Abstract
Purpose:
Physical activity levels (PALs) are associated with mortality risk and were instrumental in estimating national energy requirements, but we are unaware of population-based estimates of PALs in United States (U.S.) adults. Thus, we conducted a nationwide survey using a validated previous-day recall method to estimate PALs and the behavioral determinants of low and higher PALs.
Methods:
Participants from the AmeriSpeak panel 20–75 years of age (N=2,640) completed Activities Completed over Time in 24-hours (ACT24) previous-day recalls. PALs were estimated as the average metabolic equivalent value over 24-hours. Recalls were conducted on randomly selected days in October and November 2019. Survey sample design weights were applied to reflect the U.S. population.
Results:
Mean age was 45.3 years, 51% were female, 67% non-Hispanic White, and 37% had a BMI of ≥30 kg/m2. U.S. adults reported a mean PAL of 1.63 (95% confidence interval = 1.60, 1.65), and 39% (37–42%) of adults reported PALs ≥ 1.6 on a given day. Men reported higher PALs than women (1.67 vs. 1.59) and older adults reported lower PALs. Adults with PALs < 1.4 spent 81% (12.1 hours/d) of their waking day sedentary and 19% (2.7 hours/day) in total physical activity. Adults with PALs considered to be “active”(1.6–1.89) spent only 49% (8.0 hours/d) of their waking day sedentary, and 51% (8.3 hours/day) physically active.
Conclusions:
Our study provides novel estimates of PALs in a nationwide sample of US adults and a description of the type and intensity of sedentary and physically active behaviors contributing to low and higher PALs. These findings may inform public health messages aimed at increasing physical activity in adults and potentially contribute to obesity prevention efforts.
Keywords: DISEASE PREVENTION, OBESITY, SEDENTARY BEHAVIOR, PUBLIC HEALTH
INTRODUCTION
Obesity results, in part, from a long-term imbalance between energy intake and energy expenditure (1), and it increases risk for cardiometabolic disease (2) and many cancer types (3), making it a major public health burden. Physical activity is the most modifiable component of total energy expenditure (TEE) and higher physical activity levels have been associated with lower risk of weight gain and development of obesity in adults (4). The physical activity level (PAL), defined as the ratio of TEE to resting energy expenditure (REE), is a useful descriptive metric that reflects contributions of the fundamental behaviors in which humans engage, including sleep, sedentary behavior, and physical activity to daily energy expenditure.
PALs have been associated with lower mortality in older adults (5); they were integral to estimating daily energy requirements and the Dietary Reference Intakes for United States adults (6); and they are commonly used to estimate energy balance (7). A PAL of 1.6 or greater is classified as “active” (6) and is a level of activity that has been estimated to be consistent with “baseline activities” (i.e., sedentary, PAL < 1.4) plus an additional energy expenditure equivalent to 60 minutes/day or more of moderate intensity walking (6). In older adults, PAL values of 1.58 or greater have been associated with lower mortality risk (5). Given the role of PAL values for estimating national energy requirements, PAL estimates, based on representative samples of US adults, are critically needed as are data-driven descriptions of the combinations of different behaviors that characterize either “baseline activities” (PAL < 1.4) or a physically active lifestyle (PAL ≥ 1.6).
Activities Completed over Time in 24 hours (ACT24) is a previous day recall tool that has been shown to accurately estimate mean sedentary and active time within 2% of accelerometer-based measures of body posture, and mean TEE and PAL values within 5% of DLW-based estimates (8). Furthermore, contextual information captured by ACT24 facilitates investigation of the contributions of a variety of active and sedentary behaviors in different life domains (e.g., work, transportation, household activity, exercise) to estimated PALs. National estimates of physical activity and sedentary behavior as measured by accelerometry are available from representative samples of US adults (9, 10), but algorithms to predict energy expenditure from these data from waist-worn accelerometers appear to underestimate PAL levels (8). To our knowledge prediction algorithms for energy expenditure have not yet been applied to the wrist-worn accelerometer data collected in the US between 2011–14 (11).
Estimates of PALs from the doubly labeled water (DLW) and measured REE would be ideal, but to date such studies have not been completed in representative samples of US adults, perhaps due to their cost and logistical demands. PAL data from DLW measured in selected and convenience samples of adults are available, (12, 13) but the lack of representativeness of study participants creates uncertainty and is a known limitation for population-level estimation (14). Furthermore, DLW- or accelerometer-based estimates of PAL levels provide little detail regarding the different life domains that may contribute to either low or higher PALs. Nationally representative estimates of PALs and the behavioral patterns associated with lower and higher PALs in US adults could inform future work on daily energy requirements and inform obesity prevention strategies.
Thus, we collected estimates of PALs in a nationwide sample of 2,640 US adults using ACT24 recalls and here we report nationwide values for US adults overall and by gender, age, race and ethnicity, and region of the country for: (1) mean PALs and the prevalence of PALs ≥ 1.6, and 2) estimates of the type, intensity, and duration of behaviors associated with different PAL levels.
METHODS
Study population and design
Participants were members of the AmeriSpeak panel, a probability-based survey designed to represent the US population ages 20–75 (15, 16). AmeriSpeak was developed and is maintained by the National Opinion Research Center (NORC) at the University of Chicago, including obtaining and maintaining informed consent. Data collection for this study was completed by the NORC between 10/16/2019 and 11/11/2019 from a general sample of the AmeriSpeak panel 20 to 75 years of age. On an unannounced randomly selected day of the week, participants were sent electronic invitations to complete a short online-survey and a previous-day recall. Those completing the first recall were sent an unannounced invitation to complete a second recall 1–2 weeks later, again on a randomly selected day. Recalls could only be completed on the targeted recall day. The online survey included questions about self-rated health, physical activity, and reported height and weight. Additional demographic information was derived from previous AmeriSpeak data collection efforts. Participants were compensated $15 for each recall completed.
