Abstract
Aims
Epigenetic clocks are widely applied as surrogates for biological age in different tissues and/or diseases, including several neurodegenerative diseases. Despite white matter (WM) changes often being observed in neurodegenerative diseases, no study has investigated epigenetic ageing in white matter.
Methods
We analysed the performances of two DNA methylation‐based clocks, DNAmClockMulti and DNAmClockCortical, in post‐mortem WM tissue from multiple subcortical regions and the cerebellum, and in oligodendrocyte‐enriched nuclei. We also examined epigenetic ageing in control and multiple system atrophy (MSA) (WM and mixed WM and grey matter), as MSA is a neurodegenerative disease comprising pronounced WM changes and α‐synuclein aggregates in oligodendrocytes.
Results
Estimated DNA methylation (DNAm) ages showed strong correlations with chronological ages, even in WM (e.g., DNAmClockCortical, r = [0.80–0.97], p < 0.05). However, performances and DNAm age estimates differed between clocks and brain regions. DNAmClockMulti significantly underestimated ages in all cohorts except in the MSA prefrontal cortex mixed tissue, whereas DNAmClockCortical tended towards age overestimations. Pronounced age overestimations in the oligodendrocyte‐enriched cohorts (e.g., oligodendrocyte‐enriched nuclei, p = 6.1 × 10−5) suggested that this cell type ages faster. Indeed, significant positive correlations were observed between estimated oligodendrocyte proportions and DNAm age acceleration estimated by DNAmClockCortical (r > 0.31, p < 0.05), and similar trends were obtained with DNAmClockMulti. Although increased age acceleration was observed in MSA compared with controls, no significant differences were detected upon adjustment for possible confounders (e.g., cell‐type proportions).
Conclusions
Our findings show that oligodendrocyte proportions positively influence epigenetic age acceleration across brain regions and highlight the need to further investigate this in ageing and neurodegeneration.
Keywords: DNA methylation ageing, epigenetic clock, multiple system atrophy, oligodendrocytes, post‐mortem brain tissue, white matter
Estimates of DNA methylation age differed between clocks and brain regions. Pronounced age overestimations in oligodendrocyte‐enriched cohorts suggest that oligodendrocytes age faster than other brain cell types. Additionally, positive correlations were observed between oligodendrocyte proportions and DNA methylation age acceleration. Although increased age acceleration was observed in MSA compared with controls, no significant differences were detected after adjustment for possible confounders. These findings highlight the need to investigate further the influence of oligodendrocytes on ageing and neurodegeneration.
Key points.
DNAmClockCortical and DNAmClockMulti are applicable to white matter from different brain regions.
In white matter tissues of cortical and subcortical regions, DNAmClockCortical performs better than DNAmClockMulti.
DNAmClockCortical shows lower accuracy (performs sub‐optimally) in cerebellar white matter compared with DNAmClockMulti.
Using these two clocks, epigenetic age acceleration was not observed in MSA compared with controls upon adjustment for possible confounders such as cellular proportions, suggesting their limited applicability in diseases affecting specific cell types.
Oligodendrocyte proportions are positively correlated with epigenetic age acceleration across brain regions.
INTRODUCTION
DNA methylation‐based estimators of chronological age, termed ‘epigenetic clocks’, make use of penalised regression models such as elastic net regression to select signature CpG sites (CpGs) as biomarkers that correlate with chronological age [1, 2]. Multiple clocks have been developed for use as molecular indicators of DNA methylation (DNAm) ages in different human tissues such as peripheral blood [3], multi‐tissues (DNAmClockMulti) [1] and the brain cortex (DNAmClockCortical) [2]. These epigenetic clocks are being increasingly used to determine the biological age of tissues and organs in various contexts; epigenetic age acceleration has been reported in multiple tissues, including the peripheral blood and post‐mortem brain tissues, in neurodegenerative disorders such as Alzheimer's disease (AD), Huntington's disease (HD) and Parkinson's disease (PD) [4, 5, 6].
The DNAmClockMulti has been applied in tissues from several brain regions such as the dorsolateral prefrontal cortex (DLPFC) [6], frontal, occipital, temporal and parietal lobes, cerebellum, hippocampus, midbrain, caudate nucleus and cingulate gyrus [4, 7]; similarly, the DNAmClockCortical has specifically been tested in the dorsolateral prefrontal cortex and posterior cingulate cortex [8, 9]. However, the sensitivity of the different clocks to tissue‐specific changes (e.g., different cell‐type proportions) varies depending on the tissues used in the reference training data, with a higher sensitivity likely to be observed in tissue‐specific clocks compared with pan/multi‐tissue clocks [10]. Moreover, when clocks were trained using data from one tissue at a time, their performances in predicting age in another tissue worsened [11]. However, the performance of these clocks in tissues that are particularly enriched for specific brain cell types, such as oligodendrocytes in the case of white matter, remains unexplored.
About half of the human brain is made up of white matter, which primarily comprises myelinated axons and glial cell types such as astrocytes, microglia and oligodendrocytes, with oligodendrocytes being by far the most abundant cell type [12]. White matter has been shown to play prominent roles in the normal functioning of the brain including cognitive [13] and motor functions [14]. Many neurodegenerative diseases show white matter changes, including AD, PD and multiple system atrophy (MSA) [15, 16, 17]. MSA is a rare adult‐onset progressive neurodegenerative disorder with prominent white matter involvement [15]. MSA belongs to the group of α‐synucleinopathies along with PD and Dementia with Lewy bodies (DLB) [18]. However, pathological hallmarks of MSA include the abnormal accumulation of misfolded α‐synuclein primarily in the oligodendrocytes rather than in neurons, and these aggregates are termed glial cytoplasmic inclusions [19]. MSA is a predominantly sporadic disease, with a complex aetiology involving the interplay of genetic, epigenetic and environmental factors [20]. Recent epigenome‐wide association studies have revealed aberrant DNA methylation changes in the MSA post‐mortem brain tissue [21, 22, 23].
We, therefore, investigated the performances of DNAmClockMulti and DNAmClockCortical in white matter from multiple brain regions and compared them with tissues comprising a mixture of grey and white matter in neurologically healthy controls as well as in a disease context. As MSA is a neurodegenerative disease model involving white matter pathological hallmarks, we investigated if patients with MSA exhibited accelerated ageing in the white matter of different brain regions such as the cerebellum and frontal and occipital lobes, as well as prefrontal cortex grey and white matter mixed tissue.
MATERIALS AND METHODS
Cohort description
The first cohort (Cohort 1) consisted of white matter tissue carefully dissected from the cerebellum, and frontal and occipital lobes of post‐mortem brain tissues obtained from brains donated to the Queen Square Brain Bank. Cohort 1 comprised a total of 127 samples from MSA cases (N = 77) and neurologically healthy controls (N = 50), which included 93 samples from a previously published study [21] and 34 newly profiled samples obtained from the same brain bank. Cohort 2 consisted of samples from a publicly available dataset (GSE143157) comprising grey and white matter tissue mix from the prefrontal cortex of MSA cases (N = 40) and controls (N = 37) [22]. We further included a white matter cohort—Cohort 3, which consisted of control samples (N = 9) from the corpus callosum, the biggest white matter structure of the brain, obtained from a publicly available dataset (GSE109381) [24]. As MSA is characterised by oligodendroglial pathology, we included an additional Cohort 4, which consists of sorted SOX10+ (oligodendrocyte‐enriched) immunolabelled populations from bulk DLPFC healthy control tissue (N = 15) [25]. The demographic details of all cohorts including sample numbers and chronological age are described in Table S1.
