Abstract
Background
Insomnia has been closely associated with cardiovascular disease (CVD) including myocardial infarction (MI). Our study aims to assess the eligibility of insomnia as a potential risk factor for MI.
Methods
PubMed, Scopus, and Web of Science were searched using terms; such as “Insomnia” and “MI.” Only observational controlled studies with data on the incidence of MI among insomniacs were included. Revman software version 5.4 was used for the analysis.
Results
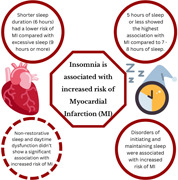
Our pooled analysis showed a significant association between insomnia and the incidence of MI compared with noninsomniacs (relative risk [RR] = 1.69, 95% confidence interval [CI] = 1.41–2.02, p < .00001). Per sleep duration, we detected the highest association between ≤5 h of sleep, and MI incidence compared to 7−8 h of sleep (RR = 1.56, 95% CI = 1.41–1.73). Disorders of initiating and maintaining sleep were associated with increased MI incidence (RR = 1.13, 95% CI = 1.04–1.23, p = .003). However, subgroup analysis of nonrestorative sleep and daytime dysfunction showed an insignificant association with MI among both groups (RR = 1.06, 95% CI = 0.91–1.23, p = .46). Analysis of age, follow‐up duration, sex, and comorbidities showed a significant association in insomniacs.
Conclusion
Insomnia and ≤5 h of sleep are highly associated with increased incidence of MI; an association comparable to that of other MI risk factors and as such, it should be considered as a risk factor for MI and to be incorporated into MI prevention guidelines.
Keywords: insomnia, myocardial infarction, sleep disorders, STEMI
1. INTRODUCTION
Insomnia is the most common sleep disorder and is known to negatively impact the general health of the population and the quality of life. 1 , 2 Due to its difficulty to treat, it has contributed to a significant socioeconomic burden on a global scale; as many of its sufferers have reported decreased productivity and absenteeism at work. 3 In the modern era, insomnia is becoming increasingly common with a prevalence of 10%–15% in the United States. 2
There have been multiple studies linking insomnia to the increased risk of cardiovascular and metabolic diseases. 4 , 5 Among insomniacs, there is an alteration of the hypothalamic‐pituitary‐adrenal axis with higher levels of adrenocorticotropic hormone (ACTH) and cortisol compared to healthy individuals. 6 Elevation of cortisol has been associated with myocardial infarction (MI); whereas individuals who suffered from an acute MI, have been shown to have higher levels of cortisol in the month preceding their MI compared with healthy individuals. 7 An experiment conducted on mice has shown that chronic stress and elevated cortisol led to the acceleration of atherosclerosis which could potentially lead to MI. 8 Insomniacs suffer from both chronic stress and elevated cortisol due to the lack of sleep, which exacerbates their risk of developing MI.
As of the time of writing this paper, Insomnia isn't considered a risk factor for MI 9 ; our study aims to analyze the current literature and assess the eligibility of insomnia as a risk factor for MI.
2. METHODS
The protocol for this paper was registered on PROSPERO (CRD42022348707) and the regulations of the preferred reporting items of systematic reviews and meta‐analyses (PRISMA) were followed. 10
2.1. Search strategy
A literature search of the following databases (PubMed, Scopus, and Web of Science) on May 17, 2022, using key terms such as “Insomnia,” “sleep complaints,” “sleep initiation,” “Myocardial Infarction,” “MI,” and “STEMI,” was performed to identify studies of interest. (View the supplementary material for the full search strategy).
2.2. Insomnia definition
Insomnia was defined according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM); codes 307.4 (a disorder of initiating or maintaining sleep) and 780.5 (insomnia, unspecified). We also utilized the Diagnostic and Statistical Manual of Mental Disorders (DSM‐5), which stated that insomnia is a sleep disorder characterized by the presence of any of the following three symptoms: (1) difficulty initiating sleep, (2) difficulty maintaining sleep, (3) early morning awakening with inability to return to sleep. 11 In addition to that, we included an objective measure of insomnia which is the sleep duration. 12 Obstructive sleep apnea (OSA) and other sleep apneas weren't included in our study.
