Abstract
Background
ED data are an important source of surveillance data for monitoring many conditions of public health concern and are especially useful in describing trends related to new, or unusual public health events. The COVID-19 pandemic led to significant changes in emergency care seeking behavior. We described the trends in all-cause emergency department (ED) visit volumes by race, ethnicity, and age using ED data from the National Syndromic Surveillance Program (NSSP) during December 30, 2018–April 2, 2022.
Methods
We described total and race, ethnicity, and age group-specific ED visit volumes during the COVID-19 pandemic by comparing quarterly visit volumes during the pandemic period to the relevant quarters in 2019. We quantified the variability of ED visits volumes by calculating the coefficient of variation in mean weekly ED visit volume for each quarter during Q1 2019–Q1 2022.
Results
Overall ED visits dropped by 32% during Q2 2020, when the COVID-19 pandemic began, then rebounded to 2019 baseline by Q2 2021. ED visits for all race, ethnicity, and age groups similarly dropped in Q2 2020 and adults of all race and ethnicity groups rebounded to at or above pre-pandemic levels while children remained at or below the pre-pandemic baseline except during Q3 2021. There was larger variation in mean weekly ED visits compared to the respective quarter in 2019 for 6 of 9 quarters during Q1 2020–Q1 2022.
Conclusions
ED utilization fluctuated considerably during the COVID-19 pandemic. Overall ED visits returned to within 5% of 2019 baseline during Q2 2021, however, ED visits among children did not return to the 2019 baseline until Q3 2021, then again dropped below the 2019 baseline in Q4 2021. Trends in ED visit volumes were similar among race and ethnicity groups but differed by age group. Monitoring ED data stratified by race, ethnicity and age can help understand healthcare utilization trends and overall burden on the healthcare system as well as facilitate rapid identification and response to public health threats that may disproportionately affect certain populations.
Keywords: COVID-19, Emergency department, Race and ethnicity, Surveillance
1. Introduction
The COVID-19 pandemic led to significant changes in emergency care seeking behavior, with weekly volume of overall emergency department (ED) visits dropping by 42% in spring 2020 compared to spring 2019, and only slightly rebounding in adults by summer 2020 [1]. During December 2020–January 2021, overall ED visit volumes remained 25% lower than during the same time period a year prior [2]. Despite the overall declines, hospital systems and clinicians have described increases in visits for higher acuity conditions such as cardiac arrest during weeks with COVID-19 surges [3]. Changes in all-cause ED visit volume throughout the course of the COVID-19 pandemic by race, ethnicity and age have not been well quantified at the national level.
ED data are an important source of surveillance data for monitoring many conditions of public health concern and are especially useful in describing trends in acute conditions such as myocardial infarction or stroke, or trends related to new, or unusual public health events not identified using existing surveillance systems, such as the E-Cigarette, or Vaping, Product Use–Associated Lung Injury (EVALI) response [4]. ED data also provide a complimentary data source to identify ED visits related to conditions of concern, such as adverse events following the roll-out of the COVID-19 vaccine [5]. Understanding the overall changes in ED visit volumes during the COVID-19 pandemic is imperative when describing trends of any condition because of the large fluctuations in the denominator of total ED visits. Further, understanding how overall ED visit volumes fluctuated by race, ethnicity and age group during the COVID-19 pandemic provides important context that is necessary when describing demographic-specific trends in events of public health concern during the pandemic and in the future.
This work aims to describe the changes in overall ED visit volumes by race, ethnicity, and age using ED data from the National Syndromic Surveillance Program (NSSP) during December 30, 2018–April 2, 2022. We describe how all-cause ED visit volume changed by the demographic characteristics during the COVID-19 pandemic by comparing quarterly visit volumes for each group during the pandemic period (Q1 2020–Q1 2022) to the relevant quarters in 2019. We also quantified the large fluctuations in ED visit volumes observed during the COVID-19 pandemic by calculating coefficient of variation in mean weekly ED visit volumes for each quarter during Q1 2019–Q1 2022.
