Abstract
Rhabdomyosarcoma accounts for almost 20% of all primary malignant neoplasms of the heart. These tumors usually arise from the ventricular walls. In adult patients, they sometimes arise from the atrial walls and mimic atrioventricular valve stenosis. We describe a case of left atrial rhabdomyosarcoma that presented as severe mitral stenosis and required emergency surgery. The atrial mass was detected by transthoracic and transesophageal echocardiography, but only histopathology confirmed the nature of the lesion. Although rhabdomyosarcomas of the heart are highly lethal, operation is indicated for emergency cases, in order to clarify the diagnosis, relieve symptoms, and improve short-term survival.
Key words: Diagnosis; heart neoplasms, pathology; heart neoplasms/surgery; rhabdomyosarcoma; sarcoma/classification
Primary malignant neoplasms of the heart are rare. Rhabdomyosarcoma accounts for about 20% of these lesions and is the most common. Symptoms differ in accordance with the location of the mass; unfortunately, by the time the patient becomes symptomatic, the tumor usually has metastasized to other organs. Diagnosis frequently is obtained by transthoracic or transesophageal echo-cardiography, but there is no consensus about whether to treat or how to treat, because the benefits of surgery and postoperative chemotherapy or radiotherapy are unclear, and long-term prognosis is poor.
We describe a case of rhabdomyosarcoma that presented in an unusual manner and required emergency surgery.
Case Report
In February 1998, a 68-year-old woman was referred to our unit on an emergency basis with a diagnosis, obtained by transthoracic echocardiography, of severe mitral valve stenosis and large thrombus formation in the left atrium. During the previous 6 months, she had complained of increasing shortness of breath, dyspnea on exertion, and chest pain. Thallium scintigraphy scan performed in August 1997 had revealed good left ventricular function and no signs of myocardial ischemia.
Upon physical examination, the patient was dyspneic at rest, sweaty, and hypotensive. Peripheral arterial pulses were present. Pulmonary edema and bilateral pleural effusion were diagnosed by clinical examination. The liver was palpable about 5 cm from the lower costal border. Electrocardiography showed sinus tachycardia (>120 beats/minute). Chest radiography demonstrated cardiomegaly and confirmed both pulmonary edema and pleural effusions. Transthoracic echocardiography revealed non-calcified, moderate mitral stenosis (mitral area, 1.4 cm2) and a large mass. This mass was attached to the posterior wall of the left atrium, mimicking a large thrombus, and it extended to the posterior mitral valve leaflet. Coronary angiography, performed because of the patient's history of chest pain, showed isolated critical stenosis of the left anterior descending (LAD) coronary artery. Left ventriculography was not performed because of the patient's rapid hemodynamic deterioration.
The patient was immediately transferred to the operating room. A median sternotomy was performed, and she underwent cardiopulmonary bypass. Moderate systemic hypothermia (30 °C) and cold crystalloid cardioplegia (with St. Thomas's No. 2 solution) were used for myocardial protection. Left atriotomy revealed a very large mass (9 × 8 × 5 cm) that appeared to be capsulated. It adhered to the posterior wall of the left atrium, partially obstructing the right pulmonary veins and reducing the mitral valve area. We excised the mass except for the affected part of the atrial wall (Fig. 1), performed mitral valve commissurotomy, and grafted the LAD with autologous saphenous vein. Cardiopulmonary bypass time was 96 minutes and cross-clamp time was 52 minutes.
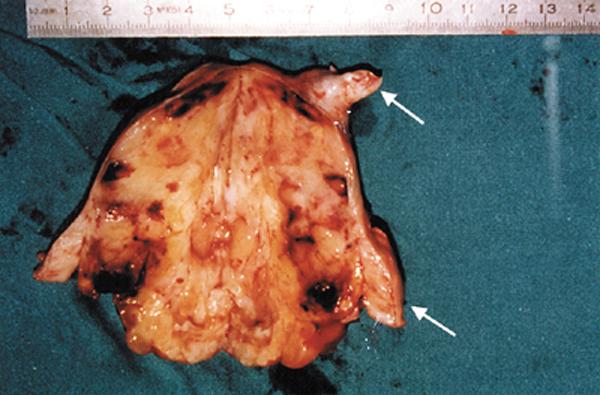
Fig. 1 Internal surface of the neoplasm (in cross section): there are both necrotic and hemorrhagic areas. Arrows indicate obstruction of the right pulmonary veins.
