international cooperation papers, it ranks lower in the closeness centrality indicators, indicating that China’s cooperation objects are relatively fixed and the scope of cooperation is limited.
Figure 4.
The co-authorship map of countries. The thickness of the connecting lines shows the frequency of cooperation, “total link strength” represents the number of papers produced by inter-country collaboration.
Table 1.
Centrality of Inter-Country Cooperation
| Country | NP | Centrality | Total-Link-Strength |
|---|---|---|---|
| Germany | 83 | 0.34 | 59 |
| USA | 459 | 0.24 | 112 |
| Canada | 93 | 0.18 | 76 |
| England | 32 | 0.12 | 39 |
| Netherlands | 12 | 0.09 | 34 |
| Australia | 10 | 0.07 | 16 |
| Egypt | 9 | 0.06 | 1 |
| Argentina | 9 | 0.06 | 11 |
| China | 145 | 0.06 | 27 |
| Italy | 55 | 0.05 | 37 |
The Analysis of Authors and Co-Authorship
The core author is not only the backbone of academic innovation and discipline development, but also one of the important factors to enhance the academic influence and competitiveness of journals. Price studied the relationship between the number of scientists and the number of scientific literatures, and noticed the great role of elites in the development of science, as well as the quantitative relationship between scientists at different levels of ability, and put forward “Price’s Law” in 1963, that is, half of the papers on the same topic were written by a group of high-productivity authors, and this set of authors was equal to about the square root of the total number of authors. According to Price’s Law, the minimum number of papers published by core authors in a certain field is m = 0.749 × nmax1/2, where nmax represents the number of papers published by the most prolific authors in the field. In this study, the author with the highest number of publications was NICKEL JC, with a total of 76 publications. After calculations, we get m≈6.5, so we conclude that authors with more than 7 papers published are defined as the core authors in the UCPPS field.
What Price’s law reveals is that the so-called “core” authors are found from the perspective of the volume of publications. However, the importance and influence of an author can be measured only by the volume of his or her output, which is somewhat one-sided. In 2005, Jorge Hirsch proposed h-index to measure core scientists, which point out that the h-index of a scholar is the number of papers that have been cited at least h times.13 It can reflect the influence of a scientist’s academic papers and also the number of important papers he or she has produced. But h-index is insensitive to highly cited articles. Subsequently, the g-index is proposed as an improvement of the h-index, shows that when a set of articles ranked in descending order of their citations, the g-index is the order of the largest paper with at least g² cumulative citations g.14 We use h-index, g-index, total number of citations (TC), number of publications (NP), to evaluate the influence of relevant authors (Table 2).
Table 2.
Top 10 Authors Related to UCPPS
| Name | h-Index | g-Index | TC | NP |
|---|---|---|---|---|
| Nickel JC | 41 | 64 | 4191 | 76 |
| Landis JR | 30 | 44 | 2275 | 44 |
| Shoskes DA | 28 | 42 | 2097 | 42 |
| Schaeffer AJ | 27 | 44 | 2306 | 44 |
| Kusek JW | 21 | 25 | 1717 | 25 |
| Krieger JN | 20 | 36 | 1403 | 36 |
| Clemens JQ | 18 | 32 | 1226 | 32 |
| Mullins C | 18 | 21 | 832 | 21 |
| Pontari MA | 18 | 23 | 1339 | 23 |
| Clauw DJ | 17 | 22 | 927 | 22 |
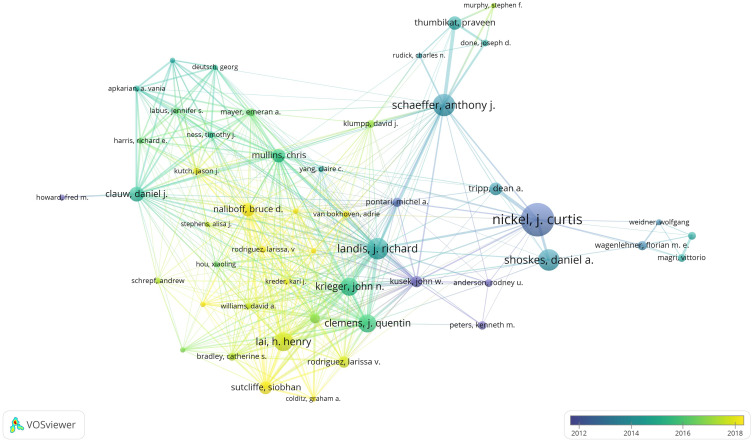
Co-authorship map reflects the collaborative relationships of research teams in the field, we visualize the cooperation network for core authors by VOSviewer. At the same time, we added a time dimension to show the passage of time through the gradual change of color. The analysis results are shown in Figure 5. In Figure 5, the node size represents the number of papers published, the node color represents the time distribution, and the line represents the partnership. As can be seen from the picture, the co-occurrence network of high-productivity authors in UCPPS is an overall network graph with high connectivity, which means that there is a wide range of cooperation among these authors, a high degree of cooperation between different teams.
Figure 5.
The co-authorship map of authors related to UCPPS. The size of the nodes indicates the number of documents published by the author in collaboration, and the thickness of the edges indicates the frequency of collaboration; the gradual change of color shows the passage of time.