DNA methylation profiling and data preprocessing
For the newly profiled samples from Cohort 1 (N = 34 samples), genomic DNA was extracted from frozen brain tissues using a previously established phenol‐chloroform‐isoamyl alcohol extraction method. Bisulphite conversion was then carried out with 750 ng of DNA using the EZ DNA Methylation Kit (Zymo Research, Irvine, USA), followed by genome‐wide methylation profiling using the Infinium HumanMethylationEPIC Bead Chip (Illumina). Bisulphite conversion and methylation profiling were carried out at UCL genomics, and the raw intensity files (.idat) were generated. Methylation profiles of 97 samples (a subset of Cohort 1) generated by Bettencourt et al. [21], 77 methylation profiles from the publicly available Cohort 2 [22] and 15 SOX10+ methylation profiles of Cohort 4 [25] had been previously generated using the Infinium HumanMethylationEPIC BeadChip (Illumina), whereas nine methylation profiles of Cohort 3 [24] had been previously generated using the Infinium HumanMethylation450K BeadChip (Illumina). All cohorts were subjected to harmonised quality control checks and preprocessing.
Raw intensity files for all cohorts were imported into R using the WateRmelon package [26]. The following preprocessing and quality control checks were performed: (i) Raw intensities were visualised to identify and filter out atypical and failed samples, (ii) outlier detection to identify and remove outliers, (iii) bisulphite conversion assessment, where intensities from the probes were converted into percentages and samples with <80% bisulphite conversion were removed, and (iv) probe filtering to identify poorly performing probes by assessing the bead counts and detection‐values. Samples with >1% probes above the 0.05 detection p‐value threshold, probes with a beadcount of <3 in 5% of the samples and sites for which over 1% of samples showed a detection p‐value >0.05 were discarded. Samples were also discarded if sex predictions did not match with phenotypic sex. Following the preprocessing, dasen normalisation was carried out. Cell‐type proportions of neuron‐enriched (NeuN+), oligodendrocyte‐enriched (SOX10+) and other glial brain cell type (NeuN−/SOX10−) populations in the bulk tissues were estimated using the CETYGO package (https://github.com/ds420/CETYGO) and a sorted cell‐type reference dataset as described by Shireby et al. [25]. CETYGO estimates cell proportions and quantifies the CEll TYpe deconvolution GOodness (CETYGO) score of a set of cellular heterogeneity variables derived from a genome‐wide DNA methylation profile for an individual sample by capturing the deviation between the DNAm profile of a sample and its expected profile.
DNA methylation age estimation
Normalised beta values were used for the estimation of DNA methylation (DNAm) ages using two established epigenetic clocks trained to predict chronologic age, the DNAmClockMulti [1], which employs 353 CpGs curated from analysis of DNA methylation from 51 different tissues and cell types, and the DNAmClockCortical [2] designed using 347 CpGs to specifically predict age in the human cortex. DNAm ages for DNAmClockMulti were calculated using the advanced analysis with normalisation, on the online calculator (http://dnamage.genetics.ucla.edu/). The DNAm ages for DNAmClockCortical were calculated as described by Shireby et al. [2].
Statistics
All statistical analyses were performed in R (ver. 4.1.1). For both clocks, DNAm age acceleration was calculated as (1) the difference between the predicted DNAm age and chronological age and (2) residuals obtained by linear regression of DNAm age on chronological age and adjusting for possible confounders such as cell proportions (either neuronal or oligodendroglial) and duplicated individuals with multiple data points. Cohort 1 consisted of a subset of tissues for multiple brain regions obtained from the same individuals, therefore, mixed effects linear regression models were implemented using the lme4 package (https://github.com/lme4/lme4/) [27], where DNAm age was regressed against chronological age, estimated cell proportions and individual. For the mixed‐effect regression models, chronological age and cellular proportions derived using CETYGO [25] were considered as fixed effects, and the individual's ID was included as a random effect. For Cohorts 2, 3 and 4, as there was only one sample per individual, we employed standard linear regression models where DNAm age was regressed with both age and cell proportion estimates. Furthermore, as post‐mortem interval (PMI) was available for Cohort 1, on a separate analysis, we also included PMI as a fixed effect in addition to chronological age and cell proportion estimates and included individual as a random effect in the mixed effects linear regression model. Correlations between chronological and epigenetic ages for the different groups were calculated using Pearson's coefficient. Comparisons across groups/brain regions were performed using the Kruskal–Wallis test, and pairwise comparisons between the groups (MSA vs. controls) within each brain region were performed using pairwise Wilcoxon test with the Benjamini–Hochberg multiple testing correction. Correlations between epigenetic age acceleration (i.e., residuals obtained by linear regression of DNAm age on chronological age) and cell‐type proportions (e.g., estimates of oligodendrocyte proportions) were calculated using Pearson's coefficient.
RESULTS
Comparison of the performances of DNAmClockMulti and DNAmClockCortical in white matter from different brain regions and correlations with chronological age
Using data derived from both neurologically healthy controls and MSA, we investigated the performances of both DNAmClockMulti and DNAmClockCortical in white matter dissected from the frontal and occipital lobes and cerebellum, as well as from the corpus callosum and sorted oligodendrocyte‐enriched nuclei (SOX10+), and compared them with prefrontal cortex tissue constituting a mix of grey and white matter. The composition of prefrontal cortex tissue resembles that of the datasets used to train and test both clocks. As expected, DNA methylation ages estimated with both clocks showed strong correlations with chronological ages in all brain regions, for both white matter and mixed tissues (Table 1). Overall, compared with the DNAmClockMulti, the DNAmClockCortical age estimates showed higher correlations with chronological age and lower errors for all cortical and subcortical regions, regardless of whether samples were from white matter or mixed tissues (Cohorts 1–4). The DNAmClockMulti age estimates, however, showed a stronger correlation with chronological age than the DNAmClockCortical for cerebellar white matter (Cohort 1).
TABLE 1.
Comparison of correlations between estimated DNA methylation age with DNAmClockMulti and DNAmClockCortical clocks and chronological age for the different brain regions and cohorts
| Tissue/region | Controls | MSA | Total | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | DNAmClockCortical | DNAmClockMulti | N | DNAmClockCortical | DNAmClockMulti | N | DNAmClockCortical | DNAmClockMulti | |||||||||||||
| r | err | p‐Value | r | err | p‐Value | r | err | p‐Value | r | err | p‐Value | r | err | p‐Value | r | err | p‐Value | ||||
| Cohort 1 | |||||||||||||||||||||
| Cerebellum (WM) | 21 | 0.46 | 3.6 | 0.036 | 0.75 | 5.8 | 9.00E‐05 | 41 | 0.74 | 5.9 | 3.20E‐08 | 0.8 | 3.8 | 3.50E‐10 | 62 | 0.8 | 5.4 | 6.20E‐15 | 0.88 | 4.5 | 4.60E‐21 |
| Frontal lobe (WM) | 23 | 0.82 | 5.1 | 1.70E‐06 | 0.74 | 12 | 5.40E‐05 | 26 | 0.83 | 5.4 | 1.60E‐07 | 0.81 | 8.3 | 5.30E‐07 | 49 | 0.86 | 5.2 | 2.50E‐15 | 0.81 | 9.7 | 1.80E‐12 |
| Occipital lobe (WM) | 6 | 0.9 | 2.6 | 0.014 | 0.83 | 16 | 0.041 | 10 | 0.78 | 5.3 | 0.078 | 0.85 | 8.7 | 0.0018 | 16 | 0.93 | 4.4 | 1.80E‐07 | 0.92 | 12 | 4.50E‐07 |
| Cohort 2 | |||||||||||||||||||||
| Prefrontal cortex (WM + GM) | 37 | 0.92 | 2.7 | 8.40E‐16 | 0.89 | 3.5 | 1.70E‐13 | 41 | 0.81 | 2.2 | 2.40E‐10 | 0.59 | 3 | 6.20E‐05 | 78 | 0.9 | 2.3 | 9.10E‐29 | 0.83 | 3 | 1.10E‐20 |
| Cohort 3 | |||||||||||||||||||||
| Corpus callosum | 9 | 0.97 | 3.6 | 1.50E‐05 | 0.93 | 8.3 | 0.00028 | ||||||||||||||
| Cohort 4 | |||||||||||||||||||||
| SOX10+ nuclei | 15 | 0.85 | 8.6 | 6.00E‐05 | 0.73 | 24 | 0.002 | ||||||||||||||
Abbreviations: err, median absolute deviation between the chronological and DNAm age; WM + GM, mix of white and grey matter; MSA, multiple system atrophy; r, correlation coefficient; WM, white matter.
