Highlights
-
-
Proprioceptive accuracy is an important aspect in the evaluation of sensorimotor functioning.
-
-
No standard, widely accepted assessment exists.
-
-
In this review, we found that different aspects of proprioception (i.e., the perception of joint position, movement and movement extent, trajectory, velocity and the sense of force, muscle tension, weight, and size) can be measured with different paradigms.
-
-
As different tests do not necessarily measure the same construct, the appropriate aspect should be measured.
Keywords: Assessment, Kinesthesia, Motor control, Proprioception, Proprioceptive accuracy
Abstract
Background
Proprioceptive accuracy refers to the individual's ability to perceive proprioceptive information, that is, the information referring to the actual state of the locomotor system, which originates from mechanoreceptors located in various parts of the locomotor system and from tactile receptors located in the skin. Proprioceptive accuracy appears to be an important aspect in the evaluation of sensorimotor functioning; however, no widely accepted standard assessment exists. In this systematic review, our goal was to identify and categorize different methods that are used to assess different aspects of proprioceptive accuracy.
Methods
A literature search was conducted in 5 different databases (PubMed, SPORTDiscus, PsycINFO, ScienceDirect, and SpringerLink).
Results
Overall, 1139 scientific papers reporting 1346 methods were included in this review. The methods assess 8 different aspects of proprioception: (a) the perception of joint position, (b) movement and movement extent, (c) trajectory, (d) velocity, and the sense of (e) force, (f) muscle tension, (g) weight, and (h) size. They apply various paradigms of psychophysics (i.e., the method of adjustment, constant stimuli, and limits).
Conclusion
As the outcomes of different tasks with respect to various body parts show no associations (i.e., proprioceptive accuracy is characterized by site-specificity and method-specificity), the appropriate measurement method for the task needs to be chosen based on theoretical considerations and/or ecological validity.
1. Introduction
Optimal motor control requires proprioceptive information, which originates from mechanoreceptors located within the locomotor system.1 To experience proprioception, the brain processes input from proprioceptors (i.e., muscle spindles, which are located in the muscle belly and process information about the length and rate of stretch, and Golgi tendon organs, which pass on information about tension and, consequently, the force of contraction) and mechanoreceptors (i.e., Pacinian, Ruffini, Merkel, and Meissner corpuscle end-organs) located in the skin and ligaments as well as in joint capsules.2 Moreover, not only afferent but efferent signals (i.e., efference copy of the motor command, sense of effort) contribute to the sensation.2 Normally developed humans are able to automatically process, integrate, and consciously perceive force, effort, weight and their body position, movement, and muscle tension based on this type of (proprioceptive) information3 and use it for goal-oriented motor behavior.4
Proprioceptive accuracy refers to the individual's ability to perceive proprioceptive information.5,6 This ability is associated with important aspects of motor control and performance. For example, proprioceptive accuracy is positively associated with sport achievement in elite athletes.7 Moreover, better proprioceptive accuracy in the elbow joint was found to be related to better throwing performance in basketball,8 darts,9 and water-polo.10 Concerning the negative aspects, worse proprioceptive accuracy predicts a higher chance of getting injured;11 also, as proprioceptive accuracy deteriorates with aging,5 it may contribute to an increased risk of falls.12 It has also been shown that physically active individuals are characterized by better proprioceptive accuracy, and physical activity can compensate for the negative impact of aging on proprioceptive accuracy.13 Proprioceptive training (i.e., “an intervention that targets the improvement of proprioceptive function”, (p2)14 often including proprioceptive accuracy) is an efficient method to prevent injuries and improve motor performance.14
Based on the aforementioned associations, proprioceptive accuracy appears to be an important characteristic in the evaluation of sensorimotor functioning, for example, for sport selection7 or for assessing the risk of injury and falls.11,15, 16, 17 Also, measuring the change in proprioceptive accuracy is often used to evaluate the effectiveness of different interventions, for example, various surgical outcomes,18 rehabilitation,19 and warming-up20 techniques.
There is a wide variety of methods that have been developed to measure various aspects of proprioceptive accuracy. Hillier and colleagues21 identified 3 clusters of methods: joint position detection, passive motion detection, and passive motion direction discrimination. Starting from a different point of view, Han and colleagues6 described 3 paradigms based on the classical methods developed for psychophysical experiments:22 (a) joint position reproduction test, based on the method of adjustment, that is, participants have to adjust the level of a stimulus to a reference; (b) active movement extent discrimination assessment, based on the method of constant stimuli, that is, the stimuli are presented in pairings, and participants have to compare them; and (c) threshold to detection of passive motion, based on the method of limits, that is, participants have to indicate when they perceive the appearance or disappearance of a stimulus.6,22 An important limitation of these reviews is their relatively narrow definition of proprioception. Han and colleagues6 defined proprioceptive accuracy as “an individual's ability to integrate the sensory signals from mechanoreceptors to thereby determine body segment positions and movements in space” (p81).6 This account does not take into consideration certain important aspects of proprioception, such as the perception of heaviness, force, and muscle tension.2 Similarly, the review of Hillier and colleagues21 also included only a narrow range of methods, namely: joint position detection, passive motion detection threshold, and passive motion direction detection. Our recent review applies a more inclusive approach to proprioception than the previous papers.6,21 A new review is also reasonable because of the growing literature on proprioception and the need to cover new tests developed since the publication of previous reviews.
