Abstract
Background
The impact of combinations of yogic practices on bronchial asthma have been studied. Such yoga modules tend to be too lengthy for comfortable practice long-term, giving high dropouts. Returning to conventional medicine despite improvement is common. This study tested a shorter, easier yoga routine to improve asthma condition.
Material and methods
Sixty young adults aged 18-30 years diagnosed with bronchial asthma of mild to moderate severity were randomly assigned to the Yoga Group, add-on yoga therapy and continuing prescribed medication, or the Control Group, continuing prescribed medication only. Measurements on days 0 and 90, included Asthma Quality of Life Questionnaire, Hamilton Anxiety Rating Scale, Beck’s Depression Inventory and Pulmonary Function Tests. The yoga therapy module, practised 30 mins daily, included four kinds of yoga breathing practices, and ended with guided relaxation.
Results
All Asthma Quality of Life subdomains improved greatly for the Yoga Group as did Hamilton Anxiety and Becks Depression Inventory scores, t statistics were high (40 -75), all p<.0001. Pulmonary Function also improved greatly in all variables, with smaller t statistics from 2 to 14. The Control Group showed some small improvements. Differences observed in scores were highly significant, with large effect sizes. Finally, no dropouts occurred.
Discussion
Zero dropouts represents an unprecedented result. The yoga module was completely acceptable to participants, Yoga Group improvements were highly significant. The study indicates that the new yoga module effectively improves quality of life, levels of anxiety, depression and pulmonary function in young adults with above-stated bronchial asthma.
Keywords: Anxiety and depression, Asthma, Pulmonary function, Quality of life, Yoga
1. Introduction
The Global Initiative for Asthma (GINA) rates bronchial asthma a heterogeneous condition characterized by chronic inflammation of the airways causing respiratory symptoms: shortness of breath, chest tightness, wheeze and cough varying in intensity over time; also, variable outbreath limitation [1]. Also, shortness of breath and breathing difficulties caused by asthma attacks cause acute levels of emotional distress: panic during an attack, anxiety anticipating the next attack, and depression due to conventional treatments not improving the underlying condition, making treatment ongoing [2].
The World Health Organization's World Health Survey found bronchial asthma prevalent in young adults [3]. Doctors have diagnosed asthma in 4.3% of young adults aged 18–45 years globally. 4.5% reported taking medication for asthma, while 8.6% reported experience of wheezing in the previous year [4]. In 2016, the condition caused some 420,000 fatalities [5]. A 2018 study concluded that, for adolescents, 77% of asthma is undiagnosed [6], meaning that they suffer asthma attacks without even temporary respiratory relief. These figures demand novel approaches to treatment.
One possibility is traditional medicine. Doctors and scientists have explored classical Yoga, with its various limbs (Anga) [7] and yoga-based activities (Kriya) [8,9] as means of treating various medical conditions for half a century [[10], [11], [12], [13], [14], [15], [16], [17], [18]]. As a result, ‘Yoga therapy’ is now recognized as a formal medical system, with an holistic approach addressing both physical and psychological conditions i.e. stress and derived physical pathologies.
The expansion of Yoga's popularity globally has led to it being researched and applied to many conditions in many countries [19,20]. Many clinical trials have been carried out to evaluate the effects of Yoga practices on various medical conditions including asthma [[21], [22], [23], [24]].
Yoga's application to asthma was first studied in 1985–1986 [12,13]. Its potential benefits for associated problems were assessed later. Yoga – chair breathing was studied for acute asthma attacks [21], finding reduced sympathetic reactivity after Yoga training shown by significantly reduced DBP, (p < 0.01), after hand grip tests. Clinical research on asthmatic university students has employed various Yoga techniques [22]. A randomized controlled trial on the effects of Yoga lifestyle modification suggested that Yoga improves quality of life reducing rescue medication usage [23]. Another study [24] found improved quality of life in females with asthma. Universal findings of these studies are that groups trained in Yoga experience significantly fewer numbers of weekly asthma attacks, and improved scores for drug treatment and peak breath flow rate.
Yoga therapy is now considered a specific form of traditional complementary and alternative medicine [25,26]. Much physiologic research has been conducted on Yogic treatments over the past 3 decades [27]. Regular Yoga brings flexibility, strength and endurance on the physical level, and friendliness, compassion, calmness and well-being on the mental level [28]. Yoga's positive effects on physiologic and psychologic function improve patient quality of life [29]. For bronchial asthma, Yoga therapies are appropriate, as the ailment is psychosomatic [30].
Classical Yoga brings homeostasis to the entire organism. Correct breathing improves the ‘vital breath’ [31]; regularity in breathing rhythms helps both mind and body [32]. Yoga's fourth Anga, Pranayama, brings deeper understanding of this. The Sanskrit word ‘Ayama’ means expansion, so ‘Pranayama’ can be understood to mean ‘expansion of Prana’, subtle energy. By prolonging or shortening the breathing cycle, Pranayama helps to maintain health, increasing length of life [33]. Excess sympathetic nervous system activity causes psychosomatic ailments; slow rhythmic breathing reduces them [34]. A major problem in most studies is dropout levels, usually 10–20% [[35], [36], [37]], reducing efficacy of the concerned Yoga therapy , e.g. one study [38] reported 20% dropout in the Yoga group, and 16.7% in controls. Removing dropout is a major need for Yoga therapy.