The Analysis of Relevant Journals
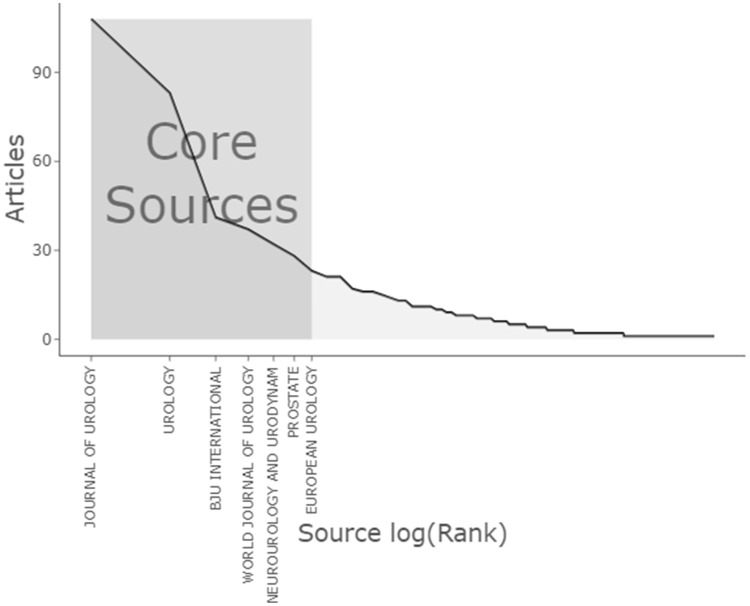
The development of science always follows certain laws. On the one hand, modern science and technology intersect and interpenetrate each other. On the other hand, there is a tendency for small subjects to be integrated into large subjects. Bradford summed up the law of dispersion of literature starting from the law of scientific unity. Bradford pointed out that if scientific journals are arranged in decreasing order according to the number of papers published in a certain discipline, then the journals can be divided into a core area dedicated to this discipline and several areas containing the same number of papers as the core area.15 In Figure 6, according to Bradford’s Law, the 244 document sources were divided in to three zones, zone 1 had 7 journals, zone 2 had 32, and zone 3 had 205.The journals in the zone 1 (core area) include Journal of Urology, Urology, BJU International, World Journal of Urology, Neurourology and Urodynamics, Prostate and European Urology. Journal of Urology ranked first with 108 publications, accounting for 10.6% of the total, and “Urology” ranked second with 83 publications.
Figure 6.
Journals clustering through Bradford’s law. According to Bradford’s Law, the logarithm of the number of ranked journals (Source log(rank)) is the horizontal coordinate, and the corresponding number of papers (Articles) is the vertical coordinate.
Subsequently, we applied h-index, g-index, total number of citations, number of publications to evaluate the impact of relevant journals. As we can see from Table 3, Journal of Urology has the highest h-index, g-index, total number of articles published and total number of citations, and is deservedly the most influential journal in UCPPS. International Urogynecology Journal, Journal of Sexual Medicine, Pain appeared in the table, although they were not rated as core journals according to Bradford’s Law. It is worth mentioning that Pain has an average number of citations per article of 23.6, which is even higher than Prostate.
Table 3.
Top 10 Journals Related to UCPPS
| Element | h-Index | g-Index | TC | NP |
|---|---|---|---|---|
| Journal of Urology | 45 | 64 | 4780 | 108 |
| Urology | 31 | 49 | 2699 | 83 |
| Bju International | 26 | 41 | 1756 | 41 |
| World Journal of Urology | 21 | 32 | 1074 | 37 |
| European Urology | 20 | 23 | 1485 | 23 |
| Journal of Sexual Medicine | 14 | 17 | 526 | 17 |
| Prostate | 13 | 21 | 462 | 28 |
| International Urogynecology Journal | 11 | 14 | 362 | 14 |
| Neurourology and Urodynamics | 11 | 17 | 332 | 32 |
| Pain | 11 | 15 | 354 | 15 |
The Analysis of Co-Cited References
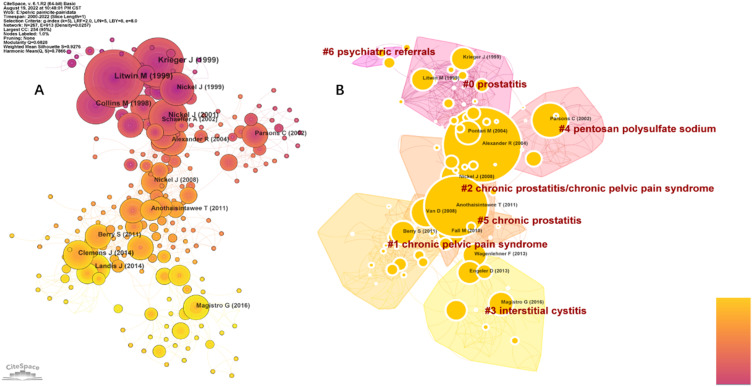
Co-citation network based on CiteSpace generated references of UCCPS papers. Each node in the graph represents a document, and the line between each node indicates the citation relationship between the documents; the automatic clustering labels use LLR algorithm. Cluster size in graph A indicates the number of citations, reflecting the degree of attention the clusters have received. The size of the nodes in the graph B reflects the centrality of the article, centrality depicts the node establishing a bridge between 2 unrelated nodes, with a high mediated centrality highlighting the importance of the node in the knowledge structure.
Figure 7A and Table 4 show the high co-cited articles, Litwin M developed of a psychometric index of symptom and quality of life impact in men with chronic prostatitis,16 The article by Krieger J refined the definition and classification of prostatitis,16 Collins M explored the epidemiology of physician visits for genitourinary symptoms or a diagnosis of prostatitis.17 The “Multidisciplinary Approach to Chronic Pelvic Pain Research” (MAPP) research network was established to better understand and treat UCPPS,18 Magistro G evaluated the best available practical evidence recommendations and randomized controlled trials of CP/CPPS treatments and management.19 These high co-citation articles build the knowledge base of UCPPS. Figure 7B shows the largest 7 clusters of co-cited references. From the point of time distribution, the research direction and contents of UCPPS has obvious stage characteristics: while the early researchers focused on chronic prostatitis, in recent years more attention has been paid to interstitial cystitis.
Figure 7.
(A) The network of co-cited references. (B) The network of co-cited references clusters. Cluster size in graph (A) indicates the number of citations, reflecting the degree of attention the clusters have received. The size of the nodes in the graph (B) reflects the centrality of the article, centrality depicts the node establishing a bridge between 2 unrelated nodes, with a high mediated centrality highlighting the importance of the node in the knowledge structure.
Table 4.
