Abstract
Aims
Although the delivery catheter system for pacemaker-lead implantation is a new alternative to the stylet system, no randomized controlled trial has addressed the difference in right ventricular (RV) lead placement accuracy to the septum between the stylet and the delivery catheter systems. This multicentre prospective randomized controlled trial aimed to prove the efficacy of the delivery catheter system for accurate delivery of RV lead to the septum.
Methods and results
In this trial, 70 patients (mean age 78 ± 11 years; 30 men) with pacemaker indications of atrioventricular block were randomized to the delivery catheter or the stylet groups. Right ventricular lead tip positions were assessed using cardiac computed tomography within 4 weeks of pacemaker implantation. Lead tip positions were classified into RV septum, anterior/posterior edge of the RV septal wall, and RV free wall. The primary endpoint was the success rate of RV lead tip placement to the RV septum.
Results
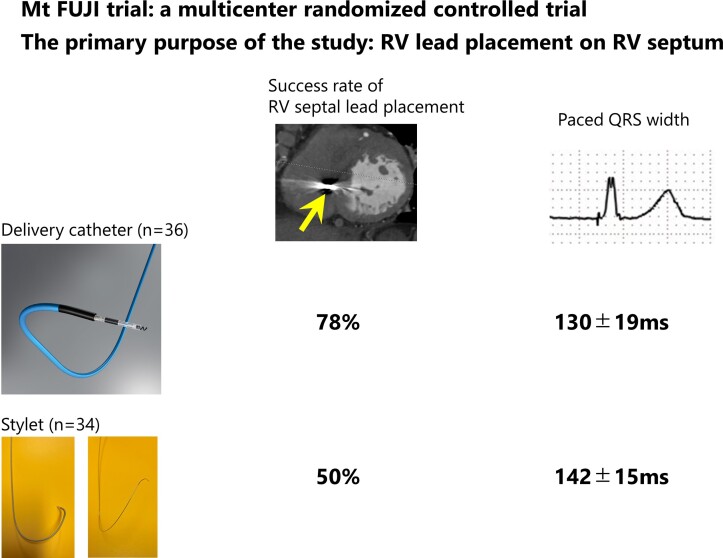
Right ventricular leads were implanted as per allocation in all patients. The delivery catheter group had higher success rate of RV lead deployment to the septum (78 vs. 50%; P = 0.024) and narrower paced QRS width (130 ± 19 vs. 142 ± 15 ms P = 0.004) than those in the stylet group. However, there was no significant difference in procedure time [91 (IQR 68–119) vs. 85 (59–118) min; P = 0.488] or the incidence of RV lead dislodgment (0 vs. 3%; P = 0.486).
Conclusion
The delivery catheter system can achieve a higher success rate of RV lead placement to the RV septum and narrower paced QRS width than the stylet system.
Trial registration number
jRCTs042200014 (https://jrct.niph.go.jp/en-latest-detail/jRCTs042200014)
Keywords: Pacemaker, Atrioventricular block, Right ventricular septal pacing, Delivery catheter, Stylet
Graphical Abstract
Graphical Abstract.
Outcome comparison between delivery catheter and stylet systems. The delivery catheter system can achieve a higher RV lead placement on the RV septum success rate and a narrower paced QRS width than the stylet system. RV, right ventricular.
What’s new?
Mt FUJI trial was the first randomized controlled study to reveal a higher success rate of RV lead placement to the RV septum compared with the stylet system in patients with pacemaker indications due to atrioventricular block.
Paced QRS duration was narrower in the delivery catheter group than in the stylet group.
A delivery catheter system may be considered as the primary choice for achieving RV septal pacing.
Introduction
Although pacemaker implantation is the cornerstone of treatment for atrioventricular block (AVB), some patients experience pacing-induced cardiomyopathy, leading to a decrease in LV ejection fraction and an increase in the incidence of new-onset atrial fibrillation and heart failure. This could be due to dyssynchronous left ventricular contractions caused by right ventricular (RV) apical pacing.1 The RV septum has been considered as an alternative pacing site with less dyssynchrony compared with the RV apex because of its proximity to the conduction system. Although some studies have reported that RV septal pacing could reduce LV dyssynchrony,2,3 a retrospective propensity-matched case–control study4 and a prospective randomized controlled trial5 have failed to show the prognostic benefit of RV septal pacing compared with RV apical pacing. This may be partially due to the low success rate of RV lead placement on the RV septum suggested by a study assessing the accuracy of septal lead placement by computed tomography (CT).6–8 We recently reported that unexpected RV free-wall pacing could attenuate RV septal pacing efficacy in patients undergoing fluoroscopic-guided RV lead implantation on the RV septum.7 Some techniques, including the use of the right anterior oblique (RAO) view,6,9 individualized left anterior oblique (LAO) view,10 and right ventriculography11 have been advocated to achieve a higher success rate of RV septal pacing. One possible breakthrough is the use of a delivery catheter system. Our single-centre case–control study reported that catheter-based RV lead implantation could achieve more accurate RV lead placement on the RV septum assessed by CT, than the traditional stylet-based technique.12 However, this result has not been confirmed by a prospective randomized controlled study. Therefore, this multicentre prospective randomized controlled trial named Mt FUJI (coMparison of delivery caTheter- and stylet-based RV lead placement at the RV septum under FlUoroscopic guidance Judged by cardIac CT) aimed to prove the efficacy of the delivery catheter system for accurate RV lead anchoring to the RV septum.