Development of survey sample weights
The AmeriSpeak panel was enrolled using a two-stage sampling design, where the US was divided into 136 strata (e.g. metropolitan statistical areas, counties) and then primary sampling units (PSU, e.g. census tracts, block groups) were sampled from those strata (15). For analytic purposes the 136 strata were combined into 47 virtual strata and each one was divided into 2–113 virtual PSU. Panelists each have a final panel base sampling weight (e.g. a previously calculated weight from the AmeriSpeak panel) and then, for each recall, we calculated study-specific sampling weights that further adjust for non-response in our study and that were raked to external population totals associated with age, sex, education, race/Hispanic ethnicity, housing tenure, telephone status, and Census Division derived from the Current Population Survey (15). We calculated study-specific sampling weights for each day of the week separately (e.g., the participants who completed the recall on a Monday are weighted to represent the US population) and then further normalized the weights so each day contributed equally to the analyses (i.e., after weighting, each day of the week has an equal number of recalls).
Activities completed over time in 24-Hours (ACT24)
Unannounced ACT24 recalls were completed on randomly selected days of the week using an automated online self-administered previous-day recall (8). To complete a recall (on a smartphone, tablet, or computer) participants were asked to report how they spent their time in-bed/sleeping, physically active, and in sedentary behaviors on the previous day (midnight-midnight) by selecting from more than 170 individual activities organized in 14 major categories (see Supplemental Table 1, Supplemental Digital Content, ACT24 Major Categories and selectable behaviors). After an activity was selected, a series of follow-up questions assessed the duration of the activity, body position, and other details. Activities reported are linked to the Compendium of Physical Activities (17) and data were scored to estimate energy expenditure using metabolic equivalent (MET) values for each activity reported. PAL values were calculated by dividing total MET-hours reported in-bed/sleeping, sedentary, and in physical activity by the total number of hours/day reported on each recall (e.g., 24 hours). Sedentary behaviors were defined as those involving sitting/reclining and little energy expenditure (typically ≤ 1.5 METs) outside of time in-bed for the primary sleep period, or that is during the waking day. Time-use in specific life domains was classified using ACT24 major category labels in a manner consistent with the American Time-use Survey (ATUS) lexicon (18) (see Supplemental Table 2, Supplemental Digital Content, Time-use classifications derived from ACT24 Major Category reports). Quality control checks were completed and for recalls with more than one activity reported at the same time (overlaps), the most active behaviors for the overlapping time were selected, and the total amount of time reported in each behavior was recalculated. An earlier computer-only version of ACT24 was found to accurately estimate mean TEE and PAL within 5% in comparison to DLW-based estimates, and within 2% of mean time spent sedentary and physically active in comparison to activPAL (8). In 47 adults 20–73 years of age, we found the current version of ACT24 to provide accurate estimates of mean sedentary behavior (9.1 (SD=2.3) vs. 9.3 (2.1) hours/day) and physical activity (6.4 (SD=2.1) vs. 6.3 (1.9) hours/day) vs. activPAL. Correlations between measures were also relatively high (Spearman rho=0.61 and 0.65 for sedentary and active duration, respectively; unpublished observations). Similar recall-based assessment methods have been found to provide useful estimates of domain-specific behaviors in middle-aged and older adults (19, 20).
Statistical analysis
We first described the demographic characteristics for the participants, overall and by gender. For continuous variables, we calculated weighted means. For categorical variables, we tabulated the actual (i.e., unweighted) number of participants and the weighted percentages in each category. Reported PAL values were used to classify population groups as sedentary (PAL=1.0–1.39), low active (PAL=1.4–1.59), active (PAL=1.6–1.89), and very active (PAL=1.9–4.8) (6).
We then described the PAL of the population overall and by demographic categories. We report mean PAL values and the proportion with a PAL of 1.6 or more. In each of the four PAL categories, we also estimated time and energy expenditure (MET-hours/day) spent in-bed/sleeping, sedentary, and by physical activity intensity (i.e., light, moderate, vigorous). We also estimated time spent sedentary and in physical activity in different life domains in each of the four PAL categories. To test for overall associations by demographic factors and for statistical differences between PAL categories we performed linear regression with the categorical/ordinal demographic variable as the independent variable.
All analyses were conducted using Stata 16.1 while considering survey sampling weights as described above.
RESULTS
Of 15,153 AmeriSpeak panelists invited, 2,877 completed the short survey and at least one provisionally valid recall, for a completion rate of 19.0% (n=2,838 first recalls, n=1,737 second recalls). The demographic characteristics of respondents were like those of US adults in terms of age, sex, race and ethnicity, marital status, and home ownership, but lower income individuals were overrepresented and higher income groups were underrepresented (see Supplemental Table 3, Supplemental Digital Content, Demographic characteristics (%) in the unweighted and weighted samples and the Current Population Survey (CPS)). From 4,575 total recalls, following quality control checks we excluded recalls (in this order) with more than 1 hr/d of unknown time (gaps; private un-reported time; n=293 [6.4%] recalls), 2 or more hours/day of overlapping time (n=91 [2.0%] recalls), and recalls with 0 sedentary hours (n=24 [0.5%] recalls). Following exclusions, survey sample weights were recalculated for 2,640 participants with at least one valid recall (n=2,478 first recalls, n=1,689 second recalls).
Mean age in the population was 45.3 years and 51% were females (Table 1). About two-thirds were non-Hispanic-white, 35% had a high school education or less, 41% reported a household income of <$50,000, and 67% were currently working for pay. Thirty-seven percent reported a BMI of 30 kg/m2 or more and 58% reported meeting the current guideline for aerobic physical activity (21).
Table 1.
