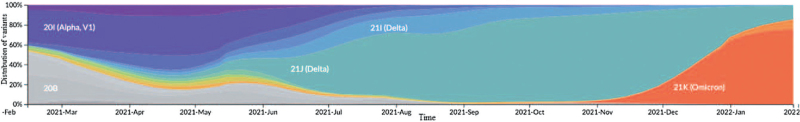
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new virus, still full of surprises. As of September 2022, there have been over 605 million confirmed cases of coronavirus disease 2019 (COVID-19), including 6.5 million deaths reported to the World Health Organization (WHO).[1] SARS-CoV-2 is a bad virus, which often produces new variants that scape natural immunity and sometimes vaccines [Figure 1].[2]
Figure 1.
Worldwide temporal distribution of SARS-CoV-2 variants from February 2021 to February 2022. Source: Genomic epidemiology of novel coronavirus - Global subsampling.[2] SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2. 20B, 21I (Alpha, V1), 21J (Delta), 21I (Delta) and 21K (Omicron) represent name of viral clade.
“2022 must be the year we end the pandemic.” This is not only wishful thinking but a verbatim quote from a conversation with journalists of Dr. Tedros Adhanom Ghebreyesus, WHO Director-General, in Geneva on December 20, 2021.[3]
Similarly, Bill Gates stated, “I think the acute phase of the pandemic will come to a close sometime in 2022. There's no question that the Omicron variant is concerning, but I’m still hopeful that, at some point next year, Covid-19 will become an endemic disease in most places.”[4]
Mankind has survived devastating pandemics, such as the Plague of Justinian (541-542 AD), the bubonic plague that afflicted the Byzantine Empire and Mediterranean port cities, causing 25 million deaths, halving the population of Europe. Or the 1918 Influenza A/H1N1 pandemic, causing 17 to 100 million deaths. These whooping numbers were ridiculed by The Black Death (1346–1353 AD), another outbreak of Yersinia pestis that ravaged Europe, Africa, and Asia, with an estimated overall death toll between 75 and 200 million people.
Regrettably, the level of disinformation and un-coordination has been unprecedented at all levels of COVID-19,[5] and lessons from recent history are yet to be learned, as elegantly stated elsewhere.[6] Barely 2 years from the alert on December 31, 2019 in Wuhan, Hubei Province, China, due to a cluster of 27 hospitalized patients with pneumonia of unknown etiology,[7] and after >294,000 peer-reviewed publications on all sorts of COVID-19-related topics,[8] many questions remain unanswered. To start with, it is still questioned what was the origin of this new virus,[9] although both bats and pangolin have been usual suspects.[10] Additionally, as novelist Albert Camus[11] described in La Peste, a novel on an outbreak of plague sweeping the French Algerian city of Oran, COVID-19 shows many examples of panic, hopelessness, despair, denialists, conspiration theories, fake news, irrationality, and pandemic tiredness.
All human pandemics have eventually come to an end. Therefore, the ongoing COVID-19 pandemic will end, somehow, sometimes, even though this is something difficult to admit when we face the great surge of cases due to the Omicron variant. The key issue is not when (probably there will be nothing as an end), but if we can set up the conditions to control COVID-19 the sooner the better with the minimum toll possible. Synergic and incremental efforts and investments from multiple stake-holders at the global, regional, national, and subnational levels will be required to achieve this goal. These efforts will no doubt arise opposition, and some might be difficult to implement. But inaction will produce a much greater burden in terms of suffering, lost lives, and economic costs.
By revisiting how previous pandemics were ended or controlled,[12] and further implementing/reinforcing individual and community strategies of proven efficacy,[13–15] we can summarize a set of interventions [Table 1] that could contribute to the end of the COVID-19 pandemic.[16] If today we cannot predict when, we can reasonably say how: by applying in a smart, empathic, and consistent way the former list of interventions. Additionally, a key, new scientific landmark is still pending for the progressive elimination of SARS-CoV-2 across the globe. On the horizon are new, more effective vaccines, and potentially antivirals, that interrupt virus transmission,[17–19] and produce neutralizing antibodies to provide sterilizing immunity against re-infection.[20,21] They are eagerly awaited. Further, traditional Chinese Medicine has already been included in COVID-19 treatment guidelines[22] and maybe incorporated in future updates of international guidelines.[23]
Table 1.