Methods
Study design
The details of the design and rationale of the Mt FUJI trial have been previously described.13 Briefly, the Mt FUJI trial is a multicentre, prospective, single-blind, randomized controlled trial to compare the accuracy of RV lead deployment to the RV septum between delivery catheter- and stylet-based pacemaker implantation procedures. The trial enrolled 70 patients from seven tertiary hospitals in Japan from June 2020 to March 2021. Patients were eligible if they had pacemaker indication due to AVB, age > 20 years, and provided written informed consent. The exclusion criteria included LV ejection fraction <35%, persistent atrial fibrillation, congenital heart disease, prior open-heart surgery, and chronic renal failure on haemodialysis. Patients were randomly assigned to either the delivery catheter or stylet group. The patients in this trial were blinded to the treatment allocation. However, practitioners were not blinded to treatment allocation because of the nature of the intervention. The primary endpoint was the success rate of RV lead tip deployment onto the RV septum confirmed by cardiac CT. The secondary endpoints included paced QRS width, procedure time, fluoroscopic time, number of attempts to affix the RV lead, RV lead parameters including R-wave amplitude, pacing threshold, impedance, and incidence of RV lead dislodgment at discharge. All study activities were coordinated by the Center for Clinical Research at the Hamamatsu University Hospital in Hamamatsu, Shizuoka, Japan. This study complied with the Declaration of Helsinki and the Clinical Trials Act. The study protocol was approved by the Clinical Research Review Board of Hamamatsu University School of Medicine (approval number: C010-2019) and by the hospital administrator in each participating hospital. Written informed consent was obtained from all patients or their legal guardians before inclusion and randomization.
Pacemaker implantation procedure
The details of the pacemaker implantation procedure of the Mt FUJI trial have been previously described.13 Briefly, pacemaker implantation was performed under local anaesthesia by experienced operators. An RV lead was intended to be placed on the RV septum in all patients under fluoroscopic guidance. Left bundle branch area pacing (LBBAP) or His-bundle pacing was not attempted in any cases. An LAO view of 40–60° was used to confirm whether the RV tip was facing towards the spine. In the RAO view of 30°, the cardiac silhouette was divided perpendicularly into quadrants. The tip of the RV lead was intended to anchor to the second or the third quadrant.6 However, the RV lead was sometimes screwed in at the stable position to avoid the lead dislodgement, even if the location of the RV lead tip seemed to be out of the target position in the LAO and RAO views. In the stylet group, a conventional manually shaped stylet, a steerable stylet (Locator™; Abbott), or a preshaped stylet (Ez stylet™; Japan Lifeline, Tokyo, Japan) was used. The selection of stylet was left to the operator’s discretion. C315-HIS (Medtronic, Minneapolis, MN, USA) was recommended as the delivery catheter, and the use of other delivery catheters, such as C315-S5 and C315-S10, was allowed as a second option.
Endpoint measures
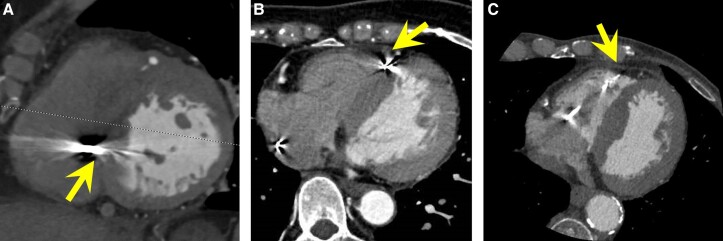
Electrocardiography (ECG)-gated cardiac CT was performed in all patients within 4 weeks after pacemaker implantation. The use of the contrast medium was recommended unless the study patients had renal dysfunction or severe allergic diseases. Computed tomography scans were analysed in the axial view or multiplanar-reconstructed views. Two trained investigators (H.H. and A.M.), without knowledge of the allocation and clinical outcomes, independently evaluated the CT scans. The third electrophysiological specialist from a different hospital (M.S.) was consulted when there was interobserver disagreement. The lead tip positions were classified as RV septum, anterior/posterior edge of the RV septal wall, and RV free wall (Figure 1). If patients experienced RV lead dislodgment before undergoing ECG-gated cardiac CT, we considered them to have failed in RV septal lead placement, irrespective of the result of a re-implantation procedure.
Figure 1.
Representative cases of RV lead positions assessed by ECG-gated CT. (A) RV septum, (B) anterior edge of the RV septal wall, and (C) RV free wall. CT, computed tomography; ECG, electrocardiography; RV, right ventricular.
