Abstract
Background and Hypothesis:
While individuals at clinical high-risk (CHR) for psychosis experience higher levels of discrimination than healthy controls, it is unclear how these experiences contribute to the etiology of attenuated positive symptoms. The present study examined the association of perceived discrimination with positive symptoms in a cohort from the North American Prodrome Longitudinal Study (NAPLS2). It predicted that CHR individuals will report higher levels of lifetime and past year perceived discrimination related to their race and ethnicity (ethnoracial discrimination) and that this form of discrimination will be significantly associated with baseline positive symptoms.
Study Design:
Participants included 686 CHR and 252 healthy controls. The present study examined data from the perceived discrimination (PD) scale, the Brief Core Schema Scale, and the Scale for the Psychosis-Risk Symptoms. Structural equation modeling was employed to examine whether negative schema of self and others mediated the relation of past year ethnoracial PD to baseline suspiciousness symptoms.
Results:
CHR individuals report higher levels of past year and lifetime PD compared to healthy controls. Lifetime ethnoracial PD was associated with suspiciousness and total positive symptoms. Negative schema of self and others scores partially mediated the relation of past year ethnoracial PD to suspiciousness, one of five positive symptom criteria for CHR.
Conclusions:
For CHR individuals, past year ethnoracial discrimination was associated with negative beliefs about themselves and others, which was associated with suspiciousness. These findings contribute to an emerging literature characterizing the mechanisms by which discrimination contributes to the positive symptoms characterizing the CHR syndrome.
Keywords: clinical high-risk, perceived discrimination, racism, suspiciousness, paranoia, psychosis
Introduction
Given the heterogeneity of clinical presentations and numerous risk factors, psychosis likely reflects a final common pathway, in which many different potential risk trajectories can lead to similar pathology (Uhlhaas et al., 2017). Conversion to psychosis likely involves the interaction of biologically-based diathesis with environmental and social stressors (Jones and Fernyhough, 2007). While psychosis assessment efforts have largely focused on the identification of biological risk factors (Cannon, 2020), there has been increasing interest in how social and environmental factors alter psychosis risk (Gur et al., 2019; van Os et al., 2010). Sophisticated meta-analytical work suggest that psychosis is associated with early life adversity (Rutten and Mill, 2009), growing up in an urbanized area (Kelly et al., 2010; Krabbendam, 2005; March et al., 2008), possibly cannabis use (Auther et al., 2015, 2012; van Winkel and Genetic Risk and Outcome of Psychosis (GROUP) Investigators, 2011), childhood trauma (Arseneault et al., 2011), and minority group position (Morgan et al., 2010).
Although initial evidence for minority group status as a psychosis risk factor consisted of studies based in Europe and the United Kingdom (Cooper et al., 2008; Karlsen et al., 2005; Veling, 2013; Veling et al., 2007), recent efforts have focused on the role of racial and ethnic (ethnoracial) minority status in the United States (U.S.) (Anglin et al., 2021), given the country’s long-standing history of structural racism and social inequality (Phelan et al., 2010). Racial categories are socially constructed rather than biologically-based (Bryant et al., 2022; Smedley and Smedley, 2005). Minority group status confers risk through impacting how one is perceived and treated by others in various social contexts (Clark et al., 1999; Harrell, 2000). It is not merely group membership itself which contributes to increased risk for psychosis in Black, Indigenous, and People of Color (BIPOC) individuals in the U.S., but rather the increased stressors associated with navigating social environments as an ethnoracial minority (Phelan and Link, 2015). This is evidenced by the fact that discrimination is specifically associated with psychosis symptoms in racial and ethnic minorities (Anglin et al., 2021). Discrimination has also been strongly associated with the development of depressive symptoms in ethnoracial minorities (Khan et al., 2017; Nadimpalli et al., 2015; Smith et al., 2006; Yelton et al., 2022).
There is evidence that discrimination is a risk factor for those at clinical high-risk (CHR) for psychosis. In CHR individuals, lifetime experiences of discrimination are associated with reduced cortical thickness across time (Collins et al., 2021), higher levels of negative schema of self and others (NSSO) scores (Saleem et al., 2014) and is a predictor of conversion to psychosis from the CHR state (Stowkowy et al., 2016). Despite emerging evidence for the role of discrimination in the etiology of psychosis, its relation to attenuated psychotic symptoms (APS) is less clear. APS represent the subclinical symptoms of psychosis which are used to identify adolescents and young adults at clinical high-risk (McGlashan et al., 2010). While some (Anglin et al., 2018, 2016, 2014; Stowkowy et al., 2016) report a strong association between discrimination and APS, these studies were conducted in non-clinical samples and assessed APS symptoms through administration of the Prodromal Questionnaire (PQ) (Loewy et al., 2005), a self-report measure, rather than using the Structured Clinical Interview for Psychosis-Risk Symptoms (SIPS)(Miller et al., 2003), one of the gold-standard clinical interviews for diagnosing the CHR syndrome. Although scores on the PQ are highly correlated with the SIPS (Loewy et al., 2011), the PQ’s specificity for diagnosing CHR symptoms is very low, unless the SIPS is used as the final diagnostic instrument (Kline et al., 2012). Furthermore, the validity of the PQ’s total distress scale scores have been called into question for use with BIPOC individuals (Cicero et al., 2019). The only study to date that has assessed the effects of discrimination on positive symptoms in a clinical CHR sample through the use of a structured clinical interview (Saleem et al., 2014) found no association between discrimination and APS, despite reporting that CHR individuals experiencing higher levels of discrimination compared to healthy controls. The lack of an association between discrimination and positive symptoms may have been due to that study being underpowered, as it only utilized a partial CHR sample (N=360) of the North American Prodromal Longitudinal Study 2 (NAPLS-2) cohort. Overall these mixed results require reconciliation in order to determine if discrimination is a major risk factor for APS. It is unlikely that discrimination is related to psychosis conversion but not positive symptoms, given that increased severity of positive symptoms are required to determine that an individual has converted to psychosis from the CHR state. CHR individuals are a heterogenous group, the majority of whom will not convert to psychosis. It is possible that the relation of discrimination to APS operates differently for those who convert to psychosis compared to those who do not.
One potential explanation for this discrepancy is that the relation of discrimination to APS is indirect; discrimination may exert its effects on positive symptoms through its relation to other risk factors. In a Dutch study, experiences of discrimination contributed to the development of a paranoid attributional style and thereby increase the likelihood of psychotic-like experiences (Janssen et al., 2003). Furthermore, it is more likely that specific forms of discrimination, such as ethnoracial discrimination, exert their effects of specific positive symptoms, such as suspiciousness, rather than simply increasing total positive symptoms. This is well-supported by several past studies in which CHR individuals endorsed negative beliefs about self and others at a higher rate than healthy controls (Saleem et al., 2014) and these beliefs have been associated with specific attenuated positive symptoms (Perivoliotis et al., 2009; Smith et al., 2006; Stowkowy and Addington, 2012). The development of negative schemas about oneself and others is a core feature of depressive symptomology, which has been associated with both positive symptoms (Berg et al., 2011; Smith et al., 2006) and discrimination in CHR individuals. CHR individuals endorse higher levels of co-morbid depression compared to healthy controls (Smith et al., 2006) and the comorbidity of depression in CHR individuals has been associated with increased risk of conversion (Schirmbeck et al., 2021). Therefore, it may be that negative beliefs about self and others partially mediates the relation of ethnoracial discrimination to suspiciousness symptoms.