2.3. Inclusion and exclusion criteria
We screened the studies according to the following criteria:
Inclusion criteria: Studies selected must be in the English language; controlled observational studies with data on the incidence of myocardial infarction among adults (≥18 years) suffering from insomnia, including cross‐sectional, case–control, and cohort studies were included.
Exclusion criteria: Editorials, commentaries, reviews, systematic reviews, meta‐analyses, case reports, case series, animal studies, studies without data about the risk of myocardial infarction in patients suffering from insomnia, and studies lacking a control group were excluded; in case of duplicate studies, the most recent study with the largest study population was included.
2.4. Study selection
Two independent reviewers (T.S. and M.A.) screened the studies according to our criteria. If a consensus is not achieved, a third independent reviewer (R.S.) was consulted to resolve the conflict.
2.5. Data extraction and quality assessment
Each study was extracted by two reviewers independently (R.E. and S.G.). The data was then compared to confirm accuracy. If a consensus is not achieved, a third independent reviewer (R.S.) was consulted to resolve the conflict.
For the baseline and summary, the following data were extracted from the eligible studies: the last name of the first author, year of publication, study design, number of participants, age of participants, sex of participants, average body mass index, the prevalence of smoking, the prevalence of alcohol, and baseline diseases.
For the outcomes, the following data were extracted: MI incidence, sleep duration, DIMS, nonrestorative sleep and daytime dysfunction, age, sex, hypertension, diabetes, and hyperlipidemia among insomnia and noninsomnia groups.
The risk of bias was assessed utilizing Newcastle‐Ottawa Scale (NOS) items, 13 with a total score of nine points, to evaluate the quality of observational studies. We defined the observational studies with a NOS score of ≥7 stars as high quality and NOS score of <7 stars as low quality.
3. RESULTS
3.1. Literature search
A complete search of the literature yielded 1226 studies, and after duplicate removal, there were 944 studies eligible for the title and abstract screening. Of the 944, 625 were irrelevant and 319 studies were eligible for full‐text screening. Finally, 9 14 , 16 , 17 , 18 , 19 , 20 , 21 , 22 studies were included in the meta‐analysis after the full‐text screening, as shown in the PRISMA diagram (Figure 1).
Figure 1.

PRISMA flow diagram showing the study selection process. Characteristics of the included studies.
The total number of patients included in the study is 1 184 256 patients; 153 881 patients in the insomnia group, and 1 030 375 patients in the noninsomnia group. A summary of the included studies and patients' baseline data are shown in Table 1. The overall quality of the included studies was high as shown in (Supporting Information: Table S1).
Table 1.
Baseline characteristics and summary of the included studies.
| Author (Year) | Country | Study design | Follow‐up duration (years) | Sample size | Age, mean (SD) | Male, no. (%) | Smoking, No. (%) | BMI, mean (SD) | Alcohol No. (%) | Baseline diseases | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chung 2013 | Taiwan | Prospective | 9–13 | 147 297 | 51.3 (16.7) | 53 547 | ‐ | ‐ | ‐ | DM | This nationwide population‐based cohort study provides evidence that patients with non‐apnea sleep disorders are at higher risk of |
| HTN | |||||||||||
| Hyperlipidemia | developing acute coronary syndrome. | ||||||||||
| Cohort | COPD | ||||||||||
| CVA | |||||||||||
| Elwood 2006 | UK | Prospective Cohort | 10 | 1874 | ‐ | 1874 (100) | 637 | 26.8 (3.7) | ‐ | ‐ | The risk of an ischemic stroke is increased in men whose sleep is frequently disturbed, and |
| (34) | |||||||||||
| daytime sleepiness is associated with a significant increase in ischemic heart disease events. | |||||||||||
