Abstract
Study Objectives
To investigate medical students’ sleep quality and duration prior to a major clinical assessment, and their association with clinical performance.
Methods
Third year medical students were surveyed following the end of year Observed Structured Clinical Examination (OSCE) using a self-completed questionnaire. The questionnaire focussed on sleep in the month and night before the assessment. OSCE scores were linked to questionnaire data for analysis.
Results
The response rate was 76.6% (216/282). Poor sleep quality (Pittsburgh Sleep Quality Index > 5) was reported by 56.9% (123/216) and 34.7% (75/216) of students the month and night before the OSCE, respectively. Sleep quality the night before the OSCE was significantly associated with OSCE score (p = .038), but not sleep quality in the preceding month. The night before the OSCE, students obtained an average of 6.8 h sleep (median 7, SD 1.5, range 2–12 h). Short sleep duration (≤6 h) was reported by 22.7% (49/216) and 38.4% (83/216) of students in the month and the night before the OSCE, respectively. Sleep duration the night before the OSCE was significantly associated with OSCE score (p = .026), but no significant association was found between OSCE score and sleep duration in the preceding month. Use of medication to help with sleep was reported by 18.1% (39/216) of students in the preceding month and by 10.6% (23/216) in the night before the OSCE.
Conclusions
Medical students’ sleep quality and duration the night before a clinical assessment were correlated with their performance in that assessment.
Keywords: sleep quality, sleep duration, medical students, performance, clinical assessment, undergraduate medical education
Statement of Significance.
Sleep is important for memory and learning as well as for psychological wellbeing. Poor sleep impacts academic performance, but the impact on medical students’ clinical performance is less clear. This study showed medical students commonly have poor quality sleep as well as less than the recommended number of hours. Higher sleep quality and recommended sleep duration the night before an Observed Structured Clinical Examination (OSCE) was associated with better clinical performance—although causation cannot be inferred. Medical students using medication to help with sleep appears to be common and requires further exploration. In addition, future research is required to explore factors contributing to sufficient sleep for an individual and whether improved sleep quality and duration could impact clinical performance.
Introduction
The term ‘sleep health’ has been used to conceptualize sleep as more than the presence or absence of a sleep disorder [1]. This holistic view is congruent with the wide-ranging impacts of sleep on an individual’s health, quality of life, and ability to function. Sleep is important for memory [2, 3], creative problem-solving [4], and motor skills [5] as well as playing a critical role in emotional regulation [6]. Sleep also plays a crucial role in psychological wellbeing, as poor sleep quality has been associated with depression, anxiety, and thoughts of self-harm [7, 8]. Poor sleep quality and short sleep duration have also been shown to be significantly associated with an increased risk of adverse outcomes such as accidents [9]. This evidence highlights the importance of optimal sleep health for those in the medical profession given the specific requirements of the role of a doctor, which involve managing stress, thinking critically, and making decisions, whilst dealing with shift work, night duty and being on call.
It is known that sleep deteriorates in the first year of working as a doctor [10]. Kalmbach et al. prospectively studied medical interns (Postgraduate Year 1) to look at the role of pre-internship sleep disturbance on subsequent sleep and anxiety during internship [11]. The study found that pre-internship (final year medical students) poor sleepers (defined by the Pittsburgh Sleep Quality Index [12]) had more than twice the odds of having short sleep duration (≤6 h) during internship, than pre-internship good sleepers [11]. Therefore, increasing medical students’ and educators’ awareness of the potential impact of insufficient sleep is vital. It may present an opportunity for early intervention during undergraduate training, to divert a trajectory leading towards suboptimal health and performance.
In New Zealand, a survey of university students (including medical students) showed that almost 40% had significant sleep issues lasting for more than a month [13]. Sleep disruption is more prevalent in medical students than both non-medical university students, and the general population [14–16]. It has been proposed that this may be related to factors such as academic load, attitudes and expectations, and lifestyle factors [17].