List of interventions to stop/control COVID-19.
| Type | Intervention |
| Non-pharmacological | Universal hygiene interventions (hand hygiene, face masks, social distance, ventilation) Screening and case-finding of asymptomatic carriers of SARS-CoV-2 and of pauci-symptomatic COVID-19 |
| Total and partial lockdowns | |
| Bats (and other animals) for planetary health | |
| Pharmacological | Vaccines |
| Antivirals | |
| Combined management strategies of clinical cases | |
| Testing traditional Chinese Medicine in non-Chinese populations | |
| Fostering a more comprehensive health governance | Better coordination and cooperation of international and national health authorities/agencies |
| Fast, complete, transparent data sharing of clinical and epidemiological data, with the capacity to perform and update real-time meta-analyses and identify risk and protective factors of COVID-19 and its sequelae | |
| Consistency in the legal and executive views on individual civil rights in the exceptional circumstances of pandemic risk | |
| Avoid electoral and political use of Public Health interventions | |
| Unified, clear, simple messages to the general population, to avoid misinformation | |
| Advancing on Universal Health Access to health care systems of good quality, particularly at the primary health care level. |
COVID-19: Coronavirus disease 2019.
All of the above should be accompanied by significantly more financial support to national and international Public Health agencies that should work independently of any political drivers. Without health, there is no economy.
Last but not least, inequity is at the root of many health problems. The 12.5+ billion doses of vaccines administered to date, and the few new treatments, have been appallingly and utterly unevenly distributed in low and middle-income countries.[1]
“If we are to end the pandemic in the coming year, we must end inequity,” Dr. Tedros also said.[3] The final answer to COVID-19 will not be only medical, but research-based and focused on solid science and implementation research[24] as well as on advancing universal coverage with health services of good quality, particularly at the primary care level.[25] All with a truly global, planetary perspective.[26] It is now time to sit down, prioritize, administer, and implement in practice such a road map.
Footnotes
How to cite this article: Soriano JB, Infante A. Aiming for the end of the COVID-19 pandemic: the what, how, who, where, and when. Chin Med J 2023;136:1–3. doi: 10.1097/CM9.0000000000002149
References
- 1. WHO Coronavirus (COVID-19) Dashboard. Available from: https://covid19.who.int. [Accessed September 13, 2022] [Google Scholar]
- 2. Genomic epidemiology of novel coronavirus - Global subsampling. Available from: https://nextstrain.org/ncov/global. [Accessed February 10, 2022] [Google Scholar]
- 3. WHO Director-General's opening remarks at the media briefing for Geneva-based journalists - 20 December 2021. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-for-geneva-based-journalists—20-december-2021. [Accessed January 8, 2022] [Google Scholar]
- 4.Gates Notes; the blog of Bill Gates. YEAR IN REVIEW. Reasons for optimism after a difficult year. Available from: https://www.gatesnotes.com/About-Bill-Gates/Year-in-Review-2021?WT.mc_id=20211202100000_YIR2021_BG-EM_&WT.tsrc=BGEM. [Accessed January 9, 2022]. [Google Scholar]
- 5.Morley J, Machado CCV, Burr C, Cowls J, Joshi I, Taddeo M, Floridi L. The ethics of AI in health care: A mapping review. Soc Sci Med 2020; 260:113172. [DOI] [PubMed] [Google Scholar]
- 6.Abraham T. Twenty-first century plague. The story of SARS. Baltimore, MA, USA: The Johns Hopkins University Press; 2004. [Google Scholar]
- 7.Emergencies preparedness, response. Pneumonia of unknown cause -China. Available in press from: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/. [Accessed January 5, 2020]. [Google Scholar]
- 8.COVID-19 in PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/?term=covid-19&sort=date&size=200. [Accessed September 13, 2022]. [Google Scholar]
- 9.Lytras S, Xia W, Hughes J, Jiang X, Robertson DL. The animal origin of SARS-CoV-2. Science 2021; 373:968–970. doi: 10.1126/science. abh0117. [DOI] [PubMed] [Google Scholar]
