Abstract
Objectives
Informal caregiving is becoming increasingly important in dementia care, but causes a considerable burden on caregivers which impacts their wellbeing. We aimed to develop and pilot test a digital monitoring tool (REsilience Monitor for INformal caregivers in Dementia [REMIND]) for wellbeing and resilience of informal caregivers to provide timely support and thereby prevent their overburden and eventually crises admissions of persons with dementia.
Methods
A human‐centered design method based on co‐creation with informal caregivers and professionals was used to design REMIND. During co‐creation meetings and in‐between sprint sessions, a point of focus was formulated, and a prototype was created. Case manager‐caregiver duos pilot‐tested REMIND for 3 months. Semi‐structured interviews were conducted to determine usability and acceptability. Thematic analysis was applied to the transcripts.
Results
Informal caregivers and professionals with varying backgrounds participated in three co‐creation meetings. Defined point of focus was to develop a tool that is able to provide insight into the experienced burden of informal caregivers. The REMIND prototype consisted of weekly questions about wellbeing and resilience for informal caregivers and a dashboard with answers for case managers. Eight case managers and 13 informal caregivers considered REMIND easy‐to‐use. Informal caregivers mentioned that REMIND stimulated self‐reflection. Case managers appreciated the tool's ability to gain insight in the actual wellbeing of informal caregivers.
Conclusions
The REMIND tool developed in co‐creation with end‐users potentially increases insight in actual wellbeing of informal caregivers for both caregivers and case managers. A long‐term (controlled) follow‐up study is needed to evaluate REMIND's impact on caregiver burden and crisis admissions.
Keywords: case management, dementia, informal caregiver support, informal caregiver wellbeing, monitoring, primary care
Key points
Informal caregivers find it difficult to acknowledge feeling overburdened to healthcare professionals but also to themselves.
Healthcare professionals often do not notice informal caregiver overburden and therefore cannot provide timely support.
A monitoring tool enables informal caregivers to self‐reflect on their wellbeing.
Digital monitoring of wellbeing and burden facilitates informal caregivers to easily report their burden to a healthcare professional.
Healthcare professionals gained better insights about the actual wellbeing of informal caregivers by using the monitoring tool.
1. INTRODUCTION
The majority of people with dementia live at home, often resulting in complex care situations in the primary care setting. 1 A substantial part of the care for these people is provided by informal caregivers. Informal care is non‐professional care provided by someone from a person's social environment, usually a partner or child. 2 Providing this care causes a considerable burden on informal caregivers, 3 it is therefore essential that these informal caregivers experience sufficient support to perform their caregiving tasks.
In the Netherlands, people with dementia and their informal caregivers receive support from a case manager, who coordinates the care and examines the informal caregiver's wellbeing a few times per year. 4 Still, 39% of informal caregivers for people with dementia experience a heavy burden and 14% feel overburdened. 4 These caregivers frequently feel stressed and frustrated, are depressed or have depressive symptoms 5 , 6 , 7 and their perceived burden increases the risk for institutionalization of people with dementia. 7 , 8 , 9 If wellbeing and resilience are preserved, the risk of overburden decreases. 10 , 11
Measuring resilience may importantly contribute to identification of informal caregivers in need of supportive interventions to improve their wellbeing. 12 If case managers have a better understanding of caregivers' resilience they can offer the right support at the right time. Adequate support will not only benefit the wellbeing of both the person with dementia and informal caregiver, but also society as a whole since it may decrease healthcare costs by reducing the number of unexpected hospital and nursing home admissions. 13 , 14
However, due to frequent fluctuations in wellbeing and resilience, 15 assessment only a few times a year, as is currently performed by Dutch case managers, may give a distorted view on informal caregivers' actual burden. Monitoring informal caregivers' burden frequently was suggested a promising solution. 5 , 16 It may reveal early deterioration of wellbeing and resilience, and subsequently enable timely interventions to decrease the development of mental health problems (e.g. depressive symptoms or overburden), increase their perseverance time 17 , 18 and reduce acute admissions.
Previous studies showed that informal caregivers experienced that monitoring can be beneficial, especially because it supports a shift from reactive to pro‐active care. 19 It remains unclear how monitoring should be executed to contribute to informal caregivers' wellbeing and decreased feelings of burden in this population and whether it could support case managers to apply timely interventions. User‐friendly tools to monitor the wellbeing of informal caregivers are also scarce, and refer to other conditions or combined interventions. 20 , 21 Therefore, we co‐creatively developed a digital tool to monitor informal caregivers' wellbeing and resilience to provide timely support which may eventually prevent or delay (acute) hospital and nursing home admissions. 22 , 23 The aim of this paper is to describe the development and pilot‐test the feasibility and acceptability of the tool.
2. METHODS
2.1. Design
Between November 2018 and February 2021, a human centered design approach based on co‐creation and iteration was used by inviting informal caregivers and healthcare professionals to participate in the development process of the tool. 24 , 25 We used the human centered design approach developed by the Hasso‐Plattner Institute of Design at Stanford (d.school). Their approach includes the empathize, define, ideate, prototype and test phase (see Figure 1). 26 Human centered design approach is an iterative non‐scientific design process in which the test phase is considered an essential part of the developmental process. In this study, we separate the first four HCD phases from the test phase. The first four phases were performed from a co‐design perspective without application of traditional scientific methods. In the test phase, feasibility and applicability of the tool were studied using a traditional qualitative study design.
FIGURE 1.
