Abstract
Fingolimod-induced lymphopenia is a risk factor for severe monkeypox infection. As monkeypox was recently declared a Public Health Emergency of International Concern, vaccination should be evaluated in patients with MS before immunosuppressive treatment, particularly in patients receiving sphingosine-1-phosphate receptor modulators.1,2
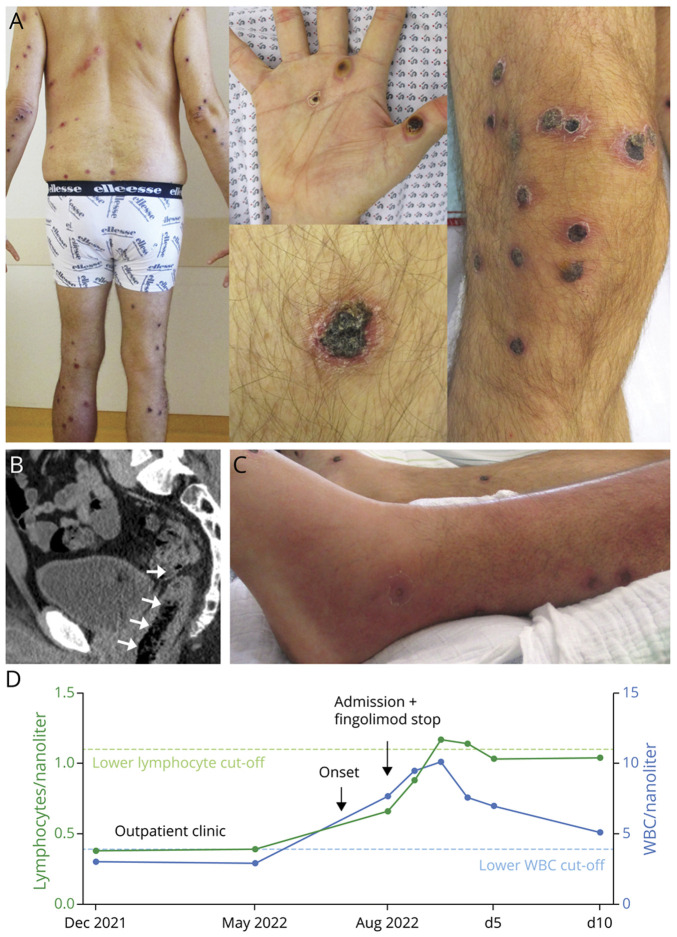
A 46-year old man with controlled relapsing-remitting multiple sclerosis (MS) and long-term fingolimod treatment developed multiple painful skin lesions (Figure, A). Outpatient skin swab revealed monkeypox virus infection. No fever was detected, but the disease course was complicated by prolonged cutaneous, oral and perianal manifestations, proctitis (Figure, B), gastrointestinal bleeding with the need for blood transfusions, lower leg phlegmon (Figure, C), lymphadenopathy, and hyperbilirubinemia. Furthermore, the patient presented acute urinary retention and hematuria.
Figure. Clinical Presentation and Laboratory Results of a MS Patient With Monkeypox.
(A) Monkeypox rash with approximately 180 skin lesions. (B) Abdominal CT reveals proctitis with perirectal fat stranding (arrows). (C) Bacterial superinfection manifested as lower leg phlegmon. (D) The patient presented preinfection lymphopenia and leucopenia. After symptom onset and fingolimod discontinuation, white blood cells (WBC) increased rapidly. d = day of hospitalization.
At admission, moderate lymphopenia (Figure, D) was detected and fingolimod was stopped. Six days after discontinuation, flow cytometry still revealed severe T-cell lymphopenia (0.67/nL, CD4+ 0.24/nL). Nevertheless, the patient improved with supportive treatment and was released 35 days after symptom onset.
Fingolimod-induced lymphopenia is a risk factor for severe monkeypox infection. As monkeypox was recently declared a Public Health Emergency of International Concern, vaccination should be evaluated in patients with MS before immunosuppressive treatment, particularly in patients receiving sphingosine-1-phosphate receptor modulators.1,2
Acknowledgment
L. Müller-Jensen dedicates this work to Prof. Dr. A. Müller-Jensen who has been an invaluable mentor and supporter.
Author Contributions
L. Müller-Jensen: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data; H. Kriedemann: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design, analysis or interpretation of data; K. Anvari: Major role in the acquisition of data; P. Huehnchen: Study concept or design; analysis or interpretation of data; V. Siffrin: Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data.
Study Funding
The authors report no targeted funding.
Disclosure
L. Müller-Jensen and P. Huehnchen are participants in the BIH Charité (Junior) Clinician Scientist Program funded by the Charité—Universitätsmedizin Berlin and the Berlin Institute of Health at Charité (BIH). Go to Neurology.org/N for full disclosures.
References
- 1.Adler H, Gould S, Hine P, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022, 22 (8):1153-1162. doi: 10.1016/s1473-3099(22)00228-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wenham C, Eccleston-Turner M. Monkeypox as a PHEIC: implications for global health governance. Lancet. 2022:S6736(22):1-3. doi: 10.1016/S0140-6736(22)01437-4 [DOI] [PMC free article] [PubMed] [Google Scholar]