With these requirements in mind, this study investigated a new 30-min Yoga module, that had been well-tested on patients during its development. Here, we report effects of 90 days practice on patient quality of life, anxiety, depression, and pulmonary function in young adults aged 18 to 30 diagnosed with bronchial asthma of mild to moderate severity.
The study's aims were to demonstrate the practicality and advantages of the shorter Yoga treatment module. Its objectives were to assess changes in quality of life, anxiety, depression and pulmonary function, pre-post the 90-day intervention. Study hypotheses: there would be significant improvements in each of these measures following 90 days' Yoga module practice.
2. Methodology
2.1. Experimental design
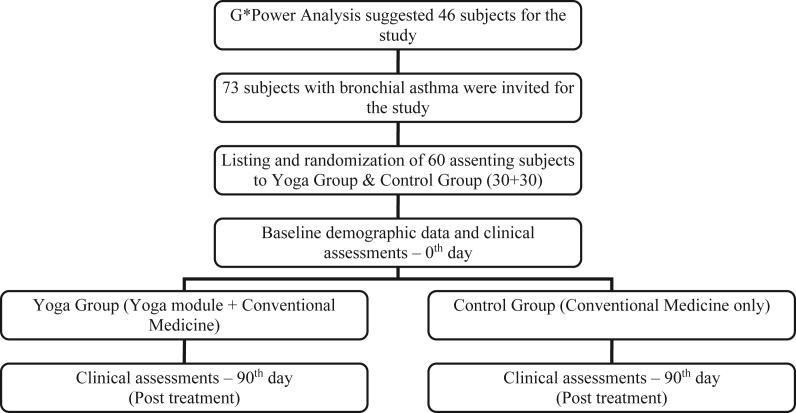
Randomized Control Trial – those who signed the Informed Consent were first grouped according to gender; the two gender groups were then randomly assigned either to the Yoga Group or the Control Group. See Fig. 1.
Fig. 1.
Flow chart of the RCT.
2.2. Participants
Bronchial Asthma patients aged 18–30 years in the city of Mangalore were requested to participate in the study. By the time 60 (30 male and 30 female) had agreed and signed the Informed Consent form, 73 had been approached.
2.3. Inclusion criteria
Male or Female; Age Range – 18 to 30 years; not previously receiving Yoga Therapy; clinical diagnosis of Asthma rated mild to moderate according to standard diagnostic criteria (GINA- 2014 Persistent Bronchial Asthma Severity); Non-smokers or Not smoked for at least 6 months.
2.4. Exclusion criteria
Clinical diagnosis of Asthma, rated severe according to standard diagnostic criteria; smoker within past 6 months; hypertensive; pregnant/lactating women; acute infection within past 6 weeks; associated chronic respiratory disease e.g. pulmonary tuberculosis, lung cancer or autoimmune lung disease; other serious systemic illness, e.g. hepatic, renal, cardiac or CNS; major psychiatric illness.
2.5. Intervention
The Yoga Group was given the newYoga module (Table 1) to practice as an add-on therapy while continuing to take their prescribed conventional medication. A sound-attenuated hall was used for daily instruction, administered via a pre-recorded audio, thus avoiding any instructor bias. The instructor was, however, available throughout each session in order to answer questions, and to help to make the practice more precise where necessary. The Control Group continued their prescribed conventional medication with no Yoga practice of any kind permitted before the 90-day intervention was over.
Table 1.
Yoga Module Practiced by the Yoga Group.
| Sl. No. | Practice | Duration |
|---|---|---|
| 1. | Rhythmic Abdominal Breathing | 5 min |
| 2. | Vakshasthala Shaktivikasa Vyayama | 5 min |
| 3. | Kapalabhati | 5 min |
| 4. | Bhastrika Pranayama | 10 min |
| 5. | Guided Relaxation | 5 min |
Comment: Table 1 Lists the Practices in the Add-on Yoga Module given to the Yoga Group.
2.6. Details of components of the intervention
2.6.1. Rhythmic abdominal breathing
A standard Yoga breathing practice basic to Pranayama with a long history of application. Practised with the body vertical, it uses deep, slow breathing: pulling the abdomen in on exhalation and pushing it out in inhalation, reestablishing the correct pattern of breathing in those habitually breathing too shallow or otherwise wrongly. (Five minutes).
2.6.2. Vakshasthala shaktivikasa vyayama
A well-known Yoga practice used for asthma [39,40]. Procedure 1: Start standing straight with the feet together and arms beside the body. Swing the arms up and backwards, tracing a semi-circle while inhaling through the nose. Then lean back, holding the breath as long as possible. Bring the arms down slowly while exhaling, reaching the starting posture. Do this 5 times. Procedure 2: Start standing straight with feet together and arms beside the body. Bend backwards during inhalation stretching the arms backward, expanding the chest. Maintain this posture, holding the breath. When exhaling, let the arms, back and chest slowly return to the starting position. Do this 5 times. (Five minutes).
2.6.3. Kapalabhati
A much-researched standard Yoga kriya [41]. Sit cross-legged (sukhasana) or in kneeling position (vajrasana); exhale actively and inhale passively at a rate of 60 cycles per minute, in groups of 30 followed by 5–10 s’ rest. (Five minutes).