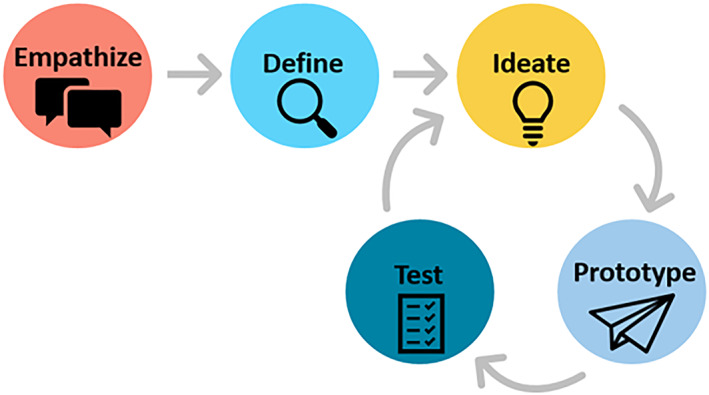
Graphical representation of a human centered design methodology.
2.2. Development
2.2.1. Participants
Potential end‐users, being informal caregivers and healthcare professionals, were invited via email to participate in the co‐creation meetings via the DementiaNet program. 27 , 28 Additionally, Informal caregivers recruited from the authors' network and via newsletters were asked to participate. For healthcare professionals purposive sampling was used by selecting persons who were: (1) working regularly with persons with dementia (in the primary care setting) and (2) working in the region Nijmegen or surroundings. We recruited professionals with varying backgrounds for all co‐creation meetings. The combination of end‐users present, differed between the meetings. The experts that prepared and participated in the meetings were researchers, clinicians, innovation experts and application developers involved in the project initiation; all were employees of the Radboudumc or application developers building the tool.
2.2.2. Methods
Three co‐creation meetings with end‐users and experts took place between November 2018 and July 2019, with a duration of 2 h. The overall structure of the meetings was similar; starting plenary with an introduction and purpose of the meetings, thereafter the topic was discussed in separate groups of professionals and informal caregivers. The meetings ended with a plenary discussion to exchange and specify ideas and search for similarity and synchronization. Moderators (experts from the project team) were present to lead the group‐ and plenary discussions. After each meeting, the project team discussed the outcomes and discussed the practical implications for the design of the tool. In between the group meetings, experts worked according to short sprint sessions 29 : after these short building trajectories the application and dashboard were discussed with the end‐users and consequently the project team made adjustments when needed. The meetings were audio recorded and verbal consent was asked at the start of the meeting.
1. Empathize
In the empathize phase, the wishes and needs of end‐users, healthcare professionals and informal caregivers, were identified by discussing the care pathway of persons with dementia in small groups to secure involvement of participants. During this first co‐creation session, current difficulties were also identified by the informal caregivers and professionals.
2. Define
During the second co‐creation meeting the exact problem, “point of focus,” the tool needed to address was determined during the define phase by discussing this in separate groups of healthcare professionals and informal caregivers. Thereafter, consensus was reached during a plenary discussion and possible digital solutions to address the point of focus were discussed.
3. Ideate
During the second co‐creation meeting the outcomes of the previous phases were summarized, application developers presented their first ideas based on these outcomes and concrete ideas for the lay‐out, user‐friendliness and content of the prototype were further discussed with the end‐users and experts. During the third co‐creation meeting, a schematic version of the tool was designed, presented and discussed with end‐users.
4. Prototype
Application developers build the prototype in consultation with innovation experts and the authors.
2.2.3. Co‐creation meetings
Co‐creation meetings were audio recorded, outcomes were narratively summarized and further discussed with the experts. The results of the previous meeting were directly used in the next meeting.
2.3. Testing
2.3.1. Participants
For pilot testing of the first working prototype, convenience sampling was used to include case managers and informal caregivers, as the Covid‐19 pandemic prevented purposive sampling. Case managers were recruited via the DementiaNet program 27 , 28 and authors' professional networks, no exclusion criteria were applied. Each case manager invited 1–2 informal caregivers caring for a relative with dementia to participate in the pilot.
2.3.2. Methods
5. Pilot test
Case managers and informal caregivers received a written manual and instruction movie with an explanation on how to register and use the tool (designed by the experts). Additional support was available by phone or via an in‐person meeting (DO). At the start of the pilot written informed consent was asked for using their data. They were asked to use the tool for 3 months.
After this pilot period, all case managers and informal caregivers participated in semi‐structured interviews on the experienced usability, acceptability and added value of the REsilience Monitor for INformal caregivers in Dementia (REMIND)‐tool. The interviews were conducted by an independent researcher via telephone due to COVID‐19 regulations. A topic list was developed for informal caregivers and case managers separately, focusing on users' experiences in terms of perceived benefits, major concerns, and further desired functionalities and improvements, based the structure of a study on eHealth for informal caregivers. 30 The interviews were audio recorded and transcribed verbatim. The duration of the interviews varied between 15 and 30 min. Informal caregivers' adherence rate was calculated with data retrieved from the backlog of the REMIND‐tool.
2.3.3. Analysis
ATLAS.ti version 8.4.20 was used to support thematic analysis with inductive approach of the interview transcripts. 31 , 32 Data saturation was reached since the last three interviews did not reveal new themes. 33 Open coding was applied to the transcripts by two trained researchers (DO: MSc; WV: BSc). They individually coded the first four interviews, consensus on these codes was reached through discussion between the researchers (DO, WV and MN: PhD). The rest of the interviews were coded by one researcher (WV) in consultation with two trained researchers (DO, MN) using previous codes when possible and formulating new codes if needed. Hereafter, codes were categorized in code groups (DO, WV). Based on the codes and code groups, categories and themes were formulated during group discussion with the research team (WV, DO, MN, MP: MD/PhD).
3. RESULTS
3.1. Development
We describe the results of the development of REMIND per phase of the human centered design method starting with the participants present at the meetings.