For the healthy controls (Table 1), the strongest correlation was observed for the corpus callosum (Cohort 3) with DNAmClockCortical (r = 0.97), with a considerably lower error (median absolute difference, error = 3.6) when compared with that with DNAmClockMulti (r = 0.93, error = 8.3). This was followed by the prefrontal cortex grey and white matter mix (Cohort 2), where DNAmClockCortical showed a stronger correlation with similar error values (r = 0.92; error = 2.7) compared with DNAmClockMulti (r = 0.89; error = 3.5), followed by white matter from the occipital and frontal lobes (Cohort 1) (Table 1).
In MSA, correlations between the chronological age and the DNAmClockCortical age estimates were in general, similar or weaker than those observed for controls, except for the cerebellar white matter (Table 1). Moreover, error values were higher in all brain regions in MSA samples compared with that of controls; however, these differences did not reach statistical significance. Conversely, the performance of DNAmClockMulti significantly improved in the white matter tissues of MSA cases compared with controls (Table S2). However, the latter could be attributable to the lower chronological ages of the MSA cases (range 50–82 years) compared with controls (range 51–99 years), as previous reports suggest that DNAmClockMulti systematically underestimates DNAm age in individuals over ~60 years old and systematically overestimates it in individuals below ~60 years old [2].
Epigenetic age estimates vary considerably depending on the epigenetic clock used and the cellular composition of the studied tissues
We then compared the difference in the chronological age and the DNAm age estimates for the control and MSA groups predicted by the two clocks for the different cohorts comprising different brain regions and cellular compositions. Overall, DNAmClockCortical tended to overestimate age, especially for the MSA cases, with significant overestimations in the frontal lobe white matter and oligodendrocyte‐enriched nuclei, whereas DNAmClockMulti showed significant age underestimations in the white matter and oligodendrocyte‐enriched cohorts (Cohorts 1, 3, and 4) (Figure 1, Tables S3 and S4). The mean ages predicted by both DNAmClockMulti and DNAmClockCortical were closer to the actual chronological age for both control and MSA groups in the prefrontal cortex mixed tissue (Cohort 2) compared with the white matter cohorts. This result is expected, given this mixed tissue cohort is more similar to the tissue types used to train both clocks. As white matter is highly enriched for oligodendrocytes (up to 70%) [28], we included an additional cohort containing oligodendroglial‐enriched nuclei from control individuals to infer the effect of this cell type on epigenetic age estimates. For the oligodendroglial‐enriched nuclei, DNAmClockCortical significantly overestimated the age, whereas DNAmClockMulti significantly underestimated the age, similar to what was observed in white matter, but with higher error values (Figure 1, Table 1). The findings from white matter and oligodendroglial‐enriched nuclei suggest that the performances of epigenetic clocks in brain tissue are dependent on the cellular compositions of the tissues used.
FIGURE 1.
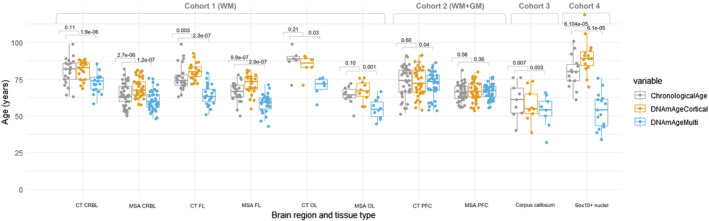
Chronological and DNAm ages for DNAmClockMulti and DNAmClockCortical for the different brain regions of control and multiple system atrophy (MSA) samples in all cohorts. CT CRBL, control cerebellum (WM); CT FL, control frontal lobe (WM); CT OL, control occipital lobe (WM); CT PFC, control prefrontal cortex (WM + GM); WM + GM, mix of white and grey matter; MSA CRBL, multiple system atrophy (MSA) cerebellum (WM); MSA FL, MSA frontal lobe (WM); MSA OL, MSA occipital lobe (WM); MSA PFC, MSA prefrontal cortex (WM + GM); WM, white matter; the p‐values were calculated using Wilcoxon signed rank exact test for paired samples.
Oligodendrocyte proportions are associated with epigenetic age acceleration
As DNA methylation patterns often are cell‐type specific, it is reasonable to hypothesise that differences in specific cell‐type proportions in a tissue sample will influence the estimates of epigenetic age based on DNA methylation levels and consequently epigenetic age acceleration. Previous work has demonstrated that a significant negative correlation exists between epigenetic age acceleration and the proportion of neurons in the prefrontal cortex [29]. We found the same direction of effect in our prefrontal cortex grey and white matter mix tissues with the DNAmClockCortical, with a significant negative correlation observed between epigenetic age acceleration and neuronal proportions (r = −0.47, p = 1.6 × 10−5) (Figure S1). As expected, in our white matter cohorts, the estimated neuronal proportions were minimal in frontal (mean 1.8 ± 0.6) and occipital lobes (mean 1.98 ± 1.6) as well as in the corpus callosum (mean 5.7 ± 0.8). Furthermore, there was no relationship between the residual neuronal proportions and epigenetic age acceleration in the white matter for these regions. The opposite was seen in the cerebellar white matter samples, where higher neuronal proportions were found, particularly in the MSA cases (mean 12.8 ± 12.7 vs. mean 7.8 ± 11.6 in the controls), and significant negative correlations were observed between the neuronal proportions and the epigenetic age acceleration measures derived from both clocks [DNAmClockCortical (r = −0.7, p = 2.4 × 10−10) and DNAmClockMulti (r = −0.54, p = 5.9 × 10−6)] (Figure S1).
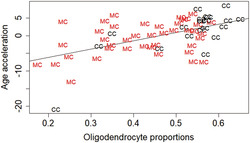
Lower neuronal proportions (i.e., higher glial proportions) have been associated with higher estimates of epigenetic ages [2] and, in this study, epigenetic ages are largely overestimated in oligodendrocytes (i.e., SOX10+ nuclei) by the DNAmClockCortical. This prompted us to interrogate whether oligodendrocyte proportions would be associated with epigenetic age acceleration. Up to now, proportions of brain cell‐type estimates obtained from DNA methylation data were restricted to neuronal versus glial cell types (with the CETS [30], minfi/wateRmelon packages [26, 31]). However, the glial group encompasses very heterogeneous cell types, from oligodendrocytes to microglia, astrocytes and other cells. By using a recently refined cell‐type deconvolution algorithm (CETYGO [25]), we dissected the proportions of oligodendrocytes from other glial cells in our cohorts. For estimates derived from both clocks, significant positive correlations were obtained between age acceleration measures and oligodendrocyte proportions for cerebellar, frontal and occipital white matter as well as for prefrontal mixed tissues (Figure 2). More details on separate correlations for controls and MSA cases can be found in Figure S2. The strongest correlations with DNAmClockCortical were found for control cerebellar white matter (r = 0.7, p = 0.00041), followed by control prefrontal cortex mixed tissue (r = 0.65, p = 1.3 × 10–0.5). For the corpus callosum (Cohort 3), the DNAmClockCortical estimates, in accordance with the other cohorts, showed a moderate positive correlation with the oligodendrocyte proportions, whereas the DNAmClockMulti showed the opposite, although none of these correlations reached statistical significance in this small cohort. Overall, epigenetic age acceleration estimates derived from DNAmClockCortical showed stronger correlations with oligodendrocyte proportions compared with that with DNAmClockMulti. This may suggest that the estimates from the DNAmClockCortical are more influenced by the variation in the oligodendrocyte composition of the tissue than those from the DNAmClockMulti. Weaker negative correlations were observed between age acceleration measures and other cell‐type proportions (NeuN−/SOX10−) for frontal and occipital white matter as well as for prefrontal mixed tissues, and no significant correlations were observed for cerebellar white matter (Figure S3). Correlations between age acceleration and the different cellular proportions were measured using the residuals obtained from regressing DNAm age against chronological age, and in the case of Cohort 1, by regressing against age as fixed effects and individual as a random effect. As for other covariates such as post‐mortem interval (PMI), available for Cohort 1 only, no significant correlation was observed between DNAm age and PMI. However, when PMI was included in the linear regression model, PMI was shown to have an effect on estimates from DNAmClockCortical (p = 0.04). Nevertheless, similar positive correlations as before were observed between age acceleration residuals and the oligodendrocyte proportions even after adjusting for PMI (Figure S4). Altogether, our data support a role for oligodendrocytes pushing towards older epigenetic age estimates, whereas it would be the other way around for neurons and the other brain cell types.
