Abstract
Positive psychological interventions (PPIs), programs that specifically target positive emotions, cognitions, and behaviors, have been shown to reduce depression and improve other aspects of psychological well-being. However, potential pathways linking PPIs to better outcomes have been under-explored. In this paper, we report the results of a randomized trial of a self-guided online delivered PPI called MARIGOLD (Mobile Affect Regulation Intervention with the Goal of Lowering Depression). Participants with elevated depression were randomized to receive MARIGOLD (n = 539) or an emotion reporting control condition (n = 63). In addition to testing direct effects of the intervention on depressive symptoms, we explored whether positive or negative emotion—operationalized as past day, past week, reactivity, or flexibility—mediated the intervention impact on depression. Results demonstrated that participants in the MARIGOLD condition had reduced depressive symptoms compared to controls and, although the effect did not reach statistical significance, reductions in past day negative emotion appeared to mediate this effect. Contrary to hypotheses, the intervention did not increase positive emotion compared to the control condition. Discussion focuses on the need for future studies to continue investigating the mechanisms of action for PPIs with emphasis on theoretically-based measurement and operationalization of emotion and other potential mediators to maximize the ultimate impact of PPIs on psychological well-being. Clinical Trials registration #NCT02861755.
Keywords: Positive psychological intervention, Positive emotion, Depression, Emotion reactivity
Depression is common in the general population and has increased in prevalence in recent years. According to the National Center for Health Statistics, in 2019, 18.5% of U.S. adults reported at least mild depression with 7% reporting moderate levels or above (Villarroel & Terlizzi, 2020). In a representative survey of U.S. adults conducted in 2017 and 2018, 8.5% of the sample reported elevated depressive symptoms. Identifying mechanisms of and efficacious treatment for depression are increasingly important as mental health effects of the COVID pandemic continue to unfold. During early 2020 at the start of the COVID pandemic, 27.8% of U.S. adults surveyed reported elevated depressive symptoms (Ettman et al., 2020).
A key feature of depression is anhedonia, or loss of pleasure, particularly in the context of stress (Pizzagalli, 2014). People with depression are less likely to try to increase or upregulate positive emotion and may even actively avoid positive stimuli compared to people without depression (Vanderlind et al., 2020). Positive psychological interventions (PPIs), which specifically target positive emotion through practices such as gratitude, savoring, and acts of kindness (Schueller et al., 2014), hold promise for people with elevated depressive symptoms (Silton et al., 2020). Although some PPIs do not find an effect on positive emotion (e.g., Hausmann et al., 2018), meta-analyses of PPIs show that, taken as a whole, they both increase positive emotion and decrease depressive symptoms in depressed and non-depressed samples (Bolier, Haverman, Kramer, et al., 2013; Carr et al., 2020; Chakhssi et al., 2018; Curry et al., 2018; Davis et al., 2016; Dickens, 2017; Hendriks et al., 2019; Kirby et al., 2017; Zeng et al., 2015). Studies comparing PPIs to anti-depressants or cognitive behavioral therapy for people with elevated depression show that PPIs are comparable to these more traditional therapies for improving happiness, reducing depressive symptoms, and increasing rates of remission (Seligman, 2006). For example, a randomized trial comparing a 10-session PPI to 10 sessions of CBT skills in women with a diagnosis of major depression or dysthymia, showed reduced depression and increased well-being in both conditions, with no significant differences between the two groups (Chaves et al., 2017).
Based on the Broaden and Build theory (Fredrickson, 1998) and revised Stress and Coping theory (Folkman, 1997), the Positive Pathways to Health theoretical model (Moskowitz, Addington, et al., 2019; Moskowitz, Cheung, et al., 2019) posits increased positive emotion as the primary mechanism through which PPIs improve physical and psychological health and well-being. Specifically, the model hypothesizes that engaging in the positive activities in PPIs increases the frequency of positive emotion which, in turn, has a range of proximal effects such as providing a timeout from stress, (Lazarus et al., 1980) prompting more adaptive coping strategies, (Folkman, 1997) broadened attention and cognition and increased behavioral action tendencies, (Fredrickson, 1998) reduced emotional reactivity to daily stress, and strengthened social relationships, which all lead to reduced stress. In turn, this reduction in stress predicts better psychological well-being (e.g., less depression).
Despite theoretical models that suggest positive emotion as a key pathway linking PPIs to reductions in depression (Layous et al., 2014; Moskowitz, Addington, et al., 2019; Schueller et al., 2014) and empirical evidence that PPIs increase positive emotion and decrease depression, few studies have examined whether positive emotion is a mechanism through which the interventions influence subsequent depression. Fredrickson et al. (2008) found that participants in a loving-kindness meditation intervention (considered a PPI because it specifically targets positive emotion) experienced significantly less depression compared to a waitlist control condition. Furthermore, increases in daily positive emotion, as reported with the Day Reconstruction Method (DRM; Kahneman et al., 2004) mediated the effect of the intervention on depression both directly as well as through increased psychological, social, and physical resources.
In a randomized trial of a 6-week PPI with dementia caregivers, investigators found that, compared to participants in an emotion reporting control condition, those in the intervention reported significant improvements on positive emotion, depression, anxiety, self-reported physical health, and positive aspects of caregiving. Positive emotion, measured through a retrospective report of emotions experienced over the past week, was a significant mediator of intervention effects on depression, although not for the other outcomes (Moskowitz, Cheung, et al., 2019). However, both the mediator and outcome were assessed at the same time point, so a reverse causal pathway from decreased depression to increased positive emotion could not be ruled out. In another test of the same intervention in people newly diagnosed with HIV, although the intervention led to increased past day positive emotion (as assessed with the DRM), decreased intrusive/avoidant thoughts about HIV, and decreased likelihood of anti-depressant use compared to an attention-matched control over 15-month post-diagnosis, positive emotion was not a significant mediator of the impact of the intervention on any of these outcomes (Moskowitz et al., 2017).
