Abstract
Introduction and importance
Infarction occurs occasionally in benign mammary tumors but is extremely rare in breast cancer, with few cases having been reported.
Presentation of case
A 53-year-old woman presented to our hospital with a mass and pain in the upper lateral region of the right breast. She underwent a needle biopsy and was histologically diagnosed as having invasive carcinoma. A ring-enhancing spherical mass was seen on contrast-enhanced computed tomography and magnetic resonance images. She underwent a right partial mastectomy with sentinel lymph node biopsy for T2N0M0 breast cancer. Macroscopically, the tumor was a yellow mass. Histopathologically, the site contained extensively necrotic tissue with foam cell aggregation, lymphocytic infiltration, and fibrosis in the periphery. No viable tumor cells were observed. The patient was followed up without postoperative chemotherapy or radiotherapy.
Clinical discussion
Ultrasound examination performed before the biopsy showed blood flow inside the tumor, but a review of the histopathological tissue after surgery revealed generally low viability of the tumor cells in the biopsy specimen, and the possibility that the tumor had a strong tendency to be necrotic from the beginning was considered. It is presumed that some immunological mechanism was working.
Conclusion
We have encountered a case of breast cancer with complete infarct necrosis. Infarct necrosis may be present if a contrast-enhanced image shows ring-like contrast.
Keywords: Breast tumor, Breast cancer, Infarction, Necrosis
Highlights
-
•
Infarct necrosis of breast cancer is very rare.
-
•
This is the first report of complete necrosis of breast cancer.
-
•
On imaging, a tumor that appears as a ring-shaped enhancing lesion may be necrotic.
1. Introduction
Infarction has been reported to occur in benign mammary gland tumors such as fibroadenoma, phyllodes tumor, and intraductal papilloma, and in the mammary glands during pregnancy and lactation. However, reports of infarction of breast cancer are extremely rare. Here we report a case of breast cancer with complete infarct necrosis of the tumor.
This report was written in accordance with the SCARE criteria [1].
2. Case presentation
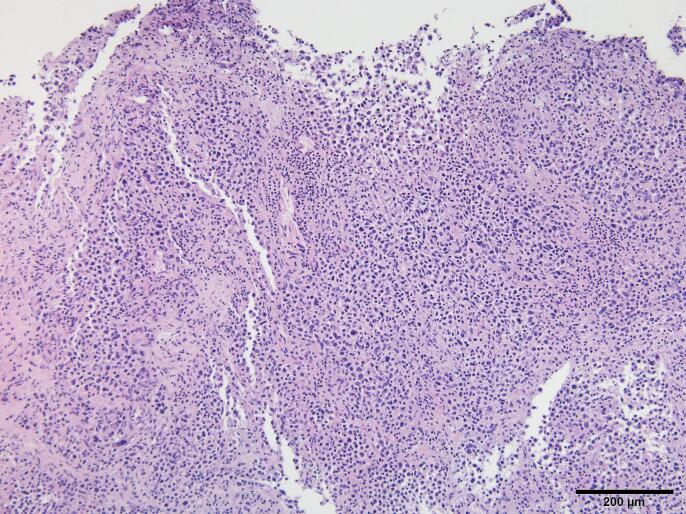
The patient was a 53-year-old woman who presented to our hospital with a palpable 2-cm mass and pain in the upper lateral region of the right breast. The patient did not have a special and family history to be specified. Mammography revealed a dense 2-cm mass with poorly defined borders and a finely serrated margin. Ultrasonography revealed a well-circumscribed 2-cm mass with heterogeneous internal echogenicity in the right breast (Fig. 1). Blood flow was observed within the tumor. There was no axillary lymph node enlargement.
Fig. 1.
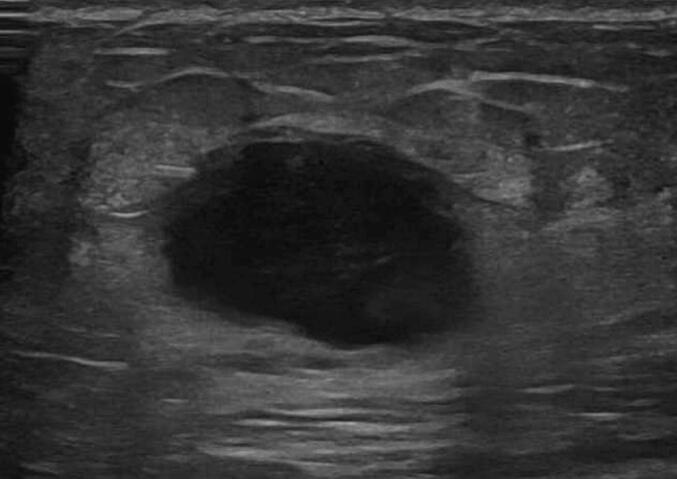
An oval, well-demarcated, hypoechoic mass with coarse margins.