2.6.4. Bhastrika pranayama
A well-authenticated Yoga pranayama [42], Sit cross-legged (sukhasana) or in kneeling position (Vajrasana); forcefully inhale and exhale through the nose, letting the abdomen rhythmically follow the breath in and out. Twenty-five strokes using: first, the left nostril; then the right nostril; finally, both nostrils. Relax 10–15 s as comfortable. Do this three times. (Ten minutes).
2.6.5. Guided relaxation
A standard, well-researched procedure developed at S-VYASA [43]. Lie supine; starting from the top of the head, relax the face, arms, back, chest, abdomen, hips and legs, while breathing deeply in and out. Picture yourself breathing easily with no resistance; then slightly move the fingers and the toes and open the eyes slowly. (Five mins).
2.7. Outcomes
All Outcome measurements were made on Day 0, before the start of the intervention and Day 90 when it ended. Quality of life was assessed using the Asthma Quality of Life Questionnaire (AQLQ) with Cronbach's α, 0.81 to 0.87, and good correlation consistency [44]. Anxiety was measured by the Hamilton Anxiety Rating Scale (HAM-A) with Cronbach's α 0.92, and high content validity [45,46]. HAM-A was among the first scales developed to assess both psychic anxiety related to stress, and associated physical complaints, somatic anxiety [45,46]. Depression was measured by Beck's Depression Inventory (BDI), a self-report rating inventory with Cronbach's α, 0.86 for psychiatric populations, 0.81 for non-psychiatric populations, i.e. good internal consistency [47]. Both the HAM-A and BDI are still in use today clinically and for research, and can be employed with confidence. Pulmonary function was assessed in the laboratory of Alva's Health Centre, Moodbidri by a qualified technician using SpiroWin, a Windows based Spirometer, © 99–07 Genesis Medical Systems Pvt. Ltd [48].
2.7.1. Asthma Quality of Life Questionnaire (AQLQ)
The AQLQ assesses problems of four kinds, physiological, emotional, social and environmental, that asthmatic adults aged 17–70 find most challenging. Its 32 questions cover four subdomains: Symptoms (11 items); Activity Limitation (12 items); Emotional Function (5 items); and Environmental Stimuli (4 items). Marked on a 7-point Likert scale, scores ranging from 1 to 7; higher scores indicate better quality of life. (1 = severely impaired, 7 = no impairment).
2.7.2. Hamilton Anxiety rating scale (HAM-a)
Comprises fourteen items scored from 0 to 4, each item relates to sets of symptoms specifically connected to one kind of anxiety. Total Scores range from 0 to 56. The instrument states that less than 17 indicates mild severity; 18 to 24, mild to moderate severity; and 25 to 30, moderate to severe anxiety.
2.7.3. Beck's Depression Inventory (BDI)
Measures characteristic attitudes and symptoms of depression using twenty-one statements with a rating scale from 0 to 3. Scores range from 0 to 63. Higher scores indicate greater symptom severity. In non-clinical populations, scores above 20 indicate depression. In those diagnosed with depression, scores of 0–13 indicate minimal depression, 14–19 mild depression, 20–28 moderate depression and 29–63 severe depression [49].
2.7.4. Pulmonary Function Test (PFT)
Pulmonary function tests are important tools in monitoring patients with respiratory pathologies. They are of great value in early diagnosis, classifying severity, evaluating disease progression and curative effect of therapies [48]. They provide information about the large and small airways, the pulmonary parenchyma and the size and integrity of the pulmonary capillary bed. Spirometry, a measure of volume against time, is the most frequently used test of lung function. A simple and quick procedure to perform; patients are asked to take maximal inspiration and then forcefully expel air for as long and as quickly as possible. Assessments include, Forced Vital Capacity (FVC), Forced Expiratory Volume1 (FEV1), FEV1/FVC%, Peak Expiratory Flow (PEF), Slow Vital Capacity (SVC), Tidal Volume (TV) & Maximum Voluntary Ventilation (MVV). FEV1 > 80% indicates mild, 50–79% moderate and 30–49% severe airflow obstruction. Forced vital capacity (FVC) is the total amount of air that can be forcibly blown out after full inspiration, measured in liters. Forced expiratory Volume in 1 s (FEV1) is the amount of air that is forcibly blown out in 1 s, measured in liters. FEV1/FVC is the ratio of FEV 1 to FVC. Peak Expiratory Flow Rate (PEFR) indicates the speed of the air moving out of lungs at the beginning of the expiration, measured in liters per second. Slow Vital Capacity (SVC) is the volume of air expired without force through the maneuver. Tidal volume (TV) is the amount of air moving in and out of the lungs with each respiration. The maximal voluntary ventilation (MVV) is the maximal volume of air movement by voluntary effort in 1 min. It is expressed in litres per minute.
2.8. Sample size
G∗Power analysis of yoga for asthma trials suggested that 46 subjects in two groups, would yield results with significance p < 0.05 level, with power at 0.2. The number 60 was set to make allowance for up to 20% dropout rate [23].
2.9. Randomization
Used the computerized random number generator https://www.calculator.net/random-number-generator.html. Blinding: not possible in this kind of Yoga study.
2.10. Statistical methods
Data were analyzed using IBM Statistical Package for the Social Sciences (SPSS) version 21. After using the Shapiro–Wilk test to assess normality of distributions, all p > 0.05, various ‘t’ tests, were used to assess statistical significances.
3. Results
Fig. 1 summarizes the processes involved in the study, its flow from recruitment of participants through randomization and informed consent, to participation and measurements. Attendance records measured adherence for each Yoga Group member, 90% being required for inclusion in the study analysis. All patients attended 100% of sessions: attrition was zero.