Observational studies indicate that beyond mean levels of past day or past week positive emotion, the emotional response to daily stressors may be particularly important in driving future levels of depression. Specifically, individuals whose positive emotion is more stable, or takes less of a “hit” in response to daily stressful events, are less likely to develop subsequent depressive symptoms (Rackoff & Newman, 2020). In a study that examined emotional reactivity to daily stress, participants who had greater decreases in positive emotion in stressful moments had larger increases in depression over 18 months (Zhaoyang et al., 2020). The same was not true of negative emotion: increases in negative emotion in stressful moments (compared to non-stressful moments) were not related to depressive symptoms over the subsequent months. Ong and Burrow (2018) found that increased reactivity of both positive and negative emotion in response to daily experiences of racial discrimination predicted elevated depressive symptoms a year later. These findings indicate that emotional reactivity (either positive or negative) mediated the impact of racial discrimination on subsequent depression (Ong & Burrow, 2018).
Although positive emotion can vary independently from negative and has unique adaptive consequences (Lyubomirsky et al., 2005), particularly under stress (Folkman & Moskowitz, 2000), the strength of the correlation between positive and negative emotion across contexts may also be an important consideration. The Dynamic Model of Affect (DMA; Zautra et al., 2001) posits that positive and negative emotion are relatively uncorrelated under lower stress conditions and provide more nuanced and complex information about the psychological context by varying independently. Under more stressful conditions, however, positive and negative emotion become more strongly inversely correlated and thus preserve cognitive resources to focus on the source of the stress. Hardy and Segerstrom (2017) compared several operationalizations of psychological flexibility as predictors of psychological well-being over 10 years. Results from daily reports of emotion and stress supported the DMA in that individuals who had a larger difference between the associations of positive with negative emotion on stress days compared to non-stress days (e.g., greater psychological flexibility across contexts) had lower distress scores a decade later.
In this paper, we report the results of a randomized trial of a multi-component PPI, called MARIGOLD (Mobile Affect Regulation Intervention with the Goal of Lowering Depression; Addington et al., 2019; Cheung et al., 2018) on depressive symptoms and positive emotion. The intervention and control content were both delivered in a self-guided online format. Based on our theoretical model (Moskowitz, Addington, et al., 2019), we hypothesized that the intervention would decrease depressive mood via increased positive emotion. We also explored whether negative emotion is influenced by the intervention and subsequently impacts depressive symptoms. In addition, guided by previous work that suggests that different retrospective reporting periods and operationalizations of emotion may be differentially influenced by the intervention (Moskowitz, Cheung, et al., 2021), we focus on the question of whether different operationalizations of positive and negative emotion—past week retrospective reports, past day retrospective reports, emotion reactivity to daily stressors, and emotional flexibility (association of positive and negative emotion on stress vs. non-stress days)—mediate the impact of MARIGOLD on depressive symptoms.
Method
The study was approved by the IRB and pre-registered through ClinicalTrials.gov (NCT02861755). Full details of the design are in Cheung et al. (2018).
Participants
All participants were recruited online through platforms such as ResearchMatch, Craigslist, and Reddit. To be eligible for the study participants had to (1) have at least mild levels of depression as indicated by a PHQ-8 depression score >5 (Kroenke et al., 2009); (2) be 18 or older; (3) have daily access to the internet; (4) own a mobile phone; (5) live in the USA; and (6) be able to read and write in English.
Procedure
Consenting participants received a baseline questionnaire and a week-long daily diary “burst” in which they were asked to report occurrence of stressful events and their emotions once each day. Those who completed the baseline assessment and at least 4 of 7 days of this first daily diary burst period were stratified based on gender and depressive symptom severity (PHQ-8 score: 5–9, mild; 10–14, moderate; 15–19, moderately severe; >20, severe), to ensure a sufficient number in each group within each condition. After stratification, we sequentially allocated participants into one of 9 study arms: 8 intervention conditions (that tested combinations of adherence enhancements (Moskowitz, Addington, et al., 2021) and one emotion-reporting control condition. Participants in all nine conditions reported their emotions daily for seven weeks. Participants in the 8 intervention conditions additionally received MARIGOLD, a 5-week multi-component PPI delivered via an online platform.
The intervention consists of 8 skills that specifically target positive emotion: Noticing positive events, capitalizing, gratitude, behavioral activation, mindfulness, positive reappraisal, personal strengths, and acts of kindness. Additional details of the intervention and rationale for inclusion of each skill can be found elsewhere (Addington et al., 2019; Cheung et al., 2018; Cohn et al., 2014; Dowling et al., 2014; Moskowitz, Cheung, et al., 2019; Moskowitz et al., 2014, 2017). The skills were delivered in a self-guided online format, and each week had associated home practice activities. Participants did not have access to all the skills at once; instead, one to three skills were released each of the 5 weeks.
In the control condition, participants were asked to log into the platform daily during the intervention period to report their emotions. Preliminary pilot studies of MARIGOLD (Addington et al., 2019) indicated that a no-treatment waitlist control might lead to worsening depressive symptoms. Thus, it was important to offer control group participants an activity that could potentially benefit them. We chose an emotion-reporting control which likely increases awareness of emotions and, therefore, may reduce depressive symptoms (Boden & Thompson, 2015) but does not have the PPI skills content that are of primary interest as an intervention here.
In addition to baseline, assessments and week-long daily diary “bursts” were also completed at post-intervention (POST; approximately 7-week post-baseline), 1 month after the end of the intervention (FU1) and 3 months after the intervention (FU2).
Measures
Depressive symptoms were assessed at each assessment point (baseline, POST, FU1, and FU2) using the CES-D (Radloff, 1977), a 20-item measure that taps into symptoms experienced over the past week. Participants are asked to report how often they have experienced each symptom from 0 = “rarely or none of the time” to 3 = “most or all of the time.” Items are summed to form a total score at each assessment point.