3.1.1. Participants end‐user meetings
Between 10 and 15 end‐users participated in each meeting. In total 24 end‐users participated, some end‐users (n = 10) were present multiple times. Informal caregivers and healthcare professionals with varying backgrounds were present. Table 1 describes the characteristics of the participants per meeting. The background of the experts involved are presented in appendix A1, though not all experts were present at each meeting.
TABLE 1.
Participant characteristics defined per meeting
| Meeting 1 | Meeting 2 | Meeting 3 | |
|---|---|---|---|
| Number of participants | 13 | 10 | 15 |
| Female, n | 12 | 6 | 14 |
| Dominant background, n | |||
| Healthcare professional | |||
| Case manager | 3 | 4 | 3 |
| General practitioner | 1 | 1 | 1 |
| Practice nurse | 1 | ‐ | 1 |
| Community nurse | 2 | 2 | 2 |
| Welfare worker | 2 | ‐ | 1 |
| Informal caregiver | 4 | 3 | 7 |
3.1.2. 1/2. Empathize and define
The following wishes and needs were identified during the first end‐user meeting. It emerged that most informal caregivers find it difficult to acknowledge feeling overburdened to professionals but also to themselves. Case managers are often not able to notice when an informal caregiver becomes overburdened, therefore they cannot provide timely support. Although case managers visit the client and informal caregiver regularly, the moment an informal caregiver becomes overburdened often happens at a different time. Informal caregivers mentioned they needed a tool where they can very easily report their increased burden to the case manager. This would also help them to reflect and become aware of their own burden. Case managers indicated the need to be sooner aware of informal caregivers' experienced burden. End‐users mentioned the tool should feel personal, just like a conversation. During an expert meeting, results were translated to concept screens for possible applications. During the second meeting the point of focus of the application was specified and defined: to monitor wellbeing and resilience of the informal caregiver to reduce crisis situations of the person with dementia.
3.1.3. 3. Ideate
During the second meeting, we presented concept screens of a possible application and dashboard, to verify and optimize the idea. Practical features were discussed, including the lay‐out, language, and for which informal caregivers (caring for a relative with early vs. advanced stage of dementia) the tool should be designed. Also, the content of the app was discussed, there should be a possibility for reflection on one's wellbeing. The idea emerged to frequently assess informal caregivers' wellbeing through weekly questions. By analyzing the answers over time, deterioration in wellbeing could then be noticed by case managers. Possible topics for questions were based on the literature 10 , 12 , 34 and emerged during the meeting: perseverance time, stress, coping, physical and mental condition of the person with dementia and the experienced social support. During expert meetings, standardized questionnaires were collected, and additional questions were formulated. Standard questionnaires to measure resilience and wellbeing included the topics perseverance time, 35 burden, 36 social support, 37 physical health, 38 mental health, 39 person with dementia, 40 , 41 and resilience. 42 , 43
In a third meeting with end‐users adjusted concept screens of the application and dashboard for case managers were presented and their relevance and user friendliness were discussed. During the meeting, the previously collected questionnaires and self‐formulated questions were evaluated until consensus was reached among end‐users. Furthermore, end‐users indicated it would be viable to fill in approximately seven questions per week.
During an expert meeting, we used the output of the meeting and the standardized questionnaires to construct two sets of questions for weekly assessment for pilot testing covering various topics, see Table 2.
TABLE 2.
Two sets of questions for weekly assessment by informal caregivers using the REMIND‐tool
| Set | Category | Question |
|---|---|---|
| 1 | Social support | Do you see enough possibilities to find alternative informal care (e.g., when you are ill or need a day off)? 37 |
| Reciprocity | Do you have enough headspace to listen to the problems of family members and friends? 36 | |
| Physical health | Did you have had any physical complaints the past week? 38 | |
| Wellbeing PwD | The person with dementia is satisfied with the day‐to‐day activities. 41 | |
| Own activities | There are enough moments where I am able to relax. 36 | |
| 2 | Mental health | Do you still enjoy things? 39 |
| Small crises | How many difficult situations did you experience with your loved one with dementia the past month? (e.g., incontinence or wandering) | |
| Social support | Do you experience incomprehension about your role as informal caregiver from your surroundings? 38 | |
| Burden | Do you ever fall out to your loved one with dementia? 43 | |
| Burden | If the care for your loved one continuous like it is now, for how long can you maintain the situation? 35 |
Abbreviation: PwD, person with dementia.
3.1.4. 4. Prototype
During expert meetings, we iteratively translated all information collected to design the tool for pilot testing which led to the first prototype of REMIND. REMIND consists of a weekly assessment for informal caregivers and a dashboard for case managers where answers are depicted as trajectories over time. Hereby, both informal caregivers themselves and their case managers obtain better insight into the wellbeing of the informal caregiver. When wellbeing of the informal caregiver deteriorates case managers can offer support in time. See Figure 2 for a screenshot of the prototypes.
FIGURE 2.
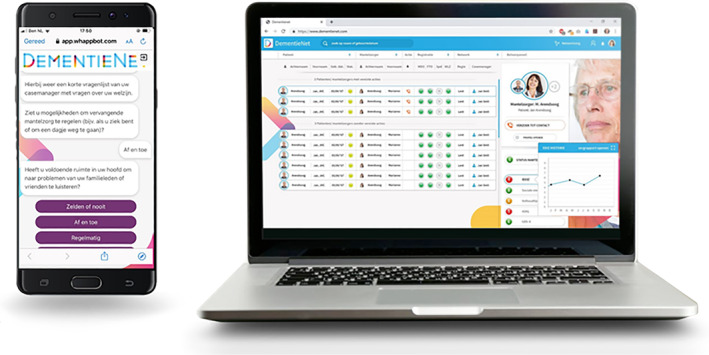
Screenshots of the questionnaire for informal caregivers and the dashboard for case managers.
