Abstract
Background:
Epilepsy accounts for a significant portion of the global disease burden. However, little is known about the disease burden of epilepsy in China and its provinces.
Methods:
We assessed the burden of epilepsy in China and its provinces, municipalities, and autonomous regions from 1990 to 2019. Burden was measured as incidence, prevalence, deaths, years lived with disability, years of life lost, and disability-adjusted life years (DALYs), by age, sex, year, and province. We used the Socio-Demographic Index (SDI) to determine the association between the provincial development level and age-standardized DALY rates of epilepsy from 1990 to 2019.
Results:
In 2019, epilepsy caused 1367.51 thousand (95% uncertainty interval [UI]: 979.92–1837.61 thousand) DALYs, and the age-standardized DALY rate was 99.77 (95% UI: 71.33–133.52)/100,000. The age-standardized incidence and prevalence rates for epilepsy in China were 24.65/100,000 and 219.69/100,000, increased by 45.00% (95% UI: 8.03–98.74%) and 35.72% (95% UI: 0.47–86.19%) compared with that in 1990, respectively. From 1990 to 2019, the proportion of DALY caused by epilepsy in the age group under 25 years steadily decreased. The proportion of DALYs caused by epilepsy in people aged 50 years and over increased from 9.45% and 10.22% in 1990 to 29.01% and 32.72% for male and female individuals in 2019, respectively. The highest age-standardized mortality rates were seen in Tibet (4.26 [95% UI: 1.43–5.66]/100,000), Qinghai (1.80 [95% UI: 1.15–2.36]/100,000), and Yunnan (1.30 [95% UI: 0.88–1.62]/100,000), and the lowest mortality rates were in Guangdong (0.48 [95% UI: 0.39–0.64]/100,000), Zhejiang (0.56 [95% UI: 0.44–0.70]/100,000), and Shanghai (0.57 [95% UI: 0.41–0.73]/100,000). The age-standardized DALY rates across the country and in provinces, municipalities, and autonomous regions generally decreased as their SDI increased.
Conclusions:
The disease burden of epilepsy is still heavy in China, especially in the western provinces. The incidence and prevalence of epilepsy increased between 1990 and 2019, and the burden of epilepsy in the elderly increases gradually. This study provides evidence on epilepsy prevention and care of different regions in China.
Keywords: Aged, Epilepsy, Global Burden of disease, Quality-adjusted life years, Disability-adjusted life years, Incidence, Prevalence, China
Introduction
Epilepsy is one of the most common neurological disorders in the world, and it affects about 70 million people.[1] It is characterized by abnormal firing of neurons in the brain, leading to recurrent seizures and neurobiological, cognitive, and psychosocial consequences.[2,3] Epilepsy not only has a serious impact on the physical and mental health of patients but also brings heavy burden to families, communities, and society.[4,5] It was estimated that around 90% of the global burden of epilepsy is carried by developing countries.[6] Although China's standardized incidence rate and prevalence are lower than the global average level,[7] China has more than 12% of epilepsy patients in the world due to its large population base.[7,8] The Global Burden of Disease (GBD) Study estimated that disability-adjusted life years (DALYs) caused by epilepsy in China in 2019 accounted for 10% of the global DALYs and 94% of that in east Asia.[9]
A detailed understanding of the epidemiological characteristics of epilepsy will help to comprehensively understand the current situation and development trend of epilepsy in China and its different provinces and provide data support for the government to deal with the public health problems caused by epilepsy and reduce the differences in epilepsy burden in different regions. DALYs can better reflect the loss of life caused by diseases, and it is a comprehensive measure of the burden of the disease.[10] However, to our knowledge, there are few studies on the burden of epilepsy in China at present, and most of them focused on the prevalence rate.[8,11] Although a study has used GBD 2016 data to analyze the trend of global epilepsy burden from 1990 to 2016 (including China), it only mentioned the epilepsy burden at the national level in China, and it is still unclear to what extent the epilepsy burden varied across different provinces in China.[7] There is also a lack of research on the current situation and temporal trend of epilepsy incidence rate and DALYs in China and its provinces among people at different ages.
The purpose of this study is to comprehensively analyze the time trend of the disease burden of epilepsy by sex and age groups in China and its provinces, municipalities, and autonomous regions from 1990 to 2019 so as to provide epidemiological evidence for the development of national and local policies to prevent and treat epilepsy.
Methods
Data source
The data of this study are from the epilepsy data of China and its provinces, municipalities, and autonomous regions from 1990 to 2019 in the GBD 2019 database.[12] The GBD 2019 adopts a unified and comparable method to comprehensively estimate the disease burden of various diseases, injuries, and risk factors by multiple indicators in 204 countries and regions around the world. Provincial-level mortality data were extracted mainly from the Disease Surveillance Point system, Maternal and Child Surveillance System, China Cancer Registry, and Chinese Center for Disease Control and Prevention cause-of-death reporting system.[13,14] Data on non-fatal outcomes of epilepsy were derived primarily from national surveys, hospital inpatient data, and published studies.[15] The detailed methods have been reported in the previous literature.[9] Socio-Demographic Index (SDI) data were obtained from the GBD 2019.
Definitions
According to the criteria of the International League Against Epilepsy (ILAE) Guidelines and International Bureau for Epilepsy (IBE), epilepsy is defined as a disorder of the brain characterized by an enduring predisposition to generate epileptic seizures.[7,16] The 9th and 10th International Classification of Diseases (ICD-9 and ICD-10) were used to define epilepsy: 345–345.91 (ICD-9), G40-G41.9, and Z82.0 (ICD-10).
