Abstract
Introduction and importance
Gastric fistula is a complication in gastrointestinal surgery. For decades, patients with gastric fistulas were treated surgically, with high morbidity and mortality. Minimally invasive treatment through endoscopic therapy with stents and interventionism has allowed improvements. We present a case of successful hybrid laparoscopy and endoscopy for the treatment of a post-Nissen fundoplication gastric fistula.
Case presentation
A 44-year-old male underwent laparoscopic Nissen fundoplication surgery; at 10 days post-surgery, he presented with oral intolerance, abdominal pain, and laboratory results showing an inflammatory response. Imaging studies indicated intra-abdominal collection; therefore, a laparoscopy revision was performed; transoperative endoscopy confirmed intra-abdominal collection and a gastric fistula. In turn, we performed closure with an omentum patch through the fistula fixed with OVESCO by endoscopy, with successful results.
Clinical discussion
Gastric fistula is a difficult complication to treat because exposure to secretions causes inflammation. Endoscopic techniques are described for the closure of gastrointestinal fistulas; however, several aspects must be considered for their use. Hybrid laparoscopic and endoscopic treatment in the same surgery can be useful and served as a novel and successful option in our case.
Conclusion
Hybrid treatment with endoscopy and laparoscopy can be considered an optional approach for the management of gastric fistulas greater than 1 cm and of several days of evolution.
Keywords: Gastric fistula, OVESCO, Hybrid treatment, Graham patch, Omentum patch, Nissen fundoplication, Case report
Highlights
-
•
Gastric fistula and late diagnostic gastric perforation are difficult complications to treat because the exposure to gastric secretions causes tissue inflammation.
-
•
Endoscopic and minimally invasive techniques are described for the surgical closure of gastrointestinal fistulas. These techniques are mainly used in small defects in which the tissue is viable, clear and regular.
-
•
Hybrid laparoscopic and endoscopic treatment within the same surgery is directed to the closure of this defects with everted and non-clear edges can be useful as a novel and successful option in these cases.
-
•
In international literature, there are no available reports of hybrid approaches that allow laparoscopic and endoscopic management for closure of chronic defects or that do not have the optimum tissue characteristics.
1. Introduction
Gastrointestinal fistulas depict a serious complex pathological entity, gastrointestinal fistulas are defined as an abnormal communication between two surfaces. According to literature, as much as 75 to 85 % of gastrointestinal fistulas appear postoperatively, and any intervention performed in the stomach can evolve or develop into a gastrointestinal fistula. The most common surgical interventions include partial gastrectomy, anti-reflux surgery, laparoscopic sleeve gastrectomy, and laparoscopic gastric bypass, among others [1].
Conventionally, the treatment of gastric leaks or fistulas has been mainly surgical; nevertheless, during the last decade, endoscopic management has been described with effectiveness results close to 90 % and lower morbidity compared to classic treatments. Among endoscopic methods, endo-clips have been described, however initially, these were poorly effective for the closure of perforations greater than 10 mm due to their grip restriction.
After some time, the Over-The-Scope Clip (OVESCO) system was developed, which consists on the usage of rounded clips preassembled onto a plastic cap at the distal end of the endoscope, creating a strong grip and enough pressure without inducing ischemia or laceration. The use, efficacy and safety of OVESCO system have been described with a clinical success rate of 70 %–100 % for the closure of gastric wall perforations due to enclosing 2 or 3 layers of the gastric wall in comparison to conventional clips [1].
In the literature, there are no descriptions of hybrid, laparoscopic and endoscopic management for the treatment of gastric fistula. Therefore, we consider this an interesting discussion to present a successful hybrid treatment in a postoperative gastric fistula with inflammatory tissue, everted and non-clear edges. The case report was conducted according to the SCARE 2020 guidelines [2].
2. Case report
A 44-year-old man, with a 10-year history of gastroesophageal reflux disease, presented episodes of heartburn that subsided with the intake of proton pump inhibitors, however, the heartburn intensified during the last 12 months. The last endoscopic study showed serious esophageal changes secondary to gastroesophageal reflux. Biopsy results revealed Barret's esophagus. Laparoscopic Nissen fundoplication was therefore programmed.
During the surgical procedure, a type II hiatal hernia with open diaphragmatic pillars was found. Hiatoplasty and Nissen fundoplication were performed using simple Ethibond sutures (Fig. 1). During the procedure there were no complications and the patient was transferred to the recovery room. After 24 h the patient was discharged.
Fig. 1.

Image of the fundoplication.
Ten days after surgery, the patient was seen in the emergency room due to oral intolerance, not quantified elevated body temperature and abdominal pain. The patient was tachycardic, and during physical examination he showed vague abdominal pain without signs of peritoneal irritation. In the laboratory the presence of leukocytosis with significant neutrophilia was highlighted. Ultrasound imaging of the abdominal cavity showed a liquid-like image with a volume of 50 ml located in the subhepatic region, compatible with an intra-abdominal collection.