Descriptive characteristics of the study sample
| All Participants | Male | Female | |
|---|---|---|---|
| Overall | 2,640 (100.0) | 1,460 (49.4) | 1,179 (50.6) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Age (years) | 45.3 (15.4) | 46.5 (15.5) | 44.1 (15.2) |
| Frequency (weighted %) | Frequency (weighted %) | Frequency (weighted %) | |
| Age (years) | |||
| 20–29 | 435 (20.8) | 201 (18.9) | 234 (22.6) |
| 30–39 | 718 (20.1) | 366 (17.7) | 352 (22.5) |
| 40–49 | 494 (18.0) | 304 (20.3) | 190 (15.7) |
| 50–59 | 468 (18.4) | 268 (18.2) | 200 (18.6) |
| 60–69 | 394 (16.8) | 237 (17.9) | 157 (15.8) |
| 70–74 | 131 (5.9) | 84 (7.1) | 47 (4.7) |
| Race/ethnicity | |||
| White, non-Hispanic | 1,797 (63.7) | 1,049 (66.2) | 748 (61.2) |
| Black, non-Hispanic | 282 (10.9) | 104 (8.9) | 178 (12.9) |
| Hispanic | 336 (17.0) | 148 (14.1) | 188 (19.7) |
| Asian | 105 (3.6) | 82 (5.0) | 23 (2.2) |
| Other groupsa | 120 (4.9) | 77 (5.8) | 43 (4.0) |
| Educational Attainment | |||
| High School or less | 381 (34.6) | 209 (35.4) | 172 (33.7) |
| Some college/Assoc. Degree | 1021 (29.0) | 524 (27.5) | 497 (30.5) |
| Bachelor’s Degree | 721 (20.9) | 424 (21.9) | 297 (19.9) |
| Graduate Degree | 517 (15.5) | 303 (15.1) | 214 (16.0) |
| Household Income ($) | |||
| < 50,000 | 959 (41.3) | 448 (37.3) | 510 (45.1) |
| 50,000–99,000 | 950 (34.1) | 556 (36.5) | 394 (31.8) |
| 100,000–149,000 | 449 (15.5) | 269 (15.6) | 180 (15.3) |
| 150,000+ | 282 (9.2) | 187 (10.5) | 95 (7.8) |
| Occupational Status | |||
| Working for pay | 1,933 (67.2) | 1,113 (70.2) | 820 (64.3) |
| Not working - looking/laid off | 130 (6.2) | 63 (6.0) | 67 (6.4) |
| Not working - other | 174 (7.5) | 42 (3.0) | 132 (11.8) |
| Retired | 287 (13.4) | 173 (14.2) | 114 (12.5) |
| Disabled | 116 (5.8) | 69 (6.6) | 47 (4.9) |
| Body Mass Index (kg/m2) | |||
| < 25 | 734 (27.6) | 367 (25.2) | 367 (30.0) |
| 25–29.9 | 870 (33.4) | 538 (37.5) | 332 (29.4) |
| 30+ | 960 (36.5) | 509 (34.9) | 451 (38.2) |
| Missing | 76(2.5) | 46 (2.5) | 30 (2.5) |
| Aerobic Physical Activity b | |||
| Inactive | 323 (13.9) | 169 (12.7) | 154 (15.1) |
| Insufficiently Active | 755 (27.8) | 373 (23.9) | 382 (31.5) |
| Sufficiently Active | 640 (24.1) | 343 (22.4) | 297 (25.8) |
| Highly Active | 912 (34.0) | 571 (40.9) | 341 (27.3) |
| Missing | 10 (0.2) | 4 (0.1) | 6 (0.4) |
| Region | |||
| New England | 118 (5.0) | 71 (5.8) | 47 (4.3) |
| Mid-Atlantic | 266 (11.8) | 147 (12.7) | 119 (11.0) |
| East North Central | 479 (14.7) | 257 (14.4) | 222 (14.9) |
| West North Central | 258 (6.0) | 140 (5.7) | 118 (6.2) |
| South Atlantic | 497 (22.1) | 261 (20.2) | 236 (23.8) |
| East South Central | 112 (4.7) | 70 (5.5) | 42 (3.9) |
| West South Central | 248 (11.3) | 140 (11.2) | 108 (11.4) |
| Mountain | 251 (8.9) | 147 (9.1) | 104 (8.8) |
| Pacific | 411 (15.6) | 227 (15.5) | 184 (15.6) |
Other race and ethnicity groups include two smaller groups of non-Hispanics adults reporting “Other” or two or more race or ethnicities
Aerobic Physical Activity: Inactive (0 hours/week); Insufficiently active (0.1 to 2.49 hours/week moderate or 1.24 hours/week vigorous); Sufficiently active (2.5 to 5.0 hours/week moderate or 1.25 to 2.5 hours/week vigorous); Highly active (> 5hours/week moderate or > 2.5 hours/week vigorous)
Overall, US adults reported an average PAL of 1.63 (95%CI, 1.60–1.65) and a PAL of ≥1.6 was reported by 39.6% (37.2–41.9) of the population on a given day (Figure 1). Men reported significantly higher PALs than women (1.67 vs. 1.59; PAL Δ= −0.08) and increasing age was associated with significantly lower PAL values. For example, the mean PAL value for 20–34-year-olds was 1.66 while values for 65–74-year-olds was 1.58 (PAL Δ= −0.08). Age was not significantly associated with reported prevalence of PAL greater than 1.6.
Figure 1.