Measurements
Six standard epidemiological measures including death, prevalence, incidence, DALYs, years of life lost (YLLs), and years lived with disability (YLDs) were used to estimate the trends of disease burden of epilepsy in China from 1990 to 2019. Epilepsy mortality was generated by Cause of Death Ensemble modeling methods, and the GBD 2019 adopts DisMod-MR2.1 to estimate the disease burden of non-fatal diseases.[10] The detailed approach to estimating the disease burden of epilepsy in the GBD has been described previously.[9,10] Epilepsy in China is analyzed by the following age groups: under 5 years, 5 to 9 years, 10 to 24 years, 25 to 49 years, 50 to 74 years, 75 to 84 years, and ≥85 years.
Statistical analysis
We analyzed the number of incidences, prevalence, deaths, YLDs, YLLs, and DALYs due to epilepsy in 31 mainland provinces, municipalities, and autonomous regions in China, during 1990 to 2019. YLDs were estimated by multiplying these health states by corresponding disability weights, while YLLs were calculated by multiplying the estimated number of deaths by age with a standard life expectancy at corresponding age. DALYs were computed by summing YLDs and YLLs. In order to reduce the impact of population composition in different years and regions, this study also showed the age-standardized rates of epilepsy and the changes from 1990 to 2019 by sex and province. Age-standardized rates were analyzed using a global age structure as reference.[9] The 95% uncertainty interval (UI) was a standard indicator used in the GBD calculated by taking 1000 draws from the posterior distribution in the modeling process to address the possible heterogeneity from both sampling error and non-sampling variance.[17] We reported point estimates and corresponding 95% UI for all measures. The percentage change of rates is calculated by the difference between the rates in 2019 and 1990 divided by the rate in 1990, representing the direction and magnitude of change in the past 30 years. If the 95% UI of the percentage change of rates does not include 0, then the change from 1990 to 2019 is considered statistically significant. The SDI ranges from 0 (worst) to 100 (best) and incorporates the total fertility rate in women younger than 25 years, mean education for individuals aged 15 years and older, and lag-distributed income per person. We used the SDI to determine the association between the development level and age-standardized DALY rates of epilepsy from 1990 to 2019 by locally weighed regression, which is a robust non-parametric regression and can better solve the smoothing problem for volatile data. A two-sided P value was regarded statistically significant if it was <0.05. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for tabulation of comparison between 1990 and 2019 at national and provincial levels. R version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria) was used to examine the proportion of DALYs due to epilepsy by age group and assess the association between SDI and the age-standardized DALY rate by locally weighed regression.
Results
Table 1 shows the number of incidences, prevalences, deaths, YLDs, YLLs, DALYs, and corresponding age-standardized rates and change for epilepsy by sex in China during 1990 to 2019. There were 305.74 thousand epilepsy incident cases (95% UI: 208.84–409.61 thousand), 3078.30 thousand epilepsy prevalent cases (95% UI: 2204.84–3997.32 thousand), and 11.73 thousand deaths (95% UI: 9.98–14.01 thousand) in 2019 in China, contributing to 1367.51 thousand DALYs (95% UI: 979.92–1837.61 thousand). In 2019, the age-standardized incidence and prevalence rates for epilepsy were 24.65/100,000 and 219.69/100,000, increased by 45.00% (95% UI: 8.03–98.74%) and 35.72% (95% UI: 0.47–86.19%) compared with those in 1990, respectively. The percentage change of age-standardized death and DALY rates for epilepsy were −53.34% (95% UI: −62.71 to −38.61%) and −34.98% (95% UI: −50.42 to −13.70%) from 1990 to 2019, respectively.
Table 1.
Disease burden of epilepsy in China, 1990–2019.
| Male | Female | Both | |||||||
