Abstract
Background
Safety culture is an important aspect of quality in healthcare settings. There are many risks that patients can encounter in hemodialysis settings one of which is the infection risks due to the regular need to access bloodstreams using catheters and needles. Implementation of prevention guidelines, protocols and strategies that reinforce safety culture excellence are essential to mitigate risks. The objective of this study was to identify and characterize the main strategies that enhance and improve patient safety culture in hemodialysis settings.
Methods
Medline (via PubMed) and Scopus were searched from 2010 to 2020 in English. Terms defining safety culture, patient safety were combined with the term hemodialysis during the search. The studies were chosen based on inclusion criteria.
Results
A total of 17 articles reporting on six countries were identified that met inclusion criteria following the PRISMA statement. From the 17 papers, practices that were successfully applied to improve safety culture in hemodialysis settings included (i) training of nurses on the technologies used in hemodialysis treatment, (ii) proactive risk identification tools to prevent infections (iii) root cause analysis in evaluating the errors, (iv) hemodialysis checklist to be used by the dialysis nurses to reduce the adverse events, and (v) effective communication and mutual trust between the employee and leadership to support no-blame environment, and improve the safety culture.
Conclusion
This systematic review provided significant insights on the strategies that healthcare safety managers and policy makers can implement to enhance safety culture in hemodialysis settings.
Keywords: safety culture, patient safety, kidney care, hemodialysis, quality improvement, medical error
Background
Patient safety is the establishment of top-notch medical services, which is also considered a crucial part of the quality of medical centers. It is progressively recognized that strengthening the safety culture in medical centers is vital to uphold the quality of care. Safety culture can be defined as the individual’s product, group beliefs, behavior patterns, values and attitudes, competencies, and perceptions that show or determine the commitment level of an organization to patient safety and quality care.1 Moreover, the same attributes are used to determine how the organization is committed to enhancing the quality of patient safety in renal care.
Building safety culture is fundamental for making a high quality associations in medical care.2–4 Dialysis facilities are not exceptions and need to ensure safety and quality of care and foster a culture that enhances patient safety. There are a range of risk sources and contributory factors that patients might experience in hemodialysis settings, one of which is the infection risks due to the regular need to access bloodstreams using catheters and needles. Patients might be infected in the various parts of the body such as the lungs, bones, vascular access points, bloodstreams and even the skin. These infections obtained in dialysis settings or during dialysis can extend the condition, or even lead to death which in turn disrupts the patient’s normal living and also incurs high costs of dialysis.5 Reasons why patients may acquire infections include patients staying close together, faulty equipment, blood-borne viruses, expedited turnover amid dialysis, and being constantly admitted to the center. Implementation of prevention guidelines, protocols and strategies that reinforce safety culture excellence are essential to mitigate such risks as well as adequate staff training. These settings are required to attain specific standards including adequate staff, proper and well-maintained equipment and regular maintenance of facilities.
In previous safety culture assessment of hemodialysis settings, there has been minimal incorporation of qualitative research, with none having a systematic review that gathers all reported methods to comprehensively identify the safety culture drivers in such settings. Therefore, our research aims to address the following question: “What are the safety culture assessment tools used in hemodialysis settings?” In order to address this, we identify and review the main methods, tools and strategies used to improve the safety culture at hemodialysis settings. Although safety culture can be measured and compared across institutions,6,7 the methods hospitals should use to improve safety culture have yet to be defined. To synthesize published literature and draw actionable inferences, we conducted a systematic literature review to compile all the various strategies and improvements that can be implemented to strengthen the safety culture in hemodialysis settings.
Method
This systematic literature review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.8 The PRISMA statement includes a checklist for systemic evaluations (see Supplement file). Firstly, we included the studies that focus on strategies for improving safety culture in hemodialysis settings. Secondly, our articles were selected from two databases: MEDLINE (via PubMed) and Scopus. Thirdly, we decided that our search strategies should be used in both databases including two Boolean operators; “OR” when keywords were similar (like dialysis or hemodialysis) and included “AND” for adding more keywords to the search (like safety culture, patient safety). Finally, Table 1 shows the search strategy used in MEDLINE (via PubMed), whereas the search strategy of Scopus is shown in Table 2.
Table 1.
