Abstract
The COVID-19 pandemic provides both reasons to quit smoking as well as stress that may promote increased cigarette consumption. Perceptions of COVID-19 risk related to smoking may motivate cessation among smokers. At the same time, other evidence shows that affective perceptions (i.e., worry) could lead to increased smoking as a coping mechanism. Using a sample drawn from a rural region of California (N = 295), we examined the relationship between perceptions about health risks for smokers during the pandemic and both reported increases in smoking frequency and intentions to quit smoking. We also examined whether worry about health risks mediated these relationships. High perceived risk was associated both with reported increases in smoking frequency as well as greater intentions to quit smoking. Worry partially mediated both these relationships, with worry accounting for 29.11% of the variance in the relationship between high risk perceptions and increased smoking as well as 20.17% of the relationship between risk perceptions and intentions to quit smoking. These findings suggest that while smokers’ awareness about their increased risk of COVID-19 can motivate intent to quit smoking in the future, smokers may require greater support to act on these intentions.
Keywords: Smoking, Tobacco, Risk Perceptions, COVID-19, Worry
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic remains at the forefront of public concern, even now more than two years since its emergence. (Coronavirus Disease, 2019) However, while COVID-19 motivated global efforts to mitigate this recent threat to public health, the global tobacco epidemic continues. Currently, smokers stand at the intersection of two respiratory-related pandemics. (CDC, 2020) It is important to understand smokers’ perceptions of their tobacco use during the COVID-19 pandemic, and how these perceptions relate to changes in smoking behavior.
1.1. COVID-19 may impact Tobacco use
Smoking and e-cigarette use may increase susceptibility to and severity of COVID-19, (Gaiha et al., 2020, Benowitz et al., 2022, Nishimura et al., 2023) but it is unclear whether smokers understand their increased risk. Health behavior theories suggest that high risk perceptions deter risk behaviors and promote protective health behaviors. (Rosenstock, 1974, Ajzen, 1991) In the context of smoking and COVID-19, we would expect that those who believe that smoking increases the risks associated with COVID-19 to be more motivated to reduce or quit smoking.
A large body of work shows that perceptions of risk are related to intentions to quit smoking (Borrelli et al., 2010) and smoking frequency. (Hampson et al., 2006) Emerging research has sought to understand the relationship between risk perceptions and smoking during the COVID-19 pandemic, but results have not been consistent. On the one hand, perceived vulnerability to COVID-19 predicts successful smoking cessation and decrease in smoking consumption. (Rigotti et al., 2021, Vogel et al., 2021) However, perceived susceptibility to COVID-19 also predicts increases in smoking. (Vogel et al., 2021) The contradictory role perceived susceptibility plays in smoking cessation and consumption may be due to an interplay between perceptions and affect. Affective influences on risk perceptions, such as worry, are often overlooked (Ferrer and Klein, 2015) but may play an important role in smoking behavior during the pandemic.
To this end, there is an abundance of literature linking stress levels, including mortality related stress, with smoking behaviors. (Arndt and Goldenberg, 2017) Americans report being exposed to high levels of pandemic-related stressors, (Kontoangelos et al., 2020) and are engaging in a variety of coping behaviors, including substance use. (Czeisler, 2020) Some emerging research on smoking behaviors are in line with these trends; despite desires to quit, some smokers did not change their smoking behavior (Gravely et al., 2021) or consumed more cigarettes during the pandemic. (Klemperer et al., 2020, Gonzalez et al., 2021 Jan) Worry in particular may explain smoking behaviors beyond risk perceptions alone. (Magnan, 2017) Some models include worry as a mediator between risk perceptions and smoking outcomes, concluding that risk perceptions increase worry, and worry influences behavior. (Emery et al., 2014) Indeed, general worry about contracting COVID-19 was associated with thinking about quitting smoking. (Gravely et al., 2021) The COVID-19 pandemic may simultaneously serve as both a motivator to quit and a stressor associated with increased cigarette consumption.
The aim of current study is to examine factors that may contribute to smokers’ behavior during the COVID-19 pandemic. Our work is primarily guided by the tenants of the Conditional Risk Assessment Model (Millstein and Halpern-Felsher, 2002) wherein hypothetical questions with specific framing (i.e., smoking during COVID-19) are used to assess perceived risk. (Fritz and MacKinnon, 2007) Similarly, worry about these risks can also be framed in terms of specific contexts. (Millstein and Halpern-Felsher, 2002)The aim of the current study differs from previous research in that we are specifically interested in whether smokers believed their smoking behaviors are related to their risks for COVID-19, and whether that belief is related to intentions to quit smoking.