Paced QRS width was measured by a physician who was not involved in the pacemaker implantation. The time from skin incision to skin closure was measured as surgery time, and fluoroscopic time was calculated using the fluoroscopy system. We counted the number of attempts to screw in the RV lead during the procedure. Right ventricular lead parameters, including the R-wave amplitude, pacing threshold, and impedance, were measured immediately after implantation and at discharge from the hospital using a pacemaker programmer. Right ventricular lead dislodgment at discharge was diagnosed when chest X-ray showed apparent lead perforation or lead dislocation, or abnormal RV lead parameters including an R-wave amplitude of <1.0 mV or pacing threshold of >3.0 V with a nominal pulse width were observed.
Statistical analysis
According to the previous observational studies,6,7 the successful deployment of the RV lead tip to the RV septum was estimated to be 85% in the delivery catheter group and 50% in the stylet group. A sample size of 70 patients (35 patients in the delivery catheter group and 35 patients in the stylet group) was chosen to obtain an 80% power and a confidence interval of 95% for detecting differences between the two groups after making allowance for a 5% dropout rate after randomization.
Intention-to-treat analyses were performed between the delivery catheter and the stylet groups. Continuous variables are expressed as mean ± standard deviation or median (interquartile range) and were compared using the unpaired t-test or Mann–Whitney U test. All categorical variables are expressed as raw numbers and percentages and analysed using Fisher’s exact test. Statistical significance was defined as a two-tailed P-value <0.05. All analyses were performed using the R program v3.6.3 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics
A total of 70 patients (mean age, 78 ± 11 years; 30 men) were enrolled in the Mt FUJI trial, and 36 were randomly allocated to the delivery catheter group. Patients’ baseline characteristics are shown in Table 1. The mean height and weight were 155 ± 10 cm and 53 ± 12 kg, respectively. The mean left ventricular ejection fraction was 64.4 ± 8.1%. A temporary pacing catheter was used in 25 (36%) patients before the pacemaker implantation procedure. There were no significant differences in baseline characteristics between the delivery catheter and stylet groups (Table 1).
Table 1.
Baseline characteristics between delivery catheter and stylet group
| Variables | All (n = 70) | Delivery catheter (n = 36) | Stylet (n = 34) |
|---|---|---|---|
| Age (years) | 77.8 ± 11.4 | 77.2 ± 13.0 | 78.5 ± 9.6 |
| Male sex, n (%) | 30 (43%) | 15 (42%) | 15 (44%) |
| Height (cm) | 155 ± 10 | 154 ± 11 | 155 ± 10 |
| Weight (kg) | 53 ± 12 | 51 ± 12 | 56 ± 12 |
| Body mass index (m/kg2) | 22.2 ± 3.7 | 21.4 ± 3.4 | 23.0 ± 3.9 |
| Severity of atrioventricular block | |||
| ȃMobitz II-degree, n (%) | 2 (3%) | 1 (3%) | 1 (3%) |
| ȃAdvanced, n (%) | 21 (30%) | 12 (33%) | 9 (27%) |
| ȃComplete, n (%) | 47 (67%) | 23 (64%) | 24 (71%) |
| Comorbid disease | |||
| ȃHypertension, n (%) | 53 (76%) | 26 (72%) | 27 (79%) |
| ȃDyslipidaemia, n (%) | 24 (34%) | 14 (39%) | 10 (29%) |
| ȃDiabetes mellitus, n (%) | 15 (21%) | 8 (22%) | 7 (21%) |
| ȃChronic kidney disease, n (%) | 20 (29%) | 7 (19%) | 13 (38%) |
| ȃStructural heart disease, n (%) | 18 (26%) | 11 (31%) | 7 (21%) |
| NYHA class on admission | 2 (1–3) | 2 (1.75–3) | 2 (1–3) |
| Medication | |||
| ȃAntiplatelet agent, n (%) | 17 (24%) | 10 (28%) | 7 (21%) |
| ȃDirect oral anticoagulants, n (%) | 2 (3%) | 2 (6%) | 0 (0%) |
| LVEF (%) | 64.4 ± 8.1 | 65.3 ± 7.6 | 63.4 ± 8.6 |
| ȃLVEF <50%, n (%) | 2 (3%) | 0 (0%) | 2 (6) |
| Temporary pacing catheter before pacemaker implantation, n (%) | 25 (36%) | 15 (42%) | 10 (29%) |
Structural heart disease was defined as a composite of angina pectoris, myocardial infarction, nonischaemic cardiomyopathy, and valvular heart disease.
LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
Pacemaker implantation procedure
In the stylet group, CapSureFIX™ NOVUS (Medtronic), TENDRIL STS 2088TC™ (Abbott, Chicago, IL, USA), Ingevity™ (Boston Scientific, Marlborough, MA, USA), and Solia S™ (Biotronik, Berlin, Germany) leads were used in 6, 10, 8, and 10 patients, respectively. A conventional manually shaped stylet was chosen for 28 patients. A softer stylet was used as a first choice. A steerable stylet (Locator™; Abbott) and a preshaped stylet (Ez stylet™; Japan Lifeline) were selected in three and three patients, respectively. C315-HIS (Medtronic) and 3830 SelectSecure (Medtronic) were used in all patients in the delivery catheter group. C315-S5 and C315-S10 were not used in any patients. Although crossover between stylets and delivery catheters is allowed if RV lead placement using the allocated device is difficult, no crossover occurred in this trial.