Positive and negative emotion were measured in the daily diaries and in the assessments using the Differential Emotions Scale (DES) as modified by Fredrickson (2013), which lists nine positive emotions (amused awe, content, happy, grateful, hopeful, interested, love, and pride) and eight negative emotions (angry, anxious, ashamed, contempt, disgust, embarrassed, guilty, and sad). Past week emotion was the average of positive or negative emotion items from the assessments that elicited recall over the past week. For the daily diaries, participants were asked how frequently they felt each emotion in the past day. Past day emotion is the average of positive or negative emotion over all the daily diaries completed during that week-long burst. Emotion reactivity is the extent to which positive emotion decreases or negative emotion increases in response to daily stressful events and was operationalized following the analytic methods of Ong and Burrow (2018). We assessed daily stressful events in the bursts using the Daily Inventory of Stressful Events (DISE; Almeida et al., 2011, 2002) in which participants were asked to indicate whether each of a list of 7 potentially stressful events had happened that day (e.g., had an argument or disagreement with someone or a stressful event at work) and if it did happen, to rate how stressful it was from 1 = not at all stressful to 4 = very stressful. For the present analyses, we used the number of stressful events that happened that day (0 to 7) and did not take appraisals of stressfulness into account in order to better differentiate the occurrence of the event from the emotional response to it (Leger et al., 2020; Rackoff & Newman, 2020). We used mixed effects linear regression to model the effect of count of stressful events on daily positive (or negative) emotion across bursts at each assessment period. The individual level effects were retained and used as indicators of reactivity at each time point. Finally, we calculated emotional flexibility following Hardy and Segerstrom’s (2017) calculation of Dynamic Psychological Flexibility as the difference between association of daily positive and negative emotion on stress days compared to non-stress days. We used mixed effects linear regression to model the effect of positive emotion on negative emotion at each burst on stress days (where count of stressful events ≥ 1) and, separately, on non-stress days (count of stressful events = 0). The individual level effects were retained from each model, and emotional flexibility was calculated for each participant as the difference in effect on non-stress days compared to stress days, in which a higher score indicates higher flexibility.
Analysis
Descriptive statistics were calculated for the overall sample and individually by intervention group (intervention vs. control), and differences in sample characteristics between intervention groups were calculated using t-tests for continuous variables and chi-squared tests for categorical variables. To assess the effect of intervention on each outcome and the change in outcome over time, we ran a series of mixed effects linear regression models. These intent-to-treat analyses first included the effects of intervention, linear time, and the interaction of intervention×time, as well as a random effect for intercept and slope. The second model added the effect of quadratic time, in order to account for a potential non-linear change in outcome over time. Difference in model fit was compared using a chi-squared test for the difference in log likelihood values, and results from the quadratic model were reported only if model fit was statistically significantly better; otherwise, results from the linear model were reported. Beta estimates for the effect of intervention on change in each outcome are reported along with least square means estimates for each group at each time point. Since age at baseline differed by intervention group, we included age as a covariate in our final models; results presented are adjusted for baseline age.
Participants having at least one outcome measurement were included in all models for that outcome. Missing outcome data was not imputed, as our modeling approach allowed for participants to be included even if they are missing data at some time points. Cohen’s d effect sizes (Cohen, 1988) were calculated to facilitate comparison of group differences in change from baseline to each of the three follow-up time points. Analyses were completed using SAS v 9.4, and effects were considered statistically significant at p < 0.05. To assess the possibility of each emotion operationalization mediating the effect of the intervention on depressive mood, a second set of models were run using a multilevel SEM framework (Preacher et al., 2010). In these models, we included both the direct effects of intervention and emotion and the indirect effect of intervention through emotion on both CES-D and change in CES-D over time. We conducted separate models for each of the six potential mediators. All SEM analyses were completed using MPLUS v7.4 and effects were considered statistically significant at p < 0.05.
Results
Of the 1,805 respondents who completed the screener, 1,037 (57%) were deemed eligible and entered the first daily diary burst. Fifty eight percent of these (n = 602) completed at least 4 of the 7 daily diary entries in the burst and the baseline assessment and were then sequentially assigned to one of the nine study conditions; 8 conditions in which they received the PPI alone, the PPI plus an adherence enhancement, or an emotion-reporting control condition. Details of the adherence enhancements can be found elsewhere (Moskowitz, Addington, et al., 2021). There were no differences on depressive mood among the 8 intervention conditions (with and without the adherence enhancements), so they were combined (n = 539 intervention vs. n=63 controls) for the present analyses. The CONSORT diagram appears in Fig. 1. Just over half of the participants (54%) were retained through the second follow-up assessment. Average age of the participants was 38 (range of 18 to 80). The sample was predominantly female and non-Hispanic white. Intervention and control groups did not differ at baseline on any demographic variable except age with the intervention condition being, on average, 38.7 compared to control condition with an average age of 35.1 (p = .05; Table 1). Given the baseline differences in age, we adjust all subsequent analysis for age. (Note that adjusting for age did not result in any substantive change in the results).
Fig. 1.
CONSORT
Table 1.
Sample demographics by condition
| Total sample | Intervention (N = 509) | Control (N=63) | ||
|---|---|---|---|---|
| (N=602) | p | |||
| Age M (SD) | 38.3 (13.6) | 38.7 (13.7) | 35.1 (12.2) | 0.05 |
| Gender (%) | ||||
| Male | 25.50% | 25.50% | 25.40% | 1 |
| Female | 73.60% | 73.53% | 74.60% | |
| Ethnicity (%) | ||||
| Hispanic | 17.50% | 17.65% | 15.90% | 0.73 |
| Not Hispanic | 82.50% | 82.35% | 84.10% | |
| Race (%) | ||||
| Black | 16.20% | 16.27 | 15.90% | 0.94 |
| White | 73.50% | 73.14% | 75.20% | 0.6 |
| Asian | 8.60% | 9.02% | 4.80% | 0.25 |
| Native American | 4.70% | 4.71% | 4.80% | 0.24 |
| Pacific Islander | 0.30% | 0.39% | 0.00% | 0.79 |
| Mixed/Other | 7.50% | 7.25% | 9.50% | 0.45 |
Age adjusted intervention effects on change in depression and each operationalization of emotion are in Table 2. Consistent with previous findings of PPIs, the intervention led to a significant reduction in depressive symptoms over time compared to the emotion-reporting control condition. Participants in the intervention condition reported significantly lower depression on the CES-D immediately after the intervention (POST) and at the 1-month follow-up assessment (FU1), but the difference was no longer significant at the 3-month follow-up (FU2). Both the linear and quadratic terms were significant indicating that the difference between groups lessened over time. The effect sizes (Cohen’s d; Fig. 2) for between-group difference in change from baseline to POST were d = −.60; baseline to FU1 were d = −.45; and baseline to FU2 were d = −.30; small to medium effects that were on par with other PPI effects on depression (Carr et al., 2020).