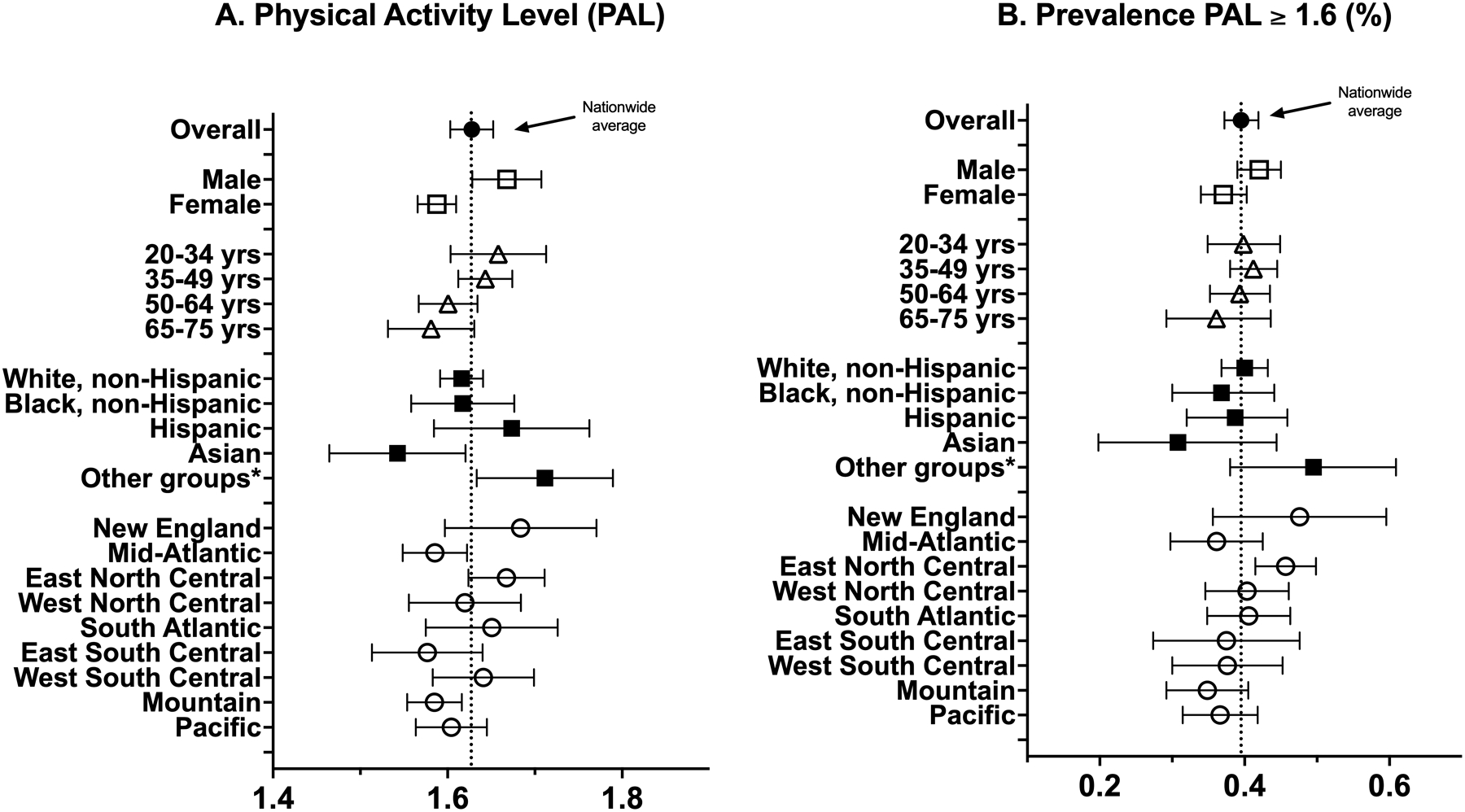
PAL and prevalence of PAL ≥ 1.6 overall and by demographic groups
Values are mean and 95% Cis
*Other race and ethnicity groups include two smaller groups of non-Hispanics adults reporting “Other” or two or more race or ethnicities
Mean PAL values were significantly associated with race and ethnicity, but the prevalence of PAL ≥1.6 was not. Asian adults reported lower PALs than the overall population, while adults representing several smaller race and ethnic groups reported higher PAL levels. Non-Hispanic Black and White adults reported similar PALs (Figure 1). Mean PAL values were also significantly associated with region of the country, but the prevalence of PAL ≥1.6 was not. The two Regions with the highest PALs were – New England (CT, MA, VT, NH, ME, RI); PAL=1.68) and East North Central (IL, IN, MI, OH, WI);PAL=1.67), and the two Regions with lowest PALs were East South Central (AL, KY, MS, TN); PAL=1.58) and the Mountain West (AZ, CO, ID, MT, NV, NM, UT, WY); PAL=1.58).
Next, we examined the duration and expenditure estimates across increasing PAL categories. The prevalence across the four PAL categories was: PAL < 1.4 (28.0%), PAL 1.4–1.59 (32.5%), PAL 1.6–1.89 (22.3%), and PAL ≥1.9 (17.3%). The major behavioral gradient associated with higher PALs, was the balance between active and sedentary time, and to a lesser extent time reported in-bed/sleeping. For example, adults reporting the lowest PALs (<1.4) reported significantly more sleep (9.2 [95%CI, 8.9–9.4] hours/day) and sedentary time (12.1 [11.8–12.4] hours/day) and significantly less time in physical activity (2.7 [2.5–2.8] hours/day). In contrast, those with PALs of 1.6–1.89 reported 7.8 [7.6–8.0] hours/day in-bed/sleeping, and roughly equal amounts of time sedentary (8.0 [7.7–8.2] hours/day) and physically active (8.3 [8.0–8.5] hours/day) (Figure 2, panel A). Adults in the most active PAL category (PAL ≥1.9) spent substantially more time in physical activity (11.0 [10.7–11.4] hours/day) compared to time reported sedentary (5.8 [5.5–6.1] hours/day). Overall, higher PAL values tended to be associated with larger amounts of time reported in light and moderate intensity activity in comparison to greater increases in amounts of vigorous intensity activity. Similar patterns were noted for increasing TEE (MET-hours/day) across the PAL categories (Figure 2, panel B).
Figure 2.