FIGURE 2.
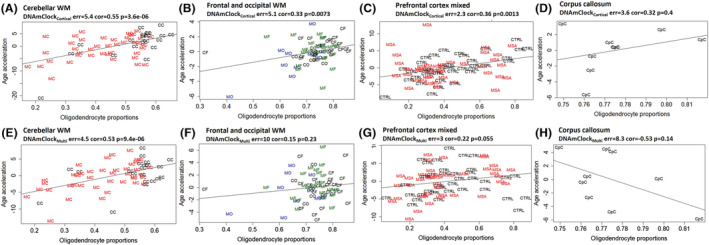
Association between epigenetic age acceleration and oligodendrocyte proportions for DNAmClockCortical and DNAmClockMulti in the different brain regions. (A–D) Age acceleration residuals (y‐axis) versus oligodendrocyte (SOX10+) proportions (x‐axis) for DNAmClockCortical in the different brain regions; (E–H) age acceleration residuals (y‐axis) versus oligodendrocyte (SOX10+) proportions (x‐axis) for DNAmClockMulti in the different brain regions. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; oligodendrocyte proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC, control cerebellum (WM); CF, control frontal lobe (WM); CO, control occipital lobe (WM); CpC, corpus callosum; GM, grey matter; MC, multiple system atrophy (MSA) cerebellum (WM); MF, MSA frontal lobe (WM); MO, MSA occipital lobe (WM); PFC, prefrontal cortex (WM + GM); WM, white matter.
Epigenetic age acceleration in the different brain regions in MSA
As increased epigenetic age acceleration has been reported to occur in neurodegenerative diseases [4, 5, 6], we investigated the presence of biological age acceleration in MSA when compared with controls based on results from the two clocks. For Cohort 1, with both DNAmClockMulti and DNAmClockCortical, increased age acceleration was observed in the MSA white matter of all brain regions when compared with the controls (Figure 3). Differences ranged between 2 years in the frontal lobe for DNAmClockCortical and 7 years in the occipital lobe for both DNAmClockMulti and DNAmClockCortical (Figure 3A,C). Pairwise comparisons revealed that these differences were statistically significant only in the occipital lobe for DNAmClockMulti (p = 0.042). In the prefrontal cortex mixed tissue (Cohort 2), ~2 years of acceleration was observed in the MSA samples with DNAmClockMulti (p = 0.038, Figure 3B). A smaller difference was found in the same direction with the DNAmClockCortical (Figure 3D).
FIGURE 3.
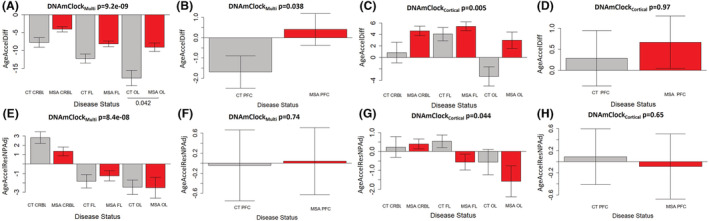
Age acceleration estimates for DNAmClockCortical and DNAmClockMulti in the different brain regions. (A–D) Age acceleration difference for DNAmClockMulti (A—Cohort 1; B—Cohort 2) and DNAmClockCortical (C—Cohort 1; D—Cohort 2) in the different brain regions, (E–H) age acceleration residual after adjusting for chronological age and neuronal proportions for the DNAmClockMulti (E—Cohort 1; F—Cohort 2) and DNAmClockCortical (G—Cohort 1; H—Cohort 2) in the different brain regions. CT CRBL, control cerebellum (WM); CT FL, control frontal lobe (WM); CT OL, control occipital lobe (WM); CT PFC, control prefrontal cortex (WM + GM); GM, grey matter; MSA CRBL, multiple system atrophy (MSA) cerebellum (WM); MSA FL, MSA frontal lobe (WM); MSA OL, MSA occipital lobe (WM); MSA PFC, MSA prefrontal cortex (WM + GM); WM, white matter; the p‐values for across group comparisons were calculated using the Kruskal–Wallis test, and p‐values for pairwise analysis between MSA and controls for each brain region were calculated using the Wilcoxon's test with Benjamini–Hochberg correction for multiple testing.
We then proceeded to verify whether the age acceleration could be influenced by possible confounding factors. Chronological age is known to have an impact on the DNAm age estimations [32]. As the chronological ages of the control group were generally higher than that of the MSA group for all brain regions, this had to be accounted for. In addition, for Cohort 1, although white matter tissue was carefully hand‐dissected and enriched for oligodendrocytes, neuronal contaminants could still be present, and therefore, the neuronal proportions needed to be accounted for. Also, Cohort 1 included multiple brain regions per individual. Therefore, the second measure of age acceleration corresponded to the residuals obtained by regressing DNAm age on chronological age and neuronal proportions as fixed effects and, in addition, by including individuals as a random effect in the case of Cohort 1. Upon adjusting for the abovementioned covariates, no significant age acceleration was observed in the MSA group in any of the brain regions (Figure 3E–H). Similar results were obtained after adjusting for oligodendrocyte proportions instead of neuronal proportions in these regression models (Figure S5). Even when accounting for PMI as a covariate in the linear regression models applied to Cohort 1, our previous observations remained unchanged, and no significant age acceleration was observed in the MSA group in any of the studied brain regions (Figure S6).
DISCUSSION
This is the first study, to our knowledge, that comprehensively analyses and describes the characteristics of DNAmClockMulti and DNAmClockCortical in white matter from multiple brain regions. The study compares the performances of the clocks in white matter from subcortical regions, corpus callosum and cerebellum, as well as in a mix of white and grey matter tissue obtained from the prefrontal cortex and in an oligodendrocyte‐enriched population. The study also considered MSA as a disease model involving white matter pathological changes and investigated the presence of increased DNAm age acceleration in different brain regions.
Both epigenetic clocks showed strong correlations with chronological age in both white matter as well as in mixed grey and white matter tissues. Lower error values for the DNAmClockCortical, and stronger correlations in white matter enriched tissues of the corpus callosum, frontal and occipital lobes and sorted SOX10+ nuclei, as well as for grey and white matter mix tissues of the prefrontal cortex indicate that the cortical clock is highly specific towards the hemispheric cortical and subcortical brain regions in both grey and white matter tissues. Conversely, stronger correlations with DNAmClockMulti in the cerebellum (white matter) indicate that the multi‐tissue clock performs better for regions of the brain other than cortical and subcortical regions. Furthermore, as reported by Shireby et al. [2], DNAmClockCortical shows reduced accuracy when applied to non‐cortical regions, which is exemplified by the weaker correlations observed between chronological and DNAm age, especially in the cerebellar control samples. Among the cortical and subcortical regions, DNAmClockCortical outperforms DNAmClockMulti, particularly in white matter tissues, with correlation coefficients and error values in ranges similar to those observed previously by Shireby et al. and Grodstein et al. for the dorsolateral prefrontal and posterior cingulate cortices [2, 8].
