Abstract
Introduction:
Approximately 25% of older cancer survivors (i.e., ≥ 65 years, with cancer history) use ≥1 mobility device, surpassing usage by other older adults. Few tools exist for older “survivors” to regain function or follow lifestyle recommendations. Our goal was to explore opportunities to leverage technology-enabled mobility devices, such as the “smart cane,” to support mobility goals in these survivors. The research objective was to assess perceptions related to acceptability, usability and preferences of participants regarding technology-enabled mobility devices in everyday life.
Materials and Methods:
We used a convergent mixed-methods design, analyzing quantitative data followed by qualitative focus groups. A pre-survey derived from the Senior Technology Acceptance Model assessed the acceptability of technology-enabled devices among participants, who also participated in one of three focus groups delivered via Zoom. The Zoom sessions included facilitated 90-min discussions and video demonstration of the smart cane. Focus group sessions were recorded and transcribed verbatim and thematic content analysis was conducted.
Results:
We recruited 12 older US survivors. Participants were 58% female, aged 68–86, and 16% non-White. From a pre-survey of participants, 83% said that they liked the idea of technology-enhanced mobility device and 100% said they thought they could be skillful at using a technology-enabled device if training was provided. Though participants were enthusiastic about the smart cane overall and felt the smart cane supported independence for older adults, the themes revealed concerns about safety, accessibility and technology support, as well as the concern for negative impact on self-image due to use of a mobility device. There was a strong preference for working with clinical professionals as the most trusted sources for referrals, if a smart cane was suggested.
Discussion:
Older survivors in our sample found the smart cane very acceptable, and supportive of independence for older adults with cancer and other conditions. Participants also provided many insights that revealed additional research needed to support access, safety and usability for older adults, older survivors and caregivers, especially by partnering with clinical professionals.
Introduction
There are more than six million US adults that use mobility devices and two-thirds are older than 65 years1. Simultaneously, the aging of the US population has increased the cancer burden for older adults. In 2016, 62% of cancer survivors (i.e., individuals with any cancer history) were 65 years or older and roughly one-third also experienced comorbidities that may impede functional independence and could hinder cancer recovery2. Nationally representative data suggest that 25% of older survivors use one or more mobility device in their daily lives, exceeding mobility device use among other adults older than 65 years3. Yet, there are few tools available to address the specific needs of older survivors. Older adults with cancer frequently experience complications related to cancer treatment, such as chemotherapy-induced peripheral neuropathy, that causes difficulty with balance and increases fall risk4. Cancer and systemic cancer treatment may also exacerbate chronic conditions (such as diabetes and cardiac disease) associated with older age5, which in turn increases the risk of physical dysfunction and disability6, 7. However, there has been limited exploration of how best to use technology and technology-enabled mobility devices to achieve supportive care recommendations that include regular physical activity and movement8. These recommendations are important for maximizing symptom management, optimizing quality of life and aiding cancer recovery9.
The purpose of our project was to explore opportunities to leverage technology-enabled mobility devices, such as the “smart cane,” to support mobility goals in older survivors. The objective of the study was to assess perceptions related to acceptability, usability and preferences of participants regarding technology-enabled mobility devices in everyday life. We intend to use these insights to inform future intervention studies with older adult survivors and to identify opportunities for collaboration within clinical and community settings.
Methods
Eligibility Criteria
We recruited volunteers that met the following eligibility criteria: (1) 65 years or older; (2) community-dwelling older adults that have completed primary cancer treatment (surgery, chemotherapy and/or radiation); (2) individuals who were able to read and speak English; (3) individuals who were willing to be audio and video recorded.
Study Design
We used a convergent mixed-methods study design to assess older participants’ perceptions about technology in general and technology-enabled mobility devices (e.g., the smart cane). The convergent design used a brief quantitative assessment (a pre-survey) to assess comfort with technology followed by qualitative focus groups to explore perceptions related to acceptability, usability, and preferences of participants.