Table 2 presents baseline demographic data for the two Groups, including age, height, weight duration of illness, and dosages of prescribed conventional medication. Baseline clinical characteristics are given for all thirteen outcome measures in Table 3. Independent Sample t-tests on pre-intervention data showed that the two groups were entirely comparable. Table 4 presents the post-intervention data. Between them, Table 3, Table 4 contain pre & post intervention means and standard deviations for all thirteen variables: four AQLQ subdomains, HAM-A and BDI scores, and the seven Pulmonary Function variables of the two groups. Table 5 presents Differences in Observed Scores (often called ‘Group Time Analysis’) showing the differences between pre-post intervention changes in the two groups, their effect sizes, confidence intervals and statistical significance.
Table 2.
Baseline demographic data of the initially randomized sample.
| Sl No | Baseline Measures | Yoga Group (Mean ± SD) | Control Group (Mean ± SD) | t Statistic (df = 58) | p Value |
|---|---|---|---|---|---|
| 1. | Age (in years) | 24.2 ± 2.63 | 22.97 ± 2.54 | 1.8 | 0.07 |
| 2. | Height (in cm) | 153.47 ± 4.04 | 154.7 ± 3.55 | −1.2 | 0.21 |
| 3. | Weight (in kg) | 42.97 ± 4.12 | 43.68 ± 3.98 | −0.7 | 0.50 |
| 4. | Asthma since (years) | 6.7 ± 2.94 | 6.43 ± 3.30 | 0.3 | 0.74 |
| 5. | Medication μg/day | 363.33 ± 97.32 | 370 ± 90.59 | −0.3 | 0.78 |
Table 3.
Baseline scores – clinical characteristics.
| Pre-Treatment |
Mean±SD |
Effect Size | t statistic | p Value | |
|---|---|---|---|---|---|
| Variable | Yoga Group | Control Group | |||
| Symptoms | 23.57 ± 4.0 | 22.57 ± 2.74 | 0.29 | 1.1 | 0.26 |
| Activity Limitations | 27.57 ± 2.94 | 28.07 ± 3.09 | 0.17 | −0.6 | 0.52 |
| Emotional Function | 11.27 ± 1.84 | 11.33 ± 1.86 | 0.04 | −0.1 | 0.89 |
| Environmental Stimuli | 9.23 ± 1.52 | 9.90 ± 1.30 | 0.47 | −1.8 | 0.07 |
| HAM-A | 28.90 ± 2.82 | 28.90 ± 2.23 | 0.00 | 0.0 | 1.00 |
| BDI | 39.07 ± 1.89 | 39.07 ± 1.89 | 0.00 | 0.0 | 1.00 |
| FVC | 1.45 ± 0.12 | 1.48 ± 0.13 | 0.28 | −1.1 | 0.28 |
| FEV1 | 0.85 ± 0.22 | 0.86 ± 0.17 | 0.08 | −0.3 | 0.75 |
| FEV1/FVC% | 56.21 ± 6.47 | 58.27 ± 8.97 | 0.26 | −1.0 | 0.31 |
| PEF | 1.20 ± 0.24 | 1.22 ± 0.33 | 0.08 | −0.3 | 0.75 |
| SVC | 1.05 ± 0.17 | 1.01 ± 0.19 | 0.22 | 0.8 | 0.40 |
| TV | 0.53 ± 0.17 | 0.56 ± 0.14 | 0.19 | −0.7 | 0.47 |
| MVV | 22.14 ± 3.41 | 23.13 ± 3.18 | 0.31 | −1.2 | 0.25 |
Comment: p values did not attain significance for any parameter, all p > 0.05.
Table 4.
Yoga Group & Control Group Scores – Post Treatment – 90th day.
| Variable | Mean ± St Dev |
Effect Size (Cohen's d) | t Statistic | p Value | 95% Confidence Interval of the Difference |
||
|---|---|---|---|---|---|---|---|
| Yoga Group | Control Group | Lower | Upper | ||||
| Symptoms | 59.40 ± 3.97 | 25.07 ± 2.42 | 10.44 | 40.4 | 0.000∗∗∗ | 32.63 | 36.03 |
| Activity Limitations | 60.50 ± 3.09 | 29.77 ± 2.55 | 10.85 | 40.4 | 0.000∗∗∗ | 29.27 | 32.20 |
| Emotional Function | 26.17 ± 1.88 | 13.0 ± 1.55 | 7.64 | 29.6 | 0.000∗∗∗ | 12.28 | 14.06 |
| Environmental Stimuli | 21.33 ± 1.52 | 11.90 ± 1.09 | 7.13 | 27.6 | 0.000∗∗∗ | 8.75 | 10.18 |
| HAM-A | 6.17 ± 1.08 | 25.23 ± 1.52 | 14.46 | 55.8 | 0.000∗∗∗ | 19.75 | 18.38 |
| BDI | 9.20 ± 0.99 | 35.07 ± 1.60 | 19.44 | 75.3 | 0.000∗∗∗ | 26.55 | 25.18 |
| FVC | 2.28 ± 0.29 | 1.78 ± 0.18 | 2.06 | 8.0 | 0.000∗∗∗ | 0.37 | 0.62 |
| FEV1 | 1.45 ± 0.23 | 1.07 ± 0.25 | 1.60 | 6.2 | 0.000∗∗∗ | 0.26 | 0.51 |
| FEV1/FVC% | 63.88 ± 7.27 | 59.0 ± 9.12 | 0.59 | 2.3 | 0.000∗∗∗ | 0.63 | 9.15 |
| PEF | 2.19 ± 0.41 | 1.62 ± 0.58 | 1.13 | 4.4 | 0.000∗∗∗ | 0.31 | 0.83 |
| SVC | 2.33 ± 0.53 | 1.41 ± 0.32 | 2.09 | 8.1 | 0.000∗∗∗ | 0.69 | 1.15 |
| TV | 0.83 ± 0.22 | 0.70 ± 0.14 | 0.7 | 2.7 | 0.000∗∗∗ | 0.03 | 0.22 |
| MVV | 44.35 ± 4.57 | 29.28 ± 3.56 | 3.68 | 14.2 | 0.000∗∗∗ | 12.95 | 17.18 |
Comment: p values are significant (<0.001) for all parameters.