Lower neuronal proportions (i.e., higher glial proportions) have been previously associated with higher cortical DNAm ages [2]. Similarly, our results in the white matter, composed of glial cells, from frontal and occipital lobes as well as in the corpus callosum corroborate those findings. In the cerebellar samples, higher estimated neuronal proportions compared with the other white matter samples and significant negative correlations between the neuronal proportions and the DNAm age acceleration measures derived from both clocks were observed. These findings are not totally unexpected as they may result from (a) the fact that it is challenging to dissect cerebellar white matter without capturing any deep nuclei, particularly in the MSA cases where the cerebellar white matter is very atrophic, increasing the likelihood of deep cerebellar nuclei contamination; and (b) the fact that the algorithm used to deconvolute cell‐type proportions utilises reference datasets derived from cortical regions and this may influence cell proportion estimates in a region‐specific manner. Despite that, strong positive correlations between the oligodendrocyte proportions and the DNAm age acceleration were also observed in the cerebellar white matter, further corroborating previous findings and what we observed in the other brain regions. Recently, studies that identify epigenetic age acceleration in specific cell populations such as sorted neurons and glia have emerged and shown that the DNAm age of glial cells is significantly higher than that of neurons from the same individual [33]. Our white matter and sorted SOX10+ nuclei cohorts represent oligodendrocyte‐enriched populations. The overestimation of epigenetic age by the DNAmClockCortical, coupled with the positive correlations observed between oligodendrocyte proportions and epigenetic age acceleration in both clocks, suggests the influence of proportions of this cell type within tissues on the precision of DNAm age estimators. Furthermore, given that the proportions of other glial cell types (NeuN−/SOX10−) are negatively correlated with epigenetic age acceleration, this further supports the hypothesis that oligodendrocytes are the drivers of the accelerated ageing in glial cells compared with neurons of the same individual previously observed [33]. Therefore, in addition to tissue specificity, proportions of different cell types should also be taken into consideration to increase the accuracy of epigenetic clocks. Our results on the varied performances of the two clocks in different tissue types and regions within the brain further support the need for the development of specific clocks for different cell types and tissues as well as clocks specifically tailored in the context of brain ageing and disease as previously suggested [2, 9].
It is of note that DNAm states have been shown to play a part in driving cell division and the differentiation of oligodendrocyte precursor cells into mature oligodendrocytes [34]. Therefore, defective DNAm changes could lead to unbalances in the number and/or function of oligodendrocytes in ageing and neurodegenerative diseases. As the differentiation of oligodendrocyte precursor cells into mature myelinating oligodendrocytes depends on high metabolic and mitochondrial demand, these cells are particularly susceptible to oxidative stress, which affects oligodendrocyte precursor cell plasticity and differentiation capacity in ageing and neurodegenerative diseases [35]. Increased numbers of oligodendrocyte precursor cells have indeed been reported in several neurodegenerative diseases, including amyotrophic lateral sclerosis [36] and MSA [37, 38]. Given the observed positive correlations between oligodendrocyte proportions and DNAm age acceleration, in both MSA and ageing controls, one may hypothesise that disruptions in the oligodendrocyte differentiation process, due to oxidative stress and other factors, are involved in the observed relationship with DNAm age acceleration and oligodendrocyte sensitivity to ageing. As the algorithm used to predict cell‐type proportions cannot distinguish cell types within the oligodendrocyte lineage (e.g., oligodendrocyte precursor cells from mature oligodendrocytes), further studies would be necessary to dissect whether specific cells within the lineage underpin the observed correlations as well as to explore the potential applicability of oligodendrocyte proportions as an ageing biomarker.
Epigenetic age acceleration in specific brain regions has been reported in other neurodegenerative diseases such as AD and HD [4, 39]; however, no studies exist on epigenetic age acceleration in the brain tissues for any of the α‐synucleinopathies. Our rigorous multi‐step analysis of the epigenetic clocks in the context of MSA demonstrates that although increased DNAm age acceleration differences were observed in multiple brain regions in the MSA group compared with controls with both epigenetic clocks, no statistical significance was observed upon adjustment for chronological age, neuronal/oligodendrocyte proportions and duplicated individuals with multiple data points. Our results highlight the importance of accounting for confounders during the estimation of age acceleration and emphasise the need for researchers to interpret the results in ageing and disease models with caution.
Our study has several limitations, the sample sizes for each of the brain regions are relatively small, and future studies with larger sample sizes would be important to further validate our observations; in addition, the chronological age for the controls was considerably higher than that for the MSA cases, and although these differences were accounted for during the statistical analysis, different age ranges may have influenced the performance of both clocks differently for MSA cases and controls; finally, both clocks used in this study have not been specifically designed for white matter tissues, and follow‐up studies with more specialised epigenetic clocks are warranted. Moreover, we cannot exclude the possibility that other factors, including variable PMI or variable number of missing probes across cohorts, could have had an impact on DNAm age predictions. However, it is of note that when accounting for PMI in the regression models used for Cohort 1, it did not change our overall results. Additionally, after following the methodology described by McEwen et al. [40], it is unlikely that the missing probes would have considerably affected the precision of the DNAm age predictions. Notwithstanding, our data point towards important contributions of oligodendrocytes in brain tissue biological ageing and emphasise the need for additional studies on brain ageing and neurodegeneration focusing on this cell type.
In conclusion, this study demonstrates that both DNAmClockCortical and DNAmClockMulti showed a high correlation between DNAm age and chronological age, even in white matter, expanding the applicability of these clocks. As expected, performances and DNAm age estimates varied considerably between clocks and tissue types. With these available tools, we could not detect changes in epigenetic age acceleration in MSA compared with controls when accounting for known confounding factors. Additional important findings from this study consist of the positive correlations observed between epigenetic age acceleration and oligodendrocyte proportions across brain regions and tissue types, with the opposite being observed for all other brain cell types. This, together with previous reports of older DNAm ages in glial cells compared with neurons from the same individual, support differential biological ageing in different brain cell types, and the possibility of accelerated ageing in oligodendrocytes. Our findings highlight the need for cell type and tissue‐specific clocks and clocks that include shared markers of common aberrant epigenomic patterns underlying neurodegeneration to accurately dissect disease‐related DNAm age acceleration from normal ageing.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
ETHICS STATEMENT
Post‐mortem brain tissue donated to the Queen Square Brain Bank (QSBB) archives, including the tissue used to generate DNA methylation data for Cohort 1, is stored under a licence from the Human Tissue Authority (No. 12198). The QSBB brain donation programme and protocols have received ethical approval for donation and research by the NRES Committee London – Central [18/LO/0721].
AUTHOR CONTRIBUTIONS
Megha Murthy contributed to the experimental work, analysis and interpretation of data and drafted the manuscript. Conceição Bettencourt made substantial contributions to the conception and supervision of the work, data interpretation and writing of the manuscript. Gemma Shireby and Jonathan Mill provided data and code for some of the data analysis. Gemma Shireby, Yasuo Miki, Emmanuelle Viré, Tammaryn Lashley, Thomas T. Warner and Jonathan Mill contributed to data interpretation, edited the manuscript and provided critical suggestions. All authors have read and approved the final manuscript.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/nan.12872.