Procedures
All procedures were approved by The Pennsylvania State University College of Medicine Institutional Review Board (CATS STUDY00015818) and deemed exempt from full board review. Due to restrictions on in-person contact due to the COVID-19 pandemic, focus groups were held using a HIPPA-compliant, remote video platform (i.e., Zoom)10. Participants were primarily recruited via the Cancer and Aging Research Group (CARG), a national consortium of researchers and advocates focused on cancer and aging in older adults11, 12. Information about the study was provided to all participants and they provided verbal consent to participate. The focus group facilitator (EV) was an experienced qualitative interviewer who followed a semi-structured interview guide that explored overall perceptions of mobility devices and technology. Focus group methodology was chosen to leverage ‘group think’ and consensus building. The main topics covered were attitudes toward mobility devices, comfort with technology overall, demonstration/reaction to the smart cane, perceived usefulness of the smart cane and general questions about feasibility with older adults (See Facilitator Guide in Supplementary Material). During the focus group, the facilitator reviewed an information sheet about the smart cane with participants and introduced and then demonstrated its features on screen. Specific features were highlighted, including the flashlight, emergency signal, and Bluetooth accessibility (see Figure 1). Three focus groups were convened with four participants each. Facilitated discussions were approximately 90 minutes in length. All focus groups were audio recorded and transcribed verbatim13.
Figure 1. What is a Smart Cane?
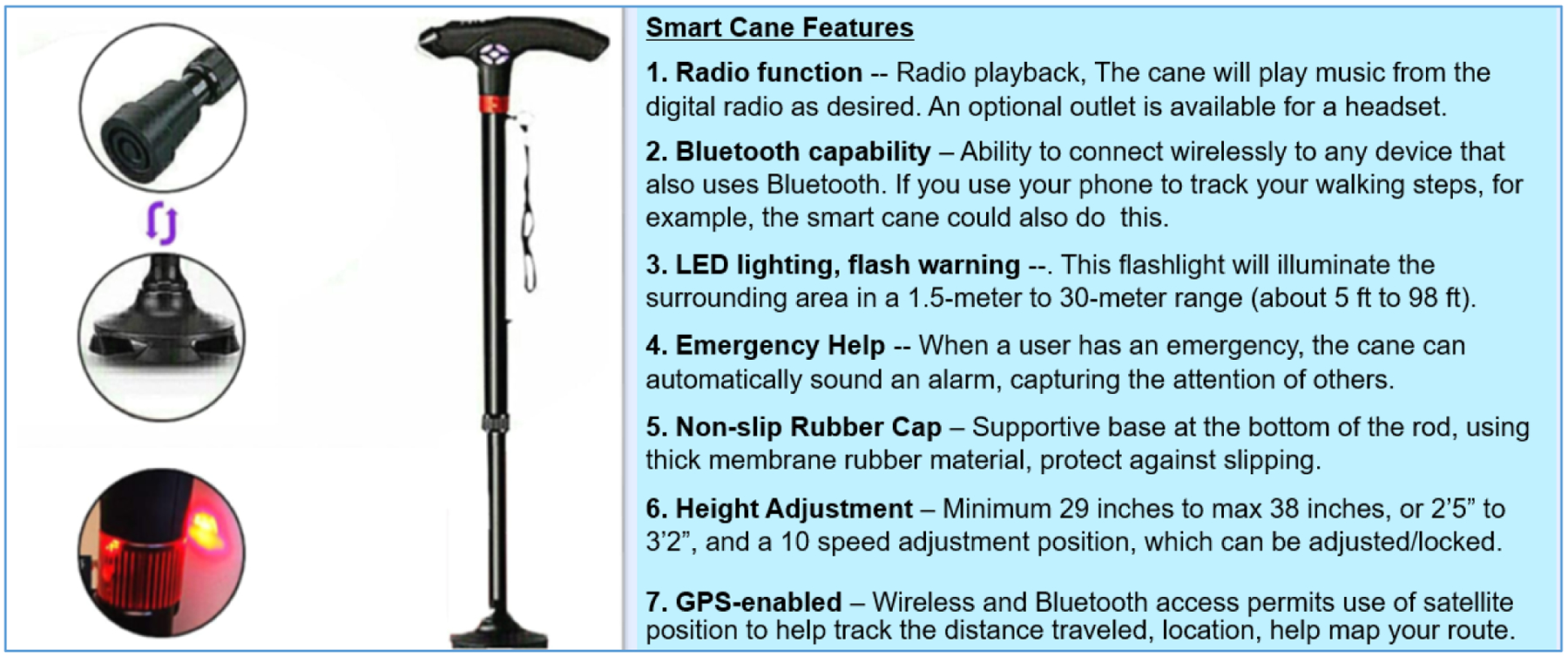
Focus group participants were given an information sheet like the figure below that described features of the cane. The smart cane product used in the sessions was purchased from an international vendor, but is similar to the Tomshine Elderly Adjustable Walking Cane now available in the United States.