The RV lead was deployed to the apex in one patient and the RV outflow tract in one patient after the failure of deployment to the RV septum in the stylet group. Post-hoc analysis of fluoroscopic images showed that the tip of the RV lead was facing towards the spine in the LAO view and positioned at the second or the third quadrant in the RAO view in 35 (97%) and 30 (83%) patients in the delivery catheter group and 31 (91%) and 25 (74%) patients in the stylet group, respectively.
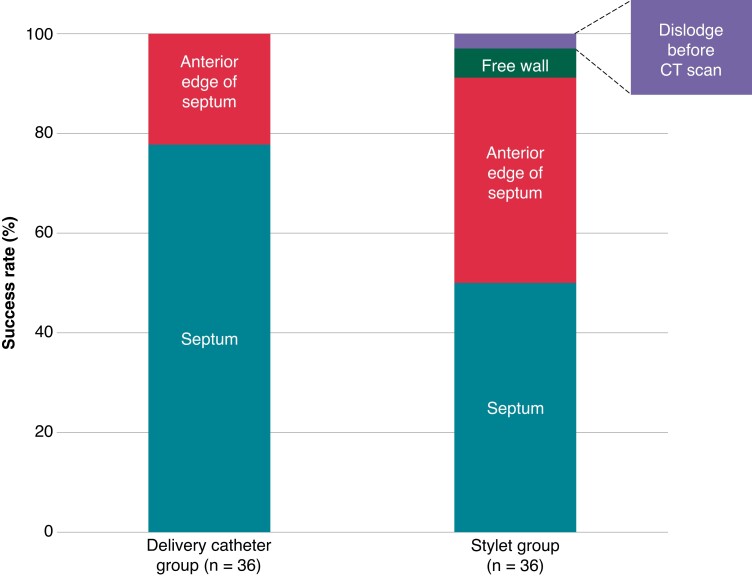
Primary and secondary endpoints
Before undergoing a cardiac CT scan, RV lead dislodgement occurred in one patient in the stylet group. Cardiac CT scans revealed that the tip of RV lead was precisely deployed on the RV septum in 28 (78%) patients in the delivery catheter group and 17 (50%) in the stylet group (P = 0.030) (Graphical Abstract). Of 16 patients in the stylet group whose lead tip was placed out of the RV septum, RV free-wall pacing occurred in two (6%). In contrast, the RV lead tip was placed on the RV free wall in none of the patients in the delivery catheter group (Figure 2). In three and three patients using a steerable stylet and a preshaped stylet, RV lead deployment on RV septum was achieved in one (33%) and one (33%) patient, respectively. The tip of RV lead was unintentionally deployed not on the RV mid-septum but on the right ventricular outflow tract (RVOT) in two patients in the delivery catheter group. These leads tips faced the groove between the septum and free wall.
Figure 2.
Primary endpoint of the Mt FUJI trial. Comparison of RV lead placement on RV septum success rate between the delivery catheter and stylet group. CT, computed tomography; RV, right ventricular.
The secondary endpoints are summarized in Table 2. There was no significant difference in procedure and fluoroscopic times, the number of attempts to screw the RV lead, and RV lead dislodgement between the groups. Conversely, the paced QRS width was narrower in the delivery catheter group than in the stylet group (P = 0.004; Graphical abstract). Unintended physiological pacing occurred in four patients (His-bundle pacing in one and LBBAP in three) in the delivery catheter group. Subgroup analysis was performed in 45 patients whose lead tip of the RV lead was at the RV septum by cardiac CTs (28 patients in the delivery catheter group and 17 patients in the stylet group). The delivery catheter group had a narrower paced QRS width than the stylet group (127 ± 16 vs. 140 ± 14 ms; P = 0.012). The R-wave amplitude and pacing threshold in the delivery catheter group did not significantly differ from the stylet group. No significant difference was observed in lead impedance before discharge between the two groups, although lead impedance at the end of the pacemaker implantation procedure in the delivery catheter group was higher than that in the stylet group.
Table 2.
Secondary endpoints between delivery catheter and stylet group
| Variables | All (n = 70) | Delivery catheter (n = 36) | Stylet (n = 34) | P-value |
|---|---|---|---|---|
| Paced QRS width (ms) | 136 ± 18 | 130 ± 19 | 142 ± 15 | 0.004 |
| Procedure time (min) | 86.0 (64.0–119.8) | 90.5 (67.8–119.3) | 85.0 (59.3–117.5) | 0.488 |
| Fluoroscopic time (min) | 15.5 (11.0–23.0) | 17.5 (12.0–23.4) | 12.5 (10.0–22.3) | 0.129 |
| Number of attempts to screw in RV lead | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.749 |
| Lead parameters at the end of pacemaker implantation procedure | ||||
| ȃR amplitude (mV) | 10.1 ± 4.6 | 10.9 ± 4.3 | 9.3 ± 4.7 | 0.176 |
| ȃThreshold (V) | 0.7 ± 0.3 | 0.7 ± 0.3 | 0.6 ± 0.2 | 0.608 |
| ȃImpedance (Ω) | 657 ± 119 | 690 ± 97 | 622 ± 130 | 0.016 |
| Lead parameters before discharge | ||||
| ȃR amplitude (mV) | 12.7 ± 4.9 | 13.8 ± 4.8 | 11.5 ± 4.8 | 0.079 |
| ȃThreshold (V) | 0.7 ± 0.3 | 0.7 ± 0.3 | 0.8 ± 0.2 | 0.703 |
| ȃImpedance (Ω) | 568 ± 88 | 567 ± 69 | 568 ± 106 | 0.943 |
| RV lead dislodgement, n (%) | 1 (1%) | 0 (0%) | 1 (3%) | 0.486 |
RV, right ventricular.
