Abstract
The use of an endovascular stent-graft prosthesis for the treatment of infrarenal abdominal aortic aneurysms is receiving increasing attention as an option that may avoid the significant morbidity and mortality associated with open surgical treatment. We studied the clinical effectiveness of stent-grafts in patients with infrarenal abdominal aortic aneurysms.
Between October 1995 and May 1998, 33 patients underwent infrarenal abdominal aortic aneurysm exclusion with a homemade polytetrafluoroethylene-covered stent, and between November 1998 and September 1999, 56 patients underwent abdominal aortic aneurysm exclusion with the Medtronic AneuRx stent-graft. Overall, these patients represented a high-risk surgical group. The technical success rate was 100% in both groups. No patient required immediate conversion to open repair. With the polytetrafluoroethy-lene-covered stent, the primary success rate was 33%, and the secondary success rate was 76%. In the AneuRx group, the primary success rate was 82.8%, and the secondary success rate was 85.3% at 6 months. There was no procedural or 1-month mortality or major morbidity in either group.
By showing that infrarenal abdominal aortic aneurysms can be treated safely and successfully with an endoluminal stent-graft, our early results provide additional support for the endovascular treatment of abdominal aortic aneurysms. Further follow-up studies will determine the long-term ability of such treatment to prevent aneurysmal rupture and death.
Key words: Aortic aneurysm, abdominal; blood vessel prosthesis implantation; clinical trials, phase III; prosthesis design; stents; treatment outcome
Abdominal aortic aneurysm (AAA) is a serious vascular disorder in which the abdominal aorta becomes permanently dilatated to at least 50% greater than its normal diameter. 1,2 In the last 30 years, the incidence of AAA has increased threefold. 2–4 The prevalence of these aneurysms in men over age 65 ranges from 4.3% to 8.8%. 4 Approximately 50% of patients with AAA who do not undergo corrective surgery die of ruptured aneurysm. 4
Repair of AAA is indicated at a diameter of 5 cm, 2,4 which is generally accepted as the size at which the risk of rupture exceeds that of open surgical repair. Out-of-hospital rupture of AAA carries a 90% mortality rate; this decreases to 50% for patients who are able to undergo emergency repair. 2 To prevent this devastating event, over 40,000 “prerupture” surgical repairs of AAAs are currently performed in the United States each year. 2 Although highly effective in preventing such rupture, open surgical repair is associated with mortality rates of 2% to 8% (average, 4%). 1,2,4 Because of the high prevalence of comorbid medical conditions in these patients, the morbidity rates are as high as 30%. 5 Surgical complications include myocardial infarction, ischemia, arrhythmia, congestive heart failure, pulmonary insufficiency, renal impairment, bleeding (requiring transfusion), distal thromboembolism, and wound infection.
Because endovascular stent-grafting is a minimally invasive procedure and therefore avoids these risks, it has gained increasing popularity with both physicians and patients. Advantages of endovascular stent-graft techniques for the repair of AAAs include reduction in complications, pain, hospitalization, and recovery time. 5–7 Stent-graft treatment of AAAs has evolved rapidly since it was 1st used for endovascular exclusion of an infrarenal AAA by Parodi and associates 3 in 1990. Although the technology is still in its infancy, substantial improvements have recently been made in the design and delivery of endovascular stent-grafts.
This study presents our initial experience with stent-graft exclusion in patients who underwent endovascular treatment of infrarenal AAAs at the Texas Heart Institute (THI). Between October 1995 and May 1998, 33 patients underwent infrarenal AAA exclusion with a homemade polytetrafluoroethylene (PTFE)-covered stent, and between November 1998 and September 1999, 56 patients underwent AAA exclusion with the Medtronic AneuRx stent-graft (Medtronic AVE; Santa Rosa, Calif).
Materials and Methods
PTFE-Covered Stent Protocol
Patients. The series included 33 patients (27 men and 6 women) who underwent infrarenal abdominal aortic aneurysm exclusion procedures between October 1995 and May 1998. Six patients required a repeat procedure, resulting in a total of 39 stent implantations. The patients' average age was 73 years. Twenty-six patients (78.8%) had concomitant coronary artery disease, and 21 (63.6%) had a history of smoking. Table I lists additional patient characteristics. All patients had multiple risk factors for open aneurysm repair. Fifteen of the patients were excluded from another ongoing protocol, using the Corvita stent-graft, because of tortuous, stenotic peripheral vessels; 3 patients were excluded from the Corvita protocol because of a serious underlying disease (malignancy or renal failure). Each patient gave informed consent for the study, which was approved by our Institutional Review Board.