Top 10 Co-Cited References Related to UCPPS
| Citation Counts | Author | DOI | Year |
|---|---|---|---|
| 88 | Litwin M | 10.1016/S0022-5347(05)68562-X | 1999 |
| 68 | Krieger J | 10.1001/jama.282.3.236 | 1999 |
| 52 | Collins M | 10.1016/S0022-5347(01)63564-X | 1998 |
| 50 | Nickel J | 10.1016/S0022-5347(05)66541-X | 2001 |
| 36 | Landis J | 10.1186/1471-2490-14-58 | 2014 |
| 36 | Magistro G | 10.1016/j.eururo.2015.08.061 | 2016 |
| 36 | Nickel J | 10.1016/S0090-4295(99)00205–8 | 1999 |
| 33 | Alexander R | 10.7326/0003-4819-141-8-200410190-00005 | 2004 |
| 30 | Schaeffer A | 10.1016/S0022-5347(05)64686–1 | 2002 |
| 29 | Pontari M | 10.1097/01.ju.0000136002.76898.04 | 2004 |
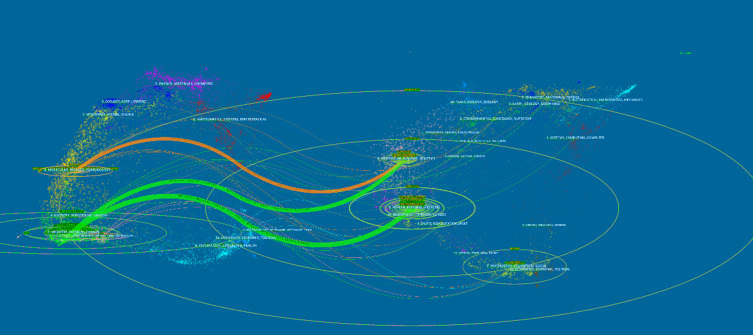
The dual-map overlay of journals demonstrated relationship distribution among journals, with citing journals on the left and cited journals on the right, and the colored paths between them suggesting the cited relationships.20 The orange path in Figure 8 indicates that the documents published in Molecular/Biology/ Genetics journals are often cited by Molecular/Biology/ Immunology journals. Relevant citations reached 2460 times.
Figure 8.
The dual-map overlay of journals on UCPPS. The dual-map overlay of journals demonstrated relationship distribution among journals, with citing journals on the left and cited journals on the right, and the colored paths between them suggesting the cited relationships.
At the same time, the two green paths show that articles in Medicine/Medical/Clinical journals often cite articles in Molecular/Biology/Genetics and Health/Nursing/Medicine journals, with a frequency of 3406 and 5656 citations, respectively.
The Analysis of Hotspots and Frontiers
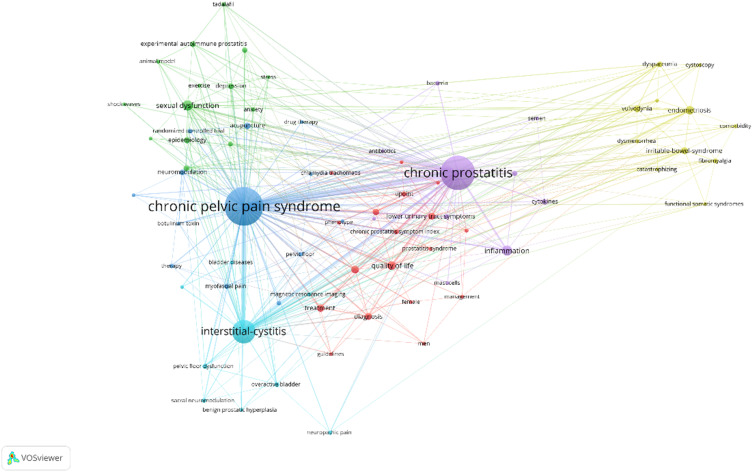
The keywords condense the core and essence of a paper, and the keyword co-occurrence analysis can reveal the research hotspots in a scientific field. The keyword co-occurrence network view of 1014 literatures were drawn by VOSviewer, and 82 key keywords with frequency greater than or equal to 5 were selected for visualization (Figure 9). In Figure 9, the circle nodes represent keywords and the connecting lines represent co-occurrence relationship, the larger the circle node, the more frequent the keyword appears and the more representative of the domain hotspot. The thickness of the line represents the strength of the association, the thicker the line, the more often they appear together in the same paper; Node colors represent different clusters, for example, study topics. “Chronic pelvic pain syndrome” is the most common keyword, with a strong association with “interstitial cystitis” and “chronic prostatitis”. Excluding search terms, we can find that inflammation, sexual dysfunction, quality of life, endometriosis, questionnaires, treatment, diagnosis, irritable-bowel-syndrome, lower urinary tract symptoms, acupuncture, NIH-CPSI, vulvodynia are mentioned many times, which means that UCPPS is primarily concerned with its diagnosis, treatment, comorbidities, and impact on patients’ lives.
Figure 9.
Map of keywords clustering analysis related to UCPPS. The circle nodes represent keywords and the connecting lines represent co-occurrence relationship, the larger the circle node, the more frequent the keyword appears and the more representative of the domain hotspot.
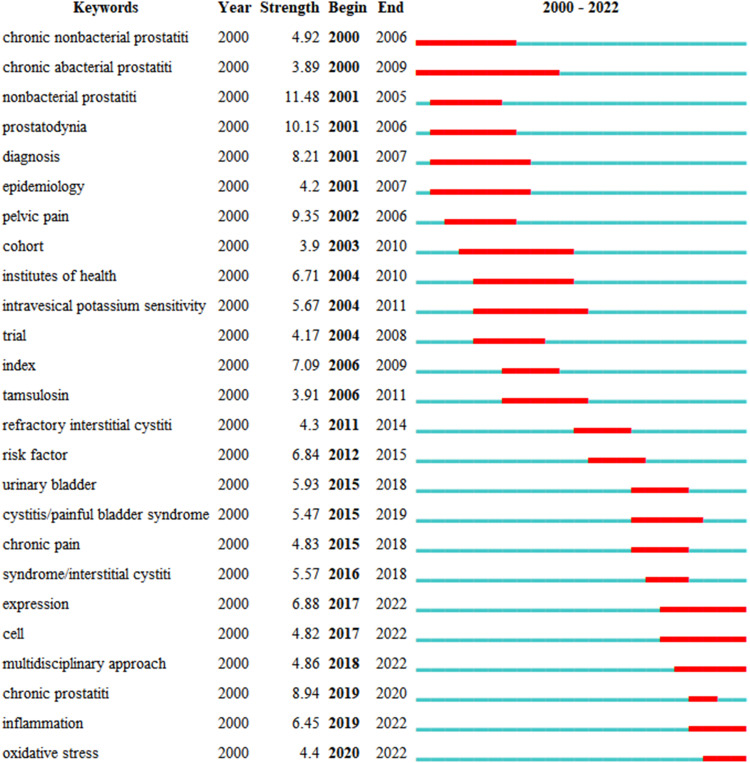
Burst keywords refer to the frequent occurrence of a certain keyword within a specific period of time, which can not only reflect the evolution of research hotspots over time, but also reflect the research trends in recent years and shed some light on future research trends. Figure 10 presents the top 25 keywords with citation bursts. The blue line indicates the time interval, while the red line indicates the time period when a keyword had a burst21 indicating a sudden increase in the frequency of use of a keyword in a certain period of time, which means the keyword is highly valued by researchers in that time period. In addition, “Strength” denotes the burst intensity, “Begin” denotes the burst start year, and “End” denotes the burst end year. As can be seen, Research in the first decade of this century focused on diagnostic criteria for UCPPS and related symptom evaluation indices, in the last decade researchers have focused on the treatment and etiology of UCPPS, particularly in the areas of inflammation and oxidative stress.