MEDLINE (via PubMed) Search Strategy
| Strategy | Keywords | # of Results |
|---|---|---|
| Attempt 1 | (safety culture[Title/Abstract]) AND ((dialysis[Title/Abstract]) OR (hemodialysis[Title/Abstract])) | 13 |
| Attempt 2 | (patient safety [Title/Abstract]) AND ((dialysis[Title/Abstract]) OR (hemodialysis[Title/Abstract])) | 214 |
Table 2.
Scopus Search Strategy
| Strategy | Keywords | # of Results |
|---|---|---|
| Attempt 1 | (“Safety culture*” AND (“Dialysis*” OR “hemodialysis*”)) [Title/Abstract] | 15 |
| Attempt 2 | (“Patient Safety*” AND (“Dialysis*” OR “hemodialysis*”)) [Title/Abstract] | 263 |
Eligibility Criteria
The inclusion criteria considered while screening and selecting the papers were based on the following: (i) studies related to improving the safety culture in hemodialysis units, (ii) studies that were published in the English language, (iii) studies published between January 2010 and December 2020, (iv) studies published in journals, (v) studies that were conducted in hemodialysis settings.
Selection Process
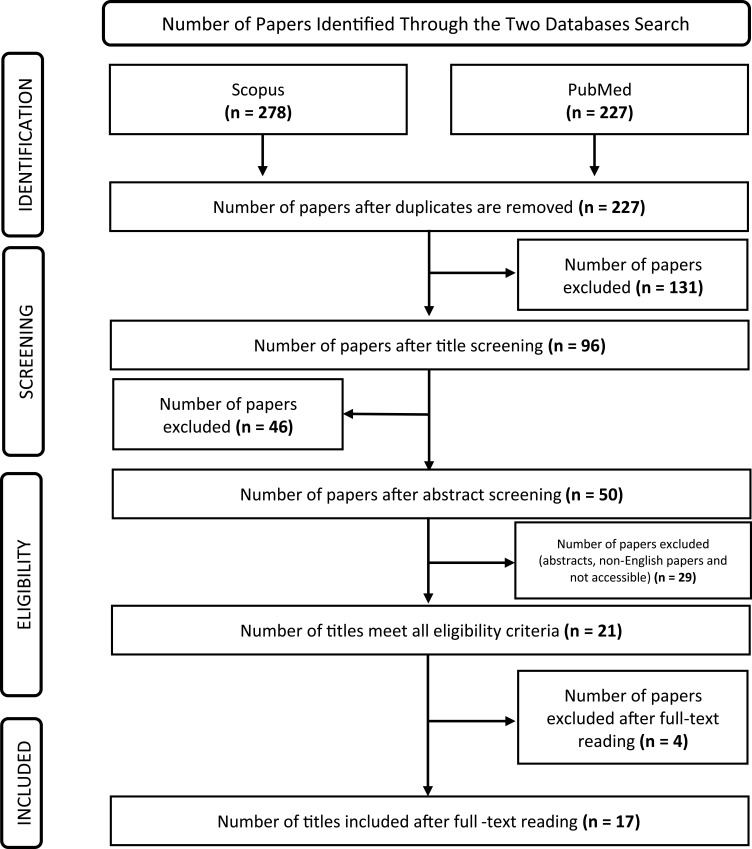
The search using the two databases (PubMed and Scopus) identified 505 titles. After eliminating duplicate titles, we were left with 227 articles for screening, which was conducted by four researchers (S.A., A.A., T.A., and A.A.). Of these, 177 were discarded after the title and abstract screening. After that, 29 papers were excluded because of not meeting the criteria’s considered for this study, such as abstracts, short conference proceedings, and non-English papers. Four papers were also removed after reading the full text and not getting useful information about safety in hemodialysis settings, leaving 17 papers for extraction and analysis. Figure 1 shows a flowchart of the article selection in detail.
Figure 1.
Study selection flowchart.