- 10.WHO calls for further studies, data on origin of SARS-CoV-2 virus, reiterates that all hypotheses remain open. Available from: https://www.who.int/news/item/30-03-2021-who-calls-for-further-studies-data-on-origin-of-sars-cov-2-virus-reiterates-that-all-hypotheses-remain-open. [Accessed January 9, 2022]. [Google Scholar]
- 11.La Peste by Albert Camus. Éditions Gallimard, Oran, France; 1947. [Google Scholar]
- 12.Honigsbaum M, Krishnan L. Taking pandemic sequelae seriously: from the Russian influenza to COVID-19 long-haulers. Lancet 2020; 396:1389–1391. doi: 10.1016/S0140-6736(20)32134-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Living guidance for clinical management of COVID-19. World Health Organization (WHO). Clinical management of COVID-19. Living Guidance; January 2021. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2. [Accessed November 23, 2021]. [Google Scholar]
- 14.An open letter by a group of public health experts; clinicians; scientists. Covid-19: an urgent call for global “vaccines-plus” action. BMJ 2022; 376:o1. doi: 10.1136/bmj. o1. [DOI] [PubMed] [Google Scholar]
- 15.Oliu-Barton M, Pradelski BSR, Algan Y, Baker MG, Binagwaho A, Dore GJ, et al. Elimination versus mitigation of SARS-CoV-2 in the presence of effective vaccines. Lancet Glob Health 2021; 10:e142–e147. doi: 10.1016/S2214-109X (21)00494-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen ZL, Zhang WJ, Lu Y, Guo C, Guo ZM, Liao CH, et al. From severe acute respiratory syndrome-associated coronavirus to 2019 novel coronavirus outbreak: similarities in the early epidemics and prediction of future trends. Chin Med J 2020; 133:1112–1114. doi: 10.1097/CM9.0000000000000776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhatta M, Nandi S, Dutta S, Saha MK. Coronavirus (SARS-CoV-2): a systematic review for potential vaccines. Hum Vaccin Immunother 2021. 1–18. doi: 10.1080/21645515.2020.1865774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calvo Fernández E, Zhu LY. Racing to immunity: journey to a COVID-19 vaccine and lessons for the future. Br J Clin Pharmacol 2021; 87:3408–3424. doi: 10.1111/bcp.14686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang HD, Tao YY, Jia SY, Li JX, Zhu FC. Coronavirus disease 2019 vaccines: landscape of global studies and potential risks. Chin Med J 2021; 134:2037–2044. doi: 10.1097/CM9.0000000000001688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim DS, Rowland-Jones S, Gea-Mallorquí E. Will SARS-CoV-2 infection elicit long-lasting protective or sterilising immunity? (2020) Implications for vaccine strategies. Front Immunol 2020; 11:571481.doi: 10.3389/fimmu.2020.571481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hassan AO, Kafai NM, Dmitriev IP, Fox JM, Smith BK, Harvey IB, et al. A single-dose intranasal ChAd vaccine protects upper and lower respiratory tracts against SARS-CoV-2. Cell 2020; 183:169–184. e13. doi: 10.1016/j.cell.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qu JM, Wang C, Cao B. Chinese Thoracic Society and Chinese Association of Chest Physicians. Guidance for the management of adult patients with coronavirus disease. Chin Med J 2020; 133:1575–1594. doi: 10.1097/CM9.0000000000000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. Living guidance for clinical management of COVID-19. WHO reference number: WHO/2019-nCoV/clinical/2021.2, Geneva; 2021. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2. [Accessed January 10, 2022]. [Google Scholar]
- 24.Wang JW, Cao B, Wang C. Science in the fight against the novel coronavirus disease 2019 (COVID-19). Chin Med J 2020; 133:1009–1011. doi: 10.1097/CM9.0000000000000777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johansen AS, Shriwise A, López-Acuña D, Vracko P. Strengthening the primary health care response to COVID-19: an operational tool for policymakers. Prim Health Care Res Dev 2021; 22:e81.doi: 10.1017/S1463423621000360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soriano JB, Soriano C, Fernández E. Respiratory planetary medicine. Arch Bronconeumol 2016; 53:297–299. doi: 10.1016/j.arbres.2016.10.016. [DOI] [PubMed] [Google Scholar]