2. Methods
2.1. Study population
The National Syndromic Surveillance Program (NSSP) is a collaboration among CDC, local and state health departments, and healthcare facilities to monitor a wide variety of health conditions by collecting electronic health data in near real-time [6]. NSSP receives de-identified records from 71% of EDs in the United States, including facilities in all 50 states and the District of Columbia [7]. To reduce artifactual impact from changes in reporting patterns, analyses were restricted to facilities with a coefficient of variation ≤40 for total visit volume and ≥ 75% complete information on race and ethnicity throughout 2019–2022. Thirty-four percent (1595) of EDs enrolled in NSSP from 38 states met the data quality thresholds and were included in this analysis. ED visits were binned into age groups (0–17, 18–64, and 65+ years) and non-mutually exclusive race and ethnicity categories [American Indian or Alaska Native; Asian; Black or African American; Hispanic or Latino; Native Hawaiian or Other Pacific Islander; or White]. Visits with multiple race or ethnicity codes were counted in each relevant race or ethnicity group. For example, if a person identifies as Hispanic or Latino and American Indian or Alaska Native, that ED visit will be counted as Hispanic or Latino and American Indian or Alaska Native or if a person identifies as multiple race groups, then that ED visit will be counted in each identified race group. If a visit has a valid race but is missing ethnicity, it is counted as that race; if a visit indicated Hispanic or Latino for ethnicity but race is missing, that visit is counted as Hispanic or Latino, and if the ethnicity is Not Hispanic or Latino but does not have a valid race code it was not included in our analysis.
2.2. ED visit volume by race, ethnicity, and age
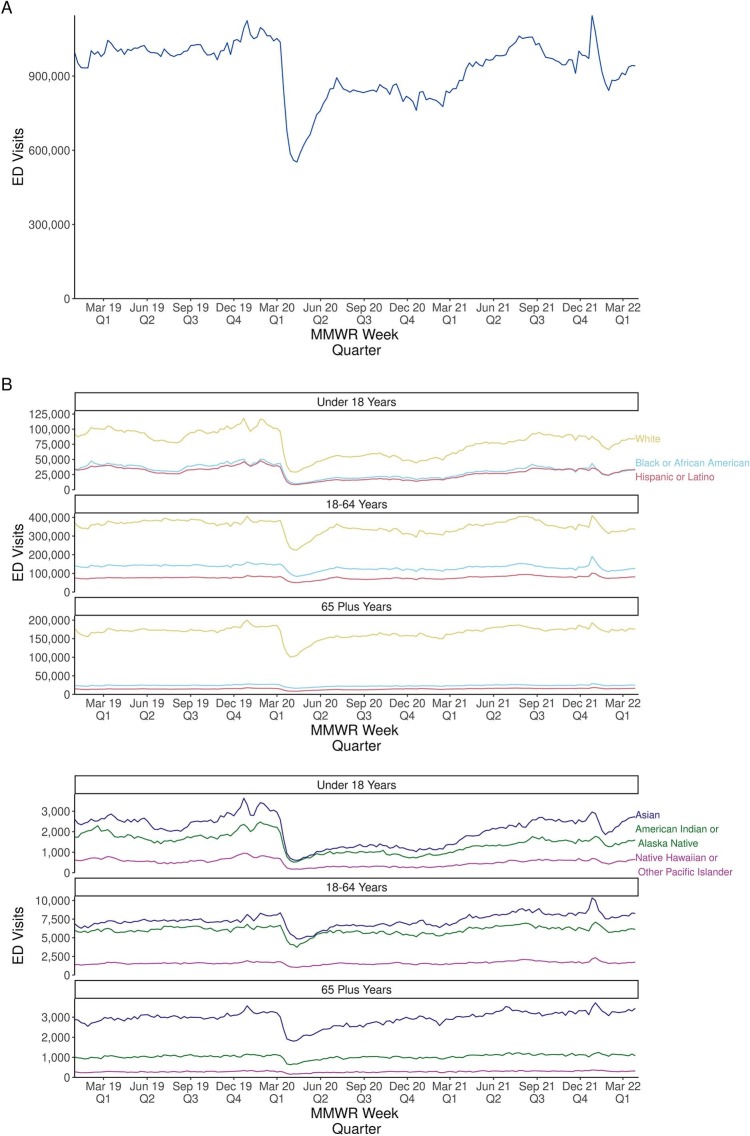
Total all-cause weekly ED visit totals were calculated during December 30, 2018–April 2, 2022 and were stratified by race, ethnicity and age group (Fig. 1 ). Weeks were defined as Sunday–Saturday following Morbidity and Mortality Weekly Report (MMWR) week formatting [8]. Quarterly mean weekly ED visits and 95% confidence intervals [95% CI = mean weekly visits +/− 1.96 * (standard deviation / square root of the number of weeks)] for each race, ethnicity, and age group were calculated for Jan 1, 2019–April 2, 2022 [quarter 1(Q1): MMWR weeks 1–13; quarter 2(Q2): weeks 14–26; quarter 3(Q3): 27–39; and quarter 4(Q4): 40–52]. Because 2020 was a leap year, there is an additional week, MMWR week 53, that is counted in Q4 2020. Percent change in mean weekly ED visits was calculated for each quarter compared to the equivalent quarter in 2019 [((mean weekly visit count for analysis quarter – mean weekly visit count for comparison quarter in 2019) / mean weekly visit count for comparison quarter in 2019)*100]. Percent change in weekly ED visits was classified into three categories: 1. Decreased: >10% below 2019 baseline; 2. Stable: between −10% below and + 10% above 2019 baseline; 3. Increased: >10% above the 2019 baseline.