3.2. Testing
3.2.1. Participant characteristics pilot test
Thirteen informal caregivers and eight case managers participated, the majority was female. Half of the informal caregivers were caring for their spouse and the other half for one of their parents. Table 3 provides an overview of the participant characteristics. All informal caregivers completed at least 95% of the weekly digital monitoring assessment.
TABLE 3.
Participant characteristics of the pilot test
| Informal caregivers (N = 13) | Case managers (N = 8) | |
|---|---|---|
| Gender, n | ||
| Male | 2 | 1 |
| Female | 11 | 7 |
| Age in years, mean (±SD) | 62.2 (±12.6) | 47 (±12.2) |
| Relation to person with dementia, n | ||
| Daughter/son | 7 | |
| Spouse | 6 | |
| Time in years, mean (±SD) | ||
| As informal caregiver | 4.8 (±3.0)* | ‐ |
| As case manager | ‐ | 5.5 (±4.8) |
Abbreviation: SD, standard deviation.
*N = 9.
3.2.2. 5. Pilot test
Eleven categories and four themes emerged from the data, which are presented in Table 4.
TABLE 4.
Themes and categories related to the use of the REMIND‐tool by case managers and informal caregivers
| Themes | Categories |
|---|---|
| Usability | Training |
| Ease of use | |
| Frequency of use | |
| Benefits and concerns monitoring | Insights by monitoring |
| Outcome monitoring | |
| Benefits and concerns assessment | Awareness and self‐reflection |
| Relevance questions | |
| Target group | |
| Future use | Future use |
| Satisfaction | |
| Suggestions for improvement |
Theme 1: Usability
Most informal caregivers and case managers did not encounter any difficulties regarding the usability of the monitor, the system was easy to use with a clear lay‐out as was the two‐factor authentication security process. Some case managers indicated that registering was difficult, due to their lack of digital skills, and for some informal caregivers, the digital aspect is still too difficult.
The majority of informal caregivers considered the frequency of the assessment (every week) as sufficient and not burdensome. “The frequency is good. Once a week is easy to oversee. If you ask questions about your emotions, then once a month is a very long period” (IC12). Some informal caregivers would prefer a larger time interval between the assessments (e.g. once per 2 weeks or monthly), as their situation was stable, and answers did not differ between the weekly intervals. Case managers mentioned that they sometimes forgot about this tool, because in this small‐scale pilot they had only one or two informal caregivers using it.
Theme 2: Benefits and concerns monitoring
All case managers recognized the potential of digital monitoring, although not all case managers obtained additional insights during the pilot period. They said that the tool could be of added value in the future, when used for a longer period of time. Case managers experienced that time is needed to visualize a trend, which is necessary for intervening.
Some case managers obtained new insights using the tool. One case manager noticed positive effects in the visualized wellbeing data the next few weeks after additional support. “In the next few weeks it was visible, the scores regarding overburden were different” (CM5).
Another case manager thought that a specific caregiver situation was very stable, however the tool revealed several stressful situations in the past week. Several case managers mentioned the tool's ability to provide information that is not mentioned during a regular visit. Informal caregivers confirmed this: when they did not want to express their feelings of burden in front of their loved one, this tool was considered a safe space to do so.
Some case managers pointed out they intervened after checking their dashboard by making a phone call or talking about the results in their next meeting. However, not all case managers acted on the results, they said they needed directions in when and how to intervene.
The feeling of being monitored by a case manager was described as comforting by informal caregivers. “If someone is keeping an eye on you that is a nice feeling” (IC9). Case managers also acknowledged this: “Personally, I think that an informal caregiver appreciates the feeling that we [the case managers] monitor the situation and that they will be contacted to check if everything is all right.” (CM7). Case managers emphasized it is important to let informal caregivers know that you have seen the results of the self‐assessment. Some informal caregivers also wondered if their case manager was checking the results, as they received little feedback. Case managers expressed that their lack of reaction to the answers could lead to a decline in informal caregivers' engagement with REMIND.
Theme 3: Benefits and concerns assessment
The majority of the informal caregivers appreciated the self‐reflection induced by REMIND. They explained that by filling‐in the weekly assessments they took a moment to reflect on the past week and it also led to insights into the burden of the caregiving. “You take a moment to reflect on the situation. What are the effects on me? And because of that monitor I take some time to reflect on it.” (IC1). One informal caregiver found it desirable to see the previous answers to gain even more insight into their own situation. Case managers indicated that some informal caregivers could benefit from the tool but were not willing to use it because monitoring was too confronting for them.
Informal caregivers perceived the tool as a valuable instrument to provide their case manager with information about their wellbeing, particularly information that was not discussed during a regular home visit.
The current questions were mainly applicable to spouses of the person with dementia, according to the care‐providing children. Informal caregivers also perceived too little variation in the weekly questions. “It (the questions) provides a general picture… it is not very specific.” (IC7). It was frequently mentioned that tailor‐made questions are essential for informal caregivers to experience the relevance also on the long term. Users mentioned that tailor‐made questions can make the tool applicable for a broad range of target groups, for example, for different caregiver roles and for caregiving outside dementia. “I do not think that there is a special target group, I think it could be applicable for everyone.” (CM2).
Theme 4: Future use
The majority of users was willing to keep using the tool after the pilot. The benefits of the tool were recognized by the users and all of them would recommend the tool to other informal caregivers and case managers.
Essential improvement suggested by users was an open text field for explanation and additional comments. Informal caregivers would appreciate some tips and tricks to deal with their loved one with dementia.
Case managers would like to receive a notification when new assessments are completed or when wellbeing decreases below a certain threshold. Almost half of the case managers mentioned that they would like this tool to be integrated within already existing system they use in daily practice.