Understanding smoking behavior during this time is particularly important for regions that struggle with limited medical resources (Cornelius, 2019) and pre-existing health disparities, (Kayhan Tetik et al., 2020, Yach, 2020) such as California’s San Joaquin Valley. Therefore, we collected our community sample from this largely under-resourced area of California to address the following questions: 1) Do perceptions of COVID-19 smoking risk relate to self-reported changes in smoking behavior?; and 2) Do smokers’ affective perceptions (i.e. worry) of the risks of smoking during the COVID-19 pandemic relate to intentions to quit and smoking consumption? We hypothesized that perceptions of COVID-19 smoking risks and worry relate to greater intentions to quit smoking, but that only worry relates to smoking consumption.
2. Methods
2.1. Sample
The current sample was drawn from California’s San Joaquin Valley, a region that is largely rural and under-resourced. (Battalio et al., 2021) The Nicotine and Cannabis Policy Center at the University of California, Merced is dedicated to providing evidence-based research and support for 11 counties of the region, including Calaveras, Fresno, Kern, Kings, Madera, Mariposa, Merced, San Joaquin, Stanislaus, Tulare, and Tuolumne counties. (Parker et al., 2020).
Our community sample was recruited through community organizations, selective Facebook ads, and smoker forums and comment boards. Participants were directed to an informed consent form prior to proceeding to the Qualtrics survey. Via Qualtrics, we were able to block multiple responses from the same IP address and included a captcha to prevent responses from automated programs. Participants were eligible if they were over 18 years old and if they had smoked in the past three months. Participants received a $5.00 Amazon gift card upon study completion. All research procedures were reviewed and approved by the University of California, Merced’s Institutional Review Board (UCM2019-63).
Data were collected June 19th-20th, 2020; during this period, California issued a mask mandate and COVID hospitalizations were continuing to rise. Approximately 345 participants responded during our data collection window; however, participants were excluded from the analyses if they were missing data on our variables of interest (n = 50). Our final analyses included 295 participants.
3. Measures
Demographic Variables: The demographic measures that we included in our model were gender (male = 0), age, household income (0 = below $50,000; 1 = above $50,000), and race/ethnicity (0 = Non-Hispanic White; 1 = Other).
Tobacco consumption: Participants were asked to report the number of cigarettes they smoked per day and whether they believed they were now smoking more or less since the start of the pandemic (0 = smoke same or less; 1 = smoke more). They were also asked about whether they planned to quit smoking in the next 30 days (0 = no; 1 = yes) and their general confidence in their ability to quit smoking (0 = not confident; 1 = neutral; 2 = confident).
Smoking Attitudes: Participants were asked six questions to assess risk perceptions of and worry about the link between smoking and COVID-19 outcomes (see Table 1). Consistent with prior research, (Fritz and MacKinnon, 2007) a principal components analysis (PCA) with orthogonal varimax rotation indicated that the six items loaded onto two factors. Factor 1 consisted of four perceptions of COVID-19 smoking attitude items, while factor 2 consisted of two worry items. The two factors accounted for 81.14% of the total variance in the items, with the first responsible for 59.64% and the second responsible for an additional 21.50%. Based on the principal components analysis, we generated two mean composite scores, where higher scores on our smoking attitudes scale indicated higher perceptions of COVID-19 and smoking risk and greater worry.
Table 1.
COVID-19 and Smoking Attitudes.
| Items | Scale | Mean (SD) |
|---|---|---|
| Smoking Attitudes | ||
|
Definitely not (0) – Definitely yes (4) | 1.64 (1.22) |
|
Definitely not (0) – Definitely yes (4) | 1.79 (1.20) |
|
Definitely not (0) – Definitely yes (4) | 1.81 (1.28) |
|
Definitely not (0) – Definitely yes (4) | 1.86 (1.18) |
| Worry | ||
|
Not at all worried (0) – Extremely worried (4) | 1.86 (0.94) |
|
Not at all worried (0) – Extremely worried (4) | 1.93 (0.99) |
3.1. Statistical analyses
We tested two separate structural equation models (SEM) to determine if smoking attitudes specific to COVID-19 are related to changes in smoking behavior, namely 1) whether the smoker believes their smoking had increased since the start of COVID-19 lockdowns and 2) whether they had plans to quit in the next 30 days. Our models further tested a potential mediation effect to determine if worry mediated the relationship between our smoking attitude items and smoking behaviors. Both models controlled for gender, race/ethnicity, nicotine dependence, confidence in quitting smoking, and income. A small subset of our participants (n = 29) reported that they had smoked in the last 3 months, but not the last 30 days. These recent quitters are excluded in our second model as they had already been abstinent for at least 30 days. They were also excluded if they did not complete the outcome measure of interest (n = 5) for a total of 261 participants. The PCA was conducted using Stata 15.1 and SEM analyses were conducted using Mplus 8.4. Based on previous literature, our sample size was appropriate assuming a small-to-medium effect size between smoking attitudes and our outcomes (Attebring et al., 2001).