Notes: PRISMA figure adapted from Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009; 6(7):e1000097. Creative Commons.9
Results
Study Characteristics
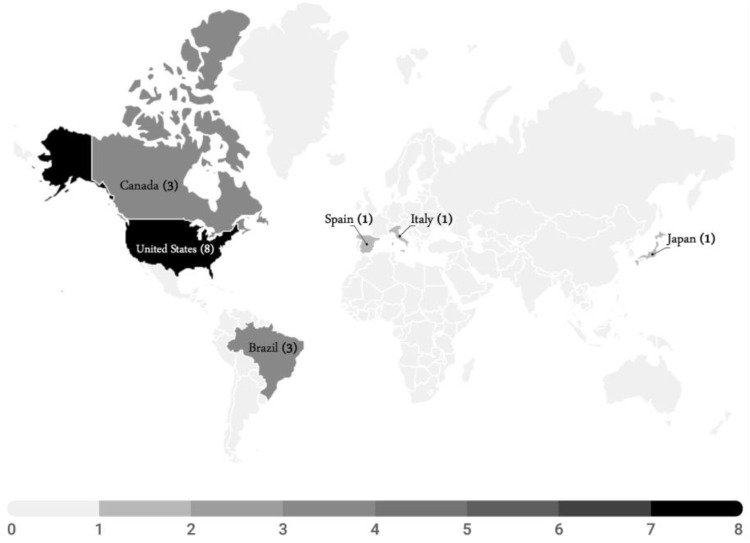
The 17 studies originated from 6 different countries, Figure 2 shows the worldwide distribution of the contributing countries. Moreover, Table 3 shows a range of quantitative and qualitative data that were extracted from the 17 included studies. Quantitative data included sample size and follow-up duration (months), whereas qualitative data included country, objective, outcome measures, results, improvement strategies and study limitations.
Figure 2.
Number of publications by country.
Table 3.
Characteristics of the Selected Studies
| Author, Year, Country | [Sample Size]/ [Follow-Up (Months)]/ [Outcome Measure/Methodology] | Objective | Results | Improvement Strategies | Limitations |
|---|---|---|---|---|---|
| B. R. P. de Andrade, F. de M. Barros, H. F. Â. de Lúcio, J. F. Campos, and R. C. da Silva 2019, Brazil16 | [23 nurses]/ [3 months]/ [Interviewed using a script] | Report nurse’s role in the management of the ICU in continuous hemodialysis. | ICU nurses in continuous hemodialysis are given the role to perform preparations and follow-up activities, by interacting with technologies based on interaction with technology and the use of specialized knowledge. |
|
Not many national experienced nurses in the ICU of continuous Hemodialysis. |
| C. Thomas-Hawkins and L. Flynn 2015, USA21 | [422 registered nurses]/ [3 months]/ [Survey] | Study the relation between patient safety culture and nurse-reported adverse events in the outpatient hemodialysis units. | 39% of nurses had recognized that patient transitions in the dialysis units were safe, and 86% had graded patient safety as either good or excellent. |
|
The staff nurse sample may have different characteristics from nurses working in hemodialysis units. |
| A. Thomas et al 2016, Canada13 | [14 nurses and 22 patients]/ [3 months]/ [Hemodialysis safety checklist (Hemo Pause)] | Determine the value of using the Hemo Pause checklist during hemodialysis sessions. | 93% of hemodialysis nurses agreed that the Hemo Pause checklist was easy to use. 93% want the checklist to be used during their hemodialysis sessions. 73% of the hemodialysis patients found that the checklist made them feel safer. 79% of nurses and 73% of patients agreed it should be expanded to other patients. |
|
|
| Kliger 2015, USA22 | [Not mentioned]/ [Not mentioned]/ [Not mentioned] | To identify the occurrence of errors, and how to reduce or eliminate them, and chances to improve the process faster. | [Not mentioned] |
|
[Not mentioned] |
| R. Garrick, A. Kliger, and B. Stefanchi 2012, USA23 | [1143]/ [3 months]/[Surveys] | Application of safety principles to dialysis facilities. | Dialysis facilities share significant safety concerns, and patients express greater concern about unit safety procedures than workers would expect. |
|
|
| T. Millson, D. Hackbarth, and H. L. Bernard 2019, USA10 | [100 dialysis patient/ month]/ [12 months]/ [Surveys among 6 facility destinations] |
|
Reviews showed improvements from 27%-82% of methods performed accurately. Circulatory system disease rates diminished from 2.33–1.07 occasions per 100 patients. |
|
|
| L. P. Wong 2019, USA18 | [Not mentioned]/ [Not mentioned] / [Surveys based on focus group] | Eliminate dialysis infections and target zero infections. | [Not mentioned] |
|
[Not mentioned] |
| B. R. P. de Andrade, F. de M. Barros, H. F. Ângela de Lúcio, J. F. Campos, and R. C. da Silva 2019, Brazil17 | [23 nurses]/ [4 months]/ [Observations and semi structured interviews] | Analyze intensive care nurses’ clinical experience and its effect on their work experiences in the continuous hemodialysis environment and patient safety in the ICU. |
|
|
Limited experienced nurses working in the ICU in the continuous Hemodialysis centers. |
| Kristina K. Davis, Kathleen G. Harris, Vrinda, Mahishi, Edward G. Bartholomew, Kevin Kenward 2016, USA11 | [599 Administrative leaders, Physician, Dietician, Nurse and others]/ [Not mentioned]/ [Modified HSOPSC Survey] | To evaluate the safety culture of hemodialysis centers via a modified HSOPSC. |
|
|
|
| Leslie P. Wong 2018, USA19 | [Not mentioned]/ [Not mentioned] / [Systems Thinking] | To provide a novel approach to prevent infections in dialysis facilities. | [Not mentioned] |
|