4. DISCUSSION
In this study, we used co‐creation to develop a tool to monitor wellbeing of informal caregivers of persons with dementia. Such a tool was considered essential by end‐users as informal caregivers mentioned to find it hard to acknowledge their caregiver burden, while case managers acknowledged to have difficulty recognizing the level of burden in time. The developed REMIND tool was perceived as user‐friendly and as an addition to regular care. Completing a weekly assessment was not perceived as burdensome by informal caregivers. Some case managers had difficulties acting upon the results, whereas others almost automatically included the outcomes in their routine. Overall, the tool increased informal caregivers' self‐reflection and insight into their caregiving burden and provided case managers with better insight into informal caregivers' wellbeing. However, several suggestions to improve adherence were mentioned, including more tailor‐made questions, open text field and providing tips and tricks for informal caregivers and add notifications for case managers.
The end‐user meetings in our study showed that informal caregiver wellbeing fluctuates and can even differ per day which was found before in the context of dementia. 15 Therefore, our study focused on continuous monitoring of the wellbeing of informal caregivers in order to facilitate timely, tailored interventions. Our study showed that the concept of monitoring informal caregivers' wellbeing has potential to prevent and manage overburden by offering timely support. Previous studies have investigated combined web‐based interventions mainly using educational/informational resources, and peer support. They found positive effects on distress, perceived burden and thus overall wellbeing, although the level of evidence is low and available studies lack methodological quality. 16 , 44 , 45 , 46 A combined intervention including monitoring did find similar results. 47
As the current level of evidence of monitoring interventions is low, 46 there is an urgent need for objective measures to evaluate differences in wellbeing as a result of these tools. Literature suggests to use standardized questionnaires to assess the effects of these interventions. 12 , 44 , 48 However, as informal caregivers in our study mentioned that their wellbeing fluctuates a lot, the validity of single of before‐and‐after measurements may be limited. Future studies should compare these measurements with frequent monitoring. Possibly, we should consider other outcomes to assess effects of monitoring interventions such as variability of resilience and wellbeing or the ability to bounce back after case manager support.
REMIND was said to improve self‐reflection among informal caregivers. This is a potentially important result, since literature showed that providing adequate support can also be hindered by the fact that informal caregivers are not always aware of their own situation and do not ask for support. 7 In this study, we ran into a phenomenon described before: some informal caregivers were afraid of being confronted with their caregiver burden and declined participation in the study. 49 This was unfortunate as the involved case managers expected this group to especially benefit from such a tool. Adherence to REMIND was high among all participating informal caregivers. Case managers however used REMIND less frequently, which is probably caused by the limited number of informal caregivers that used the tool in this pilot study. This prevented REMIND from becoming part of their daily practice routine. Including notifications may stimulate its use and help case managers to react in a timely manner. 30
Long‐term use of REMIND may be a challenge especially for informal caregivers without an urgent request for help because they are caring for persons with an early stage of dementia. A strategy mentioned to keep informal caregivers engaged was including tips and tricks to the tool (e.g. information resources or possibilities for support groups). Previous studies also demonstrated the potential of a multi‐component web‐based interventions for improving wellbeing of informal caregivers of people with dementia. 46 , 50 , 51 , 52
4.1. Strengths & limitations
A major strength of this study is the co‐creation during the developing phase by using a human centered design methodology. Informal caregivers and professionals with diverse backgrounds were included in this development phase, which has led to a concept fitting to the needs and wishes of a variety of the end‐users. 30 , 53 , 54 Another strength of this study is the diverse group of users that tested the tool, for example, caregiver spouses versus children and older versus younger case managers. This resulted in a heterogeneous perspective regarding the concept of this monitoring tool.
The users were interviewed by an independent researcher, which limits information bias and socially desirable answers. Additionally, during thematic analysis multiple researchers discussed and interpreted the results (investigator triangulation) which adds to the credibility of our findings.
A limitation is that we had to use convenience sampling due to difficulties with recruiting case managers and informal caregivers during the COVID pandemic. As a result, case managers approached more digitally skilled informal caregivers. Ideally, we would have used purposive sampling for inclusion of both case managers and informal caregivers. Moreover, we did not explicitly assess whether the participating informal caregivers were experiencing low or heavy burden. This should be taken into account during a follow‐up study. We did reach data saturation and are therefore confident that we included all relevant themes, one should therefore be cautious when interpreting these results, as they may not represent the entire population of informal caregivers.
4.2. Implications for practice and research
Our pilot study identified essential features that could be included in the next version of REMIND, such as adding notifications for case managers (in order to react in a timely manner) and making the questions more tailor‐made for informal caregivers (by making them role specific, e.g. spouse vs. child). 30 Including tips and tricks for informal caregivers can stimulate continuous engagement with the tool. After adjusting REMIND according to these practical suggestions, a larger and longer follow‐up study is needed to determine if REMIND works on a larger scale to improve our understanding of the tool's working and its quantitative effects on informal caregivers' burden. Thereafter the final step will be to perform an effect evaluation using an RCT design to identify the long‐term effect on informal caregivers' wellbeing and resilience and consequently acute admissions of their relative with dementia.
Digital solutions frequently fail to reach the implementation stage 55 ; co‐creation might be a crucial strategy to overcome this. Using co‐creation, we were able to develop a tool that suits the wishes and needs of informal caregivers and professionals. Various definitions are used for human centered design methods including co‐creation, more unified guidelines and evaluation methods may facilitate for the increased use of these co‐creative methods. 54
Lastly and very relevant today, the tool developed for this study also offers possibilities in dealing with the COVID regulations. During social periods of mandatory social distancing, digital monitoring can be a useful tool to remain in contact with each other. 16 , 30 , 44 Especially, since caregiving in COVID time is even more burdensome and reducing the caregiver burden is essential to maintain informal caregivers mental health. 44
5. CONCLUSION
A co‐creation approach resulted in REMIND, a digital well‐being and resilience monitor for informal caregivers of persons with dementia, consisting of a weekly questionnaire and information dashboard for caregivers and case managers respectively. REMIND was considered easy to use and it increased informal caregivers' self‐reflection and insight into their burden. Case managers reported better insight into caregivers' wellbeing which facilitated opportunities for earlier intervening. A future long‐term follow‐up study is warranted in order to evaluate the effectiveness and efficacy of REMIND in preventing overburden of informal caregivers and resulting crises in people with dementia.