The ways in which medical students’ sleep impacts their academic performance have been widely reported. For instance, the complexity of the relationship between sleep and mood/emotion and academic performance are detailed in a recent comprehensive review by Mehta (2022) [18]. A recent systematic review and meta-analysis of the impact of sleep disruption on academic performance in medical students showed significant associations between both poorer sleep quality and higher daytime sleepiness scores with poorer academic performance [14]. Although sleep quality appears to be correlated with academic outputs, the meta-analysis did not show a significant association between sleep duration and academic performance. However, this may be related to the significant heterogeneity in outcomes between the nine studies which included sleep duration as a variable. Despite this evidence, there is a need for more in-depth research into specific aspects of medical students’ sleep, in terms of its implications for clinical practice. For instance, as opposed to academic grades, is the duration or quality of sleep correlated with ‘hands-on performance’, i.e. the ability to demonstrate competence in a task whilst being observed (‘clinical assessment’)? Studies that have looked at the effect of sleep on academic performance in medical students have almost exclusively used (often self-reported) Grade Point Average (GPA) to represent academic performance. In reality, this could reflect test-based assessments, reports, and other non-clinical assessments as well as clinical components. It has been shown that sleep deprivation after night shift impacts medical students’ ability to pay attention [19], and that 24 h of sleep deprivation increases the time taken to complete tasks and affects judgment [20] when using paper–pencil neurocognitive testing. However, there is limited research into the clinical performance of medical students. Clinical assessments are a standard part of assessment in medical school and are often ‘high-stakes’. Given that these assessments require not only knowledge, but listening, comprehension, professionalism, verbal skills (e.g. interacting with an actor by taking a history), and/or performing an examination or procedural task (psychomotor skills) we were interested in the effect of sleep on this particular type of performance (which more closely models the future role on clinical attachments or as an intern). We were also interested in the immediacy of the effect, that is, does the sleep the night before the clinical assessment influence performance? This aspect in particular, may be one that is amenable to an educational intervention for the students.
To explore this issue further, the aims of this study were firstly, to investigate the sleep quality of medical students prior to a clinical assessment and secondly, to investigate any correlation between medical students’ sleep and their performance in a clinical assessment. As part of this, we were also interested in looking at the use of medication to help with sleep, in case students were only reporting that they slept well due to the use of medication. To achieve these aims, we determined to assess the sleep quality and duration of medical students in the month and night prior to a major clinical assessment (the Year 3 Observed Structured Clinical Examination [OSCE]), and to compare the sleep quality and duration with performance in the OSCE. This enabled us to explore our research questions of ‘What is the sleep quality of medical students in the month prior to a major clinical assessment?’, ‘Does sleep quality and duration (month before/night before) have an association with performance in a clinical assessment?’, and ‘what is the prevalence of sleeping medication use in medical students?’.
This research is the first exploration of sleep quality and performance in medical students in New Zealand and the first study we are aware of internationally to investigate the association of sleep with medical students’ performance specifically in a clinical assessment.
Methods
Study design
Prior to the Year 3 OSCE, medical students were informed of the research during a lecture. They were then sent written information about the research and the Participant Information Sheet via an electronic class notification. Directly after completion of the Year 3 OSCE, a consent form and structured self-complete questionnaire were administered by a research assistant to those who volunteered to participate. The research assistant then entered questionnaire responses and OSCE grades identified only by study participant identification numbers into a spreadsheet, which was then forwarded to the researchers. This procedure ensured that the researchers were blinded to participant identities.
Participants
Participants were Year 3 undergraduate medical students from the University of Auckland, New Zealand at the end of 2018. The students (N = 282) were invited to complete the questionnaire immediately following their compulsory end-of-year OSCE. Year 3 is the second year of the six-year Medical Programme, Year 1 being a common health science year. Year 3 involves mostly campus-based teaching and learning, including clinical skills in simulation, with only a few hospital-based clinical afternoons, and no shift-work.
Measures
The questionnaire comprised of demographic information (age, gender, ethnicity), questions related to the daily number of caffeinated drinks, frequency of at least 30 min of physical activity in an average week, breakfast consumption in an average week (these lifestyle factors will be reported elsewhere), and sleep measures. The sleep measures included questions relating to sleep the night before the Year 3 OSCE (hours of sleep, rating of sleep quality, and sleep medication use), and the Pittsburgh Sleep Quality Index (PSQI) [12]. The PSQI is a validated measure of sleep quality in the preceding month [12]. It has commonly been used as a measure of sleep quality when investigating the sleep quality of medical students [14]. The rationale for a sleep quality measure that represented data from the preceding month is that it allows the frequency and duration of any difficulties to be captured in a defined time period [12]. A measure that reflects sleep in the month prior to an assessment also enables data to be captured that represent a period of time that is often a higher stress period than other times in the year—it is possible that cumulative sleep deficits over this time could impact upon performance in a clinical assessment. This complements data from the night before the assessment. For example, for students sleeping mostly poorly for the month before the assessment but then managing a good night’s sleep on the night before the assessment there might be a different association with performance than if we were only aware of their night of good sleep. The PSQI asks questions about seven components relating to sleep quality (sleep quality, sleep onset latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction). Component scores are combined to give an overall score (range 0–21) where higher scores indicate poorer sleep quality. The overall score differentiates between ‘good sleepers’ (0–5) and ‘poor sleepers’ (6–21) (diagnostic sensitivity 89.6% and specificity 86.5%, kappa = 0.75, p < .001) [12]. A recent approach to categorization of PSQI scores has been used to denote those scoring 6–10 as ‘moderately poor sleepers’ and those scoring >10 as ‘very poor sleepers’, which is clinically useful [21]. The PSQI question relating to use of medication to help with sleep was used to determine the prevalence of use in the month preceding the OSCE.