| Variables | 1990 | 2019 | Percentage change (%) | 1990 | 2019 | Percentage change (%) | 1990 | 2019 | Percentage change (%) |
| Number (thousands) | |||||||||
| Incident cases | 110.43 (71.53–156.47) | 168.45 (116.08–226.32) | 52.54 (13.68–112.18) | 90.58 (58.57–128.44) | 137.29 (92.95–182.96) | 51.57 (12.25–111.02) | 201.01 (129.40–285.35) | 305.74 (208.84–409.61) | 52.10 (13.09–111.28) |
| Prevalent cases | 1007.96 (700.58–1366.27) | 1621.67 (1163.13–2104.25) | 60.89 (18.08–124.31) | 895.26 (626.78–1216.30) | 1456.64 (1045.64–1903.47) | 62.71 (19.52–127.50) | 1903.21 (1326.04–2587.26) | 3078.30 (2204.84–3997.32) | 61.74 (18.99–124.39) |
| Death | 11.46 (9.39–13.19) | 7.52 (6.04–9.35) | −34.37 (−49.29 to −12.08) | 7.73 (5.97–10.10) | 4.21 (3.29–5.44) | −45.49 (−61.64 to −19.11) | 19.18 (16.10–21.99) | 11.73 (9.98–14.01) | −38.85 (−51.28 to −20.17) |
| YLD | 370.77 (218.90–569.08) | 443.12 (253.38–690.04) | 19.51 (−22.11 to 85.65) | 324.21 (185.62–496.64) | 390.62 (221.36–605.39) | 20.48 (−21.04 to 86.97) | 694.97 (404.06–1061.58) | 833.74 (473.71–1278.49) | 19.97 (−21.48 to 84.98) |
| YLL | 701.15 (562.95–804.80) | 345.42 (280.10–426.50) | −50.73 (−61.67 to −34.20) | 468.50 (353.03–626.89) | 188.35 (146.44–242.31) | −59.80 (−72.65 to −39.71) | 1169.65 (962.38–1336.84) | 533.77 (453.36–633.26) | −54.36 (−63.9 to −38.25) |
| DALY | 1071.92 (857.83–1302.22) | 788.54 (579.63–1035.81) | −26.44 (−43.41 to −2.12) | 792.71 (604.50–1010.35) | 578.97 (400.84–803.37) | −26.96 (−47.74 to 2.53) | 1864.63 (1492.97–2289.80) | 1367.51 (979.92–1837.61) | −26.66 (−43.86 to −2.36) |
| Age-standardized rate (per 100,000) | |||||||||
| Incidence | 18.07 (11.85–25.35) | 26.38 (17.99–35.84) | 45.97 (8.88–100.15) | 15.86 (10.31–22.24) | 22.89 (15.43–31.61) | 44.29 (7.22–97.66) | 17.00 (11.08–23.82) | 24.65 (16.74–33.56) | 45.00 (8.03–98.74) |
| Prevalence | 166.79 (116.01–223.66) | 228.34 (162.59–298.75) | 36.91 (1.59–87.76) | 156.79 (109.67–210.26) | 211.20 (148.99–281.04) | 34.70 (0.43–86.28) | 161.87 (112.81–216.65) | 219.69 (155.39–288.28) | 35.72 (0.47–86.19) |
| Death | 1.92 (1.58–2.20) | 0.98 (0.80–1.20) | −49.09 (−60.11 to −32.43) | 1.37 (1.07–1.80) | 0.56 (0.44–0.72) | −58.87 (−71.04 to −38.49) | 1.64 (1.4–1.89) | 0.77 (0.66–0.91) | −53.34 (−62.71 to −38.61) |
| YLD | 60.73 (35.69–92.07) | 63.09 (35.39–97.18) | 3.90 (−30.97 to 59.10) | 56.33 (32.56–86.13) | 57.85 (32.63–90.85) | 2.69 (−31.51 to 55.56) | 58.56 (34.38–88.75) | 60.46 (33.99–93.29) | 3.24 (−31.28 to 56.71) |
| YLL | 109.48 (87.83–125.61) | 48.80 (40.04–59.69) | −55.42 (−65.14 to −39.10) | 79.31 (59.93–106.38) | 29.34 (22.64–37.20) | −63.01 (−75.13 to −43.84) | 94.88 (78.05–108.60) | 39.31 (33.39–46.87) | −58.56 (−67.09 to −42.52) |
| DALY | 170.2 (135.42–207.20) | 111.90 (82.53–148.14) | −34.26 (−49.36 to −12.70) | 135.64 (104.13–172.31) | 87.18 (60.39–121.55) | −35.73 (−53.92 to −9.04) | 153.44 (122.89–187.17) | 99.77 (71.33–133.52) | −34.98 (−50.42 to −13.70) |
Data are shown as n (95% UI). DALY: Disability-adjusted life years; UI: Uncertainty interval; YLD: Years lived with disability; YLL: Years of life lost.
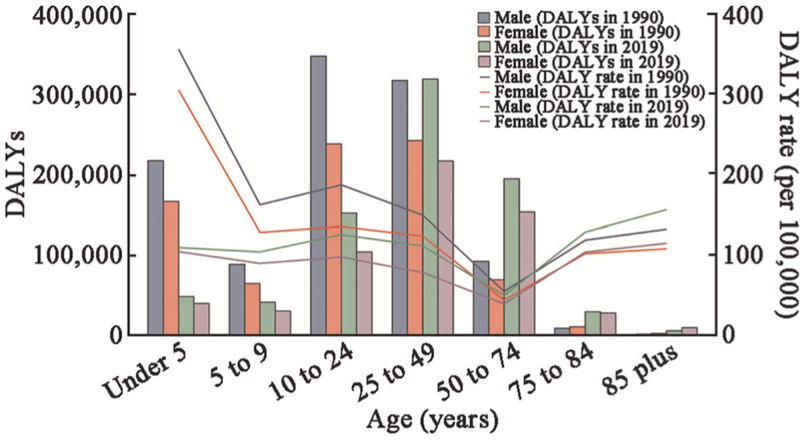
As shown in Figure 1, for both men and women, the DALY rate of epilepsy in 2019 decreased for people aged <75 years and increased for those aged ≥75 years compared with that in 1990. The DALY rate of epilepsy in children younger than 5 years was the highest in 1990 (male: 356.34 [95% UI: 224.17–435.83]/100,000; female: 305.61 [95% UI: 192.31–437.48]/100,000), while it was the highest in the elderly aged 85 years and above in 2019 (male: 156.19 [95% UI: 100.88–231.73]/100,000; female: 114.61 [95% UI: 69.87–176.98]/100,000). Whether in 1990 or 2019, the DALY rate of epilepsy in the 50 to 74 years age group was the lowest, the rate of epilepsy DALY in the 10 to 24 years age group was the second highest in all age groups, and the number of DALYs caused by epilepsy was the lowest in the 85 years and above age group.
Figure 1.
Comparison of the distribution of DALYs caused by epilepsy in different age groups and the curve of the DALY rate due to epilepsy corresponding to the age groups in 1990 and in 2019. DALY: Disability-adjusted life years.