AUTHOR CONTRIBUTIONS
Dorien L. Oostra, Marieke Perry and Minke S. Nieuwboer conceptualized the study. Dorien L. Oostra wrote the first version of the manuscript. Dorien L. Oostra and Wouter L. Vos initially coded the interviews and all authors contributed to the interpretation of the study results. All the authors critically reviewed and contributed to the final draft of the manuscript. Dorien L. Oostra submitted the paper.
CONFLICT OF INTEREST
None to declare.
ETHICS STATEMENT
The study was conducted according to the principles of the Declaration of Helsinki (2013). The research ethics committee of the Radboud university medical center stated that the study did not fall within the remit of the Medical Research Involving Human Subjects Act (WMO).
Supporting information
Supporting Information S1
ACKNOWLEDGMENT
The authors would like to thank Irma Maassen for interviewing the participants. The authors would like to thank all caregivers and professionals who participated in this study. The authors thank Medworq for their assistance with developing the tool. This work was supported by the Netherlands Organisation for Health Research and Development (ZonMw) under Grant number 733050841 and supported by the Stoffels‐Hornstra foundation.
Oostra DL, Vos WL, Olde Rikkert MGM, Nieuwboer MS, Perry M. Digital resilience monitoring of informal caregivers of persons with dementia for early detection of overburden: development and pilot testing. Int J Geriatr Psychiatry. 2023;e5869. 10.1002/gps.5869
DATA AVAILABILITY STATEMENT
Data consists of qualitative interviews in Dutch. Data is available upon reasonable request from the corresponding author.
REFERENCES
- 1. Francke A, Heide I, Bruin S, et al. Een samenhangend beeld van dementie en dementiezorg: kerncijfers, behoeften, aanbod en impact. Themarapportage van de Staat van Volksgezondheid en Zorg; 2018. [Google Scholar]
- 2. Wimo A, von Strauss E, Nordberg G, Sassi F, Johansson L. Time spent on informal and formal care giving for persons with dementia in Sweden. Health Pol. 2002;61(3):255‐11. 10.1016/s0168-8510(02)00010-6 [DOI] [PubMed] [Google Scholar]
- 3. Chiao CY, Wu HS, Hsiao CY. Caregiver burden for informal caregivers of patients with dementia: a systematic review. Int Nurs Rev. 2015;62(3):340‐350. 10.1111/inr.12194 [DOI] [PubMed] [Google Scholar]
- 4. Heide I, Veer A, Buuse S, Francke A. Dementiemonitor Mantelzorg 2020. Mantelzorgers over belasting, ondersteuning, zorg en de impact van mantelzorg op hun leven; 2020.
- 5. Baumgarten M, Battista RN, Infante‐Rivard C, Hanley JA, Becker R, Gauthier S. The psychological and physical health of family members caring for an elderly person with dementia. J Clin Epidemiol. 1992;45(1):61‐70. 10.1016/0895-4356(92)90189-t [DOI] [PubMed] [Google Scholar]
- 6. Butcher HK, Holkup PA, Buckwalter KC. The experience of caring for a family member with Alzheimer's disease. West J Nurs Res. 2001;23(1):33‐55. 10.1177/019394590102300104 [DOI] [PubMed] [Google Scholar]
- 7. Brodaty H, Donkin M. Family caregivers of people with dementia. Dialogues Clin Neurosci. 2009;11(2):217‐228. 10.31887/dcns.2009.11.2/hbrodaty [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sadak T, Zdon SF, Ishado E, Zaslavsky O, Borson S. Potentially preventable hospitalizations in dementia: family caregiver experiences. Int Psychogeriatrics. 2017;29(7):1201‐1211. 10.1017/S1041610217000217 [DOI] [PubMed] [Google Scholar]
- 9. Ledgerd R, Hoe J, Hoare Z, et al. Identifying the causes, prevention and management of crises in dementia. An online survey of stakeholders. Int J Geriatr Psychiatr. 2016;31(6):638‐647. 10.1002/gps.4371 [DOI] [PubMed] [Google Scholar]
- 10. Dias R, Santos RL, Sousa MF, et al. Resilience of caregivers of people with dementia: a systematic review of biological and psychosocial determinants. Trends Psychiatry Psychother. 2015;37(1):12‐19. 10.1590/2237-6089-2014-0032 [DOI] [PubMed] [Google Scholar]
- 11. Rosa RDL, Simões‐Neto JP, Santos RL, et al. Caregivers' resilience in mild and moderate Alzheimer's disease. Aging Ment Health. 2020;24(2):250‐258. 10.1080/13607863.2018.1533520 [DOI] [PubMed] [Google Scholar]
- 12. Joling KJ, Windle G, Dröes R.‐M, Huisman M, Hertogh CMM, Woods RT. What are the essential features of resilience for informal caregivers of people living with dementia? A Delphi consensus examination. Aging Ment Health. 2017;21(5):509‐517. 10.1080/13607863.2015.1124836 [DOI] [PubMed] [Google Scholar]
- 13. Toot S, Devine M, Akporobaro A, Orrell M. Causes of hospital admission for people with dementia: a systematic review and meta‐analysis. J Am Med Dir Assoc. 2013;14(7):463‐470. 10.1016/j.jamda.2013.01.011 [DOI] [PubMed] [Google Scholar]
- 14. Afonso‐Argilés FJ, Meyer G, Stephan A, et al. Emergency department and hospital admissions among people with dementia living at home or in nursing homes: results of the European RightTimePlaceCare project on their frequency, associated factors and costs. BMC Geriatr. 2020;20(1):1‐13. 10.1186/s12877-020-01835-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pihet S, Passini CM, Eicher M. Good and bad days: fluctuations in the burden of informal dementia caregivers, an experience sampling study. Nurs Res. 2017;66(6):421‐431. 10.1097/NNR.0000000000000243 [DOI] [PubMed] [Google Scholar]
