Abstract
Pressure control cam dislocation is a rare finding in patients with a programmable shunt valve that should be considered when evaluating patients with signs and symptoms of shunt malfunction. The objective of this paper is to review the mechanism, clinical presentation, and radiographic findings associated with pressure control cam (PCC) dislocation, in addition to presenting a novel case to add to the scarce literature on this topic. A systematic review of the literature were performed using PubMed, Embase, and Cochrane from database inception. PCC dislocation is exceedingly rare and can present with no symptoms, positional headache, neck pain, nausea, or vomiting. Skull x-ray findings demonstrate a clear black “X” at the distal end of the valve, due to the PCC disarticulation from atop the base plate of the plastic valve housing. Intraoperatively, a “Y”-shaped crack atop the plastic valve housing may be present and the PCC may be fully separated from the shunt or found at the distal end of the plastic valve housing. Prior reports of dislocation of the PCC have occurred 7-9 years after implantation, with inciting events including direct trauma, programmable valve adjustment, and utilization 3-Tesla magnetic resonance image scan.
Keywords: Codman-Hakim programmable valve, 3-Tesla MRI, Pressure Control Cam Dislocation
Introduction
Hydrocephalus includes a heterogenous group of pathologies defined by excessive cerebrospinal fluid (CSF) accumulation which develops secondary to outflow obstruction or without obstruction in idiopathic intracranial hypertension and normal pressure hydrocephalus [1]. Hydrocephalus is managed with CSF diversion into the peritoneal space through a ventricular-peritoneal shunt. Control of diverted CSF is regulated by either a fixed-pressure or programmable valve systems. Codman-Hakim programmable valve (CHPV) is the first variable pressure valve with 18 different opening pressures ranging from 30 to 200 mmH₂O and can be percutaneously or noninvasively programmed. Magnetic torque adjusts the valve settings and can be impacted by magnetic field radiography. Although CHPV has been deemed compatible with 3-Tesla (3T) magnetic resonance image (MRI), it requires immediate re-configuration of valve settings [2].
Programmable valves including CHPV have a failure rate of 2% most commonly due to valve malfunction, blockage, and adjustment difficulties [3]. Zermak et al. [4] reported that amongst 660 placed valves, there were 13 cases of valve failure mainly due to blockage of the valve or more rarely inaccurate readings of the manometer. Direct malfunction of the actual valve system itself is exceedingly rare [4].
Knowledge of radiographic, clinical presentation and a high index of suspicion is required for appropriate management of shunt malfunction [5]. We present a very rare form of shunt malfunction specific to the CHPV system, with only 3 cases reported in the literature: dislocation of the pressure control cam (PCC).
Methods
This study is a case report and systematic review of the literature. A search was conducted utilizing PubMed, Embase, and Cochrane Central electronic databases from date of inception to January 2023. The primary objective was to identify all published PCC dislocations and summarize the presenting symptoms, radiographic findings, medical management, and patient outcomes.
Case report
An 8-year-old girl with a past medical history of hydrocephalus was treated with a ventriculoperitoneal shunt placed at the age of 10 days using the CHPV shunt system. The shunt was set at 80 mmH₂O and did not require any revisions.
The patient established care with our facility at age 5 and a 3T MRI of her brain and spine were obtained as part of routine management. A preemptive skull x-ray confirmed the valve setting at 80 mmH₂O prior to MRI (Fig. 1). However, after completion of the MRI, the CHPV could not be reprogrammed back to 80 mmH₂O despite several attempts.
Fig. 1.
Lateral skull x-ray demonstrating a right frontal approach ventriculoperitoneal shunt with a normal Codman-Hakim Programmable valve set to 80 mmH2O.