Observed Structured Clinical Examination (OSCE)
The Year 3 OSCE is a three-station clinical assessment held at the end of Year 3. The purpose of the OSCE is to assess the performance of students in clinical skills (history-taking and examination skills) as part of the Clinical and Communication Skills Domain. Every station takes 10 minutes and has one trained clinician examiner. Two of the stations are physical examination stations with a ‘normal healthy model’ (recruited for the purpose) and one is a history-taking station with a ‘simulated patient’ (trained actor). Examiners are trained to use descriptive criteria to assess performance, which include a skills guide for physical examination stations. A global assessment of performance for each station, based on written standards, is utilized for each station. The OSCE is a ‘must pass’ component of the course.
Statistical analyses
Descriptive statistics were used to report the sleep quality and duration in the month before the OSCE and the night before the OSCE, along with the use of medication to help with sleep. Sleep quality the night before the OSCE was rated as either ‘very good’, ‘fairly good’, ‘fairly bad’, or ‘very bad’ based on question six of the PSQI [12]. These categories were dichotomized into either ‘good’ sleep quality or ‘poor’ sleep quality and tested for statistical association with the OSCE grade (Fail, Borderline Pass, Pass, and Distinction) using a Pearson Chi-Square analysis. For sleep quality the month before the OSCE, the linear association between PSQI [12] total score and the total OSCE score was measured using the Pearson correlation coefficient (Pearson’s r).
Sleep duration was dichotomized into ≤6 h sleep (short sleep) and >6 h to ascertain the proportion of students with short sleep duration. This definition of short sleep is in line with empirically-derived thresholds for neurobehavioural dysfunction and recent research [22]. The linear association between sleep duration the night before the OSCE and the total OSCE score was measured using Pearson’s r. The proportion of students with ≤6 h sleep and >6 h was tested for statistical association with two categories of OSCE performance (fail/borderline pass vs distinction) using a Pearson Chi-Square analysis. The linear association between the average sleep duration the month before the OSCE and the total OSCE score were measured using Pearson’s r.
To look at the characteristics of those students who failed, sleep quality, sleep duration, and medication use were tested for statistical association with OSCE performance (fail vs other grades) using a Pearson Chi-Square analysis.
Data were analyzed using IBM SPSS Statistics; Version 28.
Results
Demographic characteristics
Completed questionnaires were received from 76.6% of the students (216/282). No data are available regarding those who did not participate (Table 1).
Table 1.
Demographic characteristics of those completing the questionnaire
| Characteristic | n (%) |
|---|---|
| Age (years) | |
| 15–19 | 5 (2.3) |
| 20–24 | 182 (84.3) |
| 25–29 | 24 (11.1) |
| 30–34 | 4 (1.9) |
| 35–39 | 1 (0.4) |
| Gender | |
| Male | 94 (43.5) |
| Female | 122 (56.5) |
| Ethnicity* | |
| New Zealand European | 116 (53.7) |
| Māori | 32 (14.8) |
| Pacific peoples† | 15 (6.9) |
| Chinese | 38 (17.6) |
| Indian | 18 (8.3) |
| Other | 53 (24.5) |
*Some participants identified as more than one ethnic group.
†Samoan, Cook Island Māori, Tongan.
Sleep quality
On average, in the month before the OSCE, 93 students (43.1%) reported good sleep quality (PSQI ≤ 5), 99 students (45.8%) moderately poor sleep quality (PSQI 6–10), and 24 students (11.1%) very poor (PSQI > 10) sleep quality.