Adverse events
Eight adverse events from seven patients were reported in the Mt FUJI trial. Right ventricular and right atrial (RA) lead dislodgement and wound adhesion insufficiency were observed in one patient in the stylet group. Fever was observed in two patients in the delivery catheter group. Stroke, acute cholangitis, and RA lead dislodgement were observed in one patient in the stylet group. One patient experienced takotsubo cardiomyopathy after pacemaker implantation in the delivery catheter group. All-cause mortality, cardiac tamponade, pneumothorax, haemothorax, or haematoma were not observed in any of the study participants.
Discussion
Main findings
To the best of our knowledge, the Mt FUJI trial is the first multicentre prospective randomized control study to demonstrate the usefulness of the delivery catheter on the accurate RV septal pacing compared with the stylet system. The main findings of this study were that a higher success rate of RV lead placement on the RV septum and a narrower paced QRS duration was achieved in the delivery catheter group compared with the stylet group. Mt FUJI trial showed the utility of delivery catheter in RV septal pacing.
Methods to improve the success rate of right ventricular septal pacing
The fluoroscopic LAO view is a traditional indicator of successful RV lead placement in the RV septum. However, the success rate of RV lead deployment on RV septum using this method is relatively low.6,7,12 We previously reported that the RV lead was unexpectedly anchored on RV free wall in 8% of study subjects and the occurrence of heart failure hospitalization and cardiac death was higher in those with unexpected RV free-wall pacing than in those with RV septal pacing.7 Therefore, a robust and reproducible method for accurate RV lead deployment to the septum is needed before discussing the beneficial effect of RV septal pacing on pacing-induced cardiomyopathy, as well as reducing incidents of lead perforation14 compared with RV apical pacing. Accurate RV septal pacing may be better than RV apical pacing and even as good as LBBAP or His-bundle pacing but quicker and easier.
Individualized LAO is a refined method to improve the accuracy of fluoroscopy-guided RV septal lead placement.10 The degree of individualized LAO is reported to be >60 degrees in the majority of patients (58%).10 Therefore, LAO of 30°–40° can be insufficient to distinguish the septum from the free wall in most patients. The need for the placement of a guidewire through the superior and inferior vena cava and a lead or catheter in the RV apex to calculate individualized LAO in this method10 may lead to prolongation of procedure and fluoroscopic time.
Right ventriculography is another method to avoid unintended RV lead displacement to the non-septal site. Since the fluoroscopic cardiac silhouette in RAO view of 30° usually does not show the RV contour but the LV contour, right ventriculography helps operators to know the actual RV margin. Shimeno et al.11 reported that RV lead placement targeting the centre of the RV assessed by right ventriculography obtained at an RAO view of 30° could achieve successful RV lead deployment on RV septum in 98% of patients. However, since a contrast medium is needed, performing right ventriculography may be hesitated in patients with renal dysfunction, allergy to contrast, or bronchial asthma. Burri et al.9 simply showed that aiming to place the lead at the centre of the cardiac silhouette in RAO of 30°–40° view resulted in the accurate RV septal pacing in 93% of the patients. However, lead dislodgement occurred in 3 (5%) of 66 patients whose RV lead was anchored by the fluoroscopic RAO/LAO guidance; these findings implied that anchoring the RV lead on the RV septum using the stylet system could be difficult in some patients due to the instability.
Delivery catheters have recently become available for pacemaker-lead implantations. We recently demonstrated that delivery catheter-based RV lead placement could achieve more accurate RV lead anchoring to the RV septum than a stylet-based approach in a single-centre retrospective cohort.12 A delivery catheter is a simple and relatively easy method without a need for individualized LAO or right ventriculography.
Difference between the delivery catheter and stylet system
One of the reasons for the low RV septal implantation success rate in previous reports may be the technical difficulty of the stylet system. In fact, our findings showed that the prevalence of the RV lead placement at the fluoroscopic target area was lower in the stylet system than in the delivery catheter system. The lead is controlled by a preshaped stylet; however, the shape of the stylet is usually attenuated when inserted into the lead due to the relatively soft nature of the stylet to decrease the risk of perforation. In addition, strong backup cannot be expected because the sheath can only be inserted as far as the superior vena cava or RA. Moreover, there is a concern that the lead tip may slip towards the anterior wall when pushed for securing to the septum. Delivery catheters are available in several shapes, each designed to facilitate lead placement in the ventricular septum, His-bundle region, and atrial septum. Delivery catheters are less likely to be deformed in the heart. They have a stronger backup force for lead placement than stylet systems due to the proximity of the catheter tip to the targeted area, making it easier to place the lead tip in the targeted area.
