Abstract
Research assessing the changing epidemiology of infectious diseases in China after the implementation of new healthcare reform in 2009 was scarce. We aimed to get the latest trends and disparities of national notifiable infectious diseases by age, sex, province, and season in China from 2010 to 2019. The number of incident cases and deaths, incidence rate, and mortality of 44 national notifiable infectious diseases by sex, age groups, and provincial regions from 2010 to 2019 were extracted from the China Information System for Disease Control and Prevention and official reports and divided into six kinds of infectious diseases by transmission routes and three classes (A–C) in this descriptive study. Estimated annual percentage changes (EAPCs) were calculated to quantify the temporal trends of incidence and mortality rate. We calculated the concentration index to measure economic‐related inequality. Segmented interrupted time‐series analysis was used to estimate the impact of the COVID‐19 pandemic on the epidemic of notifiable infectious diseases. The trend of incidence rate on six kinds of infectious diseases by transmission routes was stable, while only mortality of sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases increased from 0.6466 per 100 000 population in 2010 to 1.5499 per 100 000 population in 2019 by 8.76% per year (95% confidence interval [CI]: 6.88–10.68). There was a decreasing trend of incidence rate on Class‐A infectious diseases (EAPC = −16.30%; 95% CI: −27.93 to −2.79) and Class‐B infectious diseases (EAPC = −1.05%; 95% CI: −1.56 to −0.54), while an increasing trend on Class‐C infectious diseases (EAPC = 6.22%; 95% CI: 2.13–10.48). For mortality, there was a decreasing trend on Class‐C infectious diseases (EAPC = −14.76%; 95% CI: −23.46 to −5.07), and an increasing trend on Class‐B infectious diseases (EAPC = 4.56%; 95% CI: 2.44–6.72). In 2019, the infectious diseases with the highest incidence rate and mortality were respiratory diseases (340.95 per 100 000 population), and sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (1.5459 per 100 000 population), respectively. The greatest increasing trend of incidence rate was observed in seasonal influenza, from 4.83 per 100 000 population in 2010 to 253.36 per 100 000 population in 2019 by 45.16% per year (95% CI: 29.81–62.33), especially among females and children aged 0–4 years old. The top disease with the highest mortality was still AIDs, which had the highest average yearly mortality in 24 provinces from 2010 to 2019, and its incidence rate (EAPC = 14.99%; 95% CI: 8.75–21.59) and mortality (EAPC = 9.65; 95%CI: 7.71–11.63) both increased from 2010 to 2019, especially among people aged 44–59 years old and 60 or older. Male incidence rate and mortality were higher than females each year from 2010 to 2018 on 29 and 10 infectious diseases, respectively. Additionally, sex differences in the incidence and mortality of AIDS were becoming larger. The curve lay above the equality line, with the negative value of the concentration index, which indicated that economic‐related health disparities exist in the distribution of incidence rate and mortality of respiratory diseases (incidence rate: the concentration index = −0.063, p < 0.0001; mortality: the concentration index = −0.131, p < 0.001), sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (incidence rate: the concentration index = −0.039, p = 0.0192; mortality: the concentration index = −0.207, p < 0.0001), and the inequality disadvantageous to the poor (pro‐rich). Respiratory diseases (Dec–Jan), intestinal diseases (May–Jul), zoonotic infectious diseases (Mar–Jul), and vector‐borne infectious diseases (Sep–Oct) had distinct seasonal epidemic patterns. In addition, segmented interrupted time‐series analyses showed that, after adjusting for potential seasonality, autocorrelation, GDP per capita, number of primary medical institutions, and other factors, there was no significant impact of COVID‐19 epidemic on the monthly incidence rate of six kinds of infectious diseases by transmission routes from 2018 to 2020 (all p > 0.05). The incidence rates of six kinds of infectious diseases were stable in the past decade, and incidence rates of Class‐A and Class‐B infectious diseases were decreasing because of comprehensive prevention and control measures and a strengthened health system after the implementation of the new healthcare reform in China since 2009. However, age, gender, regional, and economic disparities were still observed. Concerted efforts are needed to reduce the impact of seasonal influenza (especially among children aged 0–4 years old) and the mortality of AIDs (especially among people aged 44–59 years old and 60 or older). More attention should be paid to the disparities in the burden of infectious diseases.
Keywords: China, disparities, infectious diseases, trends
Abbreviations
- AID
acquired immunodeficiency disease
- CDC
Center for Disease Control and Prevention
- CISDCP
China Information System for Disease Control and Prevention
- COVID‐19
corona virus disease 2019
- GDP
gross domestic product
- SARS
severe acute respiratory syndrome coronavirus
1. BACKGROUND
As of May 18, 2022, 520 102 852 confirmed cases and 6 268 956 deaths of coronavirus disease 2019 (COVID‐19) placed a huge disease burden and economic loss globally. 1 The COVID‐19 epidemic indicated that infectious diseases were still critical health threats. Globally, the 21st century has witnessed a wave of severe infectious disease outbreaks including the 2003 severe acute respiratory syndrome coronavirus (SARS) outbreak, the 2009 swine flu pandemic, the 2012 middle east respiratory syndrome coronavirus outbreak, the 2013–2016 epidemic of Ebola in West Africa, the 2015 epidemic of Zika, and the latest outbreak of COVID‐19. 2 Nevertheless, some infectious diseases burden including neglected tropical diseases, acquired immunodeficiency syndrome (AIDS), tuberculosis, and malaria remained high, especially in low and lower‐middle income countries. 2 Changes in demographic aspects (urbanization, population growth, land‐use change, migration, aging, and changing birth rates, etc.), technological progression (faster global travel and trade, improved health care, etc.), and climate change may change the risk of infectious disease outbreaks. 2
As a country with the largest population in the world, China faces great pressure in the prevention and control of infectious diseases. Since the 2003 SARS outbreak, China promulgated the 2003 Emergency Regulations for Public Health Emergencies. 3 Subsequently, the Law of the People's Republic of China on prevention and control of infectious diseases proposed by the State Council of the People's Republic of China was revised in 2004, 2013, and 2020, respectively. 4 The national immunization program expanded to 13 vaccines that could control 12 infectious diseases during the childhood period in 2021. 5 Up to now, China has obtained great achievements in the prevention and control of infectious diseases, such as the eradication of smallpox and the elimination of polio, leprosy, filariasis, neonatal tetanus, blinding trachoma, and malaria. 4 However, several infectious diseases outbroke in the past two decades in China, such as hand‐foot‐mouth infectious disease caused by enterovirus type 71 (EV71) in 2008, influenza A in 2009, and COVID‐19 in 2020. 6 , 7 Meanwhile, several infectious diseases including sexually transmitted diseases (STIs) and respiratory infectious diseases were still severe public issues in China due to the relatively high incidence rate. 8 , 9
The incidence rate and mortality of infectious diseases varied in different regions and populations. 6 , 10 , 11 , 12 Yang et al. reported that the yearly incidence rate of 45 infectious diseases rose from 300.54 per 100 000 in 2004 to 483.63 per 100 000 in 2013. 10 However, Jiang et al. found that the overall incidence and mortality of notifiable infectious diseases both showed a “U” distribution from 1986 to 2016. 11 The epidemiology features of infectious diseases in China might change significantly in the past ten years due to comprehensive prevention and control measures. State Council of the People's Republic of China revised the Law of the People's Republic of China on prevention and control of infectious diseases in 2013 and 2020. 4 Moreover, several studies reported that strict precautionary measures for control of COVID‐19 epidemic including lockdowns, homestays, school closures, wearing masks, and washing hands frequently might result in changes of an epidemic of infectious disease including respiratory infectious disease, digestive tract and animal‐borne diseases, and so forth. 13 , 14 Therefore, it is necessary to understand the latest epidemiological characteristics of infectious diseases in China to provide a reference for summarizing the effects of past measures and formulating targeted measures in the future.