Figure 10.
Top 25 Keywords with the Strongest Citation Bursts. The blue line indicates the time interval, while the red line indicates the time period when a keyword had a burst.
Discussion
With further research on UCPPS, more and more academic papers are being published. It is especially important to evaluate the quality of such a large number of research papers to obtain valuable information. Multidisciplinary research plays a crucial role in understanding the etiology and treatment of UCPPS as well as improving the quality of life of patients. Visual analysis using Citespace and Vosviewer has shown an overall year-on-year increase in research on UCPPS. NICKEL JC is an outstanding contributor to the field of UCPPS. Studies on UCPPS have been cited in many influential international journals, indicating that UCPPS has received widespread attention. The Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network was formed to inform the treatment and management of UCCPS symptoms, and prepare the ground for subsequent investigators, which is also the hot issue of the moment.
Both IC/BPS and CP/CPPS are clinical syndromes characterized by pelvic pain with or without voiding symptoms such as urinary frequency and urgency. They share many similarities in terms of epidemiology, symptoms, pathogenesis and treatment. IC/BPS is two to five times more common in women than in men,22 whereas CP/CPPS is a male disease.
IC/BPS
Possible Mechanisms of IC/BPS
IC/BPS is defined as chronic bladder-related pelvic pain, pressure or discomfort with other urinary symptoms, such as persistent urge to urinate or urinary frequency, that are not confused with the disease. The cause of IC/BPS is not yet clear and the following possible mechanisms have been proposed.
Autoimmunity/Inflammation
Histological analysis of bladder specimens from patients with IC often shows mast cell infiltration, high levels of pro-inflammatory cytokines and chemokines detectable in the serum, bulbous cystoscopic haemorrhages following hydrodilation, and erosion and thinning of the bladder wall, all suggesting a role for inflammation in the pathogenesis of IC.
Infections
The high positive rate of urine cultures, alterations in urine bacterial flora or whole transcriptome analysis suggest that urinary tract infections are associated with IC/BPS. Recurrent female urinary tract infections can cause hypersensitivity symptoms in the female bladder through a variety of factors, such as induction of apoptosis in the urinary tract epithelium, increase in the number of mast cells, and decrease in epithelial calmodulin.23
Neurological Factors
Histopathology shows characteristic nerve endings proliferation and chronic peripheral neuritis in the bladder wall.24 The main neurological factors in patients with IC are: 1. increased sympathetic activity;25 2. upregulation of peripheral and central sensory innervation;26,27 3. increased nerve fibre density;28 4. neuroinflammation.29,30
Muscle Dysfunction
Permeability damage or alterations to the GAG layer or uroepithelium, increased numbers of mast cells in the pushing muscle or altered NO levels and ATP/NO ratios in patients with IC can lead to pushing muscle dysfunction and cause IC-like symptoms.31 The higher incidence of IC with a history of pelvic surgery and anal raphe pain suggests that pelvic floor muscle dysfunction may also contribute to the development of disease symptoms.32
Psychological Factors
Patients with IC often present with psychiatric abnormalities that have a significant impact on psychosocial functioning and quality of life. Pain, sleep disturbances, depression, anxiety, stress, social dysfunction and sexual dysfunction are significantly more common in patients with IC/BPS than in non-IC patients,33 and it has been suggested that IC/BPS may be part of a family of hypersensitivity disorders affecting the bladder and other somatic/invasive organs as part of a systemic disorder.34
Other Factors
IC is often combined with fibromyalgia, irritable bowel syndrome, chronic fatigue syndrome, dry syndrome and chronic headache. The mechanisms are unclear and may be part of a systemic disease.35 Components of the urine such as potassium ions may disrupt the uroepithelial function of the bladder causing symptoms, eg long-term abuse of ketamine producing IC-like symptoms may be related to the metabolites of the ketamine machine.36 Patients with IC find a reduction in subannual microvascular density and cut hyperbaric oxygen therapy relieves the symptoms of IC, suggesting that tissue hypoxia may be an etiology of IC.37 Consumption of specific foods or beverages is often a cause of exacerbation of IC symptoms, seen in 52.7–95.8% of patients, suggesting that there may be a broader range of factors in the etiology of IC that still need to be explored in further research.
Current and Potentially Viable Treatments of IC/BPS
The main aim of treatments is to improve the patient’s quality of life through controlling pain and reducing symptoms.
Conservative Treatments
Behavioral therapy and Psychotherapy are important in relieving patients’ discomfort.
Medication
Several drugs such as dulcolytin, gabapentin, montelukast, NSAIDs, sildenafil, adalimumab, certolizumab and tacrolimus are described recently to alleviate the symptoms.
Surgical Treatments
Hydrodilatation and Transurethral ablation/electrocautery have often been reported of better results. However, the reduction in bladder volume is a concern and controversial.
Cystectomy and urinary diversion will be the last option. Long-term postoperative observation is required to monitor for symptom recurrence and complications such as hydronephrosis and adenocarcinoma of the bowel segment.