The night before the OSCE, 75 students (34.7%) reported a ‘poor’ sleep quality (fairly bad or very bad).
Sleep duration
In the month before the OSCE, 22.7% (49/216) of students slept ≤6 h, and the average sleep duration was 7.1 h (median 7, SD 1.1, range 7 [3 to 10 h]). On the night before the OSCE, 38.4% (83/216) of students slept ≤6 h, and the average sleep duration was 6.8 h (median 7, SD 1.5, range 10 [2 to 12 h]).
Medication use
Overall, 18.1% (39/216) of students reported some use of medication to help with sleep in the month before the OSCE (frequency of use is presented in Table 2).
Table 2.
Use of medication to help with sleep
| Frequency of use of medication to help with sleep* | N (%) | Any use in the past month† | At least weekly use† | High use† |
|---|---|---|---|---|
| Not during the past month | 177 (81.9) | |||
| <1 × per week | 15 (6.9) | 39 | ||
| 1–2 × per week | 15 (6.9) | (18.1) | 24 | |
| ≥3 × per week | 9 (4.2) | (11.1) | 9 (4.2) |
*From Question 7 of the PSQI [12]: ‘During the past month, how often have you taken medicine to help you sleep (prescribed or “over the counter”)?
†Descriptors of use used in the analysis.
Twenty-three students (10.6%) reported using medication to help with sleep on the night before the OSCE. Of these students, 10/23 (43.5%) had a ‘poor’ sleep quality (fairly bad or very bad) and 8/23 (34.8%) slept ≤6 h.
OSCE performance
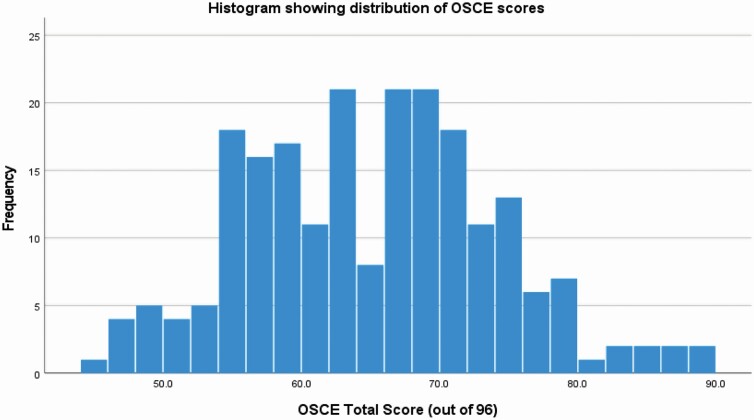
For the entire sample (N = 216), the mean OSCE score was 65 (2 significant figures [s.f]) out of a total score of 96, with a standard deviation of 9.0 (2 s.f). The distribution of OSCE scores is shown in Figure 1. The OSCE cut-point was calculated by the borderline method and was 50% in this case. The OSCE total score was normally distributed (Kolmogorov–Smirnov test, p = .070). With regards to grades, five students failed (<50% total OSCE score), 14 students had a borderline performance (50%–55%), 179 passed (56%–80%), and 18 students achieved a distinction (>80%).
Figure 1.
Histogram showing distribution of total OSCE scores.
There was no significant association between age, gender, and ethnicity (Māori vs Non-Māori) and OSCE performance (fail/borderline performance versus pass/distinction, Pearson Chi-square, p > .05 for all comparisons).
Station performance (history vs physical examination)
There was no significant difference in the global station scores between the physical examination stations (Station A and Station B) and the history station (Station C) (Station A vs Station C, Pearson Chi-Square, p = .713; or Station B vs Station C, Pearson Chi-Square, p = .387).
The impact of sleep quality
Sleep quality the month before the OSCE (PSQI score) was not significantly correlated with total OSCE score (Pearson’s r = −0.061, p = .372). However, there was a significant correlation between sleep quality (‘good’ vs ‘poor’) the night before the OSCE and the OSCE grade (fail, borderline pass, pass, and distinction) (p = .038, Pearson Chi-Square).
Distribution of grades for ‘good’ vs ‘poor’ sleep quality the night before is shown in Table 3.
Table 3.