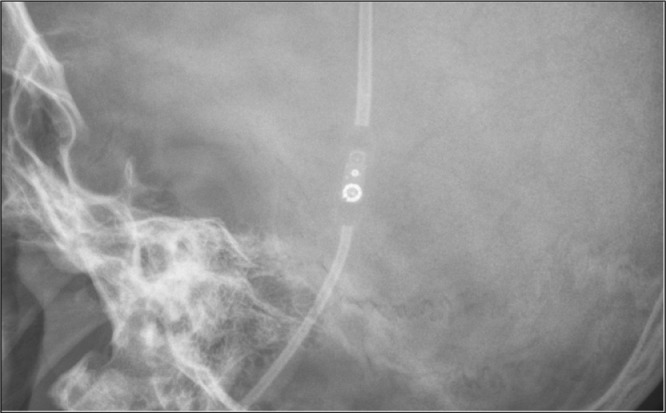
A repeat skull x-ray was obtained which showed the PCC was displaced distally from the plastic valve housing (Fig. 2). The patient denied any symptoms concerning for ventriculoperitoneal shunt malfunction including headache, nausea, or vomiting. Given the findings on her skull x-ray, the valve was deemed to no longer be intact, and the patient was taken to surgery for revision of the shunt system. The valve was replaced with a Medtronic medium pressure valve to eliminate the need for future reprogramming. On 3 year follow up, the patient remains asymptomatic, healthy and at neurologic baseline.
Fig. 2.
Lateral skull x-ray completed post 3T-MRI demonstrating a right frontal approach ventriculoperitoneal shunt (Codman-Hakim Programmable valve) with a displaced pressure control cam (black arrow) from the now apparent X-shaped base plate of the plastic valve housing.
Discussion
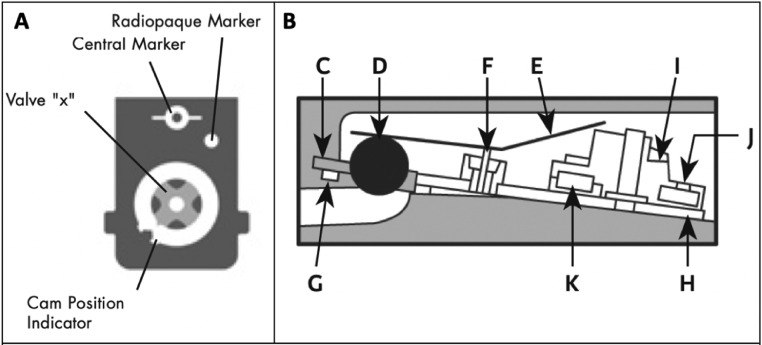
A side and top-view illustration taken from the manufacturer's website succinctly describes the delicate workings inside the CHPV (Fig. 3) [6]. The main valve involves a plastic valve housing that contains 2 opposing end openings. The proximal end contains a synthetic ruby valve ball that sits on a matching valve seat and the distal end includes a staircase shaped PCC located on a matching “X” shaped indentation. Atop the ball and PCC are multiple long levers that provide pressure for the spring. The mechanism of action relies on CSF pressure at the proximal end exceeding the intensity of spring pressure which allows the ball to rise and CSF to flow through.
Fig. 3.
Codman-Hakim programmable valve from the top view (A) and the side view (B) provided by the manufacturer. Side view illustration of the valve mechanism with the valve seat (C) valve ball (D) flat spring (E) spring calibrating fulcrum (F) O-ring (G) titanium base plate (H) pressure control cam (I) x-ray cam position indicator (J) and stepper motor (K) indicated. *Adopted from Manufacturer Website.
Obstruction of the shunt system proximal catheter or catheter disconnection is the more common causes of shunt system failure. Malfunction of the actual valve system is exceedingly rare [7]. In review of the literature, only 3 cases describe direct valve malfunction. The inciting events included direct trauma to the valve or exposure of the valve to a magnetic field. All patients presented with signs or symptoms of CSF over drainage [7], [8], [9].
Fortunately, in our patient, the shunt system malfunction was detected prior to development of clinical symptoms. It is evident on skull x-ray that the PCC is no longer in communication with the “X” shaped indentation in the plastic valve housing but rather distally displaced following the MRI.
Prior case reports of cam dislocation (Table 1) describe fractures of the plastic valve housing. Following direct trauma, Okazaki et al. [9] reported a break at the top of the plastic valve housing that allowed the cam to detach from the base plate. Following a 3T MRI scan, Watanabe et al. [8] also noted a “Y” shaped disruption on the housing and they suggested that remote trauma may have predisposed the cam to dislocation following completion of the MRI. On the other hand, Kim et al. [7], reported a case with no history of head trauma or recent MRI scan that had a minimally displaced PCC. In our case, the patient denied recent head trauma and disruption of the plastic valve housing was not present during surgery.
Table 1.