Physiotherapy
Biofeedback: reduces the resting tone of the pelvic floor muscles and works well in synergy with medication. Patients learn how to relax the pelvic floor muscles during pelvic pain, eliminating the “pain-muscle spasm-pain” cycle and improving symptoms.38
Acupuncture: Recent reports have shown that IC patients who have failed to pharmacological treatments, acupuncture may be an optional choice.39
Neuromodulation
Neuromodulation is the fourth line of treatment for patients with bladder pain syndrome/interstitial cystitis (BPS/IC) after failure of behavioral and pharmacological treatments. Sacral neuromodulation may be effective in patients with BPS without Hunner’s lesion and the effects appear to be maintained in the mid- and long-term. Selective pudendal nerve stimulation has a high response rate when pudendal neuralgia is suspected.40
Self-Management
Patients can self-manage a certain amount of their symptoms by changing behaviors, which includes their diet, fluid management and stress management.41 Corresponding timely and supportive information can effectively improve the effectiveness of patient self-management,42 suggesting that clinical workers need to pay more attention to patient feedback.
CP/CPPS
Possible Mechanisms of CP/CPPS
Chronic prostatitis is one of the most common diseases among adult men. In 1995, the NIH defines Type III chronic prostatitis as CP/CPPS based on basic and clinical research on prostatitis, which accounting for approximately 90% of chronic prostatitis. The pathogenesis of CP/CPPS is not yet clear, it can be caused by the following factors.
Pathogenic Infection
It may be associated with certain specific pathogens, such as anaerobic bacteria, L-type Aspergillus, nanobacteria or Chlamydia trachomatis, mycoplasma and other infections, and studies have shown that the local prokaryotic DNA detection rate in patients with this type is as high as 77%.43
Urinary Dysfunction
Certain factors cause excessive contraction of the urethral sphincter, resulting in bladder outlet obstruction with residual urine formation, causing urine to flow back into the prostate, which can not only bring in pathogens but also directly irritate the prostate and induce sterile chemical prostatitis, leading to abnormal urination and pain in the pelvic region.
Psychosomatic Factors
Some studies have shown that many of the mechanisms of CPPS are based on central nervous system associations. Men with depression and anxiety in the general population have higher prostatitis scores.44 Psychopathological factors and personality -specific changes are evident in more than half of patients with persistent prostatitis.45 These changes in mental and psycho-logical factors can cause autonomic dysfunction, resulting in posterior urethral neuromuscular dysfunction.46
Neuroendocrine Factors
Patients with prostatitis may have alterations in the resting state neuro-muscular junction and these patients are often prone to fluctuations in heart rate and blood pressure, suggesting a possible association with autonomic responses.47 Local stimulation of the prostate and urethra, through nerve impulses, promotes the release of norepinephrine, prostaglandins, calcitonin gene-related peptides, and substance P from sympathetic nerve endings,48 causing vesicourethral dysfunction and leading to abnormal activity of the perineum and pelvic floor muscles, with persistent pain and involvement pain in the corresponding areas outside the prostate.49
Abnormal Immune Response
Recent studies have shown that immune factors play an important role in the development of type III prostatitis. Changes in the levels of certain cytokines, such as IL-2, IL-6, IL-8, IL-10, TNF-α and MCP-1, can occur in the prostatic fluid and seminal plasma and tissues and blood of patients.50–53
Oxidative Stress
Under normal circumstances, oxygen free radicals are in a state of dynamic balance. In prostatitis, the excess production of oxygen free radicals and the relatively reduced role of the free radical scavenging system result in nerve endings supersensitive, which may also be part of the pathogenesis.
Pelvic-Related Disease Factors
Patients with prostatitis often have dilated venous plexuses in the peripheral zone of the prostate, haemorrhoids and varicose veins of the spermatic cord, suggesting that some patients’ symptoms may be related to pelvic venous congestion and blood stasis.
Lower Urinary Tract Epithelial Dysfunction
Several studies have found many similarities between CPPS and IC, and it is hypothesized that the two share a similar pathogenesis. Lower urinary tract epithelial dysfunction is caused by a disruption in the balance between potentially protective and damaging factors in the lower urinary tract epithelium.
Current and Potentially Viable Treatments of CP/CPPS
Not all patients with chronic prostatitis need treatments, the main point is to relieve pain, alleviate urinary symptoms and improve the quality of life.
Healthy Lifestyle
Patients should maintain good lifestyle habits, including abstaining from alcohol, avoiding spicy and stimulating foods, avoiding holding urine, being sedentary, keeping warm, strengthening physical exercise, and having a regular sex life, which can help improve symptoms in patients with prostatitis.
Medication
(1) Oral antibiotics such as fluoroquinolones are recommended for 2–4 weeks, and then the decision to continue antibiotic therapy is all based on feedback on efficacy. It is only recommended to continue taking it for 4–6 weeks when the symptoms are reduced.
(2) α-blocker is a basic drug for the treatment of type III prostatitis and can be used in combination with antibiotics to improve lower urinary tract symptoms and pain by relaxing the smooth muscles of the prostate and bladder.
(3) Saw Palmetto and Cernilton have previously been used successfully to improve the symptoms of CP/CPPS patients.54 This may be due to the antioxidant properties of phytotherapy as both a free radical scavenger and a xanthine oxidase inhibitor.55,56
(4) M-blockers for patients with prostatitis with manifestations of overactive bladder disorder such as urinary frequency and urgency and nocturia but without obstruction.
(5) Antidepressants and anxiolytics for patients with chronic prostatitis who have a combination of depression, anxiety and other mood disorders, antidepressants and anxiolytics can be used as an alternative treatment along with prostatitis.