Distribution of grades for ‘good’ vs ‘poor’ sleep quality the night before the OSCE
| Sleep quality the night before OSCE N (%) |
Total | ||
|---|---|---|---|
| Poor | Good | ||
| Fail | 4 (80.0%) | 1 (20.0%) | 5 |
| Borderline performance | 3 (21.4%) | 11 (78.6%) | 14 |
| Pass | 65 (36.3%) | 114 (63.7%) | 179 |
| Distinction | 3 (16.7%) | 15 (83.3%) | 18 |
| Total | 75 (34.7%) | 141 (65.3%) | 216 |
The impact of sleep duration
Average sleep duration of the month before the OSCE was not significantly correlated with total OSCE score (Pearson’s r = −0.34, p = .621). However, sleep duration the night before the OSCE was significantly correlated with the total OSCE score (Pearson’s r = 0.151, p = .026). In addition, significantly more students obtaining a borderline pass or fail grade had a short sleep the night before the OSCE compared to those obtaining a distinction (Pearson Chi-Square, p = .004,). Distribution of grades for ‘short’ vs ‘normal’ sleep duration the night before is shown in Table 4.
Table 4.
Distribution of grades for ‘short’ vs ‘normal’ sleep duration the night before the OSCE
| Sleep duration the night before OSCE N (%) |
||
|---|---|---|
| Less than or equal to 6 h | Greater than 6 h | |
| Fail or borderline performance | 12 (63.2%) | 7 (36.8%) |
| Distinction | 3 (16.7%) | 15 (83.3%) |
| Total | 15 (40.5%) | 22 (59.5%) |
Medication use
A significantly higher proportion of students who used medication to sleep the month before the OSCE had a fail/borderline grade (17.9% [7/39]) as compared with those who did not take medication to sleep (6.8% [12/177]), (Pearson Chi-Square, p = .0260).
Students receiving a ‘Fail’ grade
From our sample (N = 216), five students failed the OSCE (2.3%). Of the five students who failed, all five had a borderline performance for the physical examination station (Station B), one out of five had a borderline performance at the other physical examination station (Station A), and two of the five had a borderline performance at the history station (Station C). None of the students failed any individual station (nor did any get a distinction); however, it was their cumulative performance that resulted in their overall fail grade.
Of the students who failed, 40% (2/5) had very poor sleep quality (PSQI > 10) the month before the OSCE compared to 10.4% (22/211) who did not fail (Pearson Chi-Square, p = .038) and 80% (4/5) had poor sleep quality the night before the OSCE as compared with 33.6% (71/211) who did not fail (Pearson Chi-Square, p = .31). In addition, 40% (2/5) had a short average sleep duration the month before the OSCE compared to 22.2% (47/211) who did not fail (Pearson Chi-Square, p = .350) and 100% (5/5) had a short sleep the night before the OSCE compared to 40.0% (78/211) who did not fail (Pearson Chi-Square, p = .004).
Those who failed were not more likely to have used medication to help with sleep in the month before the OSCE (Pearson Chi-Square, p = .909) and were not more likely to have used medication to help with sleep the night before the OSCE as compared with those who did not fail (Pearson Chi-Square, p = .435).
Discussion
This study provides a snapshot of the sleep quality and duration of a cohort of medical students, as well as exploring associations between these sleep variables and students’ clinical assessment scores. Although there has been some research into sleep quality and cognitive performance assessed by computerized or paper-based tasks [19, 20, 23] this is the first study we are aware of that has measured sleep quality, duration, and correlation with performance in a clinical OSCE. Over half of the medical student sample reported poor sleep quality over the preceding month. This is higher than poor sleep reported in studies in a general population [24] and New Zealand university students (including medical students) [13]. Almost one-quarter of the medical students usually slept on average ≤6 h per night (7–9 h is recommended by National Sleep Foundation) [25].
In this study, individuals who reported sleeping on average ≤6 h per night were identified as short sleepers [26]. Almost 40% of students had a short sleep on the night before the OSCE, which has the potential to impact upon cognitive performance (particularly high-level reasoning and verbal skills) [26]. Students who achieved a distinction grade were significantly more likely to have had >6 h sleep the night before the OSCE. However, we cannot conclusively state from this that it would be advantageous to prioritize more than 6 h sleep on the night before a clinical assessment, as the study was not designed to show causality. For example, another possibility is that students who were better prepared for the OSCE felt less anxious and were thus more able to sleep for longer periods. In other words, although an association has been shown, whether sleep influenced academic output or whether academic preparation influenced sleep, cannot be stated.