Qualitative Analysis
We used an inductive approach to thematic analysis to analyze focus group transcripts using qualitative analysis software, NVivo (Release 1.0)14. To begin the analysis, a codebook was created by three co-authors (LJV, EV, SMB) after independently reviewing each transcript and creating broad categories and concepts. Then, the group arranged these concepts into a coding dictionary and organized them into a preliminary codebook. Detailed definitions and exemplar quotations were included in the codebook for each code. Next, two trained coding analysts (EV, HC) used the codebook to assign codes to the data using the constant comparison method13, 15.
Quantitative Analysis
Descriptive analyses (i.e., mean, range, percentage) were used to summarize participant characteristics and report results from the pre-survey.
Mixed Methods Integration
After independent analysis of the quantitative and qualitative datasets, a joint display was constructed to compare and contrast (‘merge’) conclusions from each dataset.
Results
Description of participants and Qualitative Results
The 12 study participants were all older survivors of various cancers. They were mostly women (58%), with a mean age of 74 years (range 68–86). Most identified as having a non-Hispanic White background, but our participants included one African-American survivor and one Asian-American survivor (about 16% of the group) (Table 1). Eighty-three percent of participants indicated they liked the idea of a technology-enhanced mobility device and 100% indicated they thought they could be skillful at using a technology-enabled device if training was provided (Table 2). More than half of participants (58%) said that a technology-enabled mobility device would be useful in their daily lives. A smaller proportion (25%) agreed with the statement that their financial situation could limit their activities in accessing/using a technology-enabled mobility device (Table 2).
Table 1.
Participant Characteristics
| Variable | Number (%) |
|---|---|
| Age (in years) | Mean age, 74 (range 68–86) |
| 65–72 | 4 (33%) |
| 73–79 | 6 (50%) |
| 80+ | 2 (17%) |
| Sex | |
| Female | 7 (58%) |
| Ethnicity | |
| Non-Hispanic White | 10 (83%) |
| Non-Hispanic African-American | 1 (8%) |
| Other (Asian-American) | 1 (8%) |
| Education | |
| High school | -- |
| Some college | 5 (42%) |
| ≥College graduate | 7 (58%) |
| Married | 8 (67%) |
| 0–2 | 9 (75%) |
| 3 or more | 3 (25%) |
| Fair/Good | 2 (17%) |
| Very Good/Excellent | 10 (83%) |
| Not at all | 5 (42%) |
| A Little | 5 (42%) |
| Moderately Limits | 2 (17%) |
| 1 year or less | 2 (17%) |
| >1–4 years | 2 (17%) |
| 5 years or more | 8 (67%) |
| Ever used any mobility device | |
| Yes | 3 (25%) |
| No | 9 (75%) |
| Breast | 4 (33%) |
| Colon/Colorectal | 2 (17%) |
| Prostate | 1 (8%) |
| Melanoma | 2 (17%) |
| Lung | 1 (8%) |
| Thyroid | 1 (8%) |
| Lymphoma | 1 (8%) |
| Surgery | 10 (83%) |
| Chemotherapy | 4 (33%) |
| Radiation | 5 (42%) |
| Immunotherapy | 3 (25%) |
| Hormonal Therapy | 2 (17%) |
Table 2.