Ishibashi et al.15 reported that a paced QRS duration of ≤132 ms was associated with a higher LV ejection fraction and higher frequency of LV synchrony, as assessed by ECG-gated myocardial perfusion single-photon emission CT imaging. A paced QRS duration of ≤132 ms was achieved in 23 of 36 (64%) patients in the delivery catheter group and 8 of 34 (24%) in the stylet group in the present study. Although the present study did not assess LV synchrony, the routine use of a delivery catheter may facilitate the maintenance of LV synchrony and LV systolic function. Notably, paced QRS duration was still narrower in the delivery catheter group than in the stylet group when subgroup analysis was performed in 45 patients whose lead tip of the RV lead was deployed on the RV septum, as judged by cardiac CTs. These findings may indicate that RV septal pacing using the delivery catheter system may improve the quality of the septal pacing compared with the stylet system. One possible mechanism is that the C315-His catheter can direct the tip of the RV lead to a basal RV septum near the conduction system because the shape is designed to achieve His-bundle pacing. Our findings showed that unintended physiological pacing occurred in four patients. Unintended physiological pacing could contribute to narrower QRS width than expected. Yamagata et al.16 reported that paced QRS duration was 130 ± 18 ms in the RV septum group using the delivery catheter, which was similar to our findings.
Conversely, RV lead placement to the RV septum was not 100% successful in the delivery catheter group. The tip of the RV lead was placed on the anterior edge of the RV septum in approximately one-fifth of the delivery catheter group patients. Performing contrast injection through delivery catheter either before or after lead deployment, referring the paced QRS morphology, and applying the strict fluoroscopic RAO criteria propounded by Burri et al.9 could improve the success rate of accurate RV septal pacing, although it was not performed in the present study. Of note, the RV lead placement on the RV outflow tract should be avoided because true septum on RVOT is small and smooth. Moreover, although C315-His was recommended as a first choice in the present study, flexible selection of the delivery catheter based on the anatomy of the heart in each patient could result in an accurate RV septal pacing.
The Mt FUJI trial demonstrated that a delivery catheter system could contribute not only the accuracy of RV lead deployment on the RV septum but also the narrowing of paced QRS complex in patients who underwent pacemaker implantation compared with the stylet system. Therefore, a delivery catheter system can be considered the primary method for achieving RV septal pacing, especially for patients dependent on RV pacing.
Study limitations
This study had several limitations. First, all study participants were Asian who are relatively short and light. Therefore, our results should be confirmed by further studies including patients of different racial and ethnic backgrounds. Second, due to its small sample size, it is difficult to assess prognosis and safety outcomes. Further studies are needed to assess the prognostic impact of RV septal pacing using a delivery catheter system in reducing lead perforation and RV pacing-induced cardiomyopathy compared with RV apical pacing. Third, the widespread use of LBBAP may take over RV septal pacing in the future17–19 and attenuate the clinical impact of the present study. However, this procedure needs the operator’s experience and skills. In addition, long-term follow-up data about LBBAP is still lacking, although MELOS study showed that complications specific to the ventricular transseptal route of the pacing lead occurred in 8.3% of the patients during the mean follow-up of 6.4 months.20 A possible concern is very late complications related to LBBAP, such as lead failure due to lead perforation or lead fracture. Therefore, RV septal pacing still remains one of the useful pacemaker implantation procedures.
Conclusion
The delivery catheter system can achieve a higher success rate of RV lead placement to the RV septum and narrower paced QRS width than the stylet system.
Contributor Information
Yoshihisa Naruse, Division of Cardiology, Internal Medicine III, Hamamatsu University School of Medicine, 1-20-1 Handayama, Higashi-ward, Hamamatsu 431-3192, Japan.
Makoto Sano, Division of Cardiology, Internal Medicine III, Hamamatsu University School of Medicine, 1-20-1 Handayama, Higashi-ward, Hamamatsu 431-3192, Japan.
Nobutake Kurebayashi, Department of Cardiology, Chutoen General Medical Center, 1-1 Shobugaike, Kakegawa, 436-0040, Japan.
Shuji Morikawa, Department of Cardiology, Chutoen General Medical Center, 1-1 Shobugaike, Kakegawa, 436-0040, Japan.
Naoki Tsurumi, Department of Cardiology, Chutoen General Medical Center, 1-1 Shobugaike, Kakegawa, 436-0040, Japan.
Tomoyuki Shiozawa, Department of Cardiology, Juntendo University Shizuoka Hospital, 1129 Nagaoka, Izunokuni, 410-2211, Japan.
Shintaro Takano, Department of Cardiology, Juntendo University Shizuoka Hospital, 1129 Nagaoka, Izunokuni, 410-2211, Japan.
Michio Ogano, Department of Cardiovascular Medicine, Shizuoka Medical Center, 762-1 Nagasawa, Sunto-gun, 411-8611, Japan.