With the objective of investigating the overall effectiveness of current prevention and control strategies, we analyzed recent trends and disparities of national notifiable infectious diseases by age, sex, season, and province in China from 2010 to 2019 as well as explored the impact of COVID‐19 on infectious diseases prevention and control in China using China Information System for Disease Control and Prevention (CISDCP) and official reports on national notifiable infectious diseases released by the Ministry of Health.
2. METHODS
2.1. Data source
Data were obtained from the database of CISDCP and official reports on national notifiable infectious diseases released by the Ministry of Health. CISDCP was a web‐based disease reporting system established in 2004 after the SARS epidemic. 15 Through the system, hospitals, and clinics from all 31 provinces in the Chinese mainland could report confirmed cases of infectious disease directly to the county and national Center for Disease Control and Prevention (CDC), allowing real‐time information to be delivered to a central database. 16 , 17 Incidence rate, mortality, number of incident cases, and deaths stratified by sex, age groups, and province were available from the public health science data center of the Chinese CDC. 18 By April 2022, only data from 2010 to 2018 could be obtained from this data center. Monthly and yearly data including incidence rate, mortality, incident cases, and deaths from 2019 to 2020 were extracted from the official reports of national notifiable infectious diseases. 19 However, data from official reports were not stratified by patients’ characteristics. Additionally, we extracted the monthly incidence rate of each notifiable infectious disease in China from Jan 2018 to Dec 2020.
2.2. Study design
A total of 44 infectious diseases were included in this study. Based on the reported notifiable infectious diseases analyzed by Yang in 2017, 10 we further added hepatitis D, and combined bacterial dysentery and amoebic dysentery into “bacterial and amoebic dysentery,” and typhoid and paratyphoid into “Typhoid and paratyphoid.” According to previous studies and the public health science data center of the Chinese CDC, we classified diseases into six categories by transmission routes (respiratory diseases, intestinal diseases, zoonotic infectious diseases, vector‐borne infectious diseases, sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases, and diseases with other transmission routes) and three categories including Class‐A, Class‐B, and Class‐C infectious diseases. 10 , 18
2.3. Statistical analysis
Yearly incidence rate, mortality, number of incident cases, and deaths of 44 national notifiable infectious diseases from 2010 to 2019 were described using heat maps and line graphs. Incidence rate and mortality of infectious diseases from 2010 to 2018 by age group and sex were analyzed in stacked columns and line graphs. Incidence rates of 44 national notifiable infectious diseases were ranked, and the ranks were compared over the years from 2010 to 2019. We described the spatial distribution of incidence rate and mortality of infectious diseases and showed the leading infectious disease of all 31 provinces in the Chinese mainland. Season distribution of the monthly incidence rate was analyzed by using rose plots.
The relative changes in the number of incident cases and deaths from 2010 to 2019 were calculated using the formula: . Estimated annual percentage changes (EAPCs) are a summary and widely used measure of the ASR tend over a specified time interval. A regression line was fitted to the natural logarithm of the ASR, that is y = α + βx + ε, where y = ln (ASR) and x = calendar year. EAPC (95% CIs) was calculated as 100 × (eβ − 1) to measure the temporal trend of ASRs in our study. 20 If the EAPC estimation and its 95% CIs were both >0 (or both <0), the ASR had an increasing trend (or a decreasing trend). 20 In addition, we assessed the economic‐related inequality in six infectious diseases by transmission routes by calculating the concentration index (C) and Lorenz curve. 21 , 22 In this study, the distribution of infectious diseases was examined by gross domestic product (GDP) per capita of the province (Chinese yuan). The Lorenz curve is obtained by plotting the cumulative percentage of yearly incidence or mortality of infectious diseases from 2010 to 2018 (Y‐axis) against the cumulative percentage of the population ranked by GDP per capita (X‐axis). The C can be calculated using the following formula 23
where h refers to the health outcome, is the mean of h, and r denotes the fractional rank of individuals in the distribution used (economic status). The concentration index ranges between −1 and +1. A value of 0 for the concentration index represents absolute fairness and there exists no economic‐related inequality. If the concentration index takes a negative value, it indicates that infectious diseases are more concentrated among poor people (pro‐rich). Conversely, if the concentration index is a positive value, it indicates that infectious diseases are more concentrated among rich people (pro‐poor). 24
We used interrupted time‐series analysis and segmented negative binomial regression model to estimate the impact of 2013 Law of the People's Republic of China on prevention and control of infectious diseases on yearly incidence rate and mortality of other notifiable infectious diseases from 2010 to 2019, after adjusting for potential year, autocorrelation, GDP per capita (Chinese yuan), and the number of primary medical institutions, professional public health institutions and Centers for Disease Control and Prevention (CDC) and health technicians per 1000 population. 25 , 26 We classified 10 years as two periods, the first was the pre‐period from 2010 to 2013, and the second was the post‐period from 2014 to 2019. In addition, the impact of the COVID‐19 pandemic on the incidence rate of six notifiable infectious disease groups was explored after adjusting for potential seasonality, autocorrelation, GDP per capita (Chinese yuan), the number of primary medical institutions, professional public health institutions and CDC, health care expenditure per capita (Chinese yuan), health technicians per 1000 population, occupational (assistant) physicians per 1000 population, occupational physicians per 1000 population, and registered nurses per 1000 population, using the monthly incidence rate in China from Jan 2018 to Dec 2020. 25 , 26 We classified 3 years as three periods, first was the pre‐COVID‐19 pandemic period from Jan 2018 to Dec 2019, the second was COVID‐19 pandemic in China period from Jan 2020 to Apr 2020, third was the normal containment/reopening phase in China from May 2020 to Dec 2020. Cumby‐Huizinga general tests were performed to assess the autocorrelation in time series. 25 , 26 In the sensitivity analysis, we applied segmented Poisson regression to examine the robustness of the results
Segmented interrupted time‐series analysis and economic‐related inequality assessment were conducted by Stata 17.0 (StataCorp LLC). Another analysis was conducted by R (version 4.1.0).
3. RESULTS
3.1. Trend of incidence rate, mortality, and number of incident cases and deaths of 44 infectious diseases from 2010 to 2019
There were 16 and four national notifiable infectious diseases that had positive growth in the number of incident cases and deaths from 2010 to 2019; specific values were seen in Supporting Information: Table S1.
All six infectious diseases by transmission routes had a stable trend of incidence rate from 2010 to 2019 (Table 1 and Supporting Information: Figure S1). There was a decreasing trend of incidence rate on Class‐A (EAPC = −16.30%; 95% CI: −27.93 to −2.79) and Class‐B infectious diseases (EAPC = −1.05%; 95% CI: −1.56 to −0.54), while Class‐C infectious diseases had an increasing trend of incidence rate (EAPC = 6.22%; 95% CI: 2.13–10.48; Table 1). In 2019, the infectious diseases classified by transmission routes with the highest incidence rate were respiratory diseases (340.95 per 100 000 population), intestinal diseases (242.90 per 100 000 population), and sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (139.70 per 100 000 population). The top disease with the highest incidence rate changed from intestinal diseases in 2010 to respiratory diseases in 2019. The top three infectious diseases with the highest incidence rate were seasonal influenza, hand, foot, and mouth disease, and infectious diarrhea in 2019. Seasonal influenza (2019: 253.36 per 100 000 population) replaced tuberculosis (2010: 74.27 per 100 000 population), and became the respiratory disease with the highest incidence rate; hand, foot, and mouth diseases, and infectious diarrhea were still the top two intestinal diseases with the highest incidence rate in 2019, like in 2010. Hepatitis B was still the sexual, blood‐borne, and mother‐to‐child‐borne infectious disease with the highest incidence rate in 2019, like in 2010. The incidence rate of tuberculosis declined largely from 74.28 per 100 000 population in 2010 to 55.55 per 100 000 population in 2019 by 3.96% per year (95% CI: −3.28 to −2.65). However, the incidence rate of seasonal influenza increased sharply from 4.83 per 100 000 population in 2010 to 253.36 per 100 000 population in 2019 by 45.16%% per year (95% CI: 29.81–62.33). The number of national notifiable infectious diseases that had an increasing and a decreasing trend of incidence rate were 10 (pertussis, scarlet fever, seasonal influenza, etc.) and 17 (H5N1, schistosomiasis, neonatal tetanus, etc.) from 2010 to 2019, respectively (Table 1 and Figure 1). The diseases with the highest increase in incidence rate were dengue, seasonal influenza, and pertussis (Table 1).