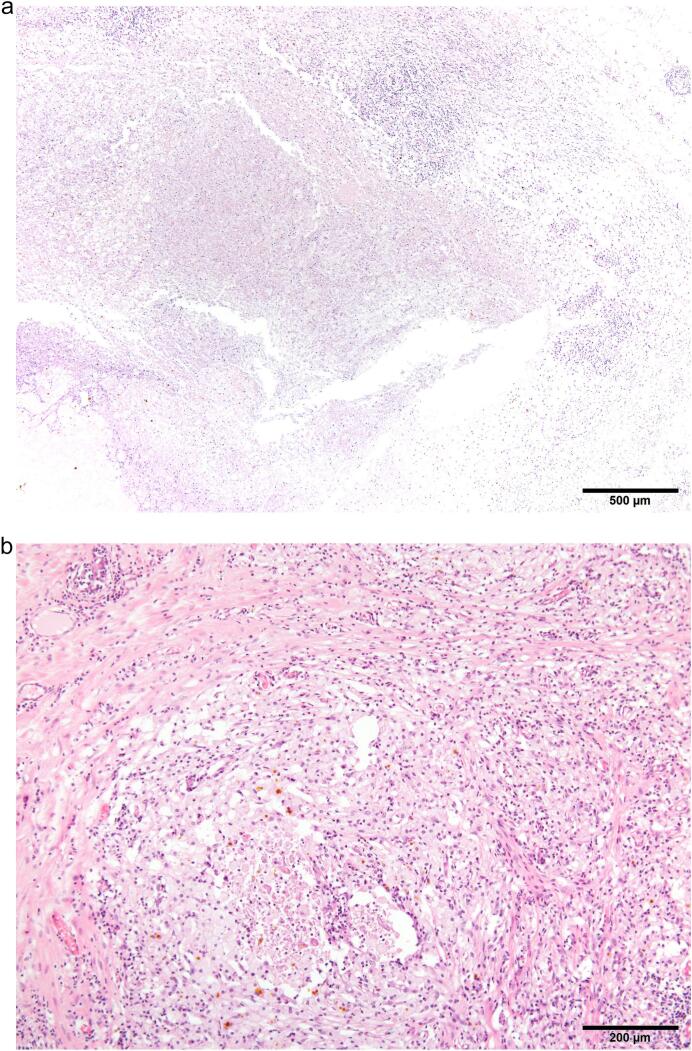
Ultrasound-guided core needle biopsy was performed. Histologically, large and small nuclei were present, and infiltrating and proliferating aberrant cells with conspicuous pleomorphism formed large alveoli. Nuclear atypia was grade 3. The tumor was estrogen receptor-negative, progesterone receptor-negative, and HER2-negative with a Ki-67 labeling index of 30 %. The diagnosis was invasive breast cancer (Fig. 2).
Fig. 2.
Aberrant infiltrating and proliferating cells with large and small nuclei and conspicuous pleomorphism forming large alveoli suggestive of invasive cancer.
Contrast-enhanced computed tomography (CT) showed a ring-enhancing mass (Fig. 3). No lymph node metastasis or metastasis to other organs was observed. Contrast-enhanced magnetic resonance imaging (MRI) showed a spherical nodule and a uniformly ring-enhancing tumor with an unclear border (Fig. 4).
Fig. 3.