[Not mentioned] |
| Attilio Di Benedetto, Francesco Pelliccia, Manuela Moretti, Wanda d’Orsi, Fernando Starace, Laura Scatizzi, Maria Teresa Parisotto, Daniele Marcelli 2011, Italy24 | [346, physicians, registered nurses and health care assistants]/ [Not mentioned]/ [Safety Climate Survey & Universal Hygiene Precautions questionnaires] | [Not mentioned] |
|
|
Both questionnaires had a predefined range of answer choices in the form of rank-based responses on a Likert-type response scale. The questionnaires did not contain any open-ended questions. Since respondents were asked to complete all questionnaires anonymously, there was no way to draw a causal distinction between the two. |
| Alexandre R. Marra, Oscar Fernando Pavão dos Santos, Miguel Cendoroglo Neto, Michael B. Edmond 2013, USA20 | [Not mentioned]/ [Not mentioned] / [Positive deviance (PD)] | This study discusses an approach for infection prevention that promotes a safe culture in healthcare settings. In addition, it allows for more resilient cultural changes that aim at improving the frontline compliance with the infection measures. | [Not mentioned] |
|
[Not mentioned] |
| Letícia Lima Aguiar 2019–2020, Brazil14 | [5 papers]/ [1 month]/ [Systematic literature review to conduct the survey questions] | Investigate the nursing care factors that are associated with the safety culture of chronic renal patients on hemodialysis. | Factors called ‘causal factors’ that were presented above 50% of the papers were selected. As a result, “effect of falls reduction” was described as a risk factor; “vascular access infections”, “medication errors”, and “hypotension” as crippling factors; and “adequate staffing” and “providing security protocols, practices, and guidelines” as safety culture strengthening factors. |
|
The study was limited to the hemodialysis nurse’s safety care in Brazil and Latin America. |
| Samuel A Silver, Alison Thomas, Andrea Rathe, Pamela Robinson, Ron Wald, Ziv Harel, and Chaim M Bell 2015, Canada15 | [20 nurses]/ [Not mentioned]/ [Delphi process based on RAND method to evaluate and review the checklist] | Foster a Hemodialysis Safety Checklist (Hemo Pause) for everyday use by nurses and patients. | From the 31 parameters founded, 19 was chosen to get the agreement from the team and Nephrology personnel which got higher than 75The result assigning the errors based on their importance using FMEA, patient body weight errors represent the highest; dysfunction/rupture of the catheter; and needle extravasation represent the lowest.% agreement. |
|
|
| María Dolores Arenas Jiménez, Gabriel Ferre, Fernando Álvarez-Ude 2017, Spain12 | [97 hemodialysis patient from 35 dialysis centers]/ [Not mentioned]/ [Failure mode and effect analysis FMEA technique] | Identify drug errors that may occur in hemodialysis systems, as well as underlying actual or possible errors, and evaluate their magnitude, frequency, and identification, using the Failure Mode and Effects Analysis (FMEA) method to determine their objectives. | As a result of prioritizing errors using FMEA, errors attributable to patient body weight rank highest, catheter dysfunction/rupture rank second, and needle extravasation rank third. |
|
|
| Hu-Chen Liu and Kenji Itoh 2013, Japan28 | [24 papers]/ [Not mentioned]/ [Questionnaire survey to dialysis experts, systematic literature review to select indicators] | Evaluate the performance of the dialysis department and comprehensively support them not only from quality and safety but also from the patients and employee’s satisfaction. | Most of the indicators were assigned negatively (meaningless to management dialysis). Patients, on the other hand, listed several important metrics, such as indicators relating to patient care and patient safety, which are crucial for health department management. |
|
|
| Lucia New, Donna Goodridge, Joanne Kappel, Gary Groot and Roy Dobson 2019, Canada25 | [30 patients]/ [5 months]/ [Face to face interview with patients (recorded interview)] | Study CKD patients’ experience in the safety of dialysis centers and reporting the incident that occurs during their treatment period. |
|
|
|
Discussion
We conducted a systematic review to identify ways of improving the safety culture at hemodialysis settings. We identified 17 eligible studies that had quantitative and qualitative data and extracted best practices to achieve an almost “zero error” hemodialysis environment.