Supporting information
Figure S1 Association between age acceleration and neuronal proportions for DNAmClockCortical and DNAmClockMulti in the different brain regions. (a‐d) Age acceleration residuals (y‐axis) versus neuronal proportions (x‐axis) for DNAmClockCortical and (e‐h) Age acceleration residuals (y‐axis) versus neuronal proportions (x‐axis) for DNAmClockMulti in the different brain regions. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; neuronal proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC – control cerebellum (WM); MC – multiple system atrophy (MSA) cerebellum (WM); CF – control frontal lobe (WM); MF – MSA frontal lobe (WM); CO – control occipital lobe (WM); MO – MSA occipital lobe (WM); PFC – prefrontal cortex (GM + WM), CpC – Corpus callosum; WM – white matter; GM – grey matter.
Figure S2 Association between age acceleration and oligodendrocyte proportions for the multiple system atrophy (MSA) cases and control groups for DNAmClockCortical and DNAmClockMulti in the different brain regions (a‐g) Age acceleration residuals (y‐axis) versus oligodendrocyte (SOX10+) proportions (x‐axis) for the DNAmClockCortical and (h‐n) Age acceleration residuals (y‐axis) versus oligodendrocyte (SOX10+) proportions (x‐axis) for the DNAmClockMulti in the different brain regions. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; oligodendrocyte proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC – control cerebellum (WM); MC – MSA cerebellum (WM); CF – control frontal lobe (WM); MF – MSA frontal lobe (WM); CO – control occipital lobe (WM); MO – MSA occipital lobe (WM); PFC ‐ prefrontal cortex (GM + WM); CpC – Corpus callosum; WM – white matter; GM – grey matter.
Figure S3 Association between age acceleration and other glial cell type (NeuN‐/SOX10‐) populations for DNAmClockCortical and DNAmClockMulti clocks in the different brain regions. (a‐d) Age acceleration residuals (y‐axis) versus other brain cell type (NeuN‐/SOX10‐) proportions (x‐axis) for the DNAmClockCortical and (e‐h) Age acceleration residuals (y‐axis) versus other brain cell type (NeuN‐/SOX10‐) proportions (x‐axis) for the DNAmClockMulti in the different brain regions. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; NeuN‐/SOX10‐ proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC – control cerebellum (WM); MC – multiple system atrophy (MSA) cerebellum (WM); CF – control frontal lobe (WM); MF – MSA frontal lobe (WM); CO – control occipital lobe (WM); MO – MSA occipital lobe (WM); PFC ‐ prefrontal cortex (GM + WM), CpC – Corpus callosum; WM – white matter; GM – grey matter.
Figure S4 Association between age acceleration and the different cell type proportions for DNAmClockCortical and DNAmClockMulti in the different brain regions after including post‐mortem interval (PMI) as a covariate in cohort 1 regression models. (a‐d) Age acceleration residuals (y‐axis) versus oligodendrocyte (NeuN‐/SOX10+) proportions (x‐axis) for both clocks; (e‐h) age acceleration residuals (y‐axis) versus neuronal (NeuN+/SOX10‐) proportions (x‐axis) for both clocks; (i‐l) age acceleration residuals (y‐axis) versus other glial cell type (NeuN‐/SOX10‐) proportions (x‐axis) for both clocks. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; cell proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC – control cerebellum (WM); MC – multiple system atrophy (MSA) cerebellum (WM); CF – control frontal lobe (WM); MF – MSA frontal lobe (WM); CO – control occipital lobe (WM); MO – MSA occipital lobe (WM); WM – white matter.
Figure S5 Age acceleration estimation after adjusting for oligodendrocyte proportions for DNAmClockCortical and DNAmClockMulti in the different brain regions (a‐d) Acceleration residual after adjusting for chronological age and oligodendrocyte proportions for the DNAmClockMulti (a ‐ cohort 1; b ‐ cohort 2) and DNAmClockCortical (c ‐ cohort 1; d ‐ cohort 2) in the different brain regions. The p‐values for across group comparisons were calculated using the Kruskal‐Wallis test and p‐values for pairwise analysis between MSA and controls for each brain region were calculated using the Wilcoxon's test with Benjamini‐Hochberg correction for multiple testing. CT CRBL – control cerebellum (WM); MSA CRBL – multiple system atrophy (MSA) cerebellum (WM); CT FL – control frontal lobe (WM); MSA FL – MSA frontal lobe (WM); CT OL – control occipital lobe (WM); MSA OL – MSA occipital lobe (WM); CT PFC – control prefrontal cortex (GM + WM); MSA PFC – MSA prefrontal cortex (GM + WM); WM – white matter; GM – grey matter.
Figure S6 Age acceleration estimation for cohort 1 in the different brain regions for (a) DNAmClockCortical and (b) DNAmClockMulti after adjusting for post‐mortem interval (PMI) (Chronological age, neuronal proportions, replicate individuals and PMI were included in the regression model). CT CRBL ‐ control cerebellum (WM); MSA CRBL – multiple system atrophy (MSA) cerebellum (WM); CT FL – control frontal lobe (WM); MSA FL – MSA frontal lobe (WM); CT OL – control occipital lobe (WM); MSA OL – MSA occipital lobe (WM); CT PFC – control prefrontal cortex (GM + WM); MSA PFC – MSA prefrontal cortex (GM + WM); WM – white matter; GM – grey matter. The p‐values for across group comparisons were calculated using the Kruskal‐Wallis test and p‐values for pairwise analysis between MSA and controls for each brain region were calculated using the Wilcoxon's test with Benjamini‐Hochberg correction for multiple testing.
Table S1 Cohort demographics.
Table S2 Difference in median absolute deviation between controls and MSA for DNAmClockMulti and DNAmClockCortical.
Table S3 Mean chronological and DNAm ages for DNAmClockMulti and DNAmClockCortical for all brain regions of control and MSA samples.
Table S4: Mean chronological and DNAm ages for DNAmClockMulti and DNAmClockCortical for control and MSA samples for all cohorts and brain regions.
ACKNOWLEDGEMENTS
The authors would like to thank Dr Sandrine Foti and Ms Gaganjit Kaur Madhan (MSc) for Cohort 1 sample processing and UCL Genomics centre for advice and processing of the EPIC arrays. Queen Square Brain Bank for Neurological Disorders receives support from the Reta Lila Weston Institute of Neurological Studies and the Medical Research Council. MM is supported by a grant from the Multiple System Atrophy Trust awarded to CB. GS was supported by a PhD studentship from the Alzheimer's Society awarded to JM. TL is supported by an Alzheimer's Research UK Senior Fellowship. TTW is supported by the Reta Lila Weston Trust and the MRC (N013255/1). CB is supported by the Multiple System Atrophy Trust and Alzheimer's Research UK.
Murthy M, Shireby G, Miki Y, et al. Epigenetic age acceleration is associated with oligodendrocyte proportions in MSA and control brain tissue. Neuropathol Appl Neurobiol. 2023;49(1):e12872. doi: 10.1111/nan.12872
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in GEO at https://www.ncbi.nlm.nih.gov/geo, accession numbers GSE143157 and GSE109381. Additional data is available in supplementary materials and upon request from the authors.