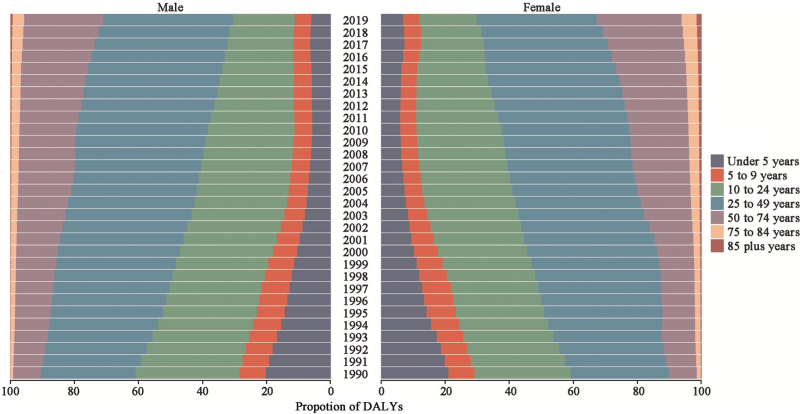
Figure 2 presents the proportion of DALYs in different age groups in China, by sex, 1990 to 2019. From 1990 to 2019, the proportion of DALY caused by epilepsy in the age group under 25 years decreased gradually. On the contrary, there was an annual increase in the proportion of DALY caused by epilepsy in the age group of 25 years and above, especially in people aged 50 years and above. The proportion of DALYs caused by epilepsy in people aged 50 years and over increased from 9.45% and 10.22% in 1990 to 29.01% and 32.72% for male and female individuals in 2019, respectively. In 2019, the proportion of DALYs caused by epilepsy in the 25 to 49 years of age was the highest (male 40.47%, female 37.43%) in all age groups.
Figure 2.
Proportion of DALYs due to epilepsy by age group in China, by sex, 1990–2019. DALY: Disability-adjusted life years.
The geographical heterogeneity in age-standardized prevalence, mortality, and DALY rates of epilepsy and percentage changes from 1990 were found at the provincial levels in 2019 [Table 2]. The highest age-standardized prevalence rates were observed in Tibet (438.85 [95% UI: 115.95–740.52]/100,000) and Ningxia (302.19 [95% UI: 93.41–497.08]/100,000) in 2019. The highest age-standardized mortality rates were seen in Tibet (4.26 [95% UI: 1.43–5.66]/100,000), Qinghai (1.80 [95% UI: 1.15–2.36]/100,000), and Yunnan (1.30 [95% UI: 0.88–1.62]/100,000), and the lowest mortality rates were observed in Guangdong (0.48 [95% UI: 0.39–0.64]/100,000), Zhejiang (0.56 [95% UI: 0.44–0.70]/100,000), and Shanghai (0.57 [95% UI: 0.41–0.73]/100,000). The highest age-standardized DALY rate was observed in Tibet (400.55 [95% UI: 193.62–601.28]/100,000), which showed a 4.92-fold difference compared with the lowest age-standardized DALY rate in Zhejiang (81.47 [95% UI: 39.97–142.55]/100,000). Declines in the age-standardized mortality and DALY rates for epilepsy were observed in all provinces during the study period, and the largest decrease was found in Jiangxi (mortality: −70.49%, DALY: −53.31%). However, over the past 30 years, the age-standardized prevalence of epilepsy has increased in all provinces of China, with the largest increase in Qinghai (80.24%) and Guangxi (53.37%).
Table 2.
Age-standardized prevalence, mortality, and DALY rate of epilepsy in 2019 and percentage changes from 1990 in different Chinese mainland provincial administrative regions.
| Age-standardized prevalence rate (/100,000) | Age-standardized mortality rate (/100,000) | Age-standardized DALY rate (/100,000) | ||||
| Provincal administrative regions | 2019 | Percentage change (%), 1990–2019 | 2019 | Percentage change (%), 1990–2019 | 2019 | Percentage change (%), 1990–2019 |
| Anhui | 194.27 (53.56, 316.04) | 48.92 (−63.06, 610.38) | 0.72 (0.58, 0.89) | −57.19 (−68.40, −39.77) | 90.47 (47.14, 154.97) | −36.79 (−67.78, 13.08) |
| Beijing | 234.59 (73.79, 364.08) | 16.33 (−66.18, 332.63) | 0.61 (0.43, 0.77) | −58.23 (−69.76, −39.31) | 88.76 (43.45, 153.00) | −36.15 (−71.31, 24.92) |
| Chongqing | 201.9 (57.12, 336.62) | 43.37 (−62.57, 554.97) | 0.69 (0.53, 0.95) | −58.42 (−69.76, −39.40) | 89.16 (47.42, 154.35) | −39.82 (−70.58, 12.56) |
| Fujian | 214.72 (64.00, 344.30) | 39.11 (−63.53, 609.02) | 0.73 (0.57, 0.90) | −57.90 (−68.37, −40.73) | 95.33 (48.95, 163.33) | −36.48 (−68.53, 20.21) |
| Gansu | 197.33 (54.54, 327.09) | 39.66 (−65.29, 575.17) | 0.95 (0.76, 1.16) | −52.24 (−63.97, −34.52) | 107.70 (61.38, 178.17) | −38.13 (−66.45, 8.52) |
| Guangdong | 214.16 (73.53, 343.18) | 45.25 (−54.83, 498.15) | 0.48 (0.39, 0.64) | −56.03 (−67.45, −39.08) | 81.69 (38.31, 146.82) | −24.80 (−65.67, 58.22) |
| Guangxi | 199.14 (59.79, 328.48) | 53.37 (−59.45, 514.65) | 0.73 (0.59, 0.94) | −42.69 (−56.50, −22.64) | 93.36 (50.18, 156.61) | −22.32 (−59.26, 44.07) |