(6) Chinese herbal medicine A randomized double-blind placebo-controlled study has shown that herbal medicines such as Ning Mi Tai Capsules are safe and effective in the treatment of type III prostate.57
(7) Botulinum toxin A may represent a promising therapeutic strategy for these patients.58 Botulinum toxin can inhibit the release of acetylcholine from nerve fiber endings, which determines a transient skeletal muscle relaxation and produces an analgesic effect by reducing muscle hyperactivity.59
The etiology of both diseases is not fully understood, but infection, immunity, inflammation, and psychosomatic factors are common influences in both. Pathogenic infection is a common factor, but there are significant differences in the microbiota of them.60 Research studies have demonstrated that symptoms of both are significantly worse during times of high mental stress.49,61 When it comes to treatment, they share the same principles of symptom improvement, pain control and quality of life. Conservative treatment includes behavioral therapy as well as psychological guidance, pharmacological treatment is mainly antibiotics and allopathic medicines, and other treatments biofeedback, massage therapy and acupuncture also have commonalities. Both are clinical syndromes characterized by pelvic pain, and it is not meaningful to try to distinguish them completely based on current definitions. The questions that need to be addressed are how patients with only pelvic pain differ from those with co-existing urinary symptoms and, in addition, what are the differences in the nature of pelvic pain in men and women.62
Conclusion
This study used a bibliometric approach to conduct a comprehensive analysis of studies related to CPPS in terms of the number of published literatures, authors, countries, journals, references, and keywords. The results show that UCPPS has attracted the attention of international scholars and there is close collaboration among scholars from various countries. The role of inflammation and oxidative stress in the disease has been the focus of current study and developmental trends in the future research. There is not yet a perfect treatment, further differentiation is needed in clinical work according to the different symptoms, which requires physicians to be flexible enough in their treatment choices to turn to other options when a particular treatment does not work. Paying attention to patient feedback is helpful, and establishing a good feedback platform is part of the effort.
Funding Statement
This study is supported by grants from Key Medical Specialty in Jiading District, Shanghai (2020-jdyxzdzk-03) Scientific Research Project of Shanghai Jiading District Health Committee (2021-KY-09), National Natural Science Foundation of China (81470919) and Hainan Provincial Natural Science Foundation of China (820MS171).
Disclosure
Jie Wang and Bin Cao share first authorship. The authors declared that they have no conflict of interest.
References
- 1.Campbell J. The fifth vital sign revisited. Pain. 2016;157(1):3–4. doi: 10.1097/j.pain.0000000000000413 [DOI] [PubMed] [Google Scholar]
- 2.Clemens JQ, Mullins C, Kusek JW, et al. The MAPP research network: a novel study of urologic chronic pelvic pain syndromes. BMC Urol. 2014;14:14. doi: 10.1186/1471-2490-14-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dagher A, Curatolo A, Sachdev M, et al. Identification of novel non-invasive biomarkers of urinary chronic pelvic pain syndrome: findings from the multidisciplinary approach to the study of chronic pelvic pain (MAPP) research network. BJU Int. 2017;120(1):130–142. doi: 10.1111/bju.13832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suskind AM, Berry SH, Ewing BA, Elliott MN, Suttorp MJ, Clemens JQ. The prevalence and overlap of interstitial cystitis/bladder pain syndrome and chronic prostatitis/chronic pelvic pain syndrome in men: results of the RAND interstitial cystitis epidemiology male study. J Urol. 2013;189(1):141–145. doi: 10.1016/j.juro.2012.08.088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daniels NA, Link CL, Barry MJ, McKinlay JB. Association between past urinary tract infections and current symptoms suggestive of chronic prostatitis/chronic pelvic pain syndrome. J Natl Med Assoc. 2007;99(5):509–516. [PMC free article] [PubMed] [Google Scholar]
- 6.Berry SH, Elliott MN, Suttorp M, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011;186(2):540–544. doi: 10.1016/j.juro.2011.03.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Latthe P, Latthe M, Say L, Gulmezoglu M, Khan KS. WHO systematic review of prevalence of chronic pelvic pain: a neglected reproductive health morbidity. Bmc Public Health. 2006;6:6. doi: 10.1186/1471-2458-6-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith DR. Bibliometrics, dermatology and contact dermatitis. Contact Dermatitis. 2008;59(3):133–136. doi: 10.1111/j.1600-0536.2008.01405.x [DOI] [PubMed] [Google Scholar]
- 9.Chen CM, CiteSpace II. Detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Tec. 2006;57(3):359–377. doi: 10.1002/asi.20317 [DOI] [Google Scholar]
- 10.Pan XL, Yan EJ, Cui M, Hua WN. Examining the usage, citation, and diffusion patterns of bibliometric mapping software: a comparative study of three tools. J Informetr. 2018;12(2):481–493. doi: 10.1016/j.joi.2018.03.005 [DOI] [Google Scholar]
- 11.van Eck NJ, Waltman L. Software survey: vOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. doi: 10.1007/s11192-009-0146-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen C, Chen Y, Hou J, Liang Y. CiteSpace I: detecting and visualizing emerging trends and transient patterns in scientific literature. J China Soc Sci Tech Inf. 2009;28(3):401–421. [Google Scholar]