Table I. Clinical Characteristics of the 33 Patients in the PTFE-Covered Stent Protocol

Aneurysms. As documented by preoperative contrast-enhanced computed tomographic (CT) scanning, the aneurysms included type I lesions (43%), type II lesions (27%), and type III lesions (30%). 8 The proximal neck of the aneurysm measured at least 1.5 cm in length. Aneurysms in which the non-aneurysmal aorta above the iliac bifurcation measured ≥10mm were repaired with a tubular graft, while those that extended to the iliac arteries (types IIa and IIb) were repaired with an aortoiliac graft.
Stent-Graft Device. Repair was accomplished with an aortic tubular stent-graft (27 lesions), an aortobi-iliac stent graft (9 lesions), or an aorto-mono-iliac stent-graft with exclusion of the contralateral limb and femoro-femoral artery bypass (3 lesions). At the time of the procedure, the stent-graft was prepared from commercially available products approved for intravascular use. These products included a stent (Wallstent®; Boston Scientific Corp.; Natick, Mass) and a thin-walled 8-mm PTFE vascular graft (Gore-Tex®; W.L. Gore & Associates, Inc.; Flagstaff, Ariz). After being cut to the desired length, the graft was predilated with a commercially available peripheral angioplasty balloon. An appropriately sized Wallstent was partially exposed on a delivery device (Unistep Plus Delivery System; Boston Scientific) by retracting the protective sheath. The stent measured either 22 or 24 mm in diameter and either 45 or 70 mm in length. The predilated graft was placed around the stent and affixed to its proximal and distal ends with 6-0 polypropylene (Prolene) sutures. The composite device was then constrained within a 14-F to 16-F Peel-Away® sheath (Cook, Inc.; Bloomington, Ind).
Endovascular Treatment Procedure. Patients were brought to the cardiac catheterization laboratory in a fasting state. Heparin was administered intravenously in an initial dose of 70 mg/kg and thereafter as needed to achieve an activated clotting time (ACT) of about 250 seconds. Lidocaine was infiltrated into the femoral area, and the femoral artery was cannulated with a 6-F sheath by means of the Seldinger technique. A PIG-GSE catheter with calibrated radio-paque markers (Cook) was inserted, and abdominal angiography was performed. A 0.035-inch Amplatz Super Stiff™ Guidewire (Boston Scientific) was advanced through the sheath to the aorta. Depending on the size of the aorta, a 40-cm-long 14-F to 16-F homeostatic sheath (Cook) was percutaneously exchanged with the 6-F sheath. A mono-iliac approach was used for tubular stent-grafts, and a bi-iliac approach was used for mono- and bi-iliac stent-graft treatment.
If the aneurysm was excessively tortuous, a bare stent was inserted to help straighten the aorta and enable better attachment and less bending of the stent-graft; otherwise, the stent-graft was deployed directly. It was advanced to the target site under fluoroscopic control, and the peel-away sheath was retracted to expose the graft, which immediately assumed its predetermined dimension. The graft was then postdilated throughout its length with an appropriate-size angioplasty balloon. If the distal aneurysm was within 1 cm of the iliac bifurcation, 1 or both iliac arteries were used for stent fixation, with an aorto-mono-iliac or bi-iliac graft. If the stent extended into 1 iliac artery and the contralateral iliac artery was excluded, the procedure was followed by an elective femorofemoral bypass. At the end of each procedure, angiography was performed to confirm that the aneurysm had been excluded from the circulation (Fig. 1). Sheaths were removed when the ACT was <150 seconds, and pressure was applied using the FemoStop device (Radi Medical Systems AB; Uppsala, Sweden) over the femoral arteries to achieve hemostasis.

Fig. 1 A) Angiogram shows an infrarenal abdominal aortic aneurysm. B) Aortic angiogram obtained after placement of a Wallstent®-PTFE stent-graft (arrow). There is no evidence of an endoleak.
Follow-Up Protocol. Postoperatively, patients were scheduled to undergo follow-up contrast-enhanced CT at 4 weeks, 3 months, 6 months, 1 year, and annually thereafter unless clinically contraindicated. If necessary, enhanced CT and duplex ultrasonography were performed at more frequent intervals. The CT scan was used to assess the size of the aneurysms and to detect contrast extravasation (endoleak) into the aneurysmal sac. Endoleak was classified as minor if the contrast agent was localized to some portion of the sac and major if it obliterated the whole sac.
AneuRx Protocol
Study Design and Patient Population. This ongoing, prospective, sequential-enrollment study of the AneuRx stent-graft in the treatment of infrarenal AAAs was part of the phase III clinical trial of this device. Our Institutional Review Board approved the study protocol as defined by Food and Drug Administration (FDA) regulations. We began enrolling patients in November 1998. All enrollees provided written informed consent.