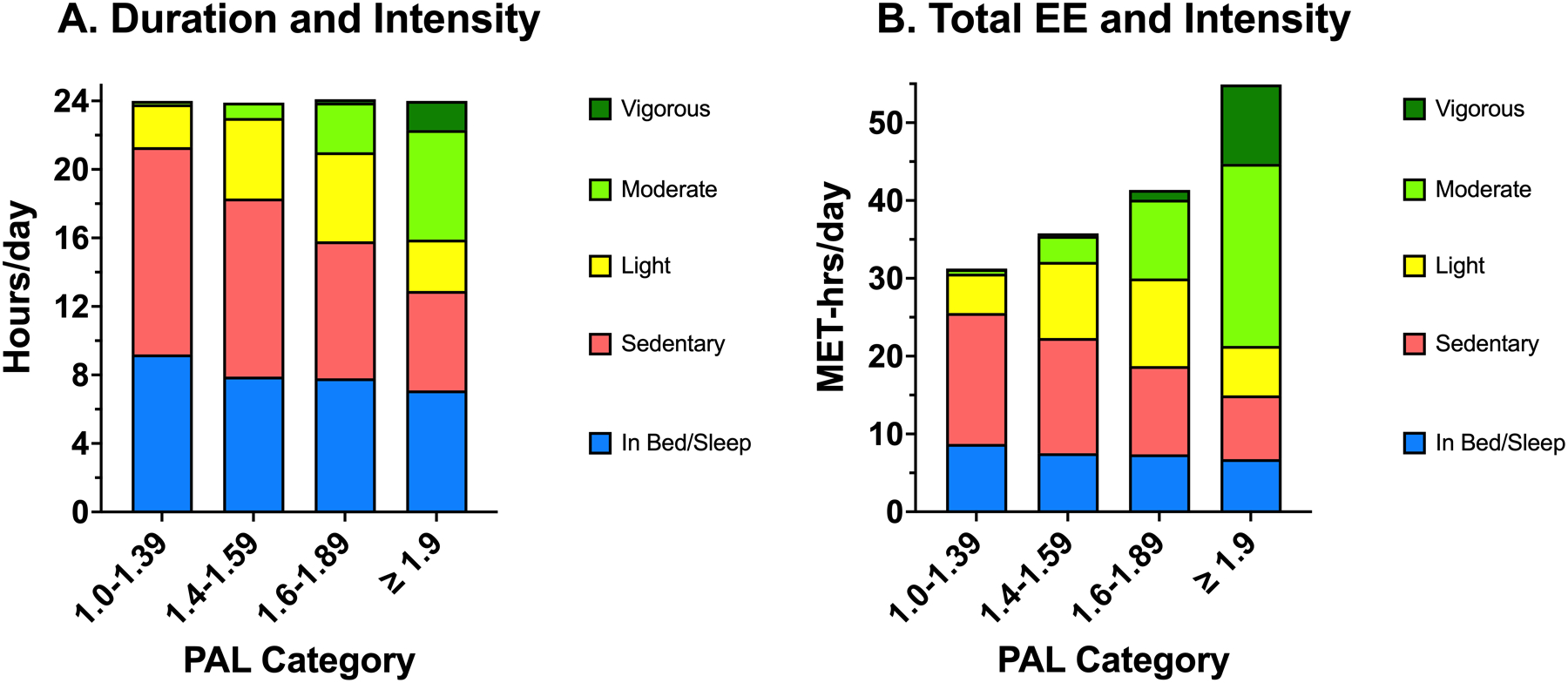
Distribution of time and energy expenditure by type/intensity across PAL categories
Figure 3 presents results in terms of the percentage of the waking day (outside of in-bed/sleep time) spent sedentary and in different physical activity intensities across the increasing PAL categories. US adults with PAL values less than 1.6 reported spending 63% or more of their waking time sedentary, and less than 37% of their time physically active. In contrast, adults with a PAL of ≥1.6 reported spending less than half of their waking day (< 49%) sedentary and a more than half of their waking day in physically active pursuits (>51%; Figure 3).
Figure 3.
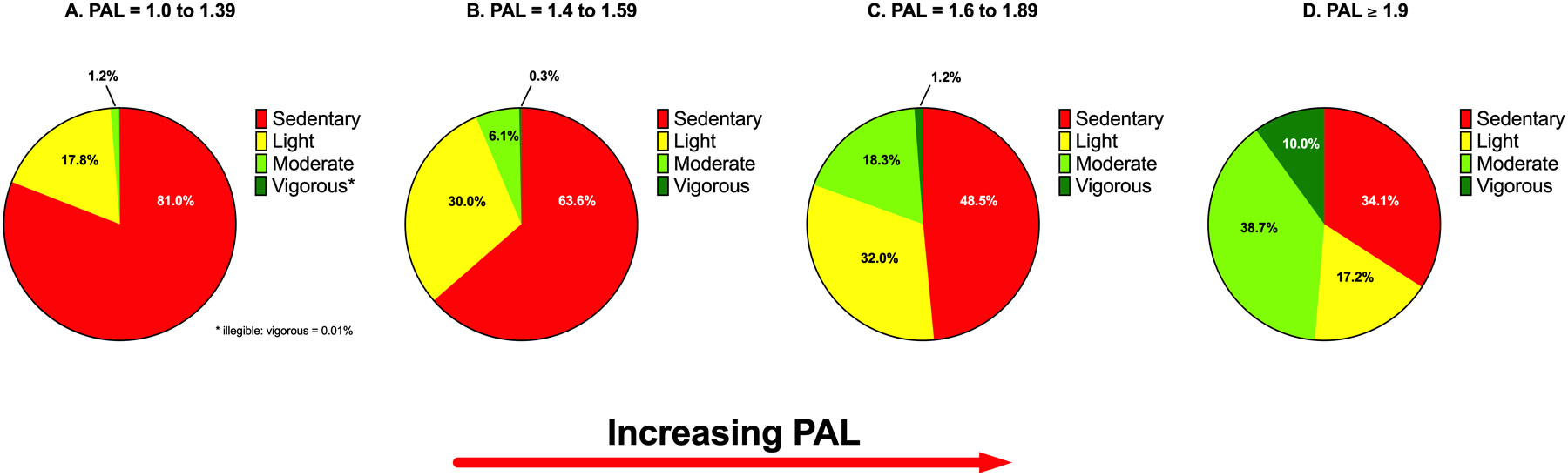
Proportion of the waking day (%)* spent sedentary and in different physical activity intensities, across PAL categories
*Waking day reflects all time reported not in-bed/sleeping
Across the four PAL categories we also examined estimates of domain-specific time use in sedentary and physically active behaviors during the waking day (Figure 3). Adults in the lowest PAL category (PAL < 1.4) reported significantly greater amounts of sedentary leisure (5.9 [5.6–6.3] hours/day) and work (2.9 [2.6–3.2] hours/day) compared to adults in the first physically active category (PAL=1.6–1.89; sedentary leisure [3.6 {3.4–3.8} hours/day], sedentary work [1.1 {1.0–1.3} hours/day]). Variation in sedentary time in other domains was less strongly related to PALs (Figure 3, panel A). Three domains of physical activity were significantly associated with PAL categories (Figure 3, panel B); the strongest associations were for household and work activities, and to a lesser extent leisure time physical activity, or exercise and recreation Work related activities were a large contributor among adults in the highest PAL category (PAL ≥1.9).
DISCUSSION
In this first nationally representative study of PALs in US adults we found that adults reported a mean PAL of 1.63 on average and about 40% of the population reported PAL values in the active category on a given day. As expected, males reported higher PALs than females, and older age was associated with lower PALs. Variation in PALs were also observed in different race and ethnic groups and by region of the country. Adults with PALs less than 1.4 reported spending 12.1 hours/day (81%) sedentary during waking hours, and most of this sedentary time was spent in leisure and occupational pursuits. In contrast, adults with PALs of 1.6 or more reported spending just under 50% of their waking time engaged in sedentary behaviors and greater amounts of time engaged in light and moderate intensity physically active pursuits at home and at work. Overall, vigorous intensity activity and exercise and fitness-oriented activities contributed only modestly to higher PALs. Results from this study provide unique estimates of PAL values in US adults as well as a detailed portrait of the type, amount and intensity of activity that contribute to lower and higher daily PALs.