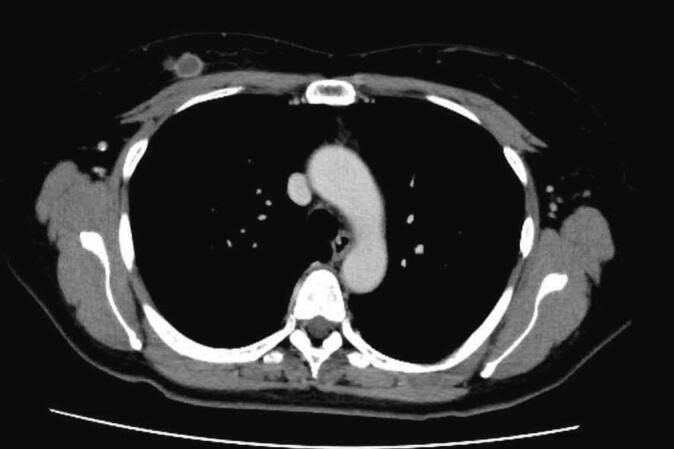
A ring-enhancing tumor is observed, but contrast enhancement is generally poor.
Fig. 4.
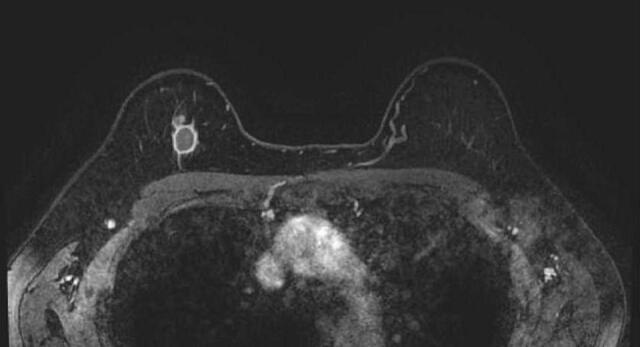
A homogeneously enhancing spherical nodule with an unclear border.
The patient was diagnosed with stage IIA T2N0M0 breast cancer, for which she underwent right partial mastectomy and sentinel lymph node biopsy. No metastases were found in the sentinel lymph nodes.
Macroscopically, the resected specimen had the appearance of a yellow, well-demarcated mass (Fig. 5). Histologically, the specimen contained an extensive area of necrotic tissue with foam cell aggregation, lymphocytic infiltration, and fibrosis in the periphery (Fig. 6a, b). No viable tumor cells were observed.
Fig. 5.

A well-demarcated yellow mass is observed.
Fig. 6.
a, b: Extensive necrotic tissue with peripheral foam cell aggregation, lymphocytic infiltration, and fibrosis. No viable tumor cells can be recognized.
Postoperative chemotherapy and radiation therapy were not administered at the patient's request. There has been no recurrence during 12 months of follow-up after surgery.
3. Discussion
Mammary gland infarction has been reported to occur frequently in benign tumors such as intraductal papilloma and fibroadenoma [2], [3] and in the mammary gland during pregnancy and lactation [4], [5], with a reported incidence of 0.5% [6]. However, infarct necrosis in breast cancer is very rare.
There have been some reports on partial infarct necrosis of breast cancer in Japan [7], [8], but this is the first report of complete necrosis of a malignant breast tumor.
The chief complaint in all the cases reported to date was a mammary mass, which was often accompanied by pain.
In terms of imaging findings, mammography and ultrasonography do not show any specific findings, but contrast-enhanced MRI or CT images may show ring-shaped hyperchromia, reflecting internal necrosis of the tumor [6]. On MRI in particular, extensive areas of no signal are observed. This is largely consistent with where necrosis is present pathologically, and the presence of no-signal areas on MRI may assist in the diagnosis of infarct necrosis.
In general, there are four causes of infarct necrosis to be considered: occlusion of feeding vessels as a result of lesions such as thromboembolism and vasculitis [9], [10]; relative ischemic necrosis associated with rapid proliferation of mammary gland cells during pregnancy and lactation [6], [11]; vascular occlusion caused by secondary vascular injury as a result of biopsy puncture [12]; and spontaneous regression associated with a tumor-specific immune mechanism.
In this case, thromboembolism and concurrent inflammatory cardiovascular disease were not observed, and pregnancy-related causes could be ruled out. What about the possibility of infarct necrosis associated with secondary vascular injury from biopsy puncture? Ultrasound examination performed before the biopsy showed blood flow inside the tumor, but a review of the histopathological tissue after surgery revealed generally low viability of the tumor cells in the biopsy specimen, and the possibility that the tumor had a strong tendency to be necrotic from the beginning was considered. Given that the tumor was painful at the time of the initial examination and that infiltration of lymphocytes was observed around the necrotic part of the tumor in the surgical specimen, it is likely that the necrosis had already started at the time of the initial examination, suggesting the presence of a tumor-specific immune mechanism. The sequence of events in this case suggests the possibility of natural disappearance of the tumor.