Between November 1998 and September 1999, 56 patients underwent AAA exclusion with the AneuRx stent-graft. This group included 49 men (87.5%) and 7 women (12.5%) whose ages ranged from 56 to 88 years (mean, 71.2 years). These patients had multiple significant comorbidities (Table II) and overall represented a high-risk group. In 78.6% of the cases, the American Society of Anesthesiologists (ASA) operative risk classification was grade IV or higher. 9 Twenty-four of the patients (42.9%) had a history of myocardial infarction, 17 (30.4%) had congestive heart failure, and 34 (60.7%) had a history of coronary revascularization. Twenty-two patients (39.3%) had chronic obstructive pulmonary disease (COPD), and 16 (28.6%) had a “hostile” abdomen because of previous abdominal surgery in the area of the aneurysm.
Table II. Comorbid Conditions of the 56 Patients in the AneuRx Protocol

Patients had to be willing to undergo follow-up examination at 1, 6, and 12 months and yearly thereafter. If they met these criteria, they were allowed into the study despite the following conditions: acute renal failure or need for chronic dialysis; previous abdominal surgery; aortic dissection; contained, controlled, ruptured aneurysms; life expectancy <1 year; pseudoaneurysm from previous surgical grafting; and smaller aneurysms that required treatment before proceeding to another treatment for comorbidities.
Exclusion criteria included age under 18 years; an acutely ruptured aneurysm; pregnant or nursing status; suprarenal, iliofemoral, or inflammatory aneurysms; connective tissue disease; hypercoagulability; active systemic infection; morbid obesity that impaired visualization of the aorta on X-ray film; inability to give informed consent; and inability to return for follow-up visits.
Before entering the study, each patient had a complete history and physical examination. Diagnostic imaging with contrast CT and angiography with a calibrated pigtail catheter (Cook) were performed to characterize the aneurysm and iliac vessels, and to ensure that each patient met the study qualifications.
Aneurysms. Candidates for the study had nonruptured infrarenal AAAs that exhibited 1 of the following characteristics: 1) a diameter of >5 cm; 2) a diameter of 4.5 to 5.0 cm, with an increase of at least 0.5 cm during the preceding 6 months; 3) a diameter twice that of the normal infrarenal aorta; or 4) a saccular shape. Additional requirements included a minimal neck, comprising a 1-cm length of non-aneurysmal aorta, measuring 18 to 25 mm in diameter and located immediately inferior to the most inferior major renal artery. The average AAA diameter was 53.8 mm (range, 30 to 85 mm). The iliac arteries were required to have a luminal caliber large enough to accommodate a 21-F delivery catheter on 1 side, a 16-F sheath on the other side, and a maximal distal diameter of 16 mm.
Stent-Graft Device. The Medtronic AneuRx stent-graft is a modular, bifurcated system designed to isolate an aneurysm from blood flow (Fig. 2). The outside of the graft is fully stented, with self-expanding nickel-titanium (nitinol) stent rings. The graft is made of thin-walled, noncrimped, woven polyester and is sutured to the nitinol stent. The basic device consists of a bifurcated main segment and a contralateral iliac segment. Additional modular components include aortic and iliac extender cuffs. The stent-graft is implanted transluminally in the aorto-iliac position via a retrograde approach from the femoral arteries, using AneuRx delivery catheters: a low-profile 21-F catheter for the main segment, and a 16-F catheter for the iliac segment. The aortic neck of the bifurcated stent-graft ranges from 20 to 28 mm in diameter. The main segment of the stent-graft has a proximal aortic cuff that secures the device in place with a frictional seal. The straight iliac limb ranges from 12 to 16 mm in diameter. Its length can be adjusted with proximal and distal extender cuffs.
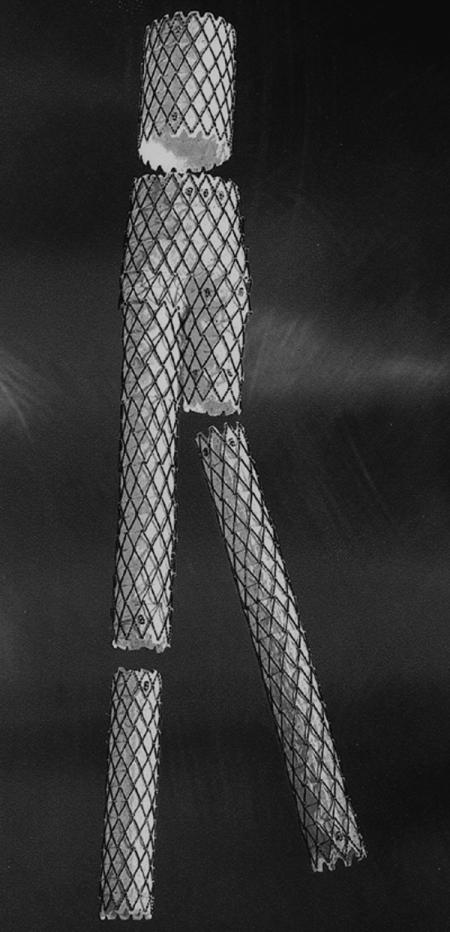
Fig. 2 The AneuRx stent-graft. The primary modular components are the main bifurcated segment and the contralateral iliac limb. Modular proximal (aortic) and distal (iliac) extender cuffs enable adjustment of the length.