| Hsu 2015 | Taiwan | Prospective Cohort | 10 | 44 080 | 47.7 (15.7) | 18 912 (42.9) | ‐ | ‐ | ‐ | Hyperlipidemia | Insomnia is associated with an increased risk of future cardiovascular events. |
| HTN | |||||||||||
| Depression | |||||||||||
| CPD | |||||||||||
| PAD | |||||||||||
| CHF | |||||||||||
| CKD | |||||||||||
| CAD | |||||||||||
| DM | |||||||||||
| Hyperlipidemia | |||||||||||
| Laugsand | Norway | Prospective Cohort | 11.4 | 51 982 | 49.4 (16.8) | 23 226 (44.6) | 14 611 (28.1) | 26.3 (4.0) | 29 278 (56.3) | DM | Insomnia is associated with a moderately increased risk for AMI. |
| HTN Dyslipidemia | |||||||||||
| Depression | |||||||||||
| Anxiety | |||||||||||
| Meisinger 2007 | Germany | Prospective Cohort | 10.1 | 6896 | 57.4 (8.0) | 3508 (50.8) | 1250 (18.1) | 27.7 (4.1) | 4692 (68.0) | Dyslipidemia | Modest associations between short sleep duration and |
| HTN Depression | |||||||||||
| difficulties maintaining sleep and incident MI were seen in middle‐aged | |||||||||||
| DM | |||||||||||
| women but not men from the general population. | |||||||||||
| Schwartz 1998 | US | Prospective Cohort | 3 | 2960 | 73 | 993 (33.5) | 518 (17.5) | ‐ | ‐ | DM | A subjective sleep complaint increases the likelihood of a first MI in older adults |
| HTN | |||||||||||
| without overt coronary heart disease independently of classic coronary risk factors and appears | |||||||||||
| Obesity | |||||||||||
| to be a marker for a syndrome of depression and malaise that may have a causal relationship to MI. | |||||||||||
| Zheng 2019 | China | Prospective Cohort | 9.6 | 487 200 | 51.0 | 199 241 (40.9) | 130 335 (26.7) | 23.6 | 73 634 (15.1) | HTN | Individual and coexisting insomnia symptoms are independent risk factors for CVD incidence, |
| DM | |||||||||||
| Anxiety Depression | especially among young adults or adults who have not developed hypertension. | ||||||||||
| Daghlas 2019 | UK | Prospective Cohort | 7.04 | 461 347 | ‐ | ‐ | ‐ | ‐ | ‐ | Hypothyroidism Hyperthyroidism | Prospective observational and MR analyses support short sleep duration as a potentially causal risk factor for MI. Investigation of sleep extension to prevent MI may be warranted. |
| Migraine | |||||||||||
| Rheumatoid Arthritis | |||||||||||
| Osteoarthritis | |||||||||||
| Deep vein thrombosis | |||||||||||
| COPD | |||||||||||
| Kalmbach 2016 | US | Cross‐sectional | ‐ | 3911 | 46.0 (13.3) | 1357 (34.7) | ‐ | 28.1 | ‐ | DM | Insomnia disorder with short sleep is the most severe phenotype of insomnia and comorbid with many cardiometabolic and psychiatric |
| HTN | |||||||||||
| Hyperlipidemia | |||||||||||
| (6.4) | |||||||||||
| illnesses, whereas morbidity profiles are highly similar between insomniacs with normal sleep duration and former insomniacs. | |||||||||||
Abbreviations: AMI, acute myocardial infarction; BMI, body mass index; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CPD, chronic pulmonary disease; CVA, cerebrovascular disease; DM, diabetes mellitus; HTN, hypertension; MI, myocardial infarction; MR, Mendelian randomization; No., number; PAD, peripheral artery disease; SD, standard deviation.
3.2. Outcomes
3.2.1. MI incidence (insomnia vs. noninsomnia)
Our pooled analysis revealed a statistically significant association between insomnia and an increased incidence of MI. Patients with insomnia were at 1.69 times greater risk for the development of MI (relative risk [RR] = 1.69, 95% confidence interval [CI] = 1.41–2.02, p < .00001). We detected a significant heterogeneity among studies (p < .00001, I 2 = 90%) that was not solved by the leave‐one‐out test, Figure 2.
Figure 2.

Forest plot of the comparison between insomnia and the incidence of MI. MI, myocardial infarction.
3.2.2. MI incidence and sleep duration
a. Five hours or less versus 6 h
Our pooled analysis revealed a statistically significant association between sleep duration and increased incidence of MI. Patients who slept 5 h or less were at 1.38 times greater risk for MI (RR = 1.38, 95% CI = 1.23–1.54, p < .00001) compared to patients who slept 6 h. We observed no heterogeneity among studies (p = .61, I 2 = 0%), Figure 3A.