Table 2.
Intervention effects on depressive mood, positive emotion, negative emotion, and emotion flexibility
| Baseline (n=602) mean (SD) |
Post (n=353) mean (SD) |
Follow-up 1 (n=320) mean (SD) |
Follow-up 2 (n=328) mean (SD) |
Overall effect (intervention × time) |
|||
|---|---|---|---|---|---|---|---|
| Depressive mood | Past week (assessment) | Intervention | 32.544 (0.57) | 23.598 (0.62) | 19.826 (0.68) | 21.227 (0.78) |
βtime=−10.211* βtime×time=1.879* |
| Control | 32.191 (1.61) | 27.819 (1.75)* | 24.862 (1.91)* | 23.321 (2.22) | |||
| Positive emotion | Past week (assessment) | Intervention | 3.994 (0.06) | 4.332 (0.06) | 4.669 (0.08) | 5.007 (0.10) | βtime=0.058 |
| Control | 3.620 (0.18) | 3.900 (0.18)* | 4.180 (0.22)* | 4.460(0.28) | |||
| Past day (daily diary) | Intervention | 3.902 (0.06) | 4.112 (0.07) | 4.322 (0.08) | 4.531 (0.10) | βtime=0.056 | |
| Control | 3.469 (0.18)* | 3.622 (0.19)* | 3.776 (0.22)* | 3.929 (0.27)* | |||
| Reactivity to stress (daily diary) | Intervention | 0.007 (0.01) | 0.009 (0.01) | 0.011 (0.02) | 0.013 (0.02) | βtime=0.0005 | |
| Control | −0.071 (0.04) | −0.070 (0.04) | −0.069 (0.04) | −0.067 (0.05) | |||
| Negative emotion | Past week (assessment) | Intervention | 4.726 (0.07) | 3.467 (0.08) | 2.990 (0.08) | 3.293 (0.10) |
βtime=−1.115* βtime×time=0.201* |
| Control | 4.881 (0.20) | 4.133 (0.2)* | 3.766 (0.24)* | 3.776 (0.28) | |||
| Past day (daily diary) | Intervention | 3.545 (0.07) | 3.007(0.07) | 2.802 (0.08) | 2.933 (0.09) |
βtime=−0.949* βtime×time=0.162* |
|
| Control | 3.493 (0.20) | 3.418 (0.21) | 3.353 (0.21)* | 3.298 (0.25) | |||
| Reactivity to stress (daily diary) | Intervention | 0.002 (0.02) | −0.0002 (0.01) | −0.001 (0.04) | −0.005 (0.02) | βtime=−0.038* | |
| Control | −0.0003 (0.04) | 0.035 (0.04) | 0.070 (0.04) | 0.105 (0.05)* | |||
| Emotional flexibility | Association of positive and negative emotion on stress vs. non-stress days (daily diary) | Intervention | 0.113 (0.02) | 0.112 (0.01) | 0.110 (0.02) | 0.110 (0.02) | βtime=0.039 |
| Control | 0.154 (0.05) | 0.114 (0.04) | 0.074 (0.05) | 0.033 (0.07) | |||
Note: Age was significant in models of: negative reactivity, negative emotion at daily burst, negative emotion at assessment level, and emotion flexibility but estimates were robust to the inclusion of the age covariate. *p < .05 for within-time point comparison
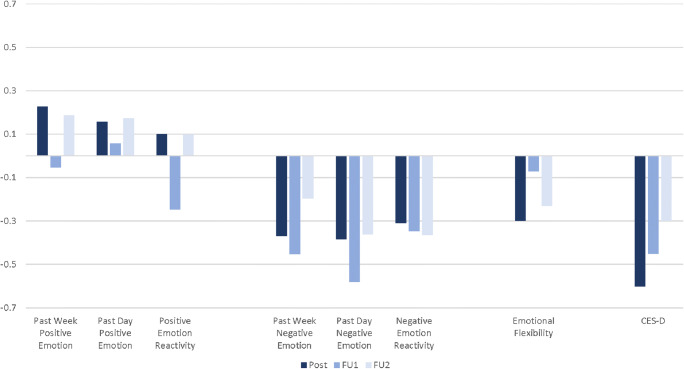
Fig. 2.
Effect sizes for between group difference in change from baseline to POST, FU1, and FU2 for emotion and depression. d = .20 can be considered small, d = .50 is medium, and d = .80 is generally considered large (Cohen, 1988).
Change in positive emotion did not differ significantly between intervention and control over time for any of the operationalizations. Within assessment points, there was some suggestion that past week reports of positive emotion were higher for the intervention group compared to the control at POST and one month later. The intervention group was significantly higher on past day positive emotion at all time points, including baseline, so the between group difference in change from baseline over time was not statistically significant. Effect sizes for between group change from baseline to POST, FU1, and FU2 across all the positive emotion variables were negligible to small (Fig. 2).
On the other hand, the intervention had a statistically significant effect on all three operationalizations of negative emotion—past week (linear and quadratic effects), past day (linear and quadratic), and negative emotion reactivity (linear only). Looking at comparisons within assessment points, the intervention group reported less negative emotion over the past week immediately post-intervention and one month later; lower past day negative emotion at 1-month follow-up (FU1), and less negative emotion reactivity at the 3-month follow-up (FU2). Effect sizes were in the small to medium range (Fig. 2).
Results for emotion flexibility indicate there was no group difference in the association of positive and negative emotion comparing days with a stressor (when the correlation is expected to be higher) to days without a stressor (when correlation is expected to be lower). Over time, this difference stayed relatively unchanged for the intervention condition reflecting a stable difference in the correlation of positive and negative emotion on stress and nonstress days across assessments. For the control condition, the difference appears to get smaller—the correlation on stress and nonstress days grows more similar over time indicating decreasing flexibility of emotional responding across stress and nonstress days. However, the difference was not statistically significant overall or within assessment at any point and effect sizes were small.