Endovascular Treatment Procedure. On the basis of diagnostic imaging, an endovascular stent-graft of the appropriate size and configuration was selected. We oversized the aortic and iliac stent graft diameters by 10% to 20% over what was measured by CT and angiography. The procedures were performed in a catheterization laboratory modified for peripheral endovascular imaging and interventional procedures. All patients underwent general anesthesia. Heparin was administered intravenously in a 70-mg/kg dose and thereafter as needed to achieve an ACT of about 250 seconds. Access for the 21-F delivery system involved surgical exposure of the femoral artery. Contralateral femoral artery access for the 16-F iliac limb device was obtained percutaneously, followed by percutaneous closure in the majority of cases with the Prostar XL Percutaneous Vascular Surgery Device (Perclose, Inc.; Menlo Park, Calif). Interventional cardiologists inserted the AneuRx stent-graft, and vascular surgeons performed the arteriotomies. Intraoperative imaging was performed with digital subtraction angiography.
Patients remained hospitalized overnight for observation and were discharged the following day, as deemed appropriate by their physician. All patients underwent abdominal radiography and physical examination before hospital discharge.
Follow-up Protocol. Follow-up evaluation was based on the results of postprocedure angiography. If no endovascular leak was present on the final postprocedure angiogram, the patient was discharged and returned for follow-up examination at 1 month. If the patient was asymptomatic at 1 month, abdominal radiography, abdominal, and peripheral ultrasonography were done to evaluate stent-graft patency and to detect migration or endoleak. If symptoms were present at 1 month, an abdominal CT scan was performed. If no endoleak was detected, the patient was scheduled for follow-up visits at 6 months, at 12 months, and annually thereafter.
If an endoleak was noted on the patient's final postprocedure angiogram, a predischarge CT scan was performed. If the endoleak sealed before hospital discharge, the follow-up schedule was the same as stated above. If persistent endoleak was present, the patient returned for another CT scan 2 weeks after hospital discharge. The leaks were treated as deemed necessary at each follow-up interval. If a leak was present on the 2-week CT scan, subsequent scans were obtained 1 month and 3 months later. Thereafter, the patient underwent follow-up study at 3-month intervals until either the endoleak sealed or alternative treatment was performed. Leakage was classified as minor if the contrast agent was localized to some portion of the sac and major if it obliterated the whole sac.
Results
PTFE-Covered Stent Protocol
The average procedure time was 299 + 72 minutes, the fluoroscopy time was 133.5 + 95.7 minutes, and the hospitalization time was 3.7 + 3.3 days. The average number of stent-grafts per procedure was 1.5 + 0.6. The immediate procedural success rate was 100%, and there were no in-hospital deaths.
The patients were followed up for a mean of 13 + 5.8 months. Eleven patients had no leakage (primary success rate 33%). Of the remaining 22 patients, 3 had major endovascular leaks, and 19 had minor leaks. Six patients, including 2 who had large leaks, were treated by means of repeat endoluminal exclusion; this was successful in 4 cases. One repeat exclusion was done in combination with coil embolization of the aneurysmal sac. One patient in whom a repeat percutaneous intervention failed and another patient who had a large aneurysm and a major leak were treated by means of an open surgical procedure. In 8 patients, the leak resolved spontaneously. When the cases involving reintervention and spontaneous closure were included, the secondary success rate was 76%. The remaining patients continue to have minor leakage and are being closely observed.
Other minor complications included femoral artery pseudoaneurysm formation (6 patients) and bleeding from the entry site that required transfusion of more than 2 units of packed red blood cells (3 patients). Table III shows the aneurysm sizes at baseline and at 3-month postoperative follow-up examination.
Table III. Maximal Aneurysm Diameter in Patients Treated with PTFE-Covered Stents

AneuRx Protocol
Results of the Primary Procedure. One-month follow-up information is available for all 56 patients, and 6-month information is available for 34 patients. Table IV presents the results of the primary procedure. The AneuRx stent-graft was deployed successfully in all 56 patients (Fig. 3); no patient required conversion to an open surgical repair. Before the procedure, 25 patients required iliac angioplasty to facilitate passage of the 21-F delivery device. After deployment of the device, 33 patients required low-pressure angioplasty of the AneuRx stent-graft to fully oppose the graft to the vessel wall. In 43 patients, the Prostar XL device was used for successful percutaneous closure of the femoral artery through which the 16-F iliac-limb device had been delivered; 3 patients had both femoral arteries closed percutaneously with the ProStar XL device. Blood loss averaged 428 mL per patient; 7 patients required packed red blood cell transfusions (total, 18 units). The average hospital stay was 2.3 days (range, 1 to 8 days).
