To the Editor: Myopia is the most common refractive error and a major reason for visual impairment. The prevalence of myopia is increasing worldwide and is particularly high in Asian countries. It affects 80% to 90% of young people in some parts of East and Southeast Asia.[1] High myopia, which is more than −6.00 D, increases the possibility of visual impairment due to ocular complications caused by extended axial length (AL), which include posterior uveioma, retinal detachment, choroidal new vascularization, and so on. Thus, the prevention and control of myopia is a difficult and important public health issue that has attracted great attention from the World Health Organization and the Chinese government.
The formation of myopia is closely related to the retinal defocal state and AL. Methods to evaluate eccentric refractive errors mainly include subjective eccentric refraction, wavefront measurements with an AHS sensor, streak retinoscopy, and photo refraction with a power refractor.[2] However, these methods have high requirements for patient cooperation, and they are time consuming and difficult to use in clinical practice. More importantly, they can only detect a small area of the retina and cannot accurately detect the peripheral defocus of each region of the retina.
Multispectral refraction topography (MRT) is a new instrument using multispectral imaging. The technology collects ocular fundus images, which are compared and analyzed by a specific computer algorithm with single spectral light of different wavelengths. Finally, it calculates the actual refractive value of each pixel point. MRT can detect the refraction of each part of the retina within a range of 45° at the posterior pole of the retina. Its accuracy and repeatability have been validated.
Therefore, this study measures the peripheral defocus of different degrees of myopia checked by MRT in young students and aims to explore the relationship between retinal defocus and myopia.
Target population and eye examinations. Our present research was a descriptive cross-sectional study, and Ethical Approval was obtained from the Ethics Committee of the Fourth Hospital of Hebei Medical University. Written informed consent was obtained from all participants. We recorded patients presenting for visual problems in an ophthalmology outpatient department of our hospital from December 1, 2021, to March 31, 2022. The inclusion criteria were as follows: (1) ages between 6 to 18 years, (2) with a best corrected visual acuity of 20/20 or better, and (3) agreement to participate and provide informed consent. The exclusion criteria were as follows: (1) acute or chronic ocular diseases, (2) a history of corneal contact lenses, such as orthokeratology lenses, and (3) a history of ocular diseases or previous ocular surgery that might influence refraction or AL.
The refractive errors of all eyes were measured by an autorefractometer (AR-360A, NIDEK Co. Ltd., Japan) after full cycloplegia, 30 min after three drops of compound tropicamide 0.5% and phenylephrine 0.5% (SINQI Pharmaceutical Co., Ltd., Shenyang, China) with an interval of 5 min so that pupils were dilated and the response to light disappeared. We collected the mean of three consecutive autorefraction results conducted as the refractive error value, which is presented as sphere (S) and cylinder (C) measurements. The final refractive error was recorded as the spherical equivalent (SE), and the SE value was the basis for grouping. The equation was SE = S + C/2. The ALs were measured by IOL Master Biometry (Master 2000, Zeiss Co., Germany) under natural light before pupil dilation. We also collected the mean of three measurements as the final result. Retinal defocus was measured by MRT (version 1.0.5T05C; Thondar, Inc.). All examinations were performed by the same well-trained experienced optometrist.
Statistical analysis was performed using SPSS 26.0 (SPSS Inc., Chicago, IL, USA). Normally distributed data are expressed as the mean ± standard deviation, and comparisons between groups were analyzed using one-way analysis of variance. A value of P < 0.05 indicated statistical significance.
In this study, 256 primary and secondary school students (512 eyes) presented to the optometry clinic of our hospital for the diminution of vision or their concerns about it. There were 98 boys and 158 girls aged 6 to 18 years. Of the 512 eyes, 74 had emmetropia (EM, −0.5 D < SE < +0.5 D), 246 had low myopia (LM, −3.0 D < SE ≤ −0.5 D), 122 had moderate myopia (MM, −6.0 D < SE ≤ −3.0 D), and 70 had high myopia (HM, SE ≥ −6.0 D). It is noteworthy that the 74 opposite eyes of those with EM included 16 eyes with EM, 38 eyes with LM, and four eyes with MM. The ages, sex, and values of AL for the four groups are presented in Supplementary Table 1.