The primary goal of the present systematic review was to identify and categorize the methods developed and used to measure proprioceptive accuracy in a comprehensive way by taking into consideration all important aspects of proprioception (i.e., sense of joint position, movement and movement extent, force, and heaviness). In doing this, this paper will help practitioners and researchers to find the method that best suits their needs for the assessment of proprioceptive accuracy.
2. Methods
The study was registered at PROSPERO Measurement of proprioceptive accuracy: a systematic literature review (CRD42020209136). While conducting this review, we followed the recommendations of the Preferred Reporting Items for Systematic Reviews and Metal-Analysis (PRISMA) statement.23 Search strategy characteristics and study inclusion/exclusion criteria are reported in Table 1. The abstracts and titles of the articles were searched in 5 different databases (PubMed, SPORTDiscus, PsycINFO, ScienceDirect, and SpringerLink), including every available article (i.e., not only free text articles), without a restriction to publication date. The search was conducted on November 11, 2020. Proprioceptive accuracy was defined as the acuity of perception of proprioceptive information, that is, the information referring to the actual state of the locomotor system. It includes the processing of input from proprioceptors located in various parts of the locomotor system and from tactile receptors on the skin. It does not include visual and vestibular information. To decide on inclusion, 2 independent authors (KS and ÁH) read the titles and abstracts of the papers as a first step. An article was excluded in this step only if both authors deemed it ineligible. In the next step, ÁH read the full text articles and made the final decision on inclusion. In case of any ambiguity, FK and EF decided on the inclusion of the article.
Table 1.
Characteristics of the literature search.
| Keyword for literature search | (“propriocept*”) AND (“accuracy” OR “acuity” OR “ability” OR “abilities” OR “awareness” OR “sensibility” OR “sensitivity” OR “weight discrimination” OR “movement discrimination” OR “movement detection” OR “joint position sense” OR “force sense” OR “movement sense” OR “movement perception” OR “force perception”) |
| Database | PubMed, SPORTDiscus, PsycINFO, ScienceDirect, and SpringerLink |
| Language | English only |
| Document type | Peer-reviewed empirical article |
| Inclusion criteria | Population: any human |
| Intervention: not necessary | |
| Comparison: not necessary | |
| Outcome: objective measure of proprioceptive accuracy | |
| Exclusion criteria | Dissertations, theoretical papers, conference materials, non-English articles |
3. Results
3.1. Included studies
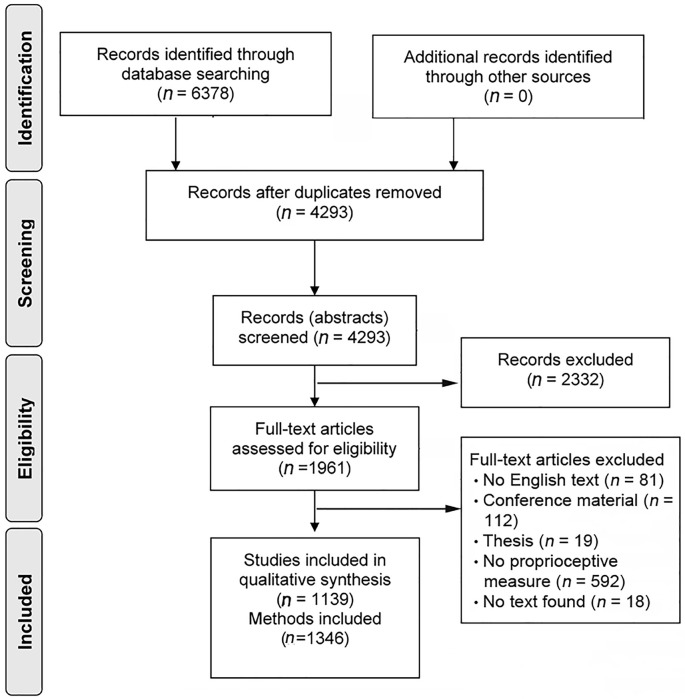
Overall, 6378 articles were identified in the database research. After removing the duplicates, 4293 remained. After reading the titles/abstracts, a further 2332 articles were excluded because they did not meet the inclusion criteria. Based on the full texts of the remaining 1961 articles, a further 822 studies were excluded. In total, 1139 studies were included in the review. Following this, 1346 proprioceptive accuracy measurements were identified in a total of 1139 papers (Fig. 1); in a number of papers, multiple methods for the assessment of proprioceptive accuracy were used in the same sample. After that, measurement techniques were clustered based on their approach to measurement (Table 2). We used 2 main criteria to categorize the methods: what aspect of proprioceptive accuracy was assessed and what psychophysical approach was applied, which could be (a) the method of adjustment, where participants have to adjust the level of a stimulus to a reference; (b) the constant methods, which include both the method of constant stimuli, where participants have to judge standard and comparison stimuli presented in pairings, and the method of single stimuli, where participants judge a single stimulus presented alone; or (c) the method of limits, where participants have to indicate the appearance or disappearance of a stimulus. The full list of included articles is available at: https://osf.io/8f2zn/.