Table IV. AneuRx Protocol: Results of the Primary Stent-Graft Procedure in 56 Patients


Fig. 3 A) Aortic angiogram from a 70-year-old man shows a 45-mm infrarenal abdominal aortic aneurysm. B) Three-dimensional reconstruction of a contrast-enhanced, spiral computed tomographic (CT) scan of the patient's abdominal aorta, showing the aneurysm. C) Aortic angiogram obtained immediately after placement of an AneuRx stent-graft in this patient. There is no evidence of an endoleak. D) Three-dimensional reconstruction of a contrast-enhanced, spiral CT scan of the abdominal aorta at 6-month follow-up examination. There is no evidence of an endoleak.
Adverse Procedural Events. No periprocedural deaths or major morbidity occurred. Two patients had iliac artery dissection related to the 21-F delivery device: 1 dissection required an iliac stent, and the other dissection was repaired at the time of surgical closure. Two other patients had thrombotic occlusion of the iliac artery, which required thrombectomy; at 1- and 6-month follow-up examination, these patients showed no evidence of limb ischemia. No embolic complications were observed.
Endoleak Rates. Ten patients (17.9%) had endo-leaks at hospital discharge, as documented by contrast CT or angiography. At 1 month, only 3 (5.4%) of 56 patients had persistent endoleaks, and no new endoleaks were seen; therefore, 7 of the 10 endoleaks present at discharge sealed spontaneously. Of the remaining 3 patients, none has had enlargement of his or her aneurysm. Of the 34 patients for whom 6-month follow-up information was available, 5 (14.7%) had endoleaks—2 new leaks in addition to the 3 mentioned above (Table V).
Table V. Types of Endoleak in Patients with AneuRx Stent-Grafts

Secondary Procedures for Endoleaks. The endoleak classification system developed by White and colleagues 10 is shown in Table VI. Two patients required proximal extender cuffs at the proximal aortic attachment site at the time of the procedure for type I endoleaks. At 1 month, neither of these patients had a persistent endoleak.
Table VI. Classification of Endoleaks 10

Of the 3 patients who had persistent endoleaks at 1 month, 1 patient required 2 coil embolization procedures for moderate type II endoleaks; the 1st procedure was performed at 1 month for inferior mesenteric artery branch collateral backflow, and the 2nd procedure was performed at 6 months for internal iliac branch collateral backflow. Despite the persistent endoleak, this patient's aneurysm has not grown; it had measured 49 mm initially and had decreased to 47 mm at 6 months. The other 2 patients who had persistent endoleaks at 1 month have not required treatment. Both endoleaks were minimal on CT, and both aneurysms have actually decreased in diameter—1 from 58 to 55 mm and the other from 45 to 40 mm.
The 2 patients in whom new endoleaks were detected at 6 months had not had postprocedural or 1-month endoleaks. The new endoleaks were categorized as type II, due to collateral back flow, and were minimal on CT. Neither aneurysm has subsequently increased in diameter or required treatment.
Mortality and Morbidity. During the first 6 months, there was no mortality. One 86-year-old patient, who had chronic lymphocytic leukemia, died of an unrelated illness after undergoing 6-month follow-up examination. One 70-year-old patient with severe COPD and ASA grade V operative risk was hospitalized with respiratory failure and had a cerebrovascular accident and multi-organ failure soon after 3-month follow-up evaluation. A CT scan showed the stent-graft to be patent, with no migration or endoleak. This patient died soon after the 6-month follow-up time period.
There has been no major morbidity at 1 month. Three patients developed localized groin infections at the surgical cut-down site and required antibiotics. Three patients had mild postprocedural hematomas that resolved with conservative therapy. No patient developed a femoral artery pseudoaneurysm or fistula. Three patients had mild hematuria, and 1 patient had a lower urinary tract infection that required antibiotics. At 1 and 6 months, no patients had stent migration or occlusion.
Discussion
In the last decade, no area of treatment of peripheral vascular disease has generated more enthusiasm than has the endovascular exclusion of AAAs. This procedure has captured the interest of vascular surgeons, interventional radiologists, and interventional cardiologists alike. Whereas vascular grafting had previously been the domain of the vascular surgeon, more recent developments in transcatheter delivery of vascular prostheses has allowed non-surgical specialists to use these devices for treatment of a variety of vascular defects. The 1st endoluminal treatment of AAAs in a clinical setting was performed in 1990 and reported by Parodi in 1991. 3 Since then, over 3,000 endoluminal AAA repairs have been performed worldwide with various devices.