Fig. 1.
Weekly trends of total all-cause ED visits (A) and ED visits by age group, race, and ethnicity (B)— National Syndromic Surveillance Program (NSSP)*, United States, December 30, 2018–March 27, 2022.
Abbreviations: ED = emergency department; NSSP = National Syndromic Surveillance Program.
* NSSP is a collaboration among CDC, local, and state health departments, and federal, academic, and private sector partners. To reduce artifactual impact from changes in reporting patterns, analyses were restricted to facilities with a coefficient of variation ≤40 and ≥ 75% complete information on race and ethnicity throughout 2019–2022. Visit data from 1595 facilities were included in this analysis. All facilities from Connecticut; District of Columbia; Georgia; Linn County, IA; Maryland; New Jersey; New York City; North Carolina; Ohio; Pennsylvania; San Mateo, CA; and Texas Region 6/5 were not included in this analysis because they did not meet the inclusion criteria.
2.3. Quarterly variation in weekly ED visit volumes
Variation in ED visit volume was assessed by calculating the coefficient of variation (CoV) of mean weekly ED visits for each quarter during quarter 12,019–quarter 12,022. CoV was calculated by dividing the mean weekly ED visit volume by the standard deviation for each quarter. Higher CoV corresponds to larger variation in weekly ED visit volumes.
3. Results
Total ED volume decreased (−32.0%) compared to 2019 at the beginning of the COVID-19 pandemic in Q2 2020 and remained decreased through Q1 2021 (range: −18.3%– -15.4%; Fig. 1, Table A.1). Total ED volume rebounded to within ±10% (range: −3.9%– +3.7%) of the 2019 baseline in Q2 2021–Q4 2021 (Fig. 1, Table A.1). When ED visits were stratified by race, ethnicity, and age group, ED visit volumes dropped dramatically for all groups in Q2 2020 (range: <18 years: −65.5% – -54.8%; 18–64 years: −29.0% – -17.7%; and ≥ 65 years: −28.9% – -19.7%) (Fig. 1, Table A.1). Adults of all race and ethnicity groups rebounded to or above pre-pandemic levels by Q2, 2021 and remained at or above the pre-pandemic baseline during Q3 2021–Q4 2021 (Table A.1). Notably, children of all race and ethnicity groups only rebounded to or above pre-pandemic levels during Q3 2021, then visits for children of all race and ethnicity groups except Asian again dropped below pre-pandemic levels during Q4 2021–Q1 2022.