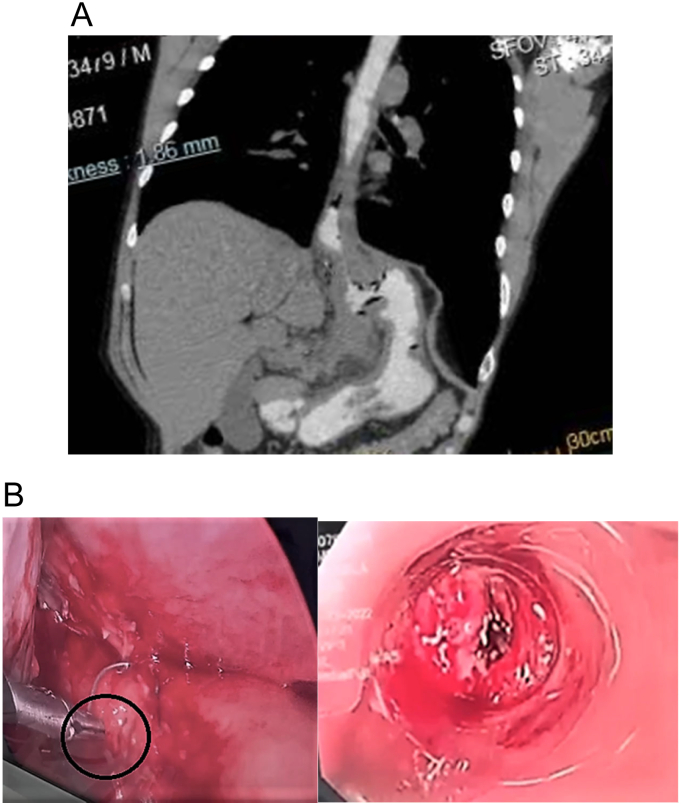
Contrast computed tomography (CT) reported a right subhepatic collection with a volume of 150 ml. Broad-spectrum antibiotic treatment was initiated, and surgical revision was decided. During laparoscopic surgery, a serious subhepatic inflammatory process on the right side was found, it comprised a purulent collection of 100 ml and an orifice of approximately 1.5 cm in diameter located on the anterior face of the previously manufactured fundoplication, it had everted and not clear edges, which were also friable; these characteristics hindered normal primary stitching. An endoscopy was performed during the surgery, and the diagnosis of gastrointestinal fistula was confirmed (Fig. 2A and B).
Fig. 2.
A Abdominal computer tomography showing subhepatic collection.
B fistula orifice found during laparoscopy and confirmed by endoscopy.
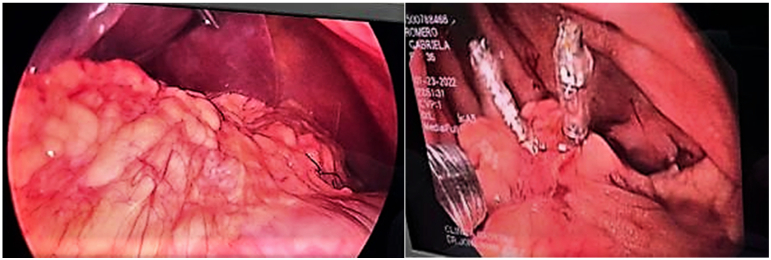
Hybrid treatment was performed, using intraoperative therapeutic endoscopy and laparoscopy. The greater omentum was introduced, approximately 15 cm, through the fistula, shaping a patch of omentum and fixating it to the gastric mucosa with the OVESCO system and two endoscopic clips using endoscopy (Fig. 3). A feeding jejunostomy was manufactured and two negative pressure drains were placed (Fig. 4).
Fig. 3.
Omentum patch fixated with the OVESCO system and intragastric clips.
Fig. 4.

Post-surgical negative pressure drains and feeding jejunostomy.
We started enteral feeding through jejunostomy 48 h after the procedures and oral feeding was started 10 days after surgery with adequate tolerance. With favorable evolution, the feeding jejunostomy was removed 20 days after surgery.
3. Discussion
Nowadays, the approach for managing postsurgical gastric fistulas or perforations is kept in constant discussion throughout the main surgical forums, as surgeons keep trying to incorporate less invasive methods as a key treatment for these pathologies to obtain better results.
The traditional handling of a postsurgical gastric fistula includes nutritional, electrolytic and infectious stabilization of the patient and drainage of the intra-abdominal collection using percutaneous or surgical methods.
The use of endoscopy in the context of a gastrointestinal fistula or gastric leakage is aimed at the treatment of extraluminal collections and the direct approach of the aforementioned defect [3]. In regard to extraluminal collections, endoscopy allows the irrigation of the extraluminal space through the gastric defect, as well as the debridement of the collection, repositioning of directed drains, and the initial internal drainage of not previously drained collections, using stents, or through double “J” or Pigtail catheters that can be placed across the defect and towards the extraluminal cavity, leading to a success rate of up to 98 %–100 % [3], [6]. Nevertheless, these therapies are aimed at dealing with the secondary defect that the leakage of gastric fluid produces, and not to the closure of a belatedly diagnosed defect or a chronic gastrointestinal fistula.