It is hoped that endoluminal grafts will help decrease the morbidity and mortality associated with AAA repair, particularly in patients who have comorbid illnesses. Initially, these devices were used only in patients with significant comorbid diseases who were thought to be too high risk or who were denied open surgical repair. Since Parodi's initial report, numerous studies have shown that endovascular treatment of AAAs can be performed safely, resulting in lower morbidity and equal or lower mortality rates than those reported for open surgical repair. 5–7 Because of these early results, the use of endovascular devices for treatment of AAAs has been proposed for patients who do not have comorbid illnesses. The major factor limiting widespread use for endovascular stents is the lack of long-term follow-up data on patients treated with these devices, especially the 2nd generation devices. A limited number of studies with 2- to 3-year follow-up have shown no significant difference in mortality between open surgical repair and endovascular exclusion. 5,7,11
Our early results are consistent with prior studies showing low morbidity and mortality for patients who have undergone endoluminal stent-graft exclusion of AAA. 5,6,11–13 Prior to the availability of 2nd generation devices such as the AneuRx device, we primarily used the homemade PTFE-covered Wallstent. We found this device very useful in patients who had narrow or tortuous iliac arteries because the introducer sheaths for these non-bifurcated stent-grafts were only 14 F to 16 F. The few major complications seen in the series of patients treated with the PTFE-covered Wallstents involved the need for conversion to a surgical procedure (2 patients), the need for blood transfusion (3 patients), and local complications at the percutaneous entry site (6 patients). The most frequent problem was endoleak, which was detected in 22 patients (67%), 3 of the leaks being considered major. Eight of the endoleaks sealed spontaneously. In other series, leakage has been observed in 9% to 44% of patients after endovascular repair. 6,11–14
Seven of our patients who had received the PTFE-covered Wallstents required reintervention for leaks, and 2 of these reinterventions consisted of open surgical procedures. The other 5 were endovascular procedures. No aneurysm rupture or death has occurred.
Local groin complications, such as pseudoaneurysm formation and hematomas, are recognized complications of percutaneous femoral procedures. Pseudoaneurysms developed in 6 (15%) of these procedures. In our experience, use of the FemoStop device to achieve hemostasis may be associated with a higher incidence of this complication.
Because stent-graft implantation with the homemade PTFE-covered Wallstent can be performed percutaneously and requires only local anesthesia, it results in less morbidity and a shorter hospital stay than open aneurysm repair. In our series, the average hospital stay was 3.7 + 3.3 days.
In our study, the maximal aneurysm diameter had increased slightly at 3 months both in the group with leakage and the group without leakage, and there was no significant difference between the 2 groups. In the studies by Malina and colleagues, 15 and by May and associates, 16 the average size of the aneurysms without leaks had decreased at 6- and 12-month follow-up examination, while the size of the aneurysms with leaks had increased. In order for such a change in size to be seen, the observation period may need to be longer than ours. The increase that we observed in aneurysm diameter in patients who were treated with the PTFE-covered Wallstent argues against its routine use for AAA exclusion.
The introduction of 2nd generation devices has practically eliminated the need for homemade devices. The AneuRx device and the Ancure® device (Guidant; Indianapolis, Ind) are the only devices currently approved by the FDA for AAA exclusion.
As mentioned above, our early results with the AneuRx device compare favorably with those reported by other groups using 2nd generation devices. Our 1-month endoleak rate of 5.4% compares very favorably with the 9% to 44% rates reported for a variety of endovascular stent-grafts. 6,7,17–22 However, our follow-up interval is too short to provide a reliable assessment of the true long-term endoleak rate or outcome.
Although 5 of our patients had endoleaks at 6 months, only 1 required treatment, and none had an increased aneurysm size. This lack of aneurysm expansion correlates well with CT characterization of these endoleaks as minimal. What to do about minimal endoleaks that are not causing aneurysm expansion is unclear. Close observation is usually sufficient, because the leaks will frequently close spontaneously. Current experience supports aggressive treatment of endoleaks that are moderate to severe or that result in aneurysm expansion, because this increases the risk of late rupture. 15,23,24 Endovascular treatment should be attempted 1st, followed by open repair if the former strategy is unsuccessful.
Most endoleaks in our patients were type IV (due to transgraft flow), 10 and occurred at stent-graft implantation (Table V). By 1 month, the majority (7 of 10; 70%) had closed spontaneously. Transgraft flow, caused by the high porosity of the thin-walled Dacron or polyester graft material, has been previously documented as a transient phenomenon that terminates spontaneously. 6,12 Patients who develop these endoleaks still need to be monitored closely, because it is often difficult to distinguish a type IV from a type III endoleak (which involves a defect in the graft fabric or between the segments of a modular, multisegmental graft). Only 1 of our patients required treatment after discharge for a persistent endoleak. This patient had a type II endoleak that involved collateral backflow from a branch of the inferior mesenteric artery and a branch of the external iliac artery. Both collateral vessels were closed successfully by means of coil embolization.