Three papers discussed how to improve and ease the process of the dialysis nurse’s job in general13–15 and concluded that developing an effective analysis tool that is affected by “predisposing factors, medication errors, disabling factors and reinforcing factors” to improve the nursing care in hemodialysis settings is an important first step. Two studies were concerned about the nurse’s role in the management of continuous hemodialysis in the intensive care unit (ICU) setting.16,17 Process improvements identified for ICU nurses working for continuous hemodialysis patients includes establishing a strong background and knowledge about the technologies they are working with, and strong training so they can anticipate any unexpected patient case. Along with this, a collaborative model should be adopted in the sector, including a systematic strategy to support and assist new nurses.
Second, designing a Hemo Pause Checklist for daily use by nurses can reduce adverse events and strengthening the safety culture in the dialysis unit by. However, more established and demonstrated patient safety estimation devices might be required. These improvements should be implemented to get the process done in the most efficient way and to prevent the errors that may occur because of a failure to follow protocols. Another three papers18–20 discussed strategies for preventing infections in hemodialysis units to improve the patient safety culture in hemodialysis units. For instance, infections may be prevented by using methods such as system thinking, recognizing the complexity of the system and interrelatedness among various system components.
Three studies identified other points of risk for adverse patient events in hemodialysis settings, such as threats to safety during a transition of care in the dialysis settings.21–23 These three papers advised implementing the root cause analysis method to determine system and process issues that lead to adverse events. One study used Failure Mode and Effect Analysis (FMEA) to find the severity, frequency and detection of each event and assigned real errors, then implemented the prevention measure that could improve patient safety culture in hemodialysis settings.19 The role of effective communication in improving the safety culture in hemodialysis settings was emphasized in multiple studies,19,21,24,25 including the responsibility of leadership to encourage open communication and mutual trust with and between employees.8,20,24 Open communication will lead to a positive safety climate and therefore will promote a free-blame environment.26,27 Another study emphasized the importance of patient and staff communication as it considered the vital role of patients’ feedback during treatment in improving safety.25 A final article suggested studying effective performance indicators and implementing them to solve any future challenges hemodialysis settings may face.28
Limitations
The search to two databases (PubMed and Scopus) because they were considered suitable for gathering all qualifying papers by the proposed topic and objectives, but this restriction may have missed some relevant articles, and some identified articles were not accessible to the research team. The search was narrowed to those published in journals and the English language. An important limitation was that most of the papers did not test their proposed improvements in the healthcare settings, so we were not able to discern the outcome of each strategy. Further, limited evidence is available regarding the role of different stakeholders, such as physicians and nurses, in the safety culture assessment and improvement. Ultimately, the inferences that can be drawn from available evidence are limited by the paucity of published research related to the safety culture in hemodialysis settings.