Figure 3.

Forest plot of the comparison between sleep duration and the incidence of MI. MI, myocardial infarction.
b. 5 hours or less versus 7–8 h
Our pooled analysis revealed a statistically significant association between sleep duration and increased incidence of MI. Patients who slept 5 h or less were at 1.56 times greater risk for MI (RR = 1.56, 95% CI = 1.41–1.73, p < .00001) compared to patients who slept 7–8 h. We observed no heterogeneity among studies (p = .57, I 2 = 0%), Figure 3B.
c. 5 hours or less versus 9 h or more
Our pooled analysis showed no statistically significant difference between 5 h or less and 9 h or more of sleep regarding the incidence of MI (RR = 1.04, 95% CI = 0.92–1.17, p = .57). We observed no heterogeneity among studies (p = .67, I 2 = 0%), Figure 3C.
d. 6 hours versus 7–8 h
Our pooled analysis revealed a statistically significant association between sleep duration and increased incidence of MI. Patients who slept 6 h were at 1.14 times greater risk for MI (RR = 1.14, 95% CI = 1.06–1.22, p = .0002) compared to patients who slept 7–8 h. We observed no heterogeneity among studies (p = .15, I 2 = 52%), Figure 3D.
e. 6 hours versus 9 h or more
Our pooled analysis revealed a statistically significant association between 9 h or more of sleep duration and an increased incidence of MI. Patients who slept 6 h were at decreased risk of myocardial infarction compared to patients who slept 9 or more hours (RR = 0.75, 95% CI = 0.68–0.83, p < .00001). We observed no heterogeneity among studies (p = .89, I 2 = 0%), Figure 3E.
f. 7–8 hours versus 9 h or more
Our pooled analysis revealed a statistically significant association between 9 h or more of sleep and an increased incidence of MI. Patients who slept 7–8 h were at decreased risk of myocardial infarction compared to patients who slept 9 or more hours (RR = 0.67, 95% CI = 0.61–0.73, p < .00001). We observed no heterogeneity among studies (p = .15, I 2 = 52%), Figure 3F.
3.2.3. Subgroup analysis of the follow‐up duration (≤5 years vs. >5 years)
In the subgroup of “follow‐up ≤5 years,” the pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI (RR = 1.52, 95% CI = 1.17–1.97, p = .002), with no heterogeneity among studies (p = .82, I 2 = 0%), Figure 4.
Figure 4.

Forest plot of insomnia and the incidence of MI comparison between ≤5 years versus >5 years follow‐up duration subgroups. MI, myocardial infarction.
In the subgroup of “follow‐up >5 years,” the pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI (RR = 1.76, 95% CI = 1.42–2.17, p < .00001), with significant heterogeneity among studies (p < .00001, I 2 = 94%) that was not solved by the leave‐one‐out test, Figure 4.
3.3. DIMS subgroup
Our pooled analysis showed a statistically significant association between DIMS and increased incidence of MI. Patients with DIMS had 1.13 times greater risk for MI compared to the control group (RR = 1.13, 95% CI = 1.04–1.23, p = .003), with no observed heterogeneity among studies (p = .58, I 2 = 0%) (Supporting Information: Figure S1).
3.3.1. Nonrestorative sleep and daytime dysfunction subgroup
Our pooled analysis showed no statistically significant difference between the nonrestorative sleep and daytime dysfunction group and control group regarding the incidence of MI (RR = 1.06, 95% CI = 0.91–1.23, p = .46). We observed no heterogeneity among studies (p = .57, I 2 = 0%) (Supporting Information: Figure S1).
3.3.2. Age (<65 vs. ≥65 years subgroups)
In the <65 years age subgroup, our pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI compared with the control group (RR = 1.68, 95% CI = 1.40–2.02, p < .00001), with significant heterogeneity among studies (p < .00001, I 2 = 89%) that was not solved by the leave‐one‐out test (Supporting Information: Figure S2).
In the ≥65 years age subgroup, our pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI (RR = 2.06, 95% CI = 1.52–2.79, p < .00001), with significant heterogeneity among studies (p = .12, I 2 = 60%) (Supporting Information: Figure S2).