The patient was easily weaned from cardiopulmonary bypass and was transferred to the intensive care unit without significant inotropic support. She was extubated 5 hours later. Liver failure syndrome with jaundice and metabolic deterioration developed on the 3rd postoperative day. Liver ultrasonography showed multiple nodular lesions, and a computed tomographic scan revealed diffuse metastatic lesions in the liver and lungs. The syndrome became progressively more severe, and the patient died on the 12th postoperative day.
Histologic analysis of the mass revealed roundish tumor cells with pleomorphic nuclei and large eosino-philic cytoplasm resembling myoblasts (Fig. 2A). Monoclonal antibody tests (positive for desmin, vimentin, and muscle actin) confirmed the histologic diagnosis of rhabdomyosarcoma with embryonic differentiation (Fig. 2B).
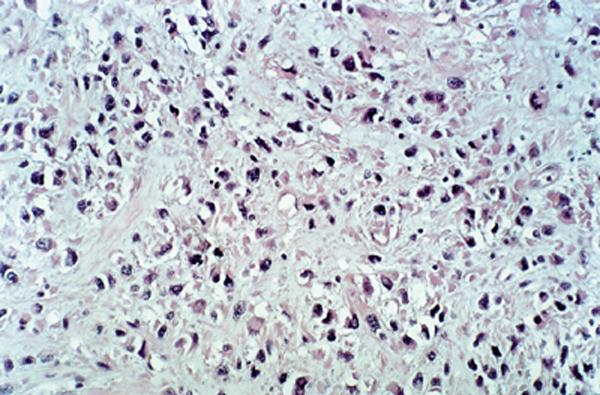
Fig. 2A Tumor cells are roundish and have pleomorphic nuclei and large eosinophilic cytoplasm (H&E, ×340). Tadpole-shaped rhabdomyoblasts are visible.
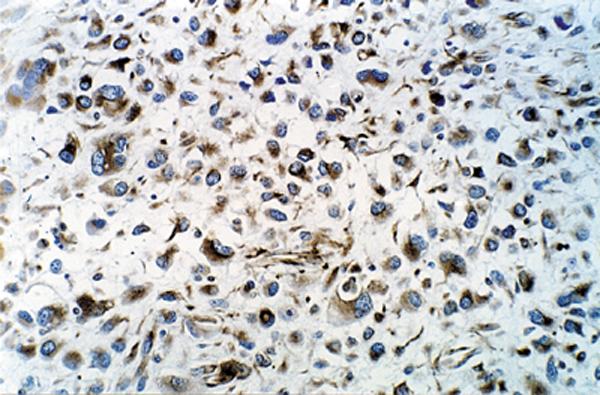
Fig. 2B Diffuse intracytoplasmic reaction positive for desmin (immunoperoxidase stain for desmin, ×610).
Discussion
Malignant neoplasms constitute about 25% of all primary cardiac tumors. 1–3 Nearly all are sarcomas, and of these rhabdomyosarcomas make up almost 20%. 1 These tumors usually arise from the ventricular walls, and they frequently interfere with valvular motion because of their intracavitary bulk. Involvement of the ventricular septum and ventricular walls, which often occurs, makes complete excision impossible. 4,5 In adult patients, these tumors sometimes arise from the atrial walls and mimic atrioventricular valve stenosis. 6–8
Like other sarcomas, rhabdomyosarcoma of the heart is very aggressive, and, as in our patient, often presents as acute cardiac failure. By the time cardiac symptoms become evident, metastatic lesions are usually diffuse. Although survival of up to 5 years has been reported, 9 prognosis is very poor: patients usually survive less than 1 year, in spite of excision of the primary tumor and subsequent radiation and chemo-therapy.