The present study sought to utilize the full sample (N=938) from the North American Prodrome Longitudinal Study (NAPLS 2) study to 1) identify whether CHR individuals experienced higher levels of both past year and lifetime PD compared to healthy controls, 2) determine whether ethnoracial discrimination was associated with both positive symptoms and with negative beliefs about self and others, and lastly 3) test whether negative beliefs about self and others mediated the relation of past year ethnoracial discrimination to suspiciousness symptoms. Specifically, it is predicted that for CHR individuals, higher levels of past year perceived discrimination related to their race and ethnicity will be associated with endorsing negative schemas about self and others, which will be associated with suspiciousness symptoms at baseline. The present study sought only to investigate the relation of PD to APS and does not make any claims regarding the relation of PD to conversion or the contribution of PD to future psychosis.
Methods
Participants
The sample (N=938) for the present study consists of 686 CHR individuals and 252 healthy controls recruited for the multisite NAPLS2 study. Individuals were determined to be at clinical high risk based on the Criteria of Prodromal Syndromes (COPS) through administration of the Structured Clinical Interview for Psychosis-Risk Syndromes (SIPS) (McGlashan et al., 2010). Exclusion criteria for CHR participants included having an IQ of < 70, having a clinically significant neurological or central nervous system disorder, and being diagnosed with a psychotic disorder. Exclusion criteria for healthy controls included meeting COPS criteria or reported a first-degree relative with a psychotic disorder.
Measures
All of the measures included in this secondary analysis of data from the NAPLS 2 study were administered at the baseline visit. While some of the included measures were repeated at subsequent study visits, the present study only analyzed data from the baseline visit. Both healthy controls and CHR participants completed all of the measures.
The Structured Clinical Interview for Psychosis-Risk Symptoms (SIPS) and the Scale for Assessment of Psychosis-Risk Symptoms (SOPS) (McGlashan et al., 2010) were administered to assess the severity of attenuated positive symptoms and whether participants met criteria for one of the CHR syndromes.
Perceived discrimination was assessed using a self-report measure of experiencing of discrimination over the past year and over one’s entire lifetime (Janssen et al., 2003). For both timeframes, participants were required to answer whether or not (“yes” or “no”) they had experienced the following types of perceived discrimination: skin color, ethnicity, appearance, gender, sexual orientation, age, religion, disability, and other. Each type of discrimination endorsed was scored as a ‘1’. For each timeframe (lifetime or past year), the total number of types of discrimination endorsed were summed in order to derive the total perceived discrimination items. All participants completed this measure at the baseline visit and it was not repeated at subsequent timepoints. In order to address ethnoracial discrimination, the following three subtypes of past year discrimination were combined: skin color, ethnicity, and appearance. These types were chosen since each relate to the experience of being discriminated against due to one’s race or ethnicity, and the fact that physical attributes are central to the function of race as a social construct (Bryant et al., 2022). Further support for combining these items was evidenced by each being highly correlated with one another (p < .001). These three items were combined for each timeframe only after examining whether each item significantly differed between healthy controls and CHR. This new composite variable is referred to as “Ethnoracial PD” and is examined as a predictor in the mediation analysis.
The Brief Core Schema Scale (BCSS) (Fowler et al., 2006) was utilized to assess participant’s negative schema of self and others. The BCSS is a self-report measure consisting of 24 items assessed on a 5-point Likert-rating scale concerning beliefs about oneself and others. Respondents indicate the extent to which they agree with a series of positive and negative statements about themselves (e.g., “I am unloved”, “I am successful”) and about others (e.g., “Others are hostile”, “Others are supportive”). The measure was completed at the baseline visit and has been validated in CHR samples (Addington and Tran, 2009) and in previous NAPLS 2 studies (Saleem et al., 2014). The present study examined participant’s total score on the combined Negative Schema of Self and Negative Schema of Others subscale of the BCSS. Past studies examining the BCSS have utilized these combined subscales and have demonstrated that they are associated with the positive symptoms of the CHR syndrome (Devoe et al., 2022; Fowler et al., 2006; Smith et al., 2006). The “Other” subscale was specifically chosen for the mediation model since it has been previously associated with suspiciousness symptoms in CHR individuals (Addington and Tran, 2009).
Procedures
The Institutional Review Board for each of the eight NAPLS 2 sites approved the study. Informed consent was obtained for participants 18 and older and parental consent was obtained for participants who were under the age of 18. Experienced clinical researchers completed all of the assessments during the baseline visit of the study including semi-structured interviews. Interrater reliability for determining the CHR diagnosis was excellent (kappa= 0.90)(Addington et al., 2015, p. 2). Additional details regarding the NAPLS 2 procedures have been reported elsewhere (Addington et al., 2012).
Statistical Analysis
All statistical analyses were performed in RStudio (RStudio, 2020). T-test and Chi-Square analysis were used to examine demographic differences between CHR individuals and health controls at baseline. Chi-Square analysis was utilized to examine differences in self-reported PD between clinical high-risk individuals and healthy controls. Each of the positive symptoms of the SIPS, as well as the total positive symptoms and total negative symptoms were examined in relation to past year and lifetime perceived discrimination. Pearson correlations were employed to examine the relation of PD to APS and BCSS scores. Pearson correlations were utilized specifically because the data were normally distributed for all three measures. A mediation analysis was conducted in order to determine whether the negative schema of self and others score of the BCSS partially mediates the relation of past year ethnoracial PD to suspiciousness symptoms. Lifetime ethnoracial discrimination was not examined in the mediation model since the Chi-Square analysis indicated that lifetime ethnicity PD did not differ significantly between CHR and healthy controls while past year ethnicity PD did differ significantly between groups. The mediation analysis was primarily conducted through simple mediation separately for each step and then confirmed through the use of structured equation modelling (SEM) (Gunzler et al., 2013) using the mediation package in R. The SEM approach utilized bootstrapped procedures (1,000 simulations) and all regression coefficients were standardized in order to compare the effect size between variables of interest.
Results
Baseline Demographic Characteristics
CHR individuals (n=686) did not differ significantly from healthy controls (n=252) at baseline with respect to sex, race, or ethnicity (Table 1). Healthy controls were significantly older, on average, compared to CHR participants (t= −3.98, p < .0001), and healthy control participants reported significantly higher levels of both paternal (χ2= 22.81, p = .004) and maternal (χ2= 23.83, p = .003) education.