3.4. Sex subgroups
In the male subgroup, our pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI (RR = 2.03, 95% CI = 1.78–2.33, p < .00001), with no significant heterogeneity among studies (p = .82, I 2 = 0%) (Supporting Information: Figure S3).
In the female subgroup, our pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI (RR = 2.24, 95% CI = 1.54–3.25, p < .0001), with no significant heterogeneity among studies (p = .08, I 2 = 68%) (Supporting Information: Figure S3).
3.5. Comorbidities subgroups
In the hypertension subgroup, the pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI (RR = 1.84, 95% CI = 1.16–2.90, p = .009), with significant heterogeneity among studies (p = .006, I 2 = 87%) (Supporting Information: Figure S4).
In the diabetes subgroup, our pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI (RR = 2.06, 95% CI = 1.05–4.04, p = .04), with significant heterogeneity among studies (p = .006, I 2 = 87%) (Supporting Information: Figure S4).
In the hyperlipidemia subgroup, our pooled analysis revealed a statistically significant association between insomnia and increased incidence of MI (RR = 1.76, 95% CI = 1.04–2.99, p = .04), we detected a significant heterogeneity among studies (p = .03, I 2 = 79%) (Supporting Information: Figure S4).
4. DISCUSSION
Our study demonstrates that insomniacs are at a higher risk of developing MI relative to noninsomniacs. According to the DSM‐5 criteria of insomnia, DIMS was significantly associated with a higher risk of MI, while nonrestorative sleep and daytime dysfunction yielded an insignificant association. Per sleep duration, patients who slept 5 h or less had the highest association with MI incidence, compared to those who slept 7−8 h. Longer sleep duration (9 h or more) wasn't protective against MI; quite to the contrary, patients who slept 6 h were at a lower risk of MI, compared to those who slept 9 h or more. Subgroup analysis of the follow‐up duration revealed that both short (5 years or less) and long (more than 5 years) durations were associated with a significant increase in the risk of MI. Both male and female insomniacs were at a higher risk of MI compared with noninsomniacs. Lastly, the presence of insomnia in addition to a comorbid disease (hypertension, dyslipidemia, or diabetes) was associated with a higher risk of MI.
Concerning the current literature and its accordance with our results, Sofi et al. 23 in their meta‐analysis, have shown that insomnia is associated with an increased risk of cardiovascular morbidity and mortality (RR = 1.45, 95% CI = 1.29−1.62). It is important to note that their search was up to 2011, and it only included 122 501 individuals; since then, multiple controlled observational studies have been published regarding this matter. After the inclusion of these studies, we managed to reach a sample size of 1, 184, 256 and analyze individual insomnia symptoms and various sleep durations.
Our results support Hu et al. 24 findings which concluded that DIMS is associated with a higher risk of CVD including myocardial infarction. On the other hand, they reported that non‐restorative sleep is significantly associated with a higher risk of CVD. This finding contradicts our subgroup analysis which showed that nonrestorative sleep and daytime dysfunction are associated with an insignificant increase in the risk of MI. Another study conducted by He et al. 25 reported a similar finding that nonrestorative sleep is associated with a higher risk of cardio‐cerebral vascular events.
Regarding sleep duration, Chandola et al. 26 stated that a short sleep duration of 5 h, wasn't significantly associated with an increased risk of coronary artery disease (CAD) including MI. This opposes our results, as we reported that sleeping 5 h or less is highly associated with an increased risk of MI compared to those who slept 7−8 h. Our findings are reinforced by Ayas et al. 27 and Nagi et al. 28 who concluded that a sleep duration of 5 h or less is associated with a higher risk of developing CAD. Our analysis has shown that longer sleep durations of 9 h or more could lead to an increased incidence of MI; a similar conclusion was demonstrated by Jike et al., 29 in their meta‐analysis, which showed that long sleep hours are associated with a higher risk of CAD (RR = 1.24, 95% CI = 1.13–1.37).
Miguel‐Yanes et al. 30 and Alkhouli et al. 31 reported that MI incidence was higher among men. Our study reported that among insomniacs, there is an increased risk of MI in both men and women. Notwithstanding, the risk of MI in our study was higher among female insomniacs.