| Guizhou | 193.20 (59.58, 322.11) | 31.20 (−66.22, 587.18) | 1.16 (0.87, 1.50) | −56.02 (−68.50, −33.09) | 119.17 (69.84, 190.21) | −46.09 (−71.19, −1.93) |
| Hainan | 200.33 (59.73, 323.60) | 42.53 (−64.65, 485.66) | 0.69 (0.55, 0.87) | −46.37 (−60.81, −22.57) | 93.16 (48.15, 162.61) | −26.10 (−66.17, 47.96) |
| Hebei | 274.49 (73.29, 456.71) | 35.13 (−67.53, 466.54) | 0.68 (0.52, 1.09) | −35.60 (−51.36, −11.92) | 109.99 (50.58, 195.92) | −16.41 (−62.33, 82.04) |
| Heilongjiang | 260.24 (77.33, 419.90) | 16.29 (−71.72, 399.30) | 0.73 (0.57, 1.05) | −50.78 (−63.62, −28.95) | 110.25 (56.70, 191.03) | −31.62 (−68.86, 40.02) |
| Henan | 201.46 (53.91, 323.07) | 34.81 (−67.45, 543.94) | 0.68 (0.54, 0.92) | −51.54 (−63.47, −33.99) | 89.04 (46.32, 151.71) | −36.84 (−69.51, 22.24) |
| Hubei | 209.98 (50.71, 338.98) | 46.54 (−64.74, 569.48) | 0.79 (0.64, 1.00) | −50.51 (−63.19, −30.35) | 97.71 (52.90, 161.92) | −32.32 (−66.98, 22.74) |
| Hunan | 206.18 (62.77, 330.76) | 29.54 (−64.15, 521.71) | 0.68 (0.54, 0.93) | −55.12 (−66.35, −37.87) | 91.28 (47.91, 154.24) | −37.64 (−68.85, 18.10) |
| Inner Mongolia | 215.11 (65.73, 342.03) | 48.68 (−55.83, 519.13) | 0.74 (0.58, 1.00) | −55.11 (−67.31, −35.94) | 97.71 (53.60, 163.22) | −35.19 (−66.59, 23.42) |
| Jiangsu | 259.40 (94.17, 408.04) | 23.37 (−62.12, 457.30) | 0.69 (0.52, 0.87) | −50.67 (−62.63, −34.38) | 101.40 (49.22, 178.06) | −30.94 (−68.81, 33.89) |
| Jiangxi | 191.30 (55.82, 310.97) | 34.24 (−67.13, 529.73) | 0.67 (0.55, 0.85) | −70.49 (−77.28, −53.97) | 89.11 (47.08, 148.70) | −53.31 (−76.73, −13.79) |
| Jilin | 224.53 (62.71, 358.50) | 21.01 (−66.73, 384.14) | 0.70 (0.55, 0.95) | −56.72 (−67.66, −40.86) | 96.75 (48.67, 162.32) | −36.12 (−69.85, 30.07) |
| Liaoning | 233.07 (70.04, 359.66) | 38.24 (−61.82, 388.13) | 0.85 (0.68, 1.05) | −39.21 (−53.91, −12.83) | 105.08 (56.40, 177.53) | −21.15 (−59.58, 45.77) |
| Ningxia | 302.19 (93.41, 497.08) | 27.25 (−66.79, 443.78) | 1.02 (0.77, 1.29) | −55.49 (−68.21, −33.64) | 136.86 (70.51, 229.31) | −40.09 (−71.24, 17.99) |
| Qinghai | 222.46 (58.44, 366.26) | 80.24 (−53.49, 780.55) | 1.80 (1.15, 2.36) | −47.34 (−61.08, −24.91) | 166.75 (102.12, 256.18) | −35.99 (−61.16, 6.96) |
| Shaanxi | 195.58 (57.73, 319.24) | 40.76 (−64.76, 519.88) | 1.01 (0.73, 1.29) | −61.23 (−71.97, −43.51) | 106.66 (61.73, 165.12) | −48.70 (−71.16, −8.66) |
| Shandong | 215.82 (59.11, 343.87) | 42.33 (−63.98, 517.14) | 0.71 (0.58, 0.89) | −48.87 (−61.09, −31.88) | 93.64 (48.69, 158.71) | −27.73 (−65.15, 36.03) |
| Shanghai | 214.29 (66.52, 342.72) | 6.06 (−67.95, 297.47) | 0.57 (0.41, 0.73) | −53.40 (−64.68, −36.60) | 83.78 (40.96, 151.32) | −33.25 (−69.23, 41.64) |
| Shanxi | 215.31 (69.07, 347.12) | 29.18 (−63.66, 445.93) | 0.83 (0.65, 1.05) | −47.76 (−62.71, −27.19) | 101.18 (53.90, 168.75) | −30.98 (−65.14, 28.84) |
| Sichuan | 238.82 (72.39, 392.16) | 41.36 (−59.49, 547.08) | 0.98 (0.76, 1.20) | −49.30 (−62.55, −31.24) | 116.87 (67.61, 191.79) | −34.22 (−64.32, 22.53) |
| Tianjin | 237.54 (72.79, 373.52) | 40.83 (−57.80, 498.80) | 0.69 (0.55, 0.87) | −40.22 (−56.27, −19.10) | 96.85 (49.36, 170.32) | −14.98 (−59.16, 63.61) |
| Tibet | 438.85 (115.95, 740.52) | 34.08 (−66.70, 626.56) | 4.26 (1.43, 5.66) | −54.00 (−65.07, −33.71) | 400.55 (193.62, 601.28) | −42.55 (−64.68, −6.69) |
| Xinjiang | 227.68 (67.80, 366.48) | 38.98 (−61.39, 564.26) | 1.27 (0.96, 1.77) | −50.57 (−63.88, −23.89) | 139.23 (78.85, 213.50) | −37.55 (−64.27, 6.24) |
| Yunnan | 210.06 (60.21, 355.06) | 36.98 (−63.88, 530.08) | 1.30 (0.88, 1.62) | −52.67 (−65.32, −32.09) | 129.71 (78.99, 204.27) | −43.13 (−67.21, 1.89) |
| Zhejiang | 209.27 (54.63, 337.12) | 46.48 (−61.39, 503.04) | 0.56 (0.44, 0.70) | −54.20 (−65.06, −37.29) | 81.47 (39.97, 142.55) | −28.71 (−66.75, 45.06) |
Data are shown as n (95% uncertainty interval). DALY: Disability-adjusted life years.