4. Results
The majority of the sample was male (86.44%) and non-Hispanic White (72.64%), which does not reflect regional demographics, but smokers in general are more likely to be male and non-Hispanic.(29) Our participants were 33.31 years old on average, and 84.80% reported an annual household income of more than $50,000. Almost half of our sample reported smoking more since the start of the COVID-19 lockdown (n = 136, 45.95%). Of our participants who reported smoking in the last 30 days (n = 261), 38.31% (n = 100) report that they plan to quit within the next month.
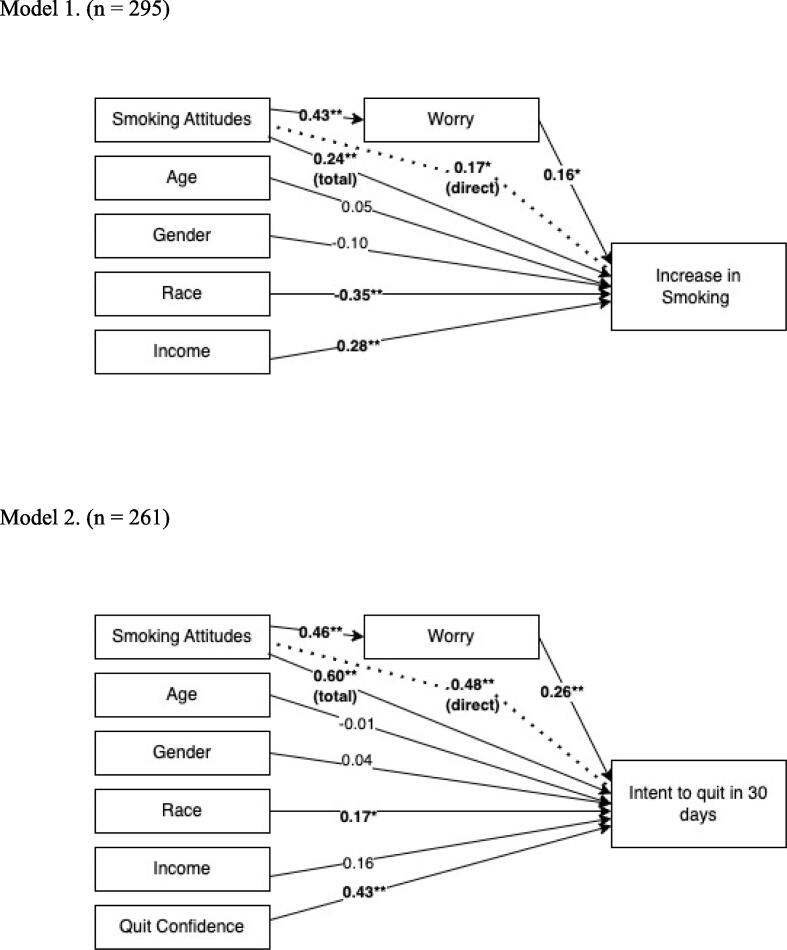
We assessed two path models used to predict either perceptions that smoking had increased since COVID-19 lockdowns had begun or intentions to quit smoking in the next 30 days. Diagrams of our path analyses and standardized beta coefficients are detailed in Fig. 1.
Fig. 1.
Models predicting self-reported changes in smoking behavior and intentions to quit.Note. values represent the standardized beta coefficients, significance of p 0.05 is indicated by * and p
COVID-19 smoking attitudes, worry about smoking and COVID-19, race, and income were all significant predictors of self-reported increased smoking behavior. Those of higher income were more likely to report increased smoking and our non-white participants were less likely to report increased smoking. As for the psychological items, recognizing a stronger link between smoking and COVID-19 outcomes and worry both independently predicted increased smoking behavior. Worry partially mediated the link between attitudes and greater increases in smoking, with stronger attitudes leading to greater worry, and greater worry relating to smoking increase. The indirect effect of worry (β = 0.069, SE = 0.31) accounted for 29.11% of the total relationship between COVID-19 smoking perceptions and smoking increase (β = 0.237, SE = 0.07).