Conclusion
Improving hemodialysis patient safety is a vital priority. The category of papers included in this review showed that risks to patient safety may relate to transitions of care, failure to use checklists to ensure compliance with protocols, and communication gaps between the hospital staff, and between the staff and patients. Therefore, this review showed that efforts should be made to overcome these gaps. Moreover, it also highlighted how to prevent infections from happening in the beginning, by implementing these improvements; the safety culture in the hemodialysis settings will turn into an almost “zero error” environment and a safe place for the patients to receive their treatments. Finally, based on our knowledge, this is the first systematic review that clustered diverse improvement strategies from selected studies in the literature and reviewed them to improve safety culture in the hemodialysis settings. This study may be a starting point for upcoming studies concerned with improving the safety culture in hemodialysis settings.
Future studies can benefit from testing the improvement strategies that were identified to prove their effectiveness, as most of the strategies proposed in this systematic literature review were not tested for impact on outcomes. Further, a comparison analysis between the proposed strategies can be conducted to provide the decision-makers with the best strategy to enhance safety culture.
Acknowledgement
This work was supported, in part, by the Khalifa University of Science and Technology under Award RCII-2019-002- Research Center for Digital Supply Chain and Operations Management. The funding body had no direct involvement in the design, data collection, analysis, and interpretation or in writing the manuscript. Professor Krista Lentine is supported by the Mid-America Transplant / Jane A. Beckman Endowed Chair in Transplantation.
Disclosure
Professor Krista Lentine reports personal fees from CareDx, personal fees from Sanofi, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Waterson P, ed. Patient Safety Culture: Theory, Methods and Application. 1st ed. CRC Press; 2018. doi: 10.1201/9781315599717 [DOI] [Google Scholar]
- 2.Reis CT, Paiva SG, Sousa P. The patient safety culture: a systematic review by characteristics of Hospital Survey on Patient Safety Culture dimensions. Int J Qual Health Care. 2018;30:660–677. doi: 10.1093/intqhc/mzy080 [DOI] [PubMed] [Google Scholar]
- 3.Simsekler MCE, Qazi A, Alalami MA, Ellahham S, Ozonoff A. Evaluation of patient safety culture using a random forest algorithm. Reliability Eng Sys Safety. 2020;204:107186. doi: 10.1016/j.ress.2020.107186 [DOI] [Google Scholar]
- 4.Alrowely Z, Baker OG. Assessing Building Blocks for Patient Safety Culture—a Quantitative Assessment of Saudi Arabia. RMHP. 2019;12:275–285. doi: 10.2147/RMHP.S223097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinangil A, Koc Y, Unsal A, et al. Effects of infectious complications on patients’ survival in peritoneal dialysis. Eur Rev Med Pharmacol Sci. 2013;17(8):1064. [PubMed] [Google Scholar]
- 6.Hao H-S, Gao H, Li T, Zhang D. Assessment and Comparison of Patient Safety Culture Among Health-Care Providers in Shenzhen Hospitals. RMHP. 2020;13:1543–1552. doi: 10.2147/RMHP.S266813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aljaffary A, Yaqoub FA, Madani RA, Aldossary H, Alumran A. Patient Safety Culture in a Teaching Hospital in Eastern Province of Saudi Arabia: assessment and Opportunities for Improvement. RMHP. 2021;14:3783–3795. doi: 10.2147/RMHP.S313368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. J Clin Epidemiol. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009; 6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Millson T, Hackbarth D, Bernard HL. A demonstration project on the impact of safety culture on infection control practices in hemodialysis. Am J Infect Control. 2019;47(9):1122–1129. doi: 10.1016/j.ajic.2019.02.026 [DOI] [PubMed] [Google Scholar]
- 11.Davis K, Harris KG, Mahishi V, Bartholomew EG, Kenward K. Perceptions of Culture of Safety in Hemodialysis Centers. Nephrology Nursing Journal: Journal of the American Nephrology Nurses’ Association. 2016;43(2):119–129. [PubMed] [Google Scholar]