Pre-Survey Results based on Senior Technology Acceptance Model*
| Senior Technology Acceptance Model Survey Results (Number, %) based on Likert Scale (1 strongly disagree to 10 strongly agree) | |
|---|---|
| Using technology-enabled mobility device would enhance my effectiveness in daily activities | |
| Disagree/Strongly Disagree | 4 (33%) |
| Agree/Strongly Agree | 7 (58%) |
| Did not answer | 1 (8%) |
| A technology-enabled mobility device would be useful in my daily life | |
| Disagree/Strongly Disagree | 4 (33%) |
| Agree/Strongly Agree | 7 (58%) |
| Did not answer | 1 (8%) |
| I like the idea of a technology-enabled mobility device | |
| Disagree/Strongly Disagree | 1 (8%) |
| Agree/Strongly Agree | 10 (83%) |
| Did not answer | 1 (8%) |
| If needed, you could be skillful at using a technology-enabled mobility device | |
| Disagree/Strongly Disagree | 0 |
| Agree/Strongly Agree | 12 (100%) |
| I could complete a task using a technology-enable mobility device if there is someone who could demonstrate how | |
| Disagree/Strongly Disagree | 0 |
| Agree/Strongly Agree | 12 (100%) |
| My financial status would not limit My financial status would not limit my activities in using a technology-enhanced mobility device | |
| Disagree/Strongly Disagree | 3 (25%) |
| Agree/Strongly Agree | 8 (67%) |
| Did not answer | 1 (8%) |
| If I wanted or needed to use a technology-enhanced mobility device, it is accessible to me. | |
| Disagree/Strongly Disagree | 0 |
| Agree/Strongly Agree | 11 (92%) |
| Did not answer | 1 (8%) |
| I feel apprehensive about the idea of using a technology-enhanced mobility device. | |
| Disagree/Strongly Disagree | 11 (92%) |
| Agree/Strongly Agree | 1 (8%) |
| I would hesitate to use a technology-enhanced mobility device for fear of making mistakes I cannot correct. | |
| Disagree/Strongly Disagree | 12 (100%) |
| Agree/Strongly Agree | 0 |
Source: Chen et al, 2020.
Main Themes from Qualitative Analysis
Five themes emerged: (1) Older adults in our sample were enthusiastic about technology-enabled canes or mobility devices that included safety and usability features; (2) While older adults in our sample were generally open to cane usage in the future if needed, they felt that using a cane could negatively impact self-image and confidence in some older adults; (3) While most of our participants were comfortable using technology in general, participants noted fear, lack of knowledge, and the perceived inability to keep up with changing technology as barriers to technology adoption among some older adults; (4) Primary barriers to smart cane use may include financial and usability concerns; (5) Participants in our sample viewed clinicians as the trusted sources from whom patients should receive smart and other mobility devices.
Theme 1: Older adults were enthusiastic about technology-enabled canes or mobility devices that included safety and usability features.
Older adults had a positive attitude toward technology and technology-enabled canes in general, especially if presented as a means to support independence. One participant said, “For me, it would mean restoring something that I’ve lost, whether it’s um, a sense of independence or whether it’s a specific activity…but it would have to be something that I feel I have lost and could regain with the use of the cane.”
However, the idea that safety features could be customized for personal needs and preferences was highly valued. One feature that was well-received was the adjustable flashlight that would be used for our outdoor walking. One adult said, “I like the light, because that’s always an issue when you’re walking, is how do you-- a cane, maybe have a bag in your other hand. How do you handle a flashlight? Some way to illuminate the pathway that you’re walking on. I think that’s very important.”
We also asked our participants if the smart cane could be helpful or a hindrance for caregiver support. The majority, many of whom had experience as both the person receiving and providing support, noted that this type of device could be very useful. “… I think that… it really will be a big relief for the caregiver, you know, that the person can use the cane, get up, and then walk a short distance to the kitchen and then maybe get a glass of water-- those kind of things the caregiver will not have to do. Just think about that.”
Theme 2: While older adults were generally open to cane usage in the future if needed, they felt that using a cane could negatively impact self-image and confidence in some older adults.
Our participants discussed the potential that some older adults find the experience of using a mobility device as stigmatizing. One participant said, “It is kind of an image thing…It’s funny because crutches-- hey, they’re acceptable, because crutches, anybody can use them. But a cane is another story, because a cane says, oh, here is an older woman who’s having trouble getting around…”.
In the literature around mobility device use and older adult acceptance, Coughlin suggests that many older adults may tend to reject helpful technologies in an effort to distance themselves from ageist stereotypes and negative associations augmented by using these devices16. These stereotypes of ‘oldness’ are often negative, depicting old age as a time of poor health, disability, dependency, declining mental and physical functioning, loneliness and incompetence17. To this point, another one of our participants said, “I think it’s a very visible sign that you’re not as young and mobile and healthy as you were at one time. I think it carries, a lot of time, a negative connotation.”
However, our participants also mentioned the benefits of using a mobility device, to restore control and confidence for older adults. As one participant put it, “I think it would give (older adults) more control. So often when you have cancer, you feel like you have no control over anything. Um, and I think this might help alleviate some of that.”
Theme 3. While most participants were comfortable using technology in general, participants noted fear, lack of knowledge, and the perceived inability to keep up with changing technology as barriers to technology adoption among some older adults
The group felt generally comfortable with technology and wanted to be have access to innovations that could enhance their lives. For example, a participant stated that “I think research has shown where there is access, that most older adults are able to learn basic communication technology and… use it well”.