Table 1.
Trends in the incidence rate and mortality of 44 national notifiable infectious diseases in China from 2010 to 2019
| Disease | Incidence rate (per 100 000) | Mortality (per 100 000) | ||||||
|---|---|---|---|---|---|---|---|---|
| 2010 | 2019 | EAPC (95% CI)* | Trend | 2010 | 2019 | EAPC (95% CI)* | Trend | |
| Respiratory diseases | 109.85 | 340.95 | 6.85% (−1.50 to 15.90) | Stable | 0.2416 | 0.2339 | 0.16% (−3.22 to 3.66) | Stable |
| Measles | 2.86 | 0.21 | −17.13% (−35.27 to 6.09) | Stable | 0.0020 | 0.0000 | −47.29% (−71.94 to −1.01) | Decrease |
| Pertussis | 0.13 | 2.15 | 36.96% (24.45–50.73) | Increase | 0.0001 | 0.0001 | −6.87% (−57.91 to 106.07) | Stable |
| Diphtheria | 0.00 | 0.00 | 0.00% (0.00–0.00) | Stable | 0.0000 | 0.0000 | 0.00% (0.00–0.00) | Stable |
| Meningococcal meningitis | 0.02 | 0.01 | −12.05% (−16.00 to −7.92) | Decrease | 0.0025 | 0.0004 | −15.15% (−21.12 to −8.73) | Decrease |
| Scarlet fever | 1.56 | 5.85 | 10.97% (3.13–19.40) | Increase | 0.0000 | 0.0000 | −44.35% (−75.81 to 28.04) | Stable |
| Tuberculosis | 74.27 | 55.55 | −2.96% (−3.28 to −2.65) | Decrease | 0.2248 | 0.2141 | 0.03% (−3.01 to 3.15) | Stable |
| SARS | 0.00 | 0.00 | 0.00% (0.00–0.00) | Stable | 0.0000 | 0.0000 | 0.00% (0.00–0.00) | Stable |
| Leprosy | 0.03 | 0.02 | −6.57% (−9.28 to −3.79) | Decrease | 0.0003 | 0.0000 | −52.80% (−79.29 to 7.58) | Stable |
| Seasonal influenza | 4.83 | 253.36 | 45.16% (29.81–62.33) | Increase | 0.0005 | 0.0193 | 54.86% (29.45–85.26) | Increase |
| Mumps | 22.37 | 21.48 | −5.78% (−13.39 to 2.50) | Stable | 0.0003 | 0.0000 | −59.23% (−79.46 to −19.09) | Decrease |
| Rubella | 3.23 | 2.33 | −23.22% (−40.28 to −1.28) | Decrease | 0.0001 | 0.0000 | −41.97% (−73.44 to 26.75) | Stable |
| H1N1a | 0.53 | 0.0110 | ||||||
| Intestinal diseases | 213.27 | 242.90 | 2.03% (−0.27 to 4.38) | Stable | 0.0768 | 0.0037 | −27.20% (−32.92 to −20.99) | Decrease |
| Cholera | 0.01 | 0.00 | −17.54% (−28.97 to −4.27) | Decrease | 0.0000 | 0.0000 | −11.80% (−50.58 to 57.41) | Stable |
| Hepatitis A | 2.64 | 1.38 | −7.28% (−9.74 to −4.75) | Decrease | 0.0003 | 0.0002 | −7.04% (−21.80 to 10.51) | Stable |
| Hepatitis E | 1.77 | 2.02 | 0.55% (−0.80 to 1.92) | Stable | 0.0026 | 0.0011 | −10.17% (−16.84 to −2.97) | Decrease |
| Bacterial and amoebic dysentery | 18.90 | 5.81 | −12.66% (−13.35 to −11.95) | Decrease | 0.0027 | 0.0001 | −32.36% (−37.89 to −26.33) | Decrease |
| Typhoid and paratyphoid | 1.05 | 0.66 | −3.93% (−6.14 to −1.68) | Decrease | 0.0002 | 0.0000 | −31.98% (−68.39 to 46.39) | Stable |
| Poliomyelitis | 0.00 | 0.00 | −33.50% (−68.53 to 40.54) | Stable | 0.0000 | 0.0000 | −25.40% (−56.42 to 27.69) | Stable |
| Infectious diarrhea | 55.93 | 95.64 | 5.84% (3.75–7.97) | Increase | 0.0032 | 0.0009 | −9.17% (−14.04 to −4.03) | Decrease |
| Hand, foot, and mouth disease | 132.96 | 137.40 | 1.50% (−2.63 to 5.81) | Stable | 0.0678 | 0.0014 | −32.63% (−40.21 to −24.10) | Decrease |
| Zoonotic infectious diseases | 3.64 | 4.16 | 0.43% (−2.93 to 3.90) | Stable | 0.1609 | 0.0234 | −18.75% (−20.28 to −17.18) | Decrease |
| Plague | 0.00 | 0.00 | −20.20% (−69.52 to 108.87) | Stable | 0.0001 | 0.0001 | −28.76% (−72.13 to 82.08) | Stable |
| Hemorrhagic fever | 0.71 | 0.69 | −1.25% (−4.68 to 2.30) | Stable | 0.0088 | 0.0032 | −9.28% (−14.91 to −3.28) | Decrease |
| Rabies | 0.15 | 0.02 | −19.61% (−20.90 to −18.29) | Decrease | 0.1509 | 0.0198 | −19.80% (−21.14 to −18.44) | Decrease |
| Leptospirosis | 0.05 | 0.02 | −12.44% (−17.60 to −6.95) | Decrease | 0.0008 | 0.0001 | −36.69% (−64.72 to 13.60) | Stable |
| Brucellosis | 2.53 | 3.15 | 1.00% (−3.57 to 5.79) | Stable | 0.0001 | 0.0001 | 13.38% (−53.56 to 176.84) | Stable |
| Hydatid disease | 0.19 | 0.29 | 5.90% (2.02–9.93) | Increase | 0.0001 | 0.0001 | −15.42% (−67.32 to 118.88) | Stable |
| H5N1 | 0.00 | 0.00 | −63.23% (−79.92 to −32.69) | Decrease | 0.0001 | 0.0000 | −58.31% (−76.43 to −26.27) | Decrease |
| H7N9 | 0.00 | −47.11% (−83.81 to 72.80) | – | 0.0001 | −25.37% (−78.72 to 161.70) | – | ||
| Vector‐borne infectious diseases | 0.96 | 1.89 | 3.85% (−11.74 to 22.19) | Stable | 0.0081 | 0.0025 | −5.11% (−14.80 to 5.68) | Stable |