Table 5.
Differences observed in scores.
| Variable | Yoga Group (Post-Pre) |
Control Group (Post-Pre) |
Effect Size Cohen's d |
t Value | p Value | 95% Confidence Interval of the Difference |
|||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Lower | Upper | ||||
| Symptoms | 35.83 | 0.46 | 2.5 | 0.86 | 48.33 | 187.18 | <0.0001 | 31.97 | 32.69 |
| Activity Limitation | 32.93 | 0.52 | 1.7 | 0.99 | 39.49 | 153 | <0.0001 | 30.82 | 31.64 |
| Emotional Function | 14.9 | 0.66 | 1.67 | 0.71 | 19.3 | 74.75 | <0.0001 | 12.88 | 13.58 |
| Environmental Stimuli | 12.1 | 0.71 | 2.00 | 1.01 | 11.57 | 44.8 | <0.0001 | 9.65 | 10.55 |
| HAM-A | 22.73 | 2.2 | 3.67 | 1.32 | 10.51 | 40.69 | <0.0001 | 18.12 | 20.0 |
| BDI | 29.87 | 2.06 | 4.00 | 0.98 | 16.04 | 62.1 | <0.0001 | 25.04 | 26.7 |
| FVC | 0.83 | 0.21 | 0.30 | 0.11 | 3.16 | 12.24 | <0.0001 | 0.44 | 0.62 |
| FEV1 | 0.61 | 0.21 | 0.21 | 0.16 | 2.14 | 8.3 | <0.0001 | 0.3 | 0.5 |
| FEV1/FVC% | 7.67 | 9.20 | 0.71 | 7.06 | 0.85 | 3.28 | 0.0017 | 2.72 | 11.2 |
| PEF | 0.99 | 0.42 | 0.39 | 0.44 | 1.39 | 5.4 | <0.0001 | 0.38 | 0.82 |
| SVC | 1.29 | 0.54 | 0.41 | 0.31 | 2.0 | 7.74 | <0.0001 | 0.65 | 1.11 |
| TV | 0.29 | 0.24 | 0.14 | 0.19 | 0.69 | 2.68 | 0.0095 | 0.04 | 0.26 |
| MVV | 22.20 | 4.06 | 6.14 | 4.11 | 3.93 | 15.23 | <0.0001 | 13.95 | 18.17 |
Caption: Table 5 presents effect size, t values and significances and 95% confidence interval of observed differences between group scores.
4. Discussion
Data analysis using parametric tests presented in Table 3, Table 4, Table 5 was based on Shapiro–Wilk's Test findings that all data distributions were consistent with normality, all p values > 0.05. But the most significant observation beside that analysis is the zero drop out level. The new intervention was both simple enough to achieve 100% adherence, and efficacious enough to obtain significant improvements in all variables measured. As is evident from Yoga studies reviewed in the introduction [[12], [13], [14], [15], [16], [17], [18],[21], [22], [23], [24],[34], [35], [36], [37], [38]] dropout presents a major challenge in most studies of Yoga therapy, whatever the pathology treated, but particularly for asthma [12,13,[21], [22], [23], [24],[35], [36], [37], [38]]. Achieving zero dropouts is a highly significant outcome.
The between groups comparisons pre- and post-intervention presented in Table 3, Table 4 using Independent Sample t Tests, show that, at baseline, the two Groups were comparable in all respects; but post intervention they were very different, as indicated by the very high t values. The add-on Yoga therapy module had clearly exerted profoundly beneficial effects on the Yoga Group. Pre-intervention, the two groups showed no significant differences, p > 0.05 for all variables. Post-intervention, differences between the two groups shown in Table 4 were very large and highly significant. However, they may be better understood in terms of the differences observed between scores presented in Table 5, which shows very high t values, significances, and Cohen's ‘d’ effect sizes. Even the smallest t values, found for Tidal Volume and FEV1/FVC variables, were 2.68 and 3.28, with p values 0.0095 and 0.0017 respectively, while all other variables had p < 0.0001.