Our study showed that regardless of age, insomniacs are associated with a higher risk of MI. Lian et al. 32 cross‐sectional study reinforce our findings; they concluded that short sleep duration is associated with a higher risk of MI in patients <65 and >65 years old. Older age is usually associated with a higher risk of MI 33 ; this is supported by the findings in our study.
4.1. Strengths
Our study has a cohort of 1 184 256 individuals, originating from six different countries (United States, United Kingdom, Norway, Germany, Taiwan, and China) and three different continents, increasing the generalizability of our findings. All of our nine included studies are controlled; eight of them are prospective cohorts; this allows us to establish causality and consider insomnia as a risk factor for MI. Additionally, we performed a subgroup analysis according to the confounding factors (age, sex, and comorbidities); enabling us to reach a stronger conclusion. Another subgroup analysis based on individual insomnia symptoms and sleep duration was conducted, to reach a more individualized conclusion that can be applied to patients suffering from different symptoms of insomnia.
4.2. Limitations
There was significant heterogeneity among the included studies; this could be attributed to the different sample sizes, ages, and follow‐up duration.
In most studies, data were obtained from questionnaires, therefore, biases may have occurred due to misinterpretation of the questions proposed.
Finally, research papers that were published in any language other than English (e.g., Chinese) were excluded and thus were not a part of the Systematic Review and Meta‐analysis.
5. CONCLUSION AND POLICY IMPLICATIONS
Insomnia has been significantly associated with an increased incidence of myocardial infarction. Subsequently, insomnia should be integrated into guidelines on the primary prevention of cardiovascular disease.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Supporting information
Supporting information.
Supporting information.
Supporting information.
Dean YE, Shebl MA, Rouzan SS, et al. Association between insomnia and the incidence of myocardial infarction: a systematic review and meta‐analysis. Clin Cardiol. 2023;46:376‐385. 10.1002/clc.23984
DATA AVAILABILITY STATEMENT
Data available upon request from the corresponding author.
REFERENCES
- 1. Darchia N, Oniani N, Sakhelashvili I, et al. Relationship between sleep disorders and health related quality of life‐results from the Georgia SOMNUS study. Int J Environ Res Public Health. 2018;15(8):1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kaur H, Spurling BC, Bollu PC. Chronic insomnia. StatPearls [Internet]. StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK526136/ [PubMed] [Google Scholar]
- 3. Hui SA, Grandner MA. Trouble sleeping associated with lower work performance and greater health care costs: longitudinal data from Kansas state employee wellness program. J Occup Environ Med. 2015;57(10):1031‐1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Deschênes SS, Burns RJ, Graham E, Schmitz N. Depressive symptoms and sleep problems as risk factors for heart disease: a prospective community study. Epidemiol Psychiatric Sci. 2019;29:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grandner MA, Jackson NJ, Pak VM, Gehrman PR. Sleep disturbance is associated with cardiovascular and metabolic disorders. J Sleep Res. 2012;21(4):427‐433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vgontzas AN, Tsigos C, Bixler EO, et al. Chronic insomnia and activity of the stress system. J Psychosom Res. 1998;45(1):21‐31. [DOI] [PubMed] [Google Scholar]
- 7. Faresjö T, Strömberg S, Jones M, et al. Elevated levels of cortisol in hair precede acute myocardial infarction. Sci Rep. 2020;10(1):22456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Okutsu M, Lira VA, Higashida K, Peake J, Higuchi M, Suzuki K. Corticosterone accelerates atherosclerosis in the apolipoprotein E‐deficient mouse. Atherosclerosis. 2014;232(2):414‐419. [DOI] [PubMed] [Google Scholar]
- 9. Anand SS, Islam S, Rosengren A, et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur Heart J. 2008;29(7):932‐940. [DOI] [PubMed] [Google Scholar]
- 10. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. American Psychiatric Association . Diagnostic and Statistical Manual for Mental Disorders DSM‐IIIR. American Psychiatric Association; 1987:3‐24. [Google Scholar]