To date, none of our patients has required open surgical repair. The most likely reasons for this are careful selection of patients whose aneurysm dimensions are amenable to endovascular repair, and aggressive use of iliac angioplasty to facilitate delivery of the stent-graft. This result is very encouraging, because most reports cite a surgical conversion rate of 2% to 20%. 7,11,13,25,26
Thus far, we have noted no stent migration or displacement, but our short follow-up period has not allowed adequate time for full postexclusion aneurysm morphologic changes to occur. 14 The longitudinal columnar support and flexible endograft structure provided by the AneuRx stent-graft should be able to accommodate the morphologic changes that the excluded aneurysm may undergo over time.
The 3 patients who had localized groin infections at the surgical cut-down site were morbidly obese. Since treating these cases, we have changed our preoperative scrub regimen to include chlorhexidine gluconate (Hibiclens) and povidine-iodine (Betadine). We have been giving all patients oral antibiotics for 3 days after the procedure.
Because of the number of groin complications noted with the homemade PTFE-covered Wallstent, we initially decided to access and close the 16-F and 21-F access sites surgically. Because of the above-mentioned groin infections, however, we have been accessing and closing the 16-F access site percutaneously. We were able to close the 16-F femoral artery access site percutaneously in 43 of the 56 patients with a 10-F Prostar XL percutaneous vascular surgery device. We were also able to close the 21-F access site in 3 patients using 2 Prostar XL devices (10 F and 8 F, respectively) as described by Haas. 27 We hope that with improved endovascular devices the entire procedure will be performed percutaneously, eliminating the need for open surgical exposure of the femoral arteries.
In conclusion, our early results compare favorably with those reported in previous series of endovascular stent-graft repair of infrarenal AAAs. The procedure can be performed safely, with low morbidity and mortality. It results in a shorter hospital stay and less use of blood product than open surgical repair. To date, there are no reliable long-term follow-up data concerning the durability and efficacy of the endovascular stent-graft procedure in the prevention of rupture and death in patients who have AAAs. Nevertheless, design of endovascular stent-grafts continues to progress, and this less invasive procedure should soon gain widespread acceptance as an alternative treatment for selected infrarenal AAAs, especially in patients at high risk for open surgical repair.
Footnotes
Address for reprints: Zvonimir Krajcer, MD, 6624 Fannin Street, Suite 2780, Houston, TX 77030
References
- 1.van der Vliet JA, Boll AP. Abdominal aortic aneurysm. Lancet 1997;349:863–6. [DOI] [PubMed]
- 2.Ernst CB. Abdominal aortic aneurysm. N Engl J Med 1993;328:1167–72. [DOI] [PubMed]
- 3.Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg 1991;5:491–9. [DOI] [PubMed]
- 4.Zarins CK, Harris EJ Jr. Operative repair for aortic aneurysms: the gold standard. J Endovasc Surg 1997;4:232–41. [DOI] [PubMed]
- 5.Zarins CK, White RA, Schwarten D, Kinney E, Diethrich EB, Hodgson KJ, et al. AneuRx stent graft versus open surgical repair of abdominal aortic aneurysms: multicenter prospective clinical trial. J Vasc Surg 1999;29:292–308. [DOI] [PubMed]
- 6.Blum U, Voshage G, Lammer J, Beyersdorf F, Tollner D, Kretschmer G, et al. Endoluminal stent-grafts for infrarenal abdominal aortic aneurysms. N Engl J Med 1997; 336:13–20. [DOI] [PubMed]
- 7.White GH, Yu W, May J, Waugh R, Chaufour X, Harris JP, et al. Three-year experience with the White-Yu Endo-vascular GAD Graft for transluminal repair of aortic and iliac aneurysms. J Endovasc Surg 1997;4:124–36. [DOI] [PubMed]
- 8.Schumacher H, Eckstein HH, Kallinowski F, Allenberg JR. Morphometry and classification in abdominal aortic aneurysms: patient selection for endovascular and open surgery. J Endovasc Surg 1997;4:39–44. [DOI] [PubMed]
- 9.American Society of Anesthesiologists (ASA) Physical Status Classification. In: Schwartz SI, Shires GT, Spencer FC, Daly JM, Fischer JE, Galloway AC, editors. Principles of Surgery. 7th Edition. New York: McGraw-Hill, 1999: 1705.