Test results indicate significant differences in every measure: all four AQLQ subdomains significant at p < 0.0001. Improvements for the Yoga Group were: Symptoms, 23.6 to 59.4, 46.5% of possible score; Activity Limitation 27.6 to 60.5, 39.2%; Emotional Function 11.3 to 26.2, 42.6%; Environmental Stimuli 9.2 to 21.3, 43.2%. Control Group scores changed: Symptoms, 22.6 to 25.1, 3.25% of possible score; Activity Limitation 28.1 to 29.8, 2.0%; Emotional Function 11.3 to 13.0, 4.9%; Environmental Stimuli 9.9 to 11.9, 7.1%, all far less than the Yoga Group. Changes in HAM-A and BDI scores were also highly significant, both p < 0.0001. In detail, the Yoga Group HAM-A scores decreased 28.9 to 6.17, 40.59% of possible score, while BDI scores decreased 39.07 to 9.2, 47.41% of possible score. Control Group scores decreased only 28.9 to 25.23, 6.5%, for HAM-A; and 39.07 to 35.07, 6.3% for BDI, far, far less. For Pulmonary Function, the corresponding improvements in Group means were: For the Yoga Group, FVC: 1.4 to 2.3, 64%; FEV1: 0.8 to 1.45, 81%; FEV1/FVC %: 56.2 to 63.9, 13.7%; PEF: 1.2 to 2.2, 83%; SVC: 1.0 to 2.3, 130%; TV: 0.5 to 0.8, 60%; MVV: 22.1 to 44.3, 104%. Control Group scores also improved, but by much less: FVC: 1.5 to 1.8, 20%; FEV1: 0.9 to 1.1, 22%; FEV1/FVC %: 58.3 to 59.0, 1.2%; PEF: 1.2 to 1.6, 33%; SVC: 1.0 to 1.4, 40%; TV: 0.6 to 0.7, 17%; and MVV: 23.1 to 29.3, 26.8%; as can be seen, all far less than for the Yoga Group. The improvements in all seven pulmonary function measures for the Control Group suggest some kind of ‘study effect’, which should be checked in future studies.
Significances of the differences in changes between the two Groups are presented in Table 5, Differences Observed in Scores. As can be seen, the between-groups differences are all significant at the level p < 0.0001, except for Tidal Volume, TV, with a Cohen's d of 2.68 and p = 0.0095, and FEV1/FVC with Cohen's d, 3.28, and p = 0.0017.
These detailed results indicate statistically significant benefit to quality of life, levels of anxiety and depression, and pulmonary functions in the asthma patients studied. Some might argue that the levels of significance indicate that the number of participants was set too high, but they can be attributed to the unprecedented, high level of adherence, 100%, and to the zero drop outs. G∗ power analysis was correctly based on data from previous Yoga therapy for asthma studies; departing from its requirements would have been inappropriate.
Since the study design had ensured that the two groups contained equal numbers of males and females, results were checked for possible gender difference; the means did not show any.
Cohen's d values showed that effect sizes for the Yoga Group were very large for all AQLQ and psychology variables. For pulmonary functions, they were smaller, but still respectable. Yoga therapists can rest assured that the new module will benefit quality of life, anxiety and depression levels, and pulmonary functions in asthma patients of mild to moderate severity aged 18 to 30. Clearly, the module also merits testing on patients outside this age range. Indeed, while under development the module was tested on three elderly patients aged 50 to 75 who practised the Yoga breathing exercises sitting in a chair, and obtained benefits similar to those sitting cross legged.
Strengths: The effect sizes, which were unexpectedly large; the zero dropout rate; and, also, participants’ statements of liking their practice of the yoga module were all strengths.
Weaknesses: Only taking measurements on Days 0 and 90 meant that improvements in the various parameters could not be followed as they developed.
Future Research: the weaknesses could be addressed by including 30-day or 45-day measurements; also, treatment duration could be extended to explore the extent to which normal health can be restored. Further variables could be investigated, particularly those concerning the biochemistry and immunology involved in bronchial asthma. Finally, patients with higher severity of bronchial asthma could be invited to participate. Since, as in this study, prescribed conventional medication would be continued as necessary, no danger would be incurred.
5. Conclusion
Overall, the study indicates that 90 days’ practice of the new Yoga module as an add-on therapy has a reliable, positive impact on quality of life, anxiety, depression, and pulmonary function in patients who are young adults with mild to moderate severity of bronchial asthma. It constitutes an effective clinical tool for physicians to prescribe as an adjuvant therapy to standard asthma treatment. Although daily supervised practice may seem a challenge to provide, the large numbers of available Yoga teachers in most cities of the world, and every part of India, suggest potentially universal use. Its applications to wider groups of patients should also be entertained.
Other information
Registration: The CTRI number is CTRI/2020/02/023,424, registration date, 2020.02.18. The S-VYASA Institutional Ethics Committee gave its approval on 2019.08.07, after application on 2019.05.25. when it was in principle approved.
Source of Funding
None
Author Contributions
First Author: Yoga Module Design and Development, Study Design, & Data Taking.
Second Author: Statistical Analysis, Article Writing and Data Presentation, Editing and Correcting - with first author present remotely.