Fig. 1.
Selection process of the articles, based on Moher and colleagues.64
Table 2.
Summary table of the proprioceptive accuracy measurement techniques.
| Aspect of proprioception | Method of adjustment | Method of constant stimuli | Method of limits |
|---|---|---|---|
| Joint position sense | Joint Position Reproduction, Pointing to Proprioceptive Target | Joint Position Discrimination | Threshold to Detection of Passive Motion |
| Movement sense | Movement Reproduction | Movement Discrimination | |
| Trajectory sense | Trajectory Reproduction | N/A | |
| Velocity sense | Velocity Reproduction | Velocity Discrimination | |
| Force sense | Force Reproduction, Keep Force Level | Force Discrimination | N/A |
| Muscle tension sense | Muscle Tension Reproduction | N/A | N/A |
| Weight sense | N/A | Weight Discrimination | N/A |
| Size sense | N/A | Size Discrimination | N/A |
Abbreviation: N/A = no method is available.
3.2. Proprioceptive accuracy measurement techniques
3.2.1. Method of adjustment
Eight different types of proprioceptive accuracy measurements using the method of adjustment were identified.
Joint Position Reproduction (n = 836). Participants have 1 or more joints of their body moved to a target position. Then they are asked to reproduce the position of the joint(s) as accurately as possible. In different versions of this task, movement can be active or passive, and the reproduction may happen with the same or with the contralateral joint (see also the discussion).
Pointing to Proprioceptive Target (n = 42). One of the body parts is set to a target position. One has to point or reach to the position of the body part as accurately as possible.
Movement Reproduction (n = 21). One of the body parts is moved through a given trajectory, with a given velocity, to a given endpoint. Participants are required to reproduce the trajectory, the speed, and the endpoint of the movement as accurately as possible.
Trajectory Reproduction (n = 2). A body part is moved along a given trajectory. Participants have to reproduce the trajectory of the movement. This can happen with the same or with the contralateral joint.
Velocity Reproduction (n = 9). A body part is set to move with a given velocity. The task of the participant is to reproduce the speed with the same or with the contralateral body part.
Force Reproduction (n = 76). The participant is guided to produce a certain level of force with a muscle or muscle group. After production, they have to reproduce the same force with the same or with the contralateral muscle.
Keep Force Level (n = 6). Participants have to produce a given amount of (submaximal) force and keep it on the same level.
Muscle Tension Reproduction (n = 1). The participant is asked to produce a given level of muscle tension with a muscle or muscle group. After the production, one has to reproduce the same level of muscle tension as accurately as possible.
3.2.2. Method of constant stimuli
Six different proprioceptive accuracy measurement types were identified that were based on the method of constant stimuli.
Joint Position Discrimination (n = 81). Participants have to compare 2 joint positions and decide whether these were the same or different (Note: The Active Movement Extent Discrimination Apparatus,6 which presented a single stimuli for judgement in each trial, was also categorized as a Joint Position Discrimination test).
Movement Discrimination (n = 6). Participants have to compare 2 movements (with a given trajectory, velocity, and endpoint) and decide if these were the same or different.
Velocity Discrimination (n = 8). Participants have to perform 2 movement velocities and decide if these were the same or different.
Force Discrimination (n = 5). Participants have to produce a given level of force twice and decide if these were the same or different level of forces.
Weight Discrimination (n = 19). Participants are presented with 2 objects and have to decide if these were of the same or different weight.
Size Discrimination (n = 3). Participants are presented with 2 objects and have to decide if these were of the same or different size.
3.2.3. Method of limits
One widely used proprioceptive accuracy measurement technique using the method of limits was identified.
Threshold to Detection of Passive Motion (n = 231). One body part of the participant is moved passively. The task is to give a signal as soon as the displacement is perceived. This paradigm is based on the ascending method of limits (i.e., the level of stimuli gradually increases until perceived), whereas we did not find any example of the descending method (i.e., level of stimulus gradually decreases until perceived) used to assess proprioceptive accuracy.
4. Discussion
In this review, we identified and categorized the existing methods used for the assessment of proprioceptive accuracy. Also, we identified 8 different aspects or “senses” of proprioception (Table 2): the ability to perceive (a) joint position, (b) movement and movement extent, (c) trajectory, and (d) velocity, the level of (e) force, (f) muscle tension, (g) weight, and (h) size of different objects based on proprioceptive information. These aspects can be measured with the classical methods of psychophysics, that is, the method of adjustment, the method of constant stimuli, and the method of limits.