A large proportion of students in this study reported poor sleep quality in the pre-assessment month (56.9%). Although only five students failed, these students were more likely to have had very poor sleep quality in the month before the OSCE as compared with the students who did not fail (p = .038). It is not known if the poor performance was due to the poor sleep, or if the poor sleep was a marker of some other factor that impacted upon performance. For example, Yassin et al (2020) found that self-reported sleep disorders (according to questionnaire responses) were common among medical students and that several sleep disorders were associated with poor academic performance (measured by GPA) [27]. In addition, the weeks before an assessment are generally the time that study and preparation for the assessment occur. Poor sleep quality in this preparatory period may impact performance as sleep after learning acquisition is thought to be beneficial for memory consolidation and performance [28]. Either way, the group of students who failed may represent those who would benefit in particular from further sleep assessment and management or education regarding sleep.
In a comprehensive meta-analysis of the prevalence of poor sleep quality in medical students, the pooled prevalence of poor sleep quality as measured by the PSQI was 52.7% (95% Confidence Interval: 45.3% to 60.1%) [17]. However, the cut-off points for poor sleep quality and the timing of the surveys (usual semester time or prior to an assessment) did vary slightly across studies. In a German study of 144 medical students undertaking a high-stakes written exam, 59% of students reported poor sleep quality (PSQI > 5) in the month before the exam [29]. The study found that academic performance correlated with stress and sleep quality in the pre-exam period (r = 0.26, p < .001 and r = 0.158, p < .03) [29]. Alotaibi et al noted the association of poor sleep quality with stress, but not academic performance measured by (self-reported) GPA [30]. It may be that the poor performance associated with poor sleep quality seen in our study is mediated by stress, or that poor sleep quality impacts the unique aspects of an observed clinical assessment (listening, comprehension, professionalism, verbal skills, and psychomotor skills) than it does other aspects of academic performance (e.g. a written exam without senior clinicians observing performance).
In contrast with our results, in a study of Australian medical students, Cevjic et al. found higher academic standing (self-reported weighted average mark) was predicted by less refreshing and shorter but more consistent sleep durations and earlier bedtimes [23]. However, the concept of nightly variability of sleep times (i.e. erratic or regular sleep–wake schedules) was not explored in the current study.
The use of medication to help with sleep on the night before the OSCE reported by 10.6% of students in the current study was an unexpected finding. The implications of this are not clear, but it requires further exploration. Of the students taking medication to help with sleep, almost half had ‘bad’ sleep quality and over a third slept ≤6 h (i.e. poor sleep quality and duration despite the use of medication to help with sleep). Use of sleeping medication is therefore clearly not a guarantee of good or sufficient sleep. This may be due to the sleep achieved with the use of sleeping medications not being a naturalistic sleep [31]. For example, brain activity measured using an electroencephalogram (EEG) shows significantly reduced slow wave activity in healthy participants taking sleeping medications compared to those taking a placebo [31]. Conversely, poor sleep is not necessarily related to the use of medication. Our study also showed that 11.1% of medical students used medication to help with sleep at least once a week in the month before the OSCE. In a study of medical students across all years of a medical programme in Brazil, of the 372 students who completed the data collection, 4.3% reported use of sleeping medication at least once a week [32]. It would be important to know what the medication use is in this current study’s cohort during the semester (away from the assessment period). Also, it would be worth exploring the reasons that students are taking medication to help with sleep and which particular medications are being used, neither of which was reported in this research. It is likely there is a heterogenous group of medications used as ‘medication to help with your sleep’ (as worded in the PSQI questionnaire). The implications of students use of sleeping medication, particularly on the night before clinical assessment is unknown.
Further research is required to answer a number of questions arising from this study. Why is sleep quality worse in lower scoring students compared to higher scoring students? Could improving sleep quality improve students’ grades? Is poor sleep quality a marker for another factor (such as psychological distress) that might impact learning and performance? Why are some students having little sleep on the night before an assessment, and could this be due to stress, cramming, or other lifestyle/medical factors? How might impaired cognitive performance due to poor sleep specifically affect exam performance? Why are students choosing to take sleeping medications? Is sleeping medication use having an impact on learning or performance? We are hoping to answer a number of these questions with research currently being undertaken in the same cohort.
Strengths
One strength of this study was its relatively large sample size and high response rate. The defined cohort means further study in this group is a possibility. Significantly, the study is opening the conversation about sleep in medical students and anchoring this debate in concerns regarding clinical performance and student wellbeing.