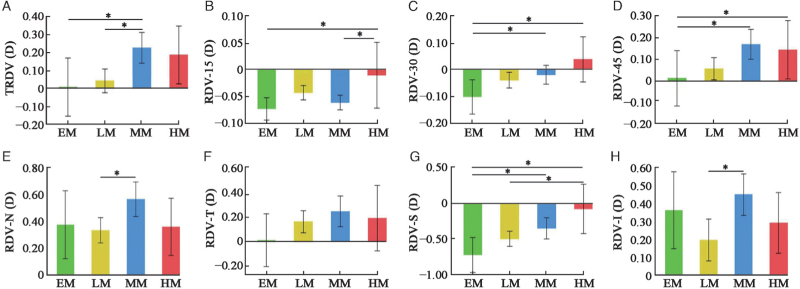
The refraction difference values (RDVs) of the four groups are shown in Supplementary Table 2. According to the values, we found that the retinal peripheral refractive error increased with increasing eccentricity. Eyes with moderate and high myopia presented relative hyperopia. The deeper the degree of myopia is, the greater the hyperopia. There was a significant difference in the value of total refraction difference value (TRDV) between group EM (0.006 ± 0.503) and group MM (0.223 ± 0.475), group LM (0.040 ± 0.533), and group MM (0.223 ± 0.475) (P < 0.05) [Figure 1A]. In the range of RDV-15, there was a significant difference between group EM (−0.073 ± 0.065) and group HM (−0.010 ± 0.176); group MM (−0.061 ± 0.076) and group HM (−0.010 ± 0.176) (P < 0.05) [Figure 1B]. In the range of RDV-30, there was a significant difference between group EM (−0.102 ± 0.199) and group MM (−0.019 ± 0.194); group EM (−0.102 ± 0.199) and group HM (0.038 ± 0.242) (P < 0.05) [Figure 1C]. In the range of RDV-45, there was a significant difference between group EM (0.013 ± 0.396) and group MM (0.168 ± 0.381); group LM (0.056 ± 0.414) and group MM (0.168 ± 0.381) (P < 0.05) [Figure 1D]. In the RDV-nasal (RDV-N) position, there was a significant difference between group LM (0.336 ± 0.763) and group MM (0.566 ± 0.710) (P < 0.05) [Figure 1E]. In the RDV-temporal (RDV-T) position, there was no significant difference among the four groups [Figure 1F]. In the RDV-superior (RDV-S) position, there was a significant difference between group EM (−0.715 ± 0.755) and group MM (−0.346 ± 0.818); group EM (−0.715 ± 0.755) and group HM (−0.075 ± 0.978); and group LM (−0.491 ± 0.852) and group HM (−0.075 ± 0.978) (P < 0.05) [Figure 1G]. In the RDV-inferior (RDV-I) position, there was a significant difference between group LM (0.198 ± 0.940) and group MM (0.449 ± 0.639) (P < 0.05) [Figure 1H].
Figure 1.
The TRDV (A), RDV-15 (B), RVD-30 (C), RVD-N (E), RVD-T (F), RDV-S (G) and RDV-I (H) of different eccentricities and quadrants in four groups. EM: Emmetropia; HM: High myopia; LM: Low myopia; MM: Middle myopia; RDV: Refraction difference value; RDV-I: RDV-inferior; RDV-N: RDV-nasal; RDV-S: RDV-superior; RDV-T: RDV-temporal; TRDV: Total refraction difference value.
The results also showed that there was a significant difference in AL among the four groups (P < 0.05) [Supplementary Figure 1A]. Furthermore, the Pearson correlation analysis indicated an obvious negative correlation of SE with AL (r = − 0.697, P < 0.05) [Supplementary Figure 1B]. Additionally, it indicated a negative correlation of SE with TRDV (r = − 0.125, P < 0.05), RDV-30 (r = − 0.097, P < 0.05), RDV-45 (r = − 0.096, P < 0.05), and RDV-S (r = − 0.166, P < 0.05). It indicated no significant correlation of SE with RDV-15 (r = − 0.026, P = 0.580), RDV-I (r = − 0.048, P = 0.307), RDV-N (r = − 0.054, P = 0.247), and RDV-T (r = − 0.052, P = 0.270).