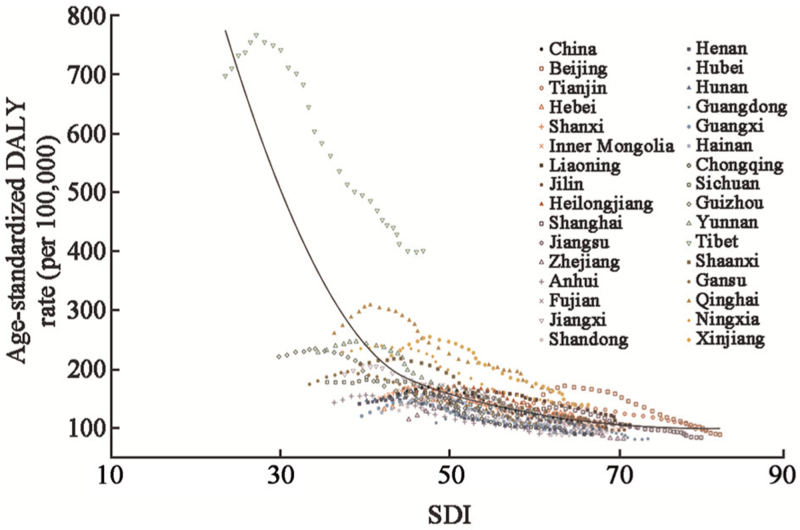
The relationship between SDI and the age-standardized DALY rates of epilepsy is shown in Figure 3. Age-standardized DALY rates of epilepsy by provinces over the period 1990 to 2019 follow a downward trajectory aligned with the predicted direction of decreasing burden of epilepsy with socioeconomic development. The age-standardized DALY rates across the country and 31 Chinese mainland provinces, municipalities, and autonomous regions generally decreased with their increased SDI. In most provinces, a steady decrease was observed over time, with values close to the expected line.
Figure 3.
Age-standardized DALY rates per 100,000 population for epilepsy in China and its provinces by SDI, 1990–2019. Points from left to right represent the values from 1990 to 2019. The black line represents the predicted values based on a regression of all province values for all years. DALY: Disability-adjusted life years; SDI: Socio-Demographic Index.
Discussion
We estimated the burden of epilepsy in the Chinese population from 1990 to 2019 using data from the GBD 2019 and indicated that the age-standardized mortality and DALY rates of epilepsy have decreased almost universally, while the age-standardized incidence and prevalence of epilepsy have risen significantly during the study period. Whether in 1990 or 2019, the DALY rate of epilepsy was the lowest in the 50 to 74 age group. From 1990 to 2019, the proportion of DALY caused by epilepsy in the age group under 25 decreased year by year. The burden of epilepsy and their percentage changes exhibited significant geographical heterogeneity.
In this study, we found a downward trend for the age-standardized mortality and DALY rates of epilepsy during the past three decades, consistent with that reported in the previous literature.[7,18] This reduction was associated with substantial economic development and improvement of health services in China in the past decades.[19] Although the age-standardized incidence rate of epilepsy in China (24.65/100,000) was lower than the global average (38.82/100,000) and that in some developed countries, such as the United States (40.44/100,000) and Japan (41.20/100,000).[19] The age-standardized incidence and prevalence rates of epilepsy showed an upward trend during the study period in China. In 2002, the IBE, the ILAE and the World Health Organization (WHO) jointly launched the Global Campaign Against Epilepsy to improve the global understanding, treatment, service, and prevention of epilepsy.[20] China has also made epilepsy a public health priority, strongly encouraging investment to reduce its burden and advocating for action to address gaps in epilepsy knowledge, care, and research.[19,21,22] The increase in the incidence rate and prevalence of epilepsy may be related to the improvement of people's awareness of epilepsy and the increase in active medical treatment.
It is well known that epilepsy affects people of all ages but more often affects young people. Although the proportion of DALYs caused by epilepsy in people over 50 years increased year by year from 1990 to 2019 in our study, the proportion of DALYs caused by epilepsy in people younger than 50 years was still dominant both in male and female individuals. Consistent with our results, previous studies have shown that the incidence of epilepsy is the highest in young children and elderly.[7,23] Epilepsy has a variety of causes including genetic, metabolic, infectious, structural, and immune factors, as well as unknown factors.[24] Major preventable causes for epilepsy include pre- or perinatal brain insults, central nervous system infections, traumatic brain injury, and stroke, which together account for an estimated 25% of epilepsy cases.[6,25,26] These causes have a high prevalence in young children and the elderly,[6,25,26] which accounts for a higher epilepsy incidence rate in these two populations. Primary prevention for these causes has a major impact on the development of epilepsy and requires improvements in maternal health care and obstetric services, infectious disease control, injury prevention, and cardiovascular health.[26] We found that the DALY rate caused by epilepsy in children younger than 5 years in 2019 was lower than that in 1990, while the DALY rate caused by epilepsy in the elderly older than 75 years was higher than that in 1990. The former may be related to the more advanced medical and health conditions and significantly improved maternal and child health care system in China.[27,28] The latter may be related to the accelerated progress of aging and the increase in life expectancy in China.[29,30]
In addition, we also found that there were significant geographical differences in the burden of epilepsy in China. The burden of epilepsy is heavier in the areas with relatively backward economic development and poor health conditions in the west, such as Tibet, Qinghai, and Xinjiang, and the DALY caused by epilepsy is lower in the faster growing provinces in the east, such as Zhejiang and Guangdong. In the past decades, the China Association Against Epilepsy (CAAE) has been a necessary force to stimulate interest in epilepsy care and research by the medical and scientific community in China.[31] The CAAE has established grading standards for a three-tier system of epilepsy centers and completed an accreditation procedure for 201 epilepsy centers.[32–34] This nationwide network promotes coordination, collaboration, and information sharing among epilepsy centers.[35] The substantial increase in the number of epileptic centers in recent decades has also played an important role in reducing the death rate of epilepsy.[33]