Table 1:
Differences in Demographic Characteristics Between Clinical High-Risk and Healthy Control Participants
| Clinical High-Risk (n=686) | Healthy Controls (n= 252) | Test Statistic2 (t or X2) | p Value 2 | |||
|---|---|---|---|---|---|---|
| Variable | Mean/N 1 | SD/% 1 | Mean/N 1 | SD/% 1 | ||
| Age (Years) | 18.53 | 4.29 | 19.87 | 4.67 | −3.98 | < .0001 |
| Sex | ||||||
| Male | 393 | 57.2% | 130 | 51.4% | 2.31 | .129 |
| Female | 294 | 42.7% | 123 | 48.6% | ||
| Race | ||||||
| First Nations | 12 | 1.7% | 3 | 1.2% | 9.66 | .482 |
| Asian | 48 | 7.0% | 27 | 10.7% | ||
| Black | 107 | 15.6% | 42 | 16.6% | ||
| Latin American | 28 | 4.1% | 10 | 4.0% | ||
| Middle Eastern | 6 | 0.9% | 2 | 0.8% | ||
| White | 400 | 58.2% | 143 | 56.5% | ||
| Multiracial | 84 | 12.2% | 25 | 9.9% | ||
| Ethnicity (Hispanic/Latinx) | ||||||
| Yes | 126 | 18.3% | 42 | 16.6% | 0.27 | .602 |
| No | 561 | 81.7% | 211 | 83.4% | ||
| Paternal Education Level | ||||||
| Primary School | 64 | 9.3% | 11 | 4.3% | 22.81 | .004 |
| Some High School | 65 | 9.5% | 12 | 4.7% | ||
| HS or Some College | 254 | 37.0% | 104 | 41.1% | ||
| College Graduate | 304 | 44.3% | 126 | 49.8% | ||
| Maternal Education Level | ||||||
| Primary School | 37 | 5.4% | 4 | 1.6% | 23.83 | .003 |
| Some High School | 54 | 7.9% | 7 | 2.8% | ||
| HS or Some College | 259 | 37.7% | 90 | 35.6% | ||
| College Graduate | 337 | 49.1% | 152 | 60.1% | ||
Reflects mean and standard deviation for continuous variables and count (n) and percentage (%) for categorical variables
Reflects test statistic and resulting p value of either a t-test for continuous variables or chi-square test for categorical variables
Perceived Discrimination
CHR individuals report significantly higher levels of past year PD compared to healthy controls (Table 2). A greater number of CHR individuals discrimination in the past year for every subtype of discrimination compared to healthy controls. Total past year PD was also significantly higher in the CHR group.
Table 2.
Group Differences in Frequency of Perceived Discrimination
| Past Year Perceived Discrimination | Lifetime Perceived Discrimination | |||||||
|---|---|---|---|---|---|---|---|---|
| Discrimination Type | Clinical High Risk (n=686) n (%) | Healthy Control (n=252) n (%) | Test Statistic X2/t | p Value | Clinical High Risk (n=686) n (%) | Healthy Control (n=252) n (%) | Test Statistic X2/t | p Value |
| Skin Color | 152 (22.2%) | 29 (11.5%) | 12.75 | *** | 263 (38.3%) | 74 (29.4%) | 6.32 | * |
| Ethnicity | 147 (21.4%) | 32 (12.7%) | 8.62 | ** | 236 (34.4%) | 75 (29.8%) | 1.59 | n.s. |
| Gender | 155 (22.6%) | 29 (11.5%) | 13.67 | *** | 231 (33.7%) | 69 (27.4%) | 3.24 | n.s. |
| Age | 197 (28.7%) | 50 (19.8%) | 7.19 | ** | 306 (44.6%) | 83 (32.9%) | 9.97 | ** |
| Appearance | 299 (43.6%) | 44 (17.5%) | 53.11 | *** | 407 (59.3%) | 83 (32.9%) | 51.05 | *** |
| Disability | 76 (11.1%) | 1 (0.4%) | 26.62 | *** | 101 (14.7%) | 3 (1.2%) | 32.94 | *** |
| Sexual Orientation | 62 (9.0%) | 9 (3.6%) | 7.18 | ** | 97 (14.1%) | 9 (3.6%) | 19.55 | *** |
| Religion | 109 (15.9%) | 16 (6.3%) | 13.49 | *** | 175 (25.5%) | 37 (14.7%) | 11.81 | *** |
| Other | 78 (11.4%) | 7 (2.8%) | 15.63 | *** | 93 (13.6%) | 9 (3.6%) | 18.04 | *** |
| Total (Mean/SD): | 1.86 (1.93) | 0.86 (1.33) | 9.93 | *** | 2.72 (2.25) | 1.73 (1.76) | 7.41 | **** |
n.s.= not statistically significant;
p < .05,
p < .01,
p< .001;
SD=standard deviation
CHR individuals reported significantly higher frequency of lifetime PD across a number of subtypes including skin color, age, appearance, disability, sexual orientation, religion, and other. However there were no between-group differences in lifetime PD for ethnicity or gender. Overall, CHR individuals reported significantly higher total lifetime PD compared to healthy controls (Table 2).
Past year PD was significantly associated with baseline paranoia/suspiciousness (P2) (r = 0.16, p < .001), perceptual aberrations (P4) (r = 0.09, p < .05), and disordered communication (P5) (r = 0.15, p < .001), but was not associated with unusual thoughts (P1) (r = 0.07, p = .052), grandiose ideas (P3) (r = 0.03, p = .489), or total negative symptoms (r = 0.04, p = .345) (Table 3). Lifetime PD was significantly associated with each of five positive symptoms (Table 2), however it was not associated with total negative symptoms at baseline (r = 0.05, p = .204). Total APS were significantly associated with both past year (r = 0.15, p < .001) and lifetime PD (r = 0.19, p < .001).
Table 3:
Perceived Discrimination and CHR Symptoms
| Clinical High Risk Sample (n=686) | ||||
|---|---|---|---|---|
| Past Year PD | Lifetime PD | |||
| Baseline Variable | Coefficient | p Value | Coefficient | p Value |
| P1 Unusual Thoughts | 0.07 | n.s. | 0.08 | * |
| P2 Suspiciousness | 0.16 | *** | 0.16 | *** |
| P3 Grandiose Ideas | 0.03 | n.s. | 0.08 | * |
| P4 Perceptual Abnormalities | 0.09 | * | 0.08 | * |
| P5 Disorganized Communication | 0.11 | ** | 0.15 | *** |
| Total Positive Symptoms | 0.15 | *** | 0.19 | *** |
| Total Negative Symptoms | 0.04 | n.s. | 0.05 | n.s. |
n.s.= not statistically significant;
p < .05,
p < .01,
p< .001
Mediation Analysis
We conducted a simple mediation analysis on baseline data from the NAPLS-2 data set (n= 680) to better understand the effects of ethnoracial discrimination on APS. We specifically examined how suspiciousness symptoms were impacted by past year ethnoracial PD via the hypothesized mediator of BCSS negative schema of self and others scores (Figure 1). The predictor, past year ethnoracial PD, was derived by combining the skin color, ethnicity, and appearance items from the Perceived Discrimination Scale for the past year timeframe. Univariate analysis indicated that past year ethnoracial PD was significantly associated with baseline suspiciousness (P2) (r = 0.16). Past year ethnoracial PD was also significantly associated with BCSS negative schema of self and others score at baseline (r = 0.27). Both the predictor and mediator were assessed through self-report measures while the outcome variable was assessed via clinical interview. The mediation was analyzed within a path analysis framework through use of the structural equation modeling (SEM) package ‘mediation’ in RStudio. Mediation effects were estimated through the product of coefficients approach (Fairchild and McDaniel, 2017). Full-information maximum likelihood was used to handle missing data. Indirect effects were computed using bootstrapping procedures (sample= 1,000), and the 95% confidence interval was computed by determining the indirect effects at the 2.5th and 97.5th percentile.