Kei Kimura, Department of Cardiovascular Medicine, Shizuoka Medical Center, 762-1 Nagasawa, Sunto-gun, 411-8611, Japan.
Keisuke Miyajima, Department of Cardiology, Seirei Mikatahara General Hospital, 3453 Mikatahara-cho, Kita-ward, Hamamatsu, 433-8558, Japan.
Ryo Sugiura, Department of Cardiology, Seirei Hamamatsu General Hospital, 2-12-1 Sumiyoshi, Naka-ward, Hamamatsu, 430-0906, Japan.
Ryuta Henmi, Department of Cardiology, Seirei Hamamatsu General Hospital, 2-12-1 Sumiyoshi, Naka-ward, Hamamatsu, 430-0906, Japan.
Masahiro Muto, Department of Cardiology, Hamamatsu Medical Center, 328 Tomitsuka-cho, Naka-ward, Hamamatsu, 432-8580, Japan.
Natsuko Hosoya, Department of Cardiology, Hamamatsu Medical Center, 328 Tomitsuka-cho, Naka-ward, Hamamatsu, 432-8580, Japan.
Hideyuki Hasebe, Division of Arrhythmology, Shizuoka Saiseikai General Hospital, 1-1-1 Kojika, Suruga-ward, Shizuoka, 422-8021, Japan.
Akira Mizukami, Department of Cardiology, Kameda Medical Center, 929 Higashi-cho, Kamogawa, 296-8602, Japan.
Keisuke Iguchi, Division of Cardiology, Internal Medicine III, Hamamatsu University School of Medicine, 1-20-1 Handayama, Higashi-ward, Hamamatsu 431-3192, Japan.
Akiko Atsumi, Department of Cardiology, Shintoshi Hospital, 703 Nakaizumi, Iwata, 438-0078, Japan.
Keiichi Odagiri, Center for Clinical Research, Hamamatsu University Hospital, 1-20-1 Handayama, Higashi-ward, Hamamatsu, 431-3125, Japan.
Yumi Kiyama, Center for Clinical Research, Hamamatsu University Hospital, 1-20-1 Handayama, Higashi-ward, Hamamatsu, 431-3125, Japan.
Yuichiro Maekawa, Division of Cardiology, Internal Medicine III, Hamamatsu University School of Medicine, 1-20-1 Handayama, Higashi-ward, Hamamatsu 431-3192, Japan.
the Mt FUJI trial investigators:
Kato Yoshinobu, Saito Hideki, Isomura Daichi, Ito Kazuki, Okazaki Ayako, Takashima Yasuyo, Watanabe Tomoyuki, Kawaguchi Yoshitaka, Wakabayashi Yasushi, Takayama Yohei, Sawasaki Kohei, Tanabe Jun, Moriya Soushi, Ishikawa Go, Takahashi Daigo, Nishio Ryota, Yasuda Kentaro, Sonoda Taketo, Yatsu Shoichiro, Shitara Jun, Wada Hideki, Ogita Manabu, Suwa Satoru, Joko Yumiko, Ogane Takashi, Suzuki Tomotaka, Iwawaki Tomoya, Inoue Naoya, Urushida Tuyoshi, Saotome Masao, Ohtani Hayato, Suwa Kenichiro, Mogi Satoshi, Narumi Taro, Sakakibara Tomoaki, and Kaneko Yutaro
Mt FUJI trial investigators
Yoshinobu Kato, Hideki Saito, Daichi Isomura, Kazuki Ito, Ayako Okazaki, Yasuyo Takashima, Tomoyuki Watanabe, Yoshitaka Kawaguchi, Yasushi Wakabayashi, Yohei Takayama, Kohei Sawasaki, Jun Tanabe, Soushi Moriya, Go Ishikawa, Daigo Takahashi, Ryota Nishio, Kentaro Yasuda, Taketo Sonoda, Shoichiro Yatsu, Jun Shitara, Hideki Wada, Manabu Ogita, Satoru Suwa, Yumiko Joko, Takashi Ogane, Tomotaka Suzuki, Tomoya Iwawaki, Naoya Inoue, Tuyoshi Urushida, Masao Saotome, Hayato Ohtani, Kenichiro Suwa, Satoshi Mogi, Taro Narumi, Tomoaki Sakakibara, and Yutaro Kaneko.
Funding
The Mt FUJI trial was conducted with financial support from Medtronic Japan Co., Ltd. (grant number: ERP-2019-12060) and HUSM Grant-in-Aid (grant number: N/A).
Data availability
Data from Mt FUJI study are available upon reasonable request.