However, there was a recognition that many older adults might not feel that way or could feel left behind by rapid advancements in technology. For example, one adult said, “I feel like the technology moves faster than (older adults) are able, actually, legitimately, to adopt it. And so I do believe some people are absolute whizzes at technology, and some people have to grapple with it. And I am actually somebody who has to grapple with it.”
When the facilitator asked “why do you think that…some older individuals are so resistant to adopting…new technology?” one participant stated that they felt a large issue was fear and feeling incompetent. “Fear is… one (reason). Because (older adults) don’t want to look stupid. They don’t want to go ask, unless it’s their immediate family. They don’t want to go ask questions-- how do I do this? Especially, you know, a person who is-- even in the hospital, we have those kiosks, you know, auto check in. They will not use it. They have to-- they have to wait in the line and stand in front of people because they don’t want to, um, look stupid. I think that’s one issue.
Theme 4: Primary barriers to Smart Cane utilization include financial and usability concerns.
Among older adults, there were many comments and questions about practical considerations with obtaining a smart cane, including ability to find the cane, the cost of purchase and any implications for healthcare coverage. At the top of the list, was the strong desire for potential reimbursement from federal payors. Said one participant, “I think one other thing as we think about smart canes, I think it’ll be very important to make sure that these devices get on the approved Medicare/Medicaid list.”
Additionally, participants worried about the danger of having a mobility device look too attractive, which could make older adults targets for theft. As one adult described it, “I’d be worried that this is all bells and whistles cane that could get stolen from somebody who’s out for a walk.” Similarly, participants commented that having a device that is too sophisticated might entail greater time and cost for users to maintain. As one participant said, “It’s just that the higher tech things are, the more things can go wrong.”
Our participants also wondered if potential users would weigh the long or short-term use of the device in their purchase decision. One participant explained, “… I don’t see this cane being used as a short-term solution if you, you know, just had a knee operation and you need…a cane 30 to 60 days. It’s probably too expensive to do that.”
Theme 5: Clinicians are viewed as the trusted sources from whom patients should receive smart and other mobility devices.
There was a strong sentiment among participants that members of the clinical team were necessary for referral and education on how to properly use a smart cane to achieve mobility goals. Physicians and nurses were mentioned as important gatekeepers, but physical therapists (PT), occupational therapists (OT) and similar clinical professional were recognized as important members of the team for training and fitting to optimize smart cane use. One participant explained, “I think PTs and OTs are it because your doctors, when you go through hip or knee surgeries, you go to physical therapy. So, who better to give it to you? I mean, you do want to run it by orthopods because they’re the ones who, you know, do the surgeries, and it’d would be interesting to get their input. But I think the ones that really need to teach it is the PT and the OT.”
We also asked participants what potential tools would be useful for training on how to use the smart cane. Many said that a video of some sort could be useful, especially if it could be accessed online (on YouTube or another consumer-friendly web site). For example, one adult said, “Well-- well, you need a video of it. You’d need a video of it, you know, a step-by-step video of how …everything works.”
Mixed Methods Integration
Table 3 provides a joint display that integrates findings on acceptability and feasibility of the technology-enabled mobility devices from the perspectives of our participants. In both the qualitative and quantitative datasets, participants found the technology acceptable, however, nuanced information about potential concerns about users’ self-image was brought out by the qualitative focus groups and may explain why participants did not give fully positive ratings in the survey (as shown in Table 2). With regards to feasibility, there was discrepancy in findings as the quantitative data indicated a lack of concern or apprehension about the use of the technology, yet qualitative analysis did reveal some concerns about technologic barriers, fear, or lack of knowledge about technology as a potential barrier to uptake.
Table 3.