Proprioceptive accuracy assessment can be operationalized by taking different approaches and different paradigms. A common misconception in the literature is that results obtained with the use of one particular method with respect to one particular body part (e.g., joint, muscle) can be generalized. In other words, it is (often implicitly) assumed that a generalizable proprioceptive accuracy exists and that each test measures this general ability. If this would be the case, a strong association between results obtained with different tests for different body parts should exist. In other words, the best performers in one particular test (e.g., Joint Position Reproduction) with respect to one particular body part (e.g., elbow) would probably be the best performers in another test (e.g., Threshold to Detection of Passive Motion) assessing another body part (e.g., knee). Empirical findings, however, do not support the existence of such a strong relationship. In fact, proprioceptive accuracy is characterized by both site-specificity and method-specificity. Table 3 summarizes the studies investigating the relationship between different tests; none of them reported a significant correlation. The existence of such a discordance is further supported by studies revealing test-specific differences in certain proprioceptive abilities. For example, Barrack and colleagues24 found that dancers perform worse than controls in Joint Position Reproduction test but are better at Threshold to Detection of Passive Motion with respect to the proprioceptive accuracy of the knee joint. It was also reported that Force Reproduction test, but not Joint Position Reproduction test is related to ankle instability index25 and ankle stiffness.26 Another example is that deficits in motor functioning, such as walking disability, sensory disturbance, and central motor conduction time, were only associated with proprioceptive accuracy assessed with the Joint Position Reproduction test and not with that measured with the Threshold to Detection of Passive Motion test in compressive neuropathy.27 Finally, experimentally-induced pain influenced the outcome of the Threshold to Detection of Passive Motion test, but did not affect participants’ performance in the Joint Position Reproduction test.28
Table 3.
Summary table of studies investigating the association between different tests of proprioceptive accuracy. None of the studies found a significant association.
| Author (year) | Test |
|---|---|
| Grob et al. (2002)57 | Joint Position Reproduction, Threshold to Detection of Passive Motion |
| Janwantanakul et al. (2003)58 | Joint Position Reproduction, Threshold to Detection of Passive Motion |
| de Jong et al. (2005)31 | Joint Position Discrimination, Threshold to Detection of Passive Motion |
| Elangovan et al. (2014)59 | Joint Position Discrimination, Joint Position Reproduction |
| Li et al. (2016)60 | Joint Position Reproduction, Threshold to Detection of Passive Motion, Force Reproduction |
| Nagai et al. (2016)36 | Joint Position Reproduction, Velocity Reproduction, Threshold to Detection of Passive Motion, Force Reproduction |
| Niespodziński et al. (2018)61 | Joint Position Reproduction, Force Reproduction |
| Yang et al. (2020)62 | Movement Discrimination, Joint Position Reproduction |
| Horváth et al. (2021)63 | Joint Position Reproduction, Weight Discrimination |
Also, evidence shows that results with respect to one body part may not be generalized to others. With respect to the Joint Position Discrimination (AMEDA) test, there is a strong correlation between the same joints on the 2 body sides, but no association between different joints.29,30 Moreover, lack of association can be observed in many cases within the same test and joint too. For example, no association was found between detection threshold when the limb is moved with different speeds.31 Finally, results may be joint-position specific; for example, people with functional ankle instability showed position-specific deficits in a Joint Position Reproduction task.32
Another consideration is related to the question of how performance in the tests should be scored. Most of the methods allow the use of many performance scores. For example, for the method of adjustment, absolute error refers to the mean absolute difference between the reference and the reproduced stimuli, constant error refers to the signed difference (indicating systematic bias in judgements), and variable error refers to the standard deviation of the error score (indicating dispersion around the constant error).33, 34, 35 In a similar vein, the method of constant stimuli allows the use of the sensitivity (proportion of correct judgements when the 2 stimuli differ) and specificity (proportion of correct judgements when the 2 stimuli are the same) indices, and the Just Noticeable Difference (the lowest level of difference that one can detect, for example, at least 50% of the time). There is no clear agreement in the literature how these tests should be scored; even the correlation between the various indices is rarely reported. From a more practical point of view, the use of multiple indices often makes the comparison of findings of various studies impossible.