- 12. Vgontzas AN, Fernandez‐Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17(4):241‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stang A. Critical evaluation of the Newcastle‐Ottawa scale for the assessment of the quality of nonrandomized studies in meta‐analyses. Eur J Epidemiol. 2010;25(9):603‐605. [DOI] [PubMed] [Google Scholar]
- 14. Chung WS, Lin CL, Chen YF, et al. Sleep disorders and increased risk of subsequent acute coronary syndrome in individuals without sleep apnea: a nationwide population‐based cohort study. Sleep. 2013;36(12):1963‐1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Daghlas I, Dashti HS, Lane J, et al. Sleep duration and myocardial infarction. JACC. 2019;74(10):1304‐1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Elwood P. Sleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohort. J Epidemiol Community Health. 2006;60(1):69‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hsu CY, Chen YT, Chen MH, et al. The association between insomnia and increased future cardiovascular events: a nationwide population‐based study. Psychosom Med. 2015;77(7):743‐751. [DOI] [PubMed] [Google Scholar]
- 18. Kalmbach DA, Pillai V, Arnedt JT, Drake CL. DSM‐5 insomnia and short sleep: comorbidity landscape and racial disparities. Sleep. 2016;39(12):2101‐2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Laugsand LE, Vatten LJ, Platou C, Janszky I. Insomnia and the risk of acute myocardial infarction: a population study. Circulation. 2011;124(19):2073‐2081. [DOI] [PubMed] [Google Scholar]
- 20. Meisinger C, Heier M, Löwel H, Schneider A, Döring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle‐aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Sleep. 2007;30(9):1121‐1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schwartz SW, Cornoni‐Huntley J, Cole SR, Hays JC, Blazer DG, Schocken DD. Are sleep complaints an independent risk factor for myocardial infarction? Ann Epidemiol. 1998;8(6):384‐392. [DOI] [PubMed] [Google Scholar]
- 22. Zheng B, Yu C, Lv J, et al. Insomnia symptoms and risk of cardiovascular diseases among 0.5 million adults: a 10‐year cohort. Neurology. 2019;93(23):e2110‐e2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF. Insomnia and risk of cardiovascular disease: a meta‐analysis. Eur J Prev Cardiol. 2014;21(1):57‐64. [DOI] [PubMed] [Google Scholar]
- 24. Hu S, Lan T, Wang Y, Ren L. Individual insomnia symptom and increased hazard risk of cardiocerebral vascular diseases: a meta‐analysis. Front Psychiatry. 2021;12:654719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. He Q, Zhang P, Li G, Dai H, Shi J. The association between insomnia symptoms and risk of cardio‐cerebral vascular events: a meta‐analysis of prospective cohort studies. Eur J Prev Cardiol. 2017;24(10):1071‐1082. [DOI] [PubMed] [Google Scholar]
- 26. Chandola T, Ferrie JE, Perski A, Akbaraly T, Marmot MG. The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort. Sleep. 2010;33(6):739‐744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205‐209. [DOI] [PubMed] [Google Scholar]
- 28. Nagai M, Hoshide S, Kario K. Sleep duration as a risk factor for cardiovascular disease—a review of the recent literature. Curr Cardiol Rev. 2010;6(1):54‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jike M, Itani O, Watanabe N, Buysse DJ, Kaneita Y. Long sleep duration and health outcomes: a systematic review, meta‐analysis and meta‐regression. Sleep Med Rev. 2018;39:25‐36. [DOI] [PubMed] [Google Scholar]
- 30. de Miguel‐Yanes JM, Jiménez‐García R, Hernandez‐Barrera V, et al. Sex differences in the incidence and outcomes of acute myocardial infarction in Spain, 2016‐2018: a matched‐pair analysis. J Clin Med. 2021;10(8):1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alkhouli M, Alqahtani F, Jneid H, Al Hajji M, Boubas W, Lerman A. Age‐stratified sex‐related differences in the incidence, management, and outcomes of acute myocardial infarction. Mayo Clin Proc. 2021;96(2):332‐341. [DOI] [PubMed] [Google Scholar]
- 32. Lian X, Gu J, Wang S, et al. Effects of sleep habits on acute myocardial infarction risk and severity of coronary artery disease in Chinese population. BMC Cardiovasc Disord. 2021;21(1):481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bhatnagar P, Wickramasinghe K, Williams J, Rayner M, Townsend N. The epidemiology of cardiovascular disease in the UK 2014. Heart. 2015;101(15):1182‐1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
Data available upon request from the corresponding author.