Our second model we used to predict intentions to quit smoking in the next 30 days is nearly identical to the first, besides the addition of a confidence in quitting variable. Greater confidence, race, COVID-19 smoking attitudes, and worry all independently predicted intentions to quit smoking in the next 30 days. Again, worry acted as a partial mediator between COVID-19 smoking attitudes and our outcome, intent to quit smoking. Perceived risks of COVID-19/smoking are related to greater worry and greater intentions to quit smoking in the next 30 days. The indirect effect of worry (β = 0.121, SE = 0.03) accounted for 20.17 % of the total relationship between COVID-19/smoking perceptions and intent to quit smoking (β = 0.60, SE = 0.06).
5. Discussion
While perceptions of COVID-19/smoking risk and worry are related to greater intentions to quit, they are also related to increases in cigarette consumption (Hypothesis 1 and 2). Worry also mediated the relationship between COVID-19 smoking risk and increases in cigarette consumption as well as intent to quit (Hypothesis 3). This suggests that awareness of the link between smoking and COVID-19 is related to increased worry, and this increased worry may be related to increased smoking, despite desires to quit.
This current study joins a growing body of evidence that shows perceptions of smoking and COVID-19 are related to intentions to quit smoking (Klemperer et al., 2020, Kayhan Tetik et al., 2020, Yach, 2020), however, worry partially mediated this effect. (Ajzen, 1991) While risk perceptions and worry may motivate desire to change in the future, the need to cope with negative affect could lead to increased smoking. (Arndt and Goldenberg, 2017) If this is the case, education about the risks of smoking during the pandemic should include information about positive coping alternatives. Our study is the first to test worry as a mediator in the context of smoking and COVID-19 using a Conditional Risk Assessment approach. With the emergence of new variants and continued vaccine hesitancy, worry and stress may continue to vacillate. Because this is a cross-sectional study, causality cannot be assured. It is also possible that rather than worry driving increases in smoking, smokers may be more worried because they increased their smoking consumption. Although this temporal order is important to consider and investigate in the future, what remains in both cases is an association between worry and smoking consumption. Moreover, regardless of the temporal order between worry and smoking behaviors, the literature strongly suggests a cyclical relationship [32]. In this regard, our study suggests a greater need for interventions that are anchored in specific worries and context in order to break the cycle between worry and smoking consumption.
Additionally, some demographics, such as income, were also associated with increased smoking despite heightened risk awareness. Our white and higher income participants were most likely to report increases in smoking behavior. It is possible that given changes in income due to the pandemic,[33] higher income smokers could afford to increase the money spent on their habit. It is also possible that higher income smokers were more likely to work in places that were covered by smokefree policies prior to the pandemic. (Gonzalez et al., 2021) While sheltering at home, these smokefree policies no longer applied.
Our limitations in this study are partly the result of our online-survey methodology. Self-report measures of smoking behavior are not ideal, but generally reliable (Attebring et al., 2001). We further acknowledge that our sample over-represents white males and high-income smokers. These race and gender demographics are typical of smokers in general (California Health Interview Survey, 2021), however, our online survey may have been more accessible to high-income smokers than low-income smokers. This may mean that our volunteer participants may have lower barriers to purchasing tobacco products and maintaining or increasing their smoking behavior. Prior to the emergence of COVID-19, we had collected data at in-person events and health fairs and would recommend a return to this methodology when safe to do so. Our study is also in a limited geographic region, and while it may reduce generalizability, it also limits confounding issues, such as variability in tobacco product price and accessibility. Our geographic region also has higher smoking rates than the remainder of the state of California (California Health Interview Survey, 2021) and is under-resourced compared to the surrounding regions. (Kayhan Tetik et al., 2020) We consider this a benefit in that these results may have implications for similar regions with at-risk populations. Providing positive coping alternatives to these regions may be particularly important to stave off increased smoking.
Public health advocates are spreading awareness about the relationship between COVID-19 and smoking, and this study supports these efforts by linking perceptions and intentions. However, these messages should be accompanied by information or resources that promote positive coping. The same worry that drives desire to change, may also drive desires to cope. At the intersection of two global pandemics and in the face of much uncertainty around COVID-19, smokers may be more motivated to take protective measures and quit smoking.