| Typhus | 0.17 | 0.08 | −10.70% (−13.73 to −7.57) | Decrease | 0.0001 | 0.0000 | −41.97% (−75.79 to 39.09) | Stable |
| Japanese encephalitis | 0.19 | 0.03 | −11.71% (−21.68 to −0.47) | Decrease | 0.0069 | 0.0009 | −7.77% (−23.54 to 11.26) | Stable |
| Kala‐azar | 0.03 | 0.01 | −6.62% (−15.28 to 2.93) | Stable | 0.0001 | 0.0000 | −46.63% (−76.87 to 23.13) | Stable |
| Malaria | 0.55 | 0.18 | −8.16% (−13.76 to −2.20) | Decrease | 0.0010 | 0.0014 | −8.59% (−20.39 to 4.96) | Stable |
| Dengue | 0.02 | 1.59 | 56.20% (9.43–122.97) | Increase | 0.0000 | 0.0002 | 137.91% (11.22–408.89) | Increase |
| Filariasis | 0.00 | 0.00 | ‐25.40% (‐56.42~27.69) | Stable | 0.0000 | 0.0000 | 0.00% (0.00~0.00) | Stable |
| Sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases | 126.89 | 139.70 | 0.72% (−0.23 to 1.69) | Stable | 0.6466 | 1.5459 | 8.76% (6.88–10.68) | Increase |
| Hepatitis B | 79.46 | 71.77 | −1.46% (−2.80 to −0.10) | Decrease | 0.0516 | 0.0320 | −6.03% (−10.07 to −1.82) | Decrease |
| Hepatitis C | 11.47 | 16.02 | 2.83% (1.20–4.48) | Increase | 0.0096 | 0.0073 | −3.13% (−6.15 to ‐−0.01) | Decrease |
| Hepatitis D | 0.03 | −5.67% (−10.81 to −0.24) | – | 0.0000 | 0.00% (0.00–0.00) | – | ||
| AIDs | 1.20 | 5.10 | 14.99% (8.75–21.59) | Increase | 0.5801 | 1.5036 | 9.65% (7.71–11.63) | Increase |
| Gonorrhea | 7.91 | 8.45 | 3.00% (0.39–5.67) | Increase | 0.0001 | 0.0000 | −31.39% (−58.46 to 13.30) | Stable |
| Syphilis | 26.86 | 38.37 | 3.31% (2.52–4.11) | Increase | 0.0052 | 0.0030 | −7.96% (−10.40 to −5.45) | Decrease |
| Diseases with other transmission routes | 22.92 | 3.04 | −11.89% (−23.22 to 1.12) | Stable | 0.0644 | 0.0031 | −33.55% (−41.82 to −24.11) | Decrease |
| Anthrax | 0.02 | 0.02 | 2.21% (−2.39 to 7.03) | Stable | 0.0004 | 0.0001 | −5.71% (−16.49 to 6.46) | Stable |
| Neonatal tetanus | 0.79 | 0.04 | −29.76% (−33.14 to −26.20) | Decrease | 0.0640 | 0.0030 | −34.03% (−42.46 to −24.36) | Decrease |
| Schistosomiasis | 0.32 | 0.01 | −32.37% (−52.13 to −4.46) | Decrease | 0.0000 | 0.0000 | −48.38% (−76.38 to 12.80) | Stable |
| Acute hemorrhagic conjunctivitis | 21.78 | 2.97 | −10.12% (−23.26 to 5.27) | Stable | 0.0000 | 0.0000 | 0.00% (0.00–0.00) | Stable |
| Class‐A infectious diseases b | 0.01 | 0.00 | −16.30% (−27.93 to −2.79) | Decrease | 0.0001 | 0.0001 | −37.17% (−72.63 to 44.23) | Stable |
| Class‐B infectious diseases b | 235.99 | 219.08 | −1.05% (−1.56 to −0.54) | Decrease | 1.1258 | 1.7907 | 4.56% (2.44–6.72) | Increase |
| Class‐C infectious diseases b | 241.52 | 513.57 | 6.22% (2.13–10.48) | Increase | 0.0725 | 0.0217 | −14.76% (−23.46 to −5.07) | Decrease |
*If the EAPC estimation and its 95% CIs were both >0 (or both <0), the ASR had an increasing trend (or a decreasing trend).
Abbreviations: 95% CI, 95% confidence interval; AID, acquired immunodeficiency disease; EAPC, estimated annual percent change; SARS, severe acute respiratory syndrome.
Influenza A H1N1 first broke out in China in 2009 and its data were combined into seasonal influenza from December 2013.
Class‐A infectious diseases include plague and cholera; Class‐B infectious diseases include infectious SARS, AIDs, viral hepatitis (not include hepatitis D), polio, H5N1, measles, hemorrhagic fever, rabies, Japanese encephalitis, dengue, anthrax, bacterial, and amoebic dysentery, tuberculosis, typhoid and paratyphoid, meningococcal meningitis, pertussis, diphtheria, tetanus, scarlet Fever, brucellosis, gonorrhea, syphilis, leptospirosis, schistosomiasis, malaria; Class‐C infectious diseases include seasonal influenza, mumps, rubella, acute hemorrhagic conjunctivitis, leprosy, typhus, kala‐azar, hydatid disease, filariasis, and infectious diarrheal diseases other than cholera, bacterial and amoebic dysentery, typhoid, and paratyphoid.
Figure 1.
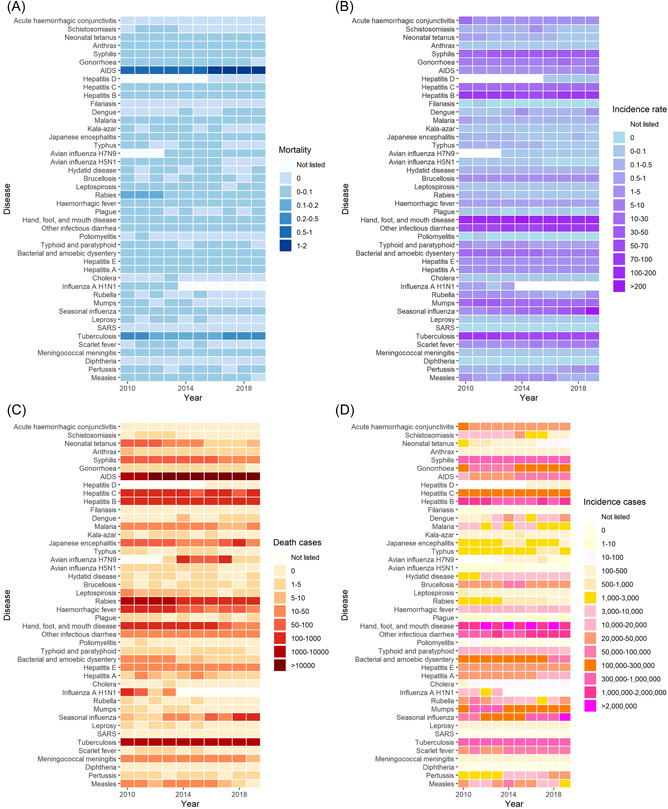
Trend of incidence rate, mortality, and number of incident cases and deaths of 44 national notifiable infectious diseases in China from 2010 to 2019. (A) Mortality. (B) Incidence rate. (C) Deaths. (D). Incident cases.