Given previous evidence from this sample that those with very high PHQ-8 scores at baseline might respond differently to the intervention (Moskowitz, Addington, et al., 2021), we reran the longitudinal models excluding those with PHQ-8 of 20 or higher (n = 83 in the intervention and n = 10 in the control were excluded). None of the effects changed appreciably. The effects of the intervention on positive emotion outcomes and emotion flexibility over time remained non-significant and intervention effects on past day negative emotion and CES-D remained significant. Effects on past week negative emotion and negative emotion reactivity were no longer significant.
Results of mediation analyses are in Table 3. The indirect effect of the intervention on change in CES-D through each emotion operationalization reached borderline statistical significance for daily negative emotion (p = .057) indicating that the intervention effects on decreased depressive symptoms were partially mediated through decreases in negative emotion as assessed in the daily diaries. Mediation effects did not approach significance for any other emotion operationalization. Figure 3 shows the mediation pathway of intervention, daily negative emotion, and CES-D. For simplicity, we include only the overall direct effects of intervention and daily negative emotion and the indirect effect of the intervention through daily negative emotion on CES-D over time in the figure, though, as specified above, the model included both within and between-subjects effects of intervention and emotion on CES-D.
Table 3.
Emotion mediators of intervention effects on change in CES-D
| Mediator | Indirect effect | p | |
|---|---|---|---|
| Positive emotion | Past week | β= 0.071 | .536 |
| Past day | β= −0.0052 | .451 | |
| Reactivity | β= −0.001 | .982 | |
| Negative emotion | Past week | β= −0.907 | .17 |
| Past day | β= 0.194 | .057 | |
| Reactivity | β= 0.115 | .191 | |
| Association of positive and negative emotion on stress vs. non-stress days | Emotional flexibility | β= 0.161 | 0.355 |
Fig. 3.
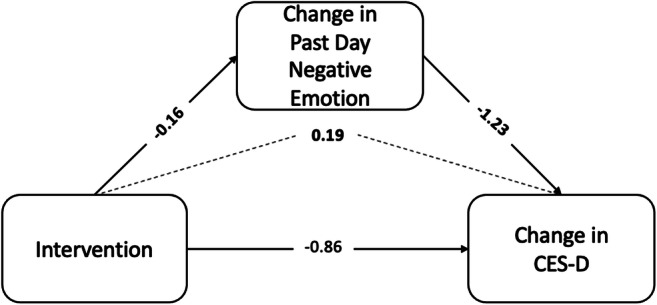
Decrease in past day negative emotion approaches statistical significance in mediating intervention effects on CES-D. Note: Model included both the direct effects of intervention and emotion and the indirect effect of intervention through emotion on both CES-D and change in CES-D over time but to simplify the figure, we depict only the overall direct effects of intervention and the indirect effect of the intervention through daily negative emotion on CES-D over time.
Discussion
Consistent with previous studies that demonstrate an effect of PPIs on depression (see Wen et al., 2020 for a review), the present trial demonstrated that MARIGOLD, a multi-component positive psychological intervention consisting of skills that target positive emotion, significantly reduced depressive symptoms compared to an emotion reporting control condition. The intervention significantly reduced negative emotion as reported over the past day in the daily diaries and over the past week in the assessments. In addition, intervention participants showed a drop in their negative emotion response to daily stress compared to the control condition.
Contrary to our hypotheses, however, none of the operationalizations of positive emotion differed significantly between the intervention and control groups over time. Examination of means within time points suggested that the intervention group showed greater improvements in past week positive emotion at the immediate post and 1-month follow-up assessments; however, the control condition also appeared to improve over time so the overall change over the follow-up period was not statistically significant. Moreover, the effects were generally small. Emotional flexibility, the operationalization that combined positive and negative emotion by examining the correlation between the two on days when a stressor occurred compared to non-stress days, did not differ between the intervention and control groups. Whereas the difference in correlation of positive and negative emotion between stress and non-stress days remained stable across assessment for the intervention condition, the difference in the control decreased, suggesting that control participants were becoming less emotionally flexible over time.
Several theoretical models (e.g., Layous et al., 2014; Moskowitz, Addington, et al., 2019; Schueller et al., 2014) suggest that positive emotion is a key pathway through which PPIs impact subsequent depression. The findings of the present study suggest that in this sample, negative emotion was a more important pathway as MARIGOLD had a larger impact on the negative emotion outcomes compared to the positive emotion outcomes. Mediation analyses that explicitly tested each emotion operationalization separately indicated that past day negative emotion as assessed in the daily diaries was a marginally significant mediator of the intervention effect on depressive mood.
There are several possible explanations for the lack of effect of MARIGOLD with respect to positive emotion outcomes. First, in contrast to other studies of PPIs in depressed samples (e.g., Bolier, Haverman, Kramer, et al., 2013), MARIGOLD did not have an upper limit of depression for inclusion so individuals with very high scores on the PHQ-8 were enrolled in the study. Previous analyses in these MARIGOLD data indicate that participants with very high depression scores responded less favorably to some of the adherence enhancements (Moskowitz, Addington, et al., 2021) so it may be that the higher levels of depression in the present sample explains the lack of support for intervention effects on positive emotion. Although exploratory analyses in which we excluded those with the highest level of depression did not support this hypothesis, a fully powered study that addresses the question of whether baseline depression level moderates intervention effects is warranted.
A second possible explanation for the lack of effect on positive emotional outcomes is that the control condition was very active and likely had an impact on the emotion outcomes. Examination of the means over time in the control condition shows decreases on the CES-D and negative emotion outcomes as well as increases for the positive emotion outcomes, although the changes are smaller than within the intervention condition. Participants in the control condition were asked to log in to the platform and report their emotions daily throughout the intervention period and emotion tracking alone likely increases awareness of emotions which has been shown to be effective in reducing depressive symptoms (Boden & Thompson, 2015). Previous phases of the MARIGOLD intervention (Addington et al., 2019) suggested that participants in a no-treatment comparison condition experienced significant increases in depression over time so it was important in this larger trial to provide an activity that could potentially be efficacious to the control condition. However, the potential beneficial effects of the emotion reporting control activities weakened the apparent impact of the intervention by comparison.