Author’s contributions: Deanna Halliday designed the survey, collected and analyzed the data, and wrote the majority of the manuscript. Anna Epperson supervised manuscript development, data reporting, and contributed to editing. MariaElena Gonzalez provided feedback via editing. Anna Song supervised survey development and study design, analyzed data, edited the draft, and provided funding.
Funding: This research was funded by the Tobacco Related Disease Research Program (TRDRP) grant number 28PC-0044.
Declaration of competing Interest
Mariaelena Gonzalez is currently appointed as an unpaid member of the California Tobacco Education Research Oversight Committee (CA TEROC). This manuscript is not associated with CA TEROC and does not represent the views or opinions of CA TEROC. No other authors have competing interests to declare. This research was funded by the Tobacco Related Disease Research Program (TRDRP) grant number 28PC-0044.
Data availability
De-identified data will be made available upon reasonable request.
References
- Ajzen I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991 Dec 1;50(2):179–211. [Google Scholar]
- Arndt J., Goldenberg J.L. Where Health and Death Intersect: Insights From a Terror Management Health Model. Curr. Dir. Psychol. Sci. 2017 Apr 1;26(2):126–131. doi: 10.1177/0963721416689563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attebring M.F., Herlitz J., Berndt A.K., Karlsson T., Hjalmarson A. Are patients truthful about their smoking habits? A validation of self-report about smoking cessation with biochemical markers of smoking activity amongst patients with ischaemic heart disease. J. Intern. Med. 2001;249(2):145–151. doi: 10.1046/j.1365-2796.2001.00770.x. [DOI] [PubMed] [Google Scholar]
- Battalio S.L., Conroy D.E., Dempsey W., Liao P., Menictas M., Murphy S., et al. Sense2Stop: A micro-randomized trial using wearable sensors to optimize a just-in-time-adaptive stress management intervention for smoking relapse prevention. Contemp. Clin. Trials. 2021 Oct;1(109) doi: 10.1016/j.cct.2021.106534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz N.L., Goniewicz M.L., Halpern-Felsher B., Krishnan-Sarin S., Ling P.M., O’Connor R.J., et al. Tobacco product use and the risks of SARS-CoV-2 infection and COVID-19: current understanding and recommendations for future research. Lancet Respir. Med. 2022 Sep 1;10(9):900–915. doi: 10.1016/S2213-2600(22)00182-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrelli B., Hayes R.B., Dunsiger S., Fava J.L. Risk perception and smoking behavior in medically ill smokers: a prospective study. Addiction. 2010;105(6):1100–1108. doi: 10.1111/j.1360-0443.2010.02900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Health Interview Survey | UCLA Center for Health Policy Research [Internet]. [cited 2021 Jan 8]. Available from: http://healthpolicy.ucla.edu/chis/Pages/default.aspx.
- CDC. COVID-19 and Your Health [Internet]. Centers for Disease Control and Prevention. 2020 [cited 2021 Jan 8]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html.