Out of six infectious diseases by transmission routes, only mortality of sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (EAPC = 8.76%; 95% CI: 6.88–10.68) increased from 0.6466 per 100 000 population in 2010 to 1.5499 per 100 000 population in 2019, while that of intestinal diseases, zoonotic infectious diseases and diseases with other transmission routes decreased from 2010 to 2019 (Table 1 and Supporting Information: Figure S1). There was a decreasing trend of mortality in Class‐C infectious diseases (EAPC = −14.76%; 95% CI: −23.46 to −5.07), while Class‐B infectious diseases had an increasing trend of mortality (EAPC = 4.56%; 95% CI: 2.44–6.72; Table 1). In 2019, the infectious diseases classified by transmission routes with the highest mortality were sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (1.5459 per 100 000 population), respiratory diseases (0.2339 per 100 000 population), zoonotic infectious diseases (0.0234 per 100 000 population). AIDS and tuberculosis were the top two infectious diseases with the highest mortality in 2019, like in 2010. The incidence rate (EAPC = 14.99%; 95% CI: 8.75–21.59) and mortality (EAPC = 9.65%; 95% CI: 7.71–11.63) of AIDS both increased from 2010 to 2019 (Table 1). The number of national notifiable infectious diseases with an increasing and decreasing trend of mortality was three (dengue, seasonal influenza, and AIDS) and 14 from 2010 to 2019, respectively (Table 1 and Figure 1).
Segmented interrupted time‐series analyses showed that, after adjusting for other confounders, the yearly incidence rate and mortality of six infectious diseases by transmission routes between the pre‐period from 2010 to 2013 and post‐period from 2014 to 2019 had no significant differences (all p > 0.05, Supporting Information: Figures S2 and S3). In addition, segmented interrupted time‐series analyses showed that, after adjusting for other confounders, there was no significant impact of the COVID‐19 epidemic on the monthly incidence rate of six infectious diseases by transmission routes from 2018 to 2020 (Supporting Information: Figure S4; all p > 0.05). In the sensitivity analysis, the results were stable after we used segmented Poisson regression models, instead of negative binomial regression models.
3.2. Ranks of incidence rate of 44 national notifiable infectious diseases in China from 2010 to 2019
The rank of incidence of 44 national notifiable infectious diseases in China from 2010 to 2019 was shown in Supporting Information: Table S2 and Figure S5. Hand, foot, and mouth disease ranked top from 2010 to 2018, and was replaced by seasonal influenza in 2019. Hand, foot, and mouth disease, other infectious diarrhea, hepatitis B, tuberculosis, syphilis, and seasonal influenza were the top six infectious diseases with the highest incidence rate from 2016 to 2019.
3.3. Age distribution of incidence rate and mortality of infectious diseases in China from 2010 to 2018
For intestinal diseases, the incidence rate and mortality were highest in people aged under 5 all the way from 2010 to 2018, followed by people aged above 60 or 5–14, 15–44, and 45–59. For sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases, the age group with the highest incidence rate shifted from 15–44 to 60 or older since 2010. For respiratory diseases, the age group with the highest incidence rate has shifted from 60 or older to 14 or younger since 2009. The mortality of respiratory diseases and sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases was highest in people aged above 60 all the way, and the mortality of intestinal diseases was highest in people aged 0–4 all the way (Figure 2).
Figure 2.
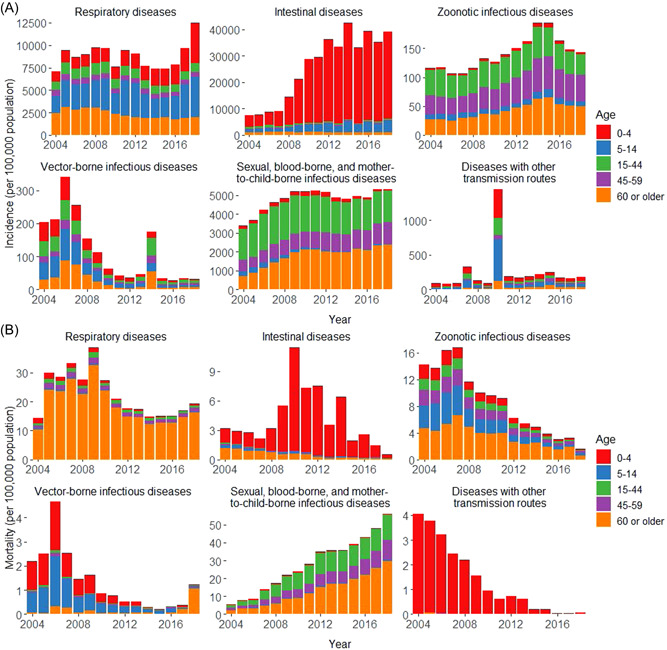
Incidence rate and mortality of six infectious diseases by transmission routes in China by age groups. (A) Incidence rate. (B) Mortality.
From 2010 to 2018, there was an increasing trend of incidence rate of respiratory diseases and intestinal diseases among people aged 0–4 years old, mainly caused by seasonal influenza and infectious diarrhea. There was an increasing trend of incidence rate of sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases among people aged 44–59 years, mainly caused by AIDs. Other aged groups had no increasing trend of incidence rate on six infectious diseases by transmission routes (Supporting Information: Tables S3–S7 and Figure S6). There was an increasing trend of mortality of sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases among people aged 44–59 years and 60 or older, mainly caused by AIDs (Supporting Information: Tables S3–S7 and Figure S6). For 44 national infectious diseases, the number of infectious diseases with an increasing trend of incidence rate was 7, 7, 8, 10, and 6 among 0–4, 5–14, 15–44, 45–59, and 60 or older age group, respectively. The number of infectious diseases with the increasing trend of mortality was 0, 1, 1, 1, and 1 among 0–4, 5–14, 15–44, 45–59, and 60 or older age group, respectively (Supporting Information: Tables S3–S7).
3.4. Sex distribution of incidence and mortality of infectious diseases in China from 2010 to 2018
Male incidence rate and mortality were higher than females each year from 2010 to 2018 on 29 and 10 infectious diseases, respectively (Supporting Information: Figures S7–S8 and Tables S8–S9). Sex differences in the incidence and mortality of AIDS were becoming larger (Supporting Information: Figures S7 and S8).
All six infectious diseases by transmission routes had a stable trend of incidence rate among males, while respiratory diseases and intestinal diseases had an increasing trend of incidence rate among females, mainly caused by seasonal influenza and other infectious diarrhea (Supporting Information: Figure S9A and Table S8). The mortality of sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases had an increasing trend of incidence rate among males and females (Supporting Information: Figure S9B and Table S9). There were seven and nine infectious diseases that had increasing incidence rates among males and females, respectively (Supporting Information: Table S8). There were two (seasonal influenza, AIDs) and one infectious disease (AIDs) that had increasing mortality among males and females, respectively (Supporting Information: Table S9).
3.5. Province distribution and economic‐related health disparities of the incidence rate and mortality of infectious diseases in China from 2010 to 2018
The leading infectious diseases classified by transmission routes across 31 provinces are seen in Supporting Information: Table S10. Of all diseases, AIDs had the highest average yearly mortality in 24 provinces, followed by tuberculosis in six provinces (Tianjin, Inner Mongolia, Liaoning, etc.) and hepatitis B in Beijing from 2010 to 2018. Out of six infectious diseases by transmission routes, respiratory diseases had two provinces (Shaanxi and Chongqing) with the increasing trend of mortality (Supporting Information: Table S11 and Figure S10), and zoonotic infectious diseases had one province (Ningxia; Supporting Information: Table S12 and Figure S11). Intestinal diseases (Supporting Information: Table S13 and Figure S12), vector‐borne infectious diseases (Supporting Information: Table S14 and Figure S13), and diseases with other transmission routes (Supporting Information: Table S15 and Figure S14) had no province with the increasing trend of mortality. The disease which had most provinces with the increasing trend of morality was sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (20/31, Supporting Information: Table S16 and Figure S15) from 2010 to 2018. The diseases which had the most provinces with the increasing trend of incidence rate were zoonotic infectious diseases (13/31, Supporting Information: Table S12 and Figure S11) and sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (11/31, Supporting Information: Table S16 and Figure S15). Tibet (EAPC = 40.70%; 95% CI = 21.16–63.41), Gansu (EAPC = 26.66%; 95% CI = 13.95–40.79), and Ningxia (EAPC = 26.65%; 95% CI = 17.18–36.88) had the highest increasing trend of zoonotic infectious diseases infection, and Tibet, Shandong, and Hainan had the increasing trend of sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases infection with more than 10.00% increases per year (Supporting Information: Table S16).