Detailed estimates of PAL values and the major behavioral contributors to these levels from more representative population-based samples of adults using either DLW or factorial estimation methods like those used here are rare, and methodological differences and the different types of populations studied (i.e., convenience or representative samples) makes absolute comparisons difficult. In a representative sample of US adults, Harms and colleagues (22) reported PALs of 1.59 for US adults between 2003–13 using time-use data and factorial methods, which is comparable to our overall estimate of 1.63. One critical difference between traditional time-use data and the information gathered by ACT24 is that the latter method was specifically designed to estimate energy expenditure, it asks about body posture to help identify sedentary behaviors, and it captures more detailed information about individual occupational activities. In contrast, time use surveys were originally designed to investigate distinct aspects of time use often related to social and economic factors, and only limited detail about occupational activities are generally assessed (i.e., total time and work and job type). These differences may account for the slightly higher PAL estimates in the current report compared to the population-based PAL estimates in the US based on traditional time use surveys (22, 23).
The only DLW-based estimates of physical activity energy expenditure in a representative sample of adults of which we are aware was reported by Brage and colleagues for adults in the United Kingdom (UK) (24). Using TEE and REE data reported in Table 1 of the Brage report we calculated PAL values for males and females aged 16–49, 50–64, and 65–91 years. Measured PAL values for males and females aged 16–49 years were 1.85 and 1.80, for those aged 50–64 years PAL values were 1.83 and 1.78, respectively, and lower PALs were reported for older adults aged 65–91 years (males PAL=1.75; females PAL=1.74). Along with the US estimate mentioned above, Harms and colleagues (22) also estimated population-based PAL estimates using time-use data in UK adults in 2001 to be 1.62 and 1.74 in Polish adults in 2012. In DLW-based estimates of PAL derived from pooled DLW studies conducted in convenience samples, Dugas and colleagues (14) reported mean PALs of 1.79 for males and 1.71 for females in studies from countries with higher human development index values. Similar mean PAL values were reported by Pontzer and colleagues in a larger set of pooled DLW data from non-representative samples of adults (12). Population measures of PAL in representative samples of US adults using other validated methods are needed to replicate and/or clarify our findings.
Nevertheless, we do note several important similarities in how many of these studies describe differences in PAL values between population sub-groups, for example differences in PAL by sex and age. In the present study males reported PALs that were on average 0.08 PAL units higher than females, while this difference in pooled DLW studies was also 0.08 PAL units (14), and the difference in UK adults aged 50–64 years was 0.05 PAL units (24). Similarly, PAL values tended to be lower with increasing age in most studies, and the gender differences in PAL shrank or disappeared in older adults in these studies (14, 24), consistent with the findings in the present report. This general tracking of important differences in population sub-groups further highlights the potential value of ACT24 or similar methods for surveillance of PAL values.
A unique aspect of the present study is our description of the type and amounts of physical activity and sedentary behaviors associated with PALs < 1.4 (low) or higher PALs (e.g., 1.6–1.89). Among the US adults reporting low PALs (28% of days sampled), sedentary behavior was the predominate behavior reported (12.1 hours/day) accounting for 81% of time spent in the waking day. In contrast, adults reporting PAL values of 1.6 to 1.89 reported spending an average of 8.0 hours/day sedentary, or 49% of the waking day. Interestingly, in a doubly labeled water study of older adults, compared to those with PALs < 1.57, individuals with PALs of 1.57–1.78 had a 36% lower mortality risk, while those with PALs > 1.78 had 57% lower mortality (5). An accelerometer-based mortality study also found that adults at low risk for mortality due to higher physical activity levels spent 49% of their waking time sedentary and 51% of their time physically active (25).
We also found that higher PAL levels were associated with greater amounts of light and moderate, and to a lesser extent vigorous intensity activity in most of the population. This finding is consistent with an earlier report by Westerterp (26) derived from DLW and accelerometer-based measures showing limited contribution of vigorous intensity activity to higher PALs. In terms of the types of behavior associated with being in either the low or higher PAL categories, sedentary leisure and work domains were linked to the higher sedentary time and low PAL levels. We have previously shown that sedentary leisure-time is mainly derived from consumption of electronic media, or screen time (27). Greater amounts of household and work-related activities, and to a lesser extent leisure-time physical activity, were associated with higher PAL levels. Similar findings have been noted in time-use studies that have focused on physical activity and energy expenditure (22, 28). Overall, time spent in sedentary behavior was a major driver of low PAL levels while daily activities done at home and work reflect the major types of behavior that got US adults into higher PAL categories.
This report has several limitations that should be considered. First, we used factorial-based methods that rely upon self-report of the durations of many different behaviors within the recall day, and table-referenced MET values to estimate PALs. This previous-day recall method, and similar methods, have been shown to be accurate for group-level estimation of active and sedentary time compared to activPAL (8, 29) and camera-based recordings (20); to accurately estimate mean PAL values compared to DLW-based estimates (8, 30); and to be free of social desirability bias (31, 32). Nevertheless, it’s possible that the current results under- or over-estimate PAL levels, and the use of PAL values will not fully adjust for differences in body mass. We employed a PAL of 1.6 as described by the Institute of Medicine (6) to estimate the prevalence of an “active” day in the population, but use of a PAL value of 1.7 (33) would produce lower prevalence estimates. It should also be noted that ACT24 has not been tested in all race and ethnic groups investigated in this report, and this should be considered when interpreting the present results. However, our finding of higher PAL values for Hispanic adults and no differences between black and white adults mirror earlier findings from population-based accelerometer studies of physical activity and sedentary time (9, 10). Another possible limitation is our application of only 1 or 2 recalls to estimate mean values in the population in one season of the year rather than to estimate habitual levels for individuals. However, day-to-day variation in behavior is expected to have minimal impact on estimation of the population mean values when days of the week are equally represented (34). We elected to collect data in the Fall of the year to minimize extremes of seasonal variation between summer and winter. Additionally, the use of unannounced recalls requiring a same-day response may have reduced our recall completion rates, which could lead to bias because of nonresponse. Although the distribution of demographic characteristics in our weighted sample approximated those of the U.S. population for several demographic factors, it is possible that inadequate representativeness or unmeasured factors strongly linked to physical activity could bias our results. A major strength of this report is our application of a validated previous-day recall tool (ACT24) in a large population-based sample of US adults enrolled in the AmeriSpeak panel (15). Ideally, we would have liked to have measures of TEE from DLW paired with REE measures in a representative sample of US adults, but the logistical and financial hurdles of obtaining such data are limiting.