- Cornelius ME. Tobacco Product Use Among Adults — United States, 2019. MMWR Morb Mortal Wkly Rep [Internet]. 2020 [cited 2021 Feb 5];69. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6946a4.htm. [DOI] [PMC free article] [PubMed]
- CDC. Coronavirus Disease 2019 (COVID-19) in the U.S. [Internet]. Centers for Disease Control and Prevention. 2020 [cited 2020 Apr 23]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
- Czeisler MÉ. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep [Internet]. 2020 [cited 2021 May 21];69. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6932a1.htm. [DOI] [PMC free article] [PubMed]
- Emery L.F., Romer D., Sheerin K.M., Jamieson K.H., Peters E. Affective and Cognitive Mediators of the Impact of Cigarette Warning Labels. Nicotine Tob. Res. 2014 Mar 1;16(3):263–269. doi: 10.1093/ntr/ntt124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer R.A., Klein W.M. Risk perceptions and health behavior. Curr. Opin. Psychol. 2015 Oct;1(5):85–89. doi: 10.1016/j.copsyc.2015.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz M.S., MacKinnon D.P. Required Sample Size to Detect the Mediated Effect. Psychol. Sci. 2007 Mar 1;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaiha S.M., Cheng J., Halpern-Felsher B. Association between Youth Smoking, Electronic Cigarette Use, and COVID-19. J. Adolesc. Health. 2020 Oct 1;67(4):519–523. doi: 10.1016/j.jadohealth.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez M., Epperson A.E., Halpern-Felsher B., Halliday D.M., Song A.V. Smokers Are More Likely to Smoke More after the COVID-19 California Lockdown Order. Int. J. Environ. Res. Public Health. 2021 Jan;18(5):2582. doi: 10.3390/ijerph18052582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravely S., Craig L.V., Cummings K.M., Ouimet J., Loewen R., Martin N., et al. Smokers’ cognitive and behavioural reactions during the early phase of the COVID-19 pandemic: Findings from the 2020 ITC Four Country Smoking and Vaping Survey. PLoS One. 2021 Jun 4;16(6):e0252427. doi: 10.1371/journal.pone.0252427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson S.E., Andrews J.A., Barckley M., Lichtenstein E., Lee M.E. Personality traits, perceived risk, and risk-reduction behaviors: A further study of smoking and radon. Health Psychol. 2006 Jul;25(4):530–536. doi: 10.1037/0278-6133.25.4.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayhan Tetik B, Gedik Tekinemre I, Taş S. The Effect of the COVID-19 Pandemic on Smoking Cessation Success. J Community Health [Internet]. 2020 Jul 8 [cited 2021 Jan 8]; Available from: https://doi.org/10.1007/s10900-020-00880-2. [DOI] [PMC free article] [PubMed]
- Klemperer E.M., West J.C., Peasley-Miklus C., Villanti A.C. Change in tobacco and electronic cigarette use and motivation to quit in response to COVID-19. Nicotine Tob. Res. 2020 Apr 28 doi: 10.1093/ntr/ntaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kontoangelos K., Economou M., Papageorgiou C. Mental Health Effects of COVID-19 Pandemia: A Review of Clinical and Psychological Traits. Psychiatry Investig. 2020 Jun;17(6):491–505. doi: 10.30773/pi.2020.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnan RE. Comparisons of health-related and appearance-related smoking risk perceptions and worry on motivation to quit. Health Psychology Open. 2017 Jul 1;4(2):2055102917729541. [DOI] [PMC free article] [PubMed]
- Millstein S.G., Halpern-Felsher B.L. Perceptions of risk and vulnerability. J. Adolesc. Health. 2002 Jul 1;31(1):10–27. doi: 10.1016/s1054-139x(02)00412-3. [DOI] [PubMed] [Google Scholar]
- Nishimura M., Asai K., Tabuchi T., Toyokura E., Kawai T., Miyamoto A., et al. Association of combustible cigarettes and heated tobacco products use with SARS-CoV-2 infection and severe COVID-19 in Japan: a JASTIS 2022 cross-sectional study. Sci. Rep. 2023 Feb 2;13(1):1120. doi: 10.1038/s41598-023-28006-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker K, Minkin R, Bennett J. Economic Fallout From COVID-19 Continues To Hit Lower-Income Americans the Hardest [Internet]. Pew Research Center’s Social & Demographic Trends Project. 2020 [cited 2021 Feb 4]. Available from: https://www.pewsocialtrends.org/2020/09/24/economic-fallout-from-covid-19-continues-to-hit-lower-income-americans-the-hardest/.
- Rigotti NA, Chang Y, Regan S, Lee S, Kelley JHK, Davis E, et al. Cigarette Smoking and Risk Perceptions During the COVID-19 Pandemic Reported by Recently Hospitalized Participants in a Smoking Cessation Trial. J GEN INTERN MED [Internet]. 2021 Jun 7 [cited 2021 Sep 15]; Available from: https://doi.org/10.1007/s11606-021-06913-3. [DOI] [PMC free article] [PubMed]
- Rosenstock I.M. Historical Origins of the Health Belief Model. Health Educaiton Monograph. 1974;2(4):328–335. [Google Scholar]
- Vogel E.A., Henriksen L., Schleicher N.C., Prochaska J.J. Perceived Susceptibility to and Seriousness of COVID-19: Associations of Risk Perceptions with Changes in Smoking Behavior. Int. J. Environ. Res. Public Health. 2021 Jan;18(14):7621. doi: 10.3390/ijerph18147621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yach D. Tobacco Use Patterns in five countries during the COVID-19 Lockdown. Nicotine Tob. Res. 2020 May 27 doi: 10.1093/ntr/ntaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified data will be made available upon reasonable request.