During Q2 2020, ED visits by all race and ethnicity and age groups decreased (>10% decrease) compared to the corresponding quarter in 2019 (Fig. 1, Table A.1). During Q4 2020, visits by American Indian or Alaska Native and White adults 18–64 years and Black adults >18 years remained decreased compared to the Q4 2019 baseline, while all other adults had returned to within ±10% of the Q4 2019 baseline. Visits among children aged <18 years from all race/ethnicity groups remained decreased compared to the Q4 2019 baseline volume of ED visits (range: −59.0% – -48.2%).
Despite the dramatic decrease in ED visits during Q2 2020, some race, ethnicity, and age groups experienced a > 10% increase in ED visits compared to 2019. In Q2 2021, ED visits among Native Hawaiian or Other Pacific Islander adults (18–64 and ≥ 65 years) increased compared to Q2 2019. During Q3 2021, ED visits among Asian children <18 years (+10.5%) and Asian adults 18–64 years (+15.8%), Hispanic or Latino adults [18–64 (+14.4%) and ≥ 65 years (+12.6%)], and Native Hawaiian or Other Pacific Islander persons of all age groups (<18: +16.0%; 18–64: +21.3%; ≥65: +12.4%) increased compared to Q3 2019. During Q4 2021, ED visits among Asian (+16.5%) and Native Hawaiian or Other Pacific Islander (+10.0%) adults aged 18–64 years increased compared to Q4 2019.
During Q1 2022, ED visits among Asian and Native Hawaiian or Other Pacific Islander adults aged 18–64 years and American Indian or Alaska Native, Asian, Hispanic or Latino, and Native Hawaiian or Other Pacific Islander adults aged ≥65 years were increased compared to the 2019 baseline.
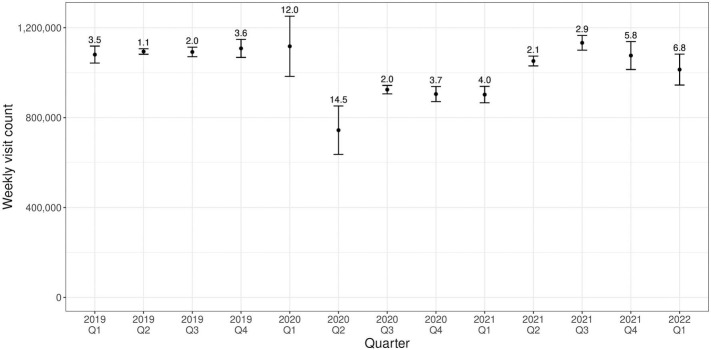
Variation in weekly mean ED visit volumes was reported as the coefficient of variation (CoV) for each quarter (Fig. 2 ). There was greater variation in quarterly mean weekly ED visits during quarters 1, 2 and 4, 2020 (CoV range: 3.7–14.5) than during all quarters in 2019 (CoV range: 1.1–3.6) (Fig. 2). Interestingly, the CoV was 2.0 for both Q3 2019 and Q3 2020, however because the mean weekly visit was lower in 2020, the standard deviation in Q3 2020 was higher than during Q3 2019. All quarters in 2021 and Q1 2022 had larger variation in mean weekly ED visits compared to the respective quarters in 2019 (CoV Q1: 2019: 3.5, 2021: 4.0, 2022: 6.8; Q2: 2019: 1.1, 2021: 2.1; Q3: 2019: 2.0, 2021: 2.9; and Q4: 2019: 3.6, 2021: 5.8) (Fig. 2).
Fig. 2.
Weekly Visit Volume Mean, Standard Deviation, and Coefficient of Variation (CoV) by Quarter — National Syndromic Surveillance Program (NSSP)*, United States, December 30, 2018–March 27, 2022.
Abbreviations: ED = emergency department; NSSP = National Syndromic Surveillance Program; CoV = coefficient of variation.