CONCLUSIONS
In this nationwide study we found the mean PAL of US adults to be 1.63 and that on a given day about 40% of the adult population reported engaging in enough physical activity to be classified as physically active by their PAL level. Notably, on physically active days (PAL > 1.6), US adults spent only about half of their waking day sedentary and the other half in physically active pursuits. Further studies of PAL could help identify modifiable psychological and contextual determinants of healthy levels of energy expenditure as well as strengthen epidemiological studies of the relationship between energy expenditure and health outcomes.
In concert with etiologic studies of mortality (e.g., (5, 25) population-based profiles of PAL levels describing the amount and or proportion of the waking day spent sedentary or physically active may inform future obesity prevention and public health messages aimed at increasing physical activity in the population.
Supplementary Material
Supplemental Table 1. ACT24 Major Categories and selectable behaviors
Supplemental Table 2. Time-use classifications derived from ACT24 Major Category reports
Supplemental Table 3. Demographic characteristics in the unweighted and weighted samples and the Current Population Survey
Figure 4.
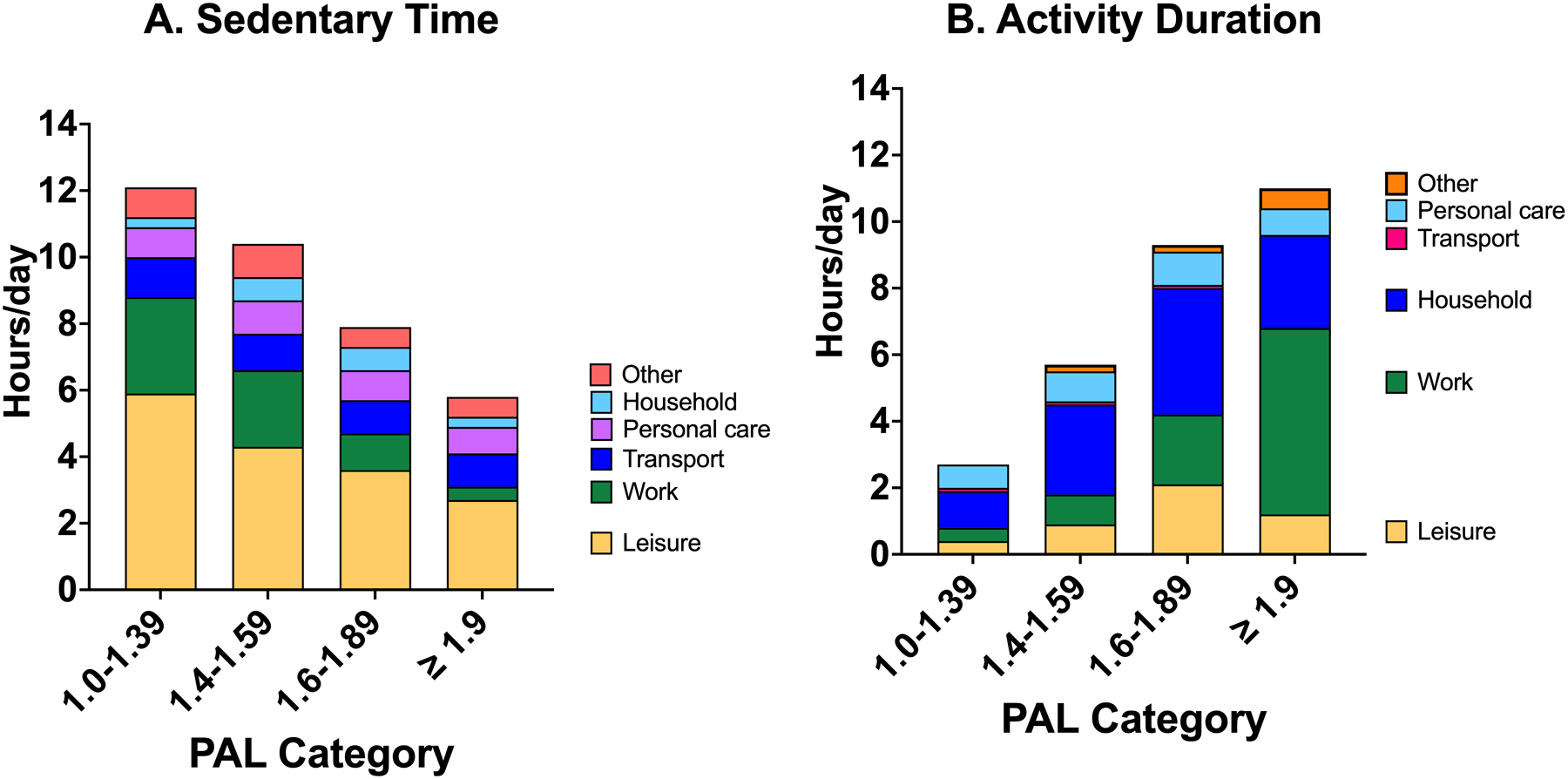
Time-use in in the waking day* in sedentary and physically active behaviors by PAL categories
*Waking day reflects all time reported not in-bed/sleeping
Acknowledgements
This research was supported by the National Institutes of Health Intramural Research Program, National Cancer Institute, Division of Cancer Epidemiology and Genetics. The authors thank the AmeriSpeak team at the University of Chicago for their expert guidance in developing and implementing this project in the field.
Conflict of Interest and Funding Source:
This research was supported by the National Institutes of Health Intramural Research Program, National Cancer Institute, Division of Cancer Epidemiology and Genetics. The authors have no conflicts of interest to disclose. Results from this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. Results of this study do not constitute endorsement by the American College of Sports Medicine.