REFERENCES
- 1. Horvath S. DNA methylation age of human tissues and cell types. Genome Biol. 2013;14(10):R115. doi: 10.1186/gb-2013-14-10-r115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shireby GL, Davies JP, Francis PT, et al. Recalibrating the epigenetic clock: implications for assessing biological age in the human cortex. Brain. 2020;143(12):3763‐3775. doi: 10.1093/brain/awaa334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hannum G, Guinney J, Zhao L, et al. Genome‐wide methylation profiles reveal quantitative views of human aging rates. Mol Cell. 2013;49(2):359‐367. doi: 10.1016/j.molcel.2012.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Horvath S, Langfelder P, Kwak S, et al. Huntington's disease accelerates epigenetic aging of human brain and disrupts DNA methylation levels. Aging (Albany NY). 2016;8(7):1485‐1512. doi: 10.18632/aging.101005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Horvath S, Ritz BR. Increased epigenetic age and granulocyte counts in the blood of Parkinson's disease patients. Aging (Albany NY). 2015;7(12):1130‐1142. doi: 10.18632/aging.100859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Levine ME, Lu AT, Bennett DA, Horvath S. Epigenetic age of the pre‐frontal cortex is associated with neuritic plaques, amyloid load, and Alzheimer's disease related cognitive functioning. Aging (Albany NY). 2015;7(12):1198‐1211. doi: 10.18632/aging.100864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Horvath S, Mah V, Lu AT, et al. The cerebellum ages slowly according to the epigenetic clock. Aging (Albany NY). 2015;7(5):294‐306. doi: 10.18632/aging.100742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grodstein F, Lemos B, Yu L, Iatrou A, De Jager PL, Bennett DA. Characteristics of epigenetic clocks across blood and brain tissue in older women and men. Front Neurosci. 2020;14:555307. doi: 10.3389/fnins.2020.555307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Grodstein F, Lemos B, Yu L, et al. The association of epigenetic clocks in brain tissue with brain pathologies and common aging phenotypes. Neurobiol Dis. 2021;157:105428. doi: 10.1016/j.nbd.2021.105428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Castle JR, Lin N, Liu J, et al. Estimating breast tissue‐specific DNA methylation age using next‐generation sequencing data. Clin Epigenetics. 2020;12(1):45. doi: 10.1186/s13148-020-00834-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Porter HL, Brown CA, Roopnarinesingh X, et al. Many chronological aging clocks can be found throughout the epigenome: implications for quantifying biological aging. Aging Cell. 2021;20(11):e13492. doi: 10.1111/acel.13492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fields RD. Neuroscience. Change in the brain's white matter. Science. 2010;330(6005):768‐769. doi: 10.1126/science.1199139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ohlhauser L, Parker AF, Smart CM, Gawryluk JR. Alzheimer's disease neuroimaging I. White matter and its relationship with cognition in subjective cognitive decline. Alzheimers Dement (Amst). 2019;11(1):28‐35. doi: 10.1016/j.dadm.2018.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sampaio‐Baptista C, Khrapitchev AA, Foxley S, et al. Motor skill learning induces changes in white matter microstructure and myelination. J Neurosci. 2013;33(50):19499‐19503. doi: 10.1523/JNEUROSCI.3048-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Del Campo N, Phillips O, Ory‐Magne F, et al. Broad white matter impairment in multiple system atrophy. Hum Brain Mapp. 2021;42(2):357‐366. doi: 10.1002/hbm.25227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mito R, Raffelt D, Dhollander T, et al. Fibre‐specific white matter reductions in Alzheimer's disease and mild cognitive impairment. Brain. 2018;141(3):888‐902. doi: 10.1093/brain/awx355 [DOI] [PubMed] [Google Scholar]
- 17. Ogawa T, Hatano T, Kamagata K, et al. White matter alterations in Parkinson's disease with levodopa‐induced dyskinesia. Parkinsonism Relat Disord. 2021;90:8‐14. doi: 10.1016/j.parkreldis.2021.07.021 [DOI] [PubMed] [Google Scholar]
- 18. Meissner WG, Fernagut PO, Dehay B, et al. Multiple system atrophy: recent developments and future perspectives. Mov Disord. 2019;34(11):1629‐1642. doi: 10.1002/mds.27894 [DOI] [PubMed] [Google Scholar]
- 19. Jellinger KA. Multiple system atrophy: an oligodendroglioneural synucleinopathy. J Alzheimers Dis. 2018;62(3):1141‐1179. doi: 10.3233/JAD-170397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sturm E, Stefanova N. Multiple system atrophy: genetic or epigenetic? Exp Neurobiol. 2014;23(4):277‐291. doi: 10.5607/en.2014.23.4.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bettencourt C, Foti SC, Miki Y, et al. White matter DNA methylation profiling reveals deregulation of HIP1, LMAN2, MOBP, and other loci in multiple system atrophy. Acta Neuropathol. 2020;139(1):135‐156. doi: 10.1007/s00401-019-02074-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rydbirk R, Folke J, Busato F, et al. Epigenetic modulation of AREL1 and increased HLA expression in brains of multiple system atrophy patients. Acta Neuropathol Commun. 2020;8(1):29. doi: 10.1186/s40478-020-00908-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. de Boni L, Gasparoni G, Welle A, et al. Epigenetic and gene expression changes of neuronal cells from MSA patients are pronounced in enzymes for cell metabolism and calcium‐regulated protein kinases. Acta Neuropathol. 2021;142(4):781‐783. doi: 10.1007/s00401-021-02357-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Capper D, Jones DTW, Sill M, et al. DNA methylation‐based classification of central nervous system tumours. Nature. 2018;555(7697):469‐474. doi: 10.1038/nature26000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shireby G, Dempster E, Policicchio S, et al. DNA methylation signatures of Alzheimer's disease neuropathology in the cortex are primarily driven by variation in non‐neuronal cell‐types. bioRxiv. 2022; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pidsley R, YW CC, Volta M, Lunnon K, Mill J, Schalkwyk LC. A data‐driven approach to preprocessing Illumina 450K methylation array data. BMC Genomics. 2013;14(1):293. doi: 10.1186/1471-2164-14-293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest package: tests in linear mixed effects models. J Stat Softw. 2017;82(13):1‐26. doi: 10.18637/jss.v082.i13 [DOI] [Google Scholar]
- 28. Hofmann K, Rodriguez‐Rodriguez R, Gaebler A, Casals N, Scheller A, Kuerschner L. Astrocytes and oligodendrocytes in grey and white matter regions of the brain metabolize fatty acids. Sci Rep. 2017;7(1):10779. doi: 10.1038/s41598-017-11103-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lu AT, Hannon E, Levine ME, et al. Genetic architecture of epigenetic and neuronal ageing rates in human brain regions. Nat Commun. 2017;8(1):15353. doi: 10.1038/ncomms15353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Guintivano J, Aryee MJ, Kaminsky ZA. A cell epigenotype specific model for the correction of brain cellular heterogeneity bias and its application to age, brain region and major depression. Epigenetics. 2013;8(3):290‐302. doi: 10.4161/epi.23924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Aryee MJ, Jaffe AE, Corrada‐Bravo H, et al. Minfi: a flexible and comprehensive Bioconductor package for the analysis of Infinium DNA methylation microarrays. Bioinformatics. 2014;30(10):1363‐1369. doi: 10.1093/bioinformatics/btu049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. El Khoury LY, Gorrie‐Stone T, Smart M, et al. Systematic underestimation of the epigenetic clock and age acceleration in older subjects. Genome Biol. 2019;20(1):283. doi: 10.1186/s13059-019-1810-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Horvath S, Oshima J, Martin GM, et al. Epigenetic clock for skin and blood cells applied to Hutchinson Gilford progeria syndrome and ex vivo studies. Aging (Albany NY). 2018;10(7):1758‐1775. doi: 10.18632/aging.101508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tiane A, Schepers M, Riemens R, et al. DNA methylation regulates the expression of the negative transcriptional regulators ID2 and ID4 during OPC differentiation. Cell Mol Life Sci. 2021;78(19‐20):6631‐6644. doi: 10.1007/s00018-021-03927-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Spaas J, van Veggel L, Schepers M, et al. Oxidative stress and impaired oligodendrocyte precursor cell differentiation in neurological disorders. Cell Mol Life Sci. 2021;78(10):4615‐4637. doi: 10.1007/s00018-021-03802-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kang SH, Li Y, Fukaya M, et al. Degeneration and impaired regeneration of gray matter oligodendrocytes in amyotrophic lateral sclerosis. Nat Neurosci. 2013;16(5):571‐579. doi: 10.1038/nn.3357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ahmed Z, Asi YT, Lees AJ, Revesz T, Holton JL. Identification and quantification of oligodendrocyte precursor cells in multiple system atrophy, progressive supranuclear palsy and Parkinson's disease. Brain Pathol. 2013;23(3):263‐273. doi: 10.1111/j.1750-3639.2012.00637.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ettle B, Schlachetzki JCM, Winkler J. Oligodendroglia and myelin in neurodegenerative diseases: more than just bystanders? Mol Neurobiol. 2016;53(5):3046‐3062. doi: 10.1007/s12035-015-9205-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pellegrini C, Pirazzini C, Sala C, et al. A meta‐analysis of brain DNA methylation across sex, age, and Alzheimer's disease points for accelerated epigenetic aging in neurodegeneration. Front Aging Neurosci. 2021;13:639428. doi: 10.3389/fnagi.2021.639428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. McEwen LM, Jones MJ, Lin DTS, et al. Systematic evaluation of DNA methylation age estimation with common preprocessing methods and the Infinium MethylationEPIC BeadChip array. Clin Epigenetics. 2018;10(1):123. doi: 10.1186/s13148-018-0556-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Association between age acceleration and neuronal proportions for DNAmClockCortical and DNAmClockMulti in the different brain regions. (a‐d) Age acceleration residuals (y‐axis) versus neuronal proportions (x‐axis) for DNAmClockCortical and (e‐h) Age acceleration residuals (y‐axis) versus neuronal proportions (x‐axis) for DNAmClockMulti in the different brain regions. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; neuronal proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC – control cerebellum (WM); MC – multiple system atrophy (MSA) cerebellum (WM); CF – control frontal lobe (WM); MF – MSA frontal lobe (WM); CO – control occipital lobe (WM); MO – MSA occipital lobe (WM); PFC – prefrontal cortex (GM + WM), CpC – Corpus callosum; WM – white matter; GM – grey matter.