In our study, all of the students had a myopia defocus within 15° eccentricity. The retina defocus of the fovea or the posterior region has less influence on the development of myopia. Students with high myopia presented an obvious hyperopia defocus at 30° and 45° eccentricity, whereas students with low and MM had relative hyperopia at 45° eccentricity. Chen et al[3] compared the peripheral refractive errors in patients with different refractive degrees and concluded that the hyperopic shift was greater in MM than in LM but was similar in EM and LM.
Notably, eyes with EM had mild hyperopia at 45° eccentricity in this study. After consulting the literature, Mutti et al[4] found that peripheral hyperopia defocus in children appears two years before the onset of myopia, indicating that it may appear in EM. To a certain degree, it confirmed that peripheral hyperopia defocus has predictive significance for the occurrence of myopia.
From the perspective of the four quadrants, we found that all of the eyes in our study showed myopic defocus in the superior retina and obvious hyperopic defocus in other areas. Moreover, the higher the degree of myopia is, the smaller the amount of myopic defocus. In addition, the AL is significantly longer with increasing myopic refraction. This finding indicates that the change in the superior retina is positively correlated with the growth of AL and the decrease in myopic defocus. Shen et al[5] compared the peripheral refractive errors in horizontal, vertical, and two diagonal meridians. They found that the hyperopic shift was greater toward the inferior visual field than toward the superior visual field in the MM and HM groups. Additionally, Gregor F. Schmid's[6] study found that the steepening of the relative peripheral eye length changed the most in the superior retina.
The specific mechanism between peripheral refractive error and myopia remains controversial. Two main views are popular: some insist that peripheral hyperopic defocus is an important trigger for the development of axial myopia, and others argue that peripheral hyperopia may be a result of eye growth.
Our study demonstrated that the retina peripheral refraction of the eyes varied from different eccentricities and quadrants. There was a growing trend with the increase in the degree of myopia in the range of RDV-30 and RDV-45. The RDV in the superior retina increased the most compared with that in the other quadrants. In addition, the degrees of myopia negatively correlated with AL, TRDV, RDV-30, RDV-45, and RDV-S. Therefore, the peripheral refraction of 30° and 45° eccentricities and the superior retina may be closely related to the onset and progression of myopia. However, the sample size of our study was relatively small, and relatively few students had high myopia, since the subjects mainly came from the nearby primary and middle schools. Therefore, conclusions need a larger size and long-term follow-up study to be confirmed.
Conflicts of interest
None.
Supplementary Material
Footnotes
How to cite this article: Zhao Q, Du X, Yang Y, Zhou Y, Zhao X, Shan X, Meng Y, Zhang M. Quantitative analysis of peripheral retinal defocus checked by multispectral refraction topography in myopia among youth. Chin Med J 2023;136:476–478. doi: 10.1097/CM9.0000000000002606
Qing Zhao and Xueli Du contributed equally to this work.
Supplemental digital content is available for this article.
References
- 1.Baird PN, Saw SM, Lanca C, Guggenheim JA, Smith Iii EL, Zhou X, et al. Myopia. Nat Rev Dis Primers 2020; 6:99.doi: 10.1038/s41572-020-00231-4. [DOI] [PubMed] [Google Scholar]
- 2.Liao Y, Yang Z, Li Z, Zeng R, Wang J, Zhang Y, et al. A quantitative comparison of multispectral refraction topography and autorefractometer in young adults. Front Med (Lausanne) 2021; 8:715640.doi: 10.3389/fmed.2021.715640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen X, Sankaridurg P, Donovan L, Lin Z, Li L, Martinez A, et al. Characteristics of peripheral refractive errors of myopic and non-myopic Chinese eyes. Vision Res 2010; 50:31–35. doi: 10.1016/j.visres.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Mutti DO, Hayes JR, Mitchell GL, Jones LA, Moeschberger ML, Cotter SA, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci 2007; 48:2510–2519. doi: 10.1167/iovs.06-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shen J, Spors F, Egan D, Liu C. Peripheral refraction and image blur in four meridians in emmetropes and myopes. Clin Ophthalmol 2018; 12:345–358. doi: 10.2147/OPTH.S151288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmid GF. Association between retinal steepness and central myopic shift in children. Optom Vis Sci 2011; 88:684–690. doi: 10.1097/OPX.0b013e3182152646. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.