Transthoracic and transesophageal echocardiography can diagnose the presence of the mass, but these imaging techniques rarely define its true nature, especially when it is located in the atria. In those cases, the tumor is usually given a presumptive diagnosis of thrombus or myxoma, and the patient is sent to surgery.
Nuclear magnetic resonance imaging can be useful in defining the nature of an intracardiac mass, especially when its anatomical location is unusual, as it was in our patient.
Despite the poor mid-term prognosis, surgery is indicated to remove the mass, thereby relieving acute symptoms and extending the life of the patient by perhaps a few months. 10–12
In our case, the unusual presentation of a rapidly evolving mitral valve stenosis led us to consider thrombus formation: although the patient had no significant arrhythmias, we suspected an undiagnosed paroxysmal atrial fibrillation.
Although rhabdomyosarcomas of the heart are highly lethal, we conclude on the basis of our experience that operation is indicated for emergency cases, in order to clarify the diagnosis, provide palliation, and improve short-term survival.
Footnotes
Address for reprints: Paolo Masiello, MD, Piazza V. Veneto 39, 84123 – Salerno, Italy
References
- 1.McAllister HA Jr, Fenoglio JJ Jr. Tumors of the cardiovascular system. Fascicle 15, second series. In: Atlas of tumor pathology. Washington, DC: Armed Forces Institute of Pathology, 1978.
- 2.Silverman NA. Primary cardiac tumors. Ann Surg 1980: 191:127–38. [DOI] [PMC free article] [PubMed]
- 3.Fine G. Primary tumors of the heart and pericardium. In: Fenoglio CM, Wolff M, editors. Progress in surgical pathology. Vol. 3. New York: Masson Publishing, 1981:37–63.
- 4.Burke AP, Cowan D, Virmani R. Primary sarcomas of the heart. Cancer 1992;69:387–95. [DOI] [PubMed]
- 5.Poole GV Jr, Meredith JW, Breyer RH, Mills SA. Surgical implications in malignant cardiac disease. Ann Thorac Surg 1983;36:484–91. [DOI] [PubMed]
- 6.Hui KS, Green LK, Schmidt WA. Primary cardiac rhabdomyosarcoma: definition of a rare entity. Am J Cardiovasc Pathol 1988;2:19–29. [PubMed]
- 7.Putnam JB Jr, Sweeney MS, Colon R, Lanza LA, Frazier OH, Cooley DA. Primary cardiac sarcomas. Ann Thorac Surg 1991;51:906–10. [DOI] [PubMed]
- 8.Villasenor HR, Fuentes F, Walker WE. Left atrial rhabdomyosarcoma mimicking mitral valve stenosis. Tex Heart Inst J 1985;12:107–10. [PMC free article] [PubMed]
- 9.Miralles A, Bracamonte L, Soncul H, Diaz del Castillo R, Akhtar R, Bors V, et al. Cardiac tumors: clinical experience and surgical results in 74 patients. Ann Thorac Surg 1991; 52:886–95. [DOI] [PubMed]
- 10.Chitwood WR Jr. Cardiac neoplasms: current diagnosis, pathology, and therapy. J Card Surg 1988;3:119–54. [DOI] [PubMed]
- 11.Murphy MC, Sweeney MS, Putnam JB Jr, Walker WE, Frazier OH, Ott DA, et al. Surgical treatment of cardiac tumors: a 25-year experience. Ann Thorac Surg 1990;49: 612–8. [DOI] [PubMed]
- 12.Mandard AM, Petiot JF, Marnay J, Mandard JC, Chasle J, de Ranieri E, et al. Prognostic factors in soft tissue sarcomas. A multivariate analysis of 109 cases. Cancer 1989;63: 1437–51. [DOI] [PubMed]