- 16. Deeken F, Rezo A, Hinz M, Discher R, Rapp MA. Evaluation of technology‐based interventions for informal caregivers of patients with dementia—a meta‐analysis of randomized controlled trials. Am J Geriatr Psychiatr. 2019;27(4):426‐445. 10.1016/j.jagp.2018.12.003 [DOI] [PubMed] [Google Scholar]
- 17. Allen AP, Buckley MM, Cryan JF, et al. Informal caregiving for dementia patients: the contribution of patient characteristics and behaviours to caregiver burden. Age ageing. 2020;49(1):52‐56. 10.1093/ageing/afz128 [DOI] [PubMed] [Google Scholar]
- 18. Sherwood PR, Given CW, Given BA, Von Eye A. Caregiver burden and depressive symptoms: analysis of common outcomes in caregivers of elderly patients. J Aging Health. 2005;17(2):125‐147. 10.1177/0898264304274179 [DOI] [PubMed] [Google Scholar]
- 19. Wrede C, Braakman‐Jansen A, van Gemert‐Pijnen L. Requirements for unobtrusive monitoring to support home‐based dementia care: qualitative study among formal and informal caregivers. Original paper. JMIR Aging. 2021;4(2):e26875. 10.2196/26875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bischoff EW, Akkermans R, Bourbeau J, van Weel C, Vercoulen JH, Schermer TR. Comprehensive self management and routine monitoring in chronic obstructive pulmonary disease patients in general practice: randomised controlled trial. BMJ. 2012;345:e7642. 10.1136/bmj.e7642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bartels SL, van Knippenberg RJ, Viechtbauer W, et al. Intervention mechanisms of an experience sampling intervention for spousal carers of people with dementia: a secondary analysis using momentary data. Aging Ment Health. 2020;26(2):1‐9. 10.1080/13607863.2020.1857692 [DOI] [PubMed] [Google Scholar]
- 22. Sanders EB‐N, Stappers PJ. Co‐creation and the new landscapes of design. CoDesign. 2008;4(1):5‐18. 10.1080/15710880701875068 [DOI] [Google Scholar]
- 23. Palumbo R. Contextualizing co‐production of health care: a systematic literature review. Int J Public Sect Manag. 2016;29(1):72‐90. 10.1108/Ijpsm-07-2015-0125 [DOI] [Google Scholar]
- 24. Flood M, Ennis M, Ludlow A, et al. Research methods from human‐centered design: potential applications in pharmacy and health services research. Res Soc Adm Pharm. 2021;17(12):2036‐2043. 10.1016/j.sapharm.2021.06.015 [DOI] [PubMed] [Google Scholar]
- 25. Melles M, Albayrak A, Goossens R. Innovating health care: key characteristics of human‐centered design. Int J Qual Health Care. 2021;33(Supplement_1):37‐44. 10.1093/intqhc/mzaa127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Standard d:school . Design Thinking Bootleg; 2021. Accessed August 18, 2021. https://dschool.stanford.edu/resources/design‐thinking‐bootleg
- 27. Nieuwboer MS, Richters A, van der Marck MA. Triple aim improvement for individuals, services and society in dementia care: the DementiaNet collaborative care approach. Z Gerontol Geriatr. 2017;50(Suppl 2):78‐83. Dreifache Verbesserung der Ziele in der Demenzversorgung fur Individuen, Gesundheitsdienstleister und die Gesellschaft: Die netzwerkbasierte Versorgung durch DementiaNet. 10.1007/s00391-017-1196-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Richters A, Nieuwboer MS, Olde Rikkert MGM, Melis RJF, Perry M, van der Marck MA. Longitudinal multiple case study on effectiveness of network‐based dementia care towards more integration, quality of care, and collaboration in primary care. PLoS One. 2018;13(6):e0198811. 10.1371/journal.pone.0198811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Barambones J, Moral C, Ferre X, Villalba‐Mora E. A Scrum‐Based Development Process to Support Co‐creation with Elders in the eHealth Domain. Springer; 2020:105‐117. [Google Scholar]
- 30. Schaller S, Marinova‐Schmidt V, Setzer M, et al. Usefulness of a tailored eHealth service for informal caregivers and professionals in the dementia treatment and care setting: the eHealthMonitor dementia portal. JMIR Res Protoc. 2016;5(2):e4354. 10.2196/resprot.4354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107‐115. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 32. Moser A, Korstjens I. Series: practical guidance to qualitative research. Part 3: sampling, data collection and analysis. Eur J Gen Pract. 2018;24(1):9‐18. 10.1080/13814788.2017.1375091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Given LM. 100 Questions (And Answers) about Qualitative Research. SAGE publications; 2015. [Google Scholar]
- 34. Ong HL, Vaingankar JA, Abdin E, et al. Resilience and burden in caregivers of older adults: moderating and mediating effects of perceived social support. BMC Psychiatr. 2018;18(1):1‐9. 10.1186/s12888-018-1616-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Richters A, Olde Rikkert MG, van Exel NJ, Melis RJ, van der Marck MA. Perseverance time of informal caregivers for institutionalized elderly: construct validity and test‐retest reliability of a single‐question instrument. J Am Med Dir Assoc. 2016;17(8):761‐762. 10.1016/j.jamda.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 36. Pot A, Dyck R, Deeg D. Ervaren druk door informele zorg‐Constructie van een schaal. Tijdschr Gerontol Geriatr. 1995;26(5):214‐219. [PubMed] [Google Scholar]