More and more initiatives such as case studies, ward rounds, lectures, training courses, “Going West” program, and an annual epilepsy summer school have been brought to many remote areas in the west of China.[19,22,36] It can also be seen from our results that the age-standardized DALY rate of epilepsy in economically underdeveloped western provinces decreased significantly during the study period. Because epilepsy burden varied substantially in different provinces, improved health care and intervention are particularly needed in those provinces with high epilepsy burden. Our study found that Tibet is the province with the highest standardized prevalence rate and standardized DALY rate. About 41% of people with epilepsy in China are estimated not to be receiving treatment, or to receive a treatment either inadequate or inappropriate.[22] The proportion of epileptic patients who did not receive standardized treatment, also known as the gap of epilepsy treatment, was determined by diagnosis and treatment defects, economic conditions, cultural beliefs, and distance from health facilities.[35,37] The largest epilepsy treatment gap in China is in Tibet, which may be related to Tibet's unique geographical environment and unique culture.[38] In addition, in economically underdeveloped areas, people's misunderstanding and lack of understanding of the nature of epilepsy lead to a serious stigma of epilepsy. Misunderstandings and negative attitudes can make epileptics feel ashamed, embarrassed, and humiliated. Feeling socially excluded will aggravate the physical, mental, and social burden of epilepsy. Shame can delay proper medical treatment and access to medical care, medical funds, and treatment.[26] Strengthening the treatment compliance of epileptic patients and publicity and education of epilepsy in poor areas with limited resources, especially in Tibet, will help reduce the frequency of seizures, improve the quality of life, and reduce the burden of disease.
However, several limitations exist in our study. First, although the GBD 2019 used a variety of modeling methods to estimate epilepsy burden in China and its provinces, it is still likely to have certain fluctuations in the estimation of burden for some provinces such as Tibet, due to low quality of local data source. Second, the data used in this study cannot assess the urban–rural differences in epilepsy burden. However, we explored the relationship between the burden of epilepsy and SDI, which is a comparable composite variable developed in the GBD study, to reflect overall socioeconomic development in each province. Third, the 95% UI used to define the precision of some indicators is wide, reflecting the overall uncertainty of those estimates, which will affect the estimated differences between provinces to a certain extent.[7] Fourth, the attributable burden of epilepsy was not estimated due to the lack of epidemiological data on risk factors of epilepsy in China. Future studies are needed to explain the observed trend and geographic variations of burden caused by epilepsy.
In conclusion, the disease burden of epilepsy is still heavy in China, especially in the western provinces. The incidence and prevalence of epilepsy increased between 1990 and 2019, and the burden of epilepsy in the elderly increased gradually. This study provides evidence on epilepsy prevention and care in different regions in China. China should continue to make epilepsy a public health priority and advocate for action to address gaps in epilepsy care to reduce the burden caused by epilepsy.
Conflicts of interest
None.
Footnotes
How to cite this article: Liu W, Xu Y, Lin Y, Wang L, Zhou M, Yin P, Zhao G. Burden of epilepsy in China and its provinces, 1990 to 2019: findings from the Global Burden of Disease Study 2019. Chin Med J 2023;136:305–312. doi: 10.1097/CM9.0000000000002526
References
- 1.Thijs RD, Surges R, O’Brien TJ, Sander JW. Epilepsy in adults. Lancet 2019; 393:689–701. doi: 10.1016/S0140-6736(18)32596-0. [DOI] [PubMed] [Google Scholar]
- 2.Fiest KM, Sauro KM, Wiebe S, Patten SB, Kwon CS, Dykeman J, et al. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology 2017; 88:296–303. doi: 10.1212/WNL.0000000000003509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neligan A, Hauser WA, Sander JW. The epidemiology of the epilepsies. Handb Clin Neurol 2012; 107:113–133. doi: 10.1016/B978-0-444-52898-8.00006-9. [DOI] [PubMed] [Google Scholar]
- 4.Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia 2014; 55:475–482. doi: 10.1111/epi.12550. [DOI] [PubMed] [Google Scholar]
- 5.Li S, Wu J, Wang W, Jacoby A, de Boer H, Sander JW. Stigma and epilepsy: the Chinese perspective. Epilepsy Behav 2010; 17:242–245. doi: 10.1016/j.yebeh.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 6.de Boer HM, Mula M, Sander JW. The global burden and stigma of epilepsy. Epilepsy Behav 2008; 12:540–546. doi: 10.1016/j.yebeh.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 7.Beghi E, Giussani G, Nichols E, Abd-Allah F, Abdela J, Abdelalim A, et al. Global, regional, and national burden of epilepsy, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18:357–375. doi: 10.1016/S1474-4422(18)30454-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gu L, Liang B, Chen Q, Long J, Xie J, Wu G, et al. Prevalence of epilepsy in the People's Republic of China: a systematic review. Epilepsy Res 2013; 105:195–205. doi: 10.1016/j.eplepsyres.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 9.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song P, Liu Y, Yu X, Wu J, Poon AN, Demaio A, et al. Prevalence of epilepsy in China between 1990 and 2015: a systematic review and meta-analysis. J Glob Health 2017; 7:020706.doi: 10.7189/jogh.07.020706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2019, 2020. Available from: https://collab2019.healthdata.org/gbd-search/. [Accessed on October 31, 2022]. [Google Scholar]