Altogether, these issues (i.e., test- and site-specificity and the lack of agreement on how tests should be scored) imply that when using the term proprioceptive accuracy, the test used, the score used to evaluate the test, and the joint measured always need to be specified. As proprioceptive accuracy is not a general ability, it cannot be assessed with the use of a single test,31 and so one should always choose a method that best suits the research or practical question at hand.36 For researchers, an important task for the future is to find the best method to measure proprioceptive accuracy. One important consideration is ecological validity, for example, how well different tests reflect the effects of injury and expertise.37,38
Moreover, there are other important factors that should be taken into consideration when choosing the appropriate test. Some tests inherently require active effort from the participants (e.g., force reproduction and discrimination, muscle tension reproduction, weight discrimination), but in other cases (e.g., joint position reproduction) the test can be based on passive movement only. For certain patient groups with movement disorders, only the passive movement versions are applicable. Because of the tight interaction between the input and output aspects of motor control,39,40 active motion involves the processing of both afferent (e.g., the feedback from muscle spindles) and efferent (i.e., the efference copy of motor command) signals. Therefore, people tend to be more accurate when active muscle activity increases, for example, by allowing active motion41 or by increasing shoulder elevation angle42 and weight bearing.43 Weight bearing can also compensate for the negative effect of experimentally induced joint effusion.44 From the viewpoint of external (ecological) validity, tests that involve active motion should be preferred, as they better reflect the individual's performance under everyday circumstances. Important for the choice of an appropriate test is that some patients with movement disorders may not be able to move the limb or joint up to a specific position even though it may have been possible passively (e.g., the affected upper or lower limb in patients with unilateral stroke), which will affect the results of the proprioceptive accuracy test dramatically. As such, it has to be considered whether the reproduction/comparison happens with the ipsilateral or with the contralateral joint. The ipsilateral version requires memory while the contralateral version requires interhemispheric transfer,5 so in patients with significant memory impairment, the ipsilateral version is not preferred. In other words, additional abilities and features beyond the processing of proprioceptive signal(s) can substantially impact performance. Another important factor that can influence the outcome of the assessment is the measured body side, as there might be differences between the dominant and subdominant limb in the processing of proprioceptive information.29,45, 46, 47, 48
The approach to proprioception and proprioceptive accuracy used in this systematic review paper is broader than that of previous literature reviews.6,21 This enabled us to explore methods not included in those reviews. It is worth noting that our definition excluded signals that do not originate in the locomotor system or the skin (and related efferent signals) but that might play an important role in the perception of our body, most importantly the visual modality. Also, because of the definition used, only methods of assessment that require the subject to consciously be aware of proprioceptive information were included. These factors may limit the ecological validity of proprioceptive accuracy tests. To reach cognitive perception of proprioceptive accuracy, proprioceptive and related somatosensory signals are processed through the conscious relay pathways (i.e., dorsal column/medial lemniscus system).49 However, in activities of daily life, movement regulation is a dominantly non-conscious (automatic) process that does not require conscious perception of proprioceptive signals.50 Proprioceptive information that does not reach conscious awareness is forwarded through the spinal reflex pathway or the spinocerebellar tract to contribute to automatic postural adjustments and balance control.51 As indicated by previous neuro-imaging research, central processing of ankle proprioception can predict balance performance in younger and older adults.52 In other words, ankle proprioception will provide important non-conscious feedback regarding body sway, which is crucial for restoring or maintaining a state of balance. Hence, some researchers incorporate “sense of balance” in the definition of proprioception.3 Following this logic, a balance task can be used as an alternative method to (indirectly) assess the functional ability to use non-conscious proprioception (to keep a state of balance), especially in situations where visual information is eliminated (i.e., where participants are blindfolded).53 In this way, some researchers attribute increased postural sway (e.g., Romberg test) to loss of proprioceptive sensation.54 However, it is important to note that balance control is a complex process depending on multiple sensorimotor mechanisms.55 So, in this way, it can be stated that an increment in postural sway cannot be attributed exclusively to a reduction in proprioceptive information as other sensory feedback systems can play an important role as well (e.g., the vestibular system and other somatosensory senses, such as plantar cutaneous foot sensation), not to speak of the required motor functions.
This review is not without shortcomings. A single author made the decision about the final inclusion of the articles at the full-text stage, which could lead to biased selection. Also, articles reporting methods that contain the search terms may be overrepresented.
To choose the appropriate method to measure proprioceptive accuracy, the first step is to decide which aspect of proprioception one wants to assess: the sense of joint position, trajectory, speed, movement and movement extent, force, muscle tension, weight, or size. For researchers, theoretical consideration may guide this decision, while for practitioners, ecological validity may be the most important factor. It is important to consider whether a passive test, where participants do not have to conduct active movement or effort, or an active test is more appropriate. In the former case, afferent sensory signals play a more dominant role, while in the latter case, efferent signals also contribute to perception. However, it is also important to note that these systems (afferent and efferent) may not be completely separable.39,40 In specific patient populations, researchers and practitioners should take into account the motor capacity, range of motion, and muscle strength of the limb or joint of interest and adapt the test to the needs of the patient. Additionally, in patients with severe memory impairment, a contralateral version is recommended. Different aspects can be measured with the method of adjustment, method of constant stimuli, or with the method of limits.6,22 Besides the decision regarding the measurement method, the relevant joint and body side should be measured with an appropriate stimulus intensity (i.e., joint position, speed, trajectory, force, contraction level, weight, or size). Importantly, one should be aware that proprioceptive accuracy is body site- and test-specific, meaning that results obtained with a given test are not generalizable for other tests nor for other joints. Accuracy might also be specific to the target stimuli (e.g., speed of motion, target joint position). Better understanding of the benefits and shortcomings of different paradigms can also be helpful in the development of novel tests meant to assess new aspects of proprioception. For example, the loss of proprioceptive accuracy over long-duration spaceflights to Macaulay et al.56 suggests that astronauts with good initial proprioceptive acuity should be selected for the journey. An important practical question is, however, how their proprioceptive accuracy should be measured.
Acknowledgments
Áron Horváth was supported by the ÚNKP-20-3 New National Excellence Program of the Ministry for Innovation and Technology from the source of the National Research, Development and Innovation Fund (ÚNKP-20-3-II-ELTE-163). Nina Jacobs was supported by the Fonds voor Wetenschappelijk Onderzoek–Vlaanderen (FWO) Research Foundation Flanders (11M2622N) and the Special Research Fund (Het Bijzonder Onderzoeksfonds, BOF) of Hasselt University (BOF19KP08).