* NSSP is a collaboration among CDC, local, and state health departments, and federal, academic, and private sector partners. To reduce artifactual impact from changes in reporting patterns, analyses were restricted to facilities with a coefficient of variation ≤40 and ≥ 75% complete information on race and ethnicity throughout 2019–2022. Visit data from 1595 facilities were included in this analysis. All facilities from Connecticut; District of Colombia; Georgia; Linn County, IA; Maryland; New Jersey; New York City; North Carolina; Ohio; Pennsylvania; San Mateo, CA; and Texas Region 6/5 were not included in this analysis because they did not meet the inclusion criteria. Coefficient of variation was calculated by dividing the mean weekly ED visit volume by the standard deviation for each quarter. Higher CoV corresponds to larger variation in weekly ED visit volumes.
4. Discussion
This analysis describes total and race, ethnicity, and age-specific changes in all-cause ED visit volumes throughout the COVID-19 pandemic, which have not been previously well described. Total ED visits dropped dramatically in Q2 2020 and remained >10% below the 2019 baseline until Q2 2021. At the beginning of the COVID-19 pandemic, during Q2 2020, all race, ethnicity and age groups experienced dramatic decreases in overall ED visits, mirroring the total ED visit trends. Adults of all race and ethnicity groups rebounded to at or above pre-pandemic levels while trends among children diverged and generally remained at or below the pre-pandemic baseline. For children aged <18 years, Q3 2021 was the only quarter where any race and ethnicity groups experienced an increase in overall ED visits since the beginning of the COVID-19 pandemic (Q2 2020). Specifically, during this time, Black or African American and Hispanic or Latino children experienced increased ED visits and Asian and Native Hawaiian or Other Pacific Islander children experienced increased overall ED visits compared to Q3 2019. The increases in pediatric ED visits during Q3 2021 mirrors increases in pediatric hospitalizations for COVID-19 observed when the Delta SARS-CoV-2 variant was the domain circulating variant [9].
Overall, the trends (decreased, stable, or increased) tended to be similar across race and ethnicity groups for each age group and quarter and the largest differences among groups in percent change of ED visits was among age groups rather than among race and ethnicity groups. For example, during Q2 2021, children from all race and ethnicity groups remained well below the 2019 baseline, while adults of all race and ethnicity groups were at or above baseline. While children had only one quarter during the COVID-19 pandemic with increased ED visits compared to 2019, adults from certain race and ethnicity groups had multiple quarters of increased ED visits compared to the 2019 baseline. Previous research suggests some parents were hesitant to seek emergency care for their children, especially early in the COVID-19 pandemic and that transmission of many pathogens, as measured by laboratory test percent positivity, was below pre-pandemic baseline levels [10,11]. While the trends in all-cause ED visits stratified by race and ethnicity were largely similar across race and ethnicity group, quantifying these stratified trends is important to understand overall changes in ED visits during the course of the pandemic. These all-cause trends stratified by race, ethnicity and age reported in this analysis can serve as the denominator when analyzing ED visits for specific conditions, and understanding how all-cause ED visits changed over the course of the pandemic provides important context when interpreting trends in ED visits for specific conditions during the course of the COVID-19 pandemic.
While ED visits may be stable or demonstrate minimal change across quarters, dramatic fluctuations in ED volume can be observed at the weekly level. It is important to monitor weekly percent or relative increases in addition to longer-term trends in ED volume because a rapid relative increase in all-cause ED visits can be an indication of an event of public health concern and may warrant further investigation. Additionally, race, ethnicity and age stratified trends in weekly percent change can be used to determine if specific population groups are being disproportionately affected. Overall, and race, ethnicity, and age-stratified ED trends and relative weekly increases are important tools in the ED surveillance toolkit to monitor for public health threats that may be disproportionately affecting specific population groups and could facilitate earlier investigation and response.