The Lorenz curves of the yearly incidence rate of six infectious diseases by transmission routes are shown in Figure 3A and Supporting Information: Figure S16. The curve of respiratory diseases (the concentration index = −0.063, p < 0.0001), sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (the concentration index = −0.039, p = 0.0192), and diseases with other transmission routes (the concentration index = −0.357, p < 0.01) all lay above the equality line, with the negative value which indicated that economic‐related health disparities and the inequality disadvantageous to the poor (pro‐rich) that these infectious diseases infection were more concentrated among the population with lower economic status, while intestinal diseases conversed (the concentration index = 0.097, p < 0.0001; Figure 3A). There were no economic‐related health disparities in the yearly incidence rate of zoonotic infectious diseases and vector‐borne infectious diseases (all p > 0.05; Supporting Information: Figure S16). The concentration indexes were stable from 2010 to 2019, and there were no significant differences between the western and eastern areas and the central areas (all p > 0.05).
Figure 3.
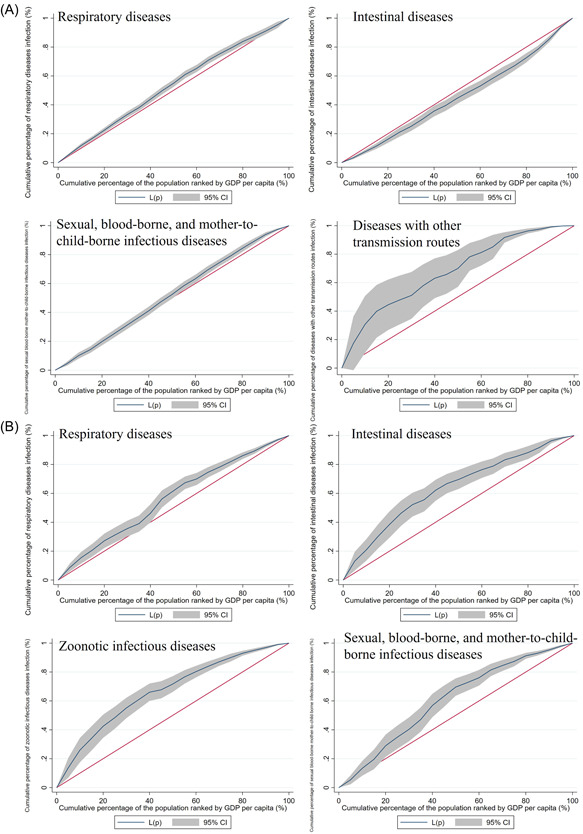
Lorenz curves of yearly incidence rate and mortality of infectious diseases by transmission routes. Red line was the equality line. (A) Incidence rate: respiratory diseases: the negative value of the concentration index of −0.063 (p < 0.0001); intestinal diseases: the positive value of the concentration index of 0.097 (p < 0.0001); sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases: the negative value of the concentration index of −0.039 (p = 0.0192); diseases with other transmission routes: the negative value of the concentration index of −0.357 (p < 0.01). (B) Mortality: respiratory diseases: the negative value of the concentration index of −0.131 (p < 0.001); intestinal diseases: the negative value of the concentration index of −0.274 (p < 0.0001); zoonotic infectious diseases: the negative value of the concentration index of −0.337 (p < 0.0001); sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases: the negative value of the concentration index of −0.207 (p = 0.0192).
The Lorenz curves of yearly mortality of six infectious diseases by transmission routes are shown in Figure 3B and Supporting Information: Figure S17. The curve of respiratory diseases (the concentration index = −0.131, p < 0.001), intestinal diseases (the concentration index = −0.274, p < 0.0001), zoonotic infectious diseases (the concentration index = −0.337, p < 0.0001) and sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (the concentration index = −0.207, p < 0.0001) all lay above the equality line, with the negative value which indicated that economic‐related health disparities and the inequality disadvantageous to the poor (pro‐rich) that these infectious diseases deaths were more concentrated among the population with lower economic status (Figure 3B). There were no economic‐related health disparities in the yearly incidence rate of vector‐borne infectious diseases and diseases with other transmission routes (all p > 0.05; Supporting Information: Figure S17). The concentration indexes were stable from 2010 to 2019 and were no significant difference between the western and eastern areas and the central area (all p > 0.05).
3.6. Seasonal distribution of incidence and mortality of infectious diseases in China from 2010 to 2019
The seasonal distribution of infectious diseases exhibits distinct patterns: respiratory diseases (mainly distributed in Dec and Jan), intestinal diseases (May–Jul), zoonotic infectious diseases (Mar–Jul), and vector‐borne infectious diseases (Sep–Oct; Figure 4).
Figure 4.
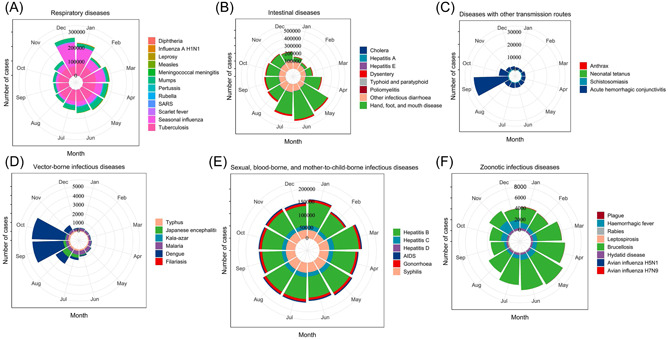
Season distribution of incident cases of notifiable infectious diseases in China from 2010 to 2019. (A) Respiratory diseases. (B) Intestinal diseases. (C) Zoonotic infectious diseases. (D) Vector‐borne infectious diseases. (E) Sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases. (F) Zoonotic infectious diseases.
4. DISCUSSION
To our knowledge, this is the first study that reported the yearly incidence rate, mortality, and trends of notifiable infectious diseases from 2010 to 2019 in the Chinese mainland, as well as the impact of the COVID‐19 pandemic on the incidence rate and mortality of other notifiable infectious diseases. The trend of incidence rate on six infectious diseases by transmission routes was stable, while only mortality of sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases from 2010 to 2019. The incidence rates of Class‐A and Class‐B infectious diseases were decreasing. In 2019, the infectious diseases with the highest incidence rate and mortality were respiratory diseases (340.95 per 100 000 population), and sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases (1.5459 per 100 000 population), respectively. For incidence, hand, foot, and mouth disease ranked top from 2010 to 2018 and was replaced by seasonal influenza in 2019. Comprehensive prevention and control measures for infectious diseases in terms of resources, systems, and laws since SARS in 2003 in China, such as the 2003 Emergency Regulations for Public Health Emergencies, 3 Law of the People's Republic of China on prevention and control of infectious diseases in 2004 and 2013 may explain the stable incidence rate and decreasing incidence rates of Class‐A and Class‐B infectious diseases from 2010 to 2019. 4 The greatest increasing trend of incidence rate was observed in seasonal influenza, especially among female and people aged 0–4 years old. The top disease with the highest mortality was still AIDs, which had the highest average yearly mortality in 24 provinces from 2010 to 2019; its incidence rate and mortality both increased from 2010 to 2019, especially among people aged 44–59 years old and 60 or older.