- 13.Ruan Z, Qi J, Qian ZM, Zhou M, Yang Y, Zhang S, et al. Disease burden and attributable risk factors of respiratory infections in China from 1990 to 2019. Lancet Reg Health West Pac 2021; 11:100153.doi: 10.1016/j.lanwpc.2021.100153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin P, Wu J, Wang L, Luo C, Ouyang L, Tang X, et al. The burden of COPD in China and its provinces: findings from the global burden of disease study 2019. Front Public Health 2022; 10:859499.doi: 10.3389/fpubh.2022.859499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu T, Wang B, Liu H, Wang H, Yin P, Dong W, et al. Prevalence and causes of vision loss in China from 1990 to 2019: findings from the Global Burden of Disease Study 2019. Lancet Public Health 2020; 5:e682–e691. doi: 10.1016/S2468-2667(20)30254-1. [DOI] [PubMed] [Google Scholar]
- 16.Reynolds EH. The ILAE/IBE/WHO epilepsy global campaign history. International League Against Epilepsy. International Bureau for Epilepsy. Epilepsia 2002; 43: (Suppl 6): 9–11. doi:10.1046/j.1528-1157.43.s.6.5.x. [DOI] [PubMed] [Google Scholar]
- 17.GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396:1160–1203. doi: 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18:459–480. doi: 10.1016/S1474-4422(18)30499-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ding D, Zhou D, Sander JW, Wang W, Li S, Hong Z. Epilepsy in China: major progress in the past two decades. Lancet Neurol 2021; 20:316–326. doi: 10.1016/S1474-4422(21)00023-5. [DOI] [PubMed] [Google Scholar]
- 20.Reynolds EH. The ILAE/IBE/WHO epilepsy global campaign history. International League Against Epilepsy. International Bureau for Epilepsy. Epilepsia 2002; 43: (Suppl 6): 9–11. doi: 10.1046/j.1528-1157.43.s.6.5.x. [DOI] [PubMed] [Google Scholar]
- 21.Covanis A, Guekht A, Li S, Secco M, Shakir R, Perucca E. From global campaign to global commitment: the World Health Assembly's Resolution on epilepsy. Epilepsia 2015; 56:1651–1657. doi: 10.1111/epi.13192. [DOI] [PubMed] [Google Scholar]
- 22.Wang WZ, Wu JZ, Wang DS, Dai XY, Yang B, Wang TP, et al. The prevalence and treatment gap in epilepsy in China: an ILAE/IBE/WHO study. Neurology 2003; 60:1544–1545. doi: 10.1212/01.wnl.0000059867.35547.de. [DOI] [PubMed] [Google Scholar]
- 23.Jeon JY, Lee H, Shin JY, Moon HJ, Lee SY, Kim JM. Increasing trends in the incidence and prevalence of epilepsy in Korea. J Clin Neurol 2021; 17:393–399. doi: 10.3988/jcn.2021.17.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, et al. ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017; 58:512–521. doi: 10.1111/epi.13709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duncan JS, Sander JW, Sisodiya SM, Walker MC. Adult epilepsy. Lancet 2006; 367:1087–1100. doi: 10.1016/S0140-6736(06)68477-8. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Epilepsy: A Public Health Imperative, 2019. Available from: https://www.who.int/publications/i/item/epilepsy-a-public-health-imperative [Accessed on October 31, 2022]. [Google Scholar]
- 27.Guo Y, Bai J, Na H. The history of China's maternal and child health care development. Semin Fetal Neonatal Med 2015; 20:309–314. doi: 10.1016/j.siny.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Li X, Krumholz HM, Yip W, Cheng KK, De Maeseneer J, Meng Q, et al. Quality of primary health care in China: challenges and recommendations. Lancet 2020; 395:1802–1812. doi: 10.1016/S0140-6736(20)30122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev 2015; 24 (Pt B):197–205. doi: 10.1016/j.arr.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016; 387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 31.China Association Against Epilepsy. Guideline of clinical diagnosis and treatment. Epilepsy. (2015 Revised). Beijing: People's Medical Publishing House; 2015. [Google Scholar]
- 32.China Association Against Epilepsy. 2022. Available from: http://www.caae.org.cn/. [Accessed on October 31, 2022]. [Google Scholar]
- 33.Lin Y, Hu S, Hao X, Duan L, Wang W, Zhou D, et al. Epilepsy centers in China: current status and ways forward. Epilepsia 2021; 62:2640–2650. doi: 10.1111/epi.17058. [DOI] [PubMed] [Google Scholar]
- 34.Li S, Ding D, Liu X. Strategies for epilepsy control in public health aspects. Acta Epileptologica 2019; 1:3.doi: 10.1186/s42494-019-0002-x. [Google Scholar]
- 35.Li S, Wang Y, Wang W, Zhou D, Zhang H, Duan L, et al. The National Comprehensive Governance for epilepsy prevention and control in China. Epilepsia Open 2022; 7:27–35. doi: 10.1002/epi4.12554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang W, Wu J, Dai X, Ma G, Yang B, Wang T, et al. Global campaign against epilepsy: assessment of a demonstration project in rural China. Bull World Health Organ 2008; 86:964–969. doi: 10.2471/blt.07.047050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meinardi H, Scott RA, Reis R, Sander JW. The treatment gap in epilepsy: the current situation and ways forward. Epilepsia 2001; 42:136–149. doi: 10.1046/j.1528-1157.2001.32800.x. [DOI] [PubMed] [Google Scholar]
- 38.Zhao Y, Zhang Q, Tsering T, Sangwan, Hu X, Liu L, et al. Prevalence of convulsive epilepsy and health-related quality of life of the population with convulsive epilepsy in rural areas of Tibet Autonomous Region in China: an initial survey. Epilepsy Behav 2008; 12:373–381. doi: 10.1016/j.yebeh.2007.10.012. [DOI] [PubMed] [Google Scholar]