Figure S2 Association between age acceleration and oligodendrocyte proportions for the multiple system atrophy (MSA) cases and control groups for DNAmClockCortical and DNAmClockMulti in the different brain regions (a‐g) Age acceleration residuals (y‐axis) versus oligodendrocyte (SOX10+) proportions (x‐axis) for the DNAmClockCortical and (h‐n) Age acceleration residuals (y‐axis) versus oligodendrocyte (SOX10+) proportions (x‐axis) for the DNAmClockMulti in the different brain regions. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; oligodendrocyte proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC – control cerebellum (WM); MC – MSA cerebellum (WM); CF – control frontal lobe (WM); MF – MSA frontal lobe (WM); CO – control occipital lobe (WM); MO – MSA occipital lobe (WM); PFC ‐ prefrontal cortex (GM + WM); CpC – Corpus callosum; WM – white matter; GM – grey matter.
Figure S3 Association between age acceleration and other glial cell type (NeuN‐/SOX10‐) populations for DNAmClockCortical and DNAmClockMulti clocks in the different brain regions. (a‐d) Age acceleration residuals (y‐axis) versus other brain cell type (NeuN‐/SOX10‐) proportions (x‐axis) for the DNAmClockCortical and (e‐h) Age acceleration residuals (y‐axis) versus other brain cell type (NeuN‐/SOX10‐) proportions (x‐axis) for the DNAmClockMulti in the different brain regions. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; NeuN‐/SOX10‐ proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC – control cerebellum (WM); MC – multiple system atrophy (MSA) cerebellum (WM); CF – control frontal lobe (WM); MF – MSA frontal lobe (WM); CO – control occipital lobe (WM); MO – MSA occipital lobe (WM); PFC ‐ prefrontal cortex (GM + WM), CpC – Corpus callosum; WM – white matter; GM – grey matter.
Figure S4 Association between age acceleration and the different cell type proportions for DNAmClockCortical and DNAmClockMulti in the different brain regions after including post‐mortem interval (PMI) as a covariate in cohort 1 regression models. (a‐d) Age acceleration residuals (y‐axis) versus oligodendrocyte (NeuN‐/SOX10+) proportions (x‐axis) for both clocks; (e‐h) age acceleration residuals (y‐axis) versus neuronal (NeuN+/SOX10‐) proportions (x‐axis) for both clocks; (i‐l) age acceleration residuals (y‐axis) versus other glial cell type (NeuN‐/SOX10‐) proportions (x‐axis) for both clocks. Age acceleration residuals were obtained by regressing DNA methylation age against confounding factors, including chronological age; cell proportions were obtained using a DNA methylation‐based cell‐type deconvolution algorithm. The correlation coefficient and p‐values shown were calculated using Pearson correlation. CC – control cerebellum (WM); MC – multiple system atrophy (MSA) cerebellum (WM); CF – control frontal lobe (WM); MF – MSA frontal lobe (WM); CO – control occipital lobe (WM); MO – MSA occipital lobe (WM); WM – white matter.
Figure S5 Age acceleration estimation after adjusting for oligodendrocyte proportions for DNAmClockCortical and DNAmClockMulti in the different brain regions (a‐d) Acceleration residual after adjusting for chronological age and oligodendrocyte proportions for the DNAmClockMulti (a ‐ cohort 1; b ‐ cohort 2) and DNAmClockCortical (c ‐ cohort 1; d ‐ cohort 2) in the different brain regions. The p‐values for across group comparisons were calculated using the Kruskal‐Wallis test and p‐values for pairwise analysis between MSA and controls for each brain region were calculated using the Wilcoxon's test with Benjamini‐Hochberg correction for multiple testing. CT CRBL – control cerebellum (WM); MSA CRBL – multiple system atrophy (MSA) cerebellum (WM); CT FL – control frontal lobe (WM); MSA FL – MSA frontal lobe (WM); CT OL – control occipital lobe (WM); MSA OL – MSA occipital lobe (WM); CT PFC – control prefrontal cortex (GM + WM); MSA PFC – MSA prefrontal cortex (GM + WM); WM – white matter; GM – grey matter.
Figure S6 Age acceleration estimation for cohort 1 in the different brain regions for (a) DNAmClockCortical and (b) DNAmClockMulti after adjusting for post‐mortem interval (PMI) (Chronological age, neuronal proportions, replicate individuals and PMI were included in the regression model). CT CRBL ‐ control cerebellum (WM); MSA CRBL – multiple system atrophy (MSA) cerebellum (WM); CT FL – control frontal lobe (WM); MSA FL – MSA frontal lobe (WM); CT OL – control occipital lobe (WM); MSA OL – MSA occipital lobe (WM); CT PFC – control prefrontal cortex (GM + WM); MSA PFC – MSA prefrontal cortex (GM + WM); WM – white matter; GM – grey matter. The p‐values for across group comparisons were calculated using the Kruskal‐Wallis test and p‐values for pairwise analysis between MSA and controls for each brain region were calculated using the Wilcoxon's test with Benjamini‐Hochberg correction for multiple testing.
Table S1 Cohort demographics.
Table S2 Difference in median absolute deviation between controls and MSA for DNAmClockMulti and DNAmClockCortical.
Table S3 Mean chronological and DNAm ages for DNAmClockMulti and DNAmClockCortical for all brain regions of control and MSA samples.
Table S4: Mean chronological and DNAm ages for DNAmClockMulti and DNAmClockCortical for control and MSA samples for all cohorts and brain regions.
Data Availability Statement
The data that support the findings of this study are available in GEO at https://www.ncbi.nlm.nih.gov/geo, accession numbers GSE143157 and GSE109381. Additional data is available in supplementary materials and upon request from the authors.