Seasonal influenza had a relatively high increasing trend of incidence rate, replaced hand, foot, and mouth disease, and became the first place with the highest incidence rate in 2019. Tuberculosis as the highest incidence rate of respiratory disease was replaced by seasonal influenza. In 2005, China rebuilt public health service facilities and formulated a new 5‐year plan for tuberculosis prevention and treatment. 27 With the economic development in China, influencing factors of incidence rate and mortality of tuberculosis including living standards, health services, medical technology, and the monitoring of infectious diseases have been improved. 28 Both the incidence rate and mortality of seasonal influenza increased from 2010 to 2019. The possible reasons for the high and uncontrollable incidence rate include high vaccination hesitation of seasonal influenza, low awareness of vaccination benefits, the insufficient number of clinics for seasonal influenza vaccination, and so forth. 29 Additionally, the diagnosis standard for confirmed influenza cases was changed in 2019, and an influenza antigen rapid test is now included in the diagnosis guidelines of influenza‐confirmed cases according to the national diagnostic and treatment protocol for seasonal influenza (2019 edition). 30 , 31 Therefore, the number of medical institutions providing rapid diagnosis services for patients with influenza has increased significantly, leading to a significant increase in the number of reported cases of influenza. 31 Our study reported that the mortality and incidence rate of AIDS increased annually from 2010 to 2019, especially among people aged 44–59 years old and 60 or older. Besides, male incidence and mortality of AIDS were both higher than females and the differences became greater from 2010 to 2019. There were many influencing factors on the effectiveness of controlling HIV/AIDS, such as the awareness of sexual health, high‐risk sex behaviors, and management of HIV/AIDS patients after interprovincial movement. 32 , 33 Our results suggested that there was a more urgent need to focus on the AIDS epidemic in China. The first edition of Chinese guidelines for the diagnosis and treatment of HIV/AIDS was published in 2005. To further reduce the mortality and incidence rate of HIV/AIDS, the 2021 edition consisted of seven highlights including first source control and early intervention, standardized diagnostic criteria, optimized programs to prevent mother‐to‐child transmission based on circumstances in China and clinical studies, prevention of mother‐to‐child transmission, single‐positive family fertility based on clinical studies of China, and so forth. 34
After the 2003 SARS outbreak, the State Council of the People's Republic of China proposed the 2003 Emergency Regulations for Public Health Emergencies. 3 Subsequently, the Law of the People's Republic of China on prevention and control of infectious diseases was revised in 2004 and 2013, respectively. 4 Due to the efforts, there were huge achievements in the prevention and control of infectious diseases including the elimination of filariasis in 2006, neonatal tetanus in 2012, blinding trachoma in 2014, and malaria in 2021. 4 Except sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases, only several provinces had an increasing trend of mortality, such as respiratory diseases in Shaanxi and Chongqing and zoonotic infectious diseases in Ningxia. However, our study found that there were still some infectious diseases that remained at high incident levels in most provinces of China, especially sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases, and zoonotic infectious diseases. Tibet had the highest increasing trend of zoonotic infectious diseases infection and sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases infection. Ningxia had the highest increasing trend of zoonotic infectious diseases infection and deaths. The possible reason was that China's territory is so broad that the existing differences between climate, demographic characteristics, virus subtypes, vaccination, public health emergencies, vector control, personal protection, and environmental sanitation may result in the geographical differences in infectious diseases epidemic. 35 , 36 Our results indicated that China faced more challenges in controlling infectious diseases in some specific provinces. Furthermore, we observed that the highest incidence of intestinal diseases was found in people aged under 5, and the highest mortality of sexual, blood‐borne, and mother‐to‐child‐borne infectious diseases was found in people aged over 60. Hand, foot, and mouth disease was the severest intestinal disease for children of 0–4 years. AIDS was the severest sexual, blood‐borne, and mother‐to‐child‐borne infectious disease among older people. Our findings provided a reference for targeted measures in surveillance and early warning of the epidemic of infectious diseases by regions and populations, as well as the investment in healthcare services (such as the vaccine immunization program, safety of blood collection), and infrastructure construction (the water supply and sanitation, massive routine vector control). 10
In this study, systematic, long‐term, and comprehensive data from CISDCP and official reports released by the Ministry of Health were used. Under regulations from the China CDC and CISDCP, health facilities need to report all cases of notifiable infectious diseases through the web‐based system, with the validity of the surveillance system being continuously monitored. Although CISDCP has not yet reached all health facilities, such as hospitals, CDCs, and community health centers, the total coverage is at least 85% throughout the country with more than 95% coverage of county‐level and above facilities each year in China. 15 However, the coverage of some provinces, particularly in the less developed provinces such as Tibet, Qinghai, and Inner Mongolia was lower. 15 Therefore, yearly incidence data from the reporting system was affected by screening intensity and thus could be underestimated due to the “iceberg phenomenon.” There were other limitations in our study. The incidence rate of some infectious diseases could also be underestimated because of ascertainment bias by self‐selection, which means individuals with a specific infectious disease are more likely to avoid screening than those without infection. 10 In addition, due to unavailable data from 2021 to 2022, the impact of the COVID‐19 epidemic on morbidity and mortality of other infectious diseases cannot be assessed. We will continue to carry out in‐depth research in the future.
5. CONCLUSIONS
The incidence rates of six kinds of infectious diseases were stable in the past decade, and incidence rates of Class‐A and Class‐B infectious diseases were decreasing, because of comprehensive prevention and control measures and a strengthened health system after the implementation of the new healthcare reform in China in 2009. However, age, gender, regional, and economic disparities were still observed. Concerted efforts are needed to reduce the impact of seasonal influenza (especially among children aged 0–4 years old) and the mortality of AIDs (especially among people aged 44–59 years old and 60 or older). The government has encouraged high‐risk populations including children aged 0–4 years to be vaccinated against seasonal influenza. Then, during the seasonal influenza epidemic, parents, children, and related caregivers should do a good job with hygiene habits and pay attention to take protection measures when going to medical institutions. In addition, strengthening health education and forming medical care programs such as more convenient medical consultation and drug supply may benefit for elderly with AIDS. Generally, more attention should be paid to the disparities in the burden of infectious diseases.
AUTHOR CONTRIBUTIONS
Min Du, Min Liu, and Jue Liu conceptualized and designed the study. Min Du, Ruitong Wang, Wenxin Yan, Qiao Liu, Chenyuan Qin, and Xuan Lv did data acquisition. Min Du and Ruitong Wang did data curation and formal analysis. Min Du, Ruitong Wang, Jie Yuan, and Xuan Lv did visualization. Min Du and Ruitong Wang did writing – original draft. Jue Liu, Min Liu, Nijuan Xiang, Wannian Liang, and Lin Zhu did writing – reviewing and editing.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Supplementary information.
ACKNOWLEDGMENTS
The authors thank you for your efforts in collecting information on national notified infectious diseases by the Chinese Disease Control and Prevention at the provincial, city, and county levels. This work was partly supported by the National Natural Science Foundation of China (72122001, 71934002), the National Key Research and Development Project of China (2021ZD0114101, 2021ZD0114104, 2021ZD0114105), the National Statistical Science Research Project (2021LY038), and the National Science and Technology Project on Development Assistance for Technology, Developing China‐ASEAN Public Health Research and Development Collaborating Center (KY202101004).