- 13.Hirsch J. An index to quantify an individual’s scientific research output. Proc Natl Acad Sci U S A. 2005;102(46):16569–16572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Egghe L. Theory and practise of the g-index. Scientometrics. 2006;69(1):131–152. doi: 10.1007/s11192-006-0144-7 [DOI] [Google Scholar]
- 15.Bradford SC. Sources of information on specific subjects 1934. J Inf Sci. 1985;10(4):176–180. doi: 10.1177/016555158501000407 [DOI] [Google Scholar]
- 16.Litwin MS, McNaughton-Collins M, Fowler FJ, et al. The national institutes of health chronic prostatitis symptom index: development and validation of a new outcome measure. J Urol. 1999;162(2):369–375. doi: 10.1016/S0022-5347(05)68562-X [DOI] [PubMed] [Google Scholar]
- 17.Collins MM, Stafford RS, O’Leary MP, Barry MJ. How common is prostatitis? A national survey of physician visits. J Urol. 1998;159(4):1224–1228. doi: 10.1016/S0022-5347(01)63564-X [DOI] [PubMed] [Google Scholar]
- 18.Landis JR, Williams DA, Lucia MS, et al. The MAPP research network: design, patient characterization and operations. BMC Urol. 2014;14. doi: 10.1186/1471-2490-14-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Magistro G, Wagenlehner FME, Grabe M, Weidner W, Stief CG, Nickel JC. Contemporary management of chronic prostatitis/chronic pelvic pain syndrome. Eur Urol. 2016;69(2):286–297. doi: 10.1016/j.eururo.2015.08.061 [DOI] [PubMed] [Google Scholar]
- 20.Chen CM, Leydesdorff L. Patterns of connections and movements in dual-map overlays: a new method of publication portfolio analysis. J Assoc Inf Sci Technol. 2014;65(2):334–351. doi: 10.1002/asi.22968 [DOI] [Google Scholar]
- 21.Chen CM, Dubin R, Kim MC. Emerging trends and new developments in regenerative medicine: a scientometric update (2000–2014). Expert Opin Biol Ther. 2014;14(9):1295–1317. doi: 10.1517/14712598.2014.920813 [DOI] [PubMed] [Google Scholar]
- 22.Malde S, Palmisani S, Al-Kaisy A, Sahai A. Guideline of guidelines: bladder pain syndrome. BJU Int. 2018;122(5):729–743. doi: 10.1111/bju.14399 [DOI] [PubMed] [Google Scholar]
- 23.Rosen JM, Klumpp DJ. Mechanisms of pain from urinary tract infection. Int J Urol. 2014;21:26–32. doi: 10.1111/iju.12309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elbadawi A. Interstitial cystitis: a critique of current concepts with a new proposal for pathologic diagnosis and pathogenesis. Urology. 1997;49(5A):14–40. doi: 10.1016/S0090-4295(99)80329-X [DOI] [PubMed] [Google Scholar]
- 25.Reche A, Buffington CAT. Increased tyrosine hydroxylase immunoreactivity in the locus coeruleus of cats with interstitial cystitis. J Urol. 1998;159(3):1045–1048. doi: 10.1016/S0022-5347(01)63833-3 [DOI] [PubMed] [Google Scholar]
- 26.Parsons CL. The role of the urinary epithelium in the pathogenesis of interstitial cystitis/prostatitis/urethritis. Urology. 2007;69:9–16. doi: 10.1016/j.urology.2006.03.084 [DOI] [PubMed] [Google Scholar]
- 27.Wada N, Ameda K, Furuno T, Okada H, Date I, Kakizaki H. Evaluation of prostaglandin E2 and E-series prostaglandin receptor in patients with interstitial cystitis. J Urol. 2015;193(6):1987–1993. doi: 10.1016/j.juro.2015.01.010 [DOI] [PubMed] [Google Scholar]
- 28.Liu BL, Yang F, Zhan HL, et al. Increased severity of inflammation correlates with elevated expression of TRPV1 nerve fibers and nerve growth factor on interstitial cystitis/bladder pain syndrome. Urol Int. 2014;92(2):202–208. doi: 10.1159/000355175 [DOI] [PubMed] [Google Scholar]
- 29.Peeker R, Enerback L, Fall M, Aldenborg F. Recruitment, distribution and phenotypes of mast cells in interstitial cystitis. J Urol. 2000;163(3):1009–1015. doi: 10.1016/S0022-5347(05)67873-1 [DOI] [PubMed] [Google Scholar]
- 30.Hofmeister MA, He F, Ratliff TL, Mahoney T, Becich MJ. Mast cells and nerve fibers in interstitial cystitis (IC): an algorithm for histologic diagnosis via quantitative image analysis and morphometry (QIAM). Urology. 1997;49(5A):41–47. doi: 10.1016/S0090-4295(99)80330-6 [DOI] [PubMed] [Google Scholar]
- 31.Munoz A, Smith CP, Boone TB, Somogyi GT. Overactive and underactive bladder dysfunction is reflected by alterations in urothelial ATP and NO release. Neurochem Int. 2011;58(3):295–300. doi: 10.1016/j.neuint.2010.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peters KM, Carrico DJ, Kalinowski SE, Ibrahim IA, Diokno AC. Prevalence of pelvic floor dysfunction in patients with interstitial cystitis. Urology. 2007;70(1):16–18. doi: 10.1016/j.urology.2007.02.067 [DOI] [PubMed] [Google Scholar]
- 33.Nickel JC, Payne CK, Forrest J, Parsons CL, Wan GJ, Xiao XY. The relationship among symptoms, sleep disturbances and quality of life in patients with interstitial cystitis. J Urol. 2009;181(6):2555–2561. doi: 10.1016/j.juro.2009.02.030 [DOI] [PubMed] [Google Scholar]
- 34.Bade J, Ishizuka O, Yoshida M. Workshop 8: future research needs for the definition/diagnosis of interstitial cystitis. Int J Urol. 2003;10:S31–S34. doi: 10.1046/j.1442-2042.10.s1.9.x [DOI] [PubMed] [Google Scholar]
- 35.Buffington CAT. Comorbidity of interstitial cystitis with other unexplained clinical conditions. J Urol. 2004;172(4):1242–1248. doi: 10.1097/01.ju.0000137953.49304.6c [DOI] [PubMed] [Google Scholar]
- 36.Soler R, Bruschini H, Freire MP, Alves MT, Srougi M, Ortiz V. Urine is necessary to provoke bladder inflammation in protamine sulfate induced urothelial injury. J Urol. 2008;180(4):1527–1531. doi: 10.1016/j.juro.2008.06.006 [DOI] [PubMed] [Google Scholar]
- 37.Rosamilia A, Cann L, Scurry J, Rogers P, Dwyer P. Bladder microvasculature and the effects of hydrodistention in interstitial cystitis. Urology. 2001;57(6 Suppl 1):132. doi: 10.1016/S0090-4295(01)01149-9 [DOI] [PubMed] [Google Scholar]
- 38.Dell JR, Parsons CL. Multimodal therapy for interstitial cystitis. J Reprod Med. 2004;49(3):243–252. [PubMed] [Google Scholar]