It is important to note that the MARIGOLD sample was not very diverse in terms of gender, race, or education so likely has limited generalizability to other groups who could potentially benefit. Furthermore, the MARIGOLD study was not designed to test questions of mediation and thus was not optimally situated to capture these effects. On the other hand, MARIGOLD is considered a high quality intervention according to the Cochrane collaboration criteria (Higgins & Green, 2008) because it met 5 of the 6 criteria including: (1) randomization concealment, (2) baseline comparability of groups (with the exception of age which was controlled in the analyses), (3) at least 50 participants in the analysis, (4) loss to follow up < 50%, and (5) the use of intent-to-treat analyses. The 6th criteria, blinding of subjects to condition, was not possible once participants started sessions in their assigned condition, although the emotion reporting was an active control condition which may have improved participant emotional responses.
Future work addressing questions of mediational pathways of PPIs should consider other potential mediators including positive cognitions and behaviors (Schueller et al., 2014) as well as an expanded focus on eudaimonic well being, which is also responsive to PPIs (Moskowitz, Cheung, et al., 2021). Additional pathways through which PPIs may impact psychological well-being, particularly in people with depression, include positive event experience and appraisal of those events (Freedman & Moskowitz, 2021). The experience of positive life events has been associated with decreased depressive symptoms (Blonski et al., 2016; Spinhoven et al., 2011) and compared to individuals without depression, individuals with depression show a greater decrease in negative emotion in response to positive events (Khazanov et al., 2019). The skills taught in MARIGOLD may bolster the experience and appraisal of positive events, which, in turn, may serve as a mechanism by the intervention impacts psychological well-being and depression. Furthermore, future studies of PPI mediation on depression should not exclude the possibility that reductions negative emotions, cognitions, and behaviors may be significant mediators as well.
The present work extends the literature on PPIs by advancing understanding of one key pathway hypothesized to link PPIs to psychological outcomes. Our hypotheses about positive emotion as the key mediator of intervention effects were not supported by these data. However, we did find evidence that decreases in negative emotion were an important pathway through which the MARIGOLD intervention influenced depression in a sample that had significantly elevated depression at baseline. Although MARIGOLD resulted in reduced depressive symptoms compared to an emotion-reporting control condition, levels of depressive symptoms remained higher than the general population norm (Radloff, 1977) at 3-month post-intervention. Furthermore, mean CES-D for both groups at the final assessment were above 20, high enough to be considered at risk for clinical depression (Vilagut et al., 2016). Whereas PPIs like MARIGOLD may not be sufficient as a stand-alone treatment for depression, they hold promise as an adjunct to more traditional depression treatments or as the initial step of a lower intensity evidence-based treatment in a stepped care treatment plan for depression (van Straten et al., 2015). Given that deficits in positive affect predict poorer treatment response in depression (e.g., Forbes et al., 2010; McMakin et al., 2012; Spijker et al., 2001), integration of PPIs into treatment plans for people with depression warrants serious consideration.
Additional Information
Funding Information
This work was funded by R34MH101265.
Conflicts of Interest
The authors declare no competing interests.
Data Availability
Data are available here: https://osf.io/d2v6m/?view_only=894e78477476477d927361a82685b5e9.
Ethical Approval
Was obtained from the institutional IRB.
Informed Consent
All participants completed an online informed consent.
References
- Addington E, Cheung EO, Bassett S, Kwok I, Schuette S, Shiu E, Yang D, Cohn MA, Leykin Y, Saslow LR, Moskowitz JT. The MARIGOLD study: Feasibility and enhancement of an online intervention to improve emotion regulation in people with elevated depressive symptoms. Journal of Affective Disorders. 2019;257:352–364. doi: 10.1016/j.jad.2019.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida DM, Wethington E, Kessler RC. The daily inventory of stressful events: An interview-based approach for measuring daily stressors. Assessment. 2002;9(1):41–55. doi: 10.1177/1073191102091006. [DOI] [PubMed] [Google Scholar]
- Almeida, D. M., Stawski, R. S., & Cichy, K. E. (2011). Combining checklist and interview approaches for assessing daily stressors: The daily inventory of stressful events. The handbook of stress science: Biology, psychology, and health (pp. 583–595).
- Blonski SC, Conradi HJ, Oldehinkel AJ, Bos EH, de Jonge P. Associations between negative and positive life events and the course of depression: A detailed repeated-assessments study. The Journal of Nervous and Mental Disease. 2016;204(3):175–180. doi: 10.1097/NMD.0000000000000445. [DOI] [PubMed] [Google Scholar]
- Boden MT, Thompson RJ. Facets of emotional awareness and associations with emotion regulation and depression. Emotion. 2015;15(3):399. doi: 10.1037/emo0000057. [DOI] [PubMed] [Google Scholar]
- Bolier L, Haverman M, Kramer J, Westerhof GJ, Riper H, Walburg JA, Boon B, Bohlmeijer E. An Internet-based intervention to promote mental fitness for mildly depressed adults: Randomized controlled trial. Journal of Medical Internet Research. 2013;15(9):e2603. doi: 10.2196/jmir.2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health. 2013;13(1):1. doi: 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr, A., Cullen, K., Keeney, C., Canning, C., Mooney, O., Chinseallaigh, E., & O’Dowd, A. (2020). Effectiveness of positive psychology interventions: A systematic review and meta-analysis. The Journal of Positive Psychology, 1–21.