Du M, Wang R, Yuan J, et al. Trends and disparities in 44 national notifiable infectious diseases in China: An analysis of national surveillance data from 2010 to 2019. J Med Virol. 2022;95:e28353. 10.1002/jmv.28353
Min Du and Ruitong Wang contributed equally to this study.
DATA AVAILABILITY STATEMENT
Our data was from the database of the China Information System for Disease Control and Prevention website (https://www.phsciencedata.cn/Share/ky_sjml.jsp?id=a56cd203-cd11-414d-9efa-d1583b97476f).
REFERENCES
- 1. WHO Coronavirus (COVID‐19) Dashboard . 2022. Accessed May 18, 2022. https://covid19.who.int/
- 2. Baker RE, Mahmud AS, Miller IF, et al. Infectious disease in an era of global change. Nat Rev Microbiol. 2022;20(4):193‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Order of The State Council of the People's Republic of China . Accessed May 19, 2022. http://www.gov.cn/gongbao/content/2003/content_62137.htm
- 4. Zhao H, Wang H, Li H, et al. Uptake and adverse reactions of COVID‐19 vaccination among people living with HIV in China: a case‐control study. Hum Vaccines Immunother. 2021;17(12):4964‐4970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Notification of the NHC on the Issuance of the Procedures and Instructions for the Immunization of Children (2021 edition) for the Vaccines of the National Immunization Programme . http://www.nhc.gov.cn/jkj/s3581/202103/590a8c7915054aa682a8d2ae8199e222.shtml
- 6. Yang WZ. [Dramatic achievements in infectious disease prevention and treatment in China during the past 70 years]. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40(12):1493‐1498. [DOI] [PubMed] [Google Scholar]
- 7. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus‐infected pneumonia. N Engl J Med. 2020;382(13):1199‐1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhao L, Wang HT, Ye RZ, et al. Profile and dynamics of infectious diseases: a population‐based observational study using multi‐source big data. BMC Infect Dis. 2022;22(1):332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li ZJ, Zhang HY, Ren LL, et al. Etiological and epidemiological features of acute respiratory infections in China. Nat Commun. 2021;12(1):5026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yang S, Wu J, Ding C, et al. Epidemiological features of and changes in incidence of infectious diseases in China in the first decade after the SARS outbreak: an observational trend study. Lancet Infect Dis. 2017;17(7):716‐725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jiang Y, Dou X, Yan C, et al. Epidemiological characteristics and trends of notifiable infectious diseases in China from 1986 to 2016. J Glob Health. 2020;10(2):020803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liu J, Zhang S, Wang Q, et al. Seroepidemiology of hepatitis B virus infection in 2 million men aged 21‐49 years in rural China: a population‐based, cross‐sectional study. Lancet Infect Dis. 2016;16(1):80‐86. [DOI] [PubMed] [Google Scholar]
- 13. Wang L, Wang K, Zhong H, et al. The effect of coronavirus 2019 disease control measures on the incidence of respiratory infectious disease and air pollutant concentrations in the Yangtze River Delta Region, China. Int J Environ Res Public Health. 2022;19(3):1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bai B, Jiang Q, Hou J. The COVID‐19 epidemic and other notifiable infectious diseases in China. Microb Infect. 2022;24(1):104881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dong Y, Wang L, Burgner DP, et al. Infectious diseases in children and adolescents in China: analysis of national surveillance data from 2008 to 2017. BMJ. 2020;369:m1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhang L, Wilson DP. Trends in notifiable infectious diseases in China: implications for surveillance and population health policy. PLoS One. 2012;7(2):e31076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang L, Wang Y, Jin S, et al. Emergence and control of infectious diseases in China. Lancet. 2008;372(9649):1598‐1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Public Health Center . https://www.phsciencedata.cn/.
- 19. Ministry of Health . http://www.nhc.gov.cn/jkj/s3578/202004/b1519e1bc1a944fc8ec176db600f68d1.shtml.
- 20. Liu Z, Jiang Y, Yuan H, et al. The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674‐683. [DOI] [PubMed] [Google Scholar]
- 21. López‐Feldman A. Decomposing inequality and obtaining marginal effects. Stata J. 2006;6(1):106‐111. [Google Scholar]
- 22. Lerman RI, Yitzhaki S. Income inequality effects by income source: a new approach and applications to the United States. Rev Econ Stat. 1985;67:151‐156. [Google Scholar]
- 23. Chen P, Li F, Harmer P. Healthy China 2030: moving from blueprint to action with a new focus on public health. Lancet Public Health. 2019;4(9):e447. [DOI] [PubMed] [Google Scholar]
- 24. Wang X, Liu J, Wang Q, et al. Economic‐related inequalities in hepatitis B virus infection among 115.8 million pregnant women in China from 2013 to 2020. EClinicalMedicine. 2022;49:101465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Baum CF, Schaffer ME. ACTEST: Stata Module to Perform Cumby‐Huizinga General Test for Autocorrelation in Time Series. 2013. http://ideas.repec.org/c/boc/bocode/s457668.html
- 26. Linden A. ITSA: Stata Module for Conducting Interrupted Time Series Analysis for Single and Multiple Groups. 2014. http://ideas.repec.org/c/boc/bocode/s457793.html
- 27. Wang L, Liu J, Chin DP. Progress in tuberculosis control and the evolving public‐health system in China. Lancet. 2007;369(9562):691‐696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cui Y, Shen H, Wang F, et al. A long‐term trend study of tuberculosis incidence in China, India and United States 1992‐2017: a joinpoint and age‐period‐cohort analysis. Int J Environ Res Public Health. 2020;17(9):3334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zheng JD, Peng ZB, Qin Y, Feng LZ, Li ZJ. [Current situation and challenges on the implementation of prevention and control programs regarding the seasonal influenza, in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2018;39(8):1041‐1044. [DOI] [PubMed] [Google Scholar]
- 30. National Diagnostic and Treatment Protocol Ffor Seasonal Influenza . (2019 edition):20220714. http://www.gov.cn/zhengce/zhengceku/201911/18/5453138/files/c8e357ca371d462b8a8f5626944ab940.pdf
- 31. Overview of Notifiable Infectious Diseases in China in December ; 2019:20220714. http://www.nhc.gov.cn/jkj/s6873/202001/ab5cbab3f8bc46c08cc7b6c4aef85441.shtml
- 32. Jin YC, Cai C, Qin QQ, Chen FF, Tang HL. [Epidemiological characteristics of newly reported HIV‐infected adolescents aged 15‐17 years outside school in China, 2011‐2019]. Zhonghua Liu Xing Bing Xue Za Zhi. 2022;43(1):32‐36. [DOI] [PubMed] [Google Scholar]
- 33. Han J, Li J, Zang CP, Liu YF. [Analysis of inter‐provincial movement and the effect of antiretroviral therapy of HIV/AIDS cases after first follow up in China, 2016‐2018]. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42(1):126‐130. [DOI] [PubMed] [Google Scholar]
- 34. He Y, Lu H. Clinical guidelines for the diagnosis and treatment of HIV/AIDS in China: their potential benefits and impact on public health. Biosci Trends. 2021;15(6):413‐417. [DOI] [PubMed] [Google Scholar]
- 35. Zhang W, Rui J, Cheng X, et al. Transmissibility of hand, foot, and mouth disease in 97 counties of China. Sci Rep. 2022;12(1):4103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wu T, Wu Z, Li YP. Dengue fever and dengue virus in the People's Republic of China. Rev Med Virol. 2022;32(1):e2245. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information.
Data Availability Statement
Our data was from the database of the China Information System for Disease Control and Prevention website (https://www.phsciencedata.cn/Share/ky_sjml.jsp?id=a56cd203-cd11-414d-9efa-d1583b97476f).