The choice of postoperative treatment was difficult in this case. The tumor tissue subtype on needle biopsy was triple-negative breast cancer, which would otherwise require chemotherapy. Furthermore, the patient had undergone a partial mastectomy, which would normally require radiotherapy to the remaining breast. The patient opted not to proceed with chemotherapy or radiotherapy, and after careful discussions with her, we accepted her wishes.
4. Conclusion
We have encountered a 53-year-old woman with complete infarct necrosis of breast cancer, which is very rare. Tumors that appear as ring-shaped enhancing lesions on contrast-enhanced MRI and CT may be caused by infarct necrosis.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Our institution does not require ethical approval for case reports that are deidentified and written retrospectively. Ethical Approval was waived by the authors institution.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Guarantor
Kimiyasu Yoneyama.
Research registration number
This is a case report, and no registration was required.
CRediT authorship contribution statement
Kimiyasu Yoneyama: Conceptualization, Investigation, Resources, Writing – Original draft preparation, Writing – Review and editing
Asuka Hara: Conceptualization, Investigation
Motohito Nakagawa: Administration, Review.
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Contributor Information
Kimiyasu Yoneyama, Email: key13213@yahoo.co.jp.
Aya Sasaki, Email: sasakiaya@tdc.ac.jp.
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Wadhwa N., Joshi R., Mangal N., Khan N.P., Joshi M. Cytopathologic diagnosis of spontaneous infarction of fibroadenoma of the breast. Turk. Patoloji Derd. 2014:237–240. doi: 10.5146/tjpath.2014.01224. [DOI] [PubMed] [Google Scholar]
- 3.Skenderi F., Krakonja F., Vranic S. Infarcted fibroadenoma of the breast: report of two new cases with review of the literature. Diagn. Pathol. 2013;8:38. doi: 10.1186/1746-1596-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosen P.P., Oberman H.A. Tumors of the Mammary Gland. Atlas of Tumor Pathology. Third Series, Fascicle 7. Armed Forces Institute of Pathology; Washington DC: 1993. pp. 26–27. [Google Scholar]
- 5.Jimenes J.F., Ryals R.O., Cohen C. Spontaneous breast infarction associated with pregnancy presenting as a palpable mass. J. Surg. Oncol. 1986;32:174–178. doi: 10.1002/jso.2930320311. [DOI] [PubMed] [Google Scholar]
- 6.Majmudar B., Rosales-Quintana S. Infarction of breast fibroadenomas during pregnancy. JAMA. 1975;231:963–964. [PubMed] [Google Scholar]
- 7.Nakanishi K., Takeuchi D., Tsushima Y., Hayashi H., Kikumori T. A case of breast cancer with infarcted necrosis. J. Jpn. Surg. Assoc. 2014;75:2707–2710. (in Japanese with English abstract) [Google Scholar]
- 8.Hosoi H., Iwai K., Watanabe M., Koinuma J., Hirano S. A case of solid tubular carcinoma of the breast with extensive infarction of the breast cancer. J. Jpn. Sug. Assoc. 2018;79:1396–1402. (in Japanese with English abstract) [Google Scholar]
- 9.Nudelman H.L., Kempson R.L. Necrosis of the breast: a rare complication of anticoagulant therapy. Am. J. Surg. 1966;111:728–733. doi: 10.1016/0002-9610(66)90051-1. [DOI] [PubMed] [Google Scholar]
- 10.Jordan J.M., Rowe W.T., Allen N.B. Wegener’s granulomatosis involving the breast: report of three cases and review of the literature. Am. J. Med. 1987;83:159–164. doi: 10.1016/0002-9343(87)90513-4. [DOI] [PubMed] [Google Scholar]
- 11.Lucey J.J. Spontaneous infarction of the breast. J. Clin. Pathol. 1975;28:937–943. doi: 10.1136/jcp.28.12.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee K.C., Chan J.K.C., Ho L.C. Histological changes in the breast after fine-needle aspiration. Am. J. Surg. Pathol. 1994;18:1039–1047. doi: 10.1097/00000478-199410000-00007. [DOI] [PubMed] [Google Scholar]