- Chakhssi F, Kraiss JT, Sommers-Spijkerman M, Bohlmeijer ET. The effect of positive psychology interventions on well-being and distress in clinical samples with psychiatric or somatic disorders: A systematic review and meta-analysis. BMC Psychiatry. 2018;18(1):211. doi: 10.1186/s12888-018-1739-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaves C, Lopez-Gomez I, Hervas G, Vazquez C. A comparative study on the efficacy of a positive psychology intervention and a cognitive behavioral therapy for clinical depression. Cognitive Therapy and Research. 2017;41(3):417–433. [Google Scholar]
- Cheung, E. O., Addington, E. L., Bassett, S. M., Schuette, S. A., Shiu, E. W., Cohn, M. A., Leykin, Y., Saslow, L. R., & Moskowitz, J. T. (2018). Study protocol and design for the MARIGOLD study: A self-paced online positive emotion skills intervention for people with elevated symptoms of depression. JMIR Research Protocols, 7(6). 10.2196/10494 [DOI] [PMC free article] [PubMed]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Erlbaum; 1988. [Google Scholar]
- Cohn MA, Pietrucha ME, Saslow LR, Hult JR, Moskowitz JT. An online positive affect skills intervention reduces depression in adults with type 2 diabetes. The Journal of Positive Psychology. 2014;9(6):523–534. doi: 10.1080/17439760.2014.920410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry OS, Rowland LA, Van Lissa CJ, Zlotowitz S, McAlaney J, Whitehouse H. Happy to Help? A systematic review and meta-analysis of the effects of performing acts of kindness on the well-being of the actor. Journal of Experimental Social Psychology. 2018;76:320–329. [Google Scholar]
- Davis DE, Choe E, Meyers J, Wade N, Varjas K, Gifford A, Quinn A, Hook JN, Van Tongeren DR, Griffin BJ. Thankful for the little things: A meta-analysis of gratitude interventions. Journal of Counseling Psychology. 2016;63(1):20. doi: 10.1037/cou0000107. [DOI] [PubMed] [Google Scholar]
- Dickens LR. Using gratitude to promote positive change: A series of meta-analyses investigating the effectiveness of gratitude interventions. Basic and Applied Social Psychology. 2017;39(4):193–208. [Google Scholar]
- Dowling GA, Merrilees J, Mastick J, Chang VY, Hubbard E, Moskowitz JT. Life enhancing activities for family caregivers of people with frontotemporal dementia. Alzheimer Disease & Associated Disorders. 2014;28(2):175–181. doi: 10.1097/WAD.0b013e3182a6b905. [DOI] [PubMed] [Google Scholar]
- Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020). Prevalence of depression symptoms in U.S. adults before and during the COVID-19 pandemic. JAMA Network Open, 3(9), e2019686–e2019686. [DOI] [PMC free article] [PubMed]
- Folkman S. Positive psychological states and coping with severe stress. Social Science and Medicine. 1997;45:1207–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- Folkman S, Moskowitz JT. Positive affect and the other side of coping. American Psychologist. 2000;55(6):647–654. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- Forbes EE, Olino TM, Ryan ND, Birmaher B, Axelson D, Moyles DL, Dahl RE. Reward-related brain function as a predictor of treatment response in adolescents with major depressive disorder. Cognitive, Affective, & Behavioral Neuroscience. 2010;10(1):107–118. doi: 10.3758/CABN.10.1.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL. What good are positive emotions? Review of General Psychology. 1998;2:300–319. doi: 10.1037/1089-2680.2.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL. Advances in experimental social psychology. Elsevier; 2013. Positive emotions broaden and build; pp. 1–53. [Google Scholar]
- Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: Positive emotions, induced through meditation, build consequential personal resources. Journal of Personality and Social Psychology. 2008;95:1045–1062. doi: 10.1037/a0013262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman ME, Moskowitz JT. Effect of positive psychological interventions on perception of positive events: An unknown outcome. European Journal of Applied Positive Psychology. 2021;5:1–13. [Google Scholar]
- Hardy, J., & Segerstrom, S. C. (2017). Intra-individual variability and psychological flexibility: Affect and health in a National U.S. sample. Journal of Research in Personality, 69, 13–21.
- Hausmann LR, Youk A, Kwoh CK, Gallagher RM, Weiner DK, Vina ER, Obrosky DS, Mauro GT, McInnes S, Ibrahim SA. Effect of a positive psychological intervention on pain and functional difficulty among adults with osteoarthritis: A randomized clinical trial. JAMA Network Open. 2018;1(5):e182533–e182533. doi: 10.1001/jamanetworkopen.2018.2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks, T., Schotanus-Dijkstra, M., Hassankhan, A., de Jong, J., & Bohlmeijer, E. (2019). The efficacy of multi-component positive psychology interventions: A systematic review and meta-analysis of randomized controlled trials. Journal of Happiness Studies, 1–34.
- Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Wiley Online Library; 2008. [Google Scholar]
- Kahneman D, Krueger AB, Schkade DA, Schwarz N, Stone AA. A survey method for characterizing daily life experience: The day reconstruction method. Science. 2004;306(5702):1776–1780. doi: 10.1126/science.1103572. [DOI] [PubMed] [Google Scholar]
- Khazanov GK, Ruscio AM, Swendsen J. The “brightening” effect: Reactions to positive events in the daily lives of individuals with major depressive disorder and generalized anxiety disorder. Behavior Therapy. 2019;50(2):270–284. doi: 10.1016/j.beth.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby JN, Tellegen CL, Steindl SR. A meta-analysis of compassion-based interventions: Current state of knowledge and future directions. Behavior Therapy. 2017;48(6):778–792. doi: 10.1016/j.beth.2017.06.003. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders. 2009;114(1):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Layous K, Chancellor J, Lyubomirsky S. Positive activities as protective factors against mental health conditions. Journal of Abnormal Psychology. 2014;123(1):3. doi: 10.1037/a0034709. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Kanner AD, Folkman S. Emotions: A cognitive-phenomenological analysis. In: Plutchik R, Kellerman H, editors. Theories of emotion. Academic Press; 1980. pp. 189–217. [Google Scholar]