References
- 1. Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KLet al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation 2003;107:2932–7. [DOI] [PubMed] [Google Scholar]
- 2. Inoue K, Okayama H, Nishimura K, Saito M, Yoshii T, Hiasa Get al. Right ventricular septal pacing preserves global left ventricular longitudinal function in comparison with apical pacing: analysis of speckle tracking echocardiography. Circ J 2011;75:1609–15. [DOI] [PubMed] [Google Scholar]
- 3. Karpawich PP, Justice CD, Chang CH, Gause CY, Kuhns LR. Septal ventricular pacing in the immature canine heart: a new perspective. Am Heart J 1991;121:827–33. [DOI] [PubMed] [Google Scholar]
- 4. Mizukami A, Matsue Y, Naruse Y, Kowase S, Kurosaki K, Suzuki Met al. Implications of right ventricular septal pacing for medium-term prognosis: propensity-matched analysis. Int J Cardiol 2016;220:214–8. [DOI] [PubMed] [Google Scholar]
- 5. Kaye GC, Linker NJ, Marwick TH, Pollock L, Graham L, Pouliot Eet al. Effect of right ventricular pacing lead site on left ventricular function in patients with high-grade atrioventricular block: results of the Protect-Pace study. Eur Heart J 2015;36:856–62. [DOI] [PubMed] [Google Scholar]
- 6. Osmancik P, Stros P, Herman D, Curila K, Petr R. The insufficiency of left anterior oblique and the usefulness of right anterior oblique projection for correct localization of a computed tomography-verified right ventricular lead into the midseptum. Circ Arrhythm Electrophysiol 2013;6:719–25. [DOI] [PubMed] [Google Scholar]
- 7. Hattori M, Naruse Y, Oginosawa Y, Matsue Y, Hanaki Y, Kowase Set al. Prognostic impact of lead tip position confirmed via computed tomography in patients with right ventricular septal pacing. Heart Rhythm 2019;16:921–7. [DOI] [PubMed] [Google Scholar]
- 8. Moore P, Coucher J, Ngai S, Stanton T, Wahi S, Gould Pet al. Imaging and right ventricular pacing lead position: a comparison of CT, MRI, and echocardiography. Pacing Clin Electrophysiol 2016;39:382–92. [DOI] [PubMed] [Google Scholar]
- 9. Burri H, Domenichini G, Sunthorn H, Ganiere V, Stettler C. Comparison of tools and techniques for implanting pacemaker leads on the ventricular mid-septum. Europace 2012;14:847–52. [DOI] [PubMed] [Google Scholar]
- 10. Squara F, Scarlatti D, Riccini P, Garret G, Moceri P, Ferrari E. Individualized left anterior oblique projection: a highly reliable patient-tailored fluoroscopy criterion for right ventricular lead positioning. Circ Arrhythm Electrophysiol 2018;11:e006107. [DOI] [PubMed] [Google Scholar]
- 11. Shimeno K, Yoshiyama T, Abe Y, Akamatsu K, Kagawa S, Matsushita Tet al. The usefulness of right ventriculography to aid anchoring a pacing lead to the right ventricular septum. Europace 2018;20:1154–60. [DOI] [PubMed] [Google Scholar]
- 12. Miyajima K, Urushida T, Naruse Y, Ito K, Kin F, Okazaki Aet al. The usefulness of a delivery catheter system for right ventricular “true” septal pacing. Heart Vessels 2021;36:1056–63. [DOI] [PubMed] [Google Scholar]
- 13. Naruse Y, Miyajima K, Sugiura R, Muto M, Ogano M, Kurebayashi Net al. Comparison of delivery catheter-based and stylet-based right ventricular lead placement at the right ventricular septum under fluoroscopic guidance judged by cardiac CT (Mt. FUJI): a study protocol for the Mt. FUJI randomised controlled trial. BMJ Open 2021;11:e046782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Waddingham PH, Elliott J, Bates A, Bilham J, Muthumala A, Honarbakhsh Set al. Iatrogenic cardiac perforation due to pacemaker and defibrillator leads: a contemporary multicentre experience. Europace 2022;24:1824–33. [DOI] [PubMed] [Google Scholar]
- 15. Ishibashi K, Yamagata K, Kiso K, Nouno Y, Ueda N, Nakajima Ket al. Retrograde penetration pacing into the conduction system as an alternative approach of his-bundle pacing: retrograde penetration pacing into the conduction system. J Cardiol 2022;79:127–33. [DOI] [PubMed] [Google Scholar]
- 16. Yamagata K, Ishibashi K, Wakamiya A, Shimamoto K, Ueda N, Kamakura Tet al. Comparison between septal pacing with the catheter delivery system and apical pacing with the stylet delivery system for ventricular lead placement: A randomized controlled trial. Circ Arrhythm Electrophysiol 2021;14:e010362. [DOI] [PubMed] [Google Scholar]
- 17. Kircanski B, Boveda S, Prinzen F, Sorgente A, Anic A, Conte Get al. Conduction system pacing in everyday clinical practice: EHRA physician survey. Europace 2023;25:682–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wu S, Sharma PS, Huang W. Novel left ventricular cardiac synchronization: left ventricular septal pacing or left bundle branch pacing? Europace 2020;22:ii10–8. [DOI] [PubMed] [Google Scholar]
- 19. Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IMet al. ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Europace 2021;2022:71–164. [Google Scholar]
- 20. Jastrzebski M, Kielbasa G, Cano O, Curila K, Heckman L, De Pooter Jet al. Left bundle branch area pacing outcomes: the multicentre European MELOS study. Eur Heart J 2022;43:4161–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data from Mt FUJI study are available upon reasonable request.