Figure 1.
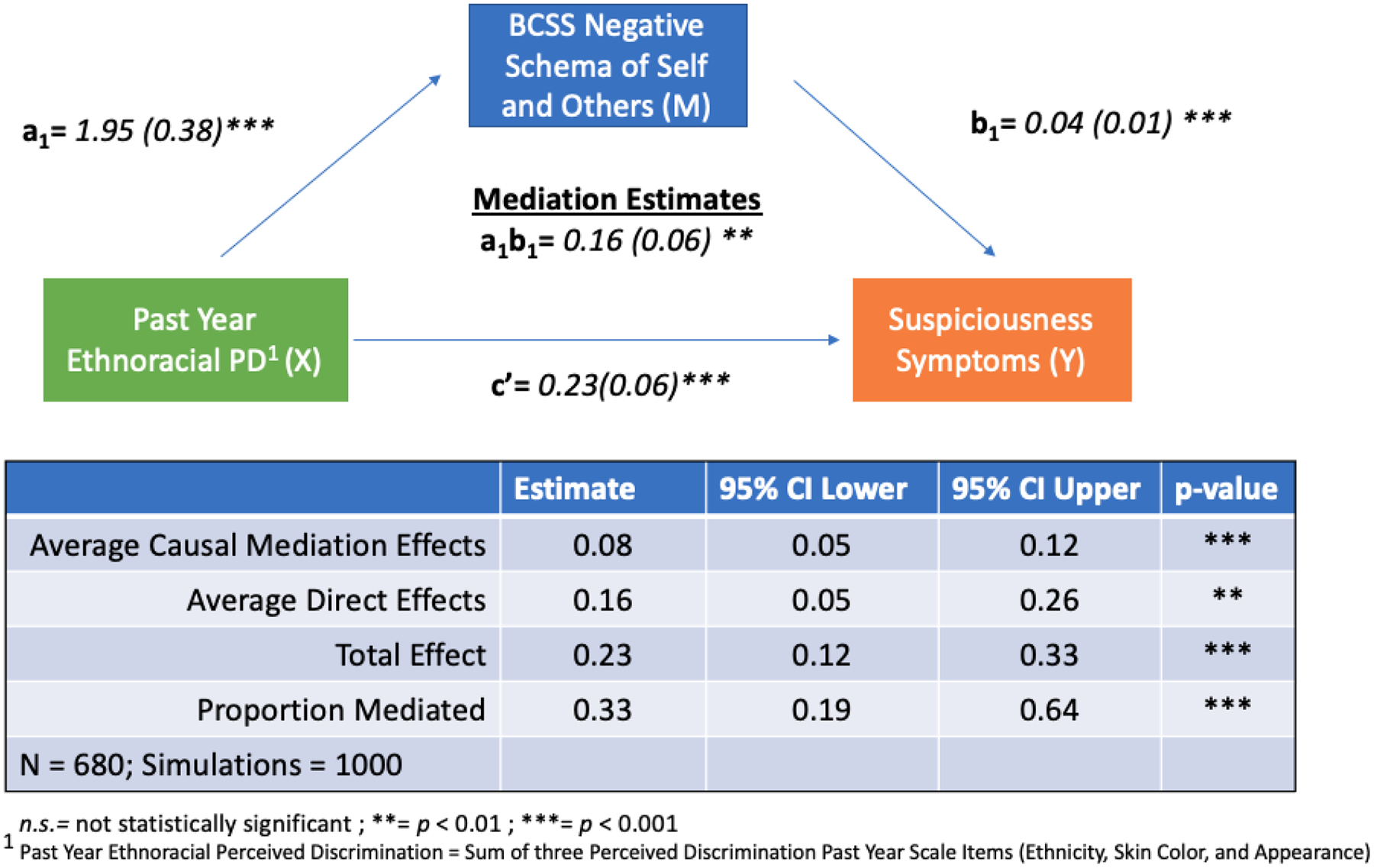
BCSS Negative Schema of Self and Others scores partially mediates the relation of past year ethnoracial discrimination and baseline suspiciousness symptoms.
Unstandardized parameter estimates for the model are shown in Figure 1 with all associated standard error (SE) estimates following in parentheses. Regressing BCSS negative schema of self and others on past year ethnoracial PD demonstrated that perceiving ethnoracial discrimination in the past year significantly increased negative beliefs about oneself and others [a1=1.95 (0.38); p < 0.001; 95%CI: 1.21, 2.68]. Regressing suspiciousness symptoms (P2) onto BCSS Negative Schema of Self and Others demonstrated that having negative beliefs about yourself and others increased suspiciousness symptoms [b1=0.04 (0.01); p < 0.001; 95% CI: 0.03, 0.05] and there was a significant direct effect of past year ethnoracial PD on suspiciousness symptoms [c’= 0.23 (0.06); p < 0.001; 95% CI: 0.12, 0.34].
Mediation analysis demonstrated that baseline BCSS negative schema of self and others score partially mediated the relation of past year ethnoracial PD to baseline suspiciousness symptoms (Figure 1) [a1b1= 0.16 (0.06); p < 0.01; 95% CI: 0.05, 0.26]. Overall, 9.16% of the variance in suspiciousness symptoms was explained by variables in the model. Proportion-mediated effect size estimates for the mediation were 33.10%. The proportion mediated is comparable to the effect size estimates of other studies that have used BCSS negative schema of self and others as a mediator (Stowkowy and Addington, 2012). The significant direct effect of past year ethnoracial PD on suspiciousness symptoms after the mediation was modeled and the small amount of variance explained by the model indicate that other mediators not examined in the present study might also contribute to better understanding the relation of PD to suspiciousness symptoms.