Vacuum therapy (vacuum) has also been described for drainage of collections in the management of gastrointestinal fistula, placing a piece of vacuum sponge at the end of a nasogastric tube that is then placed endoscopically within the extraluminal defect, a success rate up to 78–100 %, has been described [3].
Regarding the management of the gastric defect, the use of clipping or suture have been described as a definitive closure methods and, as nondefinitive methods (control of the leak without closure the defect), the use of stents and drains [4]. Endoscopic clipping can be performed using clips that cross through the endoscope (through-the-scope clips), better known as endoclips or hemoclips, which have shown to close small perforations with straight and clean edges [4]. The OTSC (Over-the-Scope-Clips) or OVESCO are nitinol devices loaded in a deployment device that is connected to the endoscope; there are 2, the OTSC (OVESCO Endoscopy, Germany) and Padlock (US Endoscopy., Mentor) [3]. These devices are capable of maintaining the total thickness of the portions of the gastrointestinal tract, which is why they are used to close defects up to 2 cm in diameter, with success rates up to 80 % in the closure of enteric leaks and up to 55 % in the closure of chronic fistulas [3], [5].
The definitive closure of gastric leaks is also achieved by employing endoscopic sutures, there are two approved devices, the Overstitch (Apollo Endosurgery) and the Overstitch Sx (Apollo Endosurgery) [3]. The suture is used for defects greater than 2 cm and that cannot be addressed using clips. One of its disadvantages is the difficulty of addressing proximal leaks because it does not allow complete mobility of the suture arm. In the same manner, the closure of defects with the OVESCO overstitch method has been described, where the suture reduces the size of the defect and in turn it can be completely closed with the OVESCO [7].
In respect to the use of endoluminal stents to divert the gastric content distally, success has been achieved; however, these stents tend to migrate, and even so, they achieve success rates, especially when other tools, such as cyanoacrylate adhesives, are incorporated [8].
4. Conclusion
Endoscopic closures are directed to viable tissue with regular and clear edges as well as a laparoscopic approach, in which a primary suture could be performed for early diagnosed perforations but with a lesser success rate when performed in late diagnosed gastrointestinal perforations or fistulas.
In international literature, at the moment, there are no reports of hybrid approaches that allow an integral comprehension of laparoscopic and endoscopic management directed to the closure of a primary defect. We report this case taking into account that the hybrid approach of a Graham patch with fixation of the OVESCO system for gastric fistulas greater than 1 cm was a success in our case. This allows us to propose this hybrid approach as an option in management of late diagnosed gastrointestinal perforations or fistulas. More research in this regard and in a larger group is needed.
Consent
Written consent was obtained from the patient for publication of this case report and adjacent images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
The study is exempt from ethical approval in our institution.
Funding
No funding or sponsorship.
Guarantor
Mauricio Palacios.
Research registration number
Not applicable – single case report.
CRediT authorship contribution statement
Mauricio Palacios and Jonathan Jerez: Study concept and surgical therapy for this patient. Juan Fernando Salazar, Mariela Andrade, Stephany Rojas Chavez y Andrea Lisintuña: Data collection. Alex Guachilema Writing-original draft preparation. Adriana Cisneros Salazar, Sandra Morocho and Karla Rivera: Editing and writing. Mauricio Palacios and Alex Guachilema: Senior author and the manuscript reviewer. All authors read and approved the final manuscript.
Declaration of competing interest
Nothing to declare.
Acknowledgement
None.
References
- 1.Bhurwal A., Mutneja H., Tawadross A., Pioppo L., Brahmbhatt B. Gastrointestinal fistula endoscopic closure techniques. Ann. Gastroenterol. 2020;33(6):554–562. doi: 10.20524/aog.2020.0543. Nov-Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 3.Siegal S.R., Pauli E.M. Endoscopic management of postoperative complications. Surg. Clin. North Am. 2020 Dec;100(6):1115–1131. doi: 10.1016/j.suc.2020.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Ge P.S., Thompson C.C. The use of the overstitch to close perforations and fistulas. Gastrointest. Endosc. Clin. N. Am. 2020 Jan;30(1):147–161. doi: 10.1016/j.giec.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baruah Anushka, Song Louis, Buttar Navtej. Endoscopic management of fistulas, perforations and leaks. Tech. Gastrointest. Endosc. 2016:17. doi: 10.1016/j.tgie.2016.02.001. [DOI] [Google Scholar]
- 6.El-Sayes I.A., Frenken M., Weiner R.A. Management of leakage and stenosis after sleeve gastrectomy. Surgery. 2017 Sep;162(3):652–661. doi: 10.1016/j.surg.2017.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Juzgado D., Sanchez-Yague A. The use of the overstitch beyond bariatric endoscopy: a pictorial description. Gastrointest. Endosc. Clin. N. Am. 2020 Jan;30(1):173–185. doi: 10.1016/j.giec.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Schulman A.R., et al. Endoscopic devices and techniques for the management of bariatric surgical adverse events (with videos) Gastrointest. Endosc. 2020 Sep;92(3):492–507. doi: 10.1016/j.gie.2020.04.002. [DOI] [PubMed] [Google Scholar]