- Leger KA, Charles ST, Almeida DM. Positive emotions experienced on days of stress are associated with less same-day and next-day negative emotion. Affective Science. 2020;1(1):20–27. doi: 10.1007/s42761-019-00001-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: Does happiness lead to success? [Meta-Analysis Research Support, Non-U.S. Gov't] Psychological Bulletin. 2005;131(6):803–855. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- McMakin DL, Olino TM, Porta G, Dietz LJ, Emslie G, Clarke G, Wagner KD, Asarnow JR, Ryan ND, Birmaher B. Anhedonia predicts poorer recovery among youth with selective serotonin reuptake inhibitor treatment–resistant depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(4):404–411. doi: 10.1016/j.jaac.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz, J., Carrico, A., Cohn, M., Duncan, L., Bussolari, C., Layous, K., Hult, J., Brousset, A., Cotten, P., & Maurer, S. (2014). Randomized controlled trial of a positive affect intervention to reduce stress in people newly diagnosed with HIV; protocol and design for the IRISS study. 2014(6), 85–100. 10.2147/OAJCT.S64645
- Moskowitz JT, Carrico AW, Duncan LG, Cohn MA, Cheung EO, Batchelder A, Martinez L, Segawa E, Acree M, Folkman S. Randomized controlled trial of a positive affect intervention for people newly diagnosed with HIV. Journal of Consulting and Clinical Psychology. 2017;85(5):409–423. doi: 10.1037/ccp0000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JT, Addington EA, Cheung EO. Positive pathways to health. General Hospital Psychiatry. 2019;61:136–138. doi: 10.1016/j.genhosppsych.2019.11.001. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT, Cheung EO, Snowberg KE, Verstaen A, Merrilees J, Salsman JM, Dowling GA. Randomized controlled trial of a facilitated online positive emotion regulation intervention for dementia caregivers. Health Psychology. 2019;38(5):391–402. doi: 10.1037/hea0000680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JT, Addington EL, Shiu E, Bassett SM, Schuette S, Kwok I, Grote V, Freedman ME, Leykin Y, Saslow LR, Cohn MA, Cheung EO. Facilitator contact, discussion boards, and virtual badges as adherence enhancements to a web-based, self-guided, positive psychological intervention for depression: Randomized controlled trial. Journal of Medical Internet Research. 2021;23(9):e25922. doi: 10.2196/25922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JT, Cheung EO, Freedman M, Fernando C, Zhang MW, Huffman JC, Addington EL. Measuring positive emotion outcomes in positive psychology interventions: A literature review. Emotion Review. 2021;13(1):60–73. [Google Scholar]
- Ong AD, Burrow AL. Affective reactivity to daily racial discrimination as a prospective predictor of depressive symptoms in African American graduate and postgraduate students. Development and Psychopathology. 2018;30(5):1649–1659. doi: 10.1017/S0954579418000950. [DOI] [PubMed] [Google Scholar]
- Pizzagalli DA. Depression, stress, and anhedonia: Toward a synthesis and integrated model. Annual Review of Clinical Psychology. 2014;10:393–423. doi: 10.1146/annurev-clinpsy-050212-185606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychological Methods. 2010;15(3):209. doi: 10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- Rackoff GN, Newman MG. Reduced positive affect on days with stress exposure predicts depression, anxiety disorders, and low trait positive affect 7 years later. Journal of Abnormal Psychology. 2020;129(8):799. doi: 10.1037/abn0000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Schueller, S., Kashdan, T., & Parks, A. (2014). Synthesizing positive psychological interventions: Suggestions for conducting and interpreting meta-analyses. International Journal of Wellbeing, 4(1).
- Seligman, M. E. (2006). Positive psychotherapy. The American psychologist. http://ft.csa.com/ids70/resolver.php?sessid=b1cbbp7qdmq281kpi0c93kvn16&server=csaweb105v.csa.com&check=07d0c0226283e61bc305d0441409d379&db=psycarticles-set-c&key=AMP%2F61%2Famp_61_8_774&mode=pdf [DOI] [PubMed]
- Silton RL, Kahrilas IJ, Skymba HV, Smith J, Bryant FB, Heller W. Regulating positive emotions: Implications for promoting well-being in individuals with depression. Emotion. 2020;20(1):93. doi: 10.1037/emo0000675. [DOI] [PubMed] [Google Scholar]
- Spijker J, Bijl R, De Graaf R, Nolen W. Determinants of poor 1-year outcome of DSM-III-R major depression in the general population: Results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Acta Psychiatrica Scandinavica. 2001;103(2):122–130. doi: 10.1034/j.1600-0447.2001.103002122.x. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Elzinga B, Roelofs K, Hovens JG, van Oppen P, Zitman FG, Penninx BW. The effects of neuroticism, extraversion, and positive and negative life events on a one-year course of depressive symptoms in euthymic previously depressed patients versus healthy controls. The Journal of Nervous and Mental Disease. 2011;199(9):684–689. doi: 10.1097/NMD.0b013e318229d21f. [DOI] [PubMed] [Google Scholar]
- van Straten A, Hill J, Richards DA, Cuijpers P. Stepped care treatment delivery for depression: A systematic review and meta-analysis. Psychological Medicine. 2015;45(2):231–246. doi: 10.1017/S0033291714000701. [DOI] [PubMed] [Google Scholar]
- Vanderlind WM, Millgram Y, Baskin-Sommers AR, Clark MS, Joormann J. Understanding positive emotion deficits in depression: From emotion preferences to emotion regulation. Clinical Psychology Review. 2020;76:101826. doi: 10.1016/j.cpr.2020.101826. [DOI] [PubMed] [Google Scholar]
- Vilagut G, Forero CG, Barbaglia G, Alonso J. Screening for depression in the general population with the Center for Epidemiologic Studies Depression (CES-D): A systematic review with meta-analysis. PLoS One. 2016;11(5):e0155431. doi: 10.1371/journal.pone.0155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarroel, M., & Terlizzi, E. (2020). Symptoms of depression among adults: United States, 2019. [PubMed]
- Wen JH, Lyubomirsky S, Sin NL. Positive Psychological Science. Routledge; 2020. Positive activity interventions targeted to improve depressive symptoms; pp. 225–245. [Google Scholar]
- Zautra A, Smith B, Affleck G, Tennen H. Examinations of chronic pain and affect relationships: Applications of a dynamic model of affect. Journal of Consulting and Clinical Psychology. 2001;69(5):786–795. doi: 10.1037//0022-006x.69.5.786. [DOI] [PubMed] [Google Scholar]
- Zeng X, Chiu CP, Wang R, Oei TP, Leung FY. The effect of loving-kindness meditation on positive emotions: A meta-analytic review. Frontiers in Psychology. 2015;6:1693. doi: 10.3389/fpsyg.2015.01693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhaoyang R, Scott SB, Smyth JM, Kang J-E, Sliwinski MJ. Emotional responses to stressors in everyday life predict long-term trajectories of depressive symptoms. Annals of Behavioral Medicine. 2020;54(6):402–412. doi: 10.1093/abm/kaz057. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available here: https://osf.io/d2v6m/?view_only=894e78477476477d927361a82685b5e9.