Authors’ contributions
ÁH took part in designing the study, in selection process, and wrote the first draft of the manuscript; EF took part in designing the study; KS took part in the selection process; NJ wrote sections of the manuscript; PM wrote sections of the manuscript; FK took part in designing the study and wrote sections of manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials
References
- 1.Riemann BL, Lephart SM. The sensorimotor system, Part II: The role of proprioception in motor control and functional joint stability. J Athl Train. 2002;37:80–84. [PMC free article] [PubMed] [Google Scholar]
- 2.Proske U, Gandevia SC. The proprioceptive senses: Their roles in signaling body shape, body position and movement, and muscle force. Physiol Rev. 2012;92:1651–1697. doi: 10.1152/physrev.00048.2011. [DOI] [PubMed] [Google Scholar]
- 3.Stillman BC. Making sense of proprioception: The meaning of proprioception, kinaesthesia and related terms. Physiotherapy. 2002;88 667–6. [Google Scholar]
- 4.Sarlegna FR, Sainburg RL. The roles of vision and proprioception in the planning of reaching movements. Adv Exp Med Biol. 2009;629 doi: 10.1007/978-0-387-77064-2_16. 317–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goble DJ. Proprioceptive acuity assessment via joint position matching: From basic science to general practice. Physical Therapy. 2010;90:1176–1184. doi: 10.2522/ptj.20090399. [DOI] [PubMed] [Google Scholar]
- 6.Han J, Waddington G, Adams R, Anson J, Liu Y. Assessing proprioception: A critical review of methods. J Sport Health Sci. 2016;5:80–90. doi: 10.1016/j.jshs.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han J, Waddington G, Anson J, Adams R. Level of competitive success achieved by elite athletes and multi-joint proprioceptive ability. J Sci Med Sport. 2015;18:77–81. doi: 10.1016/j.jsams.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 8.Sevrez V, Bourdin C. On the role of proprioception in making free throws in basketball. Res Q Exerc Sport. 2015;86:274–280. doi: 10.1080/02701367.2015.1012578. [DOI] [PubMed] [Google Scholar]
- 9.Feng J, Hung TM, Huang R, Hou S, Ren J. Role of proprioception in slow and rapid movements. Percept Mot Skills. 2020;127:281–298. doi: 10.1177/0031512519895632. [DOI] [PubMed] [Google Scholar]
- 10.Hams AH, Evans K, Adams R, Waddington G, Witchalls J. Throwing performance in water polo is related to in-water shoulder proprioception. J Sports Sci. 2019;37:2588–2595. doi: 10.1080/02640414.2019.1648987. [DOI] [PubMed] [Google Scholar]
- 11.Cameron M, Adams R, Maher C. Motor control and strength as predictors of hamstring injury in elite players of Australian football. Phys Therapy Sport. 2003;4:159–166. [Google Scholar]
- 12.Wingert JR, Welder C, Foo P. Age-related hip proprioception declines: Effects on postural sway and dynamic balance. Arch Phys Med Rehabil. 2014;95:253–261. doi: 10.1016/j.apmr.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 13.Ribeiro F, Oliveira J. Aging effects on joint proprioception: The role of physical activity in proprioception preservation. Eur Rev Aging Phys Act. 2007;4:71–76. [Google Scholar]
- 14.Aman JE, Elangovan N, Yeh IL, Konczak J. The effectiveness of proprioceptive training for improving motor function: A systematic review. Front Hum Neurosci. 2015;8:1075. doi: 10.3389/fnhum.2014.01075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoang PD, Baysan M, Gunn H, et al. Fall risk in people with MS: A Physiological Profile Assessment study. Mult Scler J Exp Transl Clin. 2016;2 doi: 10.1177/2055217316641130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994;42:1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- 17.Witchalls J, Blanch P, Waddington G, Adams R. Intrinsic functional deficits associated with increased risk of ankle injuries: A systematic review with meta-analysis. Br J Sports Med. 2012;46:515–523. doi: 10.1136/bjsports-2011-090137. [DOI] [PubMed] [Google Scholar]
- 18.Isaac SM, Barker KL, Danial IN, Beard DJ, Dodd CA, Murray DW. Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompartmental arthroplasty. Knee. 2007;14:212–217. doi: 10.1016/j.knee.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Edmonds G, Kirkley A, Birmingham TB, Fowler PJ. The effect of early arthroscopic stabilization compared to nonsurgical treatment on proprioception after primary traumatic anterior dislocation of the shoulder. Knee Surg Sports Traumatol Arthrosc. 2003;11:116–121. doi: 10.1007/s00167-003-0346-y. [DOI] [PubMed] [Google Scholar]
- 20.Subasi SS, Gelecek N, Aksakoglu G. Effects of different warm-up periods on knee proprioception and balance in healthy young individuals. J Sport Rehabil. 2008;17:186–205. doi: 10.1123/jsr.17.2.186. [DOI] [PubMed] [Google Scholar]