Discussion
The present results provides cross-sectional evidence that ethnoracial PD may relate to the etiology of suspiciousness symptoms in CHR individuals through its effects on the development of negative schemas of self and others. The BCSS negative beliefs about self and others score partially mediated the relation of past year ethnoracial PD to suspiciousness symptoms, suggesting that experiences of racial discrimination contribute to negative core beliefs about oneself and others, which, in turn, is associated with suspiciousness. These findings provide a more robust characterization of how experiences of discrimination due to one’s ethnicity or race confer increased risk for the development of suspiciousness positive symptoms. It also extends previous findings associating experiences of ethnoracial discrimination with the positive symptoms that characterize the CHR syndrome (Cooper et al., 2008; Pignon et al., 2021; Saleem et al., 2014; Stowkowy et al., 2016). Given that the mediation was only partial, it is likely that additional factors contribute to the complex relation between discrimination and APS. The risk factors for psychosis are numerous and complex and therefore it is unlikely that any single variable could explain all of the variance associated between risk factors and symptoms.
CHR individuals endorsed experiences of discrimination at a significantly higher rate than healthy controls. These findings are consistent with previous studies (Saleem et al., 2014) that examine past year PD and with previous studies (Karlsen et al., 2005; Pignon et al., 2021) that report higher levels of PD in CHR individuals who identify as ethnic/racial minorities. The present study extended these previous findings by also demonstrating that CHR individuals experience greater lifetime PD compared to healthy controls. Notably, there were no significant difference in lifetime perceived discrimination related to ethnicity and gender, although a larger proportion of the CHR sample endorsed these experiences compared to the healthy control sample. This may be due to the fact that these forms of discrimination are among the most commonly reported and often begin at very young ages (Harrell, 2000; Lee et al., 2019). It is therefore more likely to be prevalent in both clinical and non-clinical samples alike. Even though the prevalence may be similar, it is possible that these negative experiences have a disproportionate impact on CHR individuals and their mental health.
Perceived discrimination was significantly associated with total baseline attenuated positive symptoms as well as specific positive symptoms including suspiciousness. These results are consistent with previous studies that have utilized the full NAPLS 2 sample (Stowkowy et al., 2016), while studies that relied on a partial NAPLS 2 sample (Saleem et al., 2014) report no such association. The present results suggest that the discrepancy between past studies is likely a result of the differences in sample size. This is further evidenced by the fact that PD was also significantly associated with negative schema of self and others, which was not reported in a past study utilizing the smaller sample (Saleem et al., 2014). Given past findings of negative schema scores being significantly associated with depressive symptoms(Addington and Tran, 2009; Smith et al., 2006), future studies should investigate whether negative schema of self and others may also mediate the relation of PD to depression symptoms in CHR individuals.
Suspiciousness is not necessarily pathological in CHR individuals who have been the victim of ethnoracial discrimination. In response to discrimination, many individuals develop healthy suspiciousness which is considered a normative reaction of guardedness and mistrust (Fernando, 2004). Previous studies have report that Black individuals endorse higher levels of subclinical paranoia compared to White control groups, and that perceived racism predicts cultural mistrust and nonclinical paranoia in Black people (Combs et al., 2006, 2002). These reactions are an adaptive, natural response to adversity that also serve to protect against future experiences of discrimination. Healthy suspiciousness has also been described in the literature as responsive paranoia (Williams et al., 2003) or healthy cultural mistrust (Whaley, 2001). This phenomenon may explain racial differences in the experience of attenuated symptoms; in a small sample of CHR subjects, suspiciousness symptoms were associated with functional impairments in White individuals but not in Black individuals, suggesting that these beliefs operate differently for those of different backgrounds (Rakhshan Rouhakhtar et al., 2021). It also raises concerns over the validity of clinical interview measures such as the SIPS which may not attend to the nuances of these experiences and how they differ between White and BIPOC individuals. Healthy suspiciousness may be misunderstood by CHR researchers as pathological. CHR researchers should apply a multicultural and anti-racist lens to the assessment of attenuated psychotic symptoms, which includes understanding differences in the lived experiences of BIPOC rather than potentially misdiagnosing normative experiences as psychopathology. Future CHR studies may benefit from including measures of non-clinical paranoia to better capture this phenomenon.
The present study has several limitations. The cross-sectional nature of the NAPLS2 data limits our ability to infer any causality from the present results. While these results suggest an association between ethnoracial discrimination and suspiciousness symptoms, such findings must be interpreted cautiously due to their correlational nature. Ethnoracial discrimination may be one environmental stressor among many others which is associated with the development or worsening of suspiciousness symptoms. Given that participants reported on perceived discrimination, it is possible that the CHR symptoms themselves, including suspiciousness, increased reporting of PD. The current data does not permit being able to empirically test this alternative hypothesis since the discrimination experiences occurred in the past year and the positive symptoms were rated for the past month prior to the baseline visit. PD was also only collected at the baseline visit; future studies should collect these data longitudinally which would allow the ability to test whether positive symptoms or worsening of positive symptoms leads to increased reporting of perceived discrimination in CHR individuals. Past studies measuring actual ethnoracial discrimination consistently report higher levels in BIPOC CHR individuals (Anglin et al., 2018, 2016, 2014; Anglin and Lui, 2021), suggesting that the present findings reflect some level of genuine increased risk. The cross-sectional nature of the data also limits the ability to understand the temporal sequence of events; it is unclear whether participants were already experiencing attenuated symptoms when discrimination occurred in the past year. However, given that the SIPS score reflects symptom levels in the past month, it is more likely that the discrimination occurred prior to the current level of suspiciousness symptoms. The measure of discrimination was brief and did not collect information regarding the frequency or severity of these experiences. It also did not inquire as to the effects of experiencing discrimination on participants’ mental health. Future CHR studies should consider utilizing better established measures of perceived discrimination given the limitations of the measure administered in the NAPLS-2 study. There is also the possibility of recall bias as the measure is entirely based on self-report. The study also did not include other measures, such as race-based rejection sensitivity, that have been previously reported (Anglin et al., 2016) to partially account for the association of ethnoracial discrimination with attenuated positive symptoms.
While the association between discrimination and APS in CHR individuals is well-established (Anglin et al., 2018, 2016, 2014; Saleem et al., 2014; Stowkowy et al., 2016), to our knowledge this is one of the first studies to demonstrate an association of ethnoracial discrimination with CHR symptoms of suspiciousness. In CHR individuals, past year experiences of discrimination related to their ethnicity, skin color, and appearance contributed to the development of a negative schema of self and others, which in turn was associated with baseline suspiciousness symptoms. These results have several clinical implications for CHR treatment, including the potential for psychotherapeutic interventions including Cognitive Behavioral Therapy for psychosis (CBT-P) (Tarrier et al., 2004) to challenge CHR individuals’ negative beliefs. Interventions should also be developed to address the clinical impact of experiencing ethnoracial discrimination in BIPOC CHR individuals. Future longitudinal, prospective research could better explore the role of discrimination in the development or worsening of attenuated positive symptoms and the development of psychosis, and address important questions related to causality which were outside the scope of the present study. Given the growing body of research consistently reporting an association between racial discrimination and attenuated positive symptoms, future studies should collect additional detail regarding experiences of ethnoracial discrimination including the frequency, severity, and clinical impact on BIPOC individuals at clinical high-risk for psychosis.