ED visit volumes were on the rise prior to the COVID-19 pandemic, with an estimated 136.9 million visits in 2015 to an estimated 145.6 million visits in 2016 [12]. While overall ED visit volumes were generally higher during 2019 than during many periods of the COVID-19 pandemic, the larger variability experienced at times during the pandemic made planning and resource allocation difficult. These increases in ED utilization over 2019 baselines, specifically the larger variation in overall weekly ED visit counts likely increased the burden on an already taxed system, and as EDs remain the primary portal of entry to healthcare for acute conditions such as myocardial infarction, stroke, and sepsis it is imperative that EDs remain staffed and able to provide adequate care to patients. These dramatic fluctuations in ED visit volumes make healthcare planning and resource allocation difficult to forecast. Seasonal fluctuations can be factored into the planning, but these extreme and unpredictable fluctuations cause unforeseen strains on the health care system. Hospital systems should consider analyzing fluctuations in ED utilization, and if these fluctuations in total ED visit volumes exceed the capacity of existing flexible staffing and resource models, hospital systems could evaluate and revise flexible plans to account for larger fluctuations, especially during times on increased community COVID-19 levels. Hospitals could also consider using ED and wastewater surveillance data to identify early increases in community COVID-19 levels that can be used for surge staff planning and resource allocation.
This analysis is subject to at least five limitations. First, although robust, NSSP ED visit data are a convenience sample and should not be considered nationally representative as this analysis represents data from 38 of 50 states. Also, the geographic variation in COVID-19 surges coupled with the fact that specific race and ethnicity groups may be over- or under- represented based on where specific race and ethnicity groups are more highly concentrated and align with EDs that are consistently reporting into NSSP may impact race and ethnicity specific variation in ED volumes. Second, NSSP data are at the ED visit level rather than the person level so if a single person visits an ED multiple times, each visit is counted. Increases in ED visits could be partially attributed to repeat visits by the same person, however, a single person visiting an ED multiple times still contribute to increased ED volume. Third, we only included one year of pre-pandemic data as the baseline and 2019 trends may not be representative of trends from prior years. Fourth, while we can comment on overall ED visit volumes by race, ethnicity, and age group from our data, we cannot comment on underlying motivations for why people sought care in EDs versus other care settings and therefore this study is not able to draw conclusions on why changes in ED volume were observed. Fifth, there is significant variability in how race and ethnicity data are collected at the facility level. There is a need for a more standardized approach for collecting race/ethnicity data, with the emphasis of self-identification rather than race/ethnicity being assigned by a health practitioner.
In conclusion, quantifying changes in all-cause ED visits overall and by demographic characteristics is useful to understand variation in emergency services care utilization, especially during a pandemic. Monitoring ED data by race, ethnicity and age group can be used to inform outreach efforts to the groups most impacted, ensuring that patients have access to appropriate levels of care and tools to help them determine the most appropriate care setting. Using ED data stratified by race, ethnicity and age for surveillance can facilitate rapid identification and response to public health threats that may be disproportionately affecting certain populations.
* To reduce artifactual impact from changes in reporting patterns, analyses were restricted to facilities with a coefficient of variation ≤40 and ≥ 75% complete information on race and ethnicity throughout 2019–2022. Visit data from 1595 facilities were included in this analysis. All facilities from Connecticut, District of Columbia, Georgia, Linn County, IA, Maryland, New Jersey, New York City, North Carolina, Ohio, Pennsylvania, San Mateo, CA, and Texas Region 6/5 were not included in this analysis because they did not meet the inclusion criteria.
Funding/Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Amanda R. Smith: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Formal analysis, Data curation, Conceptualization. Jourdan DeVies: Methodology, Formal analysis, Data curation. Kelly Carey: Writing – review & editing, Writing – original draft, Visualization, Methodology, Formal analysis, Data curation, Conceptualization. Michael Sheppard: Writing – review & editing, Methodology, Formal analysis. Lakshmi Radhakrishnan: Writing – review & editing, Methodology, Conceptualization. Rashid Njai: Writing – review & editing, Methodology. Umed A. Ajani: Writing – review & editing, Methodology. Karl Soetebier: Writing – review & editing, Methodology. Kathleen Hartnett: Writing – review & editing, Writing – original draft, Supervision, Methodology, Conceptualization. Jennifer Adjemian: Writing – review & editing, Supervision, Methodology, Conceptualization.