- 21.Hillier S, Immink M, Thewlis D. Assessing proprioception: A systematic review of possibilities. Neurorehabil Neural Repair. 2015;29:933–949. doi: 10.1177/1545968315573055. [DOI] [PubMed] [Google Scholar]
- 22.Gescheider GA. 3rd ed. Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 1997. Psychophysics: The fundamentals; p. 435. [Google Scholar]
- 23.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barrack RL, Skinner HB, Cook SD, Haddad RJJ. Effect of articular disease and total knee arthroplasty on knee joint-position sense. J Neurophysiol. 1983;50:684–687. doi: 10.1152/jn.1983.50.3.684. [DOI] [PubMed] [Google Scholar]
- 25.Docherty CL, Arnold BL, Hurwitz S. Contralateral force sense deficits are related to the presence of functional ankle instability. J Orthop Res. 2006;24:1412–1419. doi: 10.1002/jor.20195. [DOI] [PubMed] [Google Scholar]
- 26.Docherty CL, Arnold BL, Zinder SM, Granata K, Gansneder BM. Relationship between two proprioceptive measures and stiffness at the ankle. J Electromyogr Kinesiol. 2004;14:317–324. doi: 10.1016/S1050-6411(03)00035-X. [DOI] [PubMed] [Google Scholar]
- 27.Okuda T, Ochi M, Tanaka N, Nakanishi K, Adachi N, Kobayashi R. Knee joint position sense in compressive myelopathy. Spine (Phila Pa 1976) 2006;31:459–462. doi: 10.1097/01.brs.0000199956.11646.5b. [DOI] [PubMed] [Google Scholar]
- 28.Sole G, Osborne H, Wassinger C. The effect of experimentally-induced subacromial pain on proprioception. Man Ther. 2015;20:166–170. doi: 10.1016/j.math.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 29.Han J, Anson J, Waddington G, Adams R. Proprioceptive performance of bilateral upper and lower limb joints: Side-general and site-specific effects. Exp Brain Res. 2013;226:313. doi: 10.2466/pms.1999.89.3.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Waddington G, Adams R. Ability to discriminate movements at the ankle and knee is joint specific. Perceptzral Mot Skills. 1999;89:1037–1041. doi: 10.2466/pms.1999.89.3.1037. [DOI] [PubMed] [Google Scholar]
- 31.de Jong A, Kilbreath SL, Refshauge KM, Adams R. Performance in different proprioceptive tests does not correlate in ankles with recurrent sprain. Arch Phys Med Rehabil. 2005;86:2101–2105. doi: 10.1016/j.apmr.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 32.Yokoyama S, Matsusaka N, Gamada K, Ozaki M, Shindo H. Position-specific deficit of joint position sense in ankles with chronic functional instability. J Sports Sci Med. 2008;7:480–485. [PMC free article] [PubMed] [Google Scholar]
- 33.Schutz RW, Roy EA. Absolute Error. J Mot Behav. 1973;5:141–153. doi: 10.1080/00222895.1973.10734959. [DOI] [PubMed] [Google Scholar]
- 34.Boisgontier MP, Olivier I, Chenu O, Presbypropria Nougier V. The effects of physiological ageing on proprioceptive control. Age (Dordr) 2012;34:1179–1194. doi: 10.1007/s11357-011-9300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goble DJ, Aaron MB, Warschausky S, Kaufman JN, Hurvitz EA. The influence of spatial working memory on ipsilateral remembered proprioceptive matching in adults with cerebral palsy. Exp Brain Res. 2012;223:259–269. doi: 10.1007/s00221-012-3256-8. [DOI] [PubMed] [Google Scholar]
- 36.Nagai T, Allison KF, Schmitz JL, Sell TC. Conscious proprioception assessments in sports medicine: How individuals perform each submodality? Dover, DE: SM Group, SM Online Scientific Resources. 2016 [Google Scholar]
- 37.Laboute E, Verhaeghe E, Ucay O, Minden A. Evaluation kinaesthetic proprioceptive deficit after knee anterior cruciate ligament (ACL) reconstruction in athletes. J Exp Orthop. 2019;6:6. doi: 10.1186/s40634-019-0174-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Steinberg N, Adams R, Ayalon M, Dotan N, Bretter S, Waddington G. Recent ankle injury, sport participation level, and tests of proprioception. J Sport Rehabil. 2019;28:824–830. doi: 10.1123/jsr.2018-0164. [DOI] [PubMed] [Google Scholar]
- 39.Cullen KE. Sensory signals during active versus passive movement. Curr Opin Neurobiol. 2004;14:698–706. doi: 10.1016/j.conb.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 40.Miall RC, Wolpert DM. Forward models for physiological motor control. Neural Netw. 1996;9:1265–1279. doi: 10.1016/s0893-6080(96)00035-4. [DOI] [PubMed] [Google Scholar]
- 41.Lönn J, Djupsjöbacka M, Johansson H. Replication and discrimination of limb movement velocity. Somatosens Mot Res. 2001;18:76–82. doi: 10.1080/08990220020021375. [DOI] [PubMed] [Google Scholar]