Conflict of Interest
None.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Boulet L.P., Reddel H.K., Bateman E., Pedersen S., FitzGerald J.M., O'Byrne P.M. The global initiative for asthma (GINA): 25 years later. Eur Respir J. 2019;54(2) doi: 10.1183/13993003.00598-2019. [DOI] [PubMed] [Google Scholar]
- 2.Adams R.J., Wilson D.H., Taylor A.W., Daly A., d'Espaignet E.T., Dal Grande E., et al. Psychological factors and asthma quality of life: a population based study. Thorax. 2004;59(11):930–935. doi: 10.1136/thx.2003.010256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mattiuzzi C., Lippi G. January). Worldwide asthma epidemiology: insights from the global health data exchange database. In International forum of allergy & rhinology. 2020;10(No. 1):75–80. doi: 10.1002/alr.22464. [DOI] [PubMed] [Google Scholar]
- 4.Asher M.I., García-Marcos L., Pearce N.E., Strachan D.P. Trends in worldwide asthma prevalence. Eur Respir J. 2020;56(6) doi: 10.1183/13993003.02094-2020. [DOI] [PubMed] [Google Scholar]
- 5.Chatkin J., Correa L., Santos U. External environmental pollution as a risk factor for asthma. Clin Rev Allergy Immunol. 2021:1–18. doi: 10.1007/s12016-020-08830-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aaron S.D., Boulet L.P., Reddel H.K., Gershon A.S. Underdiagnosis and overdiagnosis of asthma. Am J Respir Crit Care Med. 2018;198(8):1012–1020. doi: 10.1164/rccm.201804-0682CI. [DOI] [PubMed] [Google Scholar]
- 7.Shearer A., Lannoy R. Ashgate; Farnham, UK: 1982. Effortless being: the yoga sutras of patanjali. [Google Scholar]
- 8.Saraswati S.M., Saraswati S.S. Yoga Publications Trust; 1998. Hatha yoga pradipika. [Google Scholar]
- 9.Swathi P.S., Raghavendra B.R., Saoji A.A. Health and therapeutic benefits of Shatkarma: a narrative review of scientific studies. J Ayurveda Integr Med. 2021;12(1):206–212. doi: 10.1016/j.jaim.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wallace R.K. Physiological effects of transcendental meditation. Science. 1970;167(3926):1751–1754. doi: 10.1126/science.167.3926.1751. [DOI] [PubMed] [Google Scholar]
- 11.Wallace R.K., Benson H., Wilson A.F. A wakeful hypometabolic physiologic state. American Journal of Physiology-Legacy Content. 1971;221(3):795–799. doi: 10.1152/ajplegacy.1971.221.3.795. [DOI] [PubMed] [Google Scholar]
- 12.Nagarathna R., Nagendra H.R. Yoga for bronchial asthma: a controlled study. Br Med J. 1985;291(6502):1077–1079. doi: 10.1136/bmj.291.6502.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagendra H.R., Nagarathna R. An integrated approach of yoga therapy for bronchial asthma: a 3–54-month prospective study. J Asthma. 1986;23(3):123–137. doi: 10.3109/02770908609077486. [DOI] [PubMed] [Google Scholar]
- 14.Javnbakht M., Kenari R.H., Ghasemi M. Effects of yoga on depression and anxiety of women. Compl Ther Clin Pract. 2009;15(2):102–104. doi: 10.1016/j.ctcp.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Radhakrishna S., Nagarathna R., Nagendra H.R. Integrated approach to yoga therapy and autism spectrum disorders. J Ayurveda Integr Med. 2010;1(2):120. doi: 10.4103/0975-9476.65089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khemka S.S., Ramarao N.H., Hankey A. Effect of integral yoga on psychological and health variables and their correlations. Int J Yoga. 2011;4(2):93. doi: 10.4103/0973-6131.85492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bangalore N.G., Varambally S. Yoga therapy for schizophrenia. Int J Yoga. 2012;5(2):85. doi: 10.4103/0973-6131.98212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thirthalli J., Naveen G.H., Rao M.G., Varambally S., Christopher R., Gangadhar B.N. Cortisol and antidepressant effects of yoga. Indian J Psychiatr. 2013;55(Suppl 3):S405. doi: 10.4103/0019-5545.116315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeter P.E., Slutsky J., Singh N., Khalsa S.B.S. Yoga as a therapeutic intervention: a bibliometric analysis of published research studies from 1967 to 2013. J Alternative Compl Med. 2015;21(10):586–592. doi: 10.1089/acm.2015.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stephens I. Medical yoga therapy. Children. 2017;4(2):12. [Google Scholar]
- 21.Nagarathna R., Nagendra H.R., Seethalakshmi R. Yoga-chair breathing for acute episodes of bronchial asthma. Lung India. 1991;9(4):141. [Google Scholar]
- 22.Vedanthan P.K., Kesavalu L.N., Murthy K.C., Duvall K., Hall M.J., Baker S., et al. vol. 19. OceanSide Publications; 1998. Clinical study of yoga techniques in university students with asthma: a controlled study; p. 3. (Allergy and asthma proceedings). No. 1. [DOI] [PubMed] [Google Scholar]
- 23.Vempati R., Bijlani R.L., Deepak K.K. The efficacy of a comprehensive lifestyle modification programme based on yoga in the management of bronchial asthma: a randomized controlled trial. BMC Pulm Med. 2009;9(1):1–12. doi: 10.1186/1471-2466-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bidwell A.J., Yazel B., Davin D., Fairchild T.J., Kanaley J.A. Yoga training improves quality of life in women with asthma. J Alternative Compl Med. 2012;18(8):749–755. doi: 10.1089/acm.2011.0079. [DOI] [PubMed] [Google Scholar]