Joint display of mixed methods findings
| Salient Quantitative findings | Salient Qualitative findings | Convergence/Divergence of Qualitative and Quantitative Datasets | Conclusions | |
|---|---|---|---|---|
| Acceptability | 58% felt technology-enabled mobility devices would enhance daily activities and be useful in daily life. 83% liked the idea of technology-enabled mobility device. |
Theme 1. Older adults were enthusiastic about technology-enabled canes or mobility devices that included safety and usability features. Theme 2. While older adults were generally open to cane usage in the future if needed, they felt that using a cane could negatively impact self-image and confidence in some older adults. |
Convergence with mild divergence related to concerns about self-image when using mobility device. | Participants found the concept of technology-enabled mobility devices acceptable although some issues related to usefulness, confidence in using technology-devices and self-image may have an impact on full acceptability. |
| Feasibility | 100% reported having no concerns in items related to their own ability to use the technology-enabled mobility devices. 92% felt such technology was accessible and were not apprehensive about using technology-enhanced mobility devices. |
Theme 3. While most participants were comfortable using technology in general, participants noted fear, lack of knowledge, and the perceived inability to keep up with changing technology as barriers to technology adoption among some older adults Theme 4. Primary barriers to Smart Cane utilization include financial and usability concerns. |
Divergence Participants felt that for themselves they had no concerns, but worried that others may have tech/knowledge/fear/financial concerns |
Participants felt the use of technology-enhanced devices was feasible for themselves, although additional studies in less tech-savvy group are warranted in order to further evaluate and possibly address potential barriers. |
Discussion
In this exploratory work, our goal was to understand opportunities to leverage technology-enabled mobility devices, such as the “smart cane,” to support mobility goals in older cancer survivors. Our participants were highly receptive to the idea of a smart cane, designed specifically for older adults, including cancer survivors, who may have mobility impairments. That said, they also raised important concerns – affordability, considerations for user safety, opportunities for insurance coverage and logistical questions about updates and user training, which should be addressed before any programs or initiatives are launched.
One important takeaway from the sessions was that while our participants believed that older cancer survivors could benefit from a smart cane as part of a rehabilitation program, they also emphasized that all older adults with chronic diseases that affected mobility could similarly benefit. Additionally, we set out to recruit a sample of cancer survivors and caregivers, but all participants ended up having experience with both roles. Therefore, researchers looking to develop educational, or training programs may consider adjusting the approach to be inclusive of a variety of experiences related to chronic illnesses.
This work had some particular strengths. First, this is the first study to our knowledge of the smart cane in older adults with a history of cancer. As a growing and understudied population11, 18, such technology offers a tremendous opportunity for supportive care for older cancer survivors. We also used a convergent mixed-methods approach to glean insights using both quantitative surveys and qualitative focus groups. Doing so allowed our findings to be more nuanced and situated in deeper context than they would have been with either dataset alone (e.g., concerns about self-image with use of smart devices would not have been possible from quantitative surveys alone, yet surveys were helpful in assessing prevalence of opinions that may not have been otherwise shared during focus groups). Further, conducting the focus groups on Zoom facilitated participation from a variety of participants from all over the country, with different cancer sites and demographic backgrounds.
However, there were aspects that could be improved. Because we completed our work during the early stage of the pandemic, patient recruitment was extremely difficult, and we were unable to allow participants to handle the smart cane themselves because the sessions were held on Zoom. It is possible that this requirement to use Zoom biased our sample in favor of participants who were more technologically-savvy. Further, to be as inclusive as possible with interested participants, we did not require prior mobility impairments to participate, and, therefore, not all participants had mobility concerns for themselves. However, through our screening process, we learned that three out of the 12 participants had mobility challenges and this is consistent with estimates from nationally representative data that 25 percent of older cancer survivors have recently used one or more mobility devices in the United States3.
We also recognize that the general comfort with technology or the smart cane concept expressed by our participants may not reflect general acceptability with all older adults. As with most qualitative research, generalizability should not be inferred due to our small sample size, convenience sampling approach, and lack of diversity with regards to race. Additional research is needed to examine acceptability with the oldest adults (e.g., 85 years and older), more adults from racially/ethnically diverse backgrounds and older adults from rural communities.
That said, our study offers some important insights. The pandemic has highlighted the importance of technology access to serve the needs of older adults and demonstrated that such technology could be utilized to better serve older adults. Our findings suggest that older adults are open to such technology and appreciate its use within their lives. Thus, there is value in rising to the challenge of combating the digital divide for older adults in the United States and throughout the world19 and smart canes offer one way we might leverage technology to improve health and mobility. Future work will assess the smart cane in clinical and community settings to learn more about how best to incorporate the smart cane into supportive care programs for recovery from cancer or other chronic diseases affecting older adults.
Supplementary Material
Acknowledgements:
Shirley M. Bluethmann is supported by a Mentored Research Scholar Grant in Applied and Clinical Research, MSRG-18-136-01-CPPB, from the American Cancer Society (ACS). Drs. Bluethmann and Van Scoy were supported by the Qualitative and Mixed Methods Research Core through the Penn State CTSI (NIH UL1 TR002014). Dr. Bluethmann and Mr. O’Shea were also supported by the Cancer and Aging Research Group, funding the NIA of the National Institutes of Health (NIH) under award R33AG059206. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the ACS.