Declaration of Competing Interest
None.
Acknowledgements
Aaron Kite-Powell for guidance on analysis and proof-reading the manuscript and members of the NSSP Community of Practice who contributed expertise to development of the race and ethnicity categories.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajem.2023.04.005.
Appendix A. Supplementary data
Table A.1: Quarterly mean weekly ED visits and percent change in ED visits by age group, race, and ethnicity — National Syndromic Surveillance Program (NSSP)*, United States, December 30, 2018–April 2, 2022.
References
- 1.Hartnett K.P., Kite-Powell A., DeVies J., Coletta M.A., Boehmer T.K., Adjemian J., et al. Impact of the COVID-19 pandemic on emergency department visits — United States, January1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adjemian J., Hartnett K.P., Kite-Powell A., DeVies J., Azondekon R., Radhakrishnan L., et al. Update: COVID-19 pandemic–associated changes in emergency department visits — United States, December 2020–January 2021. MMWR Morb Mortal Wkly Rep. 2021;70:552–556. doi: 10.15585/mmwr.mm7015a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Venkatesh A.K., Janke A.T., Shu-Xia L., Rothenberg C., Goyal P., Terry A., et al. Emergency department utilization for emergency conditions during COVID-19. Ann Emerg Med. 2021 Jul;78(1):84–91. doi: 10.1016/j.annemergmed.2021.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hartnett K.P., Kite-Powell A., Patel M.T., Haag B.L., Sheppard M.J., Dias T.P., et al. Syndromic surveillance for E-cigarette, or vaping, product use-associated lung injury. N Engl J Med. 2020;382:766–772. doi: 10.1056/NEJMsr1915313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Radhakrishnan L., Stein Z., DeVies J., Smith A.R., Sheppard M.J., Hartnett K.P., et al. Syndromic surveillance of vaccine-associated adverse events in U.S. emergency departments. Vaccine. 2021;39(31):4250–4255. doi: 10.1016/j.vaccine.2021.06.030. [DOI] [PubMed] [Google Scholar]
- 6.National Syndromic Surveillance Program What is syndromic surveillance? 2023. https://www.cdc.gov/nssp/overview.html Accessed May 18, 2022.
- 7.National Syndromic Surveillance Program NSSP participation by U.S. County. 2023. https://www.cdc.gov/nssp/participation-coverage-map.html Accessed May 18, 2022.
- 8.Centers for Disease Control and Prevention MMWR week fact sheet. 2023. https://ndc.services.cdc.gov/wp-content/uploads/MMWR_Week_overview.pdf Available at: Accessed 5/23/2022.
- 9.Siegel D.A., Reses H.E., Cool A.J., Shapiro C.N., Hsu J., Boehmer T.K., et al. Trends in COVID-19 cases, emergency department visits, and hospital admissions among children and adolescents aged 0–17 years — United States, august 2020–august 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1249–1254. doi: 10.15585/mmwr.mm7036e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Macy M.L., Smith T.L., Cartland J., Golbeck E., Davis M.M. Parent-reported hesitancy to seek emergency care for children at the crest of the first wave of COVID-19 in Chicago. Acad Emerg Med. 2021;28(3):355–358. doi: 10.1111/acem.14214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodgers L., Sheppard M., Smith A., Dietz S., Jayanthi P., Yuan Y., et al. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin Infect Dis. 2021;73:S110–S117. doi: 10.1093/cid/ciab311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ACEPNow The latest emergency department utilization numbers are in. 2023. https://www.acepnow.com/article/the-latest-emergency-department-utilization-numbers-are-in/ Available at: Accessed May 18, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table A.1: Quarterly mean weekly ED visits and percent change in ED visits by age group, race, and ethnicity — National Syndromic Surveillance Program (NSSP)*, United States, December 30, 2018–April 2, 2022.