- 25.Khalsa S.B. Yoga as a therapeutic intervention. Principles and practice of stress management. 2007;3:449–462. [Google Scholar]
- 26.Sullivan M., Robertson L.C.H. Routledge; 2020. Understanding Yoga Therapy: applied philosophy and science for health and well-being. [Google Scholar]
- 27.Russo M.A., Santarelli D.M., O'Rourke D. The physiological effects of slow breathing in the healthy human. Breathe. 2017;13(4):298–309. doi: 10.1183/20734735.009817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4(2):49. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parasuraman S., Wen L.E., Zhen K.M., Hean C.K., Sam A.T. Exploring the pharmacological and pharmacotherapeutic effects of yoga. Pharmacology, Toxicology and Biomedical Reports. 2016;2(1) [Google Scholar]
- 30.Alicja M., Piotr W., Monika P., Joanna D. Asthma as a psychosomatic disorder: the causes, scale of the problem, and the association with alexithymia and disease control. Pneumonol Alergol Pol. 2012;80:13–19. [PubMed] [Google Scholar]
- 31.Muktibodhananda S. Bihar School of Yoga; Munger: 1999. Swara yoga. [Google Scholar]
- 32.Sharma V.K., Trakroo M., Subramaniam V., Rajajeyakumar M., Bhavanani A.B., Sahai A. Effect of fast and slow pranayama on perceived stress and cardiovascular parameters in young health-care students. Int J Yoga. 2013;6(2):104. doi: 10.4103/0973-6131.113400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilbert C. Clinical applications of breathing regulation: beyond anxiety management. Behav Modif. 2003;27(5):692–709. doi: 10.1177/0145445503256322. [DOI] [PubMed] [Google Scholar]
- 34.Streeter C.C., Gerbarg P.L., Saper R.B., Ciraulo D.A., Brown R.P. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012;78(5):571–579. doi: 10.1016/j.mehy.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 35.Saxena T., Saxena M. The effect of various breathing exercises (pranayama) in patients with bronchial asthma of mild to moderate severity. Int J Yoga. 2009;2(1):22–25. doi: 10.4103/0973-6131.53838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agnihotri S., Kant S., Kumar S., Mishra R.K., Mishra S.K. Impact of yoga on biochemical profile of asthmatics: a randomized controlled study. Int J Yoga. 2014;7(1):17–21. doi: 10.4103/0973-6131.123473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang Z.Y., Zhong H.B., Mao C., Yuan J.Q., Huang Y.F., Wu X.Y., et al. Yoga for asthma. Cochrane Database Syst Rev. 2016;4(4):CD010346. doi: 10.1002/14651858.CD010346.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Agnihotri S., Kant S., Mishra S.K., Verma A. Assessment of significance of Yoga on quality of life in asthma patients: a randomized controlled study. Ayu. 2017;38(1–2):28–32. doi: 10.4103/ayu.AYU_3_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brahmachari D. Vishwayatan Yogashram; 1965. Yogic suksma vyayama; pp. 37–38. [Google Scholar]
- 40.Bhatt A.A., Pandey S., Singh B., Vyas G., Shukla G.D. A comparative study of Yogic and Ayurvedic intervention in the management of Tamaka Shwasa. International Journal of Pharmaceutical and Biological Science Archive. 2019;7(5) [Google Scholar]
- 41.Vaid M., Verma S. Kapalabhati: a physiological healer in human physiological system. Yoga Mimamsa. 2021;53(1):69. [Google Scholar]
- 42.Arulmozhi S., Joice S.P., Maruthy K.N. Effect of pranayama on respiratory muscle strength in chronic asthmatics. Natl J Physiol Pharm Pharmacol. 2018;8(12):1700–1703. [Google Scholar]
- 43.Vempati R.P., Telles S. Yoga-based guided relaxation reduces sympathetic activity judged from baseline levels. Psychol Rep. 2002;90(2):487–494. doi: 10.2466/pr0.2002.90.2.487. [DOI] [PubMed] [Google Scholar]
- 44.Juniper E.F., Buist A.S., Cox F.M., Ferrie P.J., King D.R. Validation of a standardized version of the asthma quality of life Questionnaire. Chest. 1999;115(5):1265–1270. doi: 10.1378/chest.115.5.1265. [DOI] [PubMed] [Google Scholar]
- 45.Shear M.K., Vander Bilt J., Rucci P., Endicott J., Lydiard B., et al. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depress Anxiety. 2001;13(4):166–178. [PubMed] [Google Scholar]
- 46.Maier W., Buller R., Philipp M., Heuser I. The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord. 1988;14(1):61–68. doi: 10.1016/0165-0327(88)90072-9. [DOI] [PubMed] [Google Scholar]
- 47.Lasa L., Ayuso-Mateos J.L., Vázquez-Barquero J.L., Dıez-Manrique F.J., Dowrick C.F. The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis. J Affect Disord. 2000;57(1–3):261–265. doi: 10.1016/s0165-0327(99)00088-9. [DOI] [PubMed] [Google Scholar]
- 48.Li F., Huang Z.W., Wang X.F., Xu H.W., Yu H., Chen Y.B., et al. Safety and use of pulmonary function tests: a retrospective study from a single center over seven years' clinical practice. BMC Pulm Med. 2019;19(1):259. doi: 10.1186/s12890-019-1019-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gillaspy S.R., Hoff A.L., Mullins L.L., Van Pelt J.C., Chaney J.M. Psychological distress in high-risk youth with asthma. J Pediatr Psychol. 2002;27(4):363–371. doi: 10.1093/jpepsy/27.4.363. [DOI] [PubMed] [Google Scholar]