Cases of prior and current pressure control cam displacements reported in patients with the Codman-Hakim programmable valve shunt system.
| Author | Age (years)/Gender at presentation | Time from placement to symptoms | Mechanism of displacement | Symptoms | Time from mechanism to symptoms | Ventricular size at presentation | Valve replacement | Crack atop plastic housing | Valve inspection findings | Postop radiographic findings | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Okazaki et al. [9] | 7 (M) | 7 | Blow behind right ear over valve | Positional headache | 2 days | Slit like ventricles | Yes | Yes | Pressure control cam out of plastic valve housing | None reported | Resolution of symptoms |
| Watanabe et al. [8] | 57 (F) | 8 | Valve adjustment | Worsening of chronic headache and nausea | Few days | Slit like ventricles | Yes | Yes | Pressure control cam displaced distally | CTH showing resolution of slit ventricles | |
| Kim et al. [7] | 72 (F) | 9 | Completion of 3T MRI | Postural headache, neck pain, nausea | Several hours | Decreased ventricular size | Yes | Yes | Pressure control cam displaced distally | CTH showing resolution of decreased ventricle size | |
| Castillo et al. | 8 (F) | 8 | Completion of 3T MRI | None | N/A | Not preformed | Yes, to MPV | No | Not reported | Not performed |
3T MRI, 3-Tesla magnetic resonance imaging; CTH, commuted tomography of the head; F, female; M, male; MPV, medium pressure valve; N/A, not applicable.
We present the fourth case of a displaced PCC in a CHPV and the second case secondary to an MRI without history of trauma. Prior reports occurred 7-9 years following implantation with possible causative factors including trauma, valve setting adjustment, and 3T MRI completion. Symptoms of cam dislocation are often due to over-shunting resulting in positional headache, neck pain, nausea, and vomiting. Diagnosis can be made on x-ray images, which often demonstrate a clear blacked out “X” at the distal end of the valve due to PCC displacement from the base plate. Treatment requires urgent valve replacement and intraoperative findings may include disruption atop the plastic valve housing. Displacement of the PCC is a very rare complication that should be considered in patients with a CHPV that exhibit signs or symptoms of shunt malfunction.
Patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Isaacs AM, Riva-Cambrin J, Yavin D, et al. Age-specific global epidemiology of hydrocephalus: systematic review, meta-analysis and global birth surveillance [published correction appears in PLoS One. 2019 Jan 10;14(1):e0210851] PLoS One. 2018;13(10) doi: 10.1371/journal.pone.0204926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soler GJ, Bao M, Jaiswal D, et al. A review of cerebral shunts, current technologies, and future endeavors. Yale J Biol Med. 2018;91(3):313–321. [PMC free article] [PubMed] [Google Scholar]
- 3.Xu H, Wang ZX, Liu F, Tan GW, Zhu HW, Chen DH. Programmable shunt valves for the treatment of hydrocephalus: a systematic review. Eur J Paediatr Neurol. 2013;17(5):454–461. doi: 10.1016/j.ejpn.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Zemack G, Romner B. Seven years of clinical experience with the programmable Codman Hakim valve: a retrospective study of 583 patients. J Neurosurg. 2000;92(6):941–948. doi: 10.3171/jns.2000.92.6.0941. [DOI] [PubMed] [Google Scholar]
- 5.Yamashita N, Kamiya K, Yamada K. Experience with a programmable valve shunt system. J Neurosurg. 1999;91(1):26–31. doi: 10.3171/jns.1999.91.1.0026. [DOI] [PubMed] [Google Scholar]
- 6.Integralife.com. 2022. <https://www.integralife.com/file/general/1595874595.pdf> [accessed 24.07.22].
- 7.Kim SH, Lee YS, Lee MS, Suh SJ, Lee JH, Kang DG. Shunt overdrainage caused by displacement of the pressure control cam after pressure adjustment. Korean J Neurotrauma. 2016;12(2):163–166. doi: 10.13004/kjnt.2016.12.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watanabe A, Seguchi T, Hongo K. Overdrainage of cerebrospinal fluid caused by detachment of the pressure control cam in a programmable valve after 3-tesla magnetic resonance imaging. J Neurosurg. 2010;112(2):425–427. doi: 10.3171/2008.3.17688. [DOI] [PubMed] [Google Scholar]
- 9.Okazaki T, Oki S, Migita K, Kurisu K. A rare case of shunt malfunction attributable to a broken Codman-Hakim programmable shunt valve after a blow to the head. Pediatr Neurosurg. 2005;41(5):241–243. doi: 10.1159/000087481. [DOI] [PubMed] [Google Scholar]