Limitations
There were other end-of-module tests and a progress test in the period around the OSCE so the sleep patterns in the month before the clinical OSCE were reflective of an end-of-year assessment period. Future research looking at sleep patterns in a non-assessment period would give a more accurate picture of ‘baseline’ or ‘usual’ sleep patterns. Studies are needed to determine if the use of medications to help with sleep is different in a month of ‘usual’ sleep. The study used subjective recall for usual sleep duration in the past month from the PSQI rather than using an objective measure such as actigraphy. It was also not possible to capture variability in sleep timing and duration which could have been a marker for erratic sleep habits.
Conclusion
A significant number of medical students experience poor sleep quality and less than the recommended hours of sleep in the period leading up to a clinical assessment. Short sleep duration and poorer sleep quality the night before an observed clinical assessment were associated with lower scores in the assessment. The practice of using medication to help with sleep, particularly the night prior to an assessment, appears to be common, and requires further exploration. This knowledge should be embraced as an opportunity to use medical curricula to address these issues, and enable a healthier medical student population. It is also an opportunity to investigate whether an educational intervention could influence students’ sleep quality and duration; and whether improved sleep quality and duration could impact their clinical performance. Importantly, medical students can be empowered to recognize the significance of sleep for their learning, health, and future work as a health professional, and can be encouraged to take ownership of the issue to improve their self-awareness and management of their own sleep health.
Acknowledgments
Our sincere thanks to Rachael Yielder for assistance with this research and to all the medical students who participated.
Contributor Information
Karen Falloon, Clinical Skills Centre, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand.
Harsh Bhoopatkar, Clinical Skills Centre, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand.
Fiona Moir, Medical Programme Directorate, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand.
Miriam Nakatsuji, Clinical Skills Centre, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand.
Andy Wearn, Clinical Skills Centre, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand; Medical Programme Directorate, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand.
Brief biography of first author
Dr Karen Falloon MBChB, PhD, DipPaed, PGDipMedSc, FRNZCGP
Dr Karen Falloon is a fellow of the Royal New Zealand College of General Practitioners. She received the Health Research Council Clinical Research Training Fellowship to undertake a PhD in General Practice on the topic of insomnia. Karen has worked in both General Practice (GP) and in private sleep clinics and is a member of the Australasian Sleep Association where she serves on the GP education subcommittee. She currently holds academic roles in clinical education (postgraduate and undergraduate) and has research interests in the areas of sleep health, insomnia, and clinical education.
Funding
This research received funding from the University of Auckland performance-based research fund (PBRF).
Disclosure Statements
Financial Disclosure. This research received funding from the University of Auckland performance-based research fund (PBRF).
Non-financial Disclosure: A.W. was the Head of the Medical Programme at the time of research and F.M. is the Pastoral Care Chair and Wellbeing Curriculum Lead, Medical Programme Directorate and Senior Lecturer in the Department of General Practice and Primary Health Care. K.F., H.B., A.W. and M.N. teach Year 3 medical students at the Clinical Skills Centre of the University.
Study data does not reside in a preprint repository.
Ethics Approval and Consent to Participate
The study was approved by the University of Auckland Human Participants Ethics Committee (UAHPEC, approval number 022024). All participants signed informed consent after receiving a detailed participant information sheet regarding the study.
Data Availability Statement
The data for the present study will not be shared publicly as participants were informed at the time of providing consent that only researchers involved in the project would have access to the information they provided.