Footnotes
SUPPLEMENTAL DIGITAL CONTENT
SDC 1: Supplemental Digital Content.docx
REFERENCES
- 1.Schwartz MW, Seeley RJ, Zeltser LM, et al. Obesity pathogenesis: an Endocrine Society Scientific Statement. Endocr Rev. 2017;38(4):267–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet. 2014;383(9921):970–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569–78. [DOI] [PubMed] [Google Scholar]
- 4.2018 Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services, 2018. [Google Scholar]
- 5.Manini TM, Everhart JE, Patel KV, et al. Daily activity energy expenditure and mortality among older adults. JAMA. 2006;296(2):171–9. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholsterol, Protein, and Amino Acids (2005). Washington, DC: The National Academies Press; 2005. [Google Scholar]
- 7.National Institute of Diabetes and Digestive and Kidney Diseases. Body Weight Planner [cited 2022. April 8, 2022]. Available from: https://www.niddk.nih.gov/bwp.
- 8.Matthews CE, Keadle SK, Moore SC, et al. Measurement of active & sedentary behavior in context of large epidemiologic studies. Med Sci Sports Exerc. 2017;50(2):266–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. [DOI] [PubMed] [Google Scholar]
- 10.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors - United States 2003–2004. Am J Epidemiol. 2008;167(7):875–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Belcher BR, Wolff-Hughes DL, Dooley EE, et al. US Population-referenced percentiles for wrist-worn accelerometer-derived activity. Med Sci Sports Exerc. 2021;53(11):2455–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pontzer H, Yamada Y, Sagayama H, et al. Daily energy expenditure through the human life course. Science. 2021;373(6556):808–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Westerterp KR, Yamada Y, Sagayama H, et al. Physical activity and fat-free mass during growth and in later life. Am J Clin Nutr. 2021;114(5):1583–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dugas LR, Harders R, Merrill S, et al. Energy expenditure in adults living in developing compared with industrialized countries: a meta-analysis of doubly labeled water studies. Am J Clin Nutr. 2011;93(2):427–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NORC. Technical Overview of the AmerSpeak® Panel NORC’s Probability-based Household Panel Chicago: NORC; 2018. [cited 2019 02/28/2019]. Available from: http://www.norc.org/PDFs/AmeriSpeak%20Technical%20Overview%202015%2011%2025.pdf.
- 16.NORC. AmeriSpeak® Panel Demographics Report Chicago: NORC; 2018. [cited 2019 02/28/2019]. Available from: https://d3qi0qp55mx5f5.cloudfront.net/amerispeak/i/research/AmeriSpeak_Panel_Demographic_Report_2018_08_30.pdf?mtime=1535739132.
- 17.Ainsworth BE, Haskell WL, Herrmann SD, et al. Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81. [DOI] [PubMed] [Google Scholar]
- 18.Bureau of Labor Statistics. American Time Use Survey — Activity Coding Lexicons and Coding Rules Manuals 2016 [cited 2018. March 19, 2018]. Available from: https://www.bls.gov/tus/lexicons.htm.
- 19.Keadle SK, Lyden K, Hickey A, et al. Validation of a previous day recall for measuring the location and purpose of active and sedentary behaviors compared to direct observation. Int J Behav Nutr Phys Act. 2014;11:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harms T, Gershuny J, Doherty A, Thomas E, Milton K, Foster C. A validation study of the Eurostat harmonised European time use study (HETUS) diary using wearable technology. BMC Public Health. 2019;19(Suppl 2):455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd edition. Washington, DC: U.S. Department of Health and Human Services; 2018. p. 42–3. [Google Scholar]
- 22.Harms T, Berrigan D, Gershuny J. Daily metabolic expenditures: estimates from US, UK and polish time-use data. BMC Public Health. 2019;19(Suppl 2):453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deyaert J, Harms T, Weenas D, Gershuny J, Glorieux I. Attaching metabolic expenditures to standard occupational classification systems: perspectives from time-use research. BMC Public Health. 2017;17(1):620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brage S, Lindsay T, Venables M, et al. Descriptive epidemiology of energy expenditure in the UK: findings from the National Diet and Nutrition Survey 2008–15. Int J Epidemiol. 2020;49(3):1007–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matthews CE, Keadle SK, Troiano RP, et al. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in US adults. Am J Clin Nutr. 2016;104(5):1424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Westerterp KR. Pattern and intensity of physical activity. Nature. 2001;410(6828):539. [DOI] [PubMed] [Google Scholar]
- 27.Matthews CE, Carlson SA, Saint-Maurice PF, et al. Sedentary behavior in U.S. adults: fall 2019. Med Sci Sports Exerc. 2021;53(12):2512–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dong L, Block G, Mandel S. Activities contributing to total energy expenditure in the United States: results from the NHAPS study. Int J Behav Nutr Phys Act. 2004;1(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matthews CE, Keadle SK, Sampson J, et al. Validation of a previous-day recall measure of active and sedentary behaviors. Med Sci Sports Exerc. 2013;45(8):1629–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bratteby LE, Sandhagen B, Fan H, Samuelson G. A 7-day activity diary for assessment of daily energy expenditure validated by the doubly labelled water method in adolescents. Eur J Clin Nutr. 1997;51(9):585–91. [DOI] [PubMed] [Google Scholar]
- 31.Matthews CE, Keadle SK, Sampson J, et al. Validation of a previous-day recall measure of active and sedentary behaviors. Med Sci Sports Exerc. 2013;45(8):1629–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adams SA, Matthews CE, Ebbeling CB, et al. The effect of social desirability and social approval on self-reports of physical activity. Am J Epidemiol. 2005;161(4):389–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Human energy requirements: Report of a Joint FAO/WHO/UNU Expert Consultation Rome: FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS; 2004. [updated 2004; cited 2013 November 11, 2022]. Energy Requirements for Adults]. Available from: http://www.fao.org/docrep/007/y5686e/y5686e07.htm#bm07.
- 34.Gibson R. Principles of Nutritional Assessment. 2nd Edition. Oxford (United Kingdom): Oxford University Press; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. ACT24 Major Categories and selectable behaviors
Supplemental Table 2. Time-use classifications derived from ACT24 Major Category reports
Supplemental Table 3. Demographic characteristics in the unweighted and weighted samples and the Current Population Survey