Acknowledgements:
The authors would like to acknowledge Dr. Majnu John for his help and advice in reviewing the manuscript. The authors would like to acknowledge the NAPLS-2 group: J Stowkowy, T Raedler, L McGregor, D Marulanda, L Legere, L Liu, C Marshall, E Falukozi, E Fitton, K Smith (University of Calgary).T Alderman, K Shafer, I Domingues, A Hurria, H Mirzakhanian (UCSD). B Walsh, J Saksa, N Santamauro, A Carlson, J Kenney, B Roman (Yale University). K Woodberry, AJ Giuliano, W Stone, JM Rodenhiser, L Tucker, R Serur, G Min, R Szent-Imrey (Beth Israel Deaconess Medical Center/Harvard). C Bearden, P Bachman, J Zinberg, S DeSilva, A Andaya, S Uguryan (UCLA). J Brasfield, H Trotman, (Emory University). A Pelletier, K Lansing, H Mates, J Nieri, B Landaas, K Graham, E Rothman, J Hurta, Y Sierra (University of North Carolina). A Auther, R Carrion, M McLaughlin, R Olsen (Zucker Hillside Hospital).
Role of Funding Source
This study was supported by the National Institute of Mental Health (grant U01MH081984 to Dr Addington; grants U01 MH081928; P50 MH080272; Commonwealth of Massachusetts SCDMH82101008006; to Dr Seidman; grants R01 MH60720, U01MH082022; and K24 MH76191 to Dr Cadenhead; grant to Dr. Cannon; grant U01MH082004-01A1 to Dr. Perkins; grant U01MH081988 to Dr Walker; grant U01MH082022 to Dr Woods; and UO1MH081857 grant to Dr Cornblatt.
None of the funding sources had any role in the analysis, data interpretation, or writing of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
ConflictsofInterest
The authors do not have any conflicts of interest to report.
References:
- Addington J, Cadenhead KS, Cornblatt BA, Mathalon DH, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Addington JA, Cannon TD, 2012. North American Prodrome Longitudinal Study (NAPLS 2): Overview and recruitment. Schizophr. Res 142, 77–82. 10.1016/j.schres.2012.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Liu L, Buchy L, Cadenhead KS, Cannon TD, Cornblatt BA, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Bearden CE, Mathalon DH, McGlashan TH, 2015. North American Prodrome Longitudinal Study (NAPLS 2): The Prodromal Symptoms. J. Nerv. Ment. Dis 203, 328–335. 10.1097/NMD.0000000000000290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Tran L, 2009. Using the Brief Core Schema Scales with Individuals at Clinical High Risk of Psychosis. Behav. Cogn. Psychother 37, 227–231. 10.1017/S1352465809005116 [DOI] [PubMed] [Google Scholar]
- Anglin DM, Ereshefsky S, Klaunig MJ, Bridgwater MA, Niendam TA, Ellman LM, DeVylder J, Thayer G, Bolden K, Musket CW, Grattan RE, Lincoln SH, Schiffman J, Lipner E, Bachman P, Corcoran CM, Mota NB, van der Ven E, 2021. From Womb to Neighborhood: A Racial Analysis of Social Determinants of Psychosis in the United States. Am. J. Psychiatry 178, 599–610. 10.1176/appi.ajp.2020.20071091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglin DM, Greenspoon M, Lighty Q, Ellman LM, 2016. Race-based rejection sensitivity partially accounts for the relationship between racial discrimination and distressing attenuated positive psychotic symptoms: Race-based rejection sensitivity. Early Interv. Psychiatry 10, 411–418. 10.1111/eip.12184 [DOI] [PubMed] [Google Scholar]
- Anglin DM, Lighty Q, Greenspoon M, Ellman LM, 2014. Racial discrimination is associated with distressing subthreshold positive psychotic symptoms among US urban ethnic minority young adults. Soc. Psychiatry Psychiatr. Epidemiol 49, 1545–1555. 10.1007/s00127-014-0870-8 [DOI] [PubMed] [Google Scholar]
- Anglin DM, Lui F, 2021. Racial microaggressions and major discriminatory events explain ethnoracial differences in psychotic experiences. Schizophr. Res [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglin DM, Lui F, Espinosa A, Tikhonov A, Ellman L, 2018. Ethnic identity, racial discrimination and attenuated psychotic symptoms in an urban population of emerging adults: Ethnic identity and APPS. Early Interv. Psychiatry 12, 380–390. 10.1111/eip.12314 [DOI] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A, 2011. Childhood Trauma and Children’s Emerging Psychotic Symptoms: A Genetically Sensitive Longitudinal Cohort Study. Am. J. Psychiatry 168, 65–72. 10.1176/appi.ajp.2010.10040567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auther AM, Cadenhead KS, Carrión RE, Addington J, Bearden CE, Cannon TD, McGlashan TH, Perkins DO, Seidman L, Tsuang M, Walker EF, Woods SW, Cornblatt BA, 2015. Alcohol confounds relationship between cannabis misuse and psychosis conversion in a high-risk sample. Acta Psychiatr. Scand 132, 60–68. 10.1111/acps.12382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auther AM, McLaughlin D, Carrión RE, Nagachandran P, Correll CU, Cornblatt BA, 2012. Prospective study of cannabis use in adolescents at clinical high risk for psychosis: impact on conversion to psychosis and functional outcome. Psychol. Med 42, 2485–2497. 10.1017/S0033291712000803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg AO, Melle I, Rossberg JI, Romm KL, Larsson S, Lagerberg TV, Andreassen OA, Hauff E, 2011. Perceived discrimination is associated with severity of positive and depression/anxiety symptoms in immigrants with psychosis: a cross-sectional study. BMC Psychiatry 11, 77. 10.1186/1471-244X-11-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant BE, Jordan A, Clark US, 2022. Race as a Social Construct in Psychiatry Research and Practice. JAMA Psychiatry 79, 93–94. 10.1001/jamapsychiatry.2021.2877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon TD, 2020. The Current State of the Clinical High Risk for Psychosis Research Paradigm. Biol. Psychiatry 88, 284–286. 10.1016/j.biopsych.2020.06.008 [DOI] [PubMed] [Google Scholar]
- Cicero DC, Krieg A, Martin EA, 2019. Measurement Invariance of the Prodromal Questionnaire–Brief Among White, Asian, Hispanic, and Multiracial Populations. Assessment 26, 294–304. 10.1177/1073191116687391 [DOI] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR, 1999. Racism as a Stressor for African Americans. Am. Psychol 12. [DOI] [PubMed] [Google Scholar]
- Collins MA, Chung Y, Addington J, Bearden CE, Cadenhead KS, Cornblatt BA, Mathalon DH, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Cannon TD, 2021. Discriminatory experiences predict neuroanatomical changes and anxiety among healthy individuals and those at clinical high risk for psychosis. NeuroImage Clin. 31, 102757. 10.1016/j.nicl.2021.102757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combs DR, Penn DL, Cassisi J, Michael C, Wood T, Wanner J, Adams S, 2006. Perceived Racism as a Predictor of Paranoia Among African Americans. J. Black Psychol 32, 87–104. 10.1177/0095798405283175 [DOI] [Google Scholar]
- Combs DR, Penn DL, Fenigstein A, 2002. Ethnic differences in subclinical paranoia: An expansion of norms of the Paranoia Scale. Cultur. Divers. Ethnic Minor. Psychol 8, 248–256. 10.1037/1099-9809.8.3.248 [DOI] [PubMed] [Google Scholar]
- Cooper C, Morgan C, Byrne M, Dazzan P, Morgan K, Hutchinson G, Doody GA, Harrison G, Leff J, Jones P, Ismail K, Murray R, Bebbington P, Fearon P, 2008. Perceptions of disadvantage, ethnicity and psychosis. Br. J. Psychiatry 192, 185–190. 10.1192/bjp.bp.107.042291 [DOI] [PubMed] [Google Scholar]