- 42.Suprak DN, Osternig LR, van Donkelaar P, Karduna AR. Shoulder joint position sense improves with elevation angle in a novel, unconstrained task. J Orthop Res. 2006;24:559–568. doi: 10.1002/jor.20095. [DOI] [PubMed] [Google Scholar]
- 43.Stillman BC, McMeeken JM. The role of weightbearing in the clinical assessment of knee joint position sense. Aust J Physiother. 2001;47:247–253. doi: 10.1016/s0004-9514(14)60272-5. [DOI] [PubMed] [Google Scholar]
- 44.Cho YR, Hong BY, Lim SH, et al. Effects of joint effusion on proprioception in patients with knee osteoarthritis: A single-blind, randomized controlled clinical trial. Osteoarthritis Cartilage. 2011;19:22–28. doi: 10.1016/j.joca.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 45.Goble DJ, Noble BC, Brown SH. Proprioceptive target matching asymmetries in left-handed individuals. Exp Brain Res. 2009;197:403–408. doi: 10.1007/s00221-009-1922-2. [DOI] [PubMed] [Google Scholar]
- 46.Goble DJ, Brown SH. Task-dependent asymmetries in the utilization of proprioceptive feedback for goal-directed movement. Exp Brain Res. 2007;180:693–704. doi: 10.1007/s00221-007-0890-7. [DOI] [PubMed] [Google Scholar]
- 47.Goble DJ, Brown SH. Upper limb asymmetries in the matching of proprioceptive versus visual targets. J Neurophysiol. 2008;99:3063–3074. doi: 10.1152/jn.90259.2008. [DOI] [PubMed] [Google Scholar]
- 48.Han J, Waddington G, Adams R, Anson J. Bimanual proprioceptive performance differs for right- and left-handed individuals. Neurosci Lett. 2013;542:37–41. doi: 10.1016/j.neulet.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 49.Lundy-Ekman L. Elsevier Health Sciences; Amsterdam: 2013. Neuroscience–E-Book: Fundamentals for rehabilitation. [Google Scholar]
- 50.Gallagher S. Clarendon Press; Oxford: 2005. How the body shapes the mind. [Google Scholar]
- 51.MacKinnon CD. Sensorimotor anatomy of gait, balance, and falls. Handb Clin Neurol. 2018;159:3–26. doi: 10.1016/B978-0-444-63916-5.00001-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goble DJ, Coxon JP, Van Impe A, et al. Brain activity during ankle proprioceptive stimulation predicts balance performance in young and older adults. J Neurosci. 2011;31:16344–16352. doi: 10.1523/JNEUROSCI.4159-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shumway-Cook A, Horak F. Assessing the influence of sensory interaction on balance: Suggestion from the field. Phys Ther. 1986;66:1548–1550. doi: 10.1093/ptj/66.10.1548. [DOI] [PubMed] [Google Scholar]
- 54.Khasnis A, Gokula RM. Romberg's test. J Postgrad Med. 2003;49:169–172. [PubMed] [Google Scholar]
- 55.Shumway-Cook A, Woollacott MH. Lippincott Williams & Wilkins; Philadelphia, PA: 2007. Motor control: Translating research into clinical practice. [Google Scholar]
- 56.Macaulay TR, Peters BT, Wood SJ, Clément GR, Oddsson L, Bloomberg JJ. Developing proprioceptive countermeasures to mitigate postural and locomotor control deficits after long-duration spaceflight. Front Syst Neurosci. 2021;15 doi: 10.3389/fnsys.2021.658985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Grob KR, Kuster MS, Higgins SA, Lloyd DG, Yata H. Lack of correlation between different measurements of proprioception in the knee. J Bone Joint Surg Br. 2002;84:614–618. doi: 10.1302/0301-620x.84b4.11241. [DOI] [PubMed] [Google Scholar]
- 58.Janwantanakul P, Magarey ME, Jones MA, Grimmer KA, Miles TS. The effect of body orientation on shoulder proprioception. Phys Ther Sport. 2003;4:67–73. [Google Scholar]
- 59.Elangovan N, Herrmann A, Konczak J. Assessing proprioceptive function: Evaluating joint position matching methods against psychophysical thresholds. Phys Ther. 2014;94:553–561. doi: 10.2522/ptj.20130103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li L, Ji ZQ, Li YX, Liu WT. Correlation study of knee joint proprioception test results using common test methods. J Phys Ther Sci. 2016;28:478–482. doi: 10.1589/jpts.28.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Niespodziński B, Kochanowicz A, Mieszkowski J, Piskorska E, Żychowska M. Relationship between joint position sense, force sense, and muscle strength and the impact of gymnastic training on proprioception. BioMed Res Int. 2018;2018 doi: 10.1155/2018/5353242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang N, Waddington G, Adams R, Han J. Joint position reproduction and joint position discrimination at the ankle are not related. Somatosens Mot Res. 2020;37:97–105. doi: 10.1080/08990220.2020.1746638. [DOI] [PubMed] [Google Scholar]
- 63.Horváth Á, Vig L, Ferentzi E, Köteles F. Cardiac and proprioceptive accuracy are not related to body awareness, perceived body competence, and affect. Front Psychol. 2021;11 doi: 10.3389/fpsyg.2020.575574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.