- 39.Sonmez MG, Kozanhan B. Complete response to acupuncture therapy in female patients with refractory interstitial cystitis/bladder pain syndrome. Ginekol Pol. 2017;88(2):61–67. doi: 10.5603/GP.a2017.0013 [DOI] [PubMed] [Google Scholar]
- 40.Padilla-Fernandez B, Hernandez-Hernandez D, Castro-Diaz DM. Current role of neuromodulation in bladder pain syndrome/interstitial cystitis. Ther Adv Urol. 2022;14:17562872221135941. doi: 10.1177/17562872221135941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barr S. Diagnosis and management of interstitial cystitis. Obstet Gynecol Clin North Am. 2014;41(3):397–407. doi: 10.1016/j.ogc.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 42.Kim E, Brown L, Seltzer E, et al. Development of a patient-centered text message-based platform for the self-management of interstitial cystitis/bladder pain syndrome symptoms. Neurourol Urodyn. 2023;42(2):510–522. doi: 10.1002/nau.25115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schaeffer E. Re: atypical microorganisms in expressed prostatic secretion from patients with chronic prostatitis/chronic pelvic pain syndrome: microbiological results from a case-control study. J Urol. 2015;193(3):863. [DOI] [PubMed] [Google Scholar]
- 44.Koh J, Ko H, Wang S, et al. Depression and somatic symptoms may influence on chronic prostatitis/chronic pelvic pain syndrome: a preliminary study. Psychiatry Investig. 2014;11(4):495–498. doi: 10.4306/pi.2014.11.4.495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clemens J, Brown S, Calhoun E. Mental health diagnoses in patients with interstitial cystitis/painful bladder syndrome and chronic prostatitis/chronic pelvic pain syndrome: a case/control study. J Urol. 2008;180(4):1378–1382. doi: 10.1016/j.juro.2008.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shoskes D, Berger R, Elmi A, Landis J, Propert K, Zeitlin S. Muscle tenderness in men with chronic prostatitis/chronic pelvic pain syndrome: the chronic prostatitis cohort study. J Urol. 2008;179(2):556–560. doi: 10.1016/j.juro.2007.09.088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yilmaz U, Liu Y, Berger R, Yang C. Autonomic nervous system changes in men with chronic pelvic pain syndrome. J Urol. 2007;177(6):2170–2174. doi: 10.1016/j.juro.2007.01.144 [DOI] [PubMed] [Google Scholar]
- 48.Shahed AR, Shoskes DA. Correlation of beta-endorphin and prostaglandin E2 levels in prostatic fluid of patients with chronic prostatitis with diagnosis and treatment response. J Urol. 2001;166(5):1738–1741. doi: 10.1016/S0022-5347(05)65664-9 [DOI] [PubMed] [Google Scholar]
- 49.Pontari M, Ruggieri M. Mechanisms in prostatitis/chronic pelvic pain syndrome. J Urol. 2004;172(3):839–845. doi: 10.1097/01.ju.0000136002.76898.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berger RE. Effect of antibiotic therapy on interleukin-6 in fresh semen and postmasturbation urine samples of patients with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2009;73(6):1428–1429. doi: 10.1016/j.urology.2008.05.059 [DOI] [PubMed] [Google Scholar]
- 51.He L, Wang Y, Long Z, Jiang C. Clinical significance of IL-2, IL-10, and TNF-alpha in prostatic secretion of patients with chronic prostatitis. Urology. 2010;75(3):654–657. doi: 10.1016/j.urology.2009.09.061 [DOI] [PubMed] [Google Scholar]
- 52.Desireddi NV, Campbell PL, Stern JA, et al. Monocyte chemoattractant protein-1 and macrophage inflammatory protein-1 alpha as possible biomarkers for the chronic pelvic pain syndrome. J Urol. 2008;179(5):1857–1861. doi: 10.1016/j.juro.2008.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Quick ML, Mukherjee S, Rudick CN, Done JD, Schaeffer AJ, Thumbikat P. CCL2 and CCL3 are essential mediators of pelvic pain in experimental autoimmune prostatitis. Am J Physiol. 2012;303(6):R580–R589. doi: 10.1152/ajpregu.00240.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Berger RE. A pollen extract (Cernilton) in patients with inflammatory chronic prostatitis-chronic pelvic pain syndrome: a multicentre, randomised, prospective, double-blind, placebo-controlled phase 3 study comment. J Urol. 2010;183(4):1403. doi: 10.1016/j.juro.2009.12.072 [DOI] [PubMed] [Google Scholar]
- 55.Haenen G, Paquay J, Korthouwer R, Bast A. Peroxynitrite scavenging by flavonoids. Biochem Biophys Res Commun. 1997;236(3):591–593. doi: 10.1006/bbrc.1997.7016 [DOI] [PubMed] [Google Scholar]
- 56.Chang WS, Lee YJ, Lu FJ, Chiang HC. Inhibitory effects of flavonoids on xanthine oxidase. Anticancer Res. 1993;13(6A):2165–2170. [PubMed] [Google Scholar]
- 57.Zhang K, Liu YX, Yang WB, et al. Efficacy and safety of ningmitai capsule in patients with chronic prostatitis/chronic pelvic pain syndrome: a multicenter, randomized, double-blind, placebo-controlled trial. Urology. 2021;153:264–269. doi: 10.1016/j.urology.2021.01.018 [DOI] [PubMed] [Google Scholar]
- 58.Panunzio A, Tafuri A, Mazzucato G, et al. Botulinum Toxin-A injection in chronic pelvic pain syndrome treatment: a systematic review and pooled meta-analysis. Toxins. 2022;14:1. doi: 10.3390/toxins14010025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wheeler A, Smith HS. Botulinum toxins: mechanisms of action, antinociception and clinical applications. Toxicology. 2013;306:124–146. doi: 10.1016/j.tox.2013.02.006 [DOI] [PubMed] [Google Scholar]
- 60.White B, Welge M, Auvil L, et al. Microbiota of chronic prostatitis/chronic pelvic pain syndrome are distinct from interstitial cystitis/bladder pain syndrome. medRxiv. 2021;2021:3. [Google Scholar]
- 61.Ullrich PM, Turner JA, Ciol M, Berger R. Stress is associated with subsequent pain and disability among men with nonbacterial prostatitis/pelvic pain. Ann Behav Med. 2005;30(2):112–118. doi: 10.1207/s15324796abm3002_3 [DOI] [PubMed] [Google Scholar]
- 62.Pontari MA. Chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: are they related? Curr Urol Rep. 2006;7(4):329–334. doi: 10.1007/s11934-996-0013-1 [DOI] [PubMed] [Google Scholar]