- Devoe DJ, Cadenhead KS, Cornblatt B, Granholm E, Addington J, 2022. Negative symptoms: associations with defeatist beliefs, self-efficacy, and maladaptive schemas in youth and young adults at-risk for psychosis. Behav. Cogn. Psychother 50, 298–311. 10.1017/S1352465821000461 [DOI] [PubMed] [Google Scholar]
- Fairchild AJ, McDaniel HL, 2017. Best (but oft-forgotten) practices: mediation analysis. Am. J. Clin. Nutr ajcn152546. 10.3945/ajcn.117.152546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernando S, 2004. Cultural Diversity, Mental Health and Psychiatry, 0 ed. Routledge. 10.4324/9780203420348 [DOI] [Google Scholar]
- FOWLER D, FREEMAN D, SMITH B, KUIPERS E, BEBBINGTON P, BASHFORTH H, COKER S, HODGEKINS J, GRACIE A, DUNN G, GARETY P, 2006. The Brief Core Schema Scales (BCSS): psychometric properties and associations with paranoia and grandiosity in non-clinical and psychosis samples. Psychol. Med 36, 749–759. 10.1017/S0033291706007355 [DOI] [PubMed] [Google Scholar]
- Gunzler D, Chen T, Wu P, Zhang H, 2013. Introduction to mediation analysis with structural equation modeling 25, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gur RE, Moore TM, Rosen AFG, Barzilay R, Roalf DR, Calkins ME, Ruparel K, Scott JC, Almasy L, Satterthwaite TD, Shinohara RT, Gur RC, 2019. Burden of Environmental Adversity Associated With Psychopathology, Maturation, and Brain Behavior Parameters in Youths. JAMA Psychiatry 76, 966. 10.1001/jamapsychiatry.2019.0943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell SP, 2000. A Mu1tidimensional Conceptualization of Racism-Related Stress: Implicationsfor the Well-Being of People of Color 16. [DOI] [PubMed] [Google Scholar]
- Janssen I, Hanssen M, Bak M, Bijl RV, De Graaf R, Vollebergh W, McKenzie K, Van Os J, 2003. Discrimination and delusional ideation. Br. J. Psychiatry 182, 71–76. 10.1192/bjp.182.1.71 [DOI] [PubMed] [Google Scholar]
- Jones SR, Fernyhough C, 2007. A New Look at the Neural Diathesis Stress Model of Schizophrenia: The Primacy of Social-Evaluative and Uncontrollable Situations. Schizophr. Bull 33, 1171–1177. 10.1093/schbul/sbl058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsen S, Nazroo JY, McKENZIE K, Bhui K, Weich S, 2005. Racism, psychosis and common mental disorder among ethnic minority groups in England. Psychol. Med 35, 1795–1803. 10.1017/S0033291705005830 [DOI] [PubMed] [Google Scholar]
- Kelly BD, O’Callaghan E, Waddington JL, Feeney L, Browne S, Scully PJ, Clarke M, Quinn JF, McTigue O, Morgan MG, Kinsella A, Larkin C, 2010. Schizophrenia and the city: A review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophr. Res 116, 75–89. 10.1016/j.schres.2009.10.015 [DOI] [PubMed] [Google Scholar]
- Khan M, Ilcisin M, Saxton K, 2017. Multifactorial discrimination as a fundamental cause of mental health inequities. Int. J. Equity Health 16, 43. 10.1186/s12939-017-0532-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline E, Wilson C, Ereshefsky S, Tsuji T, Schiffman J, Pitts S, Reeves G, 2012. Convergent and discriminant validity of attenuated psychosis screening tools. Schizophr. Res 134, 49–53. 10.1016/j.schres.2011.10.001 [DOI] [PubMed] [Google Scholar]
- Krabbendam L, 2005. Schizophrenia and Urbanicity: A Major Environmental Influence--Conditional on Genetic Risk. Schizophr. Bull 31, 795–799. 10.1093/schbul/sbi060 [DOI] [PubMed] [Google Scholar]
- Lee RT, Perez AD, Boykin CM, Mendoza-Denton R, 2019. On the prevalence of racial discrimination in the United States. PLOS ONE 14, e0210698. 10.1371/journal.pone.0210698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewy RL, Bearden CE, Johnson JK, Raine A, Cannon TD, 2005. The prodromal questionnaire (PQ): Preliminary validation of a self-report screening measure for prodromal and psychotic syndromes. Schizophr. Res 79, 117–125. 10.1016/j.schres.2005.03.007 [DOI] [PubMed] [Google Scholar]
- Loewy RL, Pearson R, Vinogradov S, Bearden CE, Cannon TD, 2011. Psychosis risk screening with the Prodromal Questionnaire — Brief Version (PQ-B). Schizophr. Res 129, 42–46. 10.1016/j.schres.2011.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- March D, Hatch SL, Morgan C, Kirkbride JB, Bresnahan M, Fearon P, Susser E, 2008. Psychosis and Place. Epidemiol. Rev 30, 84–100. 10.1093/epirev/mxn006 [DOI] [PubMed] [Google Scholar]
- McGlashan TH, Walsh B, Woods SW, 2010. The Psychosis-Risk Syndrome: Handbook for Diagnosis and Follow-Up. Oxford University Press. [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, Perkins DO, Pearlson GD, Woods SW, 2003. Prodromal Assessment With the Structured Interview for Prodromal Syndromes and the Scale of Prodromal Symptoms: Predictive Validity, Interrater Reliability, and Training to Reliability. Schizophr. Bull 29, 703–715. 10.1093/oxfordjournals.schbul.a007040 [DOI] [PubMed] [Google Scholar]
- Morgan C, Charalambides M, Hutchinson G, Murray RM, 2010. Migration, Ethnicity, and Psychosis: Toward a Sociodevelopmental Model. Schizophr. Bull 36, 655–664. 10.1093/schbul/sbq051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadimpalli SB, James BD, Yu L, Cothran F, Barnes LL, 2015. The Association Between Discrimination and Depressive Symptoms among Older African Americans: The Role of Psychological and Social Factors. Exp. Aging Res 41, 1–24. 10.1080/0361073X.2015.978201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perivoliotis D, Morrison AP, Grant PM, French P, Beck AT, 2009. Negative Performance Beliefs and Negative Symptoms in Individuals at Ultra-High Risk of Psychosis: A Preliminary Study. Psychopathology 42, 375–379. 10.1159/000236909 [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, 2015. Is Racism a Fundamental Cause of Inequalities in Health? Annu. Rev. Sociol 41, 311–330. 10.1146/annurev-soc-073014-112305 [DOI] [Google Scholar]
- Phelan JC, Link BG, Tehranifar P, 2010. Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. J. Health Soc. Behav 51, S28–S40. 10.1177/0022146510383498 [DOI] [PubMed] [Google Scholar]
- Pignon B, Lajnef M, Kirkbride JB, Peyre H, Ferchiou A, Richard J-R, Baudin G, Tosato S, Jongsma H, de Haan L, Tarricone I, Bernardo M, Velthorst E, Braca M, Arango C, Arrojo M, Bobes J, Del-Ben CM, Di Forti M, Gayer-Anderson C, Jones PB, La Cascia C, Lasalvia A, Menezes PR, Quattrone D, Sanjuán J, Selten J-P, Tortelli A, Llorca P-M, van Os J, Rutten BPF, Murray RM, Morgan C, Leboyer M, Szöke A, Schürhoff F, 2021. The Independent Effects of Psychosocial Stressors on Subclinical Psychosis: Findings From the Multinational EU-GEI Study. Schizophr. Bull 47, 1674–1684. 10.1093/schbul/sbab060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakhshan Rouhakhtar P, Roemer C, Reeves G, Schiffman J, 2021. The associations between attenuated psychosis symptoms and functioning in Black and White youth at clinical high-risk for psychosis. Schizophr. Res 10.1016/j.schres.2021.11.032 [DOI] [PubMed] [Google Scholar]
- RStudio, T., 2020. RStudio: Integrated Development for R.