Footnotes
Conflict of Interest: The authors have declared no conflicts of interest for this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Gell NM, Wallace RB, Lacroix AZ, Mroz TM, Patel KV. Mobility device use in older adults and incidence of falls and worry about falling: Findings from the 2011–2012 National Health and Aging Trends Study. J Am Geriatr Soc. 2015;63(5):853–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “Silver Tsunami”: Prevalence Trajectories and Comorbidity Burden among Older Cancer Survivors in the United States. Cancer Epidemiology Biomarkers & Prevention. 2016;25(7):1029–1036. doi: 10.1158/1055-9965.EPI-16-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bluethmann SM, Flores E, Campbell G, Klepin HD. Mobility Device Use and Mobility Disability in U.S. Medicare Beneficiaries With and Without Cancer History. J Am Geriatr Soc. 2020;n/a. doi: 10.1111/jgs.16789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bao T, Basal C, Seluzicki C, Li SQ, Seidman AD, Mao JJ. Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence, risk factors, and fall risk. Breast Cancer Res Treat. 2016;159(2):327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sturgeon KM, Deng L, Bluethmann SM, et al. A population-based study of cardiovascular disease mortality risk in US cancer patients. Eur Heart J. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winters-Stone KM, Horak F, Jacobs PG, et al. Falls, functioning, and disability among women with persistent symptoms of chemotherapy-induced peripheral neuropathy. Journal of Clinical Oncology. 2017;35(23):2604–2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freedman VA, Kasper JD, Spillman BC, et al. Behavioral adaptation and late-life disability: a new spectrum for assessing public health impacts. Am J Public Health. 2014;104(2):e88–e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naeim A, Aapro M, Subbarao R, Balducci L. Supportive Care Considerations for Older Adults With Cancer. Journal of Clinical Oncology. 2014;32(24):2627–2634. doi: 10.1200/JCO.2014.55.3065. [DOI] [PubMed] [Google Scholar]
- 9.Ng AH, Ngo-Huang A, Vidal M, et al. Exercise Barriers and Adherence to Recommendations in Patients With Cancer. JCO Oncology Practice. 2021;17(7):e972–e981. doi: 10.1200/OP.20.00625. [DOI] [PubMed] [Google Scholar]
- 10.Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using zoom videoconferencing for qualitative data collection: perceptions and experiences of researchers and participants. International journal of qualitative methods. 2019;18:1609406919874596. [Google Scholar]
- 11.Hurria A, Levit LA, Dale W, et al. Improving the Evidence Base for Treating Older Adults With Cancer: American Society of Clinical Oncology Statement. Journal of Clinical Oncology. 2015. doi: 10.1200/JCO.2015.63.0319. [DOI] [PubMed] [Google Scholar]
- 12.Gilmore NJ, Canin B, Whitehead M, et al. Engaging older patients with cancer and their caregivers as partners in cancer research. Cancer. 2019;125(23):4124–4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hsieh H, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 14.QSR International Pty Ltd. https://www.qsrinternational.com/nvivo-qualit2021.
- 15.Strauss A, Corbin JM. Basics of qualitative research: Grounded theory procedures and techniques. Sage Publications, Inc; 1990. [Google Scholar]
- 16.Coughlin JF, D’Ambrosio LA, Reimer B, Pratt MR. Older adult perceptions of smart home technologies: implications for research, policy & market innovations in healthcare. 2007:1810–1815. [DOI] [PubMed] [Google Scholar]
- 17.Astell AJ, McGrath C, Dove E. ‘That’s for old so and so’s!’: does identity influence older adults’ technology adoption decisions?. Ageing & Society. 2020;40(7):1550–1576. [Google Scholar]
- 18.Mohile S, Dale W, Magnuson A, Kamath N, Hurria A. Research priorities in geriatric oncology for 2013 and beyond. 2013;37(3):216. [PMC free article] [PubMed] [Google Scholar]
- 19.Bluethmann SM, Coa KI, Alfano CM, Hesse BW. Electronic health information exchange opportunities for self-management of care: responses from older adults with and without cancer history in the United States. Curr Oncol Rep. 2018;20(4):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