- 37. Eijk L, Kempen G, Sonderen F. Een korte schaal voor het meten van sociale steun bij ouderen: de SSL12‐I. Tijdschr Gerontol Geriatr. 1994;25(5):192‐196. [PubMed] [Google Scholar]
- 38. Santoso AM, Lutomski JE, Hofman CS, et al. Development of a patient‐reported outcome measure for geriatric care: the older persons and informal caregivers survey short form. Value Health. 2018;21(10):1198‐1204. 10.1016/j.jval.2018.02.011 [DOI] [PubMed] [Google Scholar]
- 39. Jongenelis K, Gerritsen DL, Pot AM, et al. Construction and validation of a patient‐ and user‐friendly nursing home version of the Geriatric Depression Scale. Int J Geriatr Psychiatr. 2007;22(9):837‐842. 10.1002/gps.1748 [DOI] [PubMed] [Google Scholar]
- 40. Richters A, Melis RJ, Olde Rikkert MG, van der Marck MA. The international dementia alliance instrument for feasible and valid staging of individuals with dementia by informal caregivers. J Am Geriatr Soc. 2016;64(8):1674‐1678. 10.1111/jgs.14205 [DOI] [PubMed] [Google Scholar]
- 41. Oostra DL, Nieuwboer MS, Rikkert MGO, Perry M. Development and pilot testing of quality improvement indicators for integrated primary dementia care. BMJ Open Qual. 2020;9(2):e000916. 10.1136/bmjoq-2020-000916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194‐200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- 43. Vernooij‐Dassen MJ, Felling AJ, Brummelkamp E, Dauzenberg MG, van den Bos GA, Grol R. Assessment of caregiver's competence in dealing with the burden of caregiving for a dementia patient: a Short Sense of Competence Questionnaire (SSCQ) suitable for clinical practice. J Am Geriatr Soc. 1999;47(2):256‐257. 10.1111/j.1532-5415.1999.tb04588.x [DOI] [PubMed] [Google Scholar]
- 44. Sitges‐Maciá E, Bonete‐López B, Sánchez‐Cabaco A, Oltra‐Cucarella J. Effects of e‐Health training and social support interventions for informal caregivers of people with dementia—a narrative review. Int J Environ Res Publ Health. 2021;18(15):7728. 10.3390/ijerph18157728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fowler‐Davis S, Barnett D, Kelley J, Curtis D. Potential for digital monitoring to enhance wellbeing at home for people with mild dementia and their family carers. J Alzheim Dis. 2020;73(3):867‐872. 10.3233/Jad-190844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Boots L, de Vugt ME, Van Knippenberg R, Kempen G, Verhey F. A systematic review of Internet‐based supportive interventions for caregivers of patients with dementia. Int J Geriatr Psychiatr. 2014;29(4):331‐344. 10.1002/gps.4016 [DOI] [PubMed] [Google Scholar]
- 47. Torkamani M, McDonald L, Aguayo IS, et al. A randomized controlled pilot study to evaluate a technology platform for the assisted living of people with dementia and their carers. J Alzheim Dis. 2014;41(2):515‐523. 10.3233/Jad-132156 [DOI] [PubMed] [Google Scholar]
- 48. Lorca‐Cabrera J, Grau C, Martí‐Arques R, Raigal‐Aran L, Falcó‐Pegueroles A, Albacar‐Riobóo N. Effectiveness of health web‐based and mobile app‐based interventions designed to improve informal caregiver's well‐being and quality of life: a systematic review. Int J Med Inf. 2020;134:104003. 10.1016/j.ijmedinf.2019.104003 [DOI] [PubMed] [Google Scholar]
- 49. Dam AE, Christie HL, Smeets CM, van Boxtel MP, Verhey FR, de Vugt ME. Process evaluation of a social support platform ‘Inlife’ for caregivers of people with dementia. Internet Interv. 2019;15:18‐27. 10.1016/j.invent.2018.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hopwood J, Walker N, McDonagh L, et al. Internet‐based interventions aimed at supporting family caregivers of people with dementia: systematic review. Review. J Med Internet Res. 2018;20(6):e216. 10.2196/jmir.9548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kajiyama B, Thompson LW, Eto‐Iwase T, et al. Exploring the effectiveness of an Internet‐based program for reducing caregiver distress using the iCare Stress Management e‐Training Program. Aging Ment Health. 2013;17(5):544‐554. 10.1080/13607863.2013.775641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zwaanswijk M, Peeters JM van Beek AP, Meerveld JH, Francke AL. Informal caregivers of people with dementia: problems, needs and support in the initial stage and in subsequent stages of dementia: a questionnaire survey. 2013;7:6‐13 (1874‐4346 (Print)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Meiland F, Hattink B, Overmars‐Marx T, et al. Participation of end users in the design of assistive technology for people with mild to severe cognitive problems; the European Rosetta project. Int Psychogeriatr. 2014;26(5):769‐779. 10.1017/S1041610214000088 [DOI] [PubMed] [Google Scholar]
- 54. Göttgens I, Oertelt‐Prigione S. The application of human‐centered design approaches in health research and innovation: a narrative review of current practices. JMIR mHealth uHealth. 2021;9(12):e28102. 10.2196/28102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Matthew‐Maich N, Harris L, Ploeg J, et al. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: a scoping review. JMIR mHealth uHealth. 2016;4(2):e5127. 10.2196/mhealth.5127 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
Data consists of qualitative interviews in Dutch. Data is available upon reasonable request from the corresponding author.