- 12.Arenas Jiménez MD, Ferre G, Álvarez-Ude F. Strategies to increase patient safety in haemodialysis: application of the modal analysis system of errors and effects (FEMA system). Nefrol Engl Ed. 2017;37(6):608–621. doi: 10.1016/j.nefroe.2017.11.011 [DOI] [PubMed] [Google Scholar]
- 13.Thomas A, Silver SA, Rathe A, et al. Feasibility of a hemodialysis safety checklist for nurses and patients: a quality improvement study. Clin Kidney J. 2016;9(3):335–342. doi: 10.1093/ckj/sfw019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aguiar LL, Silva RA, Melo GAA, Pereira FGF. Factors related to hemodialysis safety culture: integrative literature review. Rev Bras Enferm. 2020;73(6):e20190624. doi: 10.1590/0034-7167-2019-0624 [DOI] [PubMed] [Google Scholar]
- 15.Silver SA, Thomas A, Rathe A, et al. Development of a Hemodialysis Safety Checklist Using a Structured Panel Process. Can J Kidney Health Dis. 2015;2:39. doi: 10.1186/s40697-015-0039-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andrade de BRP, Barros de F. Intensivist nurse performance in the collaborative model of continuous hemodialysis: links with patient safety. Rev Esc Enferm USP. 2019;53:e03475. doi: 10.1590/s1980-220x2018004603475 [DOI] [PubMed] [Google Scholar]
- 17.Andrade de BRP, Barros F. Experience Of Nurses In The Management Of Continuous Hemodialysis And Its Influences On Patient Safety. Texto Contexto - Enferm. 2019;28:e20180046. doi: 10.1590/1980-265x-tce-2018-0046 [DOI] [Google Scholar]
- 18.Wong LP. Achieving dialysis safety: the critical role of higher‐functioning teams. Semin Dial. 2019;32(3):266–273. doi: 10.1111/sdi.12778 [DOI] [PubMed] [Google Scholar]
- 19.Wong LP. Systems Thinking and Leadership: how Nephrologists Can Transform Dialysis Safety to Prevent Infections. Clin J Am Soc Nephrol. 2018;13(4):655–662. doi: 10.2215/CJN.09740917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marra AR, Pavão Dos Santos OF, Cendoroglo Neto M, Edmond MB. Positive Deviance: a New Tool for Infection Prevention and Patient Safety. Curr Infect Dis Rep. 2013;15(6):544–548. doi: 10.1007/s11908-013-0372-y [DOI] [PubMed] [Google Scholar]
- 21.Thomas-Hawkins C, Flynn L. Patient Safety Culture and Nurse-Reported Adverse Events in Outpatient Hemodialysis Units. Res Theory Nurs Pract. 2015;29(1):53–65. doi: 10.1891/1541-6577.29.1.53 [DOI] [PubMed] [Google Scholar]
- 22.Kliger AS. Maintaining Safety in the Dialysis Facility. Clin J Am Soc Nephrol. 2015;10(4):688–695. doi: 10.2215/CJN.08960914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrick R, Kliger A, Stefanchik B. Patient and Facility Safety in Hemodialysis: opportunities and Strategies to Develop a Culture of Safety. Clin J Am Soc Nephrol. 2012;7(4):680–688. doi: 10.2215/CJN.06530711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Di Benedetto A, Pelliccia F, Moretti M, et al. What causes an improved safety climate among the staff of a dialysis unit? Report of an evaluation in a large network. J Nephrol. 2011;24(5):604–612. doi: 10.5301/JN.2011.6306 [DOI] [PubMed] [Google Scholar]
- 25.New L, Goodridge D, Kappel J, Groot G, Dobson R. “I just have to take it” – patient safety in acute care: perspectives and experiences of patients with chronic kidney disease. BMC Health Serv Res. 2019;19(1):199. doi: 10.1186/s12913-019-4014-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palaian S, Buabeid M, Ashames A. Patient Safety Culture in Handling Prescriptions and Interprofessional Collaboration Practices Amongst Community Pharmacists: an Investigative Simulated Patient Study from the United Arab Emirates. RMHP. 2020;13:3201–3209. doi: 10.2147/RMHP.S282571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Simsekler MCE. The Link Between Healthcare Risk Identification and Patient Safety Culture. Int J Qual Health Care. 2019;32:574–587. doi: 10.1108/IJHCQA-04-2018-0098 [DOI] [PubMed] [Google Scholar]
- 28.Liu HC, Itoh K. Conceptual Framework for Holistic Dialysis Management Based on Key Performance Indicators: conceptual Framework of Dialysis Management. Ther Apher Dial. 2013. doi: 10.1111/1744-9987.12019 [DOI] [PubMed] [Google Scholar]