References
- 1. Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. doi: 10.5665/sleep.3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Girardeau G, et al. Brain neural patterns and the memory function of sleep. Science. 2021;374(6567):560–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Peigneux P, et al. Memory processing in relation to sleep. In: Kryger MH, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine. Philadelphia: Elsevier; 2017: 229–238. [Google Scholar]
- 4. Lewis PA, et al. How memory replay in sleep boosts creative problem-solving. Trends Cogn Sci. 2018;22(6):491–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Van Dongen HP, et al. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–126. doi: 10.1093/sleep/26.2.117 [DOI] [PubMed] [Google Scholar]
- 6. Gruber R, et al. The interplay between sleep and emotion regulation: conceptual framework empirical evidence and future directions. Curr Psychiatry Rep. 2014;16(11):500. [DOI] [PubMed] [Google Scholar]
- 7. Buysse DJ, et al. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473–480. doi: 10.1093/sleep/31.4.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pigeon WR, et al. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;1(9):e1160–e1167. [DOI] [PubMed] [Google Scholar]
- 9. Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. BMJ. 2016; 355: i5210. [DOI] [PubMed] [Google Scholar]
- 10. Kalmbach DA, et al. Effects of sleep, physical activity, and shift work on daily mood: a Prospective Mobile Monitoring Study of Medical Interns. J Gen Intern Med. 2018;33(6):914–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kalmbach DA, et al. Insomnia symptoms and short sleep predict anxiety and worry in response to stress exposure: a prospective cohort study of medical interns. Sleep Med. 2019;55:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Buysse DJ, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- 13. Samaranayake CB, et al. Sleep disorders, depression, anxiety and satisfaction with life among young adults: a survey of university students in Auckland, New Zealand. N Z Med J. 2014;127(1399):13–22. [PubMed] [Google Scholar]
- 14. Seoane HA, et al. Sleep disruption in medicine students and its relationship with impaired academic performance: a systematic review and meta-analysis. Sleep Med Rev. 2020;53:101333. [DOI] [PubMed] [Google Scholar]
- 15. Li L, et al. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res. 2018;27(3):e12648. [DOI] [PubMed] [Google Scholar]
- 16. Azad MC, et al. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. 2015;11(1):69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rao WW, et al. Sleep quality in medical students: a comprehensive meta-analysis of observational studies. Sleep Breath. 2020;24(3):1151–1165. [DOI] [PubMed] [Google Scholar]
- 18. Mehta KJ. Effect of sleep and mood on academic performance—at interface of physiology, psychology, and education. Humanit Soc Sci Commun. 2022;9(16). doi: 10.1057/s41599-021-01031-1 [DOI] [Google Scholar]
- 19. Perez-Olmos I, et al. Night shifts, sleep deprivation, and attention performance in medical students. Int J Med Educ. 2014;5:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dixit A, et al. Psychomotor performance of medical students: effect of 24 hours of sleep deprivation. Indian J. 2012;34(2):129–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Soltani M, et al. Sleepless nights: the effect of socioeconomic status, physical activity, and lifestyle factors on sleep quality in a large cohort of Australian women. Arch Women’s Ment Health. 2012;15(4):237–247. [DOI] [PubMed] [Google Scholar]
- 22. Menicucci D, et al. Sleep slow oscillations favour local cortical plasticity underlying the consolidation of reinforced procedural learning in human sleep. J Sleep Res. 2020;29(5):e13117. [DOI] [PubMed] [Google Scholar]
- 23. Cvejic E, et al. Can you snooze your way to an ‘A’? Exploring the complex relationship between sleep, autonomic activity, wellbeing and performance in medical students. Aust N Z J Psychiatry. 2018;52(1):39–46. [DOI] [PubMed] [Google Scholar]
- 24. Hinz A, et al. Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med. 2017;30:57–63. [DOI] [PubMed] [Google Scholar]
- 25. Hirshkowitz M, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. 2015;1(4):233–243. [DOI] [PubMed] [Google Scholar]
- 26. Wild CJ, et al. Dissociable effects of self-reported daily sleep duration on high-level cognitive abilities. Sleep. 2018;41(12). doi: 10.1093/sleep/zsy182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yassin A, et al. Prevalence of sleep disorders among medical students and their association with poor academic performance: a cross-sectional study. Ann Med Surg (Lond). 2020;58:124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hagewoud R, et al. A time for learning and a time for sleep: the effect of sleep deprivation on contextual fear conditioning at different times of the day. Sleep. 2010;33(10):1315–1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ahrberg K, et al. The interaction between sleep quality and academic performance. J Psychiatric Res. 2012;46(12):1618–1622. doi: 10.1093/sleep/33.10.1315 [DOI] [PubMed] [Google Scholar]
- 30. Alotaibi AD, et al. The relationship between sleep quality, stress, and academic performance among medical students. J Family Community Med. 2020;27(1):23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Arbon EL, et al. Randomised clinical trial of the effects of prolonged-release melatonin, temazepam and zolpidem on slow-wave activity during sleep in healthy people. J Psychopharmacol. 2015;29(7):764–776. [DOI] [PubMed] [Google Scholar]
- 32. Correa CC, et al. Sleep quality in medical students: a comparison across the various phases of the medical course. J Bras Pneumol. 2017;43(4):285–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data for the present study will not be shared publicly as participants were informed at the time of providing consent that only researchers involved in the project would have access to the information they provided.