- 10.White GH, May J, Waugh RC, Chaufour X, Yu W. Type III and type IV endoleak: toward a complete definition of blood flow in the sac after endoluminal AAA repair. J Endovasc Surg 1998;5:305–9. [DOI] [PubMed]
- 11.May J, White GH, Yu W, Ly CN, Waugh R, Stephen MS, et al. Concurrent comparison of endoluminal versus open repair in the treatment of abdominal aortic aneurysms: analysis of 303 patients by life table method. J Vasc Surg 1998;27:213–21. [DOI] [PubMed]
- 12.White GH, Yu W, May J, Chaufour X, Stephen MS. Endo-leak as a complication of endoluminal grafting of abdominal aortic aneurysms: classification, incidence, diagnosis, and management. J Endovasc Surg 1997;4:152–68. [DOI] [PubMed]
- 13.Parodi JC, Barone A, Piraino R, Schonholz C. Endovascular treatment of abdominal aortic aneurysms: lessons learned. J Endovasc Surg 1997;4:102–10. [DOI] [PubMed]
- 14.White RA, Donayre CE, Walot I, Kopchok GE, Wilson E Heilbron M, et al. Modular bifurcation endoprosthesis for treatment of abdominal aortic aneurysms. Ann Surg 1997; 226:381–91. [DOI] [PMC free article] [PubMed]
- 15.Malina M, Ivancev K, Chuter TA, Lindh M, Lanne T, Lindblad B, et al. Changing aneurysmal morphology after endovascular grafting: relation to leakage or persistent perfusion. J Endovasc Surg 1997;4:23–30. [DOI] [PubMed]
- 16.May J, White G, Yu W, Waugh R, Stephen M, Harris J. A prospective study of anatomico-pathological changes in abdominal aortic aneurysms following endoluminal repair: is the aneurysmal process reversed? Eur J Vasc Endovasc Surg 1996;12:11–7. [DOI] [PubMed]
- 17.Chuter TA, Wendt G, Hopkinson BR, Scott RA, Risberg B, Walker PJ, et al. Transfemoral insertion of a bifurcated endovascular graft for aortic aneurysm repair: the first 22 patients. Cardiovasc Surg 1995;3:121–8. [DOI] [PubMed]
- 18.Mialhe C, Amicabile C, Becquemin JP. Endovascular treatment of infrarenal abdominal aortic aneurysms by the Stentor system: preliminary results in 79 cases. Stentor Retrospective Study Group. J Vasc Surg 1997;26:199–209. [DOI] [PubMed]
- 19.Parodi JC. Endovascular repair of abdominal aortic aneurysms and other arterial lesions. J Vasc Surg 1995;21:549–57. [DOI] [PubMed]
- 20.Blum U, Voshage G, Beyersdorf F, Tollner D, Spillner G, Morgenroth A, et al. Two-center German experience with aortic endografting. J Endovasc Surg 1997;4:137–46. [DOI] [PubMed]
- 21.Chuter TA, Risberg B, Hopkinson BR, Wendt G, Scott RA, Walker PJ, et al. Clinical experience with a bifurcated endovascular graft for abdominal aortic aneurysm repair. J Vasc Surg 1996;24:655–66. [DOI] [PubMed]
- 22.Kretschmer G, Holzenbein T, Lammer J, Thurnher S, Minar E, Polterauer P. The first 15 months of transluminal abdominal aortic aneurysm management: a single centre experience. Eur J Vasc Endovasc Surg 1997;14:24–32. [DOI] [PubMed]
- 23.Matsumura JS, Moore WS. Clinical consequences of periprosthetic leak after endovascular repair of abdominal aortic aneurysm. Endovascular Technologies Investigators. J Vasc Surg 1998;27:606–13. [DOI] [PubMed]
- 24.Gorich J, Rilinger N, Soldner J, Kramer S, Orend KH, Schutz A, et al. Endovascular repair of aortic aneurysms: treatment of complications. J Endovasc Surg 1999;6:136–46. [DOI] [PubMed]
- 25.Allen RC, Zarins CK, Fogarty TJ. The Medtronic-AneuRx modular bifurcated graft. In: Yao JST, Pearce WH, editors. Techniques in vascular and endovascular surgery. Stamford, Conn: Appleton and Lange, 1998:401–9.
- 26.May J, White GH, Yu W, Waugh R, Stephen M, Sieunarine K, et al. Conversion from endoluminal to open repair of abdominal aortic aneurysms: a hazardous procedure. Eur J Vasc Endovasc Surg 1997;14:4–11. [DOI] [PubMed]
- 27.Haas P, Krajcer Z, Diethrich EB. Closure of large percutaneous access sites using the Prostar XL Percutaneous Vascular Surgery device. J Endovasc Surg 1999;6:168–70. [DOI] [PubMed]