- Rutten BPF, Mill J, 2009. Epigenetic Mediation of Environmental Influences in Major Psychotic Disorders. Schizophr. Bull 35, 1045–1056. 10.1093/schbul/sbp104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleem MM, Stowkowy J, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Addington J, 2014. Perceived discrimination in those at clinical high risk for psychosis: Perceived discrimination in clinical high risk. Early Interv. Psychiatry 8, 77–81. 10.1111/eip.12058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schirmbeck F, van der Burg NC, Blankers M, Vermeulen JM, McGuire P, Valmaggia LR, Kempton MJ, van der Gaag M, Riecher-Rössler A, Bressan RA, Barrantes-Vidal N, Nelson B, Amminger GP, McGorry P, Pantelis C, Krebs M-O, Ruhrmann S, Sachs G, Rutten BPF, van Os J, Nordentoft M, Glenthøj B, Fusar-Poli P, de Haan L, 2021. Impact of Comorbid Affective Disorders on Longitudinal Clinical Outcomes in Individuals at Ultra-high Risk for Psychosis. Schizophr. Bull 48, 100–110. 10.1093/schbul/sbab088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley A, Smedley BD, 2005. Race as biology is fiction, racism as a social problem is real: Anthropological and historical perspectives on the social construction of race. Am. Psychol 60, 16–26. 10.1037/0003-066X.60.1.16 [DOI] [PubMed] [Google Scholar]
- Smith B, Fowler DG, Freeman D, Bebbington P, Bashforth H, Garety P, Dunn G, Kuipers E, 2006. Emotion and psychosis: Links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. Schizophr. Res 86, 181–188. 10.1016/j.schres.2006.06.018 [DOI] [PubMed] [Google Scholar]
- Stowkowy J, Addington J, 2012. Maladaptive schemas as a mediator between social defeat and positive symptoms in young people at clinical high risk for psychosis: Maladaptive Schemas in youth at high risk for psychosis. Early Interv. Psychiatry 6, 87–90. 10.1111/j.1751-7893.2011.00297.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stowkowy J, Liu L, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Bearden CE, Mathalon DH, Addington J, 2016. Early traumatic experiences, perceived discrimination and conversion to psychosis in those at clinical high risk for psychosis. Soc. Psychiatry Psychiatr. Epidemiol 51, 497–503. 10.1007/s00127-016-1182-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarrier N, Lewis S, Haddock G, Bentall R, Drake R, Kinderman P, Kingdon D, Siddle R, Everitt J, Leadley K, Benn A, Grazebrook K, Haley C, Akhtar S, Avies L, Palmer S, Dunn G, 2004. Cognitive–behavioural therapy in first-episode and early schizophrenia: 18-month follow-up of a randomised controlled trial. Br. J. Psychiatry 184, 231–239. 10.1192/bjp.184.3.231 [DOI] [PubMed] [Google Scholar]
- Uhlhaas PJ, Gajwani R, Gross J, Gumley AI, Lawrie SM, Schwannauer M, 2017. The Youth Mental Health Risk and Resilience Study (YouR-Study). BMC Psychiatry 17, 43. 10.1186/s12888-017-1206-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J, Kenis G, Rutten BPF, 2010. The environment and schizophrenia. Nature 468, 203–212. 10.1038/nature09563 [DOI] [PubMed] [Google Scholar]
- van Winkel R, Genetic Risk and Outcome of Psychosis (GROUP) Investigators, 2011. Family-Based Analysis of Genetic Variation Underlying Psychosis-Inducing Effects of Cannabis: Sibling Analysis and Proband Follow-up. Arch. Gen. Psychiatry 68, 148–157. 10.1001/archgenpsychiatry.2010.152 [DOI] [PubMed] [Google Scholar]
- Veling W, 2013. Ethnic minority position and risk for psychotic disorders. Curr. Opin. Psychiatry 26, 166–171. 10.1097/YCO.0b013e32835d9e43 [DOI] [PubMed] [Google Scholar]
- Veling W, Selten J-P, Susser E, Laan W, Mackenbach JP, Hoek HW, 2007. Discrimination and the incidence of psychotic disorders among ethnic minorities in The Netherlands. Int. J. Epidemiol 36, 761–768. 10.1093/ije/dym085 [DOI] [PubMed] [Google Scholar]
- Whaley AL, 2001. Cultural Mistrust and Mental Health Services for African Americans: A Review and Meta-Analysis. Couns. Psychol 29, 513–531. 10.1177/0011000001294003 [DOI] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS, 2003. Racial/Ethnic Discrimination and Health:Findings From Community Studies. Am. J. Public Health 93, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yelton B, Friedman DB, Noblet S, Lohman MC, Arent MA, Macauda MM, Sakhuja M, Leith KH, 2022. Social Determinants of Health and Depression among African American Adults: A Scoping Review of Current Research. Int. J. Environ. Res. Public. Health 19, 1498. 10.3390/ijerph19031498 [DOI] [PMC free article